- 1Center for Social Security Studies, Wuhan University, Wuhan, China
- 2Department of Health Policy and Management, School of Public Health, Peking University, Beijing, China
- 3Department of Health Policy and Management, Yale School of Public Health, New Haven, CT, United States
- 4Department of Anthropology, Quaid-i-Azam University, Islamabad, Pakistan
- 5Department of Anthropology, University of Washington, Seattle, WA, United States
- 6School of Insurance and Economics, University of International Business and Economics (UIBE), Beijing, China
The Coronavirus Disease (COVID) pandemic has aroused challenges to emotional well-being of the individuals. With 1,582 respondents from the Health and Retirement Survey (HRS), this study investigates the heterogeneity in older adults' vulnerability and examines the relationship between vulnerability types, aging attitudes, and emotional responses. International Positive and Negative Affect Schedule Short-form (I-PANAS-SF) and Attitudes toward own aging (ATOT) were used to assess the emotional experiences and aging attitudes, and 14 kinds of pandemic-related deprivations evaluated vulnerability of individuals. Latent class analysis (LCA) was used to explore the vulnerability types, and weighted linear regressions examined the relationship between vulnerability, aging attitudes, and emotional responses. The results showed that the proportion for individuals with mild vulnerability (MV), healthcare use vulnerability (HV), and dual vulnerability in healthcare use and financial sustainment (DVs) was 67, 22, and 11%, respectively. Older adults aged below 65, Hispanics and non-Hispanic Blacks, and those not eligible for Medicaid were more likely to have HV or DVs. The relationship between vulnerability and positive emotions (PAs) was non-significant, yet individuals with HV (beta = 0.10, standard error [SE] = 0.16) or DVs (beta = 0.09, SE = 0.28) were likely to have more negative emotions (NAs) than their mildly vulnerable counterparts. Furthermore, aging attitudes moderated the relationship between vulnerability and emotions. The salutary effect of positive aging attitudes on emotional well-being was more significant among people with DVs than those with MV (beta = 0.20, SE = 0.04 for positive responses; beta = −0.15, SE = 0.04 for negative responses). Thus, we urge more attention for vulnerable older adults in a pandemic context. Meanwhile, encouraging positive aging attitudes might be helpful for older adults to have better emotional well-being, especially for those with DVs.
Introduction
The Coronavirus Disease (COVID-19) pandemic brought substantial mental health impacts besides direct threats to the physical health of individuals. With the influences of pandemic threats, changes in routine, worries about financial loss, and loneliness during this public health upheaval, people faced multiple challenges to emotional well-being (1). Prevailing evidence indicated that emotional distress was increased in several countries (2). According to the Strength and Vulnerability Integration Model, older adults have strength in regulating emotions with a better use of attentional strategies, appraisals, and behaviors, yet with vulnerability in modulating the high and sustained levels of physiological arousal (3). Despite older adults generally having higher levels of emotional health, they might experience heightened negative emotions (NAs) when faced with acute stresses, such as the outbreak of Severe Acute Respiratory Syndrome (SARS) (4). About one-half of older adults in the hard-hit United States reported stress related to the disease, while a quarter developed negative mental health responses (5). As emotions have a great potential in affecting life satisfaction and coping strategies, a growing body of research studies tried to explore the risk and protective factors of emotional well-being in the COVID-19 context (6, 7). Individual characteristics, such as gender, age, race, the level of education, marital status, economic status, the ability of daily activities, and self-perceived health status had been intensively examined (6, 8). However, based on our information, a few studies have examined the association between emotional well-being and vulnerability among older adults.
Vulnerability is the result of a set of risks in threat exposure, threat materialization, and lack of defense to cope with the threat (9). In previous studies, the vulnerability could be evaluated either by models targeting individuals' deficiencies in the face of hazards or by models focusing on the outcomes of these risks (10). Referring to existing studies (11–14), we measure the vulnerability during COVID-19 with the risks in pandemic-related deprivations, which are rooted in older adults' deficiencies in disease prevention, healthcare utilization, financial resilience, and housekeeping capability. More detailed, in the face of highly infectious disease, declining immune function among older adults, and defective preventive strategies of their families may put individuals at increased risk of infection (11). Besides, existing studies suggest that older adults are more likely to have inadequate healthcare use and financial hardships than their younger counterparts in emergent circumstances (15–18). Moreover, they might have to deal with overwhelming chores during the pandemic because of austere hygiene challenges and disruption in housekeeping service (19). However, the vulnerability of older adults might be heterogeneous due to differential types and volumes of resources that individuals possess. People may have different levels of risk to experience the pandemic-related deprivations and might be distinguished as having single-dimensional or multiple-dimensional vulnerability. However, most existing COVID-19-related studies treated the vulnerability of older adults homogeneously (7, 20); to date, none of them have revealed the heterogeneity in the vulnerability of the older adult population.
Previous studies proposed that vulnerability during adverse events might arouse negative emotional responses (4, 21). However, researchers have reached no consensus regarding the association between vulnerability and positive emotional responses. In some studies, positive emotions (PAs) were decreased when the person had a severer vulnerability (22, 23). By contrast, other studies found no significant reduction in PAs despite the vulnerability of older adults (24, 25). Besides differences in trauma types, variation in the affective profiles of the respondents also contributed to this inconsistency. The affective profile is a psychological trait with an orthogonal structure describing individuals prone to PAs and NAs in the face of life challenges (26). Accordingly, affective profile of an individual may involve four main types: self-fulfilling, low-affective, high affective, and self-destructive. People with a self-fulfilling profile are often more energetic and optimistic and perform better in maintaining emotional well-being than the other three affective types in stressful situations (27). In addition, emotional responses during an adverse event are linked with the rumination on pandemic-related deprivations, as the Cognitive Appraisal Theory of Emotion was noted (28). In unintentional situations, positive internal schema and PAs would sustain when older adults attribute their vulnerability to external factors. Alternatively, considering the vulnerability as a result of personal inability may lead to self-depreciation and expel PAs. Nevertheless, during the COVID-19 pandemic, how older adults conceive their vulnerability may be differential across populations (14). Thus, in the current study, we examine the relationship of vulnerability with positive and negative emotional responses, thereby evaluating the emotional well-being of older adults amidst the COVID-19 threats.
Moreover, aging attitude as a cognitive pattern might moderate the relationship between vulnerability and emotional responses. The Cognitive Vulnerability-Stress Model suggests that older adults with positive aging attitudes would have better subjective well-being during adverse events (29). When confronted with risks in pandemic-related deprivations, positive aging attitudes would improve the emotional well-being via emotional and informational processing. On the one hand, self-esteem from positive aging attitudes serves as a shield against initial negative reactions, which is helpful to restrain stress-diathesis and have better use of emotion regulation strategies (30). On the other hand, positive aging attitudes would help individuals to effectively select the pandemic-related information (31). People with positive views on aging are less likely to be impacted by discriminative information against older adults, thereby conducting fewer negative ruminations (32). However, whether the association between positive aging attitudes and emotional responses vary between vulnerability types remains unclear. Theoretically, older adults experiencing fewer dimensions of insecurities may have greater self-esteem and confidence to overcome the pandemic after comparisons with their multiple-dimensional damaged counterparts (33). Such a sense of capability is intrinsically inherent with positive aging attitudes and might amplify their salutary effects on the emotional well-being. Alternatively, positive aging attitudes might also be more important for populations with multiple-dimensional vulnerability, helping to maintain positive self-images under substantial pandemic-related deprivations (34). Given the debates above, this study tries to examine the interactive effect of vulnerability and aging attitudes on the emotional well-being of older adults.
Aims and Hypotheses
This study investigates the latent vulnerability types among American older adults and examines the relationship between vulnerability type, aging attitudes, and emotional responses in COVID-19 settings. Our first hypothesis concerns the latent vulnerability types with an investigation on disease infection, delayed healthcare use, financial hardships, and overwhelming chores. This hypothesis is exploratory, assuming older adults might be distinct as having a single-dimensional or multiple-dimensional vulnerability due to differential types and volumes of resources they possess. Moreover, the socioeconomic and health characteristics of vulnerability groups would be different. Secondly, we propose that multiple-dimensional vulnerability is associated with higher levels of negative emotional responses. In contrast, the relationship between vulnerability and positive emotional responses might be negative or non-significant. Lastly, we assume that older adults with positive aging attitudes would have more positive and fewer negative emotional responses. Meanwhile, positive aging attitudes might moderate the relationship between vulnerability and emotional responses. The salutary effect of positive aging attitudes on emotional well-being might be more significant for individuals being either single- or multiple-dimensional vulnerable in the pandemic.
Materials and Methods
Study Design and Data Collection
Health and Retirement Survey (HRS) is a national longitudinal study of older Americans' health and economic situation (https://hrsonline.isr.umich.edu/). Data in this study were used from the 2020 HRS COVID-19 Project (Early, version 1.0). The COVID-19 module administrated 50% random subsample of households initially assigned to enhance the interviewing. This 50% random subsample was further split into two random samples: the first one was released to fieldwork on June 11, 2020, while the second one was on September 24, 2020. Information in this study was gained from the first random sample of 3,266 respondents, accounting for ~25% of the original HRS sample. Due to lockdowns in the pandemic, the COVID-19 Project was conducted via telephone, with a response rate of 62%. Detailed information on sampling design, survey content, and sample weights of HRS can be found elsewhere (35). After excluding persons below age 60 and who did not report emotional responses, this study included a total of 1,582 cases. All regressions were weighted using inverse probability weights to adjust for selections and non-response in the data.
The Institutional Review Board (IRB) of the University of Michigan approved the HRS survey, while the IRB of Yale University provided approval for this study. All methods were performed in accordance with the Declaration of Helsinki. As some of the older adults could not write, all respondents provided verbal consent to this survey.
Measures
Outcome Variable
Emotional responses in this study were measured with the International Positive and Negative Affect Schedule Short-form (I-PANAS-SF) (36), which includes 10 items and estimates the degree of PAs and NAs that individuals experienced in the past month. Five positive emotional responses involved active, determined, attentive, inspired, and alert, whereas five negative responses included afraid, nervous, upset, hostile, and ashamed. Older adults were invited to rate these emotional responses on a 5-point scale according to the extent to which they have felt, while higher scores referred to more intensive affectivities. The I-PANAS-SF is psychometrically acceptable across cultures (37). In the current study, the internal consistency coefficient (Cronbach's α) for PAs and NAs was 0.811, 0.776, respectively, indicating acceptable reliability of the measurement.
Independent Variables
The vulnerability was assessed with 14 items of pandemic-related deprivations rooted in older adults' deficiencies in disease prevention, healthcare utilization, financial resilience, and housekeeping capability. With references from the Sensitivity and Resilience Model and related empirical studies (11–14), this study made use of the most typical symptoms for each dimension. Disease infection of individuals and their family members exhibited older adults' vulnerability in disease prevention. Delay for surgery, prescription filling, doctor visits, dental care, and other services expressed vulnerability in healthcare utilization. Experiences of income deduction, spending growth, food shortage, missing financial dues, asking help with bills, and other hardships showed vulnerability of the individuals in financial resilience. Then, asking for help to do chores represented a vulnerability in housekeeping capacity. We invited older adults to report if they had experienced each of the 14 items during the pandemic (since April 2020), with 0 refers to no and 1 for yes. The vulnerability was calculated as a categorical variable after latent class analyses (LCA), with 0 for mild vulnerability (MV), 1 for healthcare use vulnerability (HV), and 2 for dual vulnerability in healthcare use and financial sustainment (DVs).
Aging attitudes were examined with a brief five-item unidimensional measure that compromises the Expansion: Attitudes towards own aging (ATOA) dimensions of the Philadelphia Geriatric Center (PGC) Morale Scale (38). Items from the ATOA measure included: “I have much pep as I did last year,” “I am as happy now as when I was younger,” “Things keep getting worse as I get older,” “The older I get, the more useless I feel,” and “As I get older, things are better than I thought they would be.” A 6-point response scale was used to evaluate the degree of each item. When negative items were reverse-scored, this scale captured older adults' global positive evaluation of their aging process (39). The Cronbach's α for the scale was 0.773 in this study.
Covariates
Affective profile was determined by the mean scores of positive affections and negative affections, reported throughout 2002–2018 HRS waves. In line with previous studies (26, 40), we adopted a cutoff point at 53.2% for PAs and 48.9% for NAs to identify the orthogonal structure of individuals' affections: self-fulfilling profile (high scores in PAs but low scores in NAs); low affective profile (low scores both in PAs and NAs); high affective profile (high scores both in PAs and NAs); and self-destructive profile (low scores in PAs but high scores in NAs). Other covariates in the current study comprised sex (male/female), age (below 65/65 and older), race (Hispanic/non-Hispanic White/non-Hispanic Black/others), marital status (married or partnered/uncoupled), educational level (less than high school/high school or above), household wealth (relatively poor/mid-level/rich), Medicaid eligibility (eligible/not eligible), difficulty in daily activities (none/one and more, i.e., 9 items, such as dressing, bathing, preparing hot meals, shopping for groceries, and so on), and self-reported health status (relatively poor/relatively good). These variables have been examined to associate with the emotional well-being of older adults in the United States (6, 8, 41).
Statistical Analyses
Descriptive analyses were conducted for the outcome variable, independent variables, and covariates. We used Mplus Version 7 to conduct LCA to identify unobserved clusters of individuals that respond to measured vulnerability items with a similar pattern. In this stage, robust maximum likelihood (MLR) estimators were adopted. Indicators, such as Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample size-adjusted BIC (ssaBIC), entropy, values of the Lo-Mendell-Rueben Test (LMRT), and the Bootstrap Likelihood Ratio Test (BLRT) were used for model selection. Meanwhile, we conducted bivariate analyses between the vulnerability type and socioeconomic/health variables while considering uncertainty in membership assignment (42). In the next step, class membership was assigned to each individual based on the probability and was treated as an observed variable. We used multinomial logit regressions to examine the factors associated with the vulnerability type, of which the relative risk ratio (RRR) and 95% CI were reported. In addition, Linear regressions were conducted to examine the association between the vulnerability type, aging attitudes, and emotional responses, after adjusting for a broad spectrum of covariates, such as affective profile, sex, age, race, marital status, education, household wealth, Medicaid eligibility, difficulty in daily activities, and self-reported health. Here, standardized and unstandardized coefficients, robust SE, and 95% CI were reported. All regressions were weighted using inverse probability weights, with sample weights that have corrections for emotion non-response. List-wise deletion was used to handle missing data, and all regressions were conducted in Stata Version.
Results
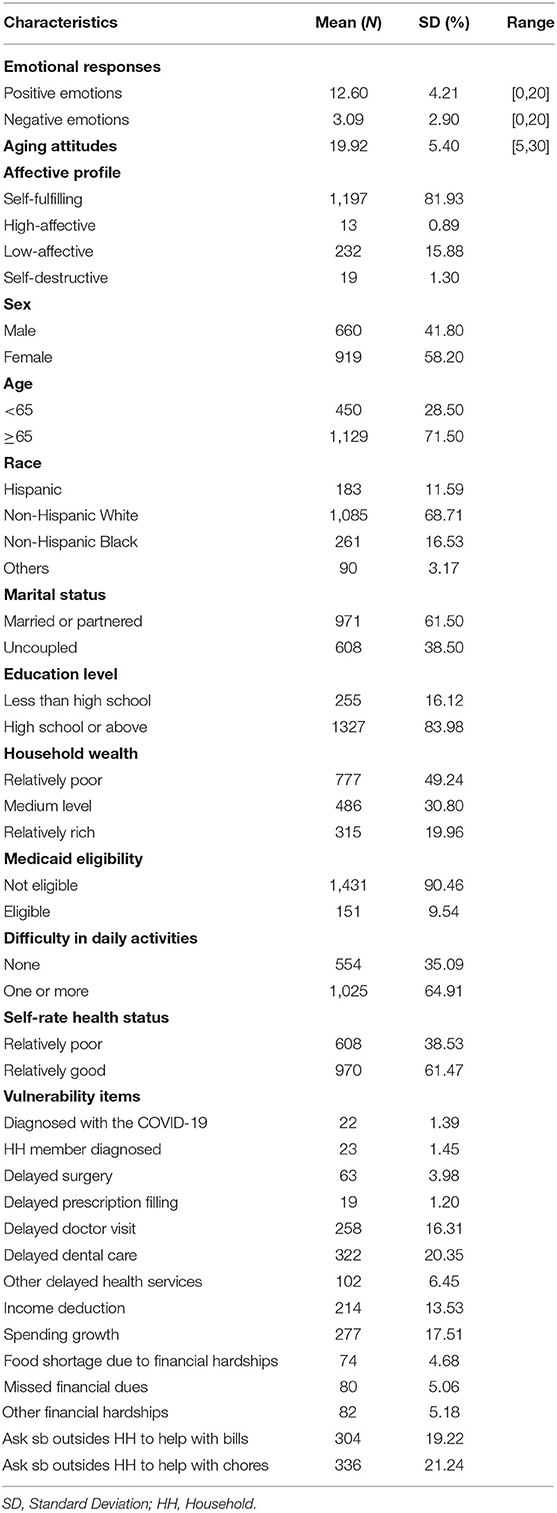
Table 1 presents the descriptive characteristics of variables in this study. Among 1,582 respondents, women (N = 919, 58.20%) and persons aged 65 years and older (N = 1,129, 71.50%) were accounted for the majority. Additionally, more than half of the respondents were non-Hispanic Whites (N = 1,085, 68.71%), married or partnered (N = 971, 61.50%), and had a high school degree or above (N = 1,327, 83.98%). Although 64.91% (N = 1,025) of the elderly had difficulty in daily activities, the proportion for self-reported poor health was only 38.53% (N = 608). In line with the high proportion of the self-fulfilling affective profile (N = 1,197, 81.93%), older adults in this study reported a relatively high level of PAs (mean = 12.60, SD = 4.21, range 0–20). By contrast, the mean score for NAs was only 3.09 (SD = 2.90, range 0–20). With regard to vulnerability items, over 20% of respondents (N = 336, 21.24%) lived with stressful chores and had to ask for help. Meanwhile, the prevalence for a delayed doctor visit and inadequate dental care was 16.31% (N = 258) and 20.35% (N = 322), respectively. Noteworthy, the most prevalent financial insecurities among older adults were income deduction (N = 214, 13.53%), spending growth (N = 277, 17.51%), and asking others to pay the bills (N = 304, 19.22%). Details are shown in Table 1.
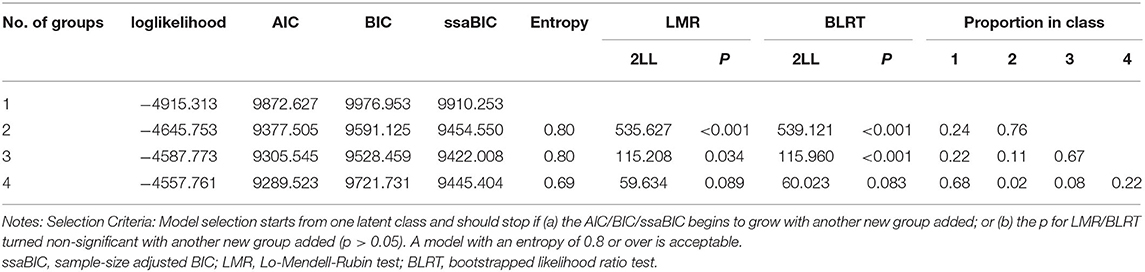
Table 2 compares the fit indices of four LCA models, from the 1-class model to the 4-class model, and decides on the 3-class model as the best. Based on the estimated probability of respondents from each latent class answering yes to vulnerability items, we further summarized the pattern of detected types as MV (including 67% respondents), HV (22% respondents), and DVs (11% respondents).
As shown in Figure 1, the probability of individuals with MV to endorse pandemic-related deprivations is almost zero except 12% for income deduction, 14% for spending growth, 19% for requesting help with bills, and 20% for requesting help with chores. Distinct from mildly vulnerable persons, older adults with HV were with significantly higher risks in delayed healthcare utilization, whose probability of experiencing delayed doctor visits and dental care were both over 60%. However, the chance for individuals from the HV group to have financial hardships was all below 10%. Meanwhile, the DVs group simultaneously demonstrated significant risks in healthcare use and financial sustainment. Apart from a 22–54% chance of having items of financial hardship, older adults with DVs had a 44% chance for delayed doctor visits and a 37% chance for delayed dental care.
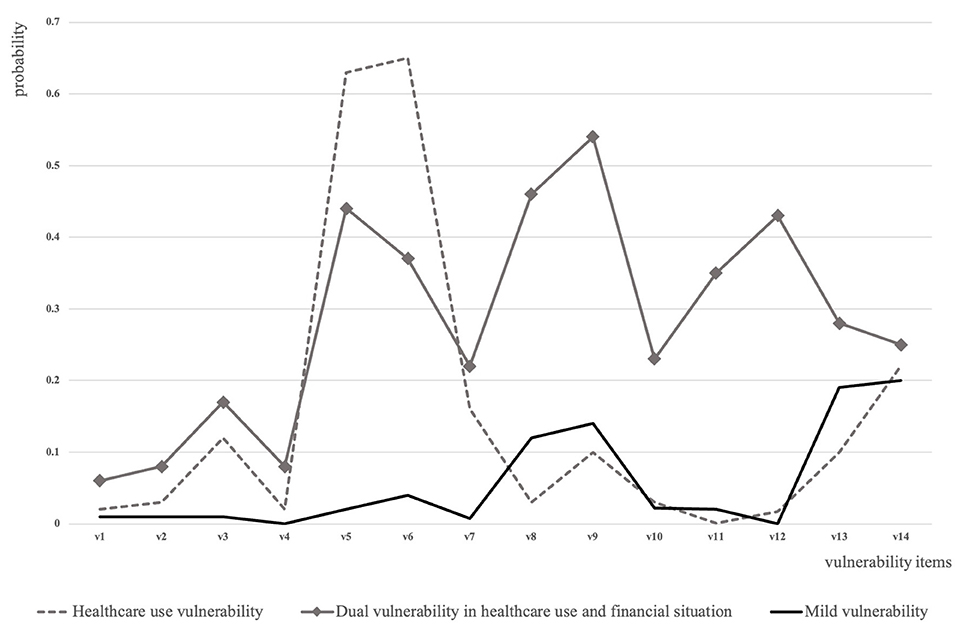
Figure 1. Vulnerability groups detected among older adults in the United States during the COVID-19 pandemic. Notes: The vulnerability type was determined by the estimated probability of respondents from each latent class answering yes to vulnerability items. The solid black line refers to the group with mild vulnerability; the dotted line refers to the group with healthcare use vulnerability; and the solid line with square marks refers to the group with dual vulnerability in healthcare use and financial sustainment. Vulnerability items are as follows: v1: had been diagnosed with the COVID-19; v2: had a household member been diagnosed with COVID-19; v3: had delayed surgery; v4: had delayed prescription filling; v5: had delayed doctor visit; v6: had delayed dental care; v7: had other delayed health services; v8: had income deduction; v9: had spending growth; v10: had food shortage due to financial hardships; v11: had missed financial dues; v12: had other financial hardships; v13: had to ask someone outsides household to help with bills; and v14: had to ask someone outsides household to help with chores.
Supplementary Table S1, Table 3 further examine the association between the vulnerability type and socioeconomic and health factors. While considering the uncertainty of membership assignment, bivariate regressions indicate that sex, marital status, age, difficulty in daily activities, affective profile, and race were significantly associated with older adults' vulnerability type (see Supplementary Table S1 for more information). With weighted multinomial regression, Table 3 demonstrates that individuals aged below 65 were more likely to have HV (RRR = 1.51, 95% CI: 1.07, 2.11) or DVs (RRR = 1.95, 95% CI: 1.05, 3.61) during the pandemic. Compared with those not eligible for Medicaid, older adults with Medicaid were less likely to have HV (RRR = 0.49, 95% CI: 0.26, 0.93). Meanwhile, Hispanics (RRR = 3.99, 95% CI: 1.89, 8.41) and non-Hispanic Blacks (RRR = 2.06, 95% CI: 1.07, 3.98) had a significantly higher risk of developing DVs. Details are presented in Table 3.
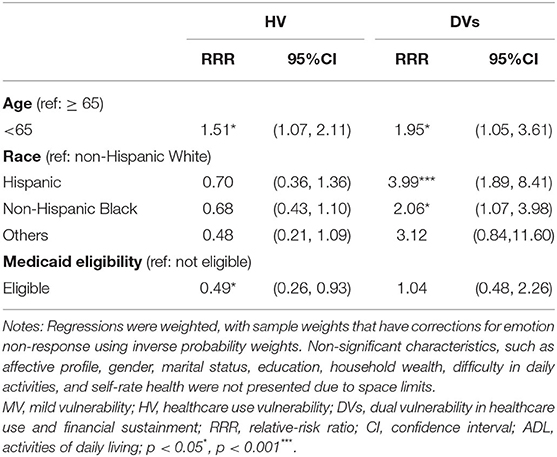
Table 3. Multinomial logit regression examining differences in risk factors across three detected latent vulnerability groups (reference group: MV, N = 1,539).
In Table 4, the relationships between vulnerability type, aging attitudes, and positive emotional responses during the COVID-19 pandemic are presented. With covariates controlled, positive attitudes toward aging were associated with a higher level of positive emotional responses among older adults (B = 0.26, beta = 0.35, 95% CI: 0.22, 0.31). Despite that Model 2 suggests no significant difference in PAs across three vulnerability groups, we found the association between positive aging attitudes and greater PAs was more significant among individuals with DVs than their mildly vulnerable counterparts (B = 0.09, beta = 0.20, 95% CI: 0.01, 0.18).
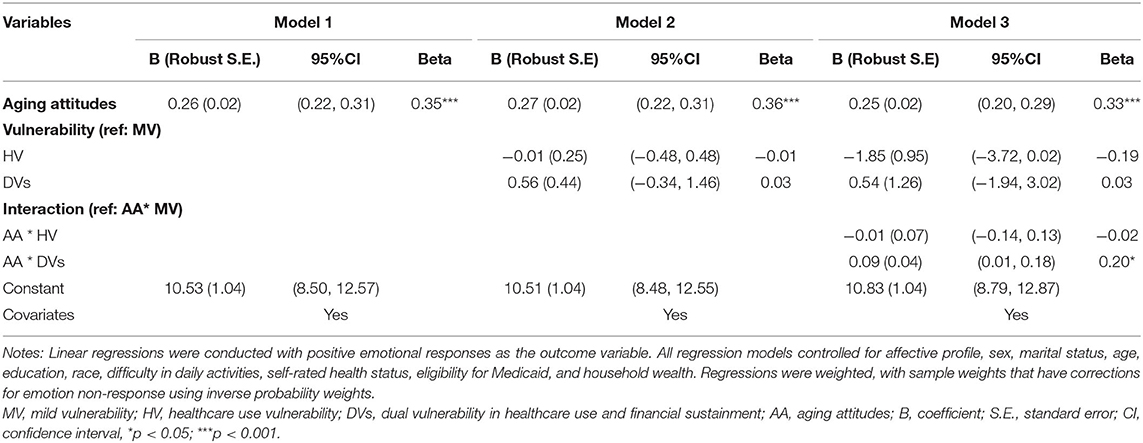
Table 4. Weighted linear regressions of the relationship between aging attitudes, vulnerability type, and positive emotional responses among older adults (N = 1,539).
Table 5 focuses on the negative emotional responses among older adults, investigating its relationship with aging attitudes and the vulnerability type. After adjusting for covariates, positive aging attitudes were associated with fewer negative emotional responses (B = −0.20, beta = −0.36, 95% CI = −0.23, −0.17). Compared with mildly vulnerable older adults, persons with HV (B = 0.74, beta = 0.10, 95% CI = 0.43, 1.06) or DVs (B = 1.05, beta = 0.09, 95% CI = 0.50, 1.59) were more likely to develop NAs. Moreover, the salutary effect of positive aging attitudes in reducing negative emotional responses was significantly stronger for older adults with DVs than those with MV (B = −0.10, beta = −0.15, 95% CI = −0.19, −0.01).
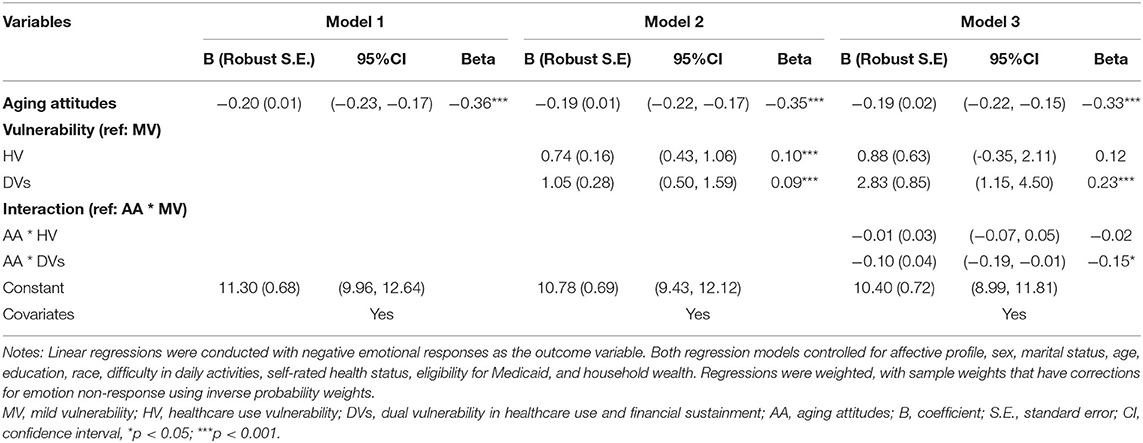
Table 5. Weighted linear regressions of the relationship between aging attitudes, vulnerability type, and negative emotional responses among older adults (N = 1,539).
Discussion
The COVID-19 pandemic has put older adults at increased risk of pandemic-related deprivations and negative emotional responses. This study reveals that older adults demonstrated three vulnerability types in the face of COVID-19 threats. The proportion of individuals with MV, HV, and DVs was 67, 22, and 11%, respectively. We found no significant difference in PAs between vulnerability types, after controlling for a broad spectrum of covariates, such as affective profile, sex, marital status, age, education, race, difficulty in daily activities, self-rated health, eligibility for Medicaid, and household wealth. However, older adults with HV or dual vulnerability were likely to have more NAs than their mildly vulnerable counterparts. In addition, positive aging attitudes were associated with better emotional well-being among older adults, and this salutary effect was more significant for individuals with dual vulnerability. Several findings of this study warrant further discussion.
First, we propose that older adults in the United States demonstrated three distinct vulnerability types during the COVID-19 pandemic. Even for people with MV, there was still a certain probability of asking for help with bills and chores. Consistent with one previous study (19), older adults with inadequate housekeeping capacity are likely to experience disrupted housekeeping services during the pandemic, thus having to request help from others with chores. Also, the risk of requesting help with bills is understandable. A previous study suggested that the compensation of employees and social benefits from the government were severely affected by COVID-19-induced restrictions (43), which are two of the most important income contributors for older adults (44). Besides the risk of stressful chores, individuals with HV demonstrated a significantly higher risk of endorsing delayed healthcare services. Theoretically, individuals with HV are more likely from states and counties endorsing the stay-at-home order, which restricts interpersonal contacts and suggests cancellation of elective care (14). Especially in hard-hit areas where health resources are massively reassigned for pandemic control, it becomes even more challenging for older adults to access non-infectious healthcare (45). Moreover, more than one in ten older adults had DVs. Possibly, individuals with dual vulnerability are those with lower socioeconomic status. On the one hand, one prior study noted that about half of the disadvantaged older adults in the United States are living without emergency savings, thereby with a significantly higher chance of experiencing financial hardships during recessions (46). Moreover, they are more likely to have increased expenditure as many of the mechanisms for navigating life on a limited budget became difficult during the pandemic (47). On the other hand, disadvantaged older adults are more likely to depend on public transportation to get healthcare services, which is at least inconvenient under the pandemic restrictions (48). Thus, we urge local governments and communities to keep a watchful eye on older adults during crises. Noteworthy, the vulnerability is more likely to be heterogeneous rather than homogenous, and a careful evaluation for older adults of their risks in trauma-related deprivations is critical before social services are conducted.
In addition, we suggest that older adults under 65 years were less likely to be mildly vulnerable, while those not eligible for Medicaid were more likely to have healthcare vulnerability, and Hispanics/non-Hispanic Blacks were prone to have dual vulnerability. In contrast with previous studies suggesting age as a risk factor of vulnerability (12, 13), we suggest that individuals aged 60–65 years were more likely to have financial hardships and inadequate healthcare services than their older counterparts. Two explanations rationalize this finding. Firstly, older adults below 65 years are more likely to be active in the labor market before the pandemic. However, they would find it difficult to reenter the workforce during the post-pandemic recession, thereby having a greater chance to experience financial hardships (1). Secondly, it is possible that individuals of older ages would ignore their physical discomforts and require lesser care and services, as they tend to have better subjective well-being and be more satisfied with life (49). Moreover, an existing study suggested that adults aged over 65 years conduct more telemedicine visits than their 55–65 years counterparts, thus at a lower risk of delaying healthcare (50). Apart from age, we also found that individuals not eligible for Medicaid are more likely to have healthcare vulnerability, as Medicaid promotes healthcare access during the pandemic (51). Furthermore, we found Hispanics and non-Hispanic Blacks are more likely to have dual vulnerability than their Whites counterparts. One recent review suggested that Hispanics and non-Hispanic Blacks experienced higher rates of infection, hospitalization, and mortality in the pandemic (52). According to Blumenshine's model (48), Hispanics and non-Hispanic Blacks depend largely on public transportation and have limited capacity to work at home, thus becoming harder to access healthcare services and sustain income during the pandemic. In a vicious cycle, they have a greater risk of infection to get a job or seek healthcare services, which intensifies the probability of inadequate healthcare use and financial hardships once individuals become infected. In a nutshell, we propose that older adults below 65 years, being Hispanics or non-Hispanic Blacks, and not eligible for Medicaid are more likely to have healthcare vulnerability or dual vulnerability during the pandemic, which is worthy of more care and services.
Third, this study reveals that the vulnerability type of older adults presented no significant relationship with PAs but was significantly associated with NAs during the pandemic. Previous evidence claimed that severe vulnerability would lead to stress and a ruined sense of self-continuity, thus reducing PAs in young adults (53). However, this study found no significant difference in PAs between older adults from different vulnerability groups. Possibly, intrinsic motivation for emotionally meaningful goals among older adults could rationalize this finding, which is examined to be helpful to sustain PAs under challenging situations (54). Often, older adults are prone to pay attention to positive stimuli over negative information during stressful events, thus being easier to develop PAs (55). However, emotional regulation strategies are harder to work on negative arousals under prolonged stress (56). With the introduction of the sense of relative deprivation (57), people with healthcare vulnerability or dual vulnerability are understandable to have a higher level of NAs. Individuals in traumatic events are prone to compare their vulnerability with others. Nevertheless, compared with mildly vulnerable counterparts, older adults with healthcare or dual vulnerability might have a sense of unfairness, which is likely to activate negative responses such as hostility and anger (58). Thus, although older adults are often more resilient in emotional well-being, their NAs should also be noted and timely intervened when individuals demonstrate healthcare or dual vulnerability in crises.
Lastly, we propose that positive aging attitudes benefited older adults' emotional well-being in the COVID-19 context, especially for individuals with DVs. As noted by prior studies, older adults have endured prevalent discrimination during the pandemic, as some young adults may blame the dramatic response of COVID-19 as an “old people problem” (59, 60). Tags, such as #BoomerRemover#, are prevalently endorsed to express the hostility toward the elderly, exacerbating social discrimination toward older adults in the pandemic settings. Often, old persons may have emotional exhaustion under ageism discrimination, yet positive aging attitudes help to promote self-appreciation and thus against negative ruminations (61). In particular, positive attitudes toward aging might be even more critical for older adults with dual vulnerability. As noted by the attribution theory (62), older adults with multiple-dimensional vulnerability are more likely to make internal attributions for their pandemic-related deprivations. Often, self-blame is associated with greater internal ageism (i.e., people feeling ashamed for their age) and more negative affections among older adults (63). However, positive aging attitudes might alleviate such internal ageism via informational and behavioral processing. On the one hand, positive aging attitudes help individuals avoid ageism information and conduct fewer negative ruminations on that (64). Also, older adults with positive aging attitudes are less likely to consider their vulnerability during the pandemic as a threat to future lives, which might lower prospective fear and worries (65). On the other hand, people with positive aging attitudes are more likely to conduct adaptative behaviors to cope with their vulnerability during the pandemic, which establishes a better sense of self-efficacy and would mitigate the internal ageism (66). Therefore, we suggest that encouraging positive aging attitudes might be a critical approach for social services to promote emotional well-being for older adults, especially those with dual vulnerability.
Strengths and Limitations
This study is among the first to explore the heterogeneity in vulnerability of the older adults during the COVID-19 pandemic. We provided novel evidence to reveal three latent groups of vulnerability and the relationship between vulnerability type, aging attitudes, and emotional responses. However, some limitations of this study should be acknowledged. First, this study reports that 1.39% of respondents were diagnosed. The lack of COVID-19 tests, especially at the beginning of the pandemic, and the potential stigma associated with the infection may contribute to the underestimation of the infection rate in this sample. Given the overstretched healthcare system and financial needs (before Medicare coverage) among infected older adults, the proportion of people with dual vulnerability might be higher in the U.S. population. Hence, it is of interest for future studies to use multiple sources of data to better represent populations who were infected with the disease. Second, based on cross-sectional data, this study cannot infer causality, although it seems plausible in the temporal sequence vulnerability and aging attitudes first, and emotional responses being the outcome. Third, there might be some confounding that was not controlled. For instance, we assumed that differences in political responses of states, territories, and counties contribute to the heterogeneity in inadequate healthcare utilization. However, residence information was lacking in this data. Lastly, the uncertainty in membership assignment was not considered in weighted regressions, despite bivariate analyses using a 3-step procedure supporting these findings.
Conclusion
This study suggests that adults aged over 60 years presented three distinct patterns of vulnerability during the pandemic. About 67% of individuals were mildly vulnerable, and more than 30% of respondents had HV or DVs. Besides, individuals not eligible for Medicaid were more likely to have healthcare vulnerability, and Hispanics and non-Hispanic Blacks were more likely to have dual vulnerability. Meanwhile, adults below 65 years were prone to have healthcare vulnerability or dual vulnerability other than MV. While older adults from different vulnerability types had no significant difference in PAs, those with HV or dual vulnerability were likely to have more NAs. Besides, positive aging attitudes were associated with more positive and fewer NAs, and this salutary effect is more significant for individuals with dual vulnerability. Thus, we urge local governments and communities to keep a watchful eye on older adults during crises, with individuals having healthcare or dual vulnerability being prioritized. In addition, encouraging positive aging attitudes might be a critical approach for social services to promote the emotional well-being of older adults, especially those with dual vulnerability.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Yale University Institutional Review Board. The patients/participants provided their verbal informed consent to participate in this study.
Author Contributions
MF carried out the statistical analysis and drafted the manuscript. JG assisted with writing the article. XC critically reviewed this article. BH, FA, and MS participated in the revision of this manuscript. QZ designed the study and revised the manuscript. All authors have read and approved the manuscript.
Funding
This study was supported by the National Social Science Fund of China (20VYJ030); the Guizhou Kong Xuetang Development Foundation; the U.S. PEPPER Center Scholar Award (P30AG021342) and an NIH/NIA grant (K01AG053408).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This study would like to thank the Health and Retirement Survey (HRS) group from the University of Michigan for conducting this survey and sharing the data.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.778084/full#supplementary-material
Abbreviations
COVID-19, Coronavirus Disease; HRS, Health and Retirement Survey; I-PANAS-SF, International Positive and Negative Affect Schedule Short-form; ATOT, Attitudes toward own aging; PGC, Philadelphia Geriatric Center; PA, Positive Affect; NA, Negative Affect; LCA, Latent Class Analysis; AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; ssaBIC, sample size-adjusted BIC; LMRT, Lo-Mendell-Rueben Test (LMRT); MV, Mild vulnerability; HV, Healthcare use vulnerability; DVs, Dual vulnerability in healthcare use and financial sustainment.
References
1. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
2. Garrett L. COVID-19: the medium is the message. Lancet. (2020) 395:942–3. doi: 10.1016/S0140-6736(20)30600-0
3. Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull. (2010) 136:1068–91. doi: 10.1037/a0021232
4. Lau ALD, Chi I, Cummins RA, Lee TMC, Chou KL, Chung LWM. The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. (2008) 12:746–60. doi: 10.1080/13607860802380607
5. Koma W, True S, Biniek JF, Cubanski J, Orgera K, Garfield R. One in Four Older Adults Report Anxiety or Depression Amid the COVID-19 Pandemic. (2020). Available online at: https://www.kff.org/medicare/issue-brief/one-in-four-older-adults-report-anxiety-or-depression-amid-the-covid-19-pandemic/ (accessed April 24, 2021).
6. Carstensen LL, Shavit YZ, Barnes JT. Age advantages in emotional experience persist even under threat from the COVID-19 pandemic. Psychol Med. (2020) 31:1374–85. doi: 10.1177/0956797620967261
7. Fingerman KL, Ng YT, Zhang S, Britt K, Colera G, Birditt KS, et al. Living alone during COVID-19: social contact and emotional well-being among older adults. J Gerontol B Psychol Sci Soc Sci. (2021) 76:e115–21. doi: 10.1093/geronb/gbaa200
8. Bui CN, Peng C, Mutchler JE, Burr JA. Race and ethnic group disparities in emotional distress among older adults during the COVID-19 pandemic. Gerontologist. (2021) 61:262–72. doi: 10.1093/geront/gnaa217
9. Perrig-Chiello P, Hutchison S, Knöpfli B. Vulnerability following a critical life event: temporary crisis or chronic distress? A psychological controversy, methodological considerations, and empirical evidence. In: Oris M, Roberts C, Joye D, Ernst Stähli M, editors. Surveying Human Vulnerabilities Across the Life Course. Life Course Research and Social Policies. New York, NY: Springer Publishing (2016). p. 87–111. doi: 10.1007/978-3-319-24157-9_4
10. Birkmann J. Measuring Vulnerability to Natural Hazards: Toward Resilient Societies (second edition). New York, NY: United Nations University Press (2016).
11. Sapountzaki K. Vulnerability management by means of resilience. Nat Hazards. (2012) 60:1267–85. doi: 10.1007/s11069-011-9908-3
12. Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. (2017) 33:293–303. doi: 10.1016/j.cger.2017.02.002
13. Schröder-Butterfill E, Marianti R. A framework for understanding old-age vulnerabilities. Ageing Soc. (2006) 26:9–35. doi: 10.1017/S0144686X05004423
14. Lee YJ. The impact of the COVID-19 pandemic on vulnerable older adults in the United States. J Gerontol Soc Work. (2020) 63:1–6. doi: 10.1080/01634372.2020.1777240
15. Crimmins EM. Age-related vulnerability to coronavirus disease 2019 (COVID-19): biological, contextual, and policy-related factors. Public Policy Aging Rep. (2020) 30:142–6. doi: 10.1093/ppar/praa023
16. Wilhelm JA, Helleringer S. Utilization of non-Ebola health care services during Ebola outbreaks: a systematic review and meta-analysis. J Glob Health. (2019) 9:010406. doi: 10.7189/jogh.09.010406
17. Choi SL, Carr D, Namkung EH. Physical disability and older adults' perceived food and economic insecurity during the COVID-19 pandemic. J Gerontol B Psychol Sci Soc Sci. (2020) 76:e249–55. doi: 10.1093/geronb/gbab162
18. D'cruz M, Banerjee D. 'An invisible human rights crisis': the marginalization of older adults during the COVID-19 pandemic - an advocacy review. Psychiatry Res. (2020) 292:113369. doi: 10.1016/j.psychres.2020.113369
19. Federman AD, Leff B, Brody AA, Lubetsky S, Siu AL, Ritchie CS, et al. Disruptions in care and support for homebound adults in home-based primary care in New York City during the COVID-19 Pandemic. Home Healthc Now. (2021) 39:211–4. doi: 10.1097/NHH.0000000000000983
20. Knepple CA, Graf AS, Hudson G, Wilson E. Age moderates perceived COVID-19 disruption on well-being. Gerontologist. (2021) 61:30–5. doi: 10.1093/geront/gnaa106
21. Bayraktar N, Dal-Yilmaz Ü. Vulnerability of elderly people in disasters: a systematic review. Turk Geriatri Dergisi. (2018) 21:467–82. doi: 10.31086/tjgeri.2018344062
22. Thomas RC, Hasher L. The influence of emotional valence on age differences in early processing and memory. Psychol Aging. (2006) 21:821–5. doi: 10.1037/0882-7974.21.4.821
23. Ebner NC, Johnson MK. Age-group differences in interference from young and older emotional faces. Cogn Emot. (2010) 24:1095–116. doi: 10.1080/02699930903128395
24. Carstensen LL, Mikels JA. At the intersection of emotion and cognition: aging and the positivity effect. Curr Dir Psychol. (2005) 14:117–21. doi: 10.1111/j.0963-7214.2005.00348.x
25. Fuller HR, Huseth-Zosel A. Lessons in resilience: initial coping among older adults during the COVID-19 pandemic. Gerontologist. (2021) 61:114–25. doi: 10.1093/geront/gnaa170
26. Norlander T, Bood SÅ, Archer T. Performance during stress: affective personality, age, and regularity of physical exercise. Soc Behav Pers. (2002) 30:495–508. doi: 10.2224/sbp.2002.30.5.495
27. Norlander T, Johansson Å, Bood SÅ. The affective personality: its relation to quality of sleep, well-being and stress. Soc Behav Pers. (2005) 33:709–22. doi: 10.2224/sbp.2005.33.7.709
28. Lazarus RS. Progress on a cognitive-motivational-relational theory of emotion. Am Psychol. (1992) 46:819–34. doi: 10.1037/0003-066X.46.8.819
29. Reichstadt J, Depp CA, Palinkas LA, Folsom DP, Jeste DV. Building blocks of successful aging: a focus group study of older adults perceived contributors to successful aging. Am J Geriatr Psychiatr. (2007) 15:194–201. doi: 10.1097/JGP.0b013e318030255f
30. Beck AT. Cognitive models of depression. In: RL Leaphy, ET, Dowd, editors. Clinical Advances in Cognitive Psychotherapy: Theory and Application. New York, NY: Springer Publishing (2002). p. 29–61.
31. Ayalon L. There is nothing new under the sun: ageism and intergenerational tension in the age of the COVID-19 outbreak. Int Psychogeriatric. (2020) 32:1221–4. doi: 10.1017/S1041610220000575
32. Hooley JM, Gotlib IH. A diathesis-stress conceptualization of expressed emotion and clinical outcome. App Prev Psycho. (2000) 9:135–51. doi: 10.1016/S0962-1849(05)80001-0
33. Chen J, Zheng K, Xia W, Wang Q, Liao Z, Zheng Y. Does inside equal outside? Relations between older adults' implicit and explicit aging attitudes and self-esteem. Front Psychol. (2012) 9:2313. doi: 10.3389/fpsyg.2018.02313
34. Bellingtier JA, Neupert SD. Negative aging attitudes predict greater reactivity to daily stressors in older adults. J Gerontol B Psychol Sci Soc Sci. (2018) 73:1155–9. doi: 10.1093/geronb/gbw086
35. Ofstedal MB, Weir DR, Chen KT, Wagner J. Updates to HRS Sample Weights. (2011). Available online at: https://hrs.isr.umich.edu/sites/default/files/biblio/dr-013.pdf (accessed October 27, 2021). doi: 10.7826/ISR-UM.06.585031.001.05.0025.2011
36. Thompson ER. Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS). J Cross-Cult Psychol. (2007) 38:227–42. doi: 10.1177/0022022106297301
37. Karim J, Weisz R, Rehman SU. International positive and negative affect schedule short-form (I-PANAS-SF): testing for factorial invariance across cultures. Proced Soc Behav Sci. (2011) 15:2016–22. doi: 10.1016/j.sbspro.2011.04.046
38. Liang J, Bollen KA. The structure of the Philadelphia Geriatric Center morale scale: a reinterpretation. Gerontology. (1983) 38:181–9. doi: 10.1093/geronj/38.2.181
39. Kim ES, Moored KD, Giasson HL, Smith J. Satisfaction with aging and use of preventive health services. Prev Med. (2014) 69:176–80. doi: 10.1016/j.ypmed.2014.09.008
40. Garcia D, Nima A al, Kjell ONE. The affective profiles, psychological well-being, and harmony: environmental mastery and self-acceptance predict the sense of a harmonious life. PeerJ. (2014) 2:e259. doi: 10.7717/peerj.259
41. de Main AS, Xie B. Social environment and mental and behavioral health outcomes in older adults: a critical review. Innov Aging. (2020) 4:467–71. doi: 10.1093/geroni/igaa057.1512
42. Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Struct Equat Model. (2014) 21:329–41. doi: 10.1080/10705511.2014.915181
43. OECD. Unprecedented Fall in OECD GDP by 9.8% in Q2 2020 (2021). Available online at: https://www.oecd.org/sdd/na/GDP-Growth-Q220.pdf (accessed October 26, 2021).
44. Lachs MS, Duke HS. Age-associated financial vulnerability: an emerging public health issue. Ann Intern Med. (2015) 163:877–8. doi: 10.7326/M15-0882
45. Cudjoe TKM, Kotwal AA. “Social Distancing” amid a crisis in social isolation and loneliness. J Am Geriatr Soc. (2020) 68:27–9. doi: 10.1111/jgs.16527
46. Dushi I, Iams HM, Trenkamp B. The importance of social security benefits to the income of the aged population. Soc Secur Bull. (2017) 77:1–12. Available online at: https://www.researchgate.net/publication/316944245_The_importance_of_social_securitity_benefits_to_the_income_of_the_aged_population/
47. Mike B, Ruth P. Pandemic Pressures Why Families on a Low Income are Spending More During Covid-19. (2021). Available online at: https://www.resolutionfoundation.org/app/uploads/2021/01/Pandemic-pressures.pdf (accessed October 27, 2021).
48. Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braveman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg Infect Dis. (2008) 14:709–15. doi: 10.3201/eid1405.071301
49. Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. (2015) 385:640–8. doi: 10.1016/S0140-6736(13)61489-0
50. Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640
51. Allen HL, Sommers BD. Medicaid and COVID-19: at the center of both health and economic crises. JAMA. (2020) 324:135–6. doi: 10.1001/jama.2020.10553
52. Mude W, Oguoma VM, Nyanhanda T, Mwanri L, Njue C. Racial disparities in COVID-19 pandemic cases, hospitalizations, and deaths: a systematic review and meta-analysis. J Glob Health. (2021) 11:050125. doi: 10.7189/jogh.11.05015
53. Fogel A. A relational perspective on the development of self and emotion. In: Bosma HA, Kunnen ES, editors. Identity and Emotion: Development Through Self-Organization. London: Cambridge University Press (2001). p. 93–119. doi: 10.1017/CBO9780511598425.009
54. Vandercammen L, Hofmans J, Theuns P. Relating specific emotions to intrinsic motivation: on the moderating role of positive and negative emotion differentiation. PLoS ONE. (2014) 9:e115396. doi: 10.1371/journal.pone.0115396
55. Bowleg L. We're not all in this together: On COVID-19, intersectionality, and structural inequality. Am J Public Health. (2020) 110:917. doi: 10.2105/AJPH.2020.305766
56. Reed AE, Chan L, Mikels JA. Meta-analysis of the age-related positivity effect: age differences in preferences for positive over negative information. Psychol Aging. (2014) 29:1–15. doi: 10.1037/a0035194
57. Barber SJ, Opitz PC, Martins B, Sakaki M, Mather M. Thinking about a limited future enhances the positivity of younger and older adults' recall: support for socioemotional selectivity theory. Mem Cognit. (2016) 44:869–82. doi: 10.3758/s13421-016-0612-0
58. Smith HJ, Pettigrew TF, Pippin GM, Bialosiewicz S. Relative deprivation: a theoretical and meta-analytic review. Pers Soc Psychol Rev. (2012) 16:203–32. doi: 10.1177/1088868311430825
59. Ayalon L, Chasteen A, Diehl M, Levy BR, Neupert SD, Rothermund K, et al. Aging in times of the COVID-19 pandemic: avoiding ageism and fostering intergenerational solidarity. aging in times of the COVID-19 pandemic: avoiding ageism and fostering intergenerational solidarity. J Gerontol B Psychol Sci Soc Sci. (2021) 18:49−52. doi: 10.1093/geronb/gbaa051
60. Calderón-Larrañaga A, Dekhtyar S, Vetrano DL, Bellander T, Fratiglioni L. COVID-19: risk accumulation among biologically and socially vulnerable older populations. Ageing Res Rev. (2020) 63:101149. doi: 10.1016/j.arr.2020.101149
61. Tornstam L. Gerotranscendence: A Developmental Theory of Positive Aging. New York, NY: Springer Publishing Company (2005).
62. Shaver KG, Drown D. On causality, responsibility, and self-blame: a theoretical note. J Pers Soc Psychol. (1986) 50:697–702 doi: 10.1037/0022-3514.50.4.697
63. Wallace LS, Chisolm DJ, Abdel-Rasoul M, DeVoe JE. Survey mode matters: adults' self-reported statistical confidence, ability to obtain health information, and perceptions of patient-health-care provider communication. J Health Psychol. (2013) 18:1036–45. doi: 10.1177/1359105312470125
64. Tarazona-Santabalbina FJ, de la Cámara de Las Heras JM, Vidán MT, García Navarro JA. Coronavirus disease 2019 (COVID-19) and ageism: a narrative review of the literature. Rev Esp Geriatr Gerontol. (2021) 56:47–53. doi: 10.1016/j.regg.2020.08.002
65. Swift HJ, Abrams D, Lamont RA, Drury L. The risks of ageism model: how ageism and negative attitudes toward age can be a barrier to active aging. Soc Issue Policy Rev. (2017) 11:195–231. doi: 10.1111/sipr.12031
Keywords: vulnerability, aging attitudes, emotion, older adults, COVID-19
Citation: Fu M, Guo J, Chen X, Han B, Ahmed F, Shahid M and Zhang Q (2022) American Older Adults in COVID-19 Times: Vulnerability Types, Aging Attitudes, and Emotional Responses. Front. Public Health 9:778084. doi: 10.3389/fpubh.2021.778084
Received: 16 September 2021; Accepted: 27 December 2021;
Published: 08 February 2022.
Edited by:
María del Mar Molero, University of Almeria, SpainReviewed by:
Rachit Sharma, Drexel University, United StatesCarlos Freire, University of A Coruña, Spain
Copyright © 2022 Fu, Guo, Chen, Han, Ahmed, Shahid and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qilin Zhang, cWlsaW56aGFuZ0B3aHUuZWR1LmNu
 Mingqi Fu
Mingqi Fu Jing Guo
Jing Guo Xi Chen3
Xi Chen3