- 1Department of Clinical Pharmacy and Pharmacy Administration, School of Pharmacy, Fudan University, Shanghai, China
- 2Department of Clinical Pharmacy, The Children's Hospital of Fudan University, Shanghai, China
Background: Self-medication of antibiotics is common in China, whereas the self-medication of other medicines is still unknown, especially for the younger children who are vulnerable to adverse drug events. The aim of this study was to estimate the prevalence of self-medication reported by parents among children under age 12 in China.
Methods: A national cross-sectional survey was conducted among parents of children under age 12 in China by using a self-administered online questionnaire. Parents were asked whether they have self-medicated their children in the past 12 months. Logistic regression analysis was performed to access the risk factors of self-medication.
Results: Eligible questionnaires were obtained from 4,608 parents. The majority of respondents were mothers aged between 30 and 39 years old who held a college degree. A total of 1,116 (or 24.21%) respondents reported self-medication in the previous year. In the logistic regression model, parents with graduate degrees were less likely to self-medicate their children [Adjusted OR (AOR) = 0.436; 95% CI = 0.296–0.641]. The odds of self-medication were associated with being a father, living in Northern China, having a child at age 6–11, even though these did not reach statistical significance.
Conclusions: Our findings indicate that self-medication are common in children under age 12, highlighting the drug safety issue in China. It seems that the educational level is the risk factors of self-medication. More targeted intervention and educational program should be implemented to improve drug safety.
Introduction
Drug safety remains a serious public health issue. The WHO estimates that about 50% of patients fail to take their medicines correctly (1). Every year, nearly nine million children aged under five die worldwide (2), a large part of which is caused by irrational drug use (2). Self-medication or self-prescription by parents is considered as one of the biggest risk factors of drug safety (3). Parental self-medication is common globally, ranging from 7 to 70% (4–8). According to a recent study, one-third of children's population in China had parental self-medication of antibiotics without consultation of physicians or healthcare providers (9). To our best knowledge, however, there is limited data on self-medication of other commonly used medications, such as cold and cough medicines, corticosteroids, and traditional Chinese medicine.
Children are still in the developmental stage, with different pharmacokinetic (PK) and pharmacodynamic (PD) characteristics. Hence, they are more vulnerable to adverse drug events compared to their adult counterparts (10). Due to limited pediatric formula available in the market (11), off-label use of medication is prevalent, ranging from 40 to 90% (12). In China, among 6,020 medicines commonly used in pediatrics, only 238 or 3.95% drugs are approved for pediatric use (13), and most of them are adult formulations with an extended use in children. In addition, the limited availability of pediatric formulations further exaggerates the issue of parental self-medication in China. Considering the adverse outcomes associated with parental self-medication (3, 14), the aim of this study was to estimate the prevalence and the associated risk factors of self-medication among children under age 12 in China.
Materials and Methods
Study Design
We employed a cross-sectional design. Parents of children under age 12 were invited to an anonymous online survey, which was available in 34 provinces, autonomous regions, and municipalities which are directly under the central government in China. The study participants were the parents of the children aged under 12 years old. The survey period was from March 2018 to November 2019. This study was approved by the Institutional Review Boards of the Children's Hospital of Fudan University. This study followed the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).
Survey Questionnaire
The questionnaire, which assessed the prevalence of self-medication use and drug related problems (DRPs), was created based on previous surveys conducted by China Population Communication Center (15). This questionnaire has been developed by an expert panel that consisted of pediatricians, pharmacists, outcomes researchers, and parents. The questionnaire included three sections. The first section asked the demographic and the socioeconomic characteristics of parents, including age, gender, education, and provinces. The second section was to access the prevalence of self-medication for their children. Parents were asked whether their children had been in self-medication in the past 12 months. For those who reported a self-medication for their children, we collected information on the drug classes they commonly used for the self-medication.
Participant Recruitment
To reach a representative sample of parents, following the previous research (16), we first selected 34 research coordinators to be the original deliverers who invited the parents in their communities to participate. Parents with children aged under 12 were invited to participate. Then, we sent out requests via WeChat private messages, including a link to the web-based questionnaire through an internet survey portal (https://www.wjx.cn/). As one of the largest social media platforms in China, WeChat has been used previously to distribute online surveys (17–19). To avoid multiple responses from the same individuals, each WeChat account was only allowed to answer the questionnaire once. A total of 5,189 parents were invited and 4,608 of them completed the survey. The response rate was 88.80%.
The accomplished questionnaire was considered as eligible if (1) all the questions were answered, (2) self-reported age of children was <12, and (3) they were parents who take care of their children. We also excluded questionnaire with the same answers to different questions to ensure the quality of survey.
Data Analysis
For descriptive analysis, frequency distributions (e.g., percentage) were estimated for categorical variables. Fisher's exact test was used to compare the difference between categorical variables. We also constructed a logistic regression model to examine the potential predictors of self-medication. Both crude and adjusted OR were estimated. Statistical significance was determined at a-level of 0.05. All statistical analyses were performed using SAS 9.4.
Results
Characteristics of Respondents
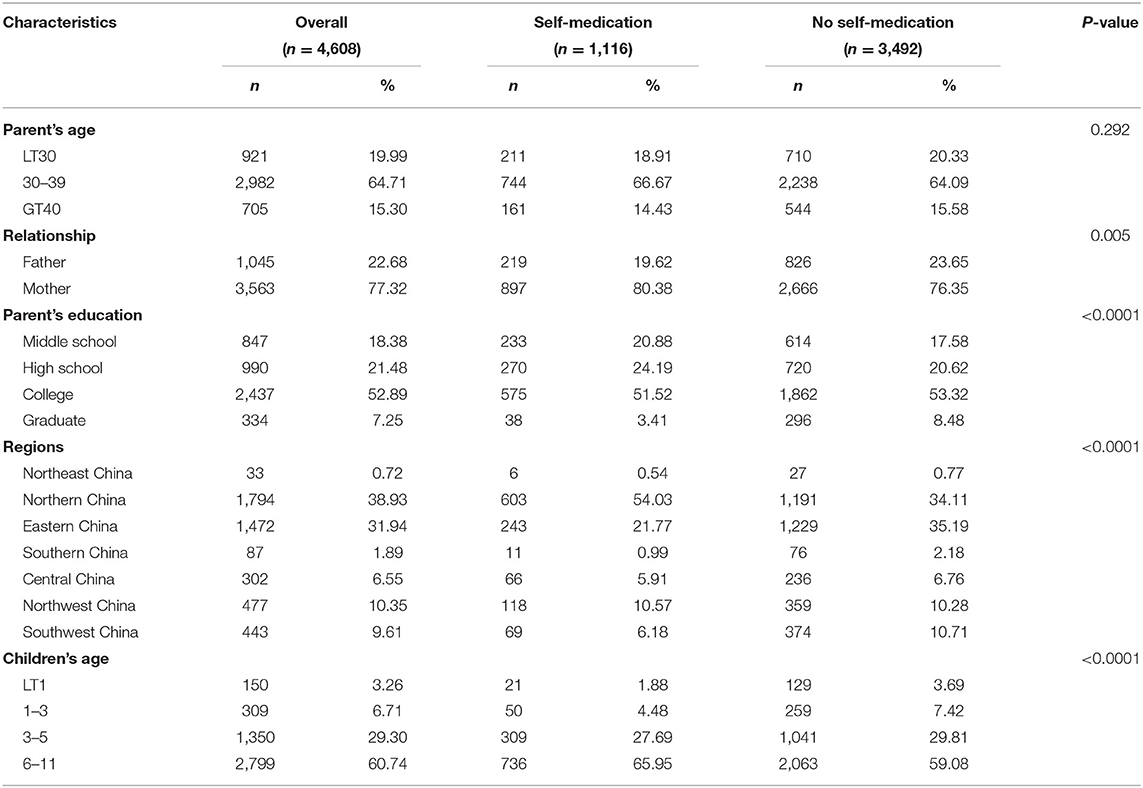
A total of 4,608 (or 88.80%) of 5,189 questionnaires were included in the analysis, after discarding 581 questionnaires that were considered ineligible based on the predefined selection criteria. As shown in Table 1, the majority (n = 2,982; 64.71%) of respondents were aged between 30 and 39 years old, 3,563 (77.32%) were mothers, and 2,437 (52.89%) held a college degree. The majority of parents had a child aged between 6 and 11 (n = 2,799; 60.74%).
Prevalence of Self-Medication
As shown in Table 1, a total of 1,116 (or 24.21%) respondents reported self-medication in the previous year. Respondents who reported self-medication for their children were more likely to be aged between 30 and 39 (66.67 vs. 64.09%), live in Northern China (54.03 vs. 34.11%), and have a child aged 6–11 (65.95 vs. 59.08%). Respondents with graduate degrees were less likely to self-medicate their children (3.41 vs. 8.48%).
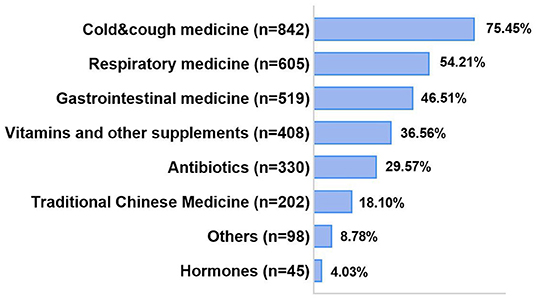
Among those reported parental self-medication, a total of 842 (75.45%) parents reported the use of cold and cough medicine (Figure 1). More than half of respondents reported self-use of respiratory medications (n = 605; 54.21%) and gastrointestinal medicine (n = 519; 46.51%). A total of 330 (or 29.57%) parents reported self-medication of antibiotics.
Risk Factors of Self-Medication
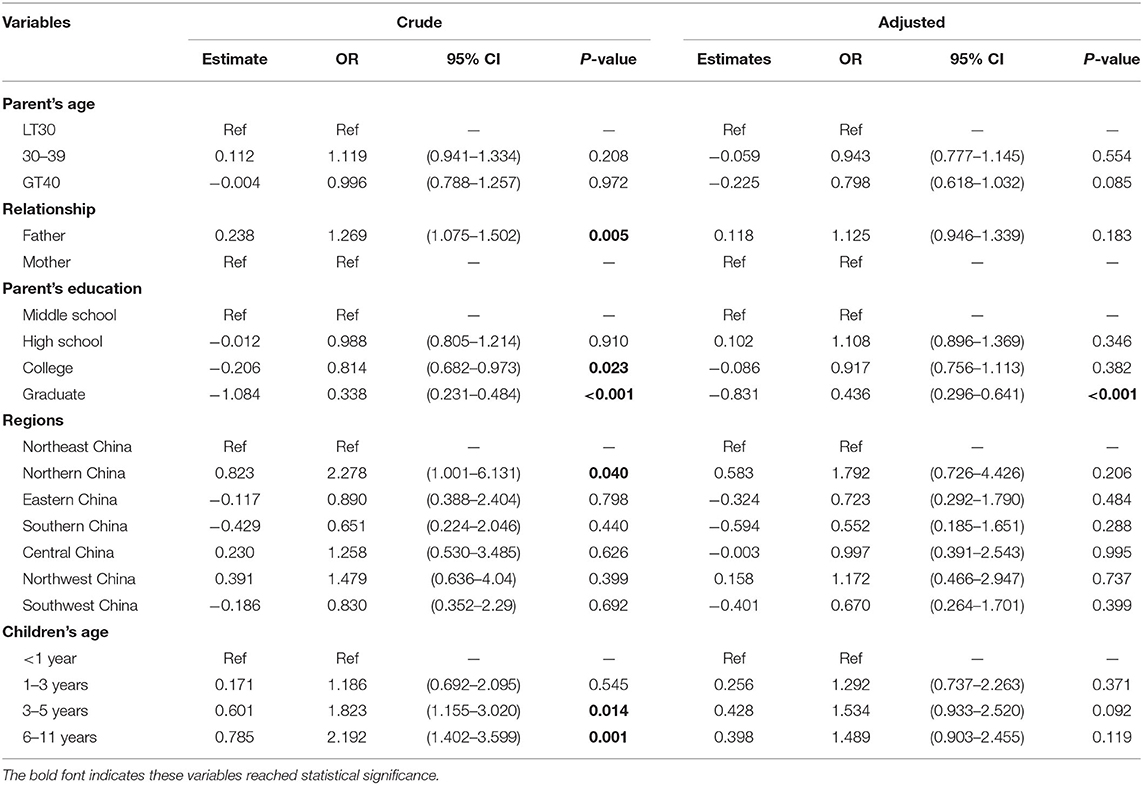
In the logistic regression model, the risk factors of self-medication were fathers (Table 2; Crude OR = 1.269; 95% CI = 1.075–1.502), living in Northeastern China (OR = 2.278; 95% CI = 1.001–6.131), and children aged 3–5 (OR = 1.823; 95% CI = 1.155–3.020), and aged 6–11 (OR = 2.192; 95% CI = 1.402–3.599). Parents with college (OR = 0.814; 95% CI = 0.682–0.973) or graduate education (OR = 0.338; 95% CI = 0.231–0.484) were less likely to self-medicate their children.
After adjusting for other risking factors, parents with graduate degrees were less likely to self-medicate their children [Table 2; Adjusted OR (AOR) = 0.436; 95% CI = 0.296–0.641]. The odds of performing self-medication were higher among fathers (OR = 1.125; 95% CI = 0.946–1.339), living in Northern China (OR = 1.792; 95% CI = 0.726–4.426), and having a child at age 6–11 (OR = 1.489; 95% CI = 0.903–2.455), even these did not score statistical significance.
Nearly half of respondents reported misuse of antibiotics (n = 1,976; 42.88%), a total of 1,654 (or 35.89%) respondents reported abuse or misuse of cold and cough medicines. The abuse or misuse of traditional Chinese medicine (TCM) was also reported among 24.48% of respondents (n = 1,128).
Discussion
In this large national survey, nearly one-fourth of parents reported self-medication in the previous year, indicating that self-medication is common in children under age 12. Our findings highlight the drug safety issue in China. The risk of self-medication reported by our study is similar to those observed in other countries. The prevalence of parental self-medication was 16.1% in Brazil (5) and 32.8% in France (6), suggesting that parental self-medication is a global issue in both developed and developing countries.
Parents are usually the main caregivers for their children, and are mainly responsible for managing the medication therapy of their children. Their knowledge level and attitude toward drug safety greatly affects whether their children use medications rationally. In this analysis, parents with higher education were less likely to perform self-medication for their children, which was different from other countries. In both Germany and Italy, educated parents were more likely to practice self-medication compared to those with lower education level (20, 21). This discrepancy may be explained by how Chinese parents with higher education are more aware of the importance of drug safety. In addition, our findings also indicate that children living in Northern China had a higher risk of self-medication than those living in other regions, which could be potentially explained by the geographic disparities in the economic development level. It seems that the risk of self-medication increases with the age of children. Particularly, our analysis suggested that children aged 6 to 11 were more likely to be self-medicated by their parents, which was consistent with findings from other countries (7, 22).
In China, antibiotics have been pervasively used for children at home or in the clinical settings. In other developing countries, the prevalence of self-medication with antibiotics was as high as 80% (23, 24), leading to the growing concern of the antimicrobial resistance (AMR). Parental self-medication of antibiotics further increases the risk of developing antimicrobial resistance. The self-medication of antibiotics was more prevalent in rural or less economically developed areas. Since parents play a key role in medication management of their children, targeted intervention should be developed for those with lower socioeconomic status to improve their knowledge on the rational drug use. For parents living in the rural or less developed areas, targeted educational campaign should be offered to improve awareness of rational use of medication.
There are several limitations in this study. First, even though this is a national survey, our findings may not reflect the risk of self-medication among the general population because only a small proportion of parents in China participated in the survey. Second, we cannot exclude the possibility of selection bias because parents with higher literacy level were more likely to participate in the survey. As such, it will be difficult to access the knowledge level of those physicians who failed to respond. Lastly, we only included a couple of predictors for self-medication in the survey. Parental self-medication may be influenced by other factors, such as level of income, non-availability of health care centers, and the number of children.
In conclusion, in this large, national survey in China, parental self-medication is prevalent in children under age 12, highlighting the drug safety issue in China. It seems that educational level is the risk factors of self-medication. More targeted intervention and educational program should be implemented to improve drug safety.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Children's Hospital of Fudan University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JY and GM: concept and design. GM: acquisition, analysis, or interpretation of data. JY: drafting of the manuscript and statistical analysis. JY, WD, and GM: critical revision of the manuscript for important intellectual content. GM, WD, and QD: administrative, technical, or material support. GM and ZL: supervision. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This research was supported by grants from the National Natural Science Funds of China (82074109, 81873078, 81374051), the Science and Research Program of Shanghai Municipal Health Commission (201740094, 2018YP001), Key Undergraduate Education Reform Projects in Shanghai in 2020 (No. 12), Shanghai Education Science and Research Project in 2019 (C19077) from Shanghai Municipal Education Commission, and Key Innovative Team of Shanghai Top-Level University Capacity Building in Clinical Pharmacy and Regulatory Science at Shanghai Medical College, Fudan University (HJW-R-2019-66-19).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are very grateful to the parents who participated in the survey.
References
1. Ofori-Asenso R, Agyeman AA. Irrational use of medicines-a summary of key concepts. Pharmacy. (2016) 4:35. doi: 10.3390/pharmacy4040035
2. Yewale VN, Dharmapalan D. Promoting appropriate use of drugs in children. Int J Pediatr. (2012) 2012:906570. doi: 10.1155/2012/906570
4. Escourrou B, Bouville B, Bismuth M, Durrieu G, Oustric S. Self-medication in children by parents: a real risk? A cross-sectional descriptive study. Rev Prat. (2010) 60(6Suppl.):27–34.
5. Arrais PS, Fernandes ME, Pizzol TD, Ramos LR, Mengue SS, Luiza VL, et al. Prevalence of self-medication in Brazil and associated factors. Rev Saude Publica. (2016) 50:13s. doi: 10.1590/s1518-8787.2016050006117
6. Valenzuela M, Sánchez Ruiz-Cabello FJ, Uberos J, Checa Ros AF, Valenzuela Ortiz C, Augustín Morales MC, et al. Self-medication, self-prescription and medicating “by proxy” in paediatrics. An Pediatr. (2017) 86:264–9. doi: 10.1016/j.anpede.2016.06.005
7. Tarciuc P, Stanescu AMA, Diaconu CC, Paduraru L, Duduciuc A, Diaconescu S. Patterns and factors associated with self-medication among the pediatric population in Romania. Medicina. (2020) 56:60312. doi: 10.3390/medicina56060312
8. Pfaffenbach G, Tourinho F, Bucaretchi F. Self-medication among children and adolescents. Curr Drug Saf. (2010) 5:324–8. doi: 10.2174/157488610792246028
9. Xu J, Wang X, Sun KS, Lin L, Zhou X. Parental self-medication with antibiotics for children promotes antibiotic over-prescribing in clinical settings in China. Antimicrob Resist Infect Control. (2020) 9:150. doi: 10.1186/s13756-020-00811-9
10. Blake KV, Zaccaria C, Domergue F, La Mache E, Saint-Raymond A, Hidalgo-Simon A. Comparison between paediatric and adult suspected adverse drug reactions reported to the European medicines agency: implications for pharmacovigilance. Paediatr Drugs. (2014) 16:309–19. doi: 10.1007/s40272-014-0076-2
11. Sachs AN, Avant D, Lee CS, Rodriguez W, Murphy MD. Pediatric information in drug product labeling. J Am Med Assoc. (2012) 307:1914–5. doi: 10.1001/jama.2012.3435
12. Sun H, Temeck JW, Chambers W, Perkins G, Bonnel R, Murphy D. Extrapolation of efficacy in pediatric drug development and evidence-based medicine: progress and lessons learned. Ther Innov Regul Sci. (2017) 2017:1–7. doi: 10.1177/2168479017725558
13. Li Z, Wang Y, Wu D, Gao X, Wang Z. Current status of pediatric labeling in China and the near future efforts needed for the country. Front Pediatr. (2014) 2:17. doi: 10.3389/fped.2014.00017
14. Lindell-Osuagwu L, Sepponen K, Farooqui S, Kokki H, Hameen-Anttila K, Vainio K. Parental reporting of adverse drug events and other drug-related problems in children in Finland. Eur J Clin Pharmacol. (2013) 69:985–94. doi: 10.1007/s00228-012-1426-z
15. China Population Communication Center. Whitepaper: Pediatric Drug Safety in China. China Population Communication Center (2016). Available online at: https://wenku.baidu.com/view/6a8d2d364493daef5ef7ba0d4a7302768e996fbc.html (accessed January 12, 2021).
16. Sun T, Gao L, Li F, Shi Y, Xie F, Wang J, et al. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open. (2017) 7:e017182. doi: 10.1136/bmjopen-2017-017182
17. Hua F, Qin D, Yan J, Zhao T, He H. COVID-19 related experience, knowledge, attitude, and behaviors among 2,669 orthodontists, orthodontic residents, and nurses in China: a cross-sectional survey. Front Med. (2020) 7:481. doi: 10.3389/fmed.2020.00481
18. Xu H, Gonzalez Mendez MJ, Guo L, Chen Q, Zheng L, Chen P, et al. Knowledge, awareness, and attitudes relating to the COVID-19 pandemic among different populations in Central China: cross-sectional survey. J Med Internet Res. (2020) 22:e22628. doi: 10.2196/22628
19. Yuan J, Shen C, Wang C, Shen G, Han B. Assessment of physician's knowledge of potential drug-drug interactions: an online survey in China. Front Med. (2021) 8:650369. doi: 10.3389/fmed.2021.650369
20. Du Y, Knopf H. Self-medication among children and adolescents in Germany: results of the National Health Survey for Children and Adolescents (KiGGS). Br J Clin Pharmacol. (2009) 68:599–608. doi: 10.1111/j.1365-2125.2009.03477.x
21. Garofalo L, Di Giuseppe G, Angelillo IF. Self-medication practices among parents in Italy. Biomed Res Int. (2015) 2015:580650. doi: 10.1155/2015/580650
22. Gohar UF, Khubaib S, Mehmood A. Self-medication trends in children by their parents. J Develop Drug. (2017) 6:173. doi: 10.4172/2329-6631.1000173
23. Simon B, Kazaura M. Prevalence and factors associated with parents self-medicating under-fives with antibiotics in Bagamoyo District Council, Tanzania: a cross-sectional study. Patient Prefer Adherence. (2020) 14:1445–53. doi: 10.2147/PPA.S263517
24. Versporten A, Bielicki J, Drapier N, Sharland M, Goossens H, Group Ap. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother. (2016) 71:1106–17. doi: 10.1093/jac/dkv418
Keywords: self-medication, self-prescription, survey, pediatric, drug safety
Citation: Yuan J, Du W, Li Z, Deng Q and Ma G (2022) Prevalence and Risk Factors of Self-Medication Among the Pediatric Population in China: A National Survey. Front. Public Health 9:770709. doi: 10.3389/fpubh.2021.770709
Received: 04 September 2021; Accepted: 10 December 2021;
Published: 09 February 2022.
Edited by:
Bhaskar Thakur, University of Texas Southwestern Medical Center, United StatesReviewed by:
Ivana I. Kavecan, University of Novi Sad, SerbiaMuhammad Aslam, Bahauddin Zakariya University, Pakistan
Copyright © 2022 Yuan, Du, Li, Deng and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guo Ma, bWcwMzI4QDEyNi5jb20=; bWcwMzI4QGZ1ZGFuLmVkdS5jbg==
†These authors have contributed equally to this work
 Jing Yuan
Jing Yuan Wandi Du1†
Wandi Du1† Guo Ma
Guo Ma