
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 November 2021
Sec. Public Health Policy
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.769176
The objective of the present study was to investigate if the policy for contracting out the Korean influenza National Immunization Program (NIP) for individuals aged ≥ 65 years affects a reduction in vaccination inequality based on gender and socioeconomic position (SEP). In South Korea, initially only public health centers provided influenza vaccination for free; however, starting from the fall of 2015, the program was expanded to include private medical institutions. The policy was expected to improve overall vaccination rate and reduce its inequality, through improving access to vaccination. The present study analyzed how the gap in the vaccination rate changed between before and after contracting out. A multivariate logistic regression model stratified by gender and SEP of individuals aged ≥ 65 years was used. The study also analyzed changes in the unvaccinated rates between before and after contracting out based on an interrupted time series model. The gap in the unvaccinated rate based on SEP present prior to contracting out of the NIP for individuals aged ≥ 65 years did not decrease afterwards. In particular, the step changes were 0.94% (95% confidence interval [CI]: 0.00, 1.89) and 1.34% (95% CI: 1.17, 1.52) in men and women, respectively. In the pre-policy period, among women, the unvaccinated rate of the medical aid beneficiaries group was 1.22-fold higher (95% CI: 1.12, 1.32) than that of the health insurance beneficiaries, and the difference was not reduced post-policy implementation (odds ratio: 1.27, 95% CI: 1.20, 1.36). The findings of the study were that contracting out of the NIP was not effective in improving vaccination rate nor resolving vaccination inequality. Future studies should focus on identifying the mechanism of vaccination inequality and exploring measures for resolving such inequality.
Coronavirus disease (COVID-19) vaccination is currently underway, and improving the vaccination rate is a key strategy for achieving herd immunity. Herd immunity is necessary to overcome the current COVID-19 pandemic (1). Effective immunization, a high-priority public health strategy for preventing disease transmission, is subject to strict governmental control in terms of planning, procurement, and service provision. In particular, guaranteeing equal access without discrimination or exclusion of specific groups is important. However, the National Health Insurance system in South Korea (2–5) creates a barrier to health care access including vaccination. In Korea, majority of the population (97%) are covered by the National Health Insurance Services, while the most disadvantaged are covered by the Medical Aid Program. In theory, the entire population have healthcare coverage. However, the required copayment is considerable (about 65%), which still hampers access to healthcare by the poor. Moreover, private healthcare facilities account for 90% of all hospital beds. Although for-profit hospitals are not allowed in Korea, many private facilities are profit driven. Under the circumstances, among various accessibility dimensions, physical and economic accessibility could deteriorate. Improvement in physical and economic accessibility is achievable through policies guaranteeing free vaccination, as well as by securing enough medical institutions that can provide such a service within a reachable distance (6). In Korea, the National Immunization Program (NIP) was initially carried out mostly by public medical institutions. To increase immunization accessibility, the Korean government then pursued a policy for expanding the NIP to include private medical institutions (7) COVID-19 vaccination was carried out in a similar manner: in the early stages, vaccination was carried out through most public medical institutions and was subsequently expanded through the NIP to include private medical institutions.
In other words, the government has contracted out the NIP from the public sector to the private sector. With “contracting out,” private entities are contracted to provide public services that used to be provided directly by the government. Expansion of the immunization program to include private medical institutions is one approach by which the Korean government is “contracting out” as part of the NIP. The Korean government explains this as a public–private partnership with private medical institutions instead of “contracting out.” However, the authors believe that understanding this concept as contracting out would be more appropriate. The contracting government plays the role of the purchaser and manager, and the contracted private medical institution plays the role of an immunization service provider based on a contract. The parties do not share finance, management, nor risks in the process of providing the immunization services (8, 9). On the one hand, given that privatization refers to all efforts to introduce market mechanisms to public service delivery by public-to-private transfer of authority over ownership, management, finance, and/or control (8, 10), contracting out the NIP could be conceptualized and considered as one type of privatization (8, 11, 12).
The goals of contracting out of the NIP are to improve the accessibility and convenience of immunization, which are consistent with the motivation for privatization of general public services. Privatization, especially the need for and implementation of contracting out, is based on the belief that private entities are able to deliver services more effectively and efficiently than public entities (12, 13). Contracting out offers the following benefits: (1) there is no need to increase the number of public servants to directly provide the service, which can help reduce government expenditure; (2) the expertise, resources, and technology of private institutions could be utilized, while the quality of service could be improved by promoting competition among private institutions by giving more choices to the users; and (3) the service delivery practice of contracted private institutions could be assessed more objectively than in the case of the government assessing its own practice. Therefore, greater emphasis is placed on the accountability of the private institutions, meaning the service providers. This could allow for more effective and efficient service delivery (14, 15). However, it is uncertain whether contracting out could actually produce such outcomes. In fact, it may produce inefficient outcomes: management and supervision costs are incurred, government accountability and public interest may be compromised, and cost savings based on reduced manpower and lower wages by private contractors could actually lead to a decline in the quality of service. For example, when the British National Health Service contracted out its cleaning service, a reduction in cleaning staff for efficiency led to an increased risk of hospital-acquired infection (16). However, empirical review and discussions on the effects of contracting out of essential public health services, not “non-essential” services, are still lacking.
South Korea expanded its influenza vaccination program for individuals aged ≥ 65 years to include private medical institutions. The advocates of the policy have claimed that it can contribute to improving the overall vaccination rate and addressing the vaccination inequality with the purpose of improving immunization accessibilities. Consequently, the proportion of vaccinations carried out in private medical institutions increased. However, the proportion of vaccinations carried out in public health centers and other public institutions decreased. Given this evidence, a previous study has reported that contracting out vaccination services does not contribute to an overall improvement in the vaccination rate (17). The present study goes a step further to identify the influence of such contracting out on gender and socioeconomic inequality in immunization. The study investigated gender-differences in the effects of contracting out of influenza vaccination for individuals aged ≥ 65 years and whether contracting out contributed to reducing the gap in vaccination rate based on socioeconomic position (SEP).
The influenza NIP in South Korea began in 1997 as a pilot program for individuals aged ≥ 65 years and patients with cardiopulmonary disease. Free vaccination for individuals aged ≥ 65 years which began in 2005 at public health centers, was not for free at private medical institutions. Therefore, out-of-pocket expenditure was incurred when individuals were vaccinated at private medical institutions. After the program was subsequently expanded to include private medical institutions starting from the 2015–2016 flu season (17), no one paid expenses for the vaccination anymore.
The present study used 2013–2019 data from the Korean Community Health Survey (KCHS) (18).
KCHS, conducted annually by the Korean Disease Control and Prevention Agency since 2008, has participation from approximately 250 public health centers throughout South Korea. The KCHS uses two rounds of systematic sampling (individuals aged ≥ 19 years) to collect nationally representative data from surveying ~2,20,000 individuals each year. The present study selected individuals aged ≥ 65 years at the time of the survey and included their “Yes” or “No” responses to whether they received annual influenza vaccination. Data from 2015, the year when contracting out of the vaccination service was implemented, were excluded since it could cause confusion in the analysis. However, the vaccination rate among the 2015 survey participants was calculated separately for subsequent calculation of the annual vaccination rate. Lastly, participants who did not respond to questions on covariates were also excluded.
The two major independent variables were the survey participation time point and medical aid beneficiary status, as a proxy indicator of SEP. For the survey participation time point, 2013 and 2014 survey participants were defined as the pre-policy implementation group (pre-group) and 2016–2019 participants were defined as the post-policy implementation group (post-group). South Korea operates a national health insurance system. While 97% of the population is covered under this system, the remaining 3% receives healthcare coverage through a tax-based system called medical aid. The medical aid beneficiaries represent the poor and socially deprived population who qualify based on the following conditions: (1) earn ≤ 40% of the standard median income; (2) inability to work due to health issues, disabilities, etc.; and (3) have no dependents (or support family). Individuals who indicated that they received medical aid benefits during the year covered by the KCHS were defined as medical aid beneficiaries, while all others were categorized as health insurance beneficiaries. The outcome variable was defined as responding “Yes” to the question “Have you received an influenza vaccination in the past year?” To analyze the changes in annual vaccination rate, the gender-stratified total vaccination rate among individuals aged ≥ 65 years for the survey year and the vaccination rate based on SEP after gender stratification were measured separately. Lastly, among the variables known to influence healthcare utilization, marital status, region (residence), recent labor (paid/unpaid) experience, monthly household income, smoking history, alcohol consumption history, hypertension, and diabetes mellitus (DM) were measured as covariates.
Participants in the 2015 survey were excluded from all analyses, except for the trend analysis on changes in annual vaccination rate. All analyses were performed separately by gender. For the vaccination rate based on the type of health coverage, differences in the distribution of baseline variables were tested using Pearson's chi-square test. To analyze the differences based on privatization policy and health coverage together, a multivariate logistic regression model stratified for policy and health coverage types was constructed. With the pre-policy implementation health insurance beneficiaries as the reference group, the odds ratios (ORs) of the unvaccinated rates for influenza in the pre-policy implementation medical aid beneficiaries, post-policy implementation health insurance beneficiaries, and post-policy implementation medical aid beneficiaries were calculated. The gap in the unvaccinated rate based on health coverage type before and after the implementation of the policy was examined separately. Changes in the unvaccinated rate between before and after the implementation of the policy were analyzed for the health insurance subscribers and medical aid beneficiaries. The additive interaction of health coverage type and policy implementation was measured by the relative excess risk due to interaction and the proportion of disease attributable to interaction. To analyze the time-series changes in the vaccination rate between before and after the implementation of the policy, an interrupted time-series model was constructed as shown below. We considered that a level change and slope change model would be appropriate to identify the impact of contracting out of the NIP, because the total number of hospitals providing free vaccination was immediately increased right after the policy change and the change could gradually change the health seeking behaviors of people (19). The model below included participants in the 2015 survey, which was conducted between August 31st and November 8th, which overlaps with the period when privatization of influenza vaccination was fully implemented. Therefore, it was assumed that the effect of the implementation of the policy would appear starting from the 2016 survey.
Yt is the unvaccinated rate at year t. T is year t. X1 is an indicator of the introduction of a new policy (after the policy is introduced, X1 = 1; otherwise, 0). β1 is the slope before the new policy, β2 is a step-down after the policy was introduced and γ1 indicates the interaction of X1 and T. δ and C are a matrix of potential confounders in t−1 year and their coefficients. With seven time points, we considered a potential confounder that was the log transformed influenza incidence in t−1 year, because the incidence in t−1 year would affect the health behaviors of people in t year. For the sensitivity analysis, we also constructed a slope change model as the simplest model with different lags, with assumption that the policy change could not affect the level change. We conduct the Cumby-Huizinga test to identify appropriate lags in the models. STATA/SE version 15 (StataCorp LLC, College Station, TX, USA) was used for all statistical analyses.
A total of 4,58,804 individuals aged ≥ 65 years participated in the surveys. Of these, 3,94,284 were included in the final analysis after excluding participants in the 2015 survey (n = 63,141) and individuals who did not provide a response for immunization status (n = 1), marital status (n = 136), smoking status (n = 23), alcohol consumption status (n = 92), and DM status (n = 1,127). Among the female health insurance subscribers, the unvaccinated rate was highest in 2013 (14.8%), and it decreased to 8.6% in 2019. Among the female medical aid recipients, the unvaccinated rates in 2013 and 2019 were 17.7 and 12.4%, respectively (Table 1). Among the male health insurance subscribers, the unvaccinated rates were highest (16.8%) and lowest (11.2%) in 2013 and 2019, respectively. Among the male medical aid recipients, the unvaccinated rates in 2013 and 2019 were 22.1 and 15.1%, respectively (Table 2). Among the overall study population, the unvaccinated rate was lowest among those aged 75–84 years, living with a partner, living in a rural region, and drinking less. Participants under hypertension and DM treatment had lower unvaccinated rates than those under no such treatment among both men and women.
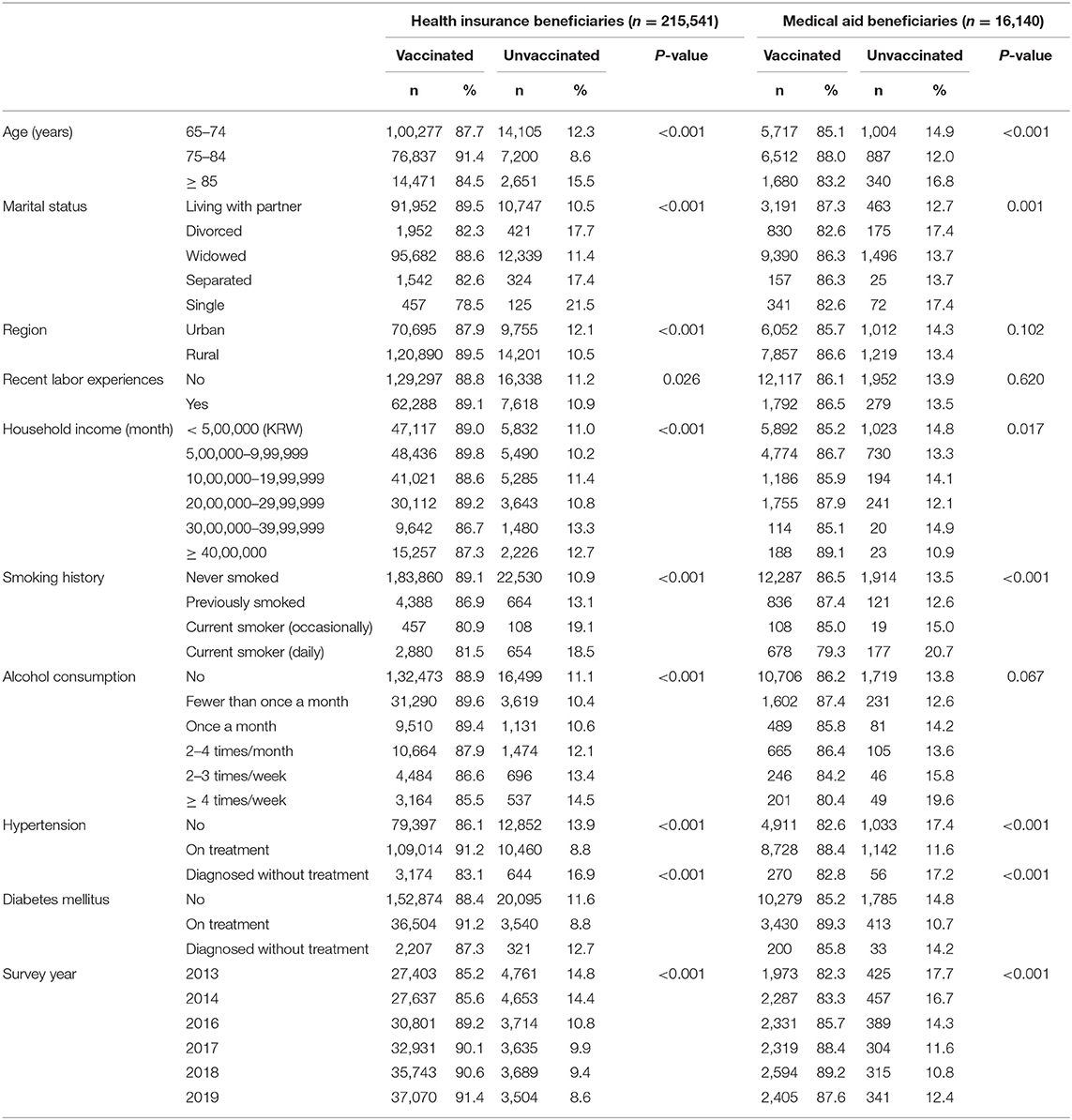
Table 1. Vaccination rates among female participants based on different baseline characteristics stratified by type of health coverage.
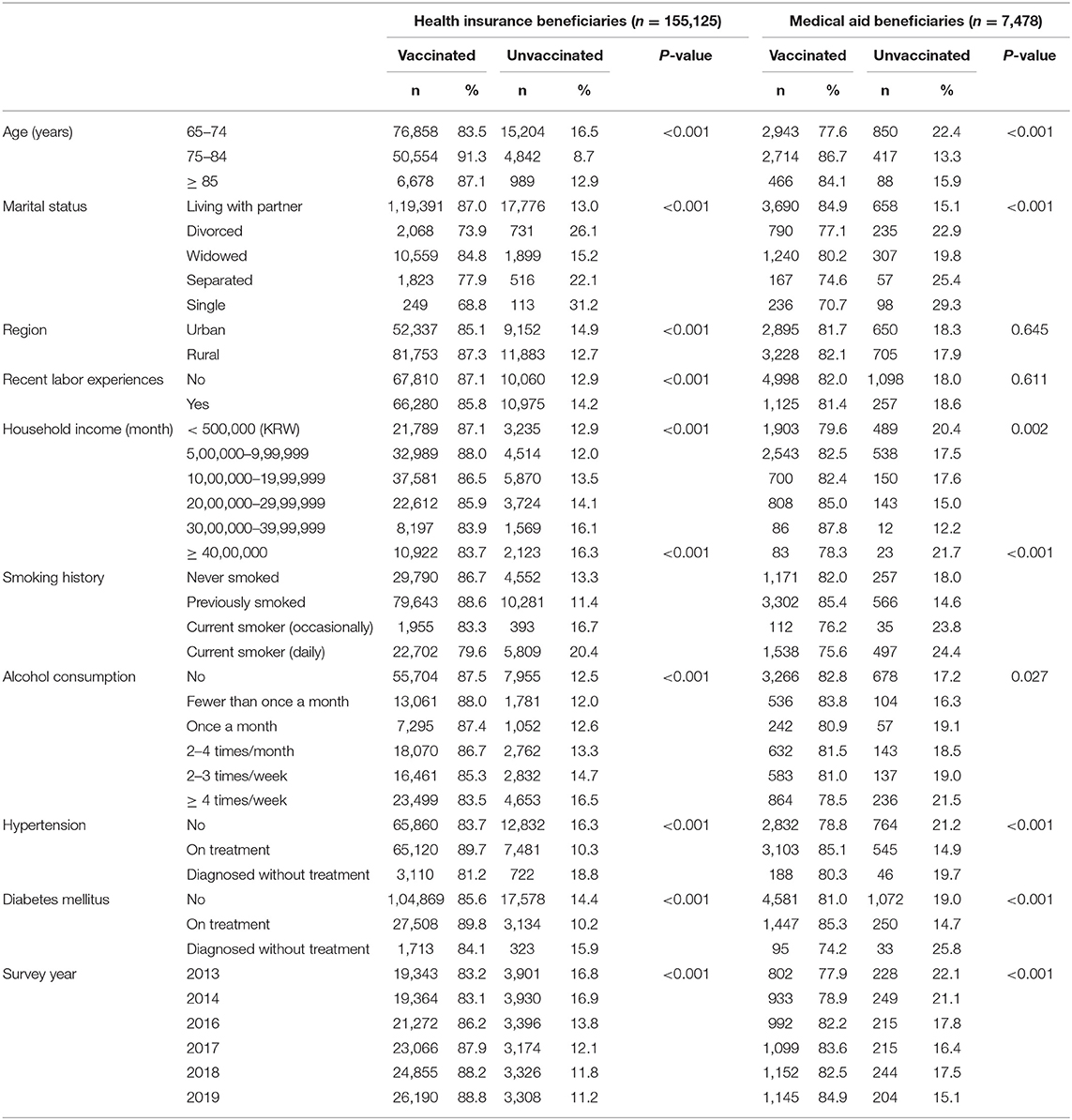
Table 2. Vaccination rates among male participants based on different baseline characteristics stratified by type of health coverage.
A stratified multivariate analysis of the changes in the unvaccinated rate based on SEP before and after the implementation of the policy was conducted. Among women, the unvaccinated rate of the pre-policy implementation health insurance beneficiaries (reference group) was 14.6%, while that of the medical aid beneficiaries was approximately 1.22-fold higher (17.2%; 95% CI: 1.12, 1.32). The unvaccinated rate of the post-policy implementation medical aid beneficiaries was ~1.27-fold (95% CI: 1.20, 1.36) higher than that of the health insurance subscribers. Both health insurance subscribers and medical aid beneficiaries showed a decrease in the unvaccinated rate between before and after the implementation of the policy, with ORs of 0.63 (95% CI: 0.61, 0.65) and 0.69 (95% CI: 0.63, 0.76), respectively. No interaction was found between the privatization policy and SEP. The pre-policy implementation SEP-based gap in the unvaccinated rate was maintained after policy implementation (Table 3). Similar results were found among the men (Table 4).
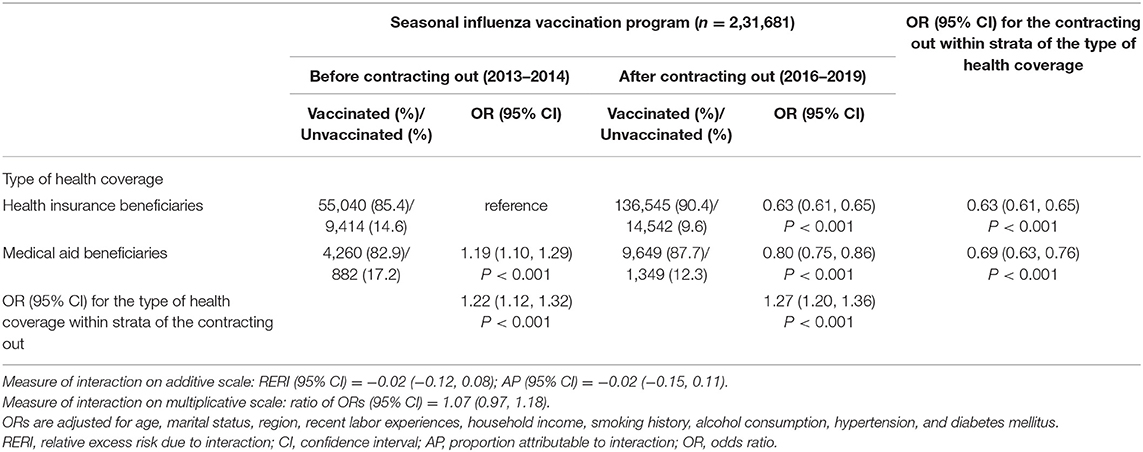
Table 3. Contracting out program-stratified association of socioeconomic position with the unvaccinated rate for seasonal influenza among women.
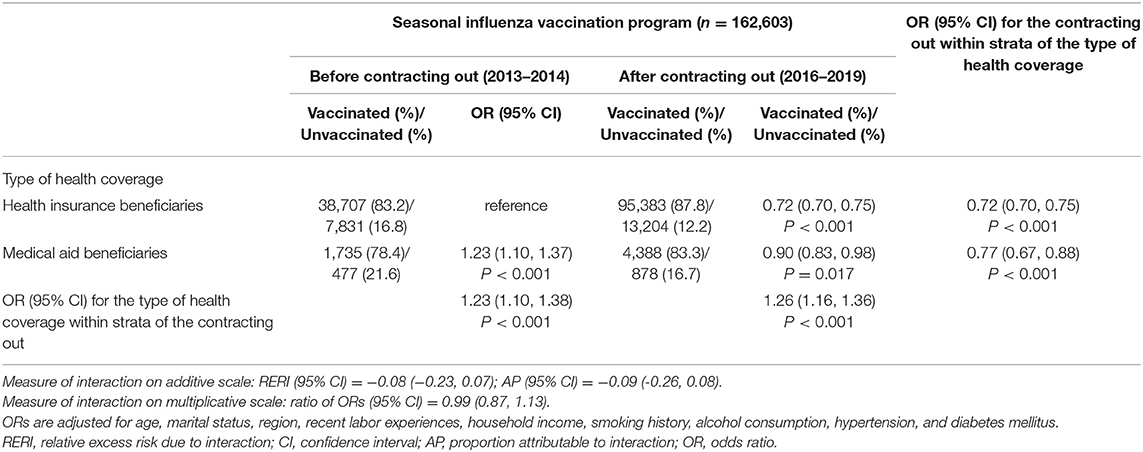
Table 4. Contracting out program-stratified association of socioeconomic position with the unvaccinated rate for seasonal influenza among men.
In the gender-stratified analysis, there was a decrease in the unvaccinated rate from before to after the implementation of the policy among both men and women. However, changes in the decreasing trend slope were not affected by the implementation of the policy, and there was no level change in the unvaccinated rate (Figure 1). In the detailed analysis, the slope change of the unvaccinated rates, which was adversely increased after the implementation of the policy among men (lag 0) and women (lag 3) were 0.94% (95% CI: 0.00, 1.89) and 1.34% (95% CI: 1.17, 1.52), respectively. In the analysis based on health coverage type, there was a 1.40% increase in the unvaccinated rate after the implementation of the policy (95% CI: 1.34, 1.46) among male health insurance beneficiaries (lag 3) with a level change (coefficient: 0.86, 95% CI: 0.78, 0.94). We mainly present the level and slope change model and additionally describe the results from the slope change model in Table 5. There were little differences between the models.

Figure 1. Change in the unvaccinated rate before and after the contracting out of the National Immunization Program [(A): male; (B): female; (C): male by the type of health coverage; (D): female by the type of health coverage; (C,D): solid line indicates health insurance beneficiaries and dashed line indicates medical aid beneficiaries].
The findings of the present study confirmed that privatization of the influenza NIP did not reduce SEP-based vaccination inequality. Analyses based on gender and SEP showed an improvement effect on the vaccination rate among female medical aid recipients. However, the results did not show privatization of the NIP as having an overall improvement effect on the vaccination rate among the general population. These findings are consistent with those of a recent South Korean study that analyzed different data sources (17). This study presented policy implementation without consideration for fundamental causes of vaccine hesitancy as one of the factors. Privatization of the NIP had little effect on improving the vaccination rate and did not reduce SEP-based vaccination inequality. This may reflect the need for more active consideration of social determinants in the NIP. Safety awareness, the gap in information access due to health literacy, the gap between urban and rural regions, financial gap, and differences in perception of authoritative government policies have been presented as social determinants of vaccine hesitancy (6).
The gender-based difference in vaccination is also important. Studies outside South Korea have reported that women generally have higher vaccine hesitancy than men (20, 21). Consequently, men have a higher influenza vaccination rate (22–25). However, in South Korea, elderly women have a higher vaccination rate, with the gender-based gap appearing especially among young-old women and men. This may be related to young-old women, aged 65–74 years, having higher outpatient service utilization rates than their male counterparts (26, 27). Moreover, a higher percentage of young-old women may have a regular source of care (28). There is a higher likelihood of women being informed about receiving free influenza vaccination at their regular outpatient medical institutions and acting on such information to actually get vaccinated. Such a phenomenon also appears to be related to the free vaccination service offered at private medical institutions as part of the public service offered by the government. The service should be accepted as a welfare service, rather than other preventive services that have out-of-pocket costs. Elderly Korean women represent the group with the lowest income among all age and gender groups (29). It is suspected that the higher vaccination rate may be related to the elimination of out-of-pocket costs for influenza vaccination at private medical institutions. These costs used to amount to 20,000–40,000 won for the poorest group before the implementation of the NIP and is still charged to the people under the age of 65. It can be viewed that the policy had a marginal benefit in this group, and could explain the largest improvement effect among female medical aid recipients after the implementation of the policy. Such a tendency might be consistent with existing evidence that service use increases among the poorest and women when public spending is increased (30, 31). However, an increase in public spending in such cases involves a concept that does not differentiate between the public or private status of the service provider. Moreover, it does not consider the contextual influence associated with how the service is provided. Therefore, it is only partially valid in explaining the policy effect in the present study.
The findings of the present study were somewhat different from those of other international academic studies on the effects of contracting out influenza vaccination. An overseas literature review evaluated the effectiveness of contracting out primary healthcare services, including vaccination, in low- and middle-income countries. The study reported that contracting out led to improved service accessibility through an expanded range of service provision, utilization, and coverage (32). A Korean study that assessed the effects of contracting out vaccination reported that contracting out increased accessibility, whereby the vaccination rate among individuals aged ≥ 65 years improved (33). However, in the present study, which conducted an analysis with consideration of the time trend, there was no significant change in increasing trend in the vaccination rate between before and after the implementation of contracting out. In other words, the increase in the vaccination rate reflected the increasing trend that presents before contracting out; therefore, it would be difficult to claim that such an effect was a result of contracting out. Meanwhile, just as in the study by Liu et al. (32), contracting out was unable to reduce SEP-based vaccination inequality. Even after contracting out, differences in influenza vaccination among health insurance subscribers and medical aid recipients remained.
Contracting out as a privatization approach does not reduce SEP-based inequality, but is likely to exacerbate it (34). The generation of a new public service user fee, an increase in the existing user fee, privatization of the social safety net, a reduction in wages and benefits, and socioeconomic segregation are the five mechanisms discussed. Influenza vaccination for the elderly Korean population adopted a privatization strategy in the form of contracting out, which is free of charge and targets the entire population aged ≥ 65 years. Therefore, instead of the first four mechanisms, the last mechanism appears to be applicable. In other words, contracting out influenza vaccination did not consider the characteristics of individuals aged ≥ 65 years nor did it include resolution of inequality as one of its goals from the beginning. Therefore, such results could be attributable to the absence of accountability and a strategy for such factors. Quantitative expansion of vaccination institutions could be a strategy that does not sufficiently consider the characteristics of the elderly population. It also does not consider the difference in accessibility by stages of healthcare use based on the SEP of the vaccination “customers” (35). The low-income class has a high likelihood of not receiving vaccination due to the burden of indirect costs, including transportation fee for going to the medical institution. However, economic accessibility from that perspective has not been considered. The need for vaccination and access to relevant information may vary depending on income level; however, such factors have not been considered. Kim et al. (33) examined the factors that influence influenza vaccination sites. They found that, among individuals aged ≥ 65 years, the OR for receiving vaccination at a public health center was significantly higher in the fourth income quartile than in the first income quartile. However, contracting out only has the goal of expanding vaccination to private medical institutions, rather than seeking the role of public health centers. Contracted providers need to only provide immunization services for vaccines requested according to the terms of the contract; thus, they have no incentive to provide services by identifying or prioritizing vulnerable populations, such as the elderly and impoverished. Therefore, contracting out vaccination by the government with the goal and strategy of only improving physical accessibility through quantitative expansion of vaccination sites could be understood as maintaining the same vaccination rate and socioeconomic inequalities affecting the vaccination rate.
Healthcare services, as public goods with non-exclusionary and non-competitive characteristics, should not have the goal of only improving the vaccination rates through improved physical accessibility. Even within public health, this is more important for immunization to prevent especially infectious diseases (36). The condition for privatization to resolve inequality is when clarification of the target population and alleviation of healthcare utilization inequalities among such a population are set as the major goals (34). For example, contracting out was able to alleviate vaccination inequality in Cambodia, where the contract stipulated equality as one of the roles of the service provider (37). In this context, contracting out healthcare services could go beyond cost saving and enhanced efficiency to ask questions about the mission and value of public health (12). The value of public health can be found in not only health promotion and prevention among individuals and populations, but also equitable and just distribution. Therefore, a key responsibility of public health is to simultaneously consider both the structural factors of diseases and the social determinants of health. Of course, it should be based on the understanding of the mechanisms behind the utilization of public health services by the target population. While the authorities identify demands, procurement, allocation and reapportion of influenza vaccines, managing leftovers, and controlling hazards, they did not address the oversight of the quality of the NIP itself. In other words, there has been no responsible stewardship on quality assurance for alleviating vaccination inequality among the elderly in the NIP. Thus, the quality control system for contracting out the NIP should be established.
The present study had some limitations. First, information about where people were vaccinated for influenza (public or private medical institution) was unavailable; thus, the study was limited to identifying the total impact of the vaccination rate. For example, if the proportions of vaccinations in the public and private sectors after contracting out were measured directly and contributing factors were identified to determine where changes in vaccination rates based on gender or insurance type occurred, more specific conclusions could have been drawn. Second, while barriers to physical and cost accessibility were partially alleviated through contracting out, information about other factors that could influence improvement in vaccination rates, such as improvement in information accessibility or acceptance, was insufficient. Therefore, the mechanism could only be estimated. Third, the study did not analyze whether the effects of contracting out appear differently according to the distribution of public/private medical resources within a region. Additional analysis that links data regarding the distribution of medical resources is warranted in the future. Fourth, the analyses did not consider potential time-varying confounders other than the incidence of influenza in the (t-1) year owing to small number of time points in the model. Finally, although cost effectiveness is one of the main reasons to contract out NIP, we could not access the information about the government expenditure on this program and the result of policy evaluation including its cost-effectiveness. Future studies should focus on the economic evaluation of the new strategy of NIP.
The number of public healthcare institutions, including public health centers is small; thus, offering vaccinations through only public institutions would limit availability and physical accessibility within the region. Therefore, increasing the number of institutions that provide such a service through contracting out could be viewed as an easy approach. However, the present study did not find any improvement that exceeded the existing increasing trend in the vaccination rate, nor did it find improvement in socioeconomic inequality. Nonetheless, a significant increase was found among poor elderly women who are medical aid recipients. This is suspected to be the effect of improved cost accessibility as a result of a waiver of out-of-pocket costs.
When contracting out, a mandate for alleviating health inequality was not specifically imposed on the private institutions. Meanwhile, public institutions are downsizing vaccination services in response to the expansion of contracting out. Furthermore, demand is also decreasing with the decreasing population size in non-urban regions. This is causing greater inequality in the distribution of private medical institutions between regions. Therefore, privatization of vaccination services is highly likely to worsen such inequality. Outcomes from contracting out, which was attempted to address insufficient public health infrastructure, need to be reassessed. In particular, it is necessary to monitor the long-term effects related to health inequality.
Publicly available datasets were analyzed in this study. This data can be found here: https://chs.kdca.go.kr/chs/rdr/rdrInfoProcessMain.do.
The studies involving human participants were reviewed and approved by Institutional Review Board of Konyang University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
HC and DM conceptualized the study. HC designed the analysis plan, performed the formal analysis, and created the figures. DM, SK, M-HK, and DJ contributed to writing the manuscript. All authors approved the final version for submission.
The study was supported by a grant from the National Research Foundation of Korea (NRF) funded by the Korean Government (Ministry of Science and ICT: MSIT; No. NRF2021R1F1A105102111) (HC).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Jentsch PC, Anand M, Bauch CT. Prioritising COVID-19 vaccination in changing social and epidemiological landscapes: a mathematical modelling study. Lancet Infect Dis. (2021) 21:1097–106. doi: 10.1016/S1473-3099(21)00057-8
2. Kim YH, Tantalean-Del-Aguila M, Dronina Y, Nam EW. Comparison of the health insurance systems of South Korea and Peru. Health Policy Manag. (2020) 30:253–62. doi: 10.4332/KJHPA.2020.30.2.253
3. Park S. Medical service utilization and out-of-pocket spending among near-poor national health insurance members in South Korea. BMC Health Serv Res. (2021) 21:1–11. doi: 10.1186/s12913-021-06881-8
4. Lee SY, Chun CB, Lee YG, Seo NK. The national health insurance system as one type of new typology: the case of South Korea and Taiwan. Health Policy. (2008) 85:105–13. doi: 10.1016/j.healthpol.2007.07.006
5. Kwon SM. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. (2009) 24:63–71. doi: 10.1093/heapol/czn037
6. Glatman-Freedman A, Nichols K. The effect of social determinants on immunization programs. Hum Vaccin Immunother. (2012) 8:293–301. doi: 10.4161/hv.19003
7. Shin T, Kim CB, Ahn YH, Kim HY, Cha BH, Uh Y, et al. The comparative evaluation of expanded national immunization policies in Korea using an analytic hierarchy process. Vaccine. (2009) 27:792–802. doi: 10.1016/j.vaccine.2008.10.075
8. Ullrich G, Essenberg H, Ratteree W, Hoffmann E, Hammouya M. The Impact of Decentralization and Privatization on Municipal Services: Report for Discussion at the Joint Meeting on the Impact of Decentralization and Privatization on Municipal Services. Geneva: ILO (2001). p. 118.
9. Johnston VR, Seidenstat P. Contracting out government services: privatization at the Millenium. Int J Public Adm. (2007) 30:231–47. doi: 10.1080/01900690601117713
10. Suleiman E, Waterbury J. The Political Economy of Public Sector Reform and Privatization. New York NY: Routledge (2019). p. 388. doi: 10.4324/9780429313707
11. Ascoli U, Ranci C. Dilemmas of the Welfare Mix: The New Structure of Welfare in an Era of Privatization. New York, NY: Springer Science & Business Media (2002). p. 264. doi: 10.1007/978-1-4757-4992-2
12. Gollust SE, Jacobson PD. Privatization of public services: organizational reform efforts in public education and public health. Am J Public Health. (2006) 96:1733–9. doi: 10.2105/AJPH.2005.068007
13. Savas ES. A. taxonomy of privatization strategies. Policy Stud J. (1989) 18:343–55. doi: 10.1111/j.1541-0072.1989.tb00837.x
14. Boston J. The challenge of evaluating systemic change: the case of public management reform. Int Public Manag J. (2000) 3:23–46. doi: 10.1016/S1096-7494(00)00033-7
15. Overman S. Great expectations of public service delegation: a systematic review. Public Manag Rev. (2016) 18:1238–62. doi: 10.1080/14719037.2015.1103891
16. Toffolutti V, Reeves A, McKee M, Stuckler D. Outsourcing cleaning services increases MRSA incidence: evidence from 126 English acute trusts. Soc Sci Med. (2017) 174:64-9. doi: 10.1016/j.socscimed.2016.12.015
17. Ko H, Kim M. Impacts of expanding provider choice for free flu vaccination among the elderly in Korea. Health Policy. (2020) 124:1115–20. doi: 10.1016/j.healthpol.2020.07.014
18. Kang YW, Ko YS, Kim YJ, Sung KM, Kim HJ, Choi HY, et al. Korea community health survey data profiles. Osong Public Health Res Perspect. (2015) 6:211–7. doi: 10.1016/j.phrp.2015.05.003
19. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2016) 46:348–55. doi: 10.1093/ije/dyw098
20. de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. (2020) 396:898–908. doi: 10.1016/S0140-6736(20)31558-0
21. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. (2021) 6:e210–21. doi: 10.1016/S2468-2667(21)00012-8
22. Hagemeister MH, Stock NK, Ludwig T, Heuschmann P, Vogel U. Self-reported influenza vaccination rates and attitudes towards vaccination among health care workers: results of a survey in a German University Hospital. Public Health. (2018) 154:102–9. doi: 10.1016/j.puhe.2017.10.027
23. Jiménez-García R, Hernández-Barrera V, de Andres AL, Jimenez-Trujillo I, Esteban-Hernández J, Carrasco-Garrido P. Gender influence in influenza vaccine uptake in Spain: time trends analysis (1995-2006). Vaccine. (2010) 28:6169-75. doi: 10.1016/j.vaccine.2010.07.029
24. Mangtani P, Breeze E, Stirling S, Hanciles S, Kovats S, Fletcher A. Cross-sectional survey of older peoples' views related to influenza vaccine uptake. BMC Public Health. (2006) 6:249. doi: 10.1186/1471-2458-6-249
25. Rodríguez-Rieiro C, Esteban-Vasallo MD, Domínguez-Berjón MF, Astray-Mochales J, Iniesta-Fornies D, Barranco-Ordoñez D, et al. Coverage and predictors of vaccination against 2009 pandemic H1N1 influenza in Madrid, Spain. Vaccine. (2011) 29:1332–8. doi: 10.1016/j.vaccine.2010.10.061
26. Jeon H, Kahng S. Age Differences in the predictors of medical service use between young-old and old-old: implications for medical service in aging society. Health Soc Welf Rev. (2012) 32:28–57. doi: 10.15709/hswr.2012.32.1.28 (In Korean).
27. Song T. An Anderson model approach to the mediation effect of stress vulnerability factors on the use of outpatient care by the elderly. Health Soc Welfare Rev. (2013) 33:547–76. (In Korean). doi: 10.15709/hswr.2013.33.1.547
28. Park E, Seo J, Jung Y, Bae J, Lee N, Kim E, et al. A Report on the Korea Health Panel Survey of 2017(II). Seoul: Korean Institute for Health and Social Affairs (2019). p. 453. (In Korean).
29. Weon S. The condition of asset poverty of the elderly in South Korea. Asian Soc Work Policy Rev. (2020) 14:158–71. doi: 10.1111/aswp.12206
30. Johannes TA, Noula AG. Gender and increased access to schooling in Cameroon: a marginal benefit incidence analysis. J Int Womens Stud. (2011) 12:94–106. Available online at: https://vc.bridgew.edu/jiws/vol12/iss1/8
31. Kruse I, Pradhan M, Sparrow R. Marginal benefit incidence of public health spending: evidence from Indonesian sub-national data. J Health Econ. (2012) 31:147–57. doi: 10.1016/j.jhealeco.2011.09.003
32. Liu X, Hotchkiss DR, Bose S. The effectiveness of contracting-out primary health care services in developing countries: a review of the evidence. Health Policy Plan. (2008) 23:1–13. doi: 10.1093/heapol/czm042
33. Kim HC, Kim DH, Park JH, Kim EY, Choi MY, Park SG, et al. Factors associated with influenza vaccination location in Korean adult population. Korean J Fam Pract. (2019) 9:431–7. doi: 10.21215/kjfp.2019.9.5.431
34. ITPI. How Privatization Increases Inequality. (2006). Available online at: https://www.inthepublicinterest.org/report-how-privatization-increases-inequality-2/ (accessed June 16, 2021).
35. Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. (2013) 12:18. doi: 10.1186/1475-9276-12-18
36. Keane C, Marx J, Ricci E, Barron G. The perceived impact of privatization on local health departments. Am J Public Health. (2002) 92:1178–80. doi: 10.2105/AJPH.92.7.1178
37. Schwartz JB, Bhushan I. Improving immunization equity through a public-private partnership in Cambodia. Bull World Health Organ. (2004) 82:661–7. Available online at: https://apps.who.int/iris/handle/10665/269235
Keywords: privatization, contracting out, public health, immunization program, vaccination, socioeconomic position, gender, inequality
Citation: Moon D, Kim S, Kim M-H, Jeong D and Choi H (2021) Contracting Out National Immunization Program Does Not Improve Vaccination Rate Nor Socioeconomic Inequality: A Case Study of Seasonal Influenza Vaccination in South Korea. Front. Public Health 9:769176. doi: 10.3389/fpubh.2021.769176
Received: 01 September 2021; Accepted: 11 October 2021;
Published: 04 November 2021.
Edited by:
Georgi Iskrov, Plovdiv Medical University, BulgariaReviewed by:
Nuria Torner, University of Barcelona, SpainCopyright © 2021 Moon, Kim, Kim, Jeong and Choi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongjo Choi, aG9uZ2pvQGtvbnlhbmcuYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.