- 1Department of Clinical Pharmacy, The First Affiliated Hospital, Zhejiang University, School of Medicine, Hangzhou, China
- 2Zhejiang Provincial Key Laboratory for Drug Evaluation and Clinical Research, Hangzhou, China
- 3College of Medicine, Affiliated Huzhou Hospital, Zhejiang University, Huzhou, China
- 4Department of Cardiology and Atrial Fibrillation Center, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 5Library, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 6Department of Colorectal Surgery, The First Affiliated Hospital, Zhejiang University, School of Medicine, Hangzhou, China
- 7Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, The First Affiliated Hospital, Zhejiang University, School of Medicine, Hangzhou, China
Objective: Data are limited on the psychological disorders of patients with cardiovascular disease during the post-COVID-19 period, although mental health status is associated with morbidity and mortality. We aimed to investigate the prevalence of anxiety and depression and risk factors among patients with cardiovascular disease in the post-pandemic period.
Method: A cross-sectional survey was conducted through opportunistic and snowball sampling in southeast China from 10 October to 24 November. Anxiety and depression were assessed on the hospital anxiety and depression scale (HADS).
Results: A total of 435 patients with hypertension (48.05%), atrial fibrillation (17.24%), coronary artery disease (14.48%), heart failure (9.89%) and other heart diseases (10.34%) completed the survey. Interestingly, most patients reported monthly income comparable to (90.11%) or even greater than (8.51%) pre-pandemic income. The occurrence of anxiety and depression was 11.72 and 9.20%, respectively. Marital status and treatment interruption during the pandemic were independent risk factors for both anxiety and depression. Moreover, current monthly income and access to telemedicine during the pandemic were independent risk factors for anxiety.
Conclusion: Patients with cardiovascular disease may experience anxiety and depression not only because of disease complications but also because of the effects of the pandemic. In facing the global challenge posed by the coronavirus, efforts should be made to improve patients' psychological well-being in the management of populations with cardiovascular disease.
Introduction
COVID-19 was declared a pandemic by the World Health Organization in March of 2020 and continues worldwide (5). First identified in Wuhan, China, in December of 2019, COVID-19 rapidly affected the entire country and then spread to the rest of the world. To effectively stem the spread of the virus, the Chinese government swiftly adopted rigorous and comprehensive measures including enforced quarantine and isolation, and mobilization of medical resources across the country (2). Since April 29th 2020, the lockdown restrictions have gradually been lifted, and virus control entered the post-pandemic stage in China (3).
Cardiovascular diseases are a leading public health problem worldwide (4). Increasing evidence indicates that patients with cardiovascular disease have a higher rate of psychological disorders than is found in the general population, and mental health status is associated with cardiovascular disease morbidity and mortality (6, 7). Previous studies have shown that large-scale disasters such as major health emergencies may trigger stress related disorders such as anxiety, sadness, insomnia and confusion (7, 8). Understanding patients' psychological distress and behavioral responses to emerging infectious diseases may be important in cardiovascular disease management (9). A variety of studies have focused on the effects of COVID-19 on the public during lockdown (10, 11); however, data on the prevalence of psychological disorders in patients with cardiovascular disease in the mitigation stage of the pandemic are limited.
In this cross-sectional study, we aimed to address the rates of anxiety and depression in patients with underlying cardiovascular disease, and to explore the related risk factors during the post-COVID-19 period in China.
Methods
Study Population and Inclusion Criteria
The participants of this cross-sectional survey were recruited from outpatients with cardiovascular disease in the Department of Cardiology of the First Affiliated Hospital, School of Medicine, Zhejiang University, a 5000-bed tertiary hospital and a major referral center between 10 October 2020 and 24 November 2020, using opportunistic and snowball sampling. The participants came from four provinces (Zhejiang, Anhui, Jiangsu and Shanghai) in southeast China, majority (70.80%) were from Zhejiang Province. The regional distribution of the respondents is presented in Figure 1. After scanning a quick response code with their mobile phones, the participants completed the questionnaire in Chinese through an online survey. Illiterate patients were asked to answer orally and have their family members fill in the questionnaire on their behalf.
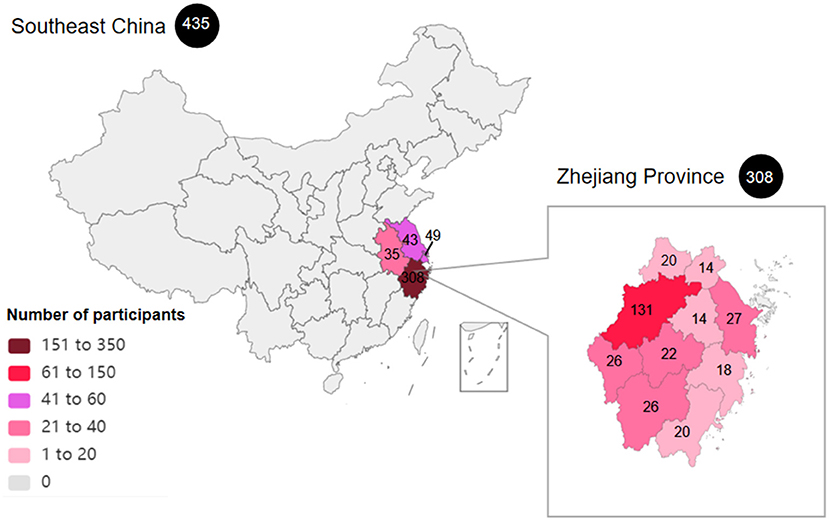
Figure 1. The regional distribution of the patients included in the study. A total of 435 respondents were included in this study from four provinces (Zhejiang, Anhui, Jiangsu and Shanghai) in southeast China. Most participants were from Zhejiang Province.
The inclusion criteria were as follows: (1) patients diagnosed by their managing cardiologists as having cardiovascular disease (including hypertension, coronary artery disease, arrhythmias, heart failure and other heart diseases) according to internationally accepted criteria and (2) patients older than 18 years of age who were current residents of China. Patients were excluded if they could not comprehend the questionnaire or refused to provide consent. The research proposal was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University, on 9 October 2020 (approval No. 2020-EC-598). Informed consent was obtained before all patients voluntarily participated in the survey.
The survey was conducted when local work and daily life gradually returned to normal in most areas of the mainland, while the Chinese government strictly continued virus control for key regions, key target groups and inbound cases (3).
Measures
We designed a two-part questionnaire for this study. First, social-demographic characteristics, clinical information on the participants and their medical experiences during the pandemic were assessed. The second part of the questionnaire comprised the Hospital Anxiety and Depression Scale (HADS) questionnaire.
The HADS questionnaire was used to investigate the rate of anxiety and depression in the participants. It comprises 14 questions: seven associated with the anxiety evaluation (HADS-A) and seven associated with the depression evaluation (HADS-D). Each item was rated on a 4-point scale ranging from 0 to 3. For both HADS-A and HADS-D, we divided the respondents into subgroups by using a cut-off of ≥8 points for depression or anxiety to define pathologic and non-pathologic values, according to the recommendations in the literature (12, 13). Good reliability and validity of the HADS have been reported in a prior study conducted among Chinese residents with cardiovascular diseases (14), in which Cronbach's α values of the HADS, HADS-A subscale and HADS-D subscale were 0.879, 0.806, and 0.806 respectively, and the intra-class correlation coefficients were 0.945, 0.921, and 0.932, respectively. In the current study, the reliability of the HADS was even better, with Cronbach's α coefficients of 0.889 (total scale), 0.804 (HADS-A subscale) and 0.812 (HADS-D subscale).
Statistical Analysis
Statistical analysis was performed in SPSS Statistics v. 22.0 (International Business Machines Corp, Armonk, NY, USA). The normally continuous variables were summarized as mean ± SD (standard deviation) and compared with Student's t-test. For non-normally distributed data, continuous variables were summarized as medians with interquartile ranges (25th and 75th percentiles), and differences in continuous variables were analyzed with the Mann–Whitney U test. Categorical data were reported as the n (%) and compared with Pearson's chi-square test. Independent risk factors for anxiety and depression were assessed with multivariable logistic regression analysis. First, we used univariable analysis to screen the candidate influencing factors, and only variables with P <0.10 were included in multivariable logistic regression models. P < 0.05 was considered statistically significant.
Results
Baseline Demographics
A total of 474 respondents were recruited, among which 435 (91.77%) were valid for analysis. During the period of our survey, there were 53,360 outpatients in our Department of Cardiology, with a participation rate of 0.82%.
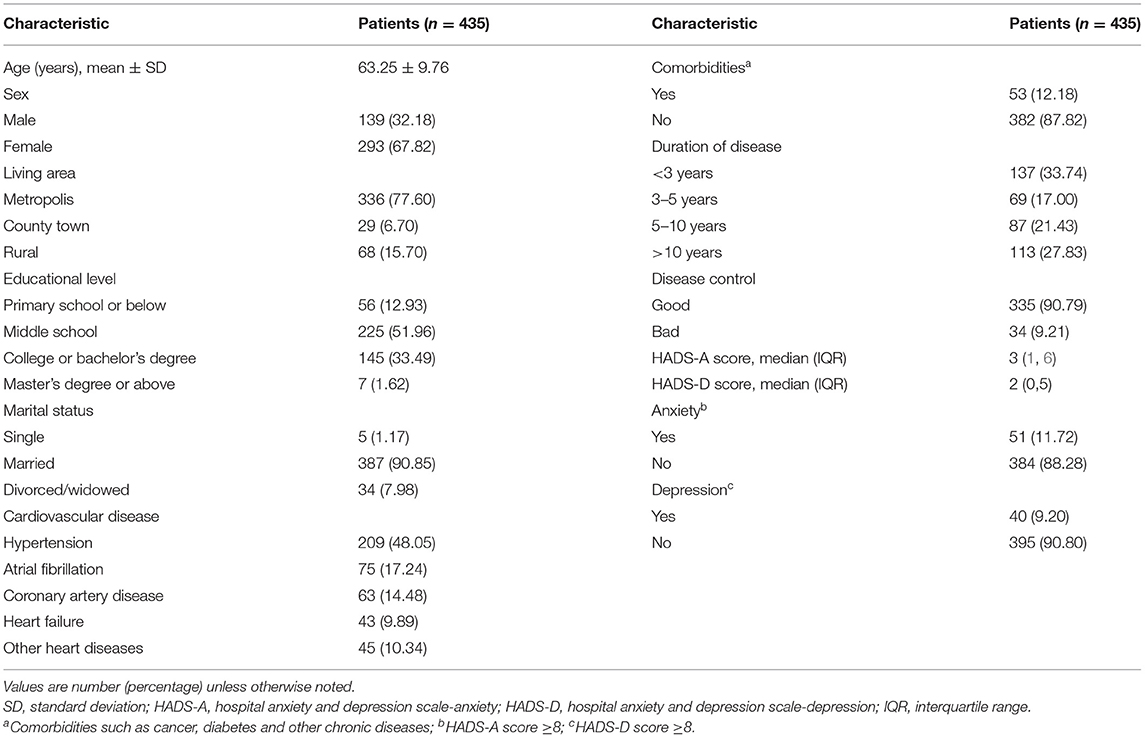
Reasons for exclusion were age younger than 18 years (n = 1) and the presence of other diseases without cardiovascular disease (n = 38). The social-demographic characteristics of respondents are presented in Table 1. In the total sample (n = 435), 139 (32.18%) participants were male, and 293 (67.82%) were female. The mean age of the participants was 63.25 years (SD = 9.76). The cardiovascular disease was characterized as follows: 209 (48.05%), 75 (17.24%), 63 (14.48%) and 43 (9.89%) patients had hypertension, atrial fibrillation, coronary artery disease and heart failure, respectively, and 45 (10.34%) respondents had other heart diseases including rheumatic heart disease, heart valve disease, arrhythmia or cardiomyopathy. A total of 53 (12.18%) patients had other comorbidities with cardiovascular disease, such as cancer, diabetes or other chronic diseases.
The Occurrence of Anxiety and Depression in the Patients
As shown in Table 1, the median HADS-A score of participants with cardiovascular disease was 3 (1,6). According to the cut-off points, 51 (11.72%) patients had anxiety. The median HADS-D score of respondents was 2 (0, 5). According to the categorization of the HADS-D score, 40 (9.20%) patients had depression.
Social and Clinical Risk Factors Associated With Anxiety and Depression
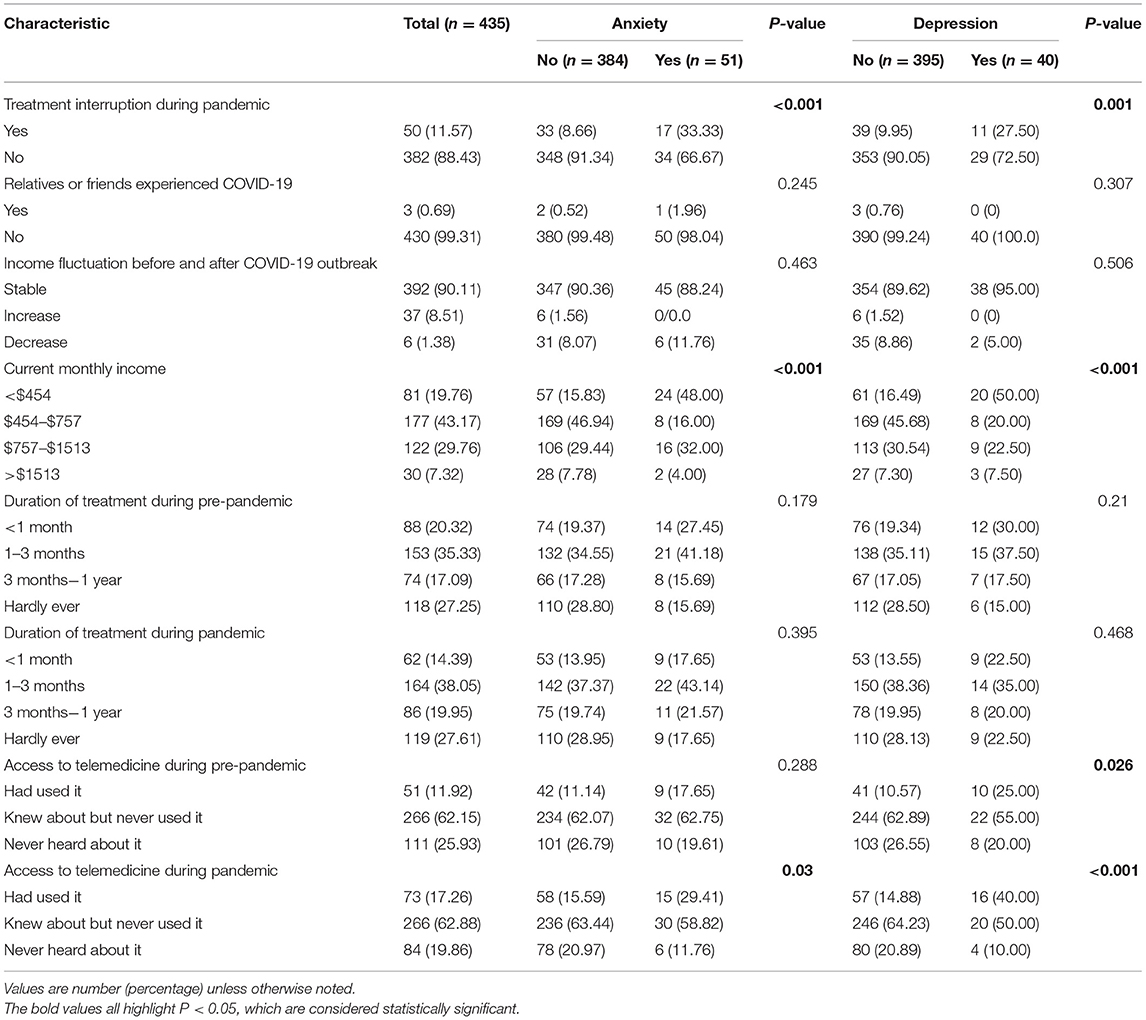
To identify the factor influencing the psychological status, we divided the participants into subgroups with anxiety/non-anxiety and depression/non-depression. Social and clinical risk factors associated with depression and anxiety are summarized in Table 2. Compared with the patients in the non-anxiety/non-depression group, both anxiety and depression were more common in patients who were living in county town or rural areas (39.22 and 47.50%, respectively), who were single/divorced/widowed (17.64 and 17.50%, respectively) and who had an educational level of primary school or below (25.49 and 32.50%, respectively).
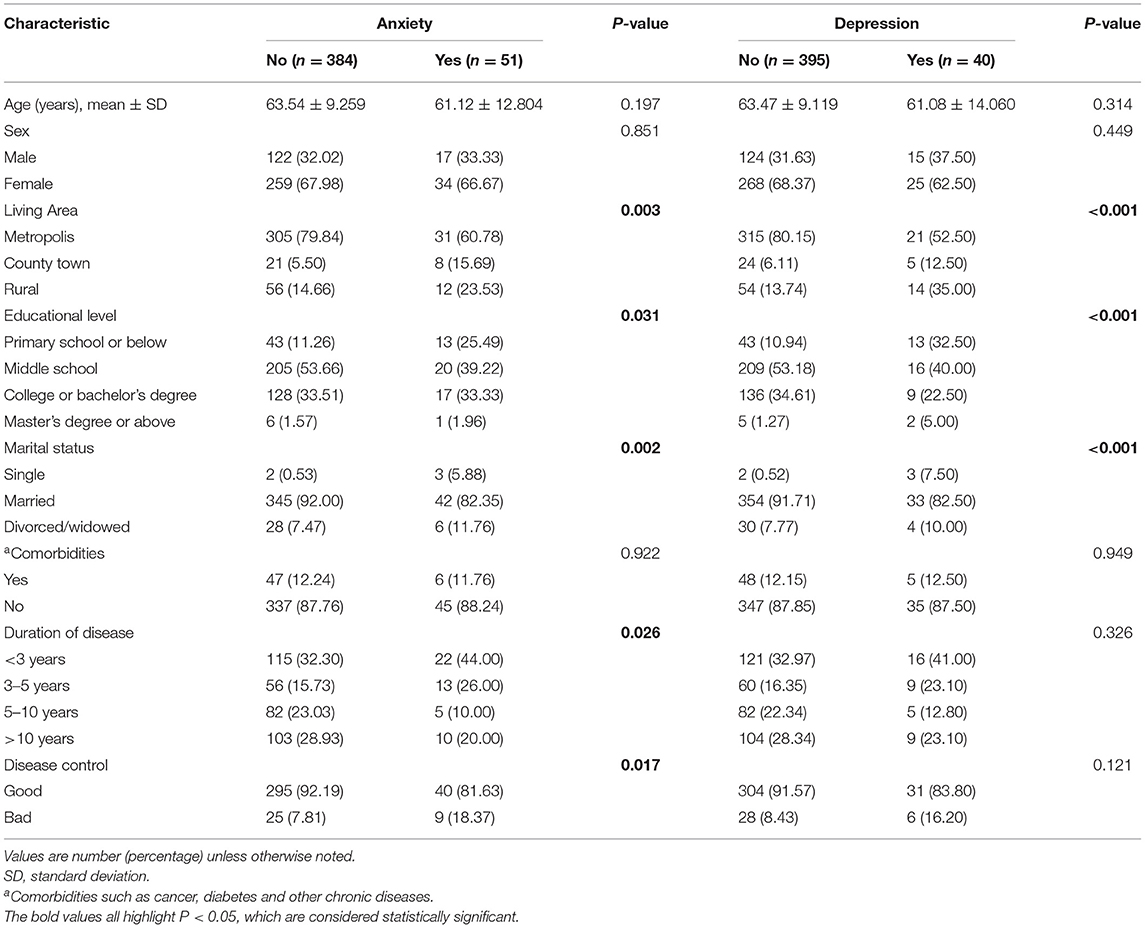
Table 2. Comparison of social and clinical features in patients in the anxiety/non-anxiety and depression/non-depression groups.
Poor disease control was noted in nine (18.37%) patients in the anxiety group and 25 (7.81%) patients in the non-anxiety group (P = 0.017). A significantly greater proportion of patients in the anxiety group than the non-anxiety group had a disease duration below 5 years (70%) and a monthly income of either $454 or below (48.00%) or $757 to $1,513 (32.00%). However, compared with those in the non-depression group, the patients in the depression group had a higher frequency of monthly income of $454 or below (50.00%) or $1,513 or above (7.50%).
COVID-19-Associated Questions and Associations With Anxiety and Depression
COVID-19-associated questions in the two subgroups are presented in Table 3. A total of 392 (90.11%) and 37 (8.51%) patients reported monthly income comparable to or higher than their pre-pandemic income respectively.
Both anxiety and depression were more common in patients who experienced treatment interruption during the pandemic (33.33 and 27.50%, respectively) and who used telemedicine more frequently during the pandemic (29.41 and 40.00%, respectively) than in patients in the non-anxiety/non-depression group. More frequent use of telemedicine during the pre-pandemic period was observed in the depression group than the non-depression group (25.00 vs 0.10.57%, P = 0.026).
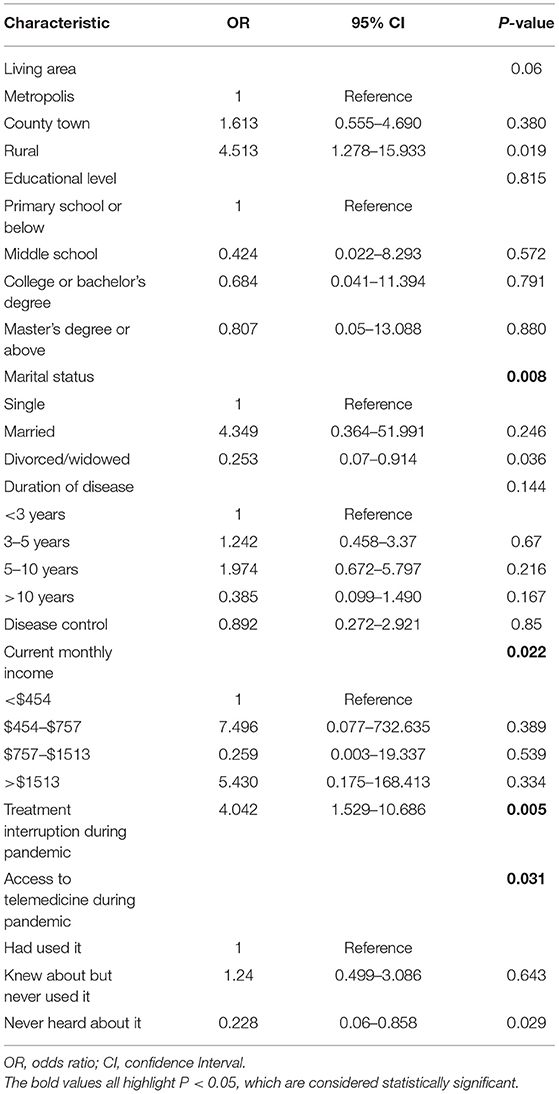
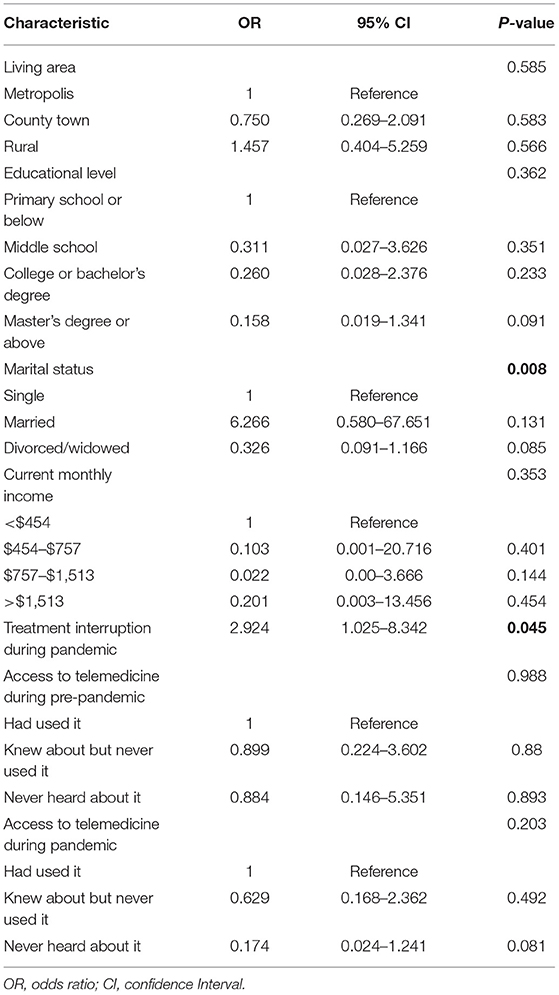
Independent Risk Factors Associated With Anxiety and Depression
Multivariable logistic regression analysis identified that marital status, current monthly income, treatment interruption during the pandemic and access to telemedicine during the pandemic were independent risk factors for anxiety (Table 4). Likewise, multivariable logistic regression analysis indicated that marital status and treatment interruption during the pandemic were independent risk factors for depression (Table 5).
Discussion
During the COVID-19 pandemic, most people experience psychological pressure because of the uncertainty of the development of the pandemic, fear of infection and decreased social activities (15). Little is known about the presence of anxiety and depression among individuals with cardiovascular disease, particularly in the post-pandemic stage.
The results of this current study indicated 11.72 and 9.20% occurrence of anxiety and depression in participants, respectively. Compared with data from the peak stage of the COVID-19 outbreak reported in other studies (18.5–23.5% occurrence of anxiety/depression), the prevalence of psychological disorders among patients with cardiovascular disease appeared to slightly decrease post-pandemic (16, 17). These results are consistent with findings from a study by Chen et al. (18) in Hubei, China, reporting that the prevalence of psychological distress decreased from more than 75% to approximately 15% during the peak and mitigation stages of the pandemic. Because psychological disorders are highly associated with cardiovascular disease morbidity and mortality (5, 13), the importance of patient mental health during the post-pandemic stage should be emphasized. Previous studies have focused only on the effects of temporal lockdown on patients with cardiovascular disease. Here, we provide initial information on patients' mental well-being during the long post-pandemic stage.
To better manage psychological disorders in patients with cardiovascular disease, emerging studies have reported on risk factors for anxiety and depression, and have indicated that female sex (19), low education (6), persistent complications and weakened physical function (20) are risk factors. The present study revealed that marital status was an independent risk factor for both anxiety and depression, and current monthly income was a risk factor for anxiety among patients with cardiovascular disease. Interestingly, most of the respondents had comparable or even greater income than pre-pandemic levels. The Chinese authorities' decisive actions and targeted measures against COVID-19, and the restoration of industrial chains, somewhat mitigated the effects of the crisis.
We observed no significant differences between the anxiety and non-anxiety cardiovascular disease subgroups in having relatives or friends who contracted COVID-19. However, the number of participants was limited, so these results may not robustly reflect real-world conditions.
We found that both anxiety and depression were more frequent in patients experiencing treatment interruption during the pandemic. Thus, ensuring a timely medical service is essential for individuals with cardiovascular disease during the pandemic. Access to telemedicine during the pandemic was confirmed to be an independent risk factor for anxiety in our research. The results of this study also suggest that the COVID-19 crisis has accelerated the spread of telemedicine. More participants have used or heard about telemedicine after the outbreak of the COVID-19 pandemic. Telemedicine may compensate for traditional health care in the management of patients with cardiovascular disease during the pandemic.
Limitations
Although this study is the first analysis addressing the prevalence of anxiety and depression in patients with cardiovascular disease during the mitigation stage of the COVID-19 pandemic, it has some limitations. First, the use of online self-reported questionnaire to measure the mental health of the participants and the small participation rate may have yielded results that do not fully reflect the real-world situation. Second, the cross-sectional research design of the study does not allow for exploration of the longitudinal effects of COVID-19 on patients with cardiovascular disease. Third, the patients' current treatment regimens were not investigated in the study. Finally, this study was conducted in patients with cardiovascular disease in China, and therefore the findings may not be applicable to other populations. Because of the dearth of data in this field, this study, regardless of its limitations, should serve as an impetus for further research in other countries and other patient groups to investigate the long-term effects of the COVID-19 pandemic.
Conclusion
Patients with cardiovascular disease may experience psychological disorders such as anxiety and depression during the post-COVID-19 period. Marital status, current monthly income, treatment interruption during the pandemic and access to telemedicine are independent risk factors. The findings of our study should be helpful in developing policies and strategies for the management of cardiovascular disease.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Clinical Research Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MW and QW were involved in the conception and study design. They were responsible for data collection together with SL, JJ, ZD, and ZS. LS was involved in the writing and revision of the manuscript. LL is a biostatistician who was responsible for the data analysis. All authors were responsible for critical revision of the manuscript.
Funding
This study was supported by the Clinical Research Fund of Zhejiang Provincial Medical Association (2018ZYC-A11), Department of Science and Technology of Zhejiang Province (grant no. LGF19H020011), and the Joint Fund of Zhejiang Provincial Natural Science Foundation (grant no. LYY19H310012), People's Republic of China.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Zhou Xu and Qiao Zhang for their technical support.
References
1. Giorgino F, Bhana S, Czupryniak L, Dagdelen S. Management of patients with diabetes and obesity in the covid-19 era: experiences and learnings from south and east Europe, the Middle East, and Africa. Diabetes Res Clin Pract. (2021) 172:108617. doi: 10.1016/j.diabres.2020.108617
2. Pei Z, Han G, Ma X, Su H. Response of major air pollutants to COVID-19 lockdowns in China. Sci Total Environ. (2020) 743:140879. doi: 10.1016/j.scitotenv.2020.140879
3. Xinhua Net,. Fighting COVID-19: China in Action. (2020). Available online at: http://www.xinhuanet.com/english/2020-06/07/c_139120424.htm (accessed December 22, 2020).
4. Goldstein BI, Carnethon MR, Matthews KA, Mcintyre RS, Miller GE, Raghuveer G. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American heart association. Circulation. (2015) 132:965–86. doi: 10.1161/CIR.0000000000000229
5. Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. (2014) 129:1350–69. doi: 10.1161/CIR.0000000000000019
6. Wang D, Dai F, Liu W, Ge L, Qi X. Longitudinal change and prognostic value of anxiety and depression in coronary heart disease patients. Ir J Med Sci. (2021) 190:107–16. doi: 10.1007/s11845-020-02302-7
7. Cosić K, Popović S, Šarlija M. Impact of Human Disasters and COVID-19 Pandemic on Mental Health: Potential of Digital Psychiatry. Psychiatr Danub. (2020) 32:25–31. doi: 10.24869/psyd.2020.25
8. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
9. Yeung NCY, Lau JTF, Choi KC, Griffiths S. Population Responses during the Pandemic Phase of the Influenza A(H1N1)pdm09 Epidemic, Hong Kong, China. Emerg. Infect. Dis. (2017) 23:813–5. doi: 10.3201/eid2305.160768
10. Shahidi DM, Ahmadzadeh Z, Younespour S. Evaluation of anxiety and depression in patients with morphea taking immunosuppressive drugs during the COVID-19 pandemic. J Dermatolog Treat. (2020) 1–7. doi: 10.1080/09546634.2020.1819528
11. Ngoc CDK, Nguyen LBT, Thi LNP, Vo VT, Phung LT, Pham GA, et al. Psychological impacts of COVID-19 during the first nationwide lockdown in Vietnam: web-based, cross-sectional survey study. JMIR Form Res. (2020) 4:e24776. doi: 10.2196/24776
12. Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. (2003) 1:29. doi: 10.1186/1477-7525-1-29
13. Bäz L, Wiesel M, Möbius-Winkler S, Westphal JG, Schulze PC, Franz M. Depression and anxiety in elderly patients with severe symptomatic aortic stenosis persistently improves after transcatheter aortic valve replacement (TAVR). Int J Cardiol. (2020) 309:48–54. doi: 10.1016/j.ijcard.2020.03.021
14. Sun ZX, Liu HX, Jiao LY, Zhou T, Yang LN, Fan JY. Reliability and validity of hospital anxiety and depression scale. Chin J Clin Electron Ed. (2017) 11:198–201. doi: 10.3877/cma.j.issn.1674-0785.2017.02.005
15. Yang BX, Xia L, Huang R, Chen P, Luo D, Liu Q. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: A survey of Chinese residents. J Nurs Manag. (2021) 29:805–12. doi: 10.1111/jonm.13221
16. Chagué F, Boulin M, Eicher J-C, Bichat F, Saint JM, Cransac-Miet A, et al. Impact of lockdown on patients with congestive heart failure during the coronavirus disease 2019 pandemic. ESC Heart Fail. (2020) 7:4420–3. doi: 10.1002/ehf2.13016
17. Lim SL, Woo KL, Lim E, Ng F, Chan MY. Impact of COVID-19 on health-related quality of life in patients with cardiovascular disease: a multi-ethnic Asian study. Health Qual Life Outcomes. (2020) 18:387. doi: 10.1186/s12955-020-01640-5
18. Chen X, Gao H, Zou Y. Changes in psychological wellbeing, attitude and information-seeking behaviour among people at the epicentre of the COVID-19 pandemic: a panel survey of residents in Hubei province, China. Epidemiol Infect. (2020) 148:e201. doi: 10.1017/S0950268820002009
19. Pajak A, Jankowski P, Kotseva K, Heidrich J, de Smedt D, De Bacquer D, et al. ‘Depression, anxiety, and risk factor control in patients after hospitalization for coronary heart disease: the EUROASPIRE III Study. Eur J Prev Cardiol. (2013) 20:331–40. doi: 10.1177/2047487312441724
Keywords: cardiovascular disease, COVID-19, anxiety, depression, risk factors
Citation: Wu M, Shen L, Wang Q, Liu L, Lu S, Jin J, Dai Z and Shu Z (2022) Anxiety and Depression Prevalence and Risk Factors Among Patients With Cardiovascular Diseases in Post-COVID-19 China. Front. Public Health 9:758874. doi: 10.3389/fpubh.2021.758874
Received: 28 August 2021; Accepted: 07 December 2021;
Published: 04 January 2022.
Edited by:
Umberto Volpe, Marche Polytechnic University, ItalyReviewed by:
Yanping Bao, Peking University, ChinaDenis Comte, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland
Copyright © 2022 Wu, Shen, Wang, Liu, Lu, Jin, Dai and Shu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiqi Wang, 1508036@zju.edu.cn
 Minglan Wu
Minglan Wu Liying Shen3
Liying Shen3 Qiqi Wang
Qiqi Wang