
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 02 December 2021
Sec. Occupational Health and Safety
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.751579
This article is part of the Research TopicAssessing Shift Work and its Health ImpactsView all 11 articles
 Yuzhou Huang1,2,3
Yuzhou Huang1,2,3 Danrong Jing1,2,3*
Danrong Jing1,2,3* Juan Su1,2,3
Juan Su1,2,3 Zhijun Huang4
Zhijun Huang4 Han Liu5
Han Liu5 Juan Tao6
Juan Tao6 Meian He7
Meian He7 Xiang Chen1,2,3,8
Xiang Chen1,2,3,8 Minxue Shen1,2,3,8,9
Minxue Shen1,2,3,8,9 Yi Xiao1,2,3*
Yi Xiao1,2,3*Purpose: Night shift work is common in the current working environment and is a risk factor for many diseases. The study aimed to explore the relationship between night shift work with chronic spontaneous urticaria (CSU), and the modification effect of circadian dysfunction on it.
Methods: A cross-sectional survey was conducted among Chinese workers. Exposure was measured by night work history and duration. Circadian dysfunction was characterized by excessive daytime sleepiness (EDS). The diagnosis of CSU was made by dermatologists who were investigating on the spot. The effect size was expressed as odds ratios (ORs).
Results: A total of 8,057 participants were recruited, and 7,411 (92%) with complete information were included in the final analyses. The prevalence rates of CSU for workers without night shift and those with night shift history were 0.73 and 1.28%, respectively. Compared with workers who never worked night shifts, the risk of CSU increased with the length of night shift work: OR = 1.55 (95% confidence interval [CI]: 0.78–3.06) for duration <5 years and OR = 1.91 (95% CI: 1.12–3.26) for duration ≥5 years. EDS s EDS has been shown to modify this combination. Among workers without EDS, there was no association between night shift and CSU (OR = 0.94; 95% CI: 0.49–1.79). Whereas, in participants with EDS, the correlation was significant (OR = 3.58; 95% CI: 1.14–11.20). However, the effect modification by sleep disturbance was not observed.
Conclusions: Night shift work is a risk factor for CSU, and there is a dose-response relationship between night shift work hours and the risk of CSU. This connection may be modified by circadian dysfunction.
Chronic spontaneous urticaria (CSU) is a common allergic skin disorder characterized by wheals or angioedema along with intense itch (1). Although it is usually self-limited and benign, it can cause severe discomfort, lasting from months to years, and rarely represents a serious systemic disease or life-threatening allergic reaction (2). It affects 0.5–1% (1) of the general population, and 0.1–0.3% (3) of children. The burden of urticaria ranked the 5th among all skin conditions according to the 2016 Global Burden of Disease Study. It was estimated that urticaria contributed to 55.49 per 100,000 years loss of healthy life globally (4). The pathophysiology of CSU has not been fully elucidated, but it is clear that the degranulation of mast cells and activation of basophil play the core role in the etiology of urticaria. Previous studies suggest that CSU occurs mostly at night or in the evening with no identifiable triggers, and the severity of cutaneous signs and symptoms is also exacerbated between midnight and morning and shows a significant 24-h rhythm (5–7).
Night shift work is defined as work performed outside of typical daytime work hours. Night shift work is common in the industry to ensure the need for 24-h operation. In industrialized countries, about 20% of the workforce is engaged in shift work (8). Night shift work is a well-established social and biological stress. Previous epidemiological studies suggest that night shift work is a risk factor for obesity (9), diabetes (10, 11), cardiovascular disease (12), breast cancer (13), and mental disorders (14, 15). Night shift work can lead to daily sleep-wake and fasting cycles, and the imbalance of the endogenous circadian timing system, which wildly affects the physiology and behavior, and harmfully influences healthy immune and allergy system.
However, no epidemiologic study has examined the association of night shift work and CSU. In the current study, we conducted a cross-sectional investigation in two groups of workers who frequently worked night shifts. The aim was to investigate the association of night shift work with CSU and to examine the effect modification by circadian dysfunction.
Cross-sectional data from two independent studies were analyzed. The study population comprised of automobile manufacture workers in Shiyan, Hubei who were participants in the Dongfeng-Tongji Cohort Study (16), and non-ferrous metal smelting workers in Hengyang, Hunan who were participants in the Hunan Chronic Disease Cohort Study (17). The Dongfeng-Tongji Cohort was established in 2008 and initially recruited retired workers. The cohort began to recruit in-service workers since 2016. In the current analysis, we used the baseline data collected from the in-service workers. The Hunan Chronic Disease Cohort Health Study was established in 2015 and recruited residents and workers in Hunan rural regions. In the current analysis, we only included participants who were workers to ensure comparability and homogeneity.
History and duration (years) of rotating night shift work were inquired in the face-to-face interview. Night shift work was defined as “at least three nights per month in addition to working days or evenings.” If a history of the night shift was reported, the cumulative night shift work was then inquired by the investigator. The duration of night shift work was categorized into three groups: never, <5 years, and ≥5 years.
Diagnosis of skin diseases and inquiry of disease history were performed by certificated dermatologists during the field survey. Clinical manifestation, disease history, and family history of participants were asked, and physical examinations were conducted to diagnose all skin diseases. CSU was diagnosed according to persistent or recurrent typical clinical manifestations of urticaria, with unknown triggers, for more than 6 weeks during the past year.
Height and weight were measured by research nurses according to standardized methods. Body mass index (BMI) was calculated as weight (kg)/height2 (m2). Marital status, socioeconomic status (annual family income and educational level), smoking habits, and passive smoke exposure, and alcohol drinking were inquired by investigators. Anxiety and depression were assessed by the 2-item Generalized Anxiety Disorder (GAD-2) (18) and 2-item Patient Health Questionnaire (PHQ-2) (19), respectively. GAD-2 ≥3 and PHQ-2 ≥3 were the cut-offs for anxiety and depression, respectively. Sleep quality and daytime sleepiness were assessed by the Pittsburgh Sleep Quality Index (PSQI) (20) and Epworth Sleepiness Scale (ESS) (21), respectively. PSQI >5 and ESS >10 were the cut-offs for sleep disturbance and excessive daytime sleepiness (EDS), respectively. History of urticaria was not adjusted since it may cause collider bias in the hypothesized pathway: history of night shift (X) → history of CSU (C1) ← genetic susceptibility (C2) → current CSU (Y).
Continuous data were presented as means and standard deviations, and between-group difference was tested using analysis of variance (ANOVA). Categorical data were presented as number (%), and the between-group difference was tested using the chi-square test. A two-level logistic regression model (participant as level-1 unit and study site as a level-2 unit) was used to estimate the association of night shift work with CSU, adjusting for level-1 covariates (age, gender, ethnicity, annual family income, cigarette smoking, alcohol drinking, anxiety, depression) and the random effect (intercept) of study sites. The effect size was presented as odds ratio (OR) and 95% confidence interval (CI). The center effect was examined using the intra-cluster correlation coefficient (ICC). Cubic spline regression was used to examine the potential non-linear association of the duration of night shift work (years) with the prevalence of CSU.
Previous studies have identified associations between circadian and health outcomes (22), and effect modification of associations between night shift work and diseases by circadian and chronotype (11, 23, 24). Therefore, we assessed possible effect modifications of the association between night shift work and CSU by EDS, an indicator of circadian dysfunction. To test for effect modification, we included a multiplicative interaction term in regression models. Stratification analysis by EDS was then conducted if a significant interaction term was identified. In addition, subgroup analysis was conducted by sleep disturbance as determined by PSQI. P < 0.05 was considered statistically significant for all tests. Statistical analysis was performed in SAS 9.4 (SAS Institute Inc., Cary, USA).
A total of 8,057 participants were recruited, and 7,411 (92%) with complete information were included in the final analyses (Figure 1). The mean age was 42.5 ± 8.4 years and 74.9% were male. Comparing the characteristics across the history and duration of night shift work, night shifts were associated with slightly older age, male gender, the Han ethnicity, lower socioeconomic stratum (income and education), smoking behavior, more impaired sleep quality, and more symptoms of depression (Table 1).
The overall prevalence of CSU was 1.07% (79/7,411). The prevalence rates in the two study sites were 1.05% (Shiyan) and 1.17% (Hengyang), respectively, and the center effect of clinical diagnosis was not identified according to the two-level null model (ICC = 0%). In workers who reported no history of night shifts, the prevalence of CSU was 0.73%, while in those who reported a history of night shifts, the prevalence rate was 1.28% (P = 0.025). Among subjects who ever worked night shifts, the prevalence rates of CSU were 1.14 and 1.33% in subjects who reported duration <5 years and ≥5 years, respectively (Supplementary Table 1).
Night shift work was significantly associated with a higher risk of CSU in a dose-response manner when adjustments were made for age and gender (Figure 2A). Compared with workers who never worked night shifts, the risk increased with the duration of night shift work: OR = 1.55 (95% CI: 0.78–3.06) for duration <5 years and OR = 1.91 (95% CI: 1.12–3.26) for duration ≥5 years. However, when more covariates were included in the models, the result was not statistically significant, although the effect size still indicated a higher risk of CSU (OR = 1.41; 95% CI: 0.82–2.44; P = 0.216).
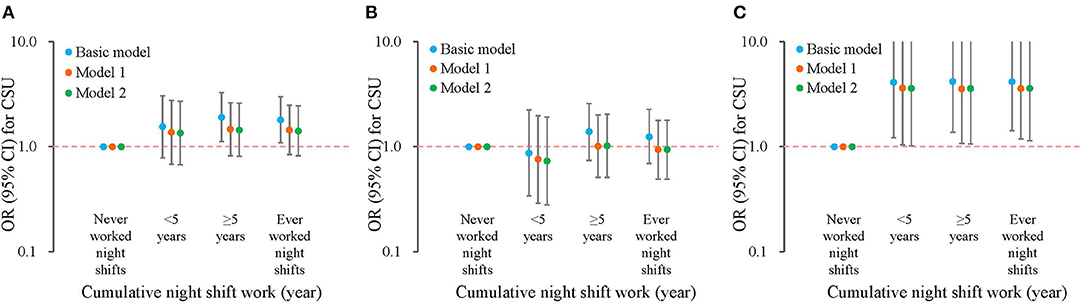
Figure 2. Association of night shift work and chronic spontaneous urticaria, stratified by excessive daytime sleepiness. The basic model was adjusted for age and gender; model 1 was additionally adjusted for ethnicity, marital status, income, educational level; model 2 was additionally adjusted for smoking, passive smoke exposure, alcohol drinking, anxiety, and depression. Logarithmic axis was used for odds ratios. (A) All participants; (B) participants without EDS; (C) participants with EDS. CSU, chronic spontaneous urticaria. EDS, excessive daytime sleepiness; OR, odds ratio; CI, confidence interval.
The possible non-linear association of the duration of night shift work as a continuous variable with CSU was examined with the cubic spline. In general, the duration of the night shift was positively associated with CSU, but variations could be observed (Figure 3A).
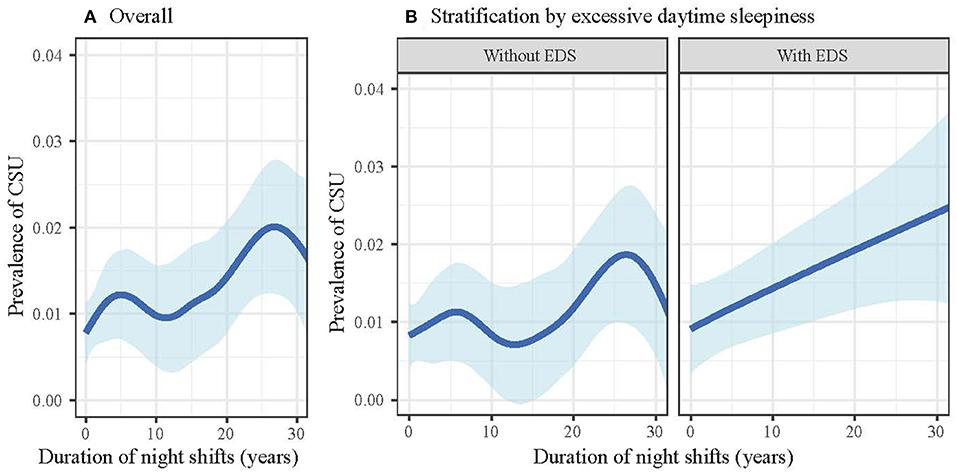
Figure 3. Duration of night shift work and the prevalence of chronic spontaneous urticaria, stratified by excessive daytime sleepiness. The blue curve signifies the estimated prevalence of urticaria, and the light blue band signifies the 95% confidence interval. (A) All participants; (B) stratification analysis by EDS. CSU, chronic spontaneous urticaria; EDS, excessive daytime sleepiness.
A multiplicative interaction term between EDS and night shift work was then included in regression models. After adjustments, a significant interaction term was identified (β = 1.33, P = 0.032), indicating a modification effect. Stratification analysis by EDS was then conducted (Supplementary Table 1). In participants without EDS, the effect size of night shift work was close to null (OR = 0.94; 95% CI: 0.49–1.79; P = 0.841) (Figure 2B). In contrast, in workers with EDS, night shift work was significantly associated with CSU (OR = 3.58; 95% CI: 1.14–11.20; P = 0.029) after full adjustments with a greater effect size (Figure 2C).
Similarly, when treating the duration of night shift as a continuous variable, the association of night shift with CSU was an irregular curve in subjects without EDS; while in those with EDS, night shift was almost linearly associated with CSU (Figure 3B). We also examined the effect of modification by sleep disturbance. However, the associations of night shift work with CSU were consistent in two subgroups (Supplementary Figure 1).
This cross-sectional study investigated the association of night shift work with CSU among Chinese workers. Unique effect modification by daytime alertness was identified, leading to differential associations of night shift work with CSU. That is, in workers with specific circadian dysfunction manifested as daytime sleepiness, the night shift was a risk factor for CSU with strong effect size, while in those with normal daytime alertness, the effect of night shift diminished substantially.
We identified a correlation between night shift work and CSU, and the risk of CSU increased with the duration of night shift work compared to workers who have never worked overnight. Since the early 1960's, many reports have confirmed the importance of circadian rhythm in allergic diseases (25, 26). Allergy-related peripheral clocks (e.g., mast cell clocks) have been considered as significant drivers for rhythmic allergic reactions. Recent studies have shown that abnormal light/dark environments that mimic jet lag can exacerbate viral-induced asthma-like inflammation. When studying the relationship between night work and food allergies, nurses who participated in night shifts had a higher incidence of food allergies than nurses worked as a regular shift schedule (27). Collectively, these studies suggest that mismatched environmental zeitgeber arrivals may exacerbate allergic reactions.
Urticaria is caused by the release of histamine and other inflammatory mediators from mast cells and basophils mediated by immunoglobulin E- and non-immunoglobulin E. (2). CSU is an endogenous disease that is closely related to autoimmunity, especially the immunoglobulin G (IgG) antibody to the alpha subunit of the IgE receptor, which is seen in 35–40% of patients. Basophils and cutaneous mast cells can be activated, leading to a late-phase-like perivascular infiltration about small venules and hive formation (28). Several in vivo studies demonstrated that circadian rhythms drive daily rhythms in IgE/mast cell-mediated allergic reactions. It was reported that wild-type mice had a 24-h time-dependent change in passive skin allergic reaction and passive systemic allergic reaction of IgE/mast cell-dependent allergic reactions (29). Similarly, this time-dependent change also did not occur in mice undergoing mechanical disruption of the central suprachiasmatic nucleus clock or in mice undergoing adrenalectomy (30, 31). These findings suggest that the circadian clock plays a crucial role in the production of daily rhythms of IgE/mast cell-mediated allergic reactions (32).
Based on the stratification analysis, we found that EDS showed a modification effect on this association. While no study or report that directly support our epidemiological finding, a genome-wide association study identified a total of 42 loci and genes to be associated with EDS (33). Among the genes involving EDS reported by Wang et al., four genes [DOCK1 (34), ERBB4 (35), SLC39A8 (36), and CACNA1C (37)] were reported to be associated with allergic reactions in previous studies. Among them, DOCK1 (34), ERBB4 (35), and SLC39A8 (36) were reported to be related to asthma, and CACNA1C (37) was proved to impact the prognosis of CSU. Despite the lack of direct evidence, we speculate that night shift may result in certain epigenetic changes on the genes that link EDS and allergy. This hypothesis needs further investigation.
The study was the first to investigate the association of night work with CSU. The study has several strengths. First, we introduced several covariates that might confound the association of night shift with CSU, including income, education, smoking, alcohol, depression, and EDS. Second, the sample size of the study was relatively large, and night shift work was common among workers; this enables us to investigate the association with sufficient power of a statistical test. Third, this was a population-based study, and the Berkson bias was minimized compared to hospital-based studies.
The primary limitation of the study is that no conclusion on the causal relationship can be drawn owing to the cross-sectional design. Second, the study population was workers; this may limit the external validity of the findings and the generalizability to populations. Last but not least, workers might be exposed to complex occupational factors that were not observed in our study. For example, the level of physical activity of workers is higher than that of the general population (38), and they may be exposed to occupational risks including heavy metals, environmental pollutants, and noise at work (39). Nevertheless, the dose and type of occupational exposures are not likely to be altered by the timing of work.
In summary, we identified a link between night shift work and CSU. Circadian dysfunction might modify the association of night work with CSU. Future research may require more delicate assessment on the exposure to night shift work as well as longitudinal observations on its effect on the incident CSU. This study has clinical implication for dermatologists and primary care physicians with respect to the treatment and management of CSU. The study also provides new evidences for mechanism studies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by this study was conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving study participants were approved by the Institutional Research Ethics Boards of Xiangya School of Public Health, Central South University (approve# XYGW-2016-10), School of Public Health, Tongji Medical College, Huazhong University of Science and Technology (approve# 2016-IEC-S128), and Hubei University of Medicine (approve# 2016-74-41). Written informed consent was obtained from all participants before the investigation. The patients/participants provided their written informed consent to participate in this study.
ZH, MH, XC, and MS designed the study. MS and DJ analyzed the data. YX and YH drafted the manuscript. YH, DJ, JS, ZH, HL, JT, MH, and XC interpreted the data and critically revised the manuscript. JS and MH obtained the funding. All authors participated in the field survey, data collection, and gave final approval to the version submitted for publication.
This work was supported by the National Key Research and Development Project of China Precision Medicine Initiative (2016YFC0900802) and the Program of Introducing Talents of Discipline to Universities (111 Project, No. B20017).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank the following dermatologists and investigators who participated in the field survey (in order of family name). Central South University: Liping Chen, Yihuan Gong, Junweichen Guo, Xiaoyan Huang, Jia Li, Dan Liu, Yuyan Ouyang, Xiangmei Ren, Ke Sha, Yajie Tang, Yaling Wang, Xingyu Zhang, Bolan Zheng, Lei Zhou, and Qian Zhou. Huazhong University of Science and Technology: Yan Li, Xiuling Liu, Yingli Nie, Huinan Suo, Bingbing Wang, Zhen Ye, Jing Yuan, Li Zhu, and Yanming Zhu. Sinopharm Dongfeng General Hospital: Yaqi Dong, Yuxia Hu, Zhenzhen Huang, Yang Jiang, Cuiting Li, Limin Luo, Ping Sheng, Jiao Wei, Yuran Wu, and Xiao Xiong. The content of this manuscript has been presented at the Conference name Virtual Conference of the Society-for-Investigative-Dermatology (SID) (40).
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.751579/full#supplementary-material
1. Zuberbier T, Aberer W, Asero R, Abdul Latiff AH, Baker D, Ballmer-Weber B, et al. The EAACI/GA(2)LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. (2018) 73:1393–414. doi: 10.1111/all.13397
2. Schaefer P. Acute and chronic urticaria: evaluation and treatment. Am Fam Phys. (2017) 95:717–24.
3. Scheindlin S. Chronic urticaria and angioedema. N Engl J Med. (2002) 347:1724. doi: 10.1056/NEJM200211213472122
4. Maxim E, Aksut C, Tsoi D, Dellavalle R. Global burden of urticaria: Insights from the 2016 Global Burden of Disease Study. J Am Acad Dermatol. (2018) 79:567–9. doi: 10.1016/j.jaad.2018.02.026
5. Yosipovitch G, Ansari N, Goon A, Chan YH, Goh CL. Clinical characteristics of pruritus in chronic idiopathic urticaria. Br J Dermatol. (2002) 147:32–6. doi: 10.1046/j.1365-2133.2002.04758.x
6. Maurer M, Ortonne JP, Zuberbier T. Chronic urticaria: an internet survey of health behaviours, symptom patterns and treatment needs in European adult patients. Br J Dermatol. (2009) 160:633–41. doi: 10.1111/j.1365-2133.2008.08920.x
7. Smolensky MH, Portaluppi F, Manfredini R, Hermida RC, Tiseo R, Sackett-Lundeen LL, et al. Diurnal and twenty-four hour patterning of human diseases: acute and chronic common and uncommon medical conditions. Sleep Med Rev. (2015) 21:12–22. doi: 10.1016/j.smrv.2014.06.005
8. Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM. Prevalence rates of work organization characteristics among workers in the U.S.: data from the 2010 National Health Interview Survey. Am J Indus Med. (2013) 56:647–59. doi: 10.1002/ajim.22108
9. Sun M, Feng W, Wang F, Li P, Li Z, Li M, et al. Meta-analysis on shift work and risks of specific obesity types. Obes Rev. (2018) 19:28–40. doi: 10.1111/obr.12621
10. Luca M, Bellia S, Bellia M, Luca A, Calandra C. Prevalence of depression and its relationship with work characteristics in a sample of public workers. Neuropsychiatric Dis Treatment. (2014) 10:519–25. doi: 10.2147/NDT.S56989
11. Vetter C, Devore EE, Ramin CA, Speizer FE, Willett WC, Schernhammer ES. Mismatch of sleep and work timing and risk of type 2 diabetes. Diabetes Care. (2015) 38:1707–13. doi: 10.2337/dc15-0302
12. Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, et al. Association between rotating night shift work and risk of coronary heart disease among women. JAMA. (2016) 315:1726–34. doi: 10.1001/jama.2016.4454
13. Pham TT, Lee ES, Kong SY, Kim J, Kim SY, Joo J, et al. Night-shift work, circadian and melatonin pathway related genes and their interaction on breast cancer risk: evidence from a case-control study in Korean women. Sci Rep. (2019) 9:10982. doi: 10.1038/s41598-019-47480-2
14. Ferri P, Guadi M, Marcheselli L, Balduzzi S, Magnani D, Di Lorenzo R. The impact of shift work on the psychological and physical health of nurses in a general hospital: a comparison between rotating night shifts and day shifts. Risk Manage Healthcare Policy. (2016) 9:203–11. doi: 10.2147/RMHP.S115326
15. Lee A, Myung SK, Cho JJ, Jung YJ, Yoon JL, Kim MY. Night shift work and risk of depression: meta-analysis of observational studies. J Korean Med Sci. (2017) 32:1091–6. doi: 10.3346/jkms.2017.32.7.1091
16. Wang F, Zhu J, Yao P, Li X, He M, Liu Y, et al. Cohort Profile: the Dongfeng-Tongji cohort study of retired workers. Int J Epidemiol. (2013) 42:731–40. doi: 10.1093/ije/dys053
17. Yang F, Yi X, Guo J, Xu S, Xiao Y, Huang X, et al. Association of plasma and urine metals levels with kidney function: A population-based cross-sectional study in China. Chemosphere. (2019) 226:321–8. doi: 10.1016/j.chemosphere.2019.03.171
18. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Internal Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
19. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
20. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
21. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. (1991) 14:540–5. doi: 10.1093/sleep/14.6.540
22. Vetter C, Chang SC, Devore EE, Rohrer F, Okereke OI, Schernhammer ES. Prospective study of chronotype and incident depression among middle- and older-aged women in the Nurses' Health Study II. J Psychiatr Res. (2018) 103:156–60. doi: 10.1016/j.jpsychires.2018.05.022
23. Videnovic A, Noble C, Reid KJ, Peng J, Turek FW, Marconi A, et al. Circadian melatonin rhythm and excessive daytime sleepiness in Parkinson disease. JAMA Neurol. (2014) 71:463–9. doi: 10.1001/jamaneurol.2013.6239
24. Strohmaier S, Devore EE, Vetter C, Eliassen AH, Rosner B, Okereke OI, et al. Night shift work before and during pregnancy in relation to depression and anxiety in adolescent and young adult offspring. Eur J Epidemiol. (2019) 34:625–35. doi: 10.1007/s10654-019-00525-2
25. Smolensky MH, Lemmer B, Reinberg AE. Chronobiology and chronotherapy of allergic rhinitis and bronchial asthma. Adv Drug Delivery Rev. (2007) 59:852–82. doi: 10.1016/j.addr.2007.08.016
26. Fishbein AB, Vitaterna O, Haugh IM, Bavishi AA, Zee PC, Turek FW, et al. Nocturnal eczema: Review of sleep and circadian rhythms in children with atopic dermatitis and future research directions. J Allergy Clin Immunol. (2015) 136:1170–7. doi: 10.1016/j.jaci.2015.08.028
27. Yang G, Zhang H, Liu Y, Feng Y, Luo XQ, Liu ZQ, et al. Alternation of circadian clock modulates forkhead box protein-3 gene transcription in CD4(+) T cells in the intestine. J Allergy Clin Immunol. (2016) 138:1446–9.e10. doi: 10.1016/j.jaci.2016.04.035
28. Kaplan AP. Diagnosis, pathogenesis, and treatment of chronic spontaneous urticaria. Allergy Asthma Proc. (2018) 39:184–90. doi: 10.2500/aap.2018.39.4121
29. Nakamura Y, Harama D, Shimokawa N, Hara M, Suzuki R, Tahara Y, et al. Circadian clock gene Period2 regulates a time-of-day-dependent variation in cutaneous anaphylactic reaction. J Allergy Clin Immunol. (2011) 127:1038–45.e1-3. doi: 10.1016/j.jaci.2011.02.006
30. Nakamura Y, Ishimaru K, Tahara Y, Shibata S, Nakao A. Disruption of the suprachiasmatic nucleus blunts a time of day-dependent variation in systemic anaphylactic reaction in mice. J Immunol Res. (2014) 2014:474217. doi: 10.1155/2014/474217
31. Nakamura Y, Nakano N, Ishimaru K, Hara M, Ikegami T, Tahara Y, et al. Circadian regulation of allergic reactions by the mast cell clock in mice. J Allergy Clin Immunol. (2014) 133:568–75. doi: 10.1016/j.jaci.2013.07.040
32. Nakao A, Nakamura Y, Shibata S. The circadian clock functions as a potent regulator of allergic reaction. Allergy. (2015) 70:467–73. doi: 10.1111/all.12596
33. Wang H, Lane JM, Jones SE, Dashti HS, Ollila HM, Wood AR, et al. Genome-wide association analysis of self-reported daytime sleepiness identifies 42 loci that suggest biological subtypes. Nat Commun. (2019) 10:3503. doi: 10.1016/j.sleep.2019.11.1140
34. Tremblay K, Lemire M, Potvin C, Tremblay A, Hunninghake GM, Raby BA, et al. Genes to diseases (G2D) computational method to identify asthma candidate genes. PLoS ONE. (2008) 3:e2907. doi: 10.1371/journal.pone.0002907
35. Park H-W, Song W-J, Cho S-H, McGeachie MJ, Martinez F, Mauger D, et al. Assessment of genetic factor and depression interactions for asthma symptom severity in cohorts of childhood and elderly asthmatics. Experi Mol Med. (2018) 50:110. doi: 10.1038/s12276-018-0110-5
36. Mak ACY, White MJ, Eckalbar WL, Szpiech ZA, Oh SS, Pino-Yanes M, et al. Whole-genome sequencing of pharmacogenetic drug response in racially diverse children with asthma. Am J Respir Crit Care Med. (2018) 197:1552–64. doi: 10.1164/rccm.201712-2529OC
37. Yan J, Li Q, Luo Y, Yan S, He Y, Chen X. [Association of CACNA1C gene genetic polymorphism with the susceptibility as well as prognosis for chronic spontaneous urticaria]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2018) 43:929–36. doi: 10.11817/j.issn.1672-7347.2018.09.001
38. Dalene K, Tarp J, Selmer R, Ariansen I, Nystad W, Coenen P, et al. Occupational physical activity and longevity in working men and women in Norway: a prospective cohort study. Lancet. (2021) 6:e386–95. doi: 10.1016/S2468-2667(21)00032-3
39. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
Keywords: circadian dysfunction, chronic spontaneous urticaria, effect modification, night shift work, excessive daytime sleepiness
Citation: Huang Y, Jing D, Su J, Huang Z, Liu H, Tao J, He M, Chen X, Shen M and Xiao Y (2021) Association of Night Shift Work With Chronic Spontaneous Urticaria and Effect Modification by Circadian Dysfunction Among Workers. Front. Public Health 9:751579. doi: 10.3389/fpubh.2021.751579
Received: 01 August 2021; Accepted: 03 November 2021;
Published: 02 December 2021.
Edited by:
Zenon Brzoza, Opole University, PolandReviewed by:
Antonino Maniaci, University of Catania, ItalyCopyright © 2021 Huang, Jing, Su, Huang, Liu, Tao, He, Chen, Shen and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Danrong Jing, MTU4NzQ4ODQ1MDZAMTYzLmNvbQ==; Yi Xiao, eGlhb3lpeHlAY3N1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.