
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health , 11 November 2021
Sec. Aging and Public Health
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.743804
This article is part of the Research Topic Aging Research and Practices in Malaysia View all 23 articles
 Zhi Ling Ng1
Zhi Ling Ng1 Hazwan Mat Din2
Hazwan Mat Din2 Nor Fadhlina Zakaria1
Nor Fadhlina Zakaria1 Liyana Najwa Inche Mat3
Liyana Najwa Inche Mat3 Wan Zul Haikal Wan Zukiman1
Wan Zul Haikal Wan Zukiman1 Anim Md Shah1
Anim Md Shah1 Ummi Nadira Daut1
Ummi Nadira Daut1 Hakimah Mohammad Sallehuddin1,2*
Hakimah Mohammad Sallehuddin1,2*Clinical practise in the ageing population is changing from organ-specific specialty care to holistic care. This is done through comprehensive geriatric assessment and multi-disciplinary team management. Hence, we adopted an approach consisting of multi-professional teachers teaching a Healthcare of Elderly Course (HEC), in a public university in Malaysia. We aimed to analyze the students' attitude, self-perceived competency and interest in geriatric medicine as a career before and after the course. We also investigated variables that might influence this interest among these students. All 96 students in the course were invited to participate in the survey. Sixty-eight (70.8%) completed both pre and post-course questionnaires. Although most students (93%) have a positive attitude (University of California at Los Angeles Geriatric Attitude Scale >3) toward older adults at baseline, it did not significantly increase post-course. We found that the mean scores for self-perceived competency increased from 3.62 (±0.76) to 3.81 (±0.56) post-course (p < 0.01). However, the students remained neutral with no significant change in the mean interest in pursuing a geriatric medicine career after the course. Students with higher self-perceived competency post-course were found to be more interested in geriatric medicine (β = 0.56, p < 0.001). In conclusion, the HEC in our centre could sustain a positive attitude and increase self-perceived competency in students. It is important to increase the preparedness of our graduates in managing older adults with frailty and multimorbidity. Future studies may involve inter-professional education of students from multiple disciplines undergoing the same course to nurture real-life collaborations in managing the ageing population.
In a rapidly ageing Asia, where it is projected to be the home of more than half of the aged population of the world by 2050, developing a competent workforce in managing ageing and age-related diseases becomes an utmost priority (1). The first national survey on the teaching of geriatric medicine in Malaysian medical schools showed that the most prominent barrier to curriculum delivery was the lack of expertise, followed by the subject not being included in the curriculum. It was shown that none of the core geriatric competencies achieved a 100% coverage, and only a third of the participating medical schools had access to geriatricians (2). The gaps in teaching the subject further led to inadequate graduates being competent in geriatric medicine. It is a vicious cycle that needs to be intervened with meticulously planned approaches.
To develop more exposure for the learners and increase doctors with expertise in the field, the Programme Standards for Undergraduate Medical Education (3) has incorporated Geriatric Medicine as one of the core competencies. Furthermore, as developing countries have limited resources, an innovative and effective curriculum must be designed. Nevertheless, in developing a curriculum, consideration must be made on understanding the attitude and interests of medical students toward ageing and a career in geriatric medicine (4). The Malaysian Society of Geriatric Medicine (MSGM) has developed a recommended undergraduate curriculum for ageing and geriatric medicine tailored for Malaysians (5). The curriculum has been validated with understanding of the unique nature and needs of our ageing population. Validation was done through a rigorous Delphi exercise with experts who teach in academic institutions and clinical geriatricians who have worked with medical officers. This combination of experts helped to address the gaps between undergraduate education and real-life practise, and fulfil the principles of outcome-based education.
A dedicated course on ageing and geriatric medicine at the undergraduate level has been shown to improve the attitude and self-perceived competency of medical undergraduates in managing older adults with frailty and multimorbidity (6). To achieve this, the teaching approach on ageing and geriatric medicine often involves multi-professional teachers and applies innovations to ensure that students graduate with adequate competency (7).
The attitude of an individual toward older adults plays an important role in this specialty learning, partly because ageism has a considerable impact on medical practises toward older adults (8). Earlier this year, the United Nations had identified ageism as a global challenge and called for urgent actions for anti-ageism strategies. Ageism is simply defined as discrimination, stereotyping and prejudice against a person based on their age. This leads to financial loss through psychological, behavioural, and physiological change (9). It is ubiquitous with every one in two people being ageist, whereby this is primarily seen in the younger population, the male gender, and those of lower education background (10). Hence, there is a need to also assess this perception among our students undergoing the course.
The medical program at Universiti Putra Malaysia (UPM) is a 5-year program and leads to the conferment of the Doctor of Medicine (MD). Our institution did not have a geriatrician in the faculty for the last two decades, but this did not hinder students from an in-depth learning about this growing population. A Healthcare of Elderly Course (HEC) has been offered as a 3-week course for undergraduate medical students since 2000. Since its inception, this course was primarily taught by visiting geriatricians from the Malaysian Ministry of Health. The clinical bedside teaching was initially carried out in the Geriatric Unit, General Hospital Seremban, under the guidance of the current Head of National Geriatric Service, Dr. Yau Weng Keong. Until the recent COVID-19 pandemic, the students continued to have bedside teaching and learning on geriatric medicine in Hospital Kuala Lumpur. This hospital is the largest public hospital under the Ministry of Health to offer such service. The COVID-19 pandemic has dramatically changed the course's content and delivery, where it involved online lectures and inconsistent contact with patients whenever the Movement Control Order was enforced in the nation. This might cause tremendous stress and anxiety to our students (11), especially when they need to learn a multi-faceted course like ageing and geriatric medicine.
This paper discusses the change in attitude, self-perceived competency, and interest in a career in geriatric medicine among undergraduate medical students of Universiti Putra Malaysia before and after an HEC. The association between attitude and previous experience of taking care of older adults was investigated. Additionally, the influence of gender, ethnicity, experience in caring for older adults, attitude toward senior citizens, and self-perceived competency on the interest to pursue a career in geriatric medicine is also discussed.
This was a Quasi-experimental without Control Groups, Pre, and Posttest study undertaken between August 2020 to November 2020 for a span of 14 weeks. All 96 medical students who underwent the 3-week HEC were invited to answer an online questionnaire before and within 2 weeks after completing the course. The curriculum allocated the students into four groups with 24 students in each group. Students rotated between Otorhinolaryngology (3 weeks), Ophthalmology (3 weeks), Family Medicine/Radiology (3 weeks), and Healthcare of Elderly (3 weeks) courses.
The 3-week HEC was embedded in the clinical year (third year) and comprised of three parts: lectures, practical sessions, and tutorials. The lectures were delivered by field experts over a week to cover various topics on ageing and geriatric medicine. These field experts were namely geriatricians, rehabilitation physicians, neurologists, occupational therapists, psycho-geriatricians, and lawyers. This was followed by a 2-week practical sessions of a geriatrician-led ward rounds, geriatric outpatient clinics, home visits, and occupational and physiotherapy clinics. The tutorial consisted of a series of seminars, where students presented and discussed healthy ageing and geriatric syndromes. At the end of the course, students were required to submit a logbook and sit for a theory examination.
Participants were aware that personal identifiable information was not collected within the questionnaire. Thus, participants remained anonymous and this encouraged truthfulness. As this course was conducted entirely in English and the students were required to attain a certain level of English proficiency before enrolling into the medical programme, their English command was adequate to complete the questionnaire.
A written informed consent was provided by every participant in this study. Information on age, gender, ethnicity, experience in taking care of older adults in the family, and the interest to pursue geriatric medicine as a career were collected from all participants through the questionnaire. Attitude was assessed using a 14-item survey by the University of California at Los Angeles Geriatric Attitude Scale (UCLA-GAS) (12) and self-perceived competencies questionnaire from (6). These questionnaires were used due to their reliability.
The online questionnaires were developed using Google Forms, and the link was shared through WhatsApp and e-mail. Likert scales from 1 (strongly agree) to 5 (strongly disagree) was used to assess attitude and self-perceived competency, and from 1 (strongly interested) to 5 (strongly disinterested) to evaluate interest to pursue a career in geriatric medicine (Supplementary Material 1). Cronbach alpha for the UCLA-GAS and Self-Perceived Competency questionnaires were 0.668 and 0.975, respectively. This study was reviewed and approved by the Universiti Putra Malaysia Ethics Committee (JKEUPM-2020-320).
All measured variables were summarised to mean (standard deviation) for continuous variable and frequency (percentage) for categorical variable. For comparisons of means between before and after course completion, repeated measure of ANOVA was used. Analysis of within-subject effects was checked using repeated measure of ANOVA, namely the assumption of compound symmetry, normality of residuals, and homogeneity of variance. Linear regression was used to analyze the association between the following:
1) previous experience of taking care of an older adult and attitude, and
2) gender, ethnicity, experience in taking care of an older adult, attitude toward older adults and self-perceived competency, and the interest to pursue a career in geriatric medicine.
Attitude and competency scores were calculated according to the responses of the students. For positive statements, the scoring systems used for the responses were as follows: a score of 5 for strongly agree, a score of 4 for agree, a score of 3 for neutral, a score of 2 for disagree, and a score of 1 for strongly disagree. Reverse scoring was done for the negative statements. The maximum score for each positive attitude, perceived competency and interest, was 5. The p < 0.05 was considered as significant. Data analysis was done using IBM SPSS version 23.
Out of the 96 students, 68 completed both pre and post-course questionnaires, resulting in a response rate of 70.8%. Nearly 30% of students responded either to the pre or post-test questionnaire (incomplete response). This might be due to the changing situation during the pandemic, where a fraction of students could not attend clinical sessions during the Movement Control Order. Hence, the inability to complete the survey. The majority of students were female (65%, n = 45). The students were mostly of the Malay ethnic group (55.9%, n = 38), followed by Chinese (23.5%, n = 16), Indian (17.6%, n = 12), and other groups (2.9%, n = 2).
The mean pre-course UCLA attitude score was 3.41 (±.36), which indicated an overall positive attitude toward older adults, at commencement of the course. Only five students, or 7.4%, demonstrated scores (<3) consistent with a negative attitude toward older adults. The mean post-course UCLA attitude score reported a slight increment to 3.45 (±.35), which was not statistically significant (p = 0.299).
Table 1 shows means, standard deviations, and p-value of the attitudes of students toward older adults for each question in the UCLA-GAS. The statement most disagreed upon was “The federal government should reallocate money to research on AIDS or paediatric diseases.” The highly agreed statements (score >4) were for “It is interesting listening to old people's accounts of their past experiences” and “It is society's responsibility to provide care for its older adults.” Upon completion of the course, three students (4.4%) reported maintaining a negative attitude. None of the mean scores of individual components showed a significant change post-course.
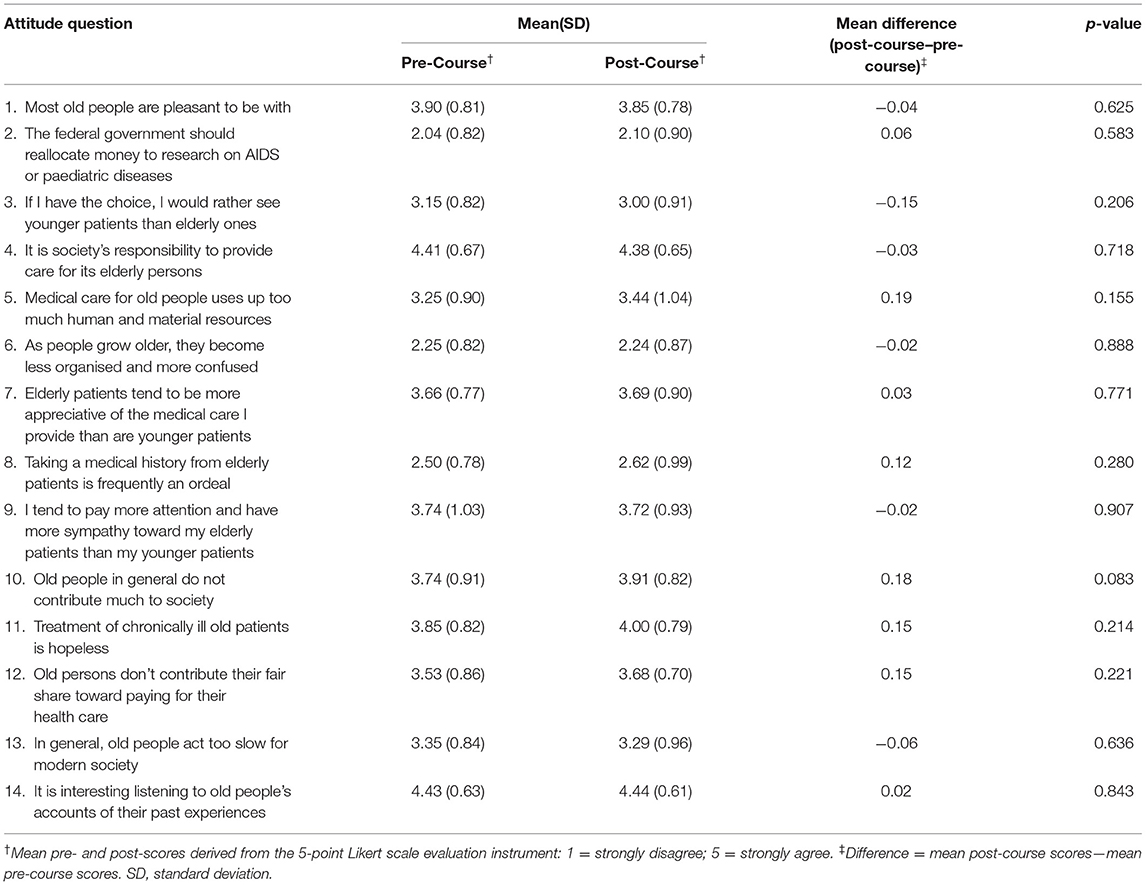
Table 1. Students' means, standard deviations, and P-value of attitudes toward older people for each question.
Self-perceived competency scores of students significantly improved upon completion of the course [mean score pre-course of 3.62 (±0.76) vs. post-course of 3.81 (±0.56); p = 0.009]. Fifty-nine students (86.8%) had a positive (>3) perception of their competency at the start of the course, and by the end of the course, sixty-six students (97.1%) had a positive perception of their competency. Table 2 shows the means, standard deviations, and p-value of the self-perceived rating scores of students for each competency question.
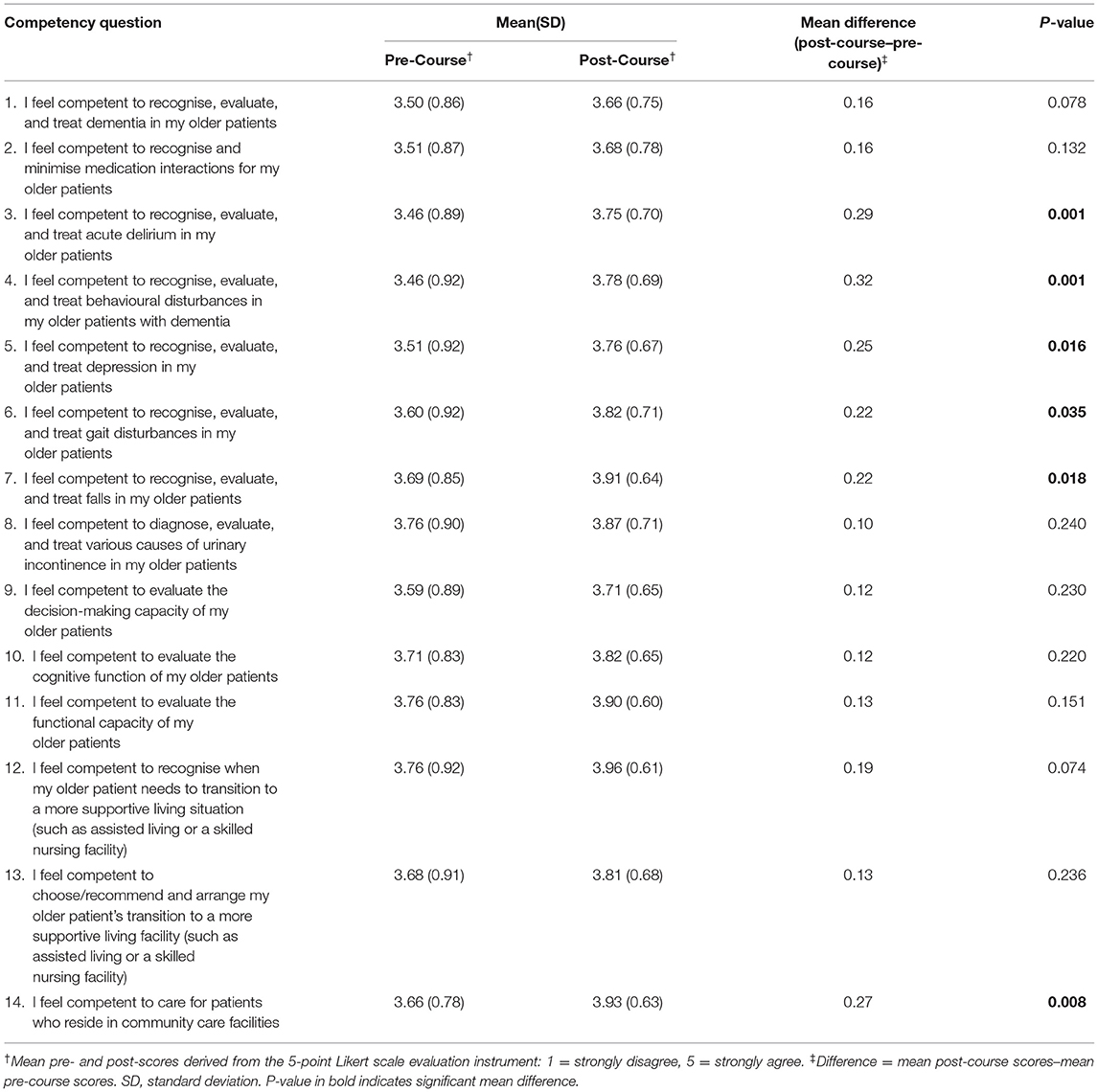
Table 2. Students' means, standard deviations, and P-value of self-perceived rating scores for each competency question.
The highest self-perceived post-course competency was noted for the statement “I feel competent to recognise when my older patient needs to transition to a more supportive living situation (such as assisted living or a skilled nursing facility),” with a post-course mean score of 3.96. Meanwhile the statement with the lowest self-perceived post-course competency was “I feel competent to recognise, evaluate, and treat dementia in my older patients,” with a post-course mean score of 3.66. The statement “I feel competent to recognise, evaluate, and treat behavioural disturbances in my older patients with dementia” and “I feel competent to recognise, evaluate, and treat acute delirium in my older patients” showed the most significant improvement post-course, with a change in mean score of 0.32 and 0.29, respectively (p < 0.001).
Most students remained neutral toward having geriatric medicine as a career of choice, both in the pre-course (52.9%) and the post-course (61.8%). At commencement, 35.4% of students were either interested or strongly interested in having geriatric medicine as a career choice, while 11.8% were either disinterested or strongly disinterested. Post-course, 29.4% of the students showed interest, while 8.8% were disinterested, and none were strongly disinterested. However, there was no significant difference in the interest of geriatric medicine as a career of choice in the pre and post-course (p > 0.95).
Among the 68 students, 48 (70.6%) had experience in taking care of older adults in their family. There was no significant association between attitude and experience in taking care of an older adult family member (p = 0.509).
Among gender, ethnicity, experience in taking care of an older adult, attitude toward older adults, and self-perceived competency, we found that only self-perceived competency of students showed a good and significant association (β = 0.56, p < 0.001) with the interest of the student in a future career in geriatric medicine (Table 3).
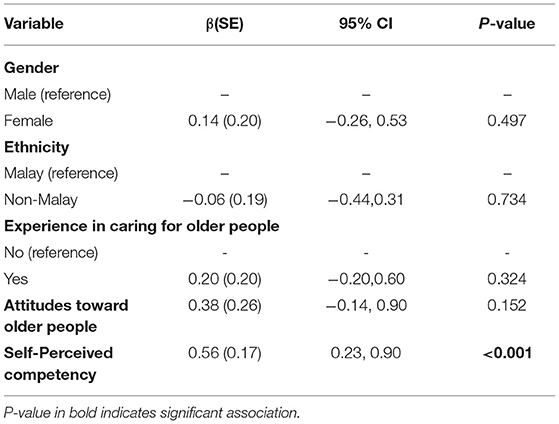
Table 3. Association between Interest in geriatric medicine as a career of choice and study variables (post-course).
In this study, it was hoped to uplift the image of clinical practise toward the ageing population. Although attitude is one of the critical constructs of ageism, the specific course did not significantly improve attitude. The UCLA-GAS may screen for stereotyping and discrimination related to ageism with acceptable reliability on four dimensions of attitude: Social Value, Medical Care, Compassion, and Resource Distribution. Among the four dimensions, attitude toward medical care contributes the most to the overall attitude (13).
The attitude of a person is a complex, multidimensional, and challenging aspect to accurately quantify in medical education research. Nevertheless, to combat ageism among medical graduates, attitude toward older adults must be accurately quantified and understood, and this should be the future work in the field of geriatric education (14). A locally developed, validated, or modified instrument will tremendously help medical educators to effectively develop geriatric medicine curricula that foster positive attitude toward older adults and combat ageism as a core graduate outcome (5, 8). Even though our study did not show any association between previous experience of caring for an older family member and attitude toward an older adult, another study among senior medical students in a public university in Malaysia (n = 116) showed that having grandparents, was a significant association (p < 0.05) (15).
Our study highlighted that the self-perceived competency of students heightened after the course. This was in line with another study in Australia (6). Students perceived themselves to be most competent in managing transitions of care and least capable in recognising, evaluating, and treating dementia. The most remarkable improvement of self-perceived competencies was in managing behavioural symptoms of dementia, followed by identifying, evaluating, and treating acute delirium. A self-assessment among graduates tends to differ with seniority, with an over estimation among the younger age group. Therefore, this assessment should be taken alongside a formal assessment by the faculty to ensure congruence (16). Student self-perceived competencies can be considered as a credit to the current curriculum. They should be conducted on a regular basis to implement necessary interventions and to enhance professional competencies and the quality of care (17). It was previously found that many medical institutions and medical educators have used the self-assessment of students as one of the measures to fulfil an outcome-based education (18).
Increasing the workforce in geriatric care has been a focus in many research on geriatric education. Our study showed that a higher self-perceived competency score had a significant association with a higher interest in pursuing a career in geriatric medicine. This might be explained by the impact of a positive influence of the module toward a career choice in geriatrics (19). Our study also showed no association between previous experience and interest. This differed from a finding in another study which found that frequent contact with an older adult and undertaking courses in ageing significantly increased the interest of students in working with older adults (19, 20). Studies have shown that medical students did not have enough exposure to older adult patients during their education and, therefore, did not see the drawbacks of ageing with multimorbidity (21, 22). Hence, having a dedicated course, such as HEC, will increase their exposure, skills, and experience at the undergraduate level. It was also suggested that a more positive attitude had been linked to a willingness to pursue geriatric medicine as a career (23, 24). However, despite generally having a positive attitude toward older adults, no significant association was found concerning the interest of our students in geriatric medicine. Only 1 in 3 students in our study considered a future career in geriatric medicine, mirroring the findings in studies done in Singapore and Ireland (19, 25).
The training of the healthcare workforce should not only focus on the attainment of knowledge and skills in managing diseases pertinent in the ageing population, but also the ability to work in an interdisciplinary team (26, 27). Therefore, a more refined older adult-friendly curriculum is recommended to nurture enthusiasm in caring for older adults (28). Although the complexity in handling older adults was found to be a significant barrier to working in the field, the exposure to a course in ageing and geriatric medicine would help spark interests (29).
This was the first study in Malaysia that assessed the attitude, self-perceived competencies, and interests of students in pursuing a geriatric medicine career before and after an HEC with multi-professional teachers at the undergraduate level. This study was carried out during the COVID-19 pandemic to assess if the change in the implemented teaching method can sustain a good attitude after the course and improve self-perceived competencies.
There a few limitations identified in this study. Firstly, the study was conducted during the COVID-19 pandemic, with limited bedside teaching in the ward and clinic. Only about half of the students could attend a clinic session with a geriatrician, while the other half received no clinical exposure. Secondly, this study had a small sample size and was conducted in a single public institution, thus limiting generalizability. Thirdly, only medical students in the early clinical years (i.e., third year) were involved in the study, thus, the findings may not apply to other different cohorts of health professionals. Finally, we did not have a control group in this study. Hence, the results may call for judicious interpretations.
Our study has shown that implementing multi-professional teachers in an HEC could sustain a positive attitude and improve self-perceived competencies among the undergraduate medical students at our learning institute. However, increasing the enthusiasm in students for pursuing a geriatric medicine career alone was not sufficient as most students remained neutral after the course. Therefore, a more refined older adult-friendly curriculum that addresses the complexity of caring for older adults is recommended to encourage a future career in the field.
In an ageing society, the training of the healthcare workforce should not only focus on knowledge and skills in managing the diseases pertinent in the ageing group but also the ability to work in an interdisciplinary team. Although our course involves multi-professional teachers, it only partially exposes our students to the reality of managing an older adult as a team. We recommend that the course employ an inter-professional teaching method in the future, which may include nursing, pharmacy, law, dietetic, physiotherapy, speech therapy, occupational therapy, and social workers. Secondly, although the UCLA-GAS was internationally validated among medical students and health professionals, there is a need to consider the multicultural background of local students. Future studies should focus on a locally validated tool to measure the attitude toward older adults and perhaps construct against ageism related stereotyping and discrimination.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Universiti Putra Malaysia Ethics Committee JKEUPM-2020-320. The patients/participants provided their written informed consent to participate in this study.
HS, NZ, and UD: conceptualisation. HM and HS: methodology. HM and NZ: formal analysis. NZ, LI, and WW: investigation. HS: writing—original draught preparation of all sections. HS and AM: writing—original draught preparation of introduction. NZ and UD: writing—original draught preparation of introduction and discussion. HM and NZ: writing—original draught preparation of methods and results. HS, NZ, UD, AM, and WW: writing—final review and editing. All authors contributed to the article and approved the submitted version.
The publication of this manuscript was supported by University Putra Malaysia Journal Publication Fund (VOT9001103).
The authors alone are responsible for the views expressed in this article. They do not necessarily represent the institutions' views, decisions, or policies in which they are affiliated to.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to express gratitude to Mr. Ravinash Kaur, the class representative, for his help in sharing the survey link with the participants.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.743804/full#supplementary-material
1. United Nations. (2019). World Population Ageing 2019. Available online at: https://www.un.org/en/global-issues/ageing
2. Sallehuddin H, Tan MP, Blundell A, Gordon A, Masud T. A national survey on the teaching provision of undergraduate geriatric medicine in Malaysia. Gerontol Geriatr Educ. (2021). doi: 10.1080/02701960.2021.1914027
3. Malaysian Medical Council M. Standards for Undergraduate Medical Education. (2019). Available online at: https://mmc.gov.my/wp-content/uploads/2020/10/STANDARDS-FOR-UNDERGRADUATE-MEDICAL-EDUCATION-Version-1.2-Updated-on-15-January-2020.pdf
4. Le Couteur DG, Bansal AS, Price DA. The attitudes of medical students towards careers in geriatric medicine. Australas J Ageing. (1997) 16:225–8. doi: 10.1111/j.1741-6612.1997.tb01060.x
5. Sallehuddin H, Tan MP, Blundell A, Gordon AL, Masud T. Development of a Malaysian undergraduate geriatric medicine curriculum. Aging Med Healthc. (2020) 11:82–8. doi: 10.33879/AMH.113.2020.05015
6. Tam KL, Chandran K, Yu S, Nair S, Visvanathan R. Geriatric medicine course to senior undergraduate medical students improves attitude and self-perceived competency scores. Australas J Ageing. (2014) 33:E6–11. doi: 10.1111/ajag.12060
7. Blundell A, Gordon AL, Masud T, Gladman J. Innovations in teaching undergraduates about geriatric medicine and ageing - results from the UK National Survey of Teaching in Ageing and Geriatric Medicine. Eur Geriatr Med. (2011) 2:12–4. doi: 10.1016/j.eurger.2010.11.013
8. Wilson MAG, Kurrle S, Wilson I. Medical student attitudes towards older people: a critical review of quantitative measures. BMC Res Notes. (2018) 11:71. doi: 10.1186/s13104-018-3186-z
9. World Health Organization. (2021). Global Report on Ageism. Available online at: https://www.who.int/publications/i/item/9789240016866
10. Officer A, Thiyagarajan JA, Schneiders ML, Nash P, De La Fuente-Núñez V. Ageism, healthy life expectancy and population ageing: how are they related? Int J Environ Res Public Health. (2020) 17:3159. doi: 10.3390/ijerph17093159
11. Sundarasen S, Chinna K, Kamaludin K, Nurunnabi M, Baloch GM, Khoshaim HB, et al. Psychological impact of COVID-19 and lockdown among university students in Malaysia: implications and policy recommendations. Int J Environ Res Public Health. (2020) 17:6206. doi: 10.3390/ijerph17176206
12. Reuben DB, Lee M, Davis J. W. Jr., Eslami MS, Osterweil DG, et al. Development and validation of a geriatrics attitudes scale for primary care residents. J Am Geriatr Soc. (1998) 46:1425–30. doi: 10.1111/j.1532-5415.1998.tb06012.x
13. Lee M, Reuben DB, Ferrell BA. Multidimensional attitudes of medical residents and geriatrics fellows toward older people. J Am Geriatr Soc. (2005) 53:489–94. doi: 10.1111/j.1532-5415.2005.53170.x
14. Wilson M, Tran Y, Wilson I, Kurrle SE. Cross-sectional study of Australian medical student attitudes towards older people confirms a four-factor structure and psychometric properties of the Australian ageing semantic differential. BMJ Open. (2020) 10:e036108. doi: 10.1136/bmjopen-2019-036108
15. Shalihin MSE, Abd Muttalib NS, Azmi NS, Zin ZNM. Knowledge and attitude towards geriatric and its associated factors among final year medical students of international islamic university Malaysia. Int J Alli Health Sci. (2021) 5:2101. Available online at: http://irep.iium.edu.my/id/eprint/89583
16. Ward M, Gruppen L, Regehr G. Measuring self-assessment: current state of the art. Adv Health Sci Educ Theory Pract. (2002) 7:63–80. doi: 10.1023/A:1014585522084
17. Abadel FT, Hattab AS. How does the medical graduates' self-assessment of their clinical competency differ from experts' assessment? BMC Med Educ. (2013) 13:24. doi: 10.1186/1472-6920-13-24
18. Yeo S, Chang BH. Students' self-assessment of achievement of terminal competency and 4-year trend of student evaluation on outcome-based education. Kor J Med Educ. (2019) 31:39–50. doi: 10.3946/kjme.2019.117
19. Ní Chróinín D, Cronin E, Cullen W, O'Shea D, Steele M, Bury G, et al. Would you be a geriatrician? Student career preferences and attitudes to a career in geriatric medicine. Age Ageing. (2013) 42:654–7. doi: 10.1093/ageing/aft093
20. Gorelik JDR, Funderburk B, Solomon DHY. Undergraduate interest in aging: is it affected by contact with older adults? Educ Gerontol. (2000) 26:623–38. doi: 10.1080/03601270050200626
21. Cankurtaran M, Halil M, Ulger Z, Dagli N, Yavuz BB, Karaca B, et al. Influence of medical education on students' attitudes towards the elderly. J Natl Med Assoc. (2006) 98:1518–22.
22. Wiese CH, Fragemann K, Keil PC, Bundscherer AC, Lindenberg N, Lassen CL, et al. Geriatrics in medical students' curricula: questionnaire-based amalysia. BMC Res Notes. (2014) 7:472. doi: 10.1186/1756-0500-7-472
23. Hughes NJ, Soiza RL, Chua M, Hoyle GE, MacDonald A, Primrose WR, et al. Medical student attitudes toward older people and willingness to consider a career in geriatric medicine. J Am Geriatr Soc. (2008) 56:334–8. doi: 10.1111/j.1532-5415.2007.01552.x
24. Sai K, Mohammed IMB, Tennakoon TP, Daud CD. Knowledge and attitudes towards elderly people and their care among medical students of melaka-manipal medical college, a cross-sectional study. J Soc Sci Hum. (2020) 6:125–37. Available online at: http://www.aiscience.org/journal/paperInfo/jssh?paperId=4904
25. Chua MP, Tan CH, Merchant R, Soiza RL. Attitudes of first-year medical students in Singapore towards older people and willingness to consider a career in geriatric medicine. Ann Acad Med Singap. (2008) 37:947–51. Available online at: http://www.annals.edu.sg/pdf/37VolNo11Nov2008/V37N11p947.pdf
26. Mezey M, Mitty E, Burger SG, McCallion P. Healthcare professional training: a comparison of geriatric competencies. J Am Geriatr Soc. (2008) 56:1724–9. doi: 10.1111/j.1532-5415.2008.01857.x
27. Schapmire TJ, Head BA, Nash WA, Yankeelov PA, Furman CD, Wright RB, et al. Overcoming barriers to interprofessional education in gerontology: the interprofessional curriculum for the care of older adults. Adv Med Educ Pract. (2018) 9:109–18. doi: 10.2147/AMEP.S149863
28. Meiboom AA, De Vries H, Scheele F, Hertogh CMPM. Raising enthusiasm for the medical care of elderly patients: a concept mapping study to find elements for an elderly friendly medical curriculum. BMC Med Educ. (2018) 18:238. doi: 10.1186/s12909-018-1344-6
Keywords: geriatric medicine, undergraduate, curriculum, Malaysia, competency
Citation: Ng ZL, Mat Din H, Zakaria NF, Inche Mat LN, Wan Zukiman WZH, Md Shah A, Daut UN and Sallehuddin HM (2021) Implementation of a Healthcare of Elderly Course With Multi-Professional Teachers for Undergraduate Medical Students in a Public University in Malaysia—A Quasi-Experimental Pre and Post Study. Front. Public Health 9:743804. doi: 10.3389/fpubh.2021.743804
Received: 19 July 2021; Accepted: 08 October 2021;
Published: 11 November 2021.
Edited by:
Devinder Kaur Ajit Singh, National University of Malaysia, MalaysiaReviewed by:
Sumaiyah Mat, National University of Malaysia, MalaysiaCopyright © 2021 Ng, Mat Din, Zakaria, Inche Mat, Wan Zukiman, Md Shah, Daut and Sallehuddin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hakimah Mohammad Sallehuddin, ZHJoYWtpbWFoQHVwbS5lZHUubXk=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.