- 1Beijing Institute of Ophthalmology, Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical University, Beijing, China
- 2Center for Clinical Epidemiology and Evidence-based Medicine, Beijing Children's Hospital, Capital Medical University, Beijing, China
- 3University of Warmia and Mazury, Olsztyn, Poland
- 4Institute for Research in Ophthalmology, Poznan, Poland
Background: To assess the impact of study-at-home during the COVID-19 pandemic on myopia development in Chinese schoolchildren.
Methods: This historical cohort involved two groups with a total of 154 children. The exposed group was formed from 77 children aged 8 to 10 years who studied at home in the 7-month period during the COVID-19 pandemic (follow-up period: January – August 2020) and did not study at home in the 7-month period before the COVID-19 outbreak (baseline period: July 2019 – January 2020). Seventy-seven children who did not undergo study-at-home (baseline period: 7 months in 2015, follow-up period: 7 months in 2016) were included in the control group. Cycloplegic refraction, axial length and uncorrected visual acuity were measured 3 times. The questionnaire mainly focused on collecting visual habits.
Results: Myopia progression was similar between the two groups in the baseline period. However, in the follow-up period the exposed group had a greater change in refraction toward myopia (−0.83 ± 0.56 D) than the control group (−0.28 ± 0.54 D; p < 0.001). In addition, the exposed group exhibited a significantly greater change in refraction toward myopia in the follow-up period (−0.83 ± 0.56 D) than in the baseline period (−0.33 ± 0.46 D; p < 0.001). Difference-in-difference analysis indicated that study-at-home accelerated the change in refraction toward myopia (t = −0.567; p < 0.001).
Conclusions: During the COVID-19 pandemic study-at-home accelerated the change of refraction toward myopia in children.
Background
The novel coronavirus disease 2019 (COVID-19) has had a global impact (1) and has affected many aspects of people's lives. During the COVID-19 pandemic, governments around the world provided distance education for children to study at home. According to the United Nations, the COVID-19 pandemic has created the largest disruption of education systems in history, affecting nearly 1.6 billion learners in more than 190 countries and all continents (2). From January 2020 to August 2020, the Ministry of Education of the People's Republic of China estimated that more than 220 million children and adolescents stayed home and engaged in online education in China (3). Previous studies have reported that closures of schools and studying at home may have elevated psychosocial stress and affected physical health (4–6).
Myopia has become a significant public health problem and is the most common cause of vision impairment in children (7), especially in East and Southeast Asia (8, 9). Insufficient time spent outdoors, and prolonged near-work activities are recognized as important risk factors for myopia (7, 10). Studies have found that the COVID-19 leads to beneficial conditions for behavioral changes in myopia, characterized by reduced outdoor activity and increased near work (11, 12). Children use electronic devices for virtual education, social interaction, and entertainment during the COVID-19 pandemic, with the amount of time Hong Kong children spend on electronic devices increasing from 2.5 h a day to nearly seven hours a day (11, 13). Liu et al. have pointed out that daily use of digital screens was positively related to the prevalence of myopia progression (14). A consequence of the forced lifestyle change during the COVID-19 pandemic would likely have a significant effect on the global burden of myopia (10, 11, 13–15). The purpose was to assess the impact of study-at-home during the COVID-19 pandemic on myopia progression in children by comparing the cycloplegic spherical equivalent, uncorrected visual acuity (UCVA) and axial length (AL). These data will provide important insight into myopia progression.
Methods
Study Population
In 2019, three of nearly 20 primary schools in Fuxing District, Handan, Hebei, China were selected for an observational study using a cohort randomization method, which was approved by the ethics committee. Comprehensive and detailed ophthalmic examinations were performed for children of grade 3 in July 2019 and January 2020. In 2020, schools were closed from January to August due to COVID-19. Therefore, the data were collected at the Third Hospital of Handan in August 2020. The children in the exposed group studied at home during the COVID-19 pandemic (January–August 2020) and did not study at home before the COVID-19 outbreak. All participants met the following inclusion criteria: the best-corrected visual acuity of all participants was at least 0.0 Log MAR in both eyes. The exclusion criteria were systemic diseases, former or current eye diseases and injury. Children with atropine or orthokeratology or any condition that might have influenced myopia were excluded.
Stratified cluster sampling was used in the ACES. The ACES is a school-based cohort study mainly designed to longitudinally observe the occurrence and development of myopia in school-aged children. Details of the ACES have been published previously (9). Children in the Anyang Children Eye Study (ACES) matched with children in the exposed group were included in the control group. All children in the control group were not exposed to exposure factors (study at home). A total of 2,850 children in ACES database were the same age and sex as those in the exposed group. According to the matching principles, children in the control were selected from 2,850 children. Matching principles: 1) age, with a difference within ± 0.25 years, 2) sex, 3) UCVA, 4) degree of myopia, and 5) AL, with a difference within ± 0.25 mm. The exclusion criteria were the same as those in the exposed group.
The study was approved by the Ethics Committee and Institutional Review Board of Beijing Tongren Hospital, Capital Medical University. Written informed consent forms were brought home by the children of exposed and control group for their parents' signature, and this study adhered to the principles of the Declaration of Helsinki.
Procedures
Children in the exposed group underwent a comprehensive and standardized ophthalmic examination to obtain data on UCVA, cycloplegic refraction and AL at baseline (July 2019), at the first follow-up (January 2020) and at the second follow-up (August 2020) in Handan Third Hospital. In addition, a detailed questionnaire was administered to children in the exposed group at the second follow-up.
Children were assessed for distance visual acuity (VA) without spectacles using a logarithmic VA chart (Precision Vision, La Salle, IL, USA) at a distance of 4 m. The chart was retro-illuminated and had 70 tumbling “E” optotypes with five letters on each line. Children were examined monocularly (left eye followed by the right eye); the detailed procedure has been described elsewhere (16). AL was measured by an IOL Master 700 (Carl Zeiss Meditec AG, Jena, Germany). Five repeated measurements were performed, and the average AL value before cycloplegia was obtained. Autorefraction keratometry (KR8800, Topcon, Tokyo, Japan) was used to measure cycloplegic autorefraction. In each child, three drops of 1% cyclopentolate (Cyclogyl, Alcon-Convreur, Rijksweg, Belgium) were administered at intervals of 5 min. If the pupil size was less than 6.0 mm or a light reflex was still present after 30 min, a fourth drop of 1% cyclopentolate was administered, and the examination was repeated after 15 min (17). Three autorefraction readings were taken, and the average was recorded.
The questionnaire used in our study was derived from that in the Anyang Children Eye Study, and the detailed procedure has been described elsewhere (11). To control for interview bias, the questionnaire was administered in a pilot study to determine validity and reliability (7). The questionnaire mainly focused on collecting near-work, outdoor activity-related and online education data, including time (hours/day) spent performing and types of near-work and outdoor activities before and during the study-at-home period. Near-work included homework, reading books, painting, playing chess, using computers, and using mobile phones. Outdoor activities were bicycle riding, running, swimming, playing football, etc. The parents and children were asked about the time (hours/day) spent engaging in and parameters of online education during the study-at-home period. All questionnaires were completed by the children and their parents together. Due to the limited literacy ability of children, the questionnaire was completed by children and parents.
Children who were enrolled in the control group underwent ophthalmic examinations in September 2014, September 2015, and September 2016. In the control group, all students had UCVA (Precision Vision, La Salle, IL, USA) measured at a 4 m distance. The charts were the same for the control and exposed groups. Children were examined monocularly (left eye followed by the right eye); the detailed procedure has been described elsewhere (16). An autorefractor (HRK7000A, Huvitz, Gunpo, South Korea) was used to measure cycloplegic refraction. Each student was first administered one drop of topical anesthetic agent (Alcaine, Alcon) to alleviate discomfort, followed by two drops of 1% cyclopentolate (Alcon) and 1 drop of Mydrin P (Santen, Japan) after a 5-min interval. Thirty min after the last drop, a third drop of cyclopentolate was administered if the pupillary light reflex was still present or the pupil size was less than 6.0 mm. Three readings of spherocylindrical auto-refraction were taken and averaged. An IOL Master (Carl Zeiss Meditec AG, Jena, Germany) was used to measure axial length. Five repeated measurements were taken and averaged before cycloplegia. The detailed procedure has been described elsewhere (9).
Definitions
The spherical equivalent (SE) was calculated according to the standard formula of the algebraic sum of the dioptric powers of the sphere and half of the cylinder (sphere +0.5 × cylinder). Myopia was defined as an SE ≤ −0.5 D and was classified as low (−3.0 D < SE ≤ −0.5 D), moderate (−6.0 D < SE ≤ −3.0 D) or high (SE ≤ −6.0 D) myopia (18). Emmetrope and hyperopia were defined as an SE between −0.5 D and +0.5 D and greater than +0.5 D, respectively (18).
In the exposed group, the period from July 2019 to August 2020 was divided into two periods: the 7-month period during the COVID-19 pandemic (follow-up period: January – August 2020) and the 7-month period before the COVID-19 outbreak (baseline period: July 2019 – January 2020). Children in the control group did not study at home from September 2014 to September 2016. In the control group, the period from September 2014 to September 2015 was considered the baseline period, and the period from September 2015 to September 2016 was considered the follow-up period.
In the control group, the changes in ophthalmic parameters in one year were calculated as the value in September 2015 minus the value in September 2014 or the value in September 2016 minus the value in September 2015. The changes in ophthalmic parameters at 7 months were calculated by the changes in ocular parameters in a year divided by 12 and multiplied by 7.
Data Management and Statistical Analysis
Data were entered into EpiData software 3.1 (The EpiData Association, Odense, Denmark), and statistical analysis was performed using an open-source R program (version 4.0.2).
The Shapiro-Wilk test was used to test for the normality of continuous variables. For normally distributed continuous variables, means and standard deviations were used to provide a basic statistical description. Median values and interquartile ranges were used for basic statistical descriptions of non-normally distributed continuous variables. The Wilcoxon rank sum test was used to compare continuous outcomes between the exposed group and the control group; the Wilcoxon signed rank test was used to compare continuous outcomes between period one and period two in the exposed group. Analysis of covariance was used to adjust the influence of axial length change and then make comparison of refraction change between different groups. The difference-in-difference approach was used to analyze the impact of study-at-home. Since large correlation coefficients were observed between the two eyes (P < 0.001), only data from right eyes were included in the analyses. Two-sided p-values less than 0.05 were considered statistically significant.
Results
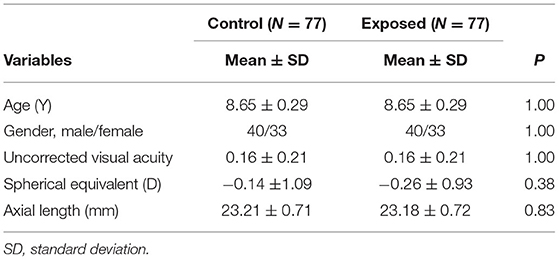
A total of 154 children aged 8.65 ± 0.29 years were included in the analysis. There were 77 children in each of the two groups and 40 (51.95%) males in each group. For the baseline period, 25 children had myopia (25/77) in each of the two groups. There were no significant differences between the two groups in uncorrected visual acuity, spherical equivalent or axial length at baseline (Table 1).
In the control group at the last follow-up 37 children had myopia (37/77); however, sixty-five children had myopia (65/77) in the exposed group at the last follow-up. No difference was observed between the two groups in the baseline period (p = 0.62). In the follow-up period, a significantly larger change in myopia progression in the exposed group (−0.83 ± 0.56 D) than in the control group (−0.28 ± 0.54 D; p < 0.001; Figure 1) was observed. The effect of axial length change on myopia progression was not statistically significant by covariance analysis (F = 0.788; p = 0.705). In addition, in the exposed group, children had a larger change in myopia progression in the follow-up period (−0.83 ± 0.56 D) than in the baseline period (−0.33 ± 0.46 D; p < 0.001; Figure 1). The effect of axial length change on myopia progression was not statistically significant by covariance analysis (F = 0.800; p = 0.692). Differences-in-differences estimation of the impact of study-at-home indicated that it accelerated myopia progression (t = −0.567; p < 0.001).
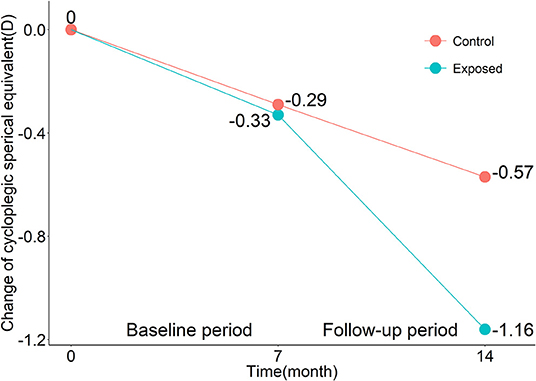
Figure 1. Mean changes in cycloplegic spherical equivalents in the exposed group and the control group over the baseline period and follow-up period.
There was no significant difference in the myopia progression in the baseline period between the exposed and control groups. However, in the follow-up period, the median myopia progression of the exposed group (−0.75 D) was significantly larger than that of the control group (−0.28 D; p < 0.001; Table 2). No differences in the change in UCVA and axial elongation were observed between the two groups (Table 2). In the exposed group, the median (quartile) myopia progression in the follow-up period was −0.75 (−1.13, −0.50) D, which was significantly different than that in the baseline period (−0.38 (−0.63, 0.00) D; p < 0.001). The changes in the UCVA between the two periods were not significantly different than those in the exposed group (0.00 vs. 0.01, p = 0.059). In the baseline period, the median (quartile) value of axial elongation was 0.20 (0.14, 0.28) mm, which was not significantly different from 0.20 (0.11, 0.38) mm in the follow-up period (p = 0.97; Table 2). In the exposed group, no difference in the change of astigmatism was observed (0.06 vs. 0.08, p = 0.19).
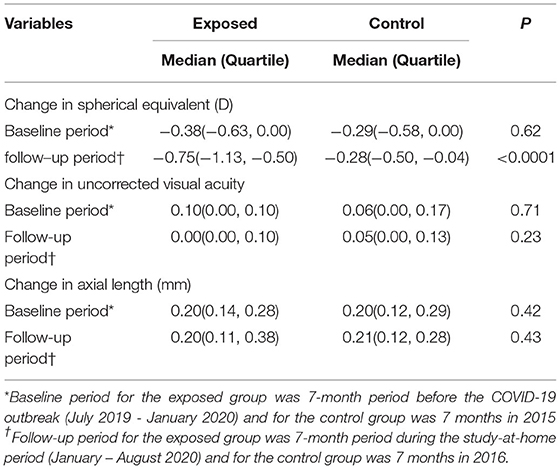
Table 2. Changes in ophthalmic parameters between the exposed and control groups in baseline period and follow-up period.
Compared with what was observed before the COVID-19 outbreak, the amount of time spent performing near-work increased during the study-at-home period from 2.96 ± 1.05 hours per day to 4.33 ± 1.04 hours per day (p < 0.001). Outdoor activities decreased from 1.84 ± 1.43 hours per day to 0.98 ± 1.01 hours per day (p < 0.001). In the control group, schoolchildren from Anyang spent 2.27 hours per day on outdoor activity, which was not significantly different than that in the baseline period of the exposed group (2.27 vs. 1.84; P = 0.25). Children in the exposed group spent 1.75 ± 0.71 hours per day engaging in online education during the COVID-19 pandemic. The details are presented in Figure 2.
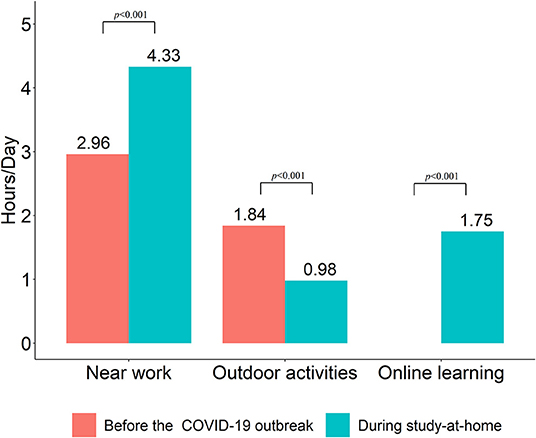
Figure 2. Time spent performing near work and outdoor activities (hours/day) before and during the study-at-home period.
Discussion
Concerns have been raised about myopia development in children during study-at-home caused by COVID-19. This study compared data on changes in ophthalmic parameters between the exposed and control groups in the baseline period (pre-COVID) and follow-up period (during COVID study-at-home). Myopia is a serious public health problem (7). In the past few decades, the prevalence of myopia has increased rapidly (7, 8). The study-at-home during the COVID-19 pandemic might have influenced myopia progression in children since it is well known that the change in visual habits may impact the burden of myopia.
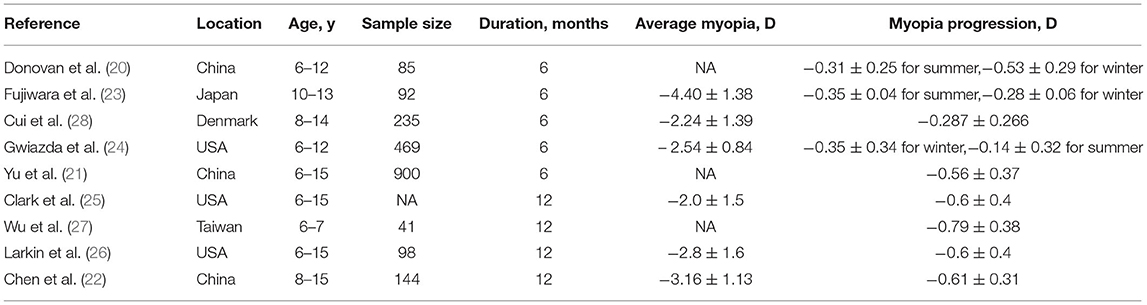
A summary of myopia progression in previous studies is shown in Table 3 (13–21). Our study found that myopia progression, at −0.3 ± 0.5 D, at 7 months before the COVID-19 outbreak was similar to those in previous studies in Chinese and foreign children, showing myopia progression of −0.3 D in 6 months or −0.6 D in a year (20, 22–26). Some studies also reported a higher myopia progression rate (21, 27). We believe that this may be related to different genetic and environmental factors as well as differences in subjects' age and the refractive errors in different studies.
We found that myopia progression during the study-at-home period was higher than the highest myopia progression during the period before COVID-19 in other studies (21). The changes in visual acuity and axial elongation were not statistically significant; we believe this might be related to the small degree and short follow-up time. The children in this study were in the developmental stage, during which the progression of myopia causes hyperopia peripheral defocus, which causes lengthening of the axis (29).
Previous investigations have reported (4–6) that home confinement during the COVID-19 was associated with the myopia shift. Wang et al. proposed that the age of 6–8 years is the critical period for the development of myopia in children, possibly because younger children's refraction status is more sensitive to environmental changes (15). The relationship between lifestyle changes and myopia has been reported in multiple studies. Liu et al. found that every additional hour of daily digital screen use was associated with an increased risk of myopia progression (5, 14).
Children's lifestyles have changed among children during the COVID-19 pandemic (12, 30). During the study-at-home period, students were away from the school classrooms and engaged in online education, which greatly increased digital screen time. In our study, we found that children spent 1.75 ± 0.71 hours per day on online education and 4.33 ± 1.04 hours per day on near work. In Spanish and Hong Kong, children spent more time on near work, and the students from Hong Kong spent nearly 7 hours/day on digital screens (12, 30). Long-term near work is considered a risk factor for the prevalence and incidence of myopia through increased accommodative demand (8, 10). Digital screen time has been reported to be a risk factor for increased myopia (5, 14, 31). Liu et al. pointed out that extended sedentary engagement with digital devices and psychosocial stress associated with prolonged social isolation were important risk factors for the development of myopia. (6, 14). During the COVID-19 pandemic, the outdoor activities of children and teenagers were reduced because of the various lockdown measures imposed on populations everywhere to contain the spread of the virus. The time of outdoor activities in Handan decreased from 1.84 ± 1.43 hours per day to 0.98 ± 1.01 hours per day. In Hong Kong, the students spent 0.4 hours/day on outdoors (30). A previous meta-analysis has found that outdoor time has a protective effect on myopia onset (32). With the spread of COVID-19, there has been an increase in quarantine dry eye patients all around the worldwide (33). During the COVID-19 pandemic, too much or too little indoor lighting can have an impact on children's vision development (34). In short, prolonged digital device time, dry eye, reduced outdoor activity time, too bright or too dark light and psychosocial pressure may all be risk factors for the progression of myopia.
However, this study has several limitations. The first is selection bias due to a relatively small sample size. Although the sample size was small, the comprehensive and detail ophthalmic examinations were performed. Mydriatic refraction data and collected visual acuity and axial length data were collected and analyzed. Second, the exposed group and the control group were from two cities in different periods, but the two cities were both in Central China. The distance between two cities is approximately sixty kilometers. The diet, climate, socioeconomic status, and culture of the two cities are similar. With all Chinese students studying at home during the COVID-19 outbreak, the best match we found was with Anyang's children's data. The ages of the experimental group and the control group were matched, and the method of difference analysis was used. These minimize the impact of children's growth and development on results. Third, the data on the time and parameters of near-work and outdoor activities were not directly measured but were acquired by questionnaires, which may have led to recall bias. Due to the limited literacy ability of children, the questionnaire was completed by children and parents. To minimize recall bias, the questionnaire should be completed by children, and the parents should confirm the children's answers. Fourth, the auto-refractors of control group and exposure group were different, which may affect the measurement results. In the future, we will study and compare the measurement errors of the two devices.
Conclusions
The natural experiment provided the empirical evidence that children who studied at home are at high risk of myopia progression. Home quarantine and study-at-home during COVID-19 may worsen the global burden of myopia. Considering the persistence of COVID-19 and potential risk of study-at-home order again, continuous attention should be given to the occurrence and development of myopia.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of the Beijing Tongren Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
DM was responsible for collecting and analyzing data, interpreting results, and writing the abstract and the paper. SW, S-ML, XY, KC, JH, XP, RY, and JF contributed to reviewing of the data, interpreting results, and writing the tables and figures. AG, Z-BJ, and NW contributed to the design of the study, review, and feedback on the paper. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Fund Sponsorship of the Capital Public Health Project (Z171100000417017), the Beijing Natural Science Foundation (JQ20029), the Capital health research and development of special (2020-2-1081), the National Natural Science Foundation of China (82071000).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Qiao C, Zhang H, He M, Ying G, Chen C, Song Y, et al. Symptomatic COVID-19 in eye professionals in Wuhan, China. Ophthalmology. (2020) 127:1268–70. doi: 10.1016/j.ophtha.2020.04.026
2. Policy Brief: Education during COVID-19 and beyond. Available online at: https://www.un.org/sites/un2.un.org/files/sg_policy_brief_covid-19_and_education_august_2020.pdf. (accessed November 07, 2021).
3. CCTV News. Ministry of Education: national elementary and middle school network cloud platform opens for free use today. Available online at: http://www.chinanews.com/sh/2020/02-17/9094648.shtml. (accessed March 03, 2020).
4. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. (2020) 395:945–7. doi: 10.1016/S0140-6736(20)30547-X
5. Liu J, Chen Q, Dang J. Understanding risks of refractive error among Chinese children amidst pandemic disruptions: results from a rapid survey. BMC Ophthalmol. (2021) 21:370. doi: 10.1186/s12886-021-02133-9
6. Liu J, Chen Q, Dang J. Examining risk factors related to digital learning and social isolation: youth visual acuity in COVID-19 pandemic. J Glob Health. (2021) 11:05020. doi: 10.7189/jogh.11.05020
7. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
8. Yotsukura E, Torii H, Inokuchi M, Tokumura M, Uchino M, Nakamura K, et al. Current prevalence of myopia and association of myopia with environmental factors among children in Japan. JAMA Ophthalmol. (2019) 137:1233–9. doi: 10.1001/jamaophthalmol.2019.3103
9. Meng B, Li SM, Yang Y, Yang ZR, Sun F, Kang MT, et al. The association of TGFB1 genetic polymorphisms with high myopia: a systematic review and meta-analysis. Int J Clin Exp Med. (2015) 8:20355–67.
10. Pellegrini M, Bernabei F, Scorcia V, Giannaccare G. May home confinement during the COVID-19 outbreak worsen the global burden of myopia? Graefe's Arch Clin Exp Ophthalmol. (2020) 258:2069–70. doi: 10.1007/s00417-020-04728-2
11. Kuehn BM. Increase in myopia reported among children during COVID-19 lockdown. JAMA. (2021) 326:999. doi: 10.1001/jama.2021.14475
12. Alvarez-Peregrina C, Martinez-Perez C, Villa-Collar C, Andreu-Vázquez C, Ruiz-Pomeda A, Sánchez-Tena Miguel Á. Impact of COVID-19 home confinement in children's refractive errors. Int J Environ Res Public Health. (2021) 18:5347. doi: 10.3390/ijerph18105347
13. Mirhajianmoghadam H, Piña A, Ostrin LA. Objective and subjective behavioral measures in myopic and non-myopic children during the COVID-19 pandemic. Transl Vis Sci Technol. (2021) 10:4. doi: 10.1167/tvst.10.11.4
14. Liu J, Li B, Sun Y, Chen Q, Dang J. Adolescent vision health during the outbreak of COVID-19: association between digital screen use and myopia progression. Front Pediatr. (2021) 9:662984. doi: 10.3389/fped.2021.662984
15. Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. (2021) 139:293–300. doi: 10.1001/jamaophthalmol.2020.6239
16. Liang YB, Friedman DS, Wong TY, Wang FH, Duan XR, Yang XH, et al. Rationale, design, methodology, and baseline data of a population-based study in rural china: the handan eye study. Ophthalmic Epidemiol. (2009) 16:115–27. doi: 10.1080/09286580902738159
17. Li SM, Liu LR Li SY, Ji YZ, Fu J, Wang Y, et al. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. (2013) 20:348–59. doi: 10.3109/09286586.2013.842596
18. El-Shazly AA, Farweez YA, Elsebaay ME, El-Zawahry WMA. Correlation between choroidal thickness and degree of myopia assessed with enhanced depth imaging optical coherence tomography. Eur J Ophthalmol. (2017) 27:577–84. doi: 10.5301/ejo.5000936
19. Li SM Li H, Li SY, Liu LR, Kang MT, Wang YP, et al. Time outdoors and myopia progression over 2 years in chinese children: the anyang childhood eye study. Invest Ophthalmol Vis Sci. (2015) 56:4734–40. doi: 10.1167/iovs.14-15474
20. Donovan L, Sankaridurg P, Ho A, Chen X, Lin Z, Thomas V, et al. Myopia progression in Chinese children is slower in summer than in winter. Optom Vis Sci. (2012) 89:1196–202. doi: 10.1097/OPX.0b013e3182640996
21. Yu S, Diao H, Zeng J. Analysis of the prevalence and situation of myopia in adolescents from south China. Eye Sci. (2015) 30:53–7.
22. Chen Y, Drobe B, Zhang C, Singh N, Speggel DP, Chen H, et al. Accommodation is unrelated to myopia progression in Chinese myopic children. Sci Rep. (2020) 10:12056. doi: 10.1038/s41598-020-68859-6
23. Fujiwara M, Hasebe S, Nakanishi R, Tanigawa K, Ohtsuki H. Seasonal variation in myopia progression and axial elongation: an evaluation of Japanese children participating in a myopia control trial. Jpn J Ophthalmol. (2012) 56:401–6. doi: 10.1007/s10384-012-0148-1
24. Gwiazda J, Deng L, Manny R, Norton TT. COMET Study Group. Seasonal variations in the progression of myopia in children enrolled in the correction of myopia evaluation trial. Invest Ophthalmol Vis Sci. (2014) 55:752–8. doi: 10.1167/iovs.13-13029
25. Clark TY, Clark RA. Atropine 0.01% eyedrops significantly reduce the progression of childhood myopia. J Ocul Pharmacol Ther. (2015) 31:541–5. doi: 10.1089/jop.2015.0043
26. Larkin GL, Tahir A, Epley KD, Beauchamp CL, Tong JT, Clark RA. Atropine 0.01% eye drops for myopia control in American children: a multiethnic sample across three US sites. Ophthalmol Ther. (2019) 8:589–98. doi: 10.1007/s40123-019-00217-w
27. Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. (2018) 125:1239–50. doi: 10.1016/j.ophtha.2017.12.011
28. Cui D, Trier K, Munk RS. Effect of day length on eye growth, myopia progression, and change of corneal power in myopic children. Ophthalmology. (2013) 120:1074–9. doi: 10.1016/j.ophtha.2012.10.022
29. Zhang ZY, Zhang XR Yu ZQ. Association of peripheral hyperopia with axial elongation in high myopia. Graefe's Arch Clin Exp Ophthalmol. (2013) 251:2277. doi: 10.1007/s00417-013-2277-8
30. Zhang X, Cheung SSL, Chan HN, Zhang Y, Wang YM, Yip BH, et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: a population-based prospective study. Br J Ophthalmol. (2021) 319307. doi: 10.1136/bjophthalmol-2021-319307
31. Lanca C, Seang-Mei S. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Opt. (2020) 40:216–29. doi: 10.1111/opo.12657
32. Deng L, Pang Y. Effect of outdoor activities in myopia control: meta-analysis of clinical studies. Optom Vis Sci. (2019) 96:276–82. doi: 10.1097/OPX.0000000000001357
33. Napoli PE, Nioi M, Fossarello M. The “Quarantine Dry Eye”: the lockdown for coronavirus disease 2019 and its implications for ocular surface health. Risk Manag Healthc P. (2021) 14:1629–36. doi: 10.2147/RMHP.S277067
Keywords: study-at-home, COVID-19, children, myopia progression, cycloplegic spherical equivalent
Citation: Ma D, Wei S, Li S-M, Yang X, Cao K, Hu J, Peng X, Yan R, Fu J, Grzybowski A, Jin Z-B and Wang N (2022) The Impact of Study-at-Home During the COVID-19 Pandemic on Myopia Progression in Chinese Children. Front. Public Health 9:720514. doi: 10.3389/fpubh.2021.720514
Received: 09 June 2021; Accepted: 06 December 2021;
Published: 06 January 2022.
Edited by:
Noor Hazilah Abd Manaf, International Islamic University Malaysia, MalaysiaReviewed by:
Ji Liu, Shaanxi Normal University, ChinaIndri Hapsari Susilowati, University of Indonesia, Indonesia
Copyright © 2022 Ma, Wei, Li, Yang, Cao, Hu, Peng, Yan, Fu, Grzybowski, Jin and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ningli Wang, d25pbmdsaSYjeDAwMDQwO3ZpcC4xNjMuY29t; Zi-Bing Jin, amluemliaW5nJiN4MDAwNDA7Zm94bWFpbC5jb20=
†These authors have contributed equally to this work
 Dandan Ma
Dandan Ma Shifei Wei
Shifei Wei Shi-Ming Li
Shi-Ming Li Xiaohui Yang1
Xiaohui Yang1 Kai Cao
Kai Cao Xiaoxia Peng
Xiaoxia Peng Ruohua Yan
Ruohua Yan Andrzej Grzybowski
Andrzej Grzybowski Zi-Bing Jin
Zi-Bing Jin Ningli Wang
Ningli Wang