
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health , 22 November 2021
Sec. Public Health Policy
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.715904
The SARS-CoV-2 pandemic has caused tragic morbidity and mortality. In attempt to reduce this morbidity and mortality, most countries implemented population-wide lockdowns. Here we show that the lockdowns were based on several flawed assumptions, including “no one is protected until everyone is protected,” “lockdowns are highly effective to reduce transmission,” “lockdowns have a favorable cost-benefit balance,” and “lockdowns are the only effective option.” Focusing on the latter, we discuss that Emergency Management principles provide a better way forward to manage the public emergency of the pandemic. Specifically, there are three priorities including the following: first, protect those most at risk by separating them from the threat (mitigation); second, ensure critical infrastructure is ready for people who get sick (preparation and response); and third, shift the response from fear to confidence (recovery). We argue that, based on Emergency Management principles, the age-dependent risk from SARS-CoV-2, the minimal (at best) efficacy of lockdowns, and the terrible cost-benefit trade-offs of lockdowns, we need to reset the pandemic response. We can manage risk and save more lives from both COVID-19 and lockdowns, thus achieving far better outcomes in both the short- and long-term.
The Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) that causes Coronavirus Disease 2019 (COVID-19) was declared a pandemic in March 2020. Governments have made (often suboptimal) decisions to manage the pandemic crisis, often focusing only on the many cases and deaths worldwide caused by COVID-19. Attempting to “flatten the curve” of cases and deaths, governments have implemented unprecedented restrictions on Charter rights and freedoms, the lockdowns and “circuit-breakers” (time-limited lockdowns that were not time-limited). By lockdown we mean any combination of non-pharmaceutical interventions (NPIs) that imposed mandated social distancing measures and/or restrictions on mobility (e.g., school closures, restaurants and large shopping centers closure, workplace closures, limits on gathering sizes, closure of public transport, stay-at-home orders, and even curfews). Many studies we will refer to used a stringency index to indicate the severity of these lockdown measures; as stringency becomes more severe, the collateral damage may become worse. We present several mistaken assumptions that we believe have led to the lockdown approach to the pandemic. We argue that a better response to the pandemic must occur, one that saves more lives, causes fewer harms, and restores trust.
Many more infections occur than are detected and diagnosed as cases. The case fatality rate is thus much higher than the infection fatality rate (IFR, the number of people with SARS-CoV-2 infection that will die of COVID-19), often over 10-times higher (1, 2). In an analysis of international reports the median IFR was 0.23%, median for people <70 years was 0.05% (99.95% infection survival) (1), and this was lower than for influenza in people <50 years (Table 1). Other reviews also found that IFR increased with age, with an inflection point at approximately age 70 years (2, 4). A review of IFR studies suggested an overall population IFR of 0.15% (3, 5). The case fatality rate in Canada is compatible with these data (Table 2).
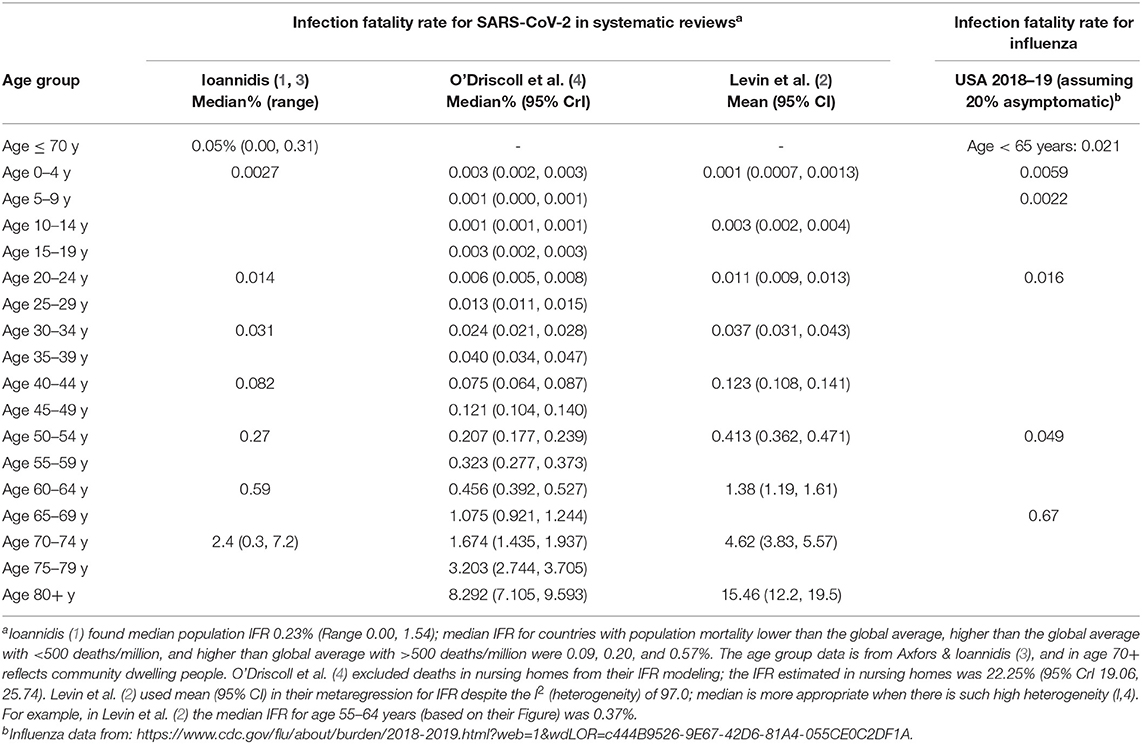
Table 1. SARS-CoV-2 age-specific infection fatality rates compared to infection fatality rates from Influenza in the United States.
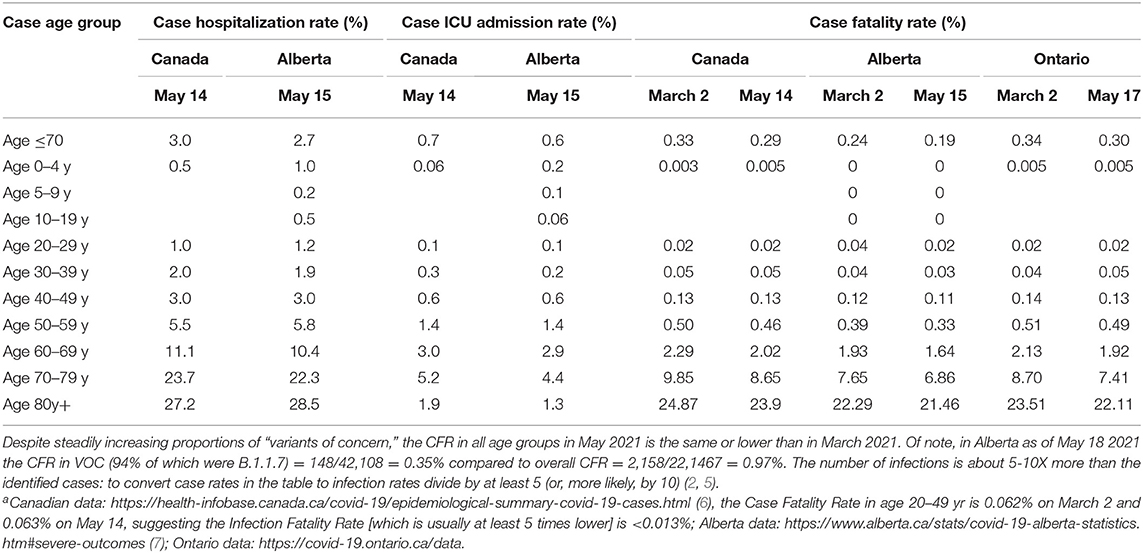
Table 2. Case hospitalization, intensive care unit, and fatality rate for SARS-CoV-2 in Canada and selected Provinces as of mid-May, 2021a.
People ≥70 years, and 60–69 years with multiple severe comorbidities (e.g., obesity, diabetes mellites, kidney-disease, dementia) are at most risk for severe outcomes from SARS-CoV-2 (6, 8). In Canada, as of March 2, 89% of deaths occurred in people ≥70 years, and most (68%) other deaths were in people 60–69 years, usually with multiple comorbidities (7, 9). Of deaths, >70% occurred in long-term care homes for older people (10). People ≥70 years accounted for many hospitalizations (55%), intensive-care admissions (39%), and deaths (89%) across Canada (7). These are the groups of people that required protection.
Another consistent association with hospitalization and mortality from COVID-19 is social vulnerability, including risks from poverty or low-income (often associated with essential high-exposure occupations without job security, unemployment, lower education attainment, lack of health insurance, and food insecurity), household composition (e.g., single parent home, people with disability) and type (e.g., household crowding, lack of a vehicle, use of public transport for work commuting), and racial or ethnic minority status (e.g., African American, American Indian, Hispanic, often with limited English-speaking ability) (11, 12). People from racial and ethnic minorities have been more adversely affected by the pandemic, and not due to inherent biologic differences. Minority groups are a proxy for the “structural racism and social inequalities [affecting their social determinants of health] embedded within the economic, political, health care, criminal justice, and other systems and social structures (13)” (13–18). These result in higher exposure to and onward transmission of SARS-CoV-2 (e.g., inability to socially distance, work from home, or even wash hands; multi-generational housing units; densely populated communities), higher susceptibility to severe COVID-19 (e.g., more chronic non-communicable diseases, poor health due to stress and food insecurity, poor access to communication, poor access to healthcare), and lack of timely access to quality healthcare once sick (11–21). Within these vulnerable groups, people who are older and people with multiple severe comorbidities require specific strategies for focused protection.
The absolute number of cases and deaths we are bombarded with daily are given without denominators nor context. In Canada, in non-pandemic 2019, there were >797 deaths/day and 291,000 deaths/yr (22). Over the past 12 months, as of March 2, 2021, there have been 21,799 COVID-19-associated deaths in Canada, thus accounting for <7% of overall deaths (7). Many of these deaths were in people who in other years may have died from other causes. Globally, over the first year of the pandemic, COVID-19 accounted for 4.1% of deaths (23, 24); motor vehicle collisions, alcohol use, tobacco use, fossil fuel combustion fine particulate matter pollution, and poor diet accounted for 2.3, 5.1, 13.7, 14.9, and 18.8% of deaths respectively (25–29).
A focus on case counts is not as important as the data about hospitalization, intensive care admission, and mortality, for several reasons: the large majority of cases (milder symptomatic cases and asymptomatic infections) are not detected because they are not tested (1, 2), lockdowns were intended to preserve hospital and intensive care healthcare capacity and prevent deaths, and the risk to everyone (anyone, of any age or demographic) is not so high that protection of all from all cases must be a goal. For example, population-wide lockdowns are not used for seasonal influenza that has similar risk as COVID-19 to those aged <50 years old. We do not close down society in attempt to protect everyone from highly prevalent causes of death including motor vehicle collisions, alcohol use, tobacco use, fossil fuel combustion, and poor diet. Instead, those people at reasonably high risk for adverse outcomes from these threats are the people who require focused protection. For COVID-19, this includes people aged ≥70 years, and people aged 60–69 years with multiple severe comorbidities. The assumption that everyone can be protected equally, when their risks are markedly different, only contributed to population fear.
Many assume there is good evidence that lockdowns are required to protect high-risk people from SARS-CoV-2 infection. The efficacy of lockdowns to reduce transmission, cases and deaths has likely, at best, been highly exaggerated. Many studies found that more restrictive lockdowns in different international locations were not associated with any clear effect on “flattening-the-curve” of cases or deaths (Tables 3, 4) (30–61). Unrecognized confounding (e.g., seasonality, population density and age-structure, life-expectancy progression, etc.) and modeling errors likely account for studies that have suggested lockdowns to be an effective strategy (31, 46, 51, 58). It is possible that lockdowns cannot markedly reduce transmission as people continue to carry out their essential activities, and as, in the attempt to avert infections inside a system, lockdown restrictions in fact create forced congestion (and hence transmission) in other parts of the system (62). For example, young people may have returned to or stayed home (where most transmission occurs) with older parents due to unemployment or university closures, and risk may have simply been shifted from the professional class to the working class, who cannot afford not to work (63, 64). The incremental effect of lockdowns on transmission to those at high-risk may be nonexistent after accounting for endogenous behavior change by individuals (52, 58). Individual endogenous level behaviors that are likely more important than lockdowns may include wearing masks, maintaining distance when encountering individuals (i.e., tailored physical distancing according to risk), and limiting large-size gatherings of individuals (65, 66).
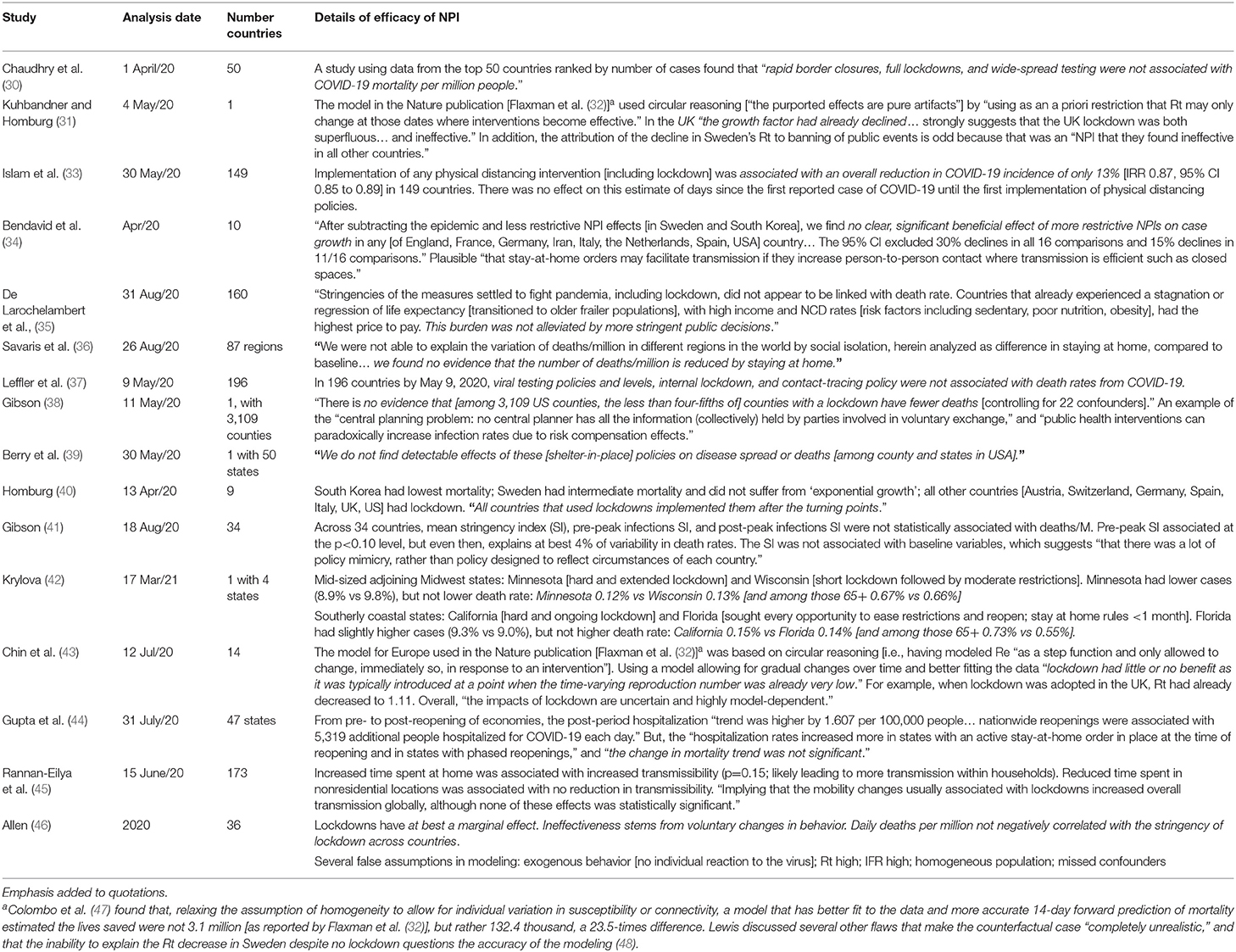
Table 3. Peer reviewed published studies suggesting that efficacy of nonpharmaceutical interventions (lockdowns) to prevent spread of COVID-19 are at best highly exaggerated.
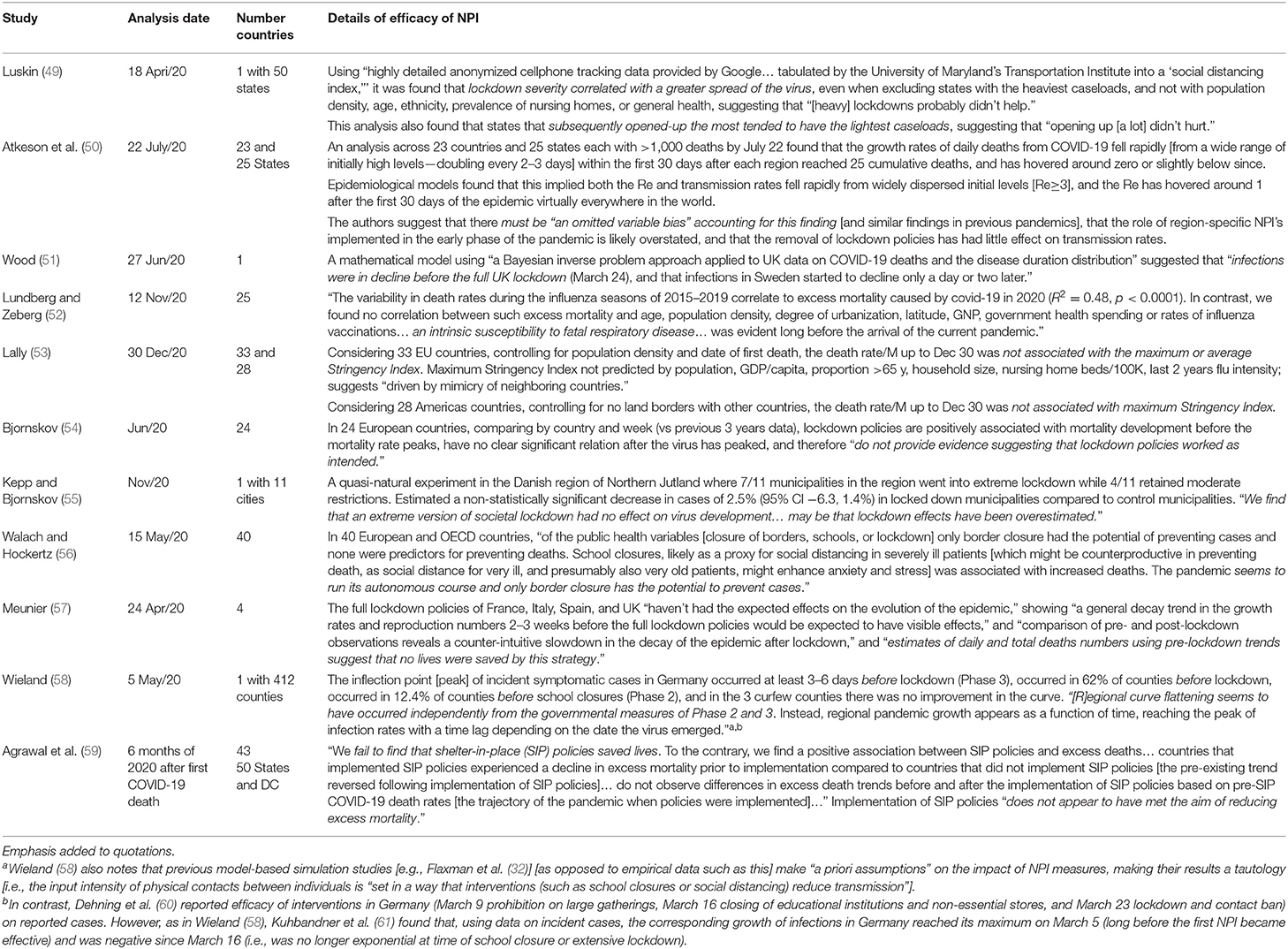
Table 4. Studies published as preprints suggesting that efficacy of nonpharmaceutical interventions (lockdowns) to prevent spread of COVID-19 are at best highly exaggerated.
We acknowledge that some studies have reported efficacy of lockdowns. In the John Snow Memorandum published in Lancet it was claimed that lockdowns were “essential to reduce mortality” (67). The two studies referenced there to support the claim (32, 60) have been refuted by several studies that point out circular and flawed methodology (31, 47, 48, 51), or use of inaccurate data (58, 61) (see Tables 3, 4 for some details of the refuting studies). Other positive studies did not control for the many possible confounders inherent in cross-country comparisons (68). Of interest, several studies have compared the timing of implementation of many different NPIs across countries to determine their (unadjusted for confounders) possible effect on the effective reproductive number (Rt) of SARS-CoV-2 in the respective countries (69–71). Although some NPIs have been suggested as effective using this methodology, these studies have also found the following: substantial variation between world geographical regions in terms of NPI effectiveness (69); less disruptive and costly NPIs can be as effective as more intrusive drastic ones (69); and inconsistent/inconclusive evidence for stay-at-home requirements, public transport closure, international travel controls, testing, contact tracing, and business closures (even finding a paradoxical increase in Rt for some interventions including closure of public transport, stay-at-home requirements, and contact tracing) (69–71). In addition, we question whether the reduction of population-wide Rt is the goal of NPIs; we argued above that the control of hospitalizations and deaths (not simply “cases”) is the goal of NPIs, and Rt may not reflect this for the most vulnerable people in the population.
These findings should not be surprising. Several earlier publications on influenza pandemic management by experts at the Centers for Disease Control, a panel convened by the US Department of Health and Human Services, and the WHO consistently recommended against closing schools, closing large gatherings, quarantine, and border screening, and instead recommended less invasive voluntary measures (72–74). Most recently, in 2019 the WHO recommended against contact tracing and home quarantine of exposed individuals, conditionally recommended workplace closures only as a last step in extraordinarily severe pandemics, and conditionally recommended avoiding crowding for “people who gather in crowded areas (e.g., large meetings, religious pilgrimages, national events and transportation hub locations)” (75). Most governments ignored these previous lessons and written pandemic plans.
In order to deny charter freedoms, “reasonable limits [that are] demonstrably justified” are necessary, which requires the due-diligence of a cost-benefit analysis (76). Several reports find that lockdowns, even if they were to be highly effective, can be predicted to cause at least 5–10-times more harm to population wellbeing and deaths in the long-term than they prevent (46, 53, 77–79). Harms include economic recession, unemployment, loneliness, poverty and food insecurity, deterioration of mental health with increased suicides and substance use, increased intimate partner violence and child abuse, lost education and future potential in children, delayed/disrupted health care for serious conditions, and increased societal inequality (79, 80). Framing a recession as being “the economy vs. lives” is a dangerous false dichotomy; as governments can spend less on the social determinants of health, including healthcare, education, roads, sanitation, housing, nutrition, vaccines, safety, social security nets, clean energy, etc., statistical lives will be lost in the years to come (77–79). Importantly, the negative effect of a drop in GDP on population wellbeing and lifespan consistently occur over the long-term, even though not detectable during the short-term due to temporary increased government spending (11, 81–83). Unemployment and loneliness are two of the strongest risk factors for shortened lifespan and chronic diseases (84).
Cost-benefit analyses of each alternative set of possible response measures should be performed, using a common metric that allows making commensurable comparisons among all outcomes, such as the WELLBY or QALY metric (77, 79, 83, 85–87). When done, these analyses have consistently found lockdowns to have higher costs than benefits (Table 5) (46, 53, 77–79, 88–93). Of note, these cost-benefit analyses have made assumptions in favor of lockdowns (i.e., marked reductions in COVID-19 fatalities), and very conservative against lockdowns (e.g., not including the predictable effects of loneliness and unemployment on lifespan and chronic disease, of societal disruption on world food insecurity and poverty rates, of interrupted health care on conditions other than COVID-19; and using the highest estimates of the value of QALY or WELLBY) (11, 77, 84, 92). Therefore, despite the difficulties inherent in complex cost-benefit analyses, the results strongly suggest that lockdowns do not have a favorable cost-benefit balance.
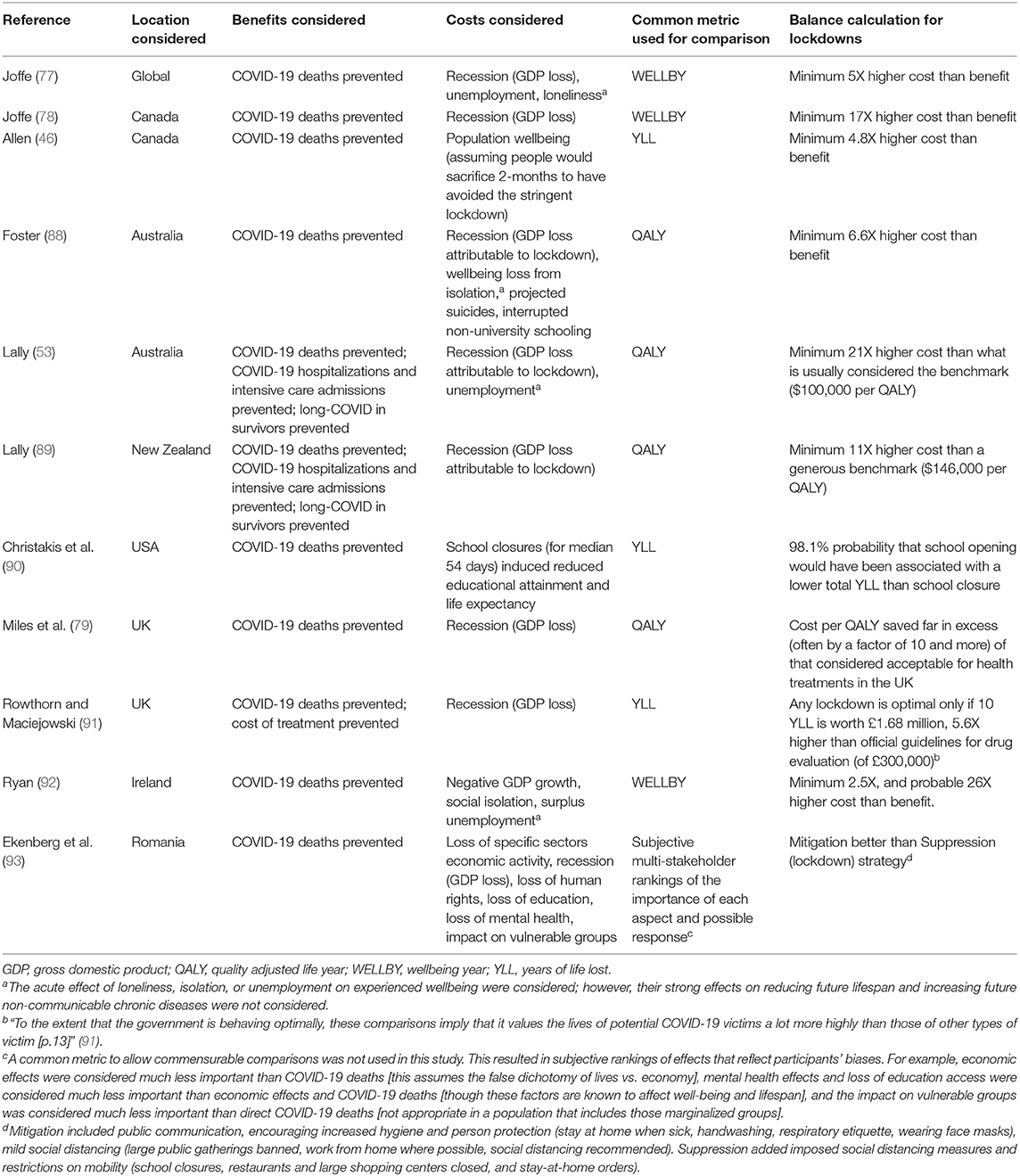
Table 5. Cost-benefit analyses of lockdowns (assuming their efficacy) as the response to the pandemic.
We believe lockdowns reflect the public's unreasonable fear of SARS-CoV-2 and lack of confidence that the government can manage the sick. In order to minimize collateral harms, this fear must be replaced by confidence. Many of the common objections regarding the cost-benefit balance and the necessity of lockdowns are considered in Tables 6, 7 (94–132). Unfortunately, as far as we are aware, governments have not done cost-benefit analyses of the lockdowns that they implemented, and thus have not done their due-diligence that is required by the Charter of Rights and Freedoms in Canada (76, 130).
The pandemic is better framed as a public emergency, not a public health emergency. This is because the pandemic is affecting all sectors of society (not just the healthcare system), and the process of emergency management (EM) is necessary to respond. A public emergency response aims to minimize the impact of the hazard, SARS-CoV-2, on our society as a whole (130–132). This requires a written EM plan released to all citizens. A coordinating agency [in Canada, the provincial EM Agency] is required to coordinate requests from the Subject Matter Agency [public health] dealing with the direct effects of the virus, while also dealing with the indirect effects of the pandemic.
Emergency Management (EM) is the prevention and mitigation of, preparedness for, response to, and recovery from emergencies regardless of the hazard/risk (130, 132). Emergency Management Agencies (EMA) are charged with this mitigation, preparedness, response, and recovery to all hazards (130, 132). These EMA are established, staffed, trained, and equipped to manage the governance, operations, planning, intelligence, logistics, communications, finances, administration, public/private sector collaboration, and training necessary to respond to any emergency (132). There are defined steps in this process. First is identification of the hazard, in this case SARS-CoV-2. Second is selection and maintenance of the aim (or mission), in this case to minimize the impact of SARS-CoV-2 on the jurisdiction (i.e., not to flatten the curve, or protect the medical system, which are incorporated into objectives). Third is to establish a comprehensive Governance Task Force to provide leadership for all policy, programs, and actions taken, led by the Premier. Fourth is a risk/hazard assessment to give detailed assessment of the risk (e.g., the extremely age-dependent mortality especially with comorbidities, impacts on critical infrastructure including healthcare, specific considerations for socially vulnerable groups). Fifth is the Mission Analysis that lays out a list of objectives of what needs to be done, including tasks given (pre-written) and tasks implied, required to meet the Aim. This always includes ways to maintain confidence in government and diminish fear, ensure mutual aid, and ensure constant communications, and in this case would also include objectives to protect seniors, and to protect critical infrastructure and essential services (e.g., new medical surge capacity, full continued education, continuity of business and economy). Sixth is Defining Courses Open/Options, how the objectives can be met, a series of courses open for each grouping of tasks as determined by assigned teams with appropriate diverse expertise (to prevent groupthink). Each course open has a full assessment of advantages/disadvantages (i.e., a cost-benefit analysis) to justify options and plan for solutions to collateral damage. Seventh is public issuing of a written, comprehensive, evidence-based pandemic response plan, which forms the basis of confidence in government, is a statement of transparent demonstrably justified due diligence, and establishes that the government has a plan, is ready to respond, and is open to suggestions to improve the plan. This giving citizens of voice is important for trust in government and policy acceptance (121).
In the 2014 Alberta Pandemic Response plans the four goals were: controlling the spread of infection and reducing illness and death from the virus, mitigating societal disruption by ensuring continuity and recovery of critical services, minimizing adverse economic impact, and supporting an efficient and effective use of resources (133). These form the basis of the Mission Analysis, overarching objectives (tasks given) in the EM process, and are broken down into smaller manageable tasks; for example, care of the most at risk, assurance of medical capacity, assurance of education, etc. Similarly, the four concurrent critical functions of EM are mitigation (i.e., attempt to separate the threat from the potential targets, or separate the targets from the potential threat), preparedness (e.g., building capability to effectively and rapidly respond when items at risk are affected by the hazard), response (e.g., execution of the capability to prevent injury and loss of life, protect property and critical resources, and meet basic human needs), and recovery (e.g., re-establishment of the economy and a state of normal life) (131, 132). These functions guide the Mission Analysis and Courses Open/Options steps of the process.
Others have suggested that decision-making has been made under “suboptimal conditions” of high stakes, time pressure, complexity, and uncertainty, leading to information-processing failures and poor outcomes (121). Further, they suggest “using reflexivity to counteract” these failures (121). The information-processing failures included several steps. First, a failure to search for and share relevant information, especially due to groupthink [e.g., “a biased sampling of information,” a “focus on agreement at all costs,” including ignoring or suppressing information not in line with the majority view] (121). Second, a failure to elaborate on and analyze information, especially due to framing effects [e.g., framed narrowly as the number of lives lost, only from COVID-19; as an action-oriented “war against an invisible enemy” with “warriors” on the “frontline” and “traitors” questioning the response] (80, 121). Third, a failure to update conclusions in the light of new information, especially due to escalation of commitment [“investing more resources in a set course of action, even in the face of clear evidence that it is not working;” giving clarity of direction by sticking to a chosen course of action] (121). Team reflexivity, “a deliberate process of discussing team goals, processes, or outcomes—can function as an antidote to biases and errors in group decision-making,” taking “steps to maximize the decision-making process and increase the chances of positive outcomes” (121). This involves several steps. First, a holistic approach, that focuses on “widening the array of opinions considered” and “avoiding an overreliance on experts” (121). Second, a frame that is broader (i.e., “societal well-being”), that “explicitly considers and weights possible consequences for a variety of societal stakeholders,” while “increasing the number of options or solutions considered” (121). Third, an ongoing process, one that constantly reassesses the situation and is “willing and able to reflect on the actions they have taken, and, when necessary, are prepared to change the current direction or make adjustments [based on the evidence]” (121). Overall, there is accountability for the decision-making process. This is what the Emergency Management process is all about: requiring that all stakeholders are included in a defined process that demands all tasks, given and implied, are developed with options based on detailed cost-benefit analysis and continual feedback so that leadership can make fully informed decisions.
We believe that these critical functions were not achieved by the lockdown approach, with ongoing deaths in long-term care homes and seniors (poor mitigation), societal disruption and economic devastation (poor recovery and response), and sub-optimal use of resources (poor preparedness and response). The concept of precision shielding can demonstrate the failure of lockdowns in many countries, including Canada. Ioannidis proposed the shielding ratio, “defined as the ratio of prevalence of infection among people in a high-risk group vs. among people in a low-risk group” that can be estimated as follows: (G) (IFRl) (1-fh)/(IFRh) [(fh-(G)(fh)], where G is the proportion of COVID-19 deaths contributed by the high-risk group, f is the relative share of the high-risk (h) or low-risk (l) group to the general population, and IFR is the infection fatality rate in the high-risk (h) or low-risk (l) group (134). For the elderly high-risk group (age ≥70 years) Canada had a shielding ratio very close to 1.0 (i.e., no shielding), and Spain and China had inverse shielding (the elderly were infected more frequently than younger populations) (134). For the nursing home residents high-risk group, inverse shielding occurred in Belgium, UK, Spain, and likely USA (134). Performing the calculation for nursing home residents in Canada as (0.73) (0.002) (1–fh)/(0.25) [(fh-(0.73) (fh)] with fh being 160,000/36,110,000, the shielding ratio was 4.9 (i.e., strong inverse shielding). In addition, for example in the United States, minority groups have had higher rates of age-adjusted hospitalizations and deaths by a factor of 2.9 and 2.0 for African Americans, 2.8 and 2.3 for Hispanic or Latino, and 3.3 and 2.4 for American Indian or Alaska Native groups, again inverse shielding (14, 135). This suggests that the non-focused measures used (i.e., lockdowns) did not protect the most vulnerable in Canada or elsewhere, leaving nursing home personnel and residents more exposed than the rest of the population, and exacerbating social inequalities in the population (134). Despite the adverse and unequal effects of lockdowns on the general population (e.g., loneliness, mental health deterioration, unemployment, recession, interrupted healthcare, and interrupted education), and the attempts to provide surge “capacity” in healthcare (e.g., by interrupting healthcare for non-COVID-19 illness), the most vulnerable groups were not protected and were even put at higher risk.
Many others have made the point that less restrictive mandates for social distancing should have been considered; this includes the studies discussed above that found more stringent measures were not associated with reduced viral transmission and deaths, and the cost-benefit studies finding stringent lockdown measures to have much higher costs than benefits. Many diverse stakeholders should be involved in planning to ensure that all costs and benefits, and all possible alternative measures are considered in a deliberative process that aims to determine the best response while minimizing cognitive biases (77, 122). Using EM principles, better priorities are clear.
First, we must protect those most at risk by separating them from the threat (mitigation). This means protection of concentrations of older people, particularly in long-term care homes. Residents and staff should be placed in quarantine, with volunteer staff asked to work 1-month-on and 1-month-off living away from their families with generous compensation. This may be done in new larger facilities to reduce staffing demands. More well-paid, well-trained staff working in only one facility with adequate personal protective equipment are required. This can prevent most deaths and much of the challenges to hospital capacity. Other seniors with multiple severe co-morbidities also require voluntary quarantine, with plans for either separate housing in temporary long-term-care-like facilities, or in-home quarantine with a voluntary primary and secondary caregiver, and home delivery of groceries and other essentials (63, 64). This would prevent most other deaths and challenges to hospital capacity. In effect, focused protection “reduces COVID-19 mortality by better protecting the elderly and other high-risk groups [while] children and low-risk adults, for whom lockdowns cause more physical and mental suffering than COVID risk does, are encouraged [for those who decide] to live near-normal lives” (63, 64, 136). This is based on evidence of the extreme age-dependent risk from COVID-19, and the extreme harms of population-wide lockdowns.
Second, we must ensure critical infrastructure is ready for people who get sick, by being capable (prepared) and executing this capability (response) to protect and treat those affected by the threat. This means building new surge capacity in hospitals, without canceling or delaying healthcare for diseases other than COVID-19. Public health leaders should be tasked with ensuring we build and segregate an appropriate number of intensive-care and hospital beds to handle any surge. Healthcare workers who are asymptomatic (and exposed or even swab positive) can continue to work in hospitals with universal staff masking policies as transmission is rare (109). The healthcare workforce can also be better preserved by not closing schools [which can deplete over 15% of the workforce due to childcare responsibilities (110)], voluntary re-deployment of retired staff, and rapid on-the-job training of senior nursing and medical trainees.
Third, we must shift the focus of response from fear to confidence. Do not chase case counts, as reducing hospitalization and mortality are the goals of mitigation. Do not lockdown everybody, as this causes immense economic and collateral damage. Keep schools open, as this prevents the predictable adverse effects on children from loss of socialization, education, earning potential, and future lifespan. In addition, children are at lower risk from SARS-CoV-2 than from seasonal influenza (Table 1), school transmission is rare, and teachers have similar or lower risk of SARS-CoV-2 transmission than other workers of their age (137–141). Removing fear will be very difficult. The public has been bombarded with fear-inducing information from the media (80, 121). Government intentionally (e.g., in the UK) or unintentionally encouraged covert psychological strategies to induce compliance with lockdowns (142, 143). This has been done by inducing fear (an inflated perceived threat level), shame (conflating compliance with virtue), and peer pressure (portraying non-compliers as a deviant minority) (142, 143). This included presenting daily death and case counts without context (i.e., without denominators, background death rates, or information about the extreme age-dependent risk), inflated predictions of future cases and deaths (using flawed forecasting) (107), repeated pictures from worst case examples of how terrible the illness can be (implying how deadly the virus can be to everyone), warning that hospital capacity will be overwhelmed if there is noncompliance, and using scary slogans (e.g., telling children not to kill their grandparents, and that normality is only possible if they get vaccinated). This may have involved “agnotology”, “the ways ignorance or doubt about certain topics is [culturally] created by means of withholding or presenting information in a certain way” (80). For example, framing as loss (i.e., deaths) and “war” with censorship of dissent (e.g., erosion of civility in academic discourse) (144–146), and reliance on social influence (e.g., group conformity, and obedience to authority) and superstitious bias (e.g., a need to see a relation between behavior, particularly sacrifices, and outcomes, even if this relation is not there) (80).
The fear can only be shifted to confidence using honest clear information provision and rational argument (147, 148). Daily messaging and presentations delivered personally by government leaders must repeatedly focus on educating the public on the difficult trade-offs involved (i.e., the benefits and harms of lockdowns, including their massive collateral damage and the false dichotomy of lives vs. the economy), the risks from SARS-CoV-2 (i.e., the extreme age-dependent risk of severe outcomes, particularly in people with co-morbidities) placed in context of other diseases and causes of death (risks the public routinely face) (147, 148), and the justification for the priorities of focused protection of people at high-risk of adverse outcomes (including how this will be done) and ensuring the medical system is robust to manage people with COVID-19 (including plans for surge capacity). By informing the public in this way that its government knows how to deal with the situation and has a written pandemic plan, the fear, societal disruption and adverse economic impacts can be mitigated. This shift will be gradual and require repeated clear accurate messaging. It will require admitting errors, explaining that there will be deaths and suffering whatever is decided, and that the goal is to have the least possible death and suffering. In addition, many have experienced emotions similar to grief, with emptiness, sadness, and loss of meaning in life from a loss of normalcy, and functional coping strategies have been blocked by lockdowns (e.g., eating healthily, seeking social support, and exercise). Improving access to better coping strategies will be important (80, 149, 150).
Each of these priorities must also include a strong health equity perspective, attempting to address upstream/midstream policy and institutional factors, and to implement downstream rapid responses in ways that ensure the well-being of all of society, including socially vulnerable groups (11, 13, 14, 81). The aim of the EM process is to design a system to protect the most at risk, wherever they are found, regardless of race, color, religion, socioeconomic level, sexual orientation, etc. Critical steps to operationalize in order to fulfill the four EM critical functions, and achieve these three priorities, are shown in Table 8, with equity considerations included.
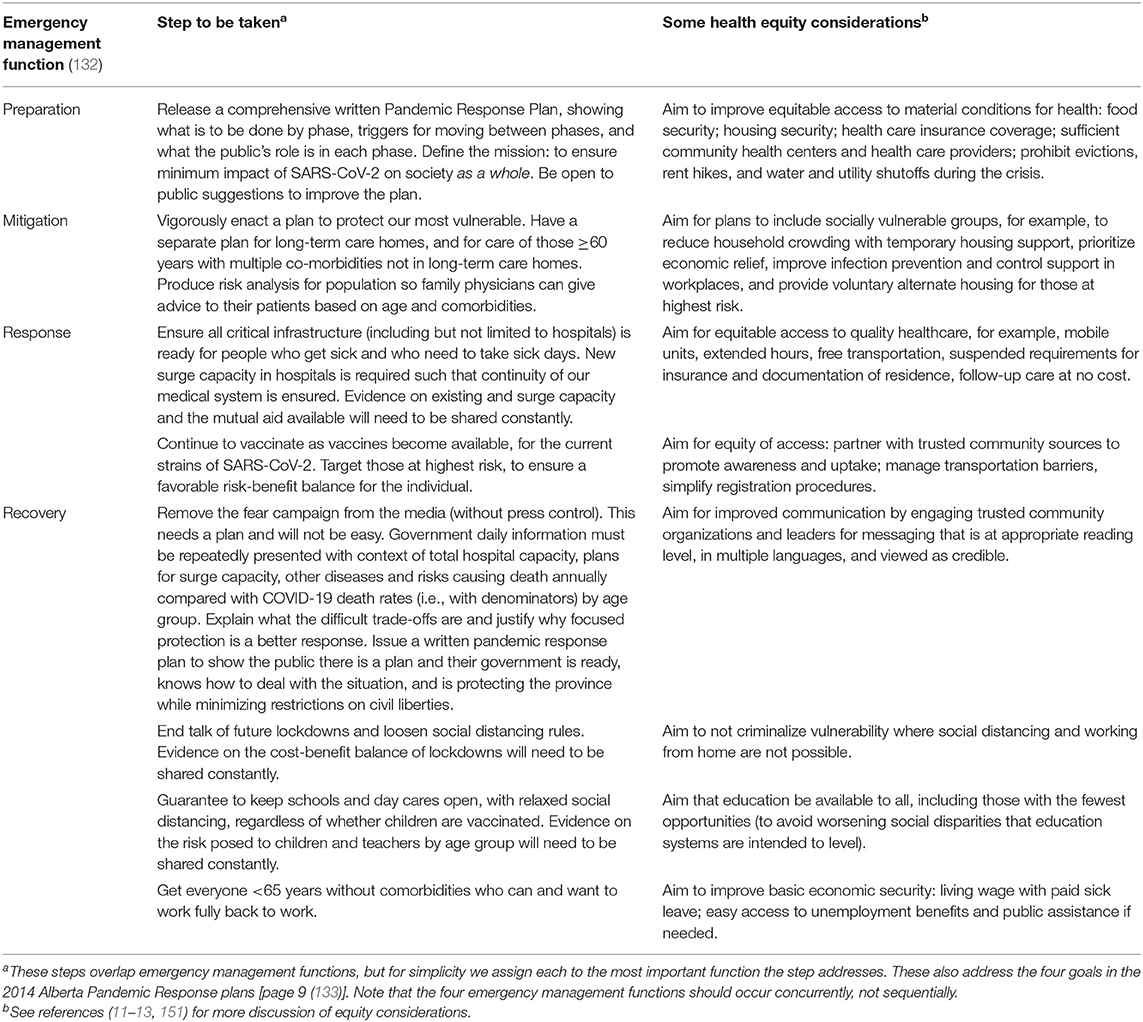
Table 8. Next steps for a better way forward focusing on the concurrent emergency management functions.
Based on EM principles, the age-dependent risk from SARS-CoV-2, the minimal (at best) efficacy of lockdowns, and the terrible cost-benefit trade-offs of lockdowns, we suggest that an EM Agency (e.g., in Canada, in each province) take charge of coordinating the pandemic response. We need to reset the pandemic response so that we can manage risk and save more lives from both COVID-19 and lockdowns, thus achieving far better outcomes in both the short- and long-term.
AJ and DR contributed to conception and design of the work, acquisition, analysis and interpretation of the data, and substantial critical revisions of the manuscript for important intellectual content, have approved the submitted version, and have participated sufficiently in the work to take public responsibility for the content. AJ wrote the first draft of the article. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
COVID-19, Coronavirus Disease 2019; EM, emergency management; IFR, infection fatality rate; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus-2.
1. Ioannidis JPA. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull World Health Organ. (2021) 99:19–33F. doi: 10.2471/BLT.20.265892
2. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. (2020) 35:1123–38. doi: 10.1007/s10654-020-00698-1
3. Axfors C, Ioannidis JPA. Infection Fatality Rate of COVID-19 in Community Dwelling Populations With Emphasis on the Elderly: An Overview. medRxiv [Preprint] (2021). doi: 10.1101/2021.07.08.21260210
4. O'Driscoll M, Dos Santos GR, Wang L, Cummings DAT, Azman AS, Paireau J, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. (2021) 590:140–5. doi: 10.1038/s41586-020-2918-0
5. Ioannidis JPA. Reconciling estimates of global spread and infection fatality rates of COVID-19: an overview of systematic evaluations. Eur J Clin Invest. (2021) 51:e13554. doi: 10.1111/eci.13554
6. Erdman R, NcRae A, MacKay E, Hicks A, Norris C, Saini V, et al. COVID-19 Scientific Advisory Group Rapid Evidence Report. Topic: What risk factors (such as age, medical conditions, or lifestyle factors) are associated with the development of severe outcomes in COVID-19? Alberta Health Services, COVID-19 Scientific Advisory Group (2020). Available online at: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-sag-risk-factors-for-severe-covid-19-outcomes-rapid-review.pdf (accessed May 26, 2021).
7. Government of Canada. Coronavirus Disease 2019 (COVID-19): Epidemiology Update (2021). Available online at: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed May 26, 2021).
8. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. (2020) 584:430–6. doi: 10.1038/s41586-020-2521-4
9. Alberta Health Services. COVID-19 Alberta Statistics (2021). Available online at: https://www.alberta.ca/stats/covid-19-alberta-statistics.htm#highlights (accessed May 26, 2021).
10. National Institute on Aging. Long Term Care COVID-19 Tracker. Canadian Summary (2021). Available online at: https://ltc-covid19-tracker.ca/ (accessed May 26, 2021).
11. Berkhout E, Galasso N, Lawson M, Morales PAR, Taneja A, Pimentel DAV. The Inequality Virus: Bringing Together A World Torn Apart by Coronavirus Through A Fair, Just and Sustainable Economy. Oxford : Oxfam International (2021).
12. Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. (2021) 4:e2036462. doi: 10.1001/jamanetworkopen.2020.36462
13. Alberti PM, Lantz PM, Wilkins CH. Equitable pandemic preparedness and rapid response: lessons from COVID-19 for pandemic health equity. J Health Politics Policy Law. (2020) 45:921–35. doi: 10.1215/03616878-8641469
14. Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed July 13, 2021).
15. Rangel JC, Ranade S, Sutcliffe P, Mykhalovskiy E, Gastaldo D, Eakin J. COVID-19 policy measures–advocating for the inclusion of the social determinants of health in modelling and decision making. J Eval Clin Pract. (2020) 26:1078–80. doi: 10.1111/jep.13436
16. Khare N, Shroff F, Nkennor B, Mukhopadhyay B. Reimagining safety in a pandemic: the imperative to dismantle structural oppression in Canada. CMAJ. (2020) 192:E1218–20. doi: 10.1503/cmaj.201573
17. Venkataramani AS, O'Brien R, Tsai AC. Declining life expectancy in the United States: the need for social policy as health policy. JAMA. (2021) 325:621–2. doi: 10.1001/jama.2020.26339
18. Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedon JC. On behalf of the Health Equality and Diversity Committee of the American Thoracic Society. The structural and social determinants of the racial/ethnic disparities in the US COVID-19 pandemic: what's our role? Am J Respir Crit Care Med. (2020) 202:943–9. doi: 10.1164/rccm.202005-1523PP
19. Bailey ZD, Feldman JM, Bassett MT. How structural racism works–racist policies as a root cause of US racial health inequities. NEJM. (2021) 384:768–73. doi: 10.1056/NEJMms2025396
20. Andrasfay T, Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. PNAS. (2021) 118:e2014746118. doi: 10.1073/pnas.2014746118
21. Cevik M, Baral SD. Networks of SARS-CoV-2 transmission. Individual and network heterogeneity should inform respiratory pandemic responses. Science. (2021) 373:162–3. doi: 10.1126/science.abg0842
22. Statistics Canada. Deaths and Mortality Rates, by Age Group (2020). Available online at: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=%201310071001 (accessed May 26, 2021).
23. World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update: Situation Reports (2021). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed July 13, 2021)
24. United Nations Department of Economic and Social Affairs Population Division. World Mortality 2019: Data Booklet (ST/ESA/SER.A/436) (2020). Available online at: https://www.un.org/en/development/desa/population/publications/pdf/mortality/WMR2019/WorldMortality2019DataBooklet.pdf (accessed July 13, 2021).
25. Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Road Traffic Injuries and Deaths-A Global Problem (2019). Available online at: https://www.cdc.gov/injury/features/global-road-safety/index.html (accessed July 13, 2021).
26. National Institute on Alcohol Abuse and Alcoholism. Alcohol Facts and Statistics (2021). Available online at: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics (accessed July 13, 2021).
27. World Health Organization. Tobacco (2020). Available online at: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed July 13, 2021).
28. Vohra K, Vodonos A, Schwartz J, Marais EA, Sulprizio MP, Mickley LJ. Global mortality from outdoor fine particle pollution generated by fossil fuel combustion: Results from GEOS-Chem. Environ Res. (2021) 195:110754. doi: 10.1016/j.envres.2021.110754
29. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
30. Chaudhry R, Dranitsaris G, Mubashir T, Bartoszko J, Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine. (2020) 25:100464. doi: 10.1016/j.eclinm.2020.100464
31. Kuhbandner C, Homburg S. Commentary: estimating the effects of nonpharmaceutical interventions on COVID-19 in Europe. Front Med. (2020) 7:580361. doi: 10.3389/fmed.2020.580361
32. Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. (2020) 584:257–61. doi: 10.1038/s41586-020-2405-7
33. Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. (2020) 370:m2743. doi: 10.1136/bmj.m2743
34. Bendavid E, Oh C, Bhattacharya J, Ioannidis JPA. Assessing mandatory stay-at-home and business closure effects on the spread of COVID-19. Eur J Clin Invest. (2021) 51:e13383. doi: 10.1111/eci.13484
35. De Larochelambert Q, Marc A, Antero J, Bourg EL, Toussaint JF. Covid-19 mortality: a matter of vulnerability among nations facing limited margins of adaptation. Front Public Health. (2020) 8:604339. doi: 10.3389/fpubh.2020.604339
36. Savaris RF, Pumi G, Dalzochio J, Kunst R. Stay-at-home policy is a case of exception fallacy: an internet-based ecological study. Sci Rep. (2021) 11:5313. doi: 10.1038/s41598-021-84092-1
37. Leffler CT, Ing E, Lykins JD, Hogan MC, McKeown CA, Grzybowski A. Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks. Am J Trop Med Hyg. (2020) 103:2400–11. doi: 10.4269/ajtmh.20-1015
38. Gibson J. Government mandated lockdowns do not reduce COVID-19 deaths: implications for evaluating the stringent New Zealand response. New Zealand Economic Papers. (2020) 1–12. doi: 10.1080/00779954.2020.1844786
39. Berry CR, Fowler A, Glazer T, Handel-Meyer S, MacMillen A. Evaluating the effects of shelter-in-place policies during the COVID-19 pandemic. PNAS. (2021) 118:e2019706118. doi: 10.1073/pnas.2019706118
40. Homburg S. Effectiveness of Corona lockdowns: evidence for a number of countries. Econst Voice. (2020) 17:20200010. doi: 10.1515/ev-2020-0010
41. Gibson J. Hard, not early: putting the New Zealand Covid-19 response in context. New Zealand Economic Papers. (2020) 1–8. doi: 10.1080/00779954.2020.1842796
42. Krylova M. Do lockdowns make a difference in a pandemic? C2C Journal. (2021). Available online at: https://c2cjournal.ca/2021/03/do-lockdowns-make-a-difference-in-a-pandemic/ (accessed November 6, 2021).
43. Chin V, Ioannidis JPA, Tanner MA, Cripps S. Effect estimates of COVID-19 non-pharmaceutical interventions are non-robust and highly model-dependent. J Clin Epidemiol. (2021) 136:96–132.43. doi: 10.1016/j.jclinepi.2021.03.014
44. Gupta S, Georgiou A, Sen S, Simon K, Karaca-Mandic P. US trends in COVID-19-associated hospitalization and mortality rates before and after reopening economies. JAMA Health Forum. (2021) 2:e211262. doi: 10.1001/jamahealthforum.2021.1262
45. Rannan-Eliya RP, Wijemunige N, Gunawardana JRNA, Amarasinghe SN, Sivagnana I, Fonseka S, et al. Increased intensity of PCR testing reduced COVID-19 transmission within countries during the first pandemic wave. Health Aff. (2021) 40:1. doi: 10.1377/hlthaff.2020.01409
46. Allen DW. Covid lockdown cost/benefits: A critical assessment of the literature. Int J Economics Business. (2021). doi: 10.1080/13571516.2021.1976051. [Epub ahead of print].
47. Colombo M, Mellor J, Colhoun HM, Gomers MGM, McKeigue PM. Trajectory of COVID-19 epidemic in Europe: Arising from S. Flaxman et al. Nature. medRxiv. Available online at: https://doi.org/10.1101/2020.09.26.20202267 (accessed September 28, 2020).
48. Lewis N. Did lockdowns really save 3 million COVID-19 deaths, as Flaxman et al. claim? (2020). Available online at: https://nicholaslewis.org/did-lockdowns-really-save-3-million-covid-19-deaths-as-flaxman-et-al-claim/ (accessed May 26, 2021).
49. Luskin DL. The failed experiment of Covid lockdowns: new data suggest that social distancing and reopening haven't determined the spread. Wall Street J. (2020). Available online at: https://www.wsj.com/articles/the-failed-experiment-of-covid-lockdowns-11599000890 (accessed November 6, 2021).
50. Atkeson A, Kopecky K, Zha T. Four Stylized Facts About COVID19. National Bureau of Economic Research (NBER) Working Paper No 27719 (2020). Available online at: https://econpapers.repec.org/paper/nbrnberwo/27719.htm (accessed May 26, 2021).
51. Wood SN. Did COVID-19 Infections Decline Before UK Lockdown? arXiv (2020). Available online at: https://arxiv.org/abs/2005.02090 (accessed May 26, 2021).
52. Lundberg JO, Zeberg H. Longitudinal Variability in Mortality Predicts Covid-19 Deaths. medRxiv (2020). Available online at: https://www.medrxiv.org/content/10.1101/2020.12.25.20248853v1 (accessed May 26, 2021).
53. Lally M. The Costs and Benefits of COVID-19 Lockdowns in Australia (2021). Available online at: https://clubtroppo.com.au/files/2021/04/THE-COSTS-AND-BENEFITS-OF-A-COVID-LOCKDOWN-6.pdf (accessed May 26, 2021)
54. Bjornskov C. Did Lockdown Work? An Economist's Cross-Country Comparison. SSRN (2020). Available online at: http://dx.doi.org/10.2139/ssrn.3665588 (accessed May 26, 2021).
55. Kepp KP, Bjornskov C. Lockdown Effects on SARS-CoV-2 Transmission–The Evidence From Northern Jutland. medRxiv (2020). Available online at: https://doi.org/10.1101/2020.12.28.20248936 (accessed May 26, 2021).
56. Walach H, Hockertz S. What Association Do Political Interventions, Environmental and Health Variables Have With the Number Of Covid-19 Cases And Deaths? A Linear Modeling Approach. medRxiv (2020). Available online at: https://doi.org/10.1101/2020.06.18.20135012 (accessed May 26, 2021).
57. Meunier T. Full Lockdown Policies in Western Europe Countries Have No Evident Impacts on the Covid-19 Pandemic. medRxiv (2020). Available online at: https://doi.org/10.1101/2020.04.24.20078717 (accessed May 26, 2021)
58. Wieland T. Flatten the Curve! Modeling SARS-CoV-2/COVID-19 Growth in Germany At the county level. medRxiv. (2020). Available online at: https://doi.org/10.1101/2020.05.14.20101667 (accessed May 26, 2021)
59. Agrawal V, Cantor JH, Sood N, Whaley CM. The Impact of the Covid-19 Pandemic and Policy Responses on Excess Mortality. NBER Working Paper No 28930 (2021). Available online at: https://www.nber.org/system/files/working_papers/w28930/w28930.pdf
60. Dehning J, Zierenberg J, Spitzner FP, Wibral M, Neto JP, Wilczek M, et al. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. (2020) 269:eabb9789. doi: 10.1126/science.abb9789
61. Kuhbandner C, Homburg S, Walach H, Hockertz S. Was Germany's Corona lockdown necessary? Advance [Preprint]. (2020). doi: 10.31124/advance.12362645
62. Frijters P. Covid-congestion Effects: Why are Lockdowns So Deadly? Club Troppo. (2021). Available online at: https://clubtroppo.com.au/2021/02/03/covid-congestion-effects-why-are-lockdowns-so-deadly/ (accessed May 26, 2021).
63. Kulldorff M, Gupta S, Bhattacharya J. Great Barrington Declaration. Frequently Asked Questions (2020). Available online at: https://gbdeclaration.org/frequently-asked-questions/ (accessed October 26, 2021).
64. Kulldorff M, Gupta S, Bhattacharya J. We Should Focus on Protecting the Vulnerable From COVID Infection. Opinion. Newsweek (2020). Available online at: https://www.newsweek.com/we-should-focus-protecting-vulnerable-covid-infection-opinion-1543225 (accessed October 26, 2021).
65. Badr HS, Bardner LM. Limitations of using mobile phone data to model COVID-19 transmission in the USA. Lancet. (2021) 21:e113. doi: 10.1016/S1473-3099(20)30861-6
66. Gatalo O, Tseng K, Hamilton A, Lin G, Klein E, CDC MInD-Healthcare Program. Associations between phone mobility data and COVID-19 cases. Lancet. (2021) 21:e111. doi: 10.1016/S1473-3099(20)30725-8
67. Alwan NA, Burgess RA, Ashworth S, Beale R, Bhadelia N, Bogaert D, et al. Scientific consensus on the COVID-19 pandemic: we need to act now. Lancet. (2020) 396:e71–2. doi: 10.1016/S0140-6736(20)32153-X
68. Pachetti M, Marini B, Giudici F, Benedetti F, Angeletti S, Ciccozzi M, et al. Impact of lockdown on Covid-19 case fatality rate and viral mutations spread in 7 countries in Europe and North America. J Transl Med. (2020) 18:338. doi: 10.1186/s12967-020-02501-x
69. Haug N, Geyrhofer L, Londei A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. (2020) 4:1303–12. doi: 10.1038/s41562-020-01009-0
70. Liu Y, Morgenstern C, Kelly J, Lowe R, CCMID COVID-19 Working Group, Jit M. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. (2021) 19:40. doi: 10.1186/s12916-020-01872-8
71. Brauner JM, Mindermann S, Sharma M, Johnston D, Salvatier J, Gavenciak T, et al. Inferring the effectiveness of government interventions against COVID-19. Science. (2021) 371:eabd9338. doi: 10.1126/science.abd9338
72. Inglesby TV, Nuzzo JB, O'Toole T, Henderson DA. Disease mitigation measures in the control of pandemic influenza. Biosecur Bioterror. (2006) 4:366–75. doi: 10.1089/bsp.2006.4.366
73. Aledort JE, Lurie N, Wasserman J, Bozzette SA. Non-pharmaceutical public health interventions for pandemic influenza: an evaluation of the evidence base. BMC Public Health. (2007) 7:208. doi: 10.1186/1471-2458-7-208
74. World Health Organization Writing Group. Nonpharmaceutical interventions for pandemic Influenza, national and community measures. Emerg Infect Dis. (2006) 12:88–94. doi: 10.3201/eid1201.051370
75. World Health Organization. Non-pharmaceutical Public Health Measures For Mitigating the Risk and Impact of Epidemic and Pandemic Influenza. Licence: CC BY-NC-SA 3.0 IGO. (2019). Available online at: https://apps.who.int/iris/bitstream/handle/10665/329438/9789241516839-eng.pdf?ua=1 (accessed May 26, 2021).
76. Justice Center for Constitutional Freedoms. Flying Blind: Government's Hasty Decisions to Lock Down Canadians While Damaging Public Health and the Economy (2020). Available online at: https://www.jccf.ca/published_reports/flying-blind-governments-hasty-decisions-to-lock-down-canadians-while-damaging-public-health-and-the-economy/ (accessed May 26, 2021).
77. Joffe AR. COVID-19: rethinking the lockdown groupthink. Front Public Health. (2021) 9:625778. doi: 10.3389/fpubh.2021.625778
78. Joffe AR. Rethinking Lockdowns: The Risks and Trade-Offs of Public Health Measures to Prevent COVID-19 Infections. Macdonald Laurier Institute (2020). Available online at: https://macdonaldlaurier.ca/files/pdf/20201209_Rethinking_lockdowns_Joffe_COMMENTARY_FWeb.pdf (accessed May 26, 2021).
79. Miles D, Stedman M, Heald A. Living with Covid-19: balancing costs against benefits in the face of the virus. Natl Inst Econ Rev. (2020) 253:R60–76. doi: 10.1017/nie.2020.30
80. Schippers MC. For the greater good? the devastating ripple effects of the Covid-19 crisis. Front Psychol. (2020) 11:577740. doi: 10.3389/fpsyg.2020.577740
81. Rangel JC. A way forward: Considering the sustainability, equity and unintended effects of social control measures as a response to the COVID-19 crisis. J Eval Clin Pract. (2021) 27:3–8. doi: 10.1111/jep.13508
82. Cervantes PAM, Lopez NR, Rambaud SC. The relative importance of globalization and public expenditure on life expectancy in Europe: An approach based on MARS methodology. Int J Environ Res Public Health. (2020) 17:8614. doi: 10.3390/ijerph17228614
83. Frijters P. Has the Coronavirus Panic Cost Us at Least 10 Million Lives Already? Club Troppo (2020). Available online at: https://clubtroppo.com.au/2020/03/18/has-the-coronavirus-panic-cost-us-at-least-10-million-lives-already/ (accessed July 13, 2021).
84. Snyder-Mackler N, Burger JR, Gaydosh L, Belsky DW, Noppert GA, Campos FA, et al. Social determinants of health and survival in humans and other animals. Science. (2020) 368:eaax9553. doi: 10.1126/science.aax9553
85. Frijters P. On Corona/Covid-19, Herd Immunity, and WELLBY Tradeoffs - Key Predictions and Numbers. Club Troppo (2020). Available online at: https://clubtroppo.com.au/2020/05/14/on-corona-covid-19-herd-immunity-and-wellby-tradeoffs-key-predictions-and-numbers/ (accessed July 13, 2021).
86. Frijters P, Clark AE, Krekel C, Layard R. A happy choice: wellbeing as the goal of government. Behav Public Policy. (2020) 4:126–65. doi: 10.1017/bpp.2019.39
87. Frijters P, Krekel C. Chapter 1: The case for wellbeing as the goal of government in the context of constraints on policy-making. In: Frijters P, Krekel C, editors. A Handbook for Wellbeing Policy-Making: History, Theory, Measurement, Implementation, and Examples. London: Oxford University Press (2021).
88. Foster G. Cost-Benefit Analysis Executive Summary. Presented to Victorian Parliament in Australia (2020). Available online at: https://parliament.vic.gov.au/images/stories/committees/paec/COVID-19_Inquiry/Tabled_Documents_Round_2/CBA_Covid_Gigi_Foster.pdf (accessed July 13, 2021).
89. Lally M. The Costs and Benefits of COVID-19 Lockdowns. Capital Financial Consultants (2020). Available online at: https://nzfc.ac.nz/papers/updated/53.pdf (accessed July 13, 2021).
90. Christakis DA, Cleve WV, Zimmerman FJ. Estimation of US children's educational attainment and years of life lost associated with primary school closures during the Coronavirus Disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2028786. doi: 10.1001/jamanetworkopen.2020.28786
91. Rowthorn R, Maciejowski J. A cost-benefit analysis of the COVID-19 disease. Oxford Review Economic Policy. (2020) 36(Suppl1):S38–S55. doi: 10.1093/oxrep/graa030
92. Ryan A. A Cost–Benefit Analysis of the COVID-19 Lockdown in Ireland. SSRN [Preprint]. (2021). doi: 10.2139/ssrn.3872861
93. Ekenberg L, Mihai A, Fasth T, Komendantova N, Danielson M. A multi-criteria framework for pandemic response measures. Front Public Health. (2021) 9:583706. doi: 10.3389/fpubh.2021.583706
94. Chief Public Health Officer of Canada. Report on the State of Public Health in Canada 2020. From Risk to Resilience: An Equity Approach to COVID-19. Ottawa: Public Health Agency of Canada (2020). Available online at: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html (accessed May 26, 2021).
95. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open. (2021) 4:e2111417. doi: 10.1001/jamanetworkopen.2021.11417
96. Sudre CH, Murray B, Varsavsky T, Graham MS, Penforld RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nature Med. (2021) 27:626–31. doi: 10.1038/s41591-021-01292-y
97. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. (2021) 27:601–15. doi: 10.1038/s41591-021-01283-z
98. Office for National Statistics. Technical article: Updated Estimates of the Prevalence of Post-Acute Symptoms Among People With Coronavirus (COVID-19) in the UK: 26 April 2020 to 1 August 2021 (2021). Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/technicalarticleupdatedestimatesoftheprevalenceofpostacutesymptomsamongpeoplewithcoronaviruscovid19intheuk/26april2020to1august2021 (accessed October 26, 2021).
99. Payne AB, Gilani Z, Godfred-Cato S, Belay ED, Feldstein LR, Patel MM, et al. Incidence of multisystem inflammatory syndrome in children among US persons infected with SARS-CoV-2. JAMA Netw Open. (2021) 4:e2116420. doi: 10.1001/jamanetworkopen.2021.16420
100. Molteni E, Sudre CH, Canas LS, Bhopal SS, Hughes RC, Antonelli M, et al. Illness Duration and Symptom Profile in a Large Cohort of Symptomatic UK School-Aged Children Tested For Sars-Cov-2. medRxiv (2021). Available online at: https://www.medrxiv.org/content/10.1101/2021.05.05.21256649v2 (accessed July 13, 2021).
101. Say D, Crawford N, McNab S, Wurzel D, Steer A, Tosif S. Post-acute COVID-19 outcomes in children with mild and asymptomatic disease. Lancet Child Adolesc Health. (2021) 5:e22–3. doi: 10.1016/S2352-4642(21)00124-3
102. Radtke T, Ulyte A, Puhan MA, Kriemler S. Long-Term Symptoms After SARS-CoV-2 Infection in School Children: Population-Based Cohort With 6-Months Follow-Up. medRxiv. (2021). Available online at: https://doi.org/10.1101/2021.05.16.21257255 (accessed July 13, 2021)
103. Buonsenso D, Munblit D, De Rose C, Sinatti D, Ricchiuto A, Carfi A, et al. Preliminary evidence on long COVID in children. Acta Paediatr. (2021) 110:2208–11. doi: 10.1111/apa.15870
104. Czeisler ME, Lane RI, Wiley JF, Czeisler CA, Howard ME, Rajaratnam SMW. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Netw Open. (2021) 4:e2037665. doi: 10.1001/jamanetworkopen.2020.37665
105. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. (2021) 16:57. doi: 10.1186/s12992-020-00589-w
106. Bagus P, Pena-Ramos JA, Sanchez-Bayon A. COVID-19 and the political economy of mass hysteria. Int J Environ Res Public Health. (2021) 18:1376. doi: 10.3390/ijerph18041376
107. Ioannidis JPA, Cripps S, Tanner MA. Forecasting for COVID-19 has failed. Int J Forecast. (2021). doi: 10.1016/j.ijforecast.2020.08.004. [Epub ahead of print].
108. Kavaliunas A, Ocaya P, Mumper J, Lindfeldt I, Kyhlstedt M. Swedish policy analysis for Covid-19. Health Policy Technol. (2020) 9:598–612. doi: 10.1016/j.hlpt.2020.08.009
109. Baker MA, Fiumara K, Rhee C, Williams SA, Tucker R, Wickner P, et al. Low risk of coronavirus disease 2019 (COVID-19) among patients exposed to infected healthcare workers. Clin Infect Dis. (2020) 73:e1878–e1880. doi: 10.1093/cid/ciaa1269
110. Bayham J, Fenichel EP. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Public Health. (2020) 5:E271–8. doi: 10.1016/S2468-2667(20)30082-7
111. Davies NG, Abbott S, Barnard RC, Jarvis CI, Kucharski AJ, Munday JD, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. (2021) 372:eabg3055. doi: 10.1126/science.abg3055
112. Ellis D, Papadopoulos D, Mukherjee S, Ukwu U, Chari N, Charitopoulos K, et al. The Course of the UK COVID-19 Pandemic; No Measurable Impact of New Variants. medRxiv (2021). Available online at: https://www.medrxiv.org/content/10.1101/2021.03.16.21253534v1 (accessed November 6, 2021).
113. Davies NG, Jarvis CI, CCMID COVID-19 Working Group, Edmunds WJ, Jewell NP, Diza-Ordaz K, et al. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. (2021) 593:270–4. doi: 10.1101/2021.02.01.21250959
114. Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. (2021) 372:n579. doi: 10.1136/bmj.n579
115. Atkeson A. A Parsimonious Behavioral SEIR Model of the 2020 COVID Epidemic in the United States and the United Kingdom. NBER Working Paper Series (2021). Available online at: http://222.nber.org/papers/w28434 (accessed May 26, 2021).
116. Frampton D, Rampling T, Cross A, Bailey H, Heaney J, Byott M, et al. Genomic characteristics and clinical effect of the emergent SARS-CoV-2 B.1.1.7 lineage in London, UK: a whole-genome sequencing and hospital-based cohort study. Lancet Infect Dis. (2021) 21:P1246–56. doi: 10.1016/S1473-3099(21)00170-5
117. Thakur R. India's Coronavirus Emergency Tells A Story Poorly Understood. Pearls and Irritations (2021). Available online at: https://johnmenadue.com/indias-coronavirus-emergency-tells-a-story-poorly-understood/ (accessed July 13, 2021).
118. Stowe J, Andrews N, Gower C, Gallagher E, Utsi L, Simmons R, et al. Effectiveness of COVID-19 vaccines against hospital admission with the Delta (B.1.617.2) variant. London: Public Health England (2021). Available online at: https://media.tghn.org/articles/Effectiveness_of_COVID-19_vaccines_against_hospital_admission_with_the_Delta_B._G6gnnqJ.pdf (accessed July 13, 2021).
119. Callaway E. Pfizer COVID vaccine protects against worrying Coronavirus variants. Nature. (2021) 593:325–6. doi: 10.1038/d41586-021-01222-5
120. Altmann DM, Boyton RJ, Beale R. Immunity to SARS-CoV-2 variants of concern. Science. (2021) 593:325–6. doi: 10.1126/science.abg7404
121. Schippers MC, Rus DC. Optimizing decision-making processes in times of COVID-19: Using reflexivity to counteract information-processing failures. Front Psychol. (2021) 12:650525. doi: 10.3389/fpsyg.2021.650525
122. Sebhatu A, Wennberg K, Arora-Jonsson S, Lindberg SI. Explaining the homogeneous diffusion of COVID-19 nonpharmaceutical interventions across heterogeneous countries. PNAS. (2020) 117:21201–8. doi: 10.1073/pnas.2010625117
123. Frijters P. What Kind of Crowd Are We Now Seeing? The 5 Surprises in This Pandemic. Club Troppo (2020). Available online at: What_kind_of_crowd_are_we_now_seeing?_The_5_surprises_in_this_pandemic._|_ClubTroppo (accessed May 26, 2021).
124. Murray DR, Schaller M, Suedfeld P. Pathogens and politics: further evidence that parasite prevalence predicts authoritarianism. PLoS ONE. (2013) 8:e62275. doi: 10.1371/journal.pone.0062275
125. Thakur R. Covid and Culture Cringe: Data Tell us All We Need to Know About Tackling the Virus. Features Australia (2020). Available online at: https://www.spectator.com.au/2020/11/covid-and-culture-cringe/ (accessed May 26, 2021).
126. Statistics Canada. Number of vehicles travelling between Canada and the United States. Available online at: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=2410000201 (accessed July 13, 2021).
127. Scally G, Gupta S. The duel: Is eliminating Covid-19 worth it? Prospect Magazine (2021). Available online at: https://www.prospectmagazine.co.uk/the-duel/duel-eliminating-covid-19-lockdowns-gabriel-scally-sunetra-gupta (accessed May 26, 2021).
128. BBC News. Covid: Sydney Lockdown Extended as Delta Outbreak Spreads (2021). Available online at: https://www.bbc.com/news/world-australia-57744902 (accessed July 13, 2021).
129. Dole N, Hemingway P. The Delta Coronavirus Variant May Be Spreading, But High Vaccination Rates Mean Israelis Stay Free. ABC News (2021). Available online at: https://www.abc.net.au/news/2021-07-03/delta-spreading-in-israel-but-vaccines-prevent-serious-cases/100249416 (accessed July 13, 2021).
130. Redman D. Due Diligence: Canadian Charter of Rights and Freedoms vs “Lockdowns”. Frontier Centre for Public Policy (2021). Available online at: https://fcpp.org/wp-content/uploads/FC-PS235_Lockdown_MA1821_F2.pdf (accessed May 26, 2021).
131. Ministers Responsible for Emergency Management. An Emergency Management Framework for Canada, 3rd Edition. Public Safety Canada: Ottawa, ON (2017). Available online at: https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2017-mrgnc-mngmnt-frmwrk/index-en.aspx (accessed May 26, 2021).
132. Redman D. An Emergency Management Doctrine. Preprints (2021). Available online at: https://doi.org/10.20944/preprints202102.0367.v1 (accessed May 26, 2021)
133. Alberta Government. Alberta's Pandemic Influenza Plan. Alberta Government: Edmonton, AB (2014). Available online at: https://open.alberta.ca/dataset/c89245b6-a7fc-4c24-be87-c2686341ffb5/resource/a652811e-42f2-4c0d-90af-54e0e759e05e/download/2014-albertas-pandemic-influenza-plan-apip-march-2014.pdf (accessed May 26, 2021).
134. Ioannidis JPA. Precision shielding for COVID-19: metrics of assessment and feasibility of deployment. BMJ Global Health. (2021) 6:e004614. doi: 10.1136/bmjgh-2020-004614
135. APM Research Lab Staff. The color of Coronavirus: COVID-19 deaths by race and ethnicity in the U.S. (2021). Available online at: https://www.apmresearchlab.org/covid/deaths-by-race (accessed July 13, 2021).
136. Kulldorff M, Gupta S, Bhattacharya J. Great Barrington Declaration. Focused Protection (2020). Available online at: https://gbdeclaration.org/focused-protection/ (accessed October 26, 2021).
137. Bark D, Dhillo N, St-Jean M, Kinniburgh B, McKee G, Choi A. SARS-CoV-2 transmission in kindergarten to grade 12 schools in the Vancouver Coastal Health region: a descriptive epidemiologic study. CMAJ Open. (2021) 9:E810–7. doi: 10.9778/cmajo.20210106
138. Fenton L, Gribben C, Caldwell D, Colville S, Bishop J, Reid M, et al. Risk of Hospitalization With COVID-19 Among Teachers Compared to Healthcare Workers and Other Working-Age Adults: A Nationwide Case-Control Study. medRxiv (2021). Available online at: https://www.medrxiv.org/content/10.1101/2021.02.05.21251189v1 (accessed May 26, 2021).
139. Somekh I, Boker LK, Shohat T, Pettoello-Mantovani M, Simoes EF, Somekh E. Comparison of COVID-19 incidence rates before and after school reopening in Israel. JAMA Netw Open. (2021) 4:e217105. doi: 10.1001/jamanetworkopen.2021.7105
140. Gandini S, Rainisio M, Iannuzzo ML, Bellerba F, Cecconi F, Scorrano L, et al. cross-sectional and prospective cohort study of the role of schools in the SARS-CoV-2 second wave in Italy. Lancet Regional Health–Europe. (2021) 5:100092. doi: 10.1016/j.lanepe.2021.100092
141. Ciaranello A, Bell T. Using data and modeling to understand the risks of in-person education. JAMA Netw Open. (2021) 4:e214619. doi: 10.1001/jamanetworkopen.2021.4619
142. Rayner G. Use of Fear to Control Behavior In Covid Crisis Was ‘Totalitarian’, Admit Scientists. The Telegraph (2021). Available online at: https://www.telegraph.co.uk/news/2021/05/14/scientists-admit-totalitarian-use-fear-control-behaviour-covid/ (accessed July 13, 2021).
143. Sidley G. A year of Fear. The Critic (2021). Available online at: https://thecritic.co.uk/a-year-of-fear/ (accessed July 13, 2021).
144. Bhopal R, Munro APS. Scholarly communications harmed by covid-19. BMJ. (2021) 372:n742. doi: 10.1136/bmj.n742
145. Ioannidis JPA. How the Pandemic is Changing the Norms of Science. Tablet Magazine (2021). Available online at: https://www.tabletmag.com/sections/science/articles/pandemic-science (accessed October 26, 2021).
146. Kulldorff M. Covid, Lockdown and the Retreat of Scientific Debate. The Spectator (2021). Available online at: https://www.spectator.co.uk/article/covid-lockdown-and-the-retreat-of-scientific-debate (accessed October 26, 2021).
147. Blastland M, Freeman ALJ, van der Linden S, Marteau TM, Spiegelhalter D. Five rules for evidence communication. Nature. (2020) 587:362–4. doi: 10.1038/d41586-020-03189-1
148. Sandman PM, Lanard J. COVID-19: The CIDRAP (Center for Infectious Disease Research and Policy, University of Minnesota) Viewpoint. Part 2: Effective COVID-19 Crisis Communication (2020). Available online at: https://www.cidrap.umn.edu/sites/default/files/public/downloads/cidrap-covid19-viewpoint-part2.pdf (accessed May 26, 2021).
149. de Jong EM, Ziegler N, Schippers MC. From shattered goals to meaning in life: Life crafting in times of the COVID-19 pandemic. Front Psychol. (2020) 11:577708. doi: 10.3389/fpsyg.2020.577708
150. Freyhofer S, Ziegler N, de Jong E, Schippers MC. Loneliness, depression, and anxiety in times of COVID-19: How coping strategies and loneliness relate to mental health outcomes and academic performance. Front Psychol. (2021) 12:682684. doi: 10.3389/fpsyg.2021.682684
Keywords: COVID-19, emergency management (EM), lockdowns, pandemic, response
Citation: Joffe AR and Redman D (2021) The SARS-CoV-2 Pandemic in High Income Countries Such as Canada: A Better Way Forward Without Lockdowns. Front. Public Health 9:715904. doi: 10.3389/fpubh.2021.715904
Received: 27 May 2021; Accepted: 29 October 2021;
Published: 22 November 2021.
Edited by:
Marisa Gilles, Western Australian Center for Rural Health (WACRH), AustraliaReviewed by:
Charles Greenfield, Western Australia Country Health Service (WACHS), AustraliaCopyright © 2021 Joffe and Redman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ari R. Joffe, YWpvZmZlQHVhbGJlcnRhLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.