
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Public Health , 27 September 2021
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.708903
Objectives: According to the World Health Organization (WHO), an early and consistent international and national response is needed to control a pandemic's spread. In this analysis, we evaluate the coordination of Canada's early response to the coronavirus (COVID-19) pandemic in terms of public health interventions and policies implemented in each province and territory.
Methods: Retrospective data was obtained from publicly accessible websites maintained by federal, provincial and territorial governmental agencies. Consistent with WHO's spreading of the disease pandemic action, individual and community-based public health interventions and policies were the focus. Time of intervention or policy, and COVID-19 cases per million at time of intervention was recorded for each province and territory.
Results: Most public health interventions and policies demonstrated wide time ranges of implementation across individual provinces and territories. At time of implementation, there were also wide variations in the number of positive COVID-19 cases in these jurisdictions. Cases per million per implemented day were also not similar across interventions or policy, suggesting that other factors may have been preferentially considered.
Conclusions: Whether an earlier and more structured national approach would have lessened the pandemic's burden is uncertain, calls for greater federal coordination and leadership should to examined.
The World Health Organization (WHO) was first made aware of a “viral pneumonia” occurring in Wuhan, China, on December 31st, 2019. Rapidly, the novel coronavirus spread outside of the Chinese borders, and by January 30th, it received the WHO's highest level of alarm (1). By March 2020, COronaVIrus Disease 2019 (COVID-19) was declared a global pandemic, and by April 2020, there were over one million cases confirmed across the world (1).
The need for an early and structured public health intervention plan to limit COVID-19's progression became paramount. In retrospect, the resounding cornerstone of the WHO's pandemic preparedness and response became leadership and coordinated actions at the global and national level (2). In Canada, its federal response initially focused on screening and isolating international travelers at risk (3). However, as the number of cases throughout the country increased, the federal and provincial responses shifted toward a more complete public health approach. The federal government expanded its actions to travel restrictions, control of borders as well as issuing public health guidance (4) while the provincial responses were focused on case management and isolation, limitation of gatherings, health workforce reassignment and closure of certain communities and non-essential businesses.
Some concerns were raised after the first wave of the COVID-19 pandemic in regards to differences between provincial interventions. In Canada, the public healthcare system is largely decentralized, as the primary responsibilities are shouldered provincially and territorially (5). However, the “Federal/Provincial/Territorial (F/P/T) Public Health Response Plan for Biological Events,” outlines that “the key objective of this plan is improving effective engagement amongst public health, health care delivery and health emergency management authorities during a coordinated F/P/T response” (6).
In our perspective, we reviewed Canada's early response to the COVID-19 pandemic in terms of public health policies and interventions. More specifically, we examined how implementation differed across provinces and if Canada met its objective of having an “overarching, consistent and coordinated plan” across the country (6).
Canada's early response was defined from the first case reported on January 25th, 2020 (7) to the end of April 2020. The 3-month time interval captured the most restrictive public health policy measures and pandemic interventions for the majority of provinces and territories, just before the spring lockdown was gradually reopened.
Time of intervention or policy, and COVID-19 cases per million at time of policy/intervention was recorded for each province and territory. Day #0 for each policy/intervention was considered when the first province implemented it. Consistent with WHO's reducing the spread of disease preparedness (2) during a pandemic, and individual and community-based public health interventions and policies were the focus. Mortality data was not captured, as death rates remained very low during the early response.
Data on daily numbers of COVID-19 cases for each province were collected from the Government of Canada's public access epidemiological tool (7). We collected data from January 25th 2020, which is when the first Canadian COVID-19 case was reported, to the end of April 2020, which is when most provinces adopted their early pandemic response interventions. If some provinces adopted their interventions later than April 2020, we expanded our data collection to those specific dates.
Data for public health interventions and policies as well as their date of implementation were extracted from provincial or territorial websites, which included the Governments of British Columbia (8), Alberta (9), Saskatchewan (10), Manitoba (11), Ontario (12), Quebec (13), New Brunswick (14), Nova Scotia (15), Prince Edward Island (16), Newfoundland and Labrador (17), Yukon (18), Northwest Territories (19), and Nunavut (20).
Continuous variables were summarized as means and standard deviations. We used Pearson's correlation to measure the correlation between the days of intervention and the number of COVID-19 cases. The days of intervention and the number of COVID-19 cases were created by taking the averages of corresponding values from the provinces. Statistical analyses were done using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
The provincial and territorial public health interventions are summarized in Table 1 and Figure 1 by date of implementation. Thirteen public health interventions (57%) out of the 24 analyzed were implemented by all provinces and territories across Canada. Most public health interventions showed wide implementation date ranges across provinces with large standard deviations. For example, declaring public health emergencies was adopted by all jurisdiction within a 10 day period, and had a standard deviation of 2.30 days. Restricting provincial border restrictions however, was only adopted by 46% (n = 6) provinces and/or territories, and had an implementation date range of 55 days and a standard deviation of 22 days.
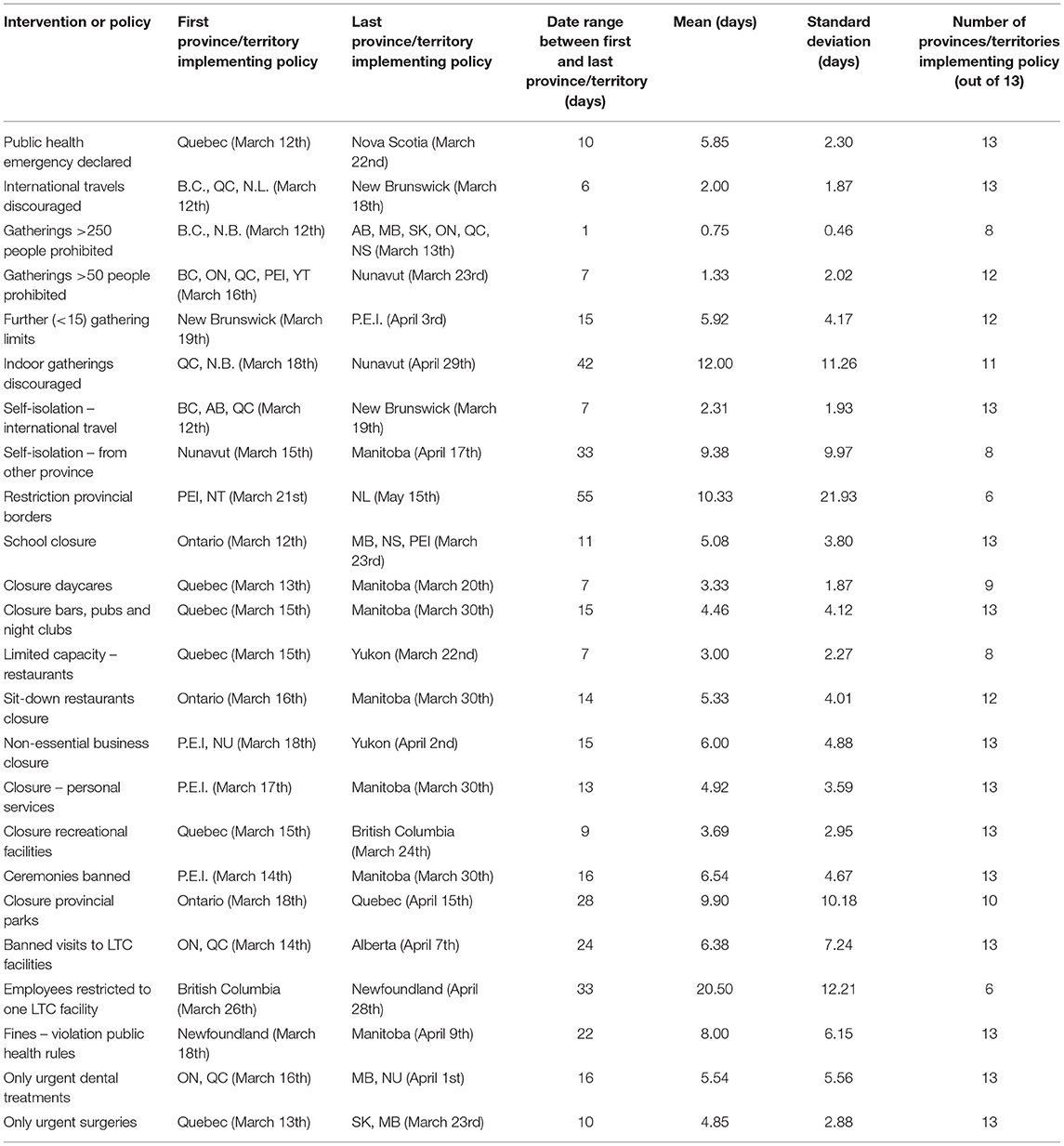
Table 1. Public health interventions during the early COVID-19 pandemic analyzed by date of implementation.
Public health interventions based on the number of cases per millions are summarized in Table 2. For most interventions, there were wide standard deviations demonstrating heterogeneity in the number of cases when provinces or territories adopted each public health intervention. Restricting gatherings of >250 people was implemented with 3.88 mean provincial cases per million, whereas restricting employees to one long term facility was implemented with 335.85 mean provincial cases per million.
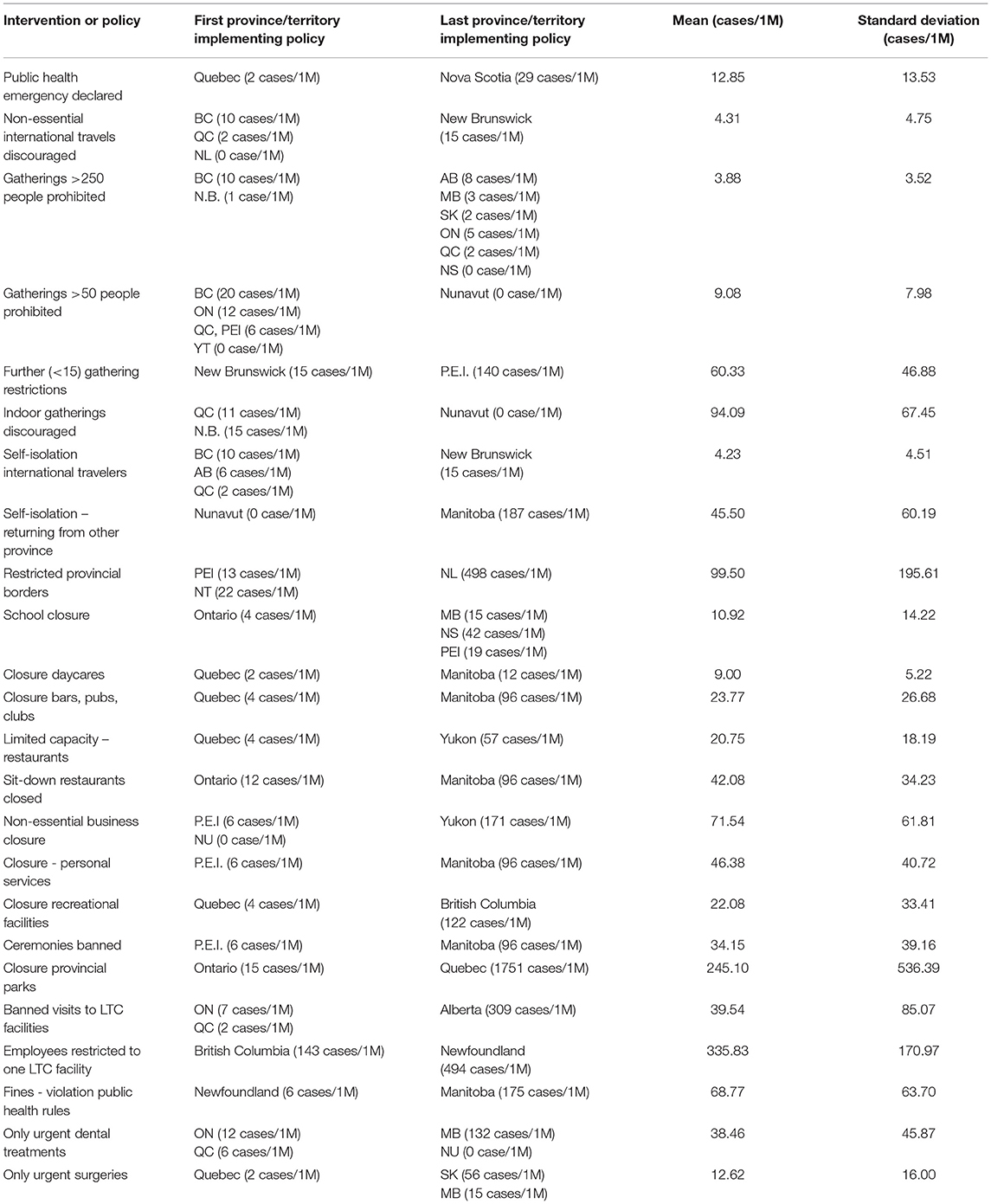
Table 2. Public health interventions during the early COVID-19 pandemic analyzed by cases per province or territory at the time of implementation.
The correlation between mean days of intervention and the number of COVID-19 cases was positive and significant (rho = 0.89; p < 0.0001). However, cases per million per implemented day was not similar across intervention or policy. For example, closure of parks, restricting long term care facility employees and restricted travel had much higher cases than other policies (Figure 2).
Provincial and territorial public health interventions adopted during the early COVID-19 pandemic response showed a large amount of heterogeneity in terms of their implementation timeline across Canada. In fact, 43% of the interventions were not adopted by all. Furthermore, their implementation did not appear to be consistent with the number of positive COVID-19 cases, suggesting other factors may have been considered.
Earlier interventions such as the declaration of a public health emergency and discouraging international travel were widely adopted by all provinces and territories and within a short period of time. However, considering the effectiveness of physical distancing measures to reduce overall community transmission (3, 21) only eight provinces adopted policies limiting gatherings to <250 people. Other establishment closures such as bars, restaurants, non-essential businesses and personal services also demonstrated large variations, despite the utility of physical distancing measures at “mixed-aged venues” (3). Surprisingly, interventions for long term care facilities showed the highest variability, despite the impact of direct measures targeted at reducing COVID-19 transmission to older citizens (3, 22). Only six provinces or territories restricted employees to work in different long-term care facilities in order to limit the spread between them. British Columbia's early approach was the most stringent, and banned visits to long-term care facilities, restricted movements of employees and made masks obligatory (23). Together, the data suggests that provincial and territorial public health policies were not implemented in a coordinated and dependent fashion.
An uncoordinated national approach is important to consider, as half of the provinces/territories did not restrict their borders to domestic travelers including between the most affected and highly populated regions. Newfoundland and Labrador closed their provincial borders early, and through modeling demonstrated how easy an infected traveler can be the cause of new exponential outbreak by solely relaxing travel bans (24). In contrast, the first human-to-human COVID-19 transmission was confirmed in Wuhan, China, on January 20th 2020 (25). Three days later, major non-pharmaceutical interventions were adopted across the country including intercity travel restrictions (26). Based on an epidemiological model, the travel restrictions did “prevent cases being exported from Wuhan to a wider area” (26) and had they been implemented earlier, the outbreak would have been controlled even further. Although a discussion of Wuhan's response vs. Western liberties is beyond the scope of this study, it nevertheless demonstrates the effectiveness of an attentive and coordinated border strategy.
Decisions to implement provincial and territorial public health interventions did not appear to be based on the number of their COVID-19 cases. Escalation of responses that included closure of schools, non-essential businesses and services occurred over a wide range of provincial/territorial positive cases and calendar days. When we considered cases per million per implemented day closure of parks, restricting long term care facility employees and restricting travel were far higher than other policies, suggesting they should have been implemented sooner. In contrast, territories like Nunavut adopted the majority of public health interventions implemented by other provinces with escalating cases, despite not having a positive case documented. Other countries were also reactive during the early COVID-19 pandemic, but implemented national public health interventions uniformly as initial cases were detected within their borders (27). Some jurisdictions were more proactive. Hong Kong, for example, restricted travelers coming from Wuhan, screened returning travelers, and limited travel even before their first case was confirmed (28). With those proactive interventions, Hong Kong was able to contain COVID-19 spread despite its proximity with Wuhan, while avoiding more extreme interventions like complete lockdown (28).
Our findings suggest that Canada's F/P/T Public Health Response Plan for Biological Events did not result in a coordinated and consistent national response.
In March, 2020, reporters commented that Canada did not learn from key lessons after SARS, with its patchwork system of basic information and sparse details on coronavirus communications (29). During the second wave, some provincial leaders were asking for a “pan-Canadian approach to travel” (30) while infectious disease specialists were calling for an “aggressive national strategy” (31). While the consequences of Canada's decentralized approach in regards to morbidity, mortality and economic loss remains uncertain, the degree of scrutiny from well-intentioned medical experts and politicians should compel a thorough review of the Response Plan and the degree of Federal coordination and involvement.
There are at least two limitations that should be addressed. First, public health decisions are based on complicated processes that must consider a plethora of information, factors, and opinions. To suggest otherwise was not our intension, but rather to examine how coordinated the decisions were. The second limitation is more philosophic in nature, as the noted decentralized approach has been suggested to enable provinces and territories to innovate and mobilize quickly. However, elsewhere we have shown the opposite (27) and that the decentralized uncoordinated approach has actually resulted in suboptimal testing, mobilization of the health care system and disease containment.
The World Health Organization has advocated for early coordinated responses during pandemics. In Canada, many provincial and territorial public health interventions were implemented across wide time ranges. Cases per million per implemented day were also not similar, suggesting that other factors may have been preferentially considered for interventions or policies. Whether an earlier and more structured national approach would have lessened the pandemic's burden is uncertain, calls for greater federal coordination and leadership should to examined.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
AC and GH developed the central idea of the study. PM provided statistical support. All authors wrote, revised, and approved the final manuscript as submitted.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization. Timeline: WHO's COVID-19 Response. (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline/#event-73 (accessed May 2, 2021).
2. World Health Organization. Pandemic Influenza Preparedness and Response: Phases 5-6 Pandemic. (2009). Available online at: https://www.who.int/influenza/resources/documents/extract_PIPGuidance09_phase5_6.pdf?ua=1 (accessed May 3, 2021).
3. Ng V, Fazil A, Waddell LA, Bancej C, Turgeon P, Otten A, et al. Projected effects of nonpharmaceutical public health interventions to prevent resurgence of SARS-CoV-2 transmission in Canada. CMAJ. (2020) 192:e1053–64. doi: 10.1503/cmaj.200990
4. Government of Canada. Government of Canada Takes Action on COVID-19. (2020). Available online at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/canadas-reponse/government-canada-takes-action-covid-19.html (accessed May 3, 2021).
5. Armstrong P, Armstrong H. Decentralised health care in Canada. BMJ. (1999) 318:1201–4. doi: 10.1136/bmj.318.7192.1201
6. Government of Canada. Federal/Provincial/Territorial Public Health Response Plan for Biological Events. (2017). Available online at: https://www.canada.ca/en/public-health/services/emergency-preparedness/public-health-response-plan-biological-events.html#s2-4 (accessed May 4, 2021).
7. Government of Canada. Coronavirus Disease 2019 (COVID-19): Epidemiological Update. (2021). Available online at: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed April 6, 2021).
8. Government of British Columbia. B.C.'s Response to COVID-19. (2021). Available online at: https://www2.gov.bc.ca/gov/content/safety/emergency-preparedness-response-recovery/covid-19-provincial-support (accessed April 8, 2021).
9. Government of Alberta. COVID-19 Info for Albertans. (2021). Available online at: https://www.alberta.ca/coronavirus-info-for-albertans.aspx (accessed April 9, 2021).
10. Government of Saskatchewan. COVID-19. (2021). Available online at: https://www.saskatchewan.ca/government/health-care-administration-and-provider-resources/treatment-procedures-and-guidelines/emerging-public-health-issues/2019-novel-coronavirus (accessed April 9, 2021).
11. Government of Manitoba. COVID-19. (2021). Available online at: https://www.gov.mb.ca/covid19/index.html (accessed April 9, 2021).
12. Government of Ontario. How Ontario is Responding to COVID-19. (2021). Available online at: https://www.ontario.ca/page/how-ontario-is-responding-covid-19 (accessed April 9, 2021).
13. Government of Quebec. Coronavirus Disease (COVID-19) in Quebec. (2021). Available online at: https://www.quebec.ca/en/health/health-issues/a-z/2019-coronavirus/ (accessed April 10, 2021).
14. Government of New Brunswick. Coronavirus Disease (COVID-19). (2021). Available online at: https://www2.gnb.ca/content/gnb/en/corporate/promo/covid-19.html (accessed April 10, 2021).
15. Government of Nova Scotia. Coronavirus (COVID-19): Government's Response to COVID-19. (2021). Available online at: https://novascotia.ca/coronavirus/ (accessed April 12, 2021).
16. Government of Prince Edward Island. COVID-19 (Coronavirus) in Prince Edward Island. (2021). Available online at: https://www.princeedwardisland.ca/en/covid19 (accessed April 12, 2021).
17. Government of Newfound and Labrador. NLife with COVID-19. (2021). Available online at: https://www.gov.nl.ca/covid-19/ (accessed April 12, 2021).
18. Government of Yukon. COVID-19 Information. (2021). Available online at: https://yukon.ca/en/covid-19-information (accessed April 12, 2021).
19. Government of Northwest Territories. GNWT's Response to COVID-19. (2021). Available online at: https://www.gov.nt.ca/covid-19/ (accessed April 12, 2021).
20. Government of Nunavut. COVID-19 (Novel Coronavirus). (2021). Available online at: https://www.gov.nu.ca/health/information/covid-19-novel-coronavirus (accessed April 13, 2021).
21. Flaxman S, Mishra S, Gandy A, Unwin JT, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. (2020) 584:257–61. doi: 10.1038/s41586-020-2405-7
22. Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ. The effect of non-pharmaceutical interventions on COVID-19 cases, deaths and demand for hospital services in the UK: a modelling study. Lancet Public Health. (2020) 5:e375–85. doi: 10.1016/S2468-2667(20)30133-X
23. Liu M, Maxwell CJ, Armstrong P, Schwandt M, Moser A, McGregor MJ, et al. COVID-19 in long-term care homes in Ontario and British Columbia. CMAJ. (2020) 192:e1540–6. doi: 10.1503/cmaj.201860
24. Linka K, Rahman P, Goriely A, Kuhl E. Is it safe to lift COVID-19 travel bans? The Newfoundland story. Comput Mech. (2020). doi: 10.1007/s00466-020-01899-x
25. Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. (2020) 323:1915–23. doi: 10.1001/jama.2020.6130
26. Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. (2020) 585:410–3. doi: 10.1038/s41586-020-2293-x
27. Cyr A, Hansen G. Canada's decentralized “Human-Driven” approach during the early COVID-19 pandemic. JMIR Public Health Surveill. (2020) 6:e20343. doi: 10.2196/20343
28. Wong SYS, Kwok KO, Chan FKL. What can countries learn from Hong Kong's response to the COVID-19 pandemic? CMAJ. (2020) 192:e511–515. doi: 10.1503/cmaj.200563
29. Ling J. Where Canada is Falling Short on Its Coronavirus Communications. (2020). Available online at: https://www.macleans.ca/news/canada/canadas-mixed-messages-on-the-coronavirus-outbreak/ (accessed April 20, 2021).
30. Coyne T. B.C Premier Calls on Feds to Discourage Canada-Wide Travel Amid COVID-1. (2020). Available online at: https://vancouverisland.ctvnews.ca/b-c-premier-calls-on-feds-to-discourage-canada-wide-travel-amid-covid-19-1.5194083 (accessed May 2, 2021).
31. Goodyear S. “You Don't Copy the Losers,” Says Doctor Pushing COVID-Zero Strategy. (2020). Available online at: https://www.cbc.ca/radio/asithappens/as-it-happens-monday-edition-1.5803690/you-don-t-copy-the-losers-says-doctor-pushing-covid-zero-strategy-1.5805367 (accessed May 2, 2021).
Keywords: Canada, COVID-19 pandemic, disease outbreak, population health, public health
Citation: Cyr A, Mondal P and Hansen G (2021) An Inconsistent Canadian Provincial and Territorial Response During the Early COVID-19 Pandemic. Front. Public Health 9:708903. doi: 10.3389/fpubh.2021.708903
Received: 12 May 2021; Accepted: 30 August 2021;
Published: 27 September 2021.
Edited by:
Hai-Feng Pan, Anhui Medical University, ChinaReviewed by:
Asmae Khattabi, National School of Public Health, MoroccoCopyright © 2021 Cyr, Mondal and Hansen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gregory Hansen, Z3JlZ29yeS5oYW5zZW5AdXNhc2suY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.