- 1Ministry of Health (MOH) Office for Healthcare Transformation, Singapore, Singapore
- 2Department of Pharmacy, Alexandra Hospital, Singapore, Singapore
- 3Department of Pharmacy, National University of Singapore, Singapore, Singapore
- 4School of Public Health, University of Illinois at Chicago, Chicago, IL, United States
- 5Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 6Emergency Medicine Department, National University Hospital, Singapore, Singapore
- 7National University of Singapore (NUS) Business School, National University of Singapore, Singapore, Singapore
- 8Global Asia Institute, National University of Singapore, Singapore, Singapore
- 9Harvard Business School, Harvard University, Boston, MA, United States
- 10Department of Medicine, National University Hospital, Singapore, Singapore
- 11Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Introduction: Hospital-at-Home (HaH) programmes are well-established in Australia, Europe, and the United States. However, there is limited experience in Asia, where the hospital is traditionally seen as a safe and trusted space for healing. This cross-sectional study aimed to explore attitudes and perceptions among patients and caregivers in Singapore toward this care model.
Methods: A quantitative study design was adopted to collect data among patients and their caregivers from medical wards within two acute hospitals in Singapore. Using a series of closed-ended and open-ended questions, the investigator-administered survey aimed to explore barriers and facilitators determining patients' and caregivers' responses. The study questionnaire was pretested and validated. Data were summarised using descriptive statistics, and logistic regression was performed to determine key factors influencing patients' decisions to enrol in such programmes.
Results: Survey responses were collected from 120 participants (101 patients, 19 caregivers; response rate: 76%), of which 87 respondents (72.5%) expressed willingness to try HaH if offered. Many respondents valued non-quantifiable programme benefits, including perceived gains in quality of life. Among them, reasons cited for acceptance included preference for the comfort of their home environment, presence of family members, and confidence toward remote monitoring modalities. Among respondents who were unwilling to accept HaH, a common reason indicated was stronger confidence toward hospital care.
Discussion: Most patients surveyed were open to having acute care delivered in their home environment, and concerns expressed may largely be addressed by operational considerations. The findings provide useful insights toward the planning of HaH programmes in Singapore.
Introduction
Hospital-at-Home (HaH) is a care model which provides hospital-level acute inpatient services in the comfort of the patient's home. An early version was described by Leff and Burton in 1996 as a “care option that could help certain patients avoid inpatient hospitalization altogether” (1). In HaH care model, remote monitoring and telecommunication technologies can be used to enable the delivery of hospital-level care, which include physician consultations, medication administration, nursing, and therapy services, clinical diagnostics, and investigations, etc.
HaH models have been implemented in countries such as Australia, the United States, Canada, the United Kingdom, and Spain (2). This model of care was implemented as a possible solution to various issues associated with delivery healthcare in hospital. These include increasing rates of nosocomial infections and the rising prevalence of patients with multiple comorbidities who require frequent readmissions (3–5). Studies have shown that the implementation of HaH can result in improved clinical outcomes, in terms of a shorter length of stay and reduced readmission rates (6, 7). It may also bring about greater patient and caregiver satisfaction, along with cost savings for both the patients and the healthcare system (7–9). Mortality rates have been shown to be equivalent to that of patients warded in hospitals, highlighting the safety of this care model (9, 10). HaH has been found to reduce mental stress and adverse hospital events such as functional decline, incontinence, and delirium experienced by elderly who undergo acute hospital admissions (5).
The rapidly ageing population in Singapore has led to growing healthcare expenditure, insufficient hospital beds, and a shortage of clinicians (6). In response to this trend, the Ministry of Health has outlined a shift in focus from hospital to community care. Aligning with this direction, HaH presents a potentially scalable alternative that can lower nationwide healthcare expenditures, alleviate care provider shortages through the use of technology and partnership with community service providers to enhance productivity, and reduce demand for inpatient beds. The necessity of implementing a more adaptable model of care has been exacerbated by the COVID-19 pandemic, which has placed huge strains on local and global healthcare systems.
There have been recent trends that set a favourable landscape for HaH, such as the rising acceptance of telehealth video consultations as an alternative to physical consults, the popularisation of transitional home care services, and the growth of private home care providers. However, because hospital services have historically been confined to the physical walls of a hospital, the public perception of HaH has yet to be well-established. Acceptance of HaH may differ from those of other countries, due to differing cultural views, financing norms and hospital cost structures, and there may be uncertainty in cost savings gained through HaH and patients' perceptions of the safety of HaH (10–12).
This study aimed to elicit attitudes and perceptions among hospitalised patients and their caregivers toward HaH in Singapore, so as to determine the prospects of developing such care models in the future.
Methods
Settings
This study was conducted at two hospitals in Singapore which currently do not have a HaH programme. National University Hospital (NUH) is an academic medical centre and major referral centre with over fifty medical, surgical, and dental specialties. Each year, the 1,239-bed hospital attends to more than one million patients. It serves as a clinical training centre and academic research centre for the medical and dental faculties of the National University of Singapore. Alexandra Hospital (AH) is a general hospital with 326 beds providing comprehensive care to residents in the southwestern region of Singapore, and provides care spanning acute, sub-acute, and rehabilitative settings.
Study Design
A cross-sectional quantitative study was conducted among patients and caregivers at both NUH and AH, from June to August 2020.
Study inclusion criteria were: (1) Patients admitted to NUH and their caregivers during the study period; or (2) Patients admitted to AH medical wards and their caregivers during the study period. All participants were 21 years or older. For this study, a caregiver was defined as the main spokesperson or family member of the patient. Caregivers were approached in the wards during visitation hours if patients were unable to respond, or if they specifically requested the investigators to speak to them instead. The study excluded patients or caregivers who were cognitively impaired and unable to provide informed consent.
Eligible patients and caregivers were recruited by a team of five trained researchers to discuss the study and obtain informed consent at both hospital sites. During the consent-taking process, patients and caregivers were also asked if they would be agreeable for the investigators to access their clinical documentation for additional data collection and be contacted for further interviews if required.
Survey Design
The questionnaire developed by the study investigators aimed to collect general information of their views on receiving inpatient care in a home setting. The survey explored the following domains: (a) background and demographic information, (b) healthcare professionals and procedures encountered during an inpatient stay, (c) perspectives if each care element were delivered at home instead (including home visits, home therapy, remote monitoring, and communication equipment), (d) general views about receiving care at home, and (e) views on the financing models for HaH. Patients and caregivers were assumed to be unfamiliar with HaH care models as this was not the standard of care in Singapore.
The study questionnaire was designed and pre-tested by the study team before actual data collection. Face and content validity were examined through cognitive debriefing, while construct validity, reliability, and internal consistency were examined using empirical data and hypothesis testing through Cronbach's alpha and intraclass correlation (13). The test-retest reliability of the questionnaire was found to be high, with an intraclass correlation of above 0.99. Cronbach's alpha in measurements of various domains were found to be within the satisfactory range of 0.69–0.87.
To determine the sample size for this study, we defined the primary outcome as the proportion of patients who would accept HaH care if it were offered. We then calculated the number of samples required using confidence level of 95% and margin of error of 10%, assuming that there would be an unequal proportion of patients who would accept HaH care compared to those who would reject HaH care. This calculation resulted in a minimum sample size of 97. Recognising a potential situation that the survey would not be carried out with patients exclusively, the study team targeted to complete 120 surveys, with at least 97 of them conducted with patients directly, and not with their caregivers or spokespersons.
Data Analysis
Patient demographics and characteristics were summarised using descriptive statistics – frequency tabulations for categorical variables and summary parameters for continuous variables (means and standard deviation). The primary outcome measure was the proportion of respondents who indicated acceptance of HaH. Secondary exploratory analyses examined the association between the primary outcome measure and selected predictive variables (including patients' age, gender, race, command of selected languages, citizenship, Barthel Index, ward location, employment status, housing type, marital status, presence of domestic helper, education, household per capita income, self-rated overall health) through logistic regression. We hypothesised that most of these demographic variables could directly or indirectly influence the decision to accept or reject the programme among our patients. Data management and analyses were performed with STATA version 13.1 (StataCorp LP, College Station, TX).
Ethics Approval
This study was approved by the National Healthcare Group Domain Specific Review Board (Ref: 2020/00127).
Results
From June 2020 to July 2020, a total of 158 patients were screened to be eligible, and 101 patients responded to the survey in person while 19 caregivers responded on behalf of the patient (response rate = 75.9%). Out of the 120 respondents who completed the survey, 92 (76.7%) respondents provided consent to access their clinical and demographic information, which were used in the study's logistic regression, from their electronic medical records (EMR).
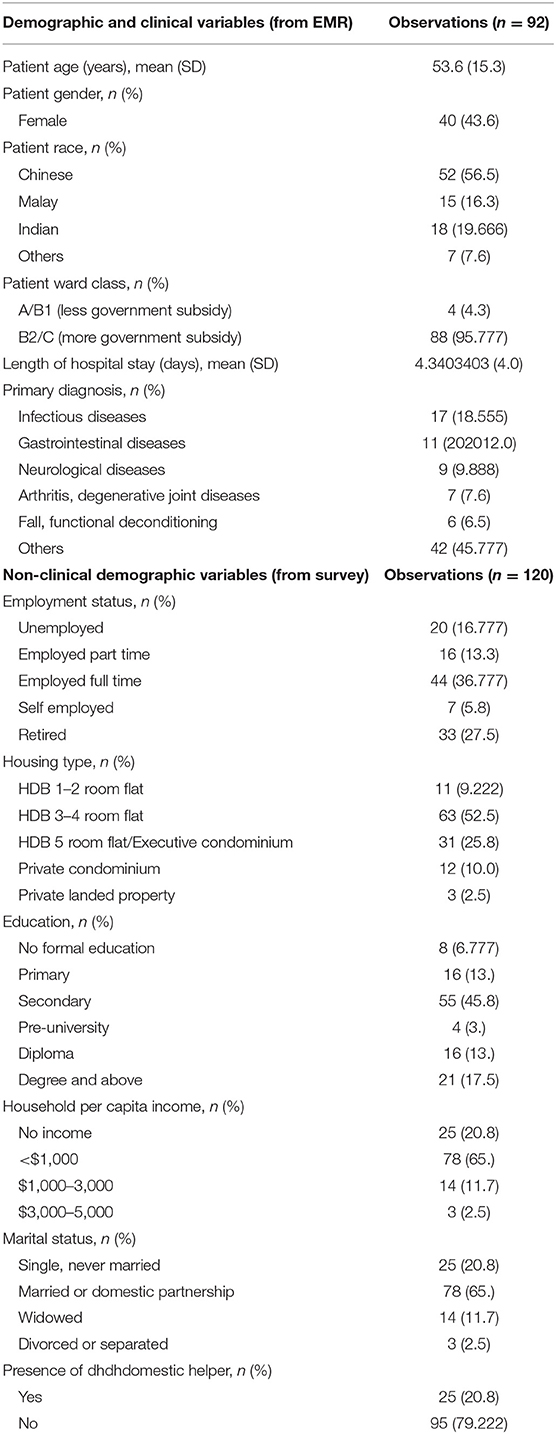
The mean age of the patients surveyed was 53.6 years. Demographic and clinical characteristics of consenting patients are summarised in Table 1.
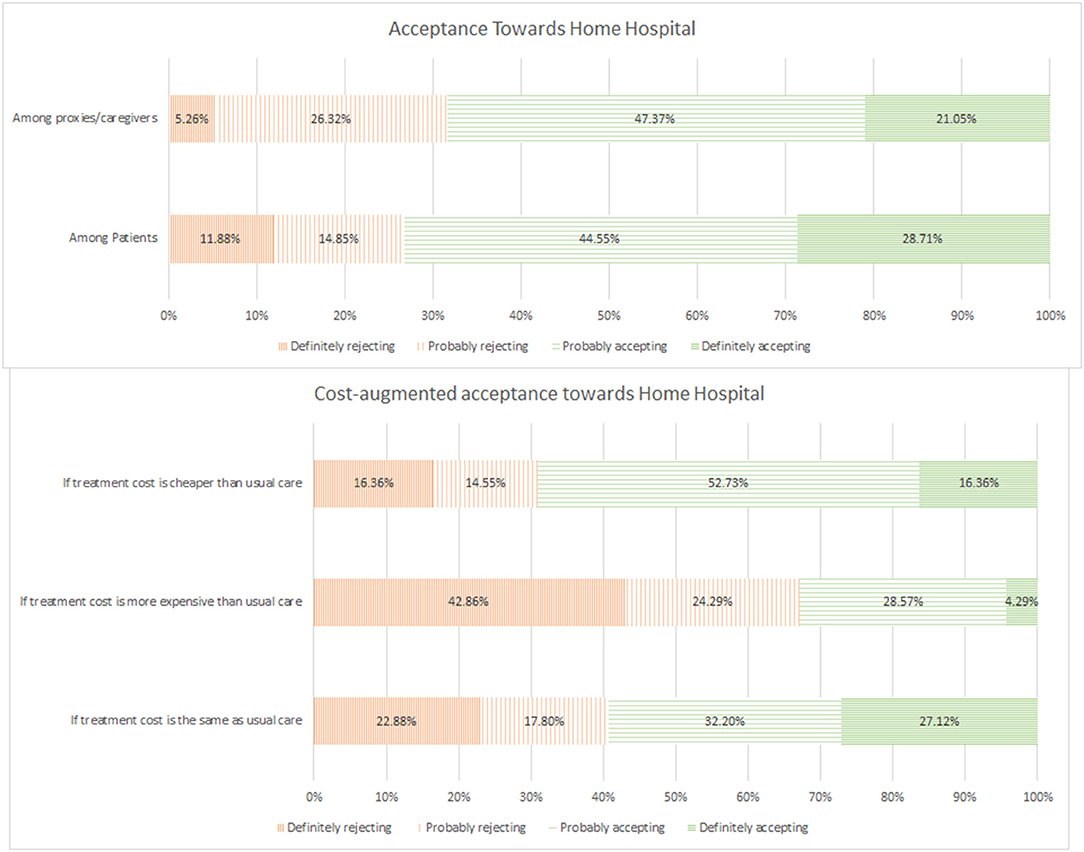
Among the 120 respondents, 87 (72.5%) expressed acceptance toward the novel care model (Figure 1); 29 (28.7%) and 45 (44.6%) patients indicated their definite and probable willingness to participate in a HaH programme, respectively, and (21.1%) and 9 (47.4%) caregivers reported definite and probable willingness to allow their loved ones undergo HaH, respectively. Commonly cited reasons for acceptance included perceived comfort at home, being surrounded by family members, and perceived confidence in remote monitoring as well as the presence of hospital providers helming the care process. On the other hand, frequently cited reasons for rejection included preference for care in hospitals, lack of confidence in technology or care modality, and doubts regarding the ability of hospital providers to deliver comparable care in the home environment.
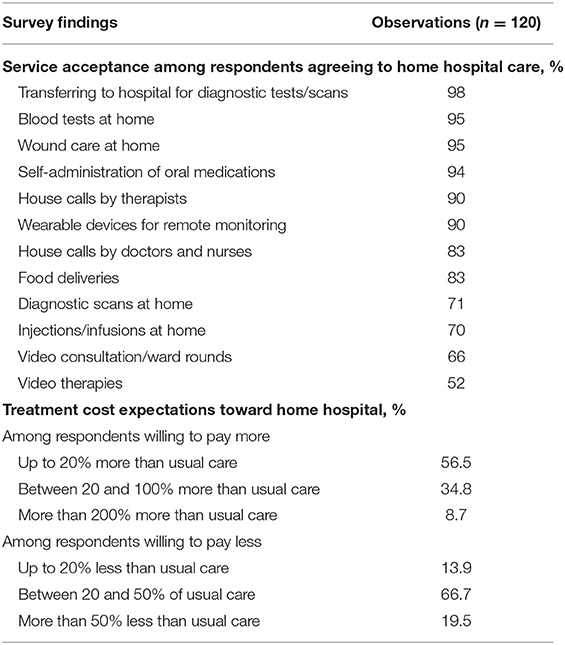
More than half of the respondents surveyed were open to consider home hospitalisation as an alternative to their current inpatient hospitalisation (Table 2). HaH acceptance seemed to be primarily driven by perceived comfort (85% of accepting patients) and the company of loved ones (85% of accepting patients). Many were not deterred by potential risks and were comfortable with remote monitoring of vital signs (82% of accepting patients) and had high level of confidence in remote care delivery (81% of accepting patients). There was also a high degree of acceptance for tests and care procedures to be carried out at home.
In contrast, rejections appeared to be driven by stronger preference for care given in hospital (74% of rejecting patients), uneasiness with remote monitoring technologies (65% of rejecting patients) and a lack of confidence toward remote care delivery (58% of rejecting patients). A good proportion of these patients also wished to have nurses “in-sight” (68% of rejecting patients) and were concerned about burdening family members (46% of rejecting patients).
From the willingness-to-pay analysis, 59.3% of respondents agreed to receive home hospital care at the same price. The acceptance rate dropped to 32.8% if they would need to pay more compared to usual care. Conversely, the proportion increased to 72.2% if they could pay at least 50% less when compared to usual care.
An exploratory analysis was carried out using multivariable logistic regression to determine if there might be factors influencing the programme's acceptance (Table 3). We did not find any statistically significant associations between the dependent variable of HaH acceptance and common socioeconomic determinants including employment status, housing type, presence of domestic helper, and education level. Conversely, HaH acceptance was associated with some factors that were indirectly related to costs of care, including ward location at the point of enrolment (patients in cheaper wards being less inclined to accept the programme compared to patients in more expensive wards, p = 0.015), and income level (households with monthly income of < $3,000 were significantly more inclined to accept the programme, p = 0.04).
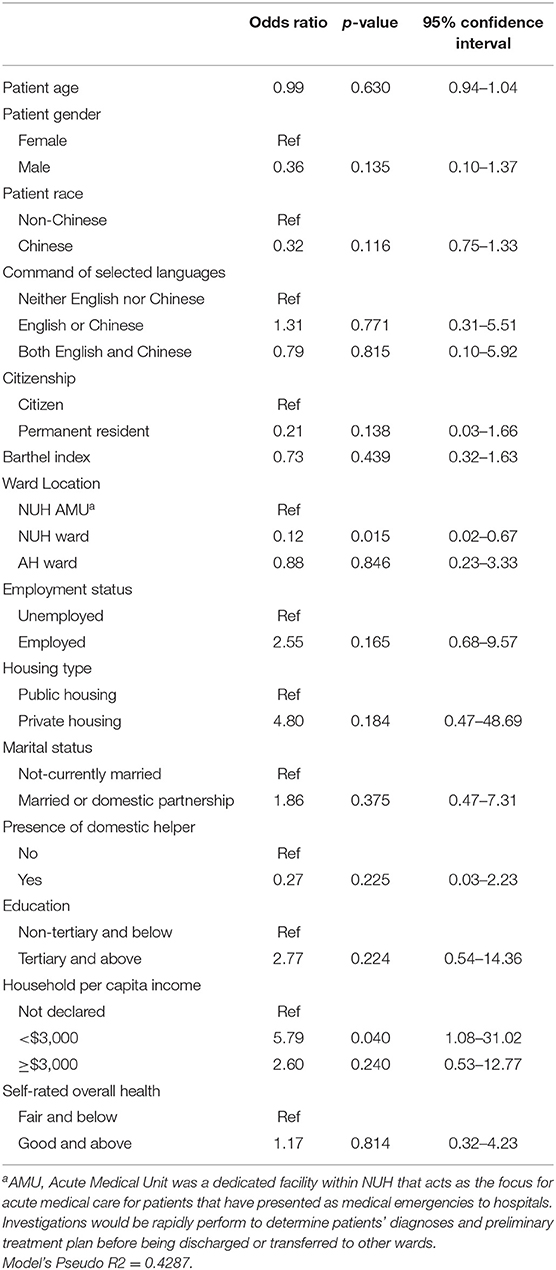
Table 3. Logistic regression model determining the association between HaH programme acceptance and selected determinants.
Discussion
This study is the first to report attitudes and perceptions of hospitalised patients and their caregivers toward HaH care model in Asia. Our findings were contrary to our initial hypothesis that a majority of respondents would prefer care within a hospital (14, 15). In a previous qualitative study investigating care expectations among patients and caregivers in Singapore, there seemed to be an appreciable degree of reluctance among patients and family members to engage in self-care or care of their loved ones in the community compared to receiving care delivered in traditional hospitals (16). We can add an implication here e.g., this highlights the potential of introducing this care model among multi-racial Singapore society (something along these lines).
Although, we had hypothesised that demographic and socioeconomic determinants would influence patients' acceptance of HaH, many anticipated associations were not observed in the regression analysis, with the exception of some factors related to healthcare financing (namely, citizenship that determines the level of government subsidies for inpatient care, and household income). The lack of association could be because the study was neither designed nor powered to detect these differences in secondary analyses. Nonetheless, the data and findings might serve as useful baselines for the planning of future targeted studies looking into quantifiable determinants of HaH acceptance among patients and caregivers.
Our findings highlight important factors for the success of HaH that should be considered when designing such programmes: (1) At the patients' end, there should be a conducive home environment for the patients to receive treatment. Similar requirements, specifically in relation to availability of lifting equipment and lighting, had also been cited as a key factor for successful implementation overseas (17); (2) At the providers' end, there needs to be an effective coordinating centre for centralised monitoring of enrolled patients to provide timely intervention and efficient care. Such a centre can provide patients with access to care teams, enable better care management, and offer psychosocial assistance when required (18); (3) At the practice level, a multidisciplinary, competent care team can be instrumental in instilling greater confidence among patients undergoing home hospitalisation (18).
These findings also validated several crucial factors for programme planners of HaH programmes as previously reported in other studies. Firstly, support for caregivers is an important component in HaH since caregivers' willingness to take on HaH-associated responsibilities affects the ability for HaH to be implemented (2); Specific to the concern over transfer of “care burden” from hospital to home, support for caregivers is integral to ensure the well-being of caregivers and encourage their involvement in HaH. This is especially relevant for the “sandwiched generation” that experiences much social and financial pressures (19). Moving forward, it may also be important to involve community service providers in sharing the caregiving responsibility. Enlisting the help of these providers yields economies of scale and counters the loss of working hours of caregivers. Apart from financial support from government policies, community service providers may be integrated with HaH to provide assistance in activities of daily living, emotional support like counselling services and provision of round-the-clock care advice (20–22). It would be ideal for these community service providers to be reliable partners to the healthcare institutions offering HaH to co-create optimal care for the patients and their caregivers.
Secondly, effective communication between care teams and patients is crucial in enhancing patients' and caregivers' confidence toward such care model. Poor communication between healthcare professionals and patients or caregivers could amplify feelings of apprehension and distress among patients and caregivers (17); Finally, suitable adoption of devices and technologies is important to facilitate care delivery. Adequate patient/caregiver training and easy-to-use devices, such as wearables for remote vital signs monitoring, had been shown to result in greater satisfaction, improved ability to use the device and better overall functioning (18).
The high HaH programme acceptance rate among patients and family members in our study highlights an opportunity for this novel model of care. Its potential ability to tackle bed shortages is especially significant among health systems grappling with ageing populations and an increasing burden of multimorbid, complex cases. Moreover, the current COVID-19 pandemic provides greater impetus for HaH implementation. Such programmes can be pivotal in decentralising care, facilitating rapid ramp-ups in bed capacity, and controlling nosocomial infections (23, 24). For selected patients, HaH could arguably be considered better care. For instance, ED and inpatient ward environments may make delirium worse, while OT assessment in home environment is more accurate (25, 26).
In terms of programme financing and sustainability, we noted that for every 10 respondents we surveyed, six of them agreed to receive home hospital care at the same price, while two more might agree to receive home hospital care if it was 50% cheaper compared to usual care. This willingness-to-pay analysis highlights the importance of appropriate financing models to support HaH to ensure that out-of-pocket payments are at least cost-neutral to inpatient care. If HaH were cheaper than inpatient care that may encourage only a marginal increase in uptake.
Notwithstanding the potential benefits of HaH, the inherent complexity of HaH poses implementation challenges and several factors should be deliberated when planning such schemes. At a broad level, contextual factors for consideration include hospital location and resources and healthcare payment structures. Given the targeted approach of these programmes, HaH may be more practical for larger hospitals with sufficient and predictable casemix to allow for greater economies of scale (27–29).
Moreover, many countries where HaH has been widely implemented (e.g., Australia, the UK) have single-payer systems and strong imperatives to keep medical costs low, whereas, greater barriers are evident in countries such as the US where payment norms are still predominantly episodic and on a fee-for-service basis (30). Nonetheless, with the shift toward value-based payments, capitation, and integrated care across health systems, a more conducive environment for HaH may be emerging (31, 32).
From this study, we have also identified three key enablers for developing successful HaH programmes. First, patients and caregivers must be engaged and assured of sufficient support and oversight from hospital's care teams during the patients' course of care at home. Second, healthcare financing must treat home hospitalisation equally as ward hospitalisation, allowing equivalent subsidies and insurance coverage such that it is cost-neutral or cost-saving to patients who select this option. Third, careful selection and implementation of easy-to-use devices and information technology enablers are key in effective delivery of care at home. In order to validate these hypotheses, further, prospective evaluation of HaH care is warranted (33).
The study has some limitations. The study respondents were relatively young (mean age 53.6 ± 15.3) compared to the approximate median age of 68 among General Medicine patients receiving public hospital care in Singapore. While these characteristics might not represent the older patient groups with the highest healthcare demands, their views were important because such patients will represent the key target segment for HaH programmes in the future, should it get mainstreamed. Secondly, caregivers surveyed in this study excluded paid domestic help. Such domestic helpers were employed by ~25% of survey respondents in this study. This could also be a topic for future exploration. Thirdly, while there were appreciable between-group differences in the willingness-to-pay analysis, they were not reproduced when we examined surrogate markers of socio-economic status in the logistic regression. While the discrepancy between results were indeed present, it was not entirely unexpected due to the small sample size of this study and the relatively large number of variables included in the logistic regression model. Nonetheless, the exploratory findings allowed us to have an indicative understanding of factors that might or might not influence our patients' decision to participate in such programmes.
Conclusion
From the programme acceptance rate reported in this study, HaH may have the potential to substitute substantial proportion of physical “bed-days” in compact urban Singapore. Our findings suggest that HaH programmes may be well-received even in Asia, where the perception of many toward hospital care remains entrenched within the walls of a traditional hospital.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by National Healthcare Group Domain Specific Review Board (Ref: 2020/00127). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Funding
This research was funded by the Ministry of Health Office for Healthcare Transformation (MOHT) to support the pre-pilot research for Hospital at Home Program in the National University Health System, Singapore. The funder declared no commercial interest in this study and played no role in the design, analysis, interpretation of this qualitative data, or the writing of this paper. JG's research was supported by a startup grant from the National University of Singapore (R-314-000-110-133). No conflict of interest has been declared by the other authors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
A MOHT employee was involved in the study as a research collaborator. He provided input in the design of the study as well as the writing of this paper in his capacity as an associate with Alexandra Hospital, National University Health System, Singapore.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.704465/full#supplementary-material
References
1. Leff B, Burton JR. Acute medical care in the home. J Am Geriatr Soc. (1996) 44:603–5. doi: 10.1111/j.1532-5415.1996.tb01452.x
2. Gonçalves-Bradley DC, Iliffe S, Doll HA, Broad J, Gladman J, Langhorne P, et al. Early discharge hospital at home (Review). Cochrane Database Syst Rev. (2017) 6:CD000356. doi: 10.1002/14651858.CD000356.pub4
3. González Ramallo VJ, Mirón Rubio M, Estrada Cuxart O, García Leoni ME. Usefulness of hospital at home in nosocomial infections: advantages and limitations. Rev Esp Quimioter. (2017) 30(Suppl. 1):61–5. Available online at: https://seq.es/seq/0214-3429/30/suppl1/13gonzalez.pdf
4. Vilà A, Villegas E, Cruanyes J, Delgado R, Sabaté R-A, Ortega J, et al. Cost-Effectiveness of a Barcelona home care program for individuals with multimorbidity. J Am Geriatr Soc. (2015) 63:1017–24. doi: 10.1111/jgs.13396
5. Pouw MA, Calf AH, Munster BCV, Maaten JCT, Smidt N, Rooij SED. Hospital at home care for older patients with cognitive impairment: a protocol for a randomised controlled feasibility trial. BMJ Open. (2018) 8:e020332. doi: 10.1136/bmjopen-2017-020332
6. Singapore Public Hospitals Cave Under Pressure of Overcrowding. Singapore Business Review. Available online at: https://sbr.com.sg/healthcare/news/singapore-public-hospitals-cave-under-pressure-overcrowding-0 (accessed August 8, 2018).
7. Levine DM, Ouchi K, Blanchfield B, Diamond K, Licurse A, Pu CT, et al. Hospital-level care at home for acutely ill adults: a pilot randomized controlled trial. J Gen Intern Med. (2018) 33:729–36. doi: 10.1007/s11606-018-4307-z
8. Leff B, Burton L, Mader S, Naughton B, Burl J, Clark R, et al. Satisfaction with hospital at home care. J Am Geriatr Soc. (2006) 54:1355–63. doi: 10.1111/j.1532-5415.2006.00855.x
9. Vianello A, Savoia F, Pipitone E, Nordio B, Gallina G, Paladini L, et al. “Hospital at Home” for neuromuscular disease patients with respiratory tract infection: a pilot study. Respir Care. (2013) 58:2061–8. doi: 10.4187/respcare.02501
10. Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. (2016) 9:CD007491. doi: 10.1002/14651858.CD007491.pub2
11. Lemelin J, Hogg WE, Dahrouge S, Armstrong CD, Martin CM, Zhang W, et al. Patient, informal caregiver and care provider acceptance of a hospital in the home program in Ontario, Canada. BMC Health Serv Res. (2007) 7:130. doi: 10.1186/1472-6963-7-130
12. Leong MQ, Lim CW, Lai YF. Comparison of Hospital-at-Home models: a systematic review of reviews. BMJ Open. (2021). 11:e043285. doi: 10.1136/bmjopen-2020-043285
13. Jaju A, Crask MR. The perfect design: optimization between reliability, validity, redundancy in scale items and response rates. Am Market Assoc. (1999) 10:127.
14. Chan A MR, Manap NB, Ting YY, Visaria A, Cheng GH-L, Goh VSM, et al. Transitions in Health, Employment, Social Engagement And Intergenerational Transfers In Singapore Study (THE SIGNS Study) – I: Descriptive Statistics and Analysis of Key Aspects of Successful Ageing. (2018). Available online at: https://www.duke-nus.edu.sg/docs/librariesprovider3/research-policy-brief-docs/the-signs-study—i-report.pdf
15. Carey K, Lin M-Y. Hospital length of stay and readmission: an early investigation. Med Care Res Rev. (2013) 71:99–111. doi: 10.1177/1077558713504998
16. Lai YF, Lum AYW, Ho ETL, Lim YW. Patient-provider disconnect: a qualitative exploration of understanding and perceptions to care integration. PLoS ONE. (2017) 12:e0187372. doi: 10.1371/journal.pone.0187372
17. Hashem F, Brigden C, Wilson P, Butler C. Understanding what works, why and in what circumstances in hospice at home services for end-of-life care: applying a realist logic of analysis to a systematically searched literature review. Palliat Med. (2020) 34:16–31. doi: 10.1177/0269216319867424
18. McBride SE, Beer JM, Mitzner TL, Rogers WA. Challenges for home health care providers: a needs assessment. Phys Occup Ther Geriatr. (2011) 29:5–22. doi: 10.3109/02703181.2011.552170
19. Sen NJ. Being Sandwiched: The Dilemma of Filial Piety on Young Parents Singapore: Today (2019). Available online at: https://www.todayonline.com/singapore/being-sandwiched-dilemma-filial-piety-young-parents (accessed October 6, 2019).
20. Greater Support for Caregivers Seniors Singapore: The Straits Times (2019). Available online at: https://www.straitstimes.com/singapore/greater-support-for-caregivers-seniors. (accessed October 6, 2019).
21. NTUCHealth. Home Care Services Singapore: NTUC Health. Available online at: https://ntuchealth.sg/home-care/#ics (accessed May 29, 2020).
22. Homage Singapore. Available online at: https://www.homage.sg/care/ (accessed October 6, 2019).
23. Heller DJ, Ornstein KA, DeCherrie LV, Saenger P, Ko FC, Rousseau CP, et al. Adapting a hospital-at-Home care model to respond to New York city's COVID-19 crisis. J Am Geriatr Soc. (2020) 68:1915–6. doi: 10.1111/jgs.16725
24. Coloma E, Nicolás D. Hospital at home units in the post-COVID 19 era. Eur J Clin Invest. (2020) 50:e13390. doi: 10.1111/eci.13390
25. Evensen S, Saltvedt I, Lydersen S, Wyller TB, Taraldsen K, Sletvold O. Environmental factors and risk of delirium in geriatric patients: an observational study. BMC Geriatr. (2018) 18:282. doi: 10.1186/s12877-018-0977-y
26. Offord N, Harriman P, Downes T. Discharge to assess: transforming the discharge process of frail older patients. Future Hosp J. (2017) 4:30–32. doi: 10.7861/futurehosp.4-1-30
27. Sitammagari K, Murphy S, Kowalkowski M, et al. Insights from rapid deployment of a “Virtual Hospital” as standard care during the COVID-19 pandemic. Ann Intern Med. (2021) 174:192–9. doi: 10.7326/M20-4076
28. Saenger P, Federman AD, DeCherrie LV. Choosing inpatient vs home treatment: why patients accept or decline hospital at home. J Am Geriatr Soc. (2020) 68:1579–83. doi: 10.1111/jgs.16486
29. Klein S, Hostetter M, McCarthy D. The Hospital at Home Model: Bringing Hospital-Level Care to the Patient the Commonwealth Fund (2016). Available online at: https://www.commonwealthfund.org/publications/case-~study/2016/aug/hospital-home-model-bringing-hospital-levelcare-patient#/ (accessed October 6, 2019).
30. Marsteller JA, Burton L, Mader SL, Naughton B, Burl J, Guido S, et al. Health care provider evaluation of a substitutive model of hospital at home. Med Care. (2009) 47:979–85. doi: 10.1097/MLR.0b013e31819c93fc
31. Eijkenaar F, Emmert M, Scheppach M, Schöffski O. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. (2013) 110:115–30. doi: 10.1016/j.healthpol.2013.01.008
Keywords: home care services, hospital-based, attitude to health, perception, hospital care, Hospital at Home
Citation: Lai YF, Lim YW, Kuan WS, Goh J, Soong JTY, Shorey S and Ko SQ (2021) Asian Attitudes and Perceptions Toward Hospital-At-Home: A Cross-Sectional Study. Front. Public Health 9:704465. doi: 10.3389/fpubh.2021.704465
Received: 05 May 2021; Accepted: 24 June 2021;
Published: 23 July 2021.
Edited by:
Michael Ekubu Otim, University of Sharjah, United Arab EmiratesReviewed by:
Prof. Mariela Deliverska, Medical University Sofia, BulgariaSyed Azizur Rahman, University of Sharjah, United Arab Emirates
Copyright © 2021 Lai, Lim, Kuan, Goh, Soong, Shorey and Ko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Feng Lai, eWlmZW5nLmxhaUBtb2h0LmNvbS5zZw==
 Yi Feng Lai
Yi Feng Lai Yee Wei Lim5
Yee Wei Lim5 Joel Goh
Joel Goh Shefaly Shorey
Shefaly Shorey