- 1Observatory of Perinatal Clinical Psychology, Section of Neuroscience, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy
- 2Units of Biostatistics and Biomathematics and Bioinformatics, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy
- 3Department of Clinical Sciences and Community Health, University of Milan, Milan, Italy
The coronavirus disease 2019 (COVID-19) pandemic is strongly changing the way most people live their lives, and disrupting specialist healthcare systems. Such public health disruptions have resulted in significant collateral damage with particular implications for vulnerable populations, including the perinatal population. This Study aims to estimate the impact of the COVID-19 pandemic on Italian maternal and perinatal health care services. A questionnaire was designed to evaluate the COVID-19 impact on Italian maternal and perinatal healthcare facilities and their activities and provision of services from March to May 2020. The survey was completed by hospital-based and community-based Italian maternal and perinatal healthcare facilities. Most of these were located in Lombardy or Veneto (the most affected Italian regions). 70% of all facilities reported that the first wave of the COVID-19 pandemic negatively influenced the functioning of one or more aspects of the perinatal service; only 28.4% of facilities all over the country continued to provide outpatient routine visits and examinations as usual; 23.4% of facilities became understaffed during the index period due to various reasons such as ward transfer and sick leave. This is the first Italian study, and among very few international studies that describe the effects of the COVID-19 pandemic on antenatal and postnatal healthcare facilities and their provision of activities and services. Our findings confirm that healthcare systems even in high-income countries were not entirely prepared to handle such a global health emergency; indeed, specialized maternal and perinatal healthcare services have been disrupted by this global health emergency.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic quickly and widely spread from the Hubei Province in the People's Republic of China, where the virus originated in December 2019, throughout the world, starting in early 2020 (1, 2). It has extensively changed the way most people live their daily life, including interpersonal relationships and health habits (3).
Furthermore, the morbidity and mortality associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have put healthcare systems worldwide under great strain (4) and also disrupted a variety of general and specialist health facilities that deliver non-COVID-19 health care services (5–10). These disruptions to public health have resulted in significant collateral damage with particular implications for vulnerable populations (11–13), including the perinatal population (7, 14–16).
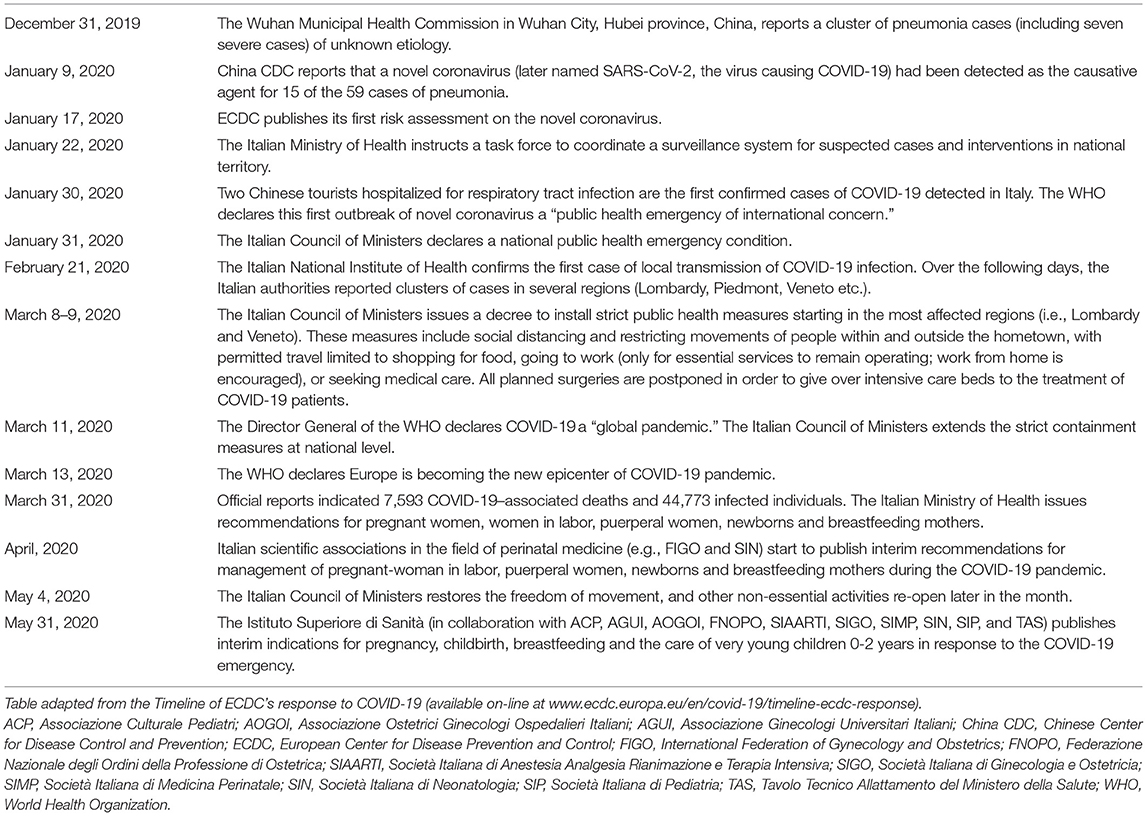
Italy was the second epicenter of the spread of COVID-19 (17) and major changes have been made to the provision of health services since the outbreak in March 2020 (see Table 1). The initial rapid spread of infections and the limited number of intensive care beds available posed a critical threat to the Italian national health system (18) and its workers (thousands of healthcare professionals have been infected by the virus and many of them have died) (19, 20). Healthcare facilities constituted the main source of virus outbreaks because of hospital overcrowding and the existence of asymptomatic cases of the virus (21). After this first wave of pandemic, which ended in May 2020, the Italian government implemented significant changes to the structure of the health system in order to stem the second wave (22). However, the effects were different in different regions. The severity and the mortality of COVID-19 infection in Lombardy (which was the Italian epicenter) and Veneto were higher during this first wave of pandemic than during the second wave (between October 2020 and January 2021). For instance, in Lombardy there were 16,362 deaths (47.7% of deaths in Italy) during the first wave and 15,515 deaths (18.9% of deaths in Italy) during the second and the third wave combined (23, 24). But this does not apply to the rest of Italy, where the trend in mortality was reversed: 34,260 and 38,535 deaths in the first and second wave, respectively (23, 24).
To date, COVID-19 studies in Italy have reported the disruption of services and substantial changes in the way clinical care is delivered for mental health (25), oncology (26), surgical arthroplasty (27), pediatrics (28) and many other specialist healthcare systems. However, at the time of writing, the status of the perinatal healthcare system has not yet been comprehensively or extensively investigated. Therefore, we sought to evaluate the impact of the COVID-19 outbreak and the containment measures on maternal and perinatal healthcare services in Italy.
Methods
Study Design and Participants
A cross-sectional survey was conducted using an online questionnaire accessible on the University of Brescia website. The questionnaire was distributed via an electronic link to the coordinators or representatives of 1,428 public and private maternal and perinatal healthcare centers located throughout Italy. A brief explanation of the study purpose and assurance of anonymity was outlined in the body of the email as well as on the first page of the questionnaire. Informed written consent was obtained from all respondents before data collection. The research was approved by the Ethics Committee of ASST Spedali Civili Hospital Brescia, Italy (Approval number: NP4221 24.06.2020). The questionnaire was made available for completion from June 30 to October 7, 2020. Data were collected using LimeSurvey.
Survey Description
The survey questionnaire was specifically created for this study: to evaluate the COVID-19 impact on both antenatal and postnatal healthcare facilities and their activities and provision of services. It was designed and trialed by a team of perinatal experts who work in maternal and perinatal clinics or are regularly involved in research in this area and in the training of healthcare workers. All the experts are members of the Observatory of Perinatal Clinical Psychology (https://www.unibs.it/it/node/988), Section of Neuroscience of the Department of Clinical and Experimental Sciences (University of Brescia, Italy). Possible misinterpretations or difficulties with wording or comprehension were discussed and resolved within the core research group. The final version of the survey questionnaire included 60 general questions, 4 additional specific questions for antenatal services and 13 for intrapartum, postnatal services. Most of the questions were closed-ended, but some optional open-ended questions were used to allow respondents to express their subjective perceptions. An example of the survey questions is “How many healthcare professionals are employed in your facility?” or “Was your facility converted into COVID-19 units during the period of health emergency (March–May 2020)?” For the latter question there were three closed-ended responses: “Yes, completely,” “Yes, but only partially,” “No”.
Statistical Analysis
Descriptive analyses were performed. Categorical variables were recorded in terms of frequency and compared across groups using the chi-square test or the Fisher's exact test, as appropriate. Analyses were performed using R version 4.0.2 (R Foundation for statistical computing, Vienna, Austria).
Results
Sample Characteristics
Seventy-seven Italian perinatal healthcare facilities completed the survey (response rate 5.4%). Of these, 46 were prenatal facilities, whereas 31 were intrapartum/postnatal or maternal facilities. Thirty-nine were located in Lombardy or Veneto (the most affected Italian regions), and the remaining were from the other ten regions. Twenty-five were hospital-based, whereas the remaining were community-based. The median of healthcare professionals working in the facilities was 10 (inter-quartile range = 37.7).
All the results, unless otherwise specified, did not yield significant differences between hospital- and community-based facilities, geographical areas, or antenatal and intrapartum/postnatal care.
Services
Seventy percent of all facilities reported that the first wave of the COVID-19 pandemic negatively influenced the functioning of one or more aspects of the maternal and perinatal services. The impact of the measures taken to prevent the spread of the virus on specific activities and services provided by Italian perinatal healthcare facilities is reported in Table 2.
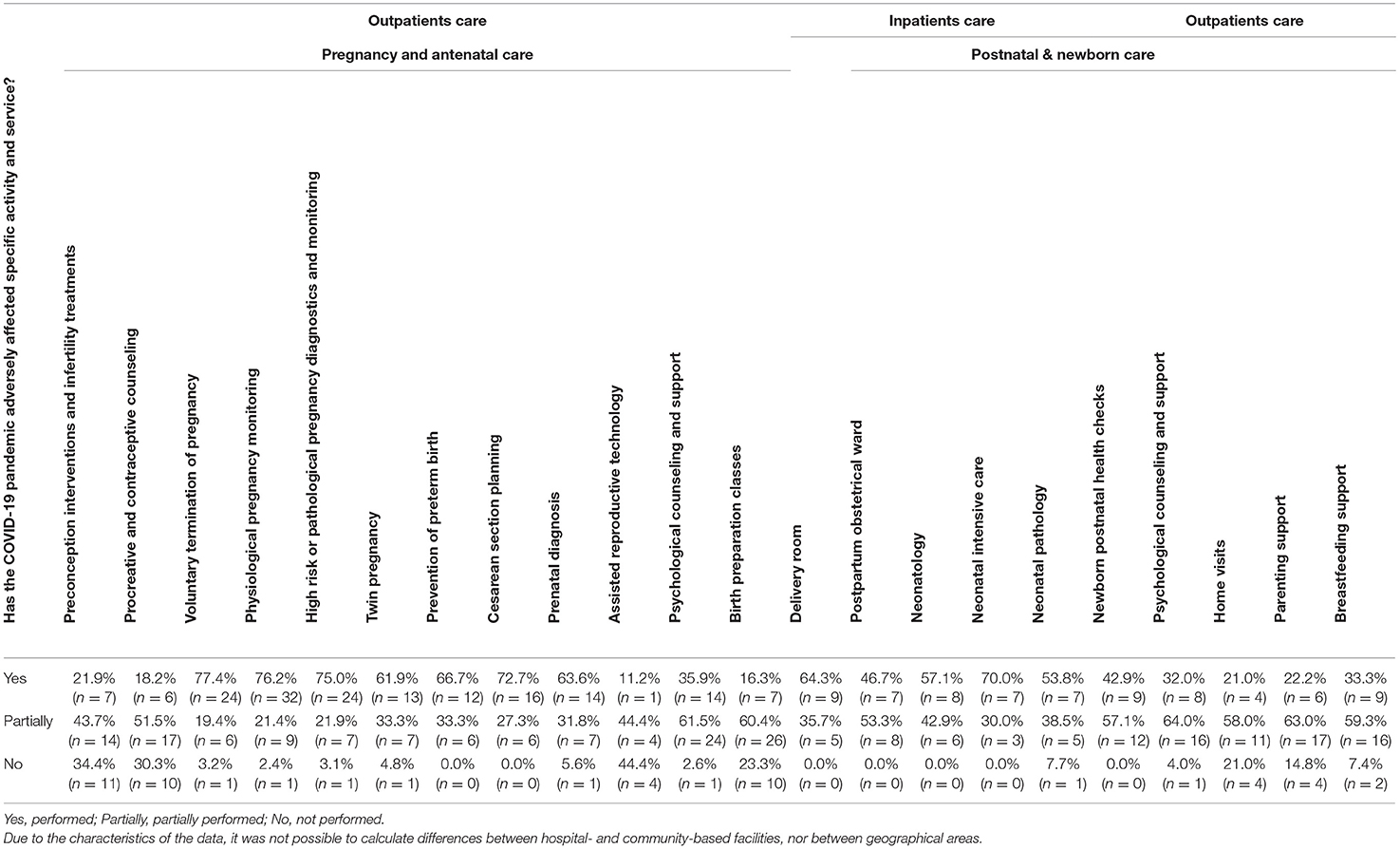
Table 2. Impact on activities and services provided by perinatal healthcare facilities in the Italian national territory.
Visits and Examinations
From March to May 2020, only 28.4% of facilities all over the country continued to provide outpatient routine visits and examinations as usual, 59.4% provided visits but to a limited extent, while 12.2% ceased their activities. However, the majority of maternal and perinatal facilities were available for emergencies, either completely (68.8%) or to a limited extent (19.7%). All the facilities in which emergency visits were ceased were community-based and, except one, were located in Lombardy or Veneto. Regarding the waiting time for first visits and control visits, most centers reported that it was not extended (61.2 and 55.4%, respectively) or only partially (29.3 and 33.8%, respectively). Most of the facilities (68.8%; 78.3% prenatal vs. 54.8% postnatal, p = 0.03) had always or almost always kept fathers out of their partners' visits and exams.
Overall, at 24.7% of the facilities a part of the staff, and at 6.5% of the facilities, all the staff, continued their job in smart working mode. Most facilities continued to provide always, or almost always, in-person visits with physicians (82%), obstetricians (82.6%), and nurses (77.1%) during the pandemic. On the other hand, only 32.8% of facilities always or almost always provided in-person psychological visits. The facilities located in Lombardy or Veneto significantly more frequent in-person visits with physicians, compared to those located in the other regions, (91.3 and 74.1%, respectively, p = 0.04) and by psychologists (38.9 and 25.0%, respectively, p = 0.02). At the same time, obstetrician and nurse visits were significantly more frequently used by hospital-based professionals than by community-based colleagues (90.5 vs. 79.2%, p = 0.02 for obstetricians; 88.2 vs. 66.7%, p = 0.02 for nurses).
Transformation Into a Dedicated COVID Facility
About a quarter of maternal or perinatal healthcare facilities (23.4%) were partially converted or transformed into COVID-19 units (16 out of 18 of these facilities were hospital-based) to provide care and support to the large number of patients infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Further, two facilities (2.6%), that is, a hospital-based obstetrics and gynecology ward and a community-based birth center, were completely converted into COVID-19 facilities.
Staff
Overall, a minority of facilities reported that some or all of the staff members (13 and 3.9%, respectively) were transferred to COVID-19 wards. This occurred significantly more frequently in hospital-based facilities than in community-based facilities. Nevertheless, almost one-fourth (23.4%) of the facilities, both hospital- and community-based, became understaffed during the index period due to various reasons such as ward transfer and sick leave.
About half of the facilities (46.0%) provided the entire staff with specific training on COVID-19 management, whereas a further 28.6% provided it only to select staff members. The remaining 25.4% did not provide any training.
Regarding the use of personal protective equipment (PPE) and the adoption of social/physical distancing, though perceived as essential and health-saving, both were considered very stressful by the staff of 68.2% of the facilities.
Discussion
Our survey provides sobering insights into disruption to care and treatment for peripartum and perinatal patients (i.e., pregnant women, new mothers and their fetus/neonate) in Italy. We analyzed responses from 77 facilities in 11 Italian regions, covering relevant aspects of the activities and services provided in ante-, intra-, and post-partum clinical settings. Our data aligns with similar studies (6, 29) revealing that the pandemic has caused disruptions, with delays, reductions or cancellations in both maternal and neonatal appointments.
Regarding check-ups and examinations, although it is fully understandable that non-urgent services, such as many routine outpatient visits, were canceled in a well-intentioned effort to contain the spread of the new coronavirus (e.g., reports clearly show that, due to the pandemic, fewer women received follow-up care after obstetric anesthesia) (30). This change in access to medical and health services adversely affected the standard of maternal and perinatal care, including the realm of mental health care but particularly that of preventive, routine, and corrective medicine (5, 6, 29). The peripartum/perinatal population is particularly vulnerable, both physically and psychologically, to altered or delayed health care, because patients need and deserve close longitudinal monitoring (31). This is true for all pregnant and postpartum women as well as their babies because, for instance, even in case of a healthy young woman with non-complicated pregnancy (at least for a certain period), a complex maternal condition or fetal anomaly requiring multiple medical subspecialty consultations could occur. We must bear in mind that routine appointments are crucial to enable parents to participate in a shared decision-making process in all the cases in which there is uncertainty about medical conditions (32). Additionally, these consultations may also alleviate unnecessary parental anxiety. All these aspects must be considered when working during disasters such as the ongoing pandemic because, as highlighted by a systematic review on the effects of disaster on pregnancy and the postpartum period, they have an indirect impact on maternal mental health and some perinatal health outcomes (33). Moreover, it has been observed that the well-documented negative influence of mother's mental health on child development (34, 35) may be even greater after a disaster than any direct effect of disaster-related prenatal stress (33).
As regards telehealth (vs in-person check-ups), our data aligns with previous studies showing that it has been rapidly adopted in perinatal care since the onset of the pandemic (36–39). Telehealth offers safe access to consultation and follow-up appointments, saving patients both time and money, but is a complex system that normally requires years of implementation and optimization (40) in order to be an effective tool for providing comprehensive and multidisciplinary perinatal care, mainly in cases where physical examination is not or is rarely necessary. Face-to-face check-ups are still essential in high-risk cases (41). However, in certain cases, such as women with gestational diabetes mellitus, self-care programs via telemedicine may be a better choice than face-to-face visits (42).
In terms of healthcare workers, obstacles to effective care appear to include understaffing and additional stress for perinatal healthcare workers, and this aligns with the previously demonstrated increase in stress during the pandemic, stemming from staff shortages, excessive workload and the use of personal protective equipment (43). In terms of the patient's couple relationship, keeping patients (mothers and babies) together with their partner/other parent is crucial for respectful and effective care. However, consistently with other studies (5, 44, 45), our data show that partners/other parents are often excluded from the mother's check-ups and examinations in an effort to protect other patients and staff from infection.
As concerns the regional differences, our results indicate that facilities located in Lombardy or Veneto experienced a greater reduction in the provision of outpatient visits, especially emergency visits, and a statistically significant higher percentage of closures of community-based facilities. This is in line, on the one hand, with the Italian geographical distribution of the infection (northern regions faced disproportionately higher numbers of infections and deaths compared with southern and central Italy) (46), and on the other hand, with other Italian studies showing significant variations across regions in the way COVID-19 has affected medical specialist departments [e.g., radiology has changed during the pandemic with a large variability among different Italian regions; (47)]. With regard to the main difference between antenatal and postnatal services, that is, the degree to which fathers are permitted to attend their partners' visits and exams, one plausible and economical explanation is that different regions adopted different approaches to patient care, for instance different Italian regions implemented different strategies in terms of hospitalization, treatment in ICUs or home care for patients infected with SARS-CoV-2 (48). Here, we point out that Italian health system is regionally decentralized (thus, Italy has twenty regional health services), a situation that is not useful in controlling a pandemic, especially if we take into account the strong political pressure toward the transfer of tax resources from the central (national) government to the regions where income is produced (49).
Taken as a whole, the results of this study suggest that Italy was not entirely prepared to handle such a pandemic; indeed, specialist perinatal healthcare services have been (and still are) disrupted at many levels by this global health emergency. This is in line with other COVID-19 studies that have reported similar situations in other high-income countries (5, 29, 36–41, 43–45, 49–51). Our findings deepen the understanding of how the pandemic has influenced Italian healthcare facilities, and can be crucial in guiding the development and implementation of effective responses and, more broadly, in supporting and strengthening perinatal health systems. From this perspective, crises are also times of opportunity (12). The COVID-19 pandemic has caused us to rethink how to improve access to and implementation of perinatal healthcare services. The improvements forced by the current pandemic will be useful during the next phases as well as during future possible national or global health crises.
Strengths and Limitations
The main strength of this research is that it is the first Italian study, and among very few international studies, that describe the effects of the COVID-19 pandemic on healthcare facilities and their provision of services. Thus, it may be helpful for the formulation of appropriate and evidence-based actions to be taken. However, in interpreting these results, certain limitations must be considered. First, the low response rate (5.4%) and of the fact that certain Italian regions are poorly represented or absent from the study. Thus, the results may not be representative of all perinatal healthcare facilities in Italy. However, it should be kept in mind that low response rates to online surveys in primary care are common and the extent to which results are affected is uncertain (52). Second, there is no information on the geographic location (urban vs. rural), patient volumes, and demographic characteristics of the responding facilities.
Conclusion
The COVID-19 pandemic has disrupted maternal and perinatal healthcare activities and services, as well as increasing levels of stress among healthcare providers. This study sheds light on the effects of the COVID-19 pandemic on maternal and perinatal healthcare facilities and provides insights for policymakers. The management, allocation, and training of peripartum/perinatal healthcare workers can and must be improved. Italian policymakers and administrators are urged to work together to improve care for the most vulnerable. Prompt and continuous evaluation, along with timely and effective information on the status of healthcare facilities is fundamental to the development and implementation of contextually relevant guidelines.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the corresponding author upon request.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of ASST Spedali Civili Hospital Brescia, Italy (NP4221 24.06.2020). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LC and AS contributed equally to the general study design. LC and AT from the Observatory of Perinatal Clinical Psychology promote and coordinate the study in each health care service. MR, SC, and BM designed the plan of statistical analysis of the study. All authors have critically reviewed and agreed this final version of the article.
Funding
This work was funded by the Observatory of Perinatal Clinical Psychology, Section of Neuroscience, Department of Clinical and Experimental Sciences, University of Brescia (Italy).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the study participants who took time to respond to this survey despite the difficult circumstances and increased workload. We would like to thank all colleagues who distributed the invitation for this survey promoted by the Observatory of Perinatal Clinical Psychology, Section of Neuroscience, Department of Clinical and Experimental Sciences, University of Brescia (Italy).
References
1. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. (2020) 24:91–8. doi: 10.1016/j.jare.2020.03.005
2. Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. (2020) 25:278–80. doi: 10.1111/tmi.13383
3. Haleem A, Javaid M, Vaishya R. Effects of COVID-19 pandemic in daily life. Curr Med Res Pract. (2020) 10:78–9. doi: 10.1016/j.cmrp.2020.03.011
4. Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P, Rada AG. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. (2020) 368:m1090. doi: 10.1136/bmj.m1090
5. Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. (2020) 5:e002967 doi: 10.1136/bmjgh-2020-002967
6. Jha D, Adhikari M, Gautam JS, Tinkari BS, Mishra SR, Khatri RB. Effect of COVID-19 on maternal and neonatal services. Lancet Glob Health. (2021) 9:e114–5. doi: 10.1016/S2214-109X(20)30482-4
7. Cena L, Biban P, Janos J, Lavelli M, Langfus J, Tsai A, Youngstrom EA, Stefana A. The collateral impact of COVID-19 emergency on neonatal intensive care units and family-centered care: challenges and opportunities. Front Psychol. (2021) 12:317. doi: 10.3389/fpsyg.2021.630594
8. Khalil A, von Dadelszen P, Kalafat E, Sebghati M, Ladhani S, Ugwumadu A, et al. Change in obstetric attendance and activities during the COVID-19 pandemic. Lancet Infect Dis. (2020) 21:e115. doi: 10.1016/S1473-3099(20)30779-9
9. Ashish KC, Gurung R, Kinney MV, Sunny AK, Moinuddin MD, Basnet O, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. (2020) 8:e1273–81. doi: 10.1016/S2214-109X(20)30345-4
10. Green L, Fateen D, Gupta D, McHale T, Nelson T, Mishori R. Providing women's health care during COVID-19: personal and professional challenges faced by health workers. Int J Gynecol Obstet. (2020) 151:3–6. doi: 10.1002/ijgo.13313
11. Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, et al. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol. (2020) 5:426–8.
12. Stefana A, Youngstrom EA, Hopwood CJ, Dakanalis A. The COVID-19 pandemic brings a second wave of social isolation and disrupted services. Eur Arch Psychiatry Clin Neurosci. (2020) 270:785–6. doi: 10.1007/s00406-020-01137-8
13. Youngstrom EA, Hinshaw SP, Stefana A, Chen J, Michael K, Van Meter A, et al. Working with bipolar disorder during the covid-19 pandemic: both crisis and opportunity. Wiki J Med. (2020) 7:6. doi: 10.15347/WJM/2020.004
14. Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. (2021) 9:e759–72. doi: 10.1016/S2214-109X(21)00079-6
15. Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. (2021) 18:10. doi: 10.1186/s12978-021-01070-6
16. Cena L, Rota M, Calza S, Massardi B, Trainini A, Stefana A. Mental health states experienced by perinatal healthcare workers during COVID-19 pandemic in Italy. Int J Environ Res Public Health. (2021) 18:6542. doi: 10.3390/ijerph18126542
17. Horowitz J, Bubola E, Povoledo E. Italy, Pandemic's New Epicenter, Has Lessons for the World. New York Times (2021). Available online at: https://www.nytimes.com/2020/03/21/world/europe/italy-coronavirus-center-lessons.htmlItaly.world/europe/italy-coronavirus-center-lessons.html (accessed April 25, 2021).
18. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. (2020) 323:1545–6. doi: 10.1001/jama.2020.4031
19. Chirico F, Nucera G. Tribute to healthcare operators threatened by the COVID-19 pandemic. J Health Soc Sci. (2020) 5:165–8. doi: 10.19204/2020/trbt1
20. Chirico F, Nucera G, Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. (2020) 41:1117. doi: 10.1017/ice.2020.148
21. Chirico F, Nucera G, Magnavita N. Hospital infection and COVID-19: do not put all your eggs on the ‘swab' tests. Infect Control Hosp Epidemiol. (2020) 42:1–2. doi: 10.1017/ice.2020.254
22. Chirico F, Sacco A, Magnavita N, Nucera G. Coronavirus disease 2019: the second wave in Italy. J Health Res. (2021) 35:359–63. doi: 10.1108/JHR-10-2020-0514
23. Chirico F, Nucera G, Szarpak L. COVID-19 mortality in Italy: the first wave was more severe and deadly, but only in Lombardy region. J Infect. (2021) 83:e16. doi: 10.1016/j.jinf.2021.05.006
24. Istituto Superiore di Sanità. COVID-19 integrated surveillance data in Italy. Available online at: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-dashboard (accessed April 25, 2021).
25. Stefana A, Youngstrom EA, Jun C, Hinshaw S, Maxwell V, Michalak E, Vieta E. The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Dis. (2020) 22:641–3. doi: 10.1111/bdi.12949
26. Indini A, Aschele C, Bruno D, Clerico M, Daniele B, Fiorentini G, et al. Reorganization of medical oncology departments during COVID-19 pandemic: a nationwide Italian survey. Eur J Cancer. (2020) 132:17–23. doi: 10.1016/j.ejca.2020.03.024
27. D'Apolito R, Faraldi M, Ottaiano I, Zagra L. Disruption of arthroplasty practice in an orthopaedic center in northern Italy during COVID-19 pandemic. J Arthroplst. (2020) 35:S6–9. doi: 10.1016/j.arth.2020.04.057
28. Silvagni D, Baggio L, Meragliotta PLT, Soloni P, La Fauci G, Bovo C, et al. Impact of COVID-19 pandemic on the characteristics of paediatric emergency room visits in a tertiary centre in Northern Italy. Res Square. (2020). doi: 10.21203/rs.3.rs-61729/v1
29. Jardine J, Relph S, Magee LA, von Dadelszen P, Morris E, Ross-Davie M, et al. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG. (2021) 128:880–9. doi: 10.1111/1471-0528.16547
30. Rimmer AA, Thomas E, Thomas OD, Helme D, Tozer J. Impact of the COVID-19 pandemic on obstetric anaesthesia: a service evaluation. Int J Obstet Anesth. (2021) 46:103041. doi: 10.1016/j.ijoa.2021.103041
31. Suellentrop K, Morrow B, Williams L, D'Angelo D, Centers for Disease Control and Prevention (CDC). Monitoring progress toward achieving Maternal and Infant Healthy People 2010 objectives-19 states, Pregnancy Risk Assessment Monitoring System (PRAMS), 2000-2003. MMWR Surveill Summ. (2006) 55:1–11.
32. Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Légaré F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. (2012) 344:344:e256 doi: 10.1136/bmj.e256
33. Harville E, Xiong X, Buekens P. Disasters and perinatal health: a systematic review. Obstetr Gynecol Surv. (2010) 65:713–728. doi: 10.1097/OGX.0b013e31820eddbe
34. Stefana A, Lavelli M. Parental engagement and early interactions with preterm infants during the stay in the neonatal intensive care unit: protocol of a mixed-method and longitudinal study. BMJ Open. (2017) 7:e013824. doi: 10.1136/bmjopen-2016-013824
35. Cena L, Palumbo G, Mirabella F, Gigantesco A, Trainini A, Stefana A. Perspectives on early screening and prompt intervention to identify and treat maternal perinatal mental health. Protocol for a prospective multicenter study in Italy. Front Psychol. (2020) 11:365 doi: 10.3389/fpsyg.2020.00365
36. Ukoha EP, Davis K, Yinger M, Butler B, Ross T, Crear-Perry, et al. Ensuring equitable implementation of telemedicine in perinatal care. Obstetr Gynecol. (2021) 137:487. doi: 10.1097/AOG.0000000000004276
37. Gutiérrez MMC, Durán-Vila A, Ruiz-Labarta J, Payá-Martínez P, Pintado Recarte P, Bujan J, et al. New Multiplatform Model for Outpatient Prenatal and Postpartum Care in a Cohort of COVID-19-Affected Obstetric Patients. Int J Environ Res Public Health. (2021) 18:5144. doi: 10.3390/ijerph18105144
38. DeMauro SB, Duncan AF, Hurt H. Telemedicine use in neonatal follow-up programs-what can we do and what we can't-lessons learned fromCOVID-19. Semin Perinatol. (2021) 151430. doi: 10.1016/j.semperi.2021.151430
39. Bishop CE, Jackson LE, Vats KR, Azzuqa AA. Prenatal neonatology telemedicine consultation for patients with fetal anomalies during the COVID-19 pandemic era: rapid implementation and lessons learned. J Perinatol. (2020) 40:1451–2. doi: 10.1038/s41372-020-00787-9
40. Jackson LE, Bishop CE, Vats KR, Azzuqa AA. Meeting families where they are: institution, evaluation, and sustainability of telemedicine prenatal neonatology consultation in the COVID-19 pandemic health emergency. Semin Perinatol. (2021) 151417. doi: 10.1016/j.semperi.2021.151417
41. Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, et al. Saving Lives, Improving Mothers' Care Rapid Report: Learning From SARS-CoV-2-Related and Associated Maternal Deaths in the UK March–May 2020. Oxford: National Perinatal Epidemiology Unit, University of Oxford (2020).
42. Moradi F, Ghadiri-Anari A, Enjezab B. COVID-19 and self-care strategies for women with gestational diabetes mellitus. Diabetes Metab Syndr. (2020) 14:1535–9. doi: 10.1016/j.dsx.2020.08.004
43. Rao SP, Minckas N, Medvedev MM, Gathara D, Prashantha YN, Estifanos AS, et al. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers' voices and experiences. BMJ Glob Health. (2021) 6:e004347. doi: 10.1136/bmjgh-2020-004347
44. Gressier F, Mezzacappa A, Lasica PA, Fourcade C, Corruble E. COVID outbreak is changing our practices of perinatal psychiatry. Arch Womens Ment Health. (2020) 23:791–2. doi: 10.1007/s00737-020-01039-7
45. Carroll WD, Strenger V, Eber E, Porcaro F, Cutrera R, Fitzgerald DA, et al. European and United Kingdom COVID-19 pandemic experience: the same but different. Paediatr Respir Rev. (2020) 35:50–6. doi: 10.1016/j.prrv.2020.06.012
46. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. (2020) 395:1225–28. doi: 10.1016/S0140-6736(20)30627-9
47. Albano D, Bruno A, Bruno F. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Eur Radiol. (2020) 30:6635–44. doi: 10.1007/s00330-020-07046-7
48. Pecoraro F, Luzi D, Clemente F. Analysis of the different approaches adopted in the italian regions to care for patients affected by COVID-19. Int J Environ Res Public Health. (2021) 18:848. doi: 10.3390/ijerph18030848
49. Magnavita N, Chirico F, Sacco A. COVID-19: from hospitals to courts. Lancet. (2021) 97:1542. doi: 10.1016/S0140-6736(21)00472-4
50. Graham WJ, Afolabi B, Benova L, Campbell OMR, Filippi V, Nakimuli A, et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: call for a service safety net. BMJ Glob Health. (2020) 5:e002754. doi: 10.1136/bmjgh-2020-002754
51. Bradfield Z, Wynter K, Hauck Y, Vasilevski V, Kuliukas L, Wilson AN, et al. Experiences of receiving and providing maternity care during the COVID-19 pandemic in Australia: a five-cohort cross-sectional comparison. PLoS ONE. (2021) 16:e0248488. doi: 10.1371/journal.pone.0248488
Keywords: health services, antenatal and postnatal healthcare services, newborn's health, women's health, public health, maternal services
Citation: Cena L, Rota M, Calza S, Massardi B, Trainini A and Stefana A (2021) Estimating the Impact of the COVID-19 Pandemic on Maternal and Perinatal Health Care Services in Italy: Results of a Self-Administered Survey. Front. Public Health 9:701638. doi: 10.3389/fpubh.2021.701638
Received: 28 April 2021; Accepted: 18 June 2021;
Published: 16 July 2021.
Edited by:
Rahul Shidhaye, Pravara Institute of Medical Sciences, IndiaReviewed by:
Francesco Chirico, Catholic University of the Sacred Heart, ItalyVincent Setlhare, University of Botswana, Botswana
Copyright © 2021 Cena, Rota, Calza, Massardi, Trainini and Stefana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Loredana Cena, bG9yZWRhbmEuY2VuYUB1bmlicy5pdA==; orcid.org/0000-0002-3162-9237
 Loredana Cena
Loredana Cena Matteo Rota
Matteo Rota Stefano Calza
Stefano Calza Barbara Massardi3
Barbara Massardi3 Alice Trainini
Alice Trainini Alberto Stefana
Alberto Stefana