
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 24 June 2021
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.698106
Background: The Coronavirus disease 2019 (COVID-19) pandemic is considered a major global public health threat affecting across the life course and socioeconomic aspects of life. Global acceptance to an effective vaccine is the most anticipated resolution. This study aims to evaluate intent to be vaccinated among public in Saudi Arabia during the second wave of the COVID-19 pandemic.
Methods: A cross-sectional web-based study was designed in Saudi Arabia. Study participants (N = 658) were recruited through snowball sampling. The SurveyMonkey platform was used to record the response. Cross-tabulation was performed by participants' intention to vaccinate against COVID-19 virus with sociodemographic characteristics and respondents' risk perception toward COVID-19, trust in the healthcare system, and their history of vaccine hesitancy behavior. Multivariable logistic regression analysis was performed to compute the predictors of vaccination intention among the study participants.
Results: Six hundred fifty-eight participants completed the survey (females = 47.4%). Of the 658 participants, 351 (53.3%) have shown intent to be vaccinated. Five hundred nineteen (78.8%) of the participants were reported to be at high risk of COVID-19, and 307 (46.6%) were reported to trust the healthcare system in the country. The multivariable analysis shows respondents with a high-risk perception (OR: 2.27, 95% CI: 1.49–3.48); higher trust in the healthcare system (OR: 3.24, 95% CI: 2.32–4.61) was found to be the significant factor affecting the decision in acceptance of the COVID-19 vaccine in Saudi Arabia.
Conclusion: Participants reported high knowledge toward COVID-19 virus, and vaccine developments. About half (46.6%) of the study participants reported refusal/hesitancy toward the vaccine during the second wave of the pandemic in Saudi Arabia. The study highlighted that higher risk perception and higher trust in the healthcare system were found to be the main reasons for participants' intentions behind the vaccination.
During the preceding years 2019–2020, all the countries worldwide were affected by a novel severe acute respiratory syndrome coronavirus-2 named COVID-19, which became an international concern. By February 2021, the World Health Organization (WHO) has declared more than 108 M confirmed cases of COVID-19 and 2.3 M deaths all over 219 countries and territories (1). Numerous studies have shown concern for the second wave of COVID-19 (2, 3).
As vaccination is considered the most effective health intervention to prevent and control COVID-19, scientists worldwide competed to develop a safe and productive vaccine in record time. By November 2020, the German company BioNTech, in cooperation with the US company Pfizer, announced that their vaccine has a more than 90% success rate. The clinical trial analysis showed that this vaccine caused no severe side effects, resulting in rapid use across the world (1). In the middle of February 2021, WHO declared that at least seven different COVID-19 vaccines have been rolling out in other countries. Moreover, 200 additional vaccines are in development, of which more than 60 are in clinical outcome (1).
The Kingdom of Saudi Arabia (KSA) was one of the very first countries in the world to grant emergency use authorization to the BNT162b2 vaccine (4) and received the first batch of the COVID-19 vaccine by December 2020 (5). One month later, over one million people were registered on the local application “Sehhaty” to receive the vaccine (6). By April 15, the Ministry of Health announced that around three million people have taken the vaccine shot without any health complications. The COVID-19 vaccine is provided free of charge to all Saudi Arabia (Saudi and non-Saudi) inhabitants, and priority is given to those with chronic diseases, health practitioners, and individuals over 65 years of age (7). As per the WHO, in Saudi Arabia, from January 3, 2020, to May 20, 2021, there have been 436,240 confirmed cases of COVID-19 with 7,201 deaths. As of May 16, 2021, a total of 11,698,875 vaccine doses have been administered (8).
The acceptance of a vaccine is a critical stage in the success of the immunization programs to accomplish high vaccination rates within the general population. The acceptance of the vaccine depends largely on many factors such as the way people perceive the threat, the thrust on the healthcare system, the vaccine safety and efficacy, and the vaccine demand within the population (9, 10). Many studies on the acceptance and the confidence in the vaccines, mainly for the newly emerging infectious diseases, showed inadequate acceptance rates. For example, during the 2009 H1N1 pandemic, it has been demonstrated that in France, the acceptance rate of the vaccine was 17%; in America, 49.6%; in Australia, 43.9%; in the UK, 56.1%; and in Greece, the rejection rate of the vaccine 63.1% (11–14). A recent study conducted in Saudi Arabia to assess the prevalence of vaccine hesitancy or delay among the Saudi population showed that 36% of children are not vaccinated fully at their age (15). The study reported that children's parents believed vaccination was ineffective or unnecessary and thought that receiving a vaccine for diseases that are no longer common is insignificant (15).
A global survey of 19 countries reported that about 71.5% of participants would be very or somewhat likely to take a COVID-19 vaccine (16). A systematic review highlighted that several countries reported the lowest COVID-19 vaccine acceptancy, which includes Kuwait (23.6%), Jordan (28.4%), Italy (53.7), Russia (54.9%), Poland (56.3%), US (56.9%), and France (58.9%). In Hong Kong, China, the willingness to accept the COVID-19 vaccine was found to be 34.8% in the third wave vs. 44.2% during the first wave (17). A study conducted among the Middle Eastern population showed that 36.8% and 26.4% of the participants answered “No” and “Not sure” when asked if they would take the vaccine once it becomes available (18). In Saudi Arabia, a study was conducted before the new COVID-19 vaccine approval and authorization of the use by our research group and aimed to understand the public willingness of a future COVID-19 vaccine. The findings showed that a high proportion (64.7%) of the study participants demonstrated intention and desire to receive the vaccine (19). About half (46.7%) of the young adult population reported taking the COVID-19 vaccine if made mandatory in Saudi Arabia (20). Another study showed that 50.52% of healthcare workers were willing to have the COVID-19 vaccine. However, 50.29% intended to delay until the vaccine's safety is confirmed (21). However, the concrete rate of hypothetical vaccine acceptance might be much inferior to the acceptance rate after the development and authorization of vaccine use through a national immunization program. The present study was conducted to assess the COVID-19 vaccine acceptance among the Saudi population and determine the demographic characteristics that might impact the vaccine uptake during the second wave of the pandemic.
A cross-sectional survey was conducted on the acceptability of a COVID-19 vaccine among the public between January 2021 and March 2021 in Saudi Arabia. The OpenEpi 3.01 (updated on April 2013) was used for the calculation of sample size considering the anticipated proportion of COVID-19 vaccine acceptance of 40% obtained from the recent studies (19–21), with absolute precision of 5 and 99% confidence interval. The sample size was estimated to be 637. Study participants were recruited through snowball sampling. Invitations to participate in the study were distributed to the respondents via Email and social media such as Twitter, Facebook, and the WhatsApp communication platform of the primary contacts of the study team and requested to transmit further for its maximum reach. Considerations were made to recruit the participants across major geographic regions of the Kingdom.
The development and validation of survey questionnaires were reported elsewhere (19). Briefly, a bilingual self-reported format questionnaire was developed using SurveyMonkey. Informed consent was obtained from all participants (18 years or older and currently living in the KSA). Detailed responses that were recorded further were only those who provided informed consent to complete the survey.
The first section of the questionnaire includes information on sociodemographic characteristics of study participants such as age, gender, marital status, education level, place of residency, occupation sector, and socioeconomic status. The second section collects information on the history of exposure to COVID-19 (travel with a confirmed COVID-19 patient, staying with a confirmed COVID-19 patient); risk perception; concerns to be affected by COVID-19; and trust in the healthcare system. The third section of the questionnaire records information on knowledge about the development of the COVID-19 vaccine and intention to be vaccinated against the COVID-19 virus.
The key outcome measures of the study were to know the respondents' intention toward acceptance of the COVID-19 vaccination. The responses were recorded in a three-point Likert scale (Yes, No, and Not sure). Descriptive statistical analysis was performed by doing cross-tabulation of demographic characteristics with the primary response variable. The variable “age” was converted into three categories: 18–25 (the reference category), 26–35, and above 35 years. Gender was reported in two categories: male and female. Marital status was presented in two categories: married and single (including widowed and divorced). Education status was captured into four categories: high school, diploma, undergraduate, and postgraduate and above. Participants' socio-economic status (SES) was reported into three categories: low, medium, and high. The family size was reported into two categories: ≤ 5 and ≥6. The place of residence was captured numerically, covering all 13 administrative regions in the KSA (Riyadh, Mekkah, Almadina Almonawra, Qaseem, Eastern Region, Aseer, Tabouk, Hail, Northern Borders, Jazan, Najran, Albaha, and Aljouf) and further grouped into five categories: East, West, North, South, and Central.
We performed both simple and multivariable logistic regression analyses to compute the odds ratio (OR) and a 95% confidence interval (CI). Chi-squared tests were performed for bivariate analysis (cross-tabulation) between the outcome variable (intend to vaccinate) and all explanatory variables. Inference on the significant association was considered with a two-tailed p ≤ 0.05. STATA 15.0 software (StataCorp LP, College Station, TX, USA) was used for all statistical analyses.
Ethical approval was granted for the study by the institutional Research Ethics Committee (SEUREC-CHS20118) of Saudi Electronic University, Riyadh, Kingdom of Saudi Arabia, and consent was taken before participation in the study. Anonymized data was used for analysis, interpretation, and reporting.
Table 1 shows the demographic characteristics of the study participants. Of the 658 participants, 286 (43.4 %) were aged 26–35 years; 312 (47.4%) were female; and 326 (49.5%) were married respondents. The majority of respondents belonged to the central provinces, 288 (43.7%), followed by western 200 (30.3%), and 170 (25.8%) eastern provinces in Saudi Arabia. The most common education level was undergraduate and below (80.2%), and the majority (n = 413) were employed in governmental or private sectors or self-employed. Only 15.19% worked in the healthcare system (hospitals, clinics, and laboratory testing and diagnosis). High responses were from respondents living in large-sized families (six children and above) (66.4%) compared to low-sized families (five children and below) (37.4%). The study has high participation of respondents with medium social-economic status (81.4%).
Table 2 presents contact history with COVID-19 patients, risk perception, and vaccination history of the study respondents. In terms of contact history with COVID-19 patients, a low proportion of respondents stated that they traveled (6.84%) or stayed (19.00%) in the same environment with a confirmed COVID-19 patient. The respondents had a high-risk perception of COVID-19 (78.88%) and agreed that they are concerned and afraid of getting the coronavirus (79.78%). A proportion of 46.6% of the respondents reported high trust in the healthcare system in Saudi Arabia to manage the current situation related to COVID-19, but 53.44% showed low trust in the healthcare system. Regarding the history of vaccine hesitancy, 81.0% disagreed with receiving one or more types of vaccine if there were doubts about its efficacy and safety, while 18.99% refused to accept any vaccination and considered it without any benefit to their health and their children's health. A proportion of 14.28% declared that they postponed a vaccine even if their physician recommended it.
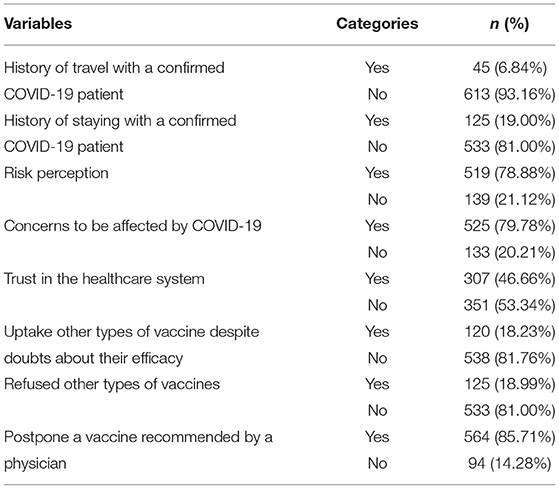
Table 2. Contact history with COVID-19 patients, risk perception, and vaccination history of the study respondents (N = 658).
Table 3 depicts the bivariate analysis for the association between socio-demographic characteristics and intention to COVID-19 vaccination. We conducted a cross-tabulation analysis to examine the distribution of intentions to uptake the COVID-19 vaccine according to the sociodemographic characteristics of the respondents. In general, 53.35% (n = 351) of the respondents declared positive intention to update the COVID-19 vaccine, while 46.65% (n = 307) responded “No or Not sure” to receive the vaccine. The cross-tabulation analysis using the chi-square test for binary or categorical variables showed that a statistically significant number of married respondents (53.85%) declared a strong intention to receive the COVID-19 vaccine when compared to the unmarried respondents (46.55 %) (p = 0.02). Moreover, by education levels, a significantly higher proportion of respondents who expressed an absolute intent to vaccinate included respondents with undergraduate education (45.30%) or postgraduate respondents (24.22%) (p = 0.01). There was also significant intention to update the COVID-19 vaccine among highly sited families with six children or more (59.26%) when compared to families with less than five children (40.74%) (p = 0.06). Respondents aged between 26 and 35 years (41.03%), male respondents (54.99%), and respondents with medium socioeconomic status (82.62%) also declared strong and definite intention to vaccination when compared to the other categories from the same class; however, these differences did not show any statistical significance (p > 0.05).
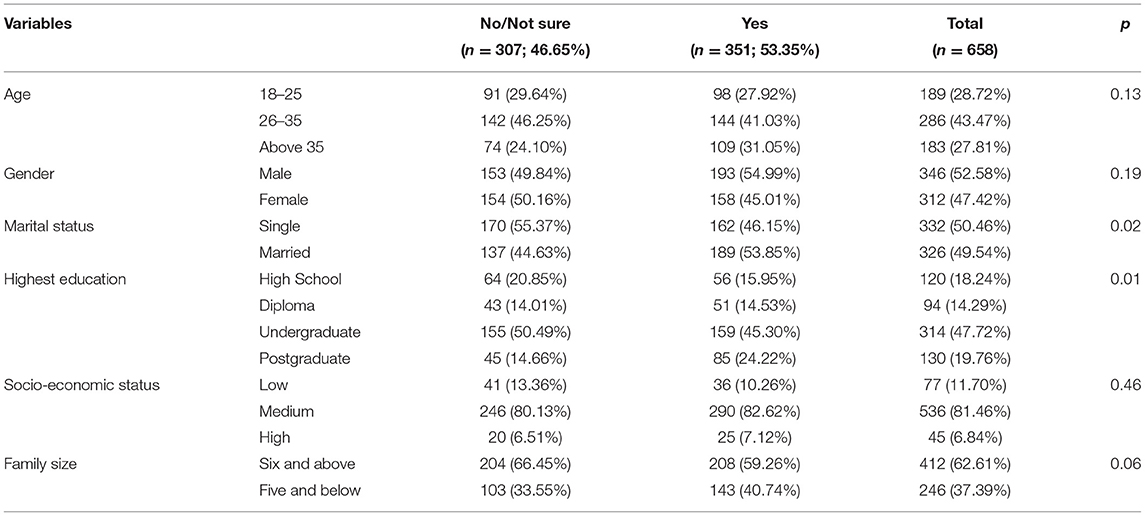
Table 3. Bivariate analysis for association between demographics characteristics and intention to COVID-19 vaccination (N = 658).
Table 4 shows the bivariate analysis for the association between intention to COVID-19 vaccination with vaccine knowledge, trust, and confidence in the coronavirus vaccination among the study respondents. Regarding the knowledge about the development of the COVID-19 vaccine, 76.07% of respondents with high levels of awareness confirmed high trust and confidence in the vaccination. In comparison, 54.07% showed no preference for the COVID-19 vaccine despite their knowledge about the importance and development of the vaccine (p < 0.001). When the respondents were asked if they trust the healthcare system in Saudi Arabia, 66.38% responded “Yes,” which could impact positively the trust and confidence in the COVID-19 vaccine (p < 0.001) when compared with respondents who showed no trust in the healthcare system (38.4%).
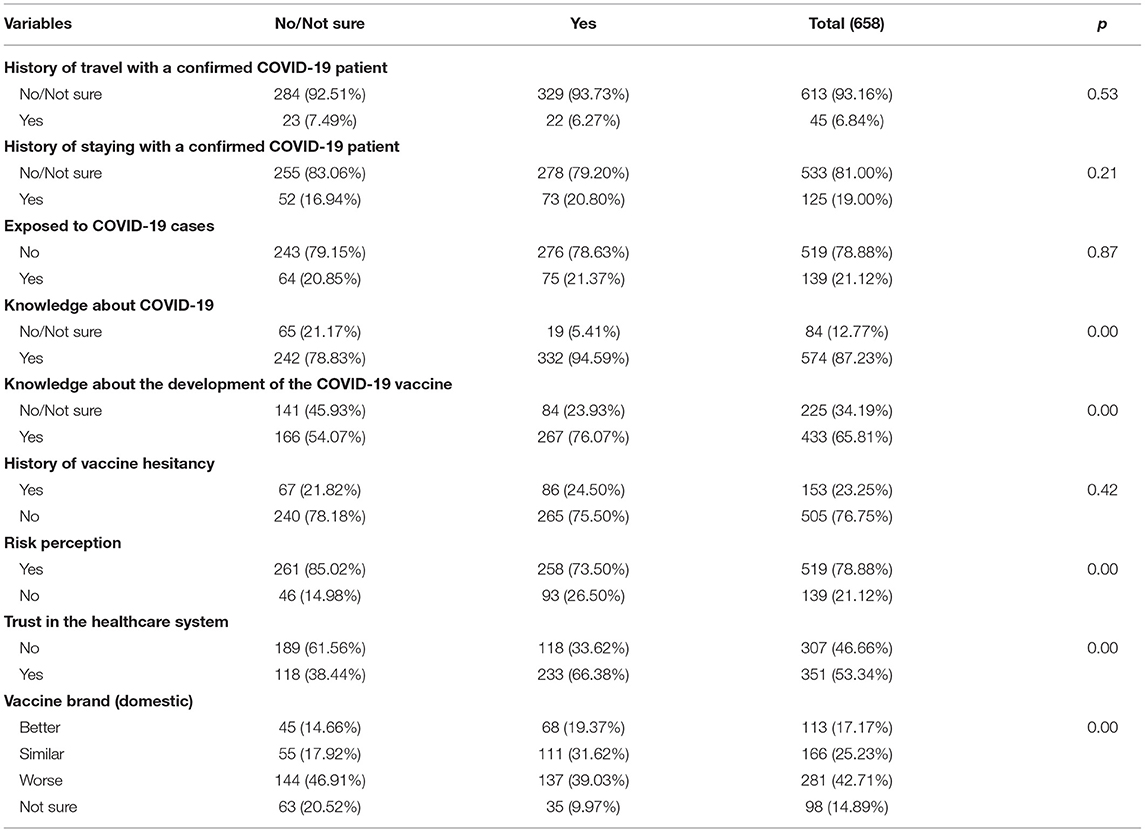
Table 4. Bivariate analysis for association between intention to COVID-19 vaccination with vaccine knowledge, trust, and confidence among the study respondents (n-658).
Moreover, a significant proportion thought that domestic vaccines are worse than imported vaccines (46.9%), affecting their trust in the COVID-19 vaccination, while only 19.37% trusted the domestic vaccines. There was also a statistically significant difference between respondents with a high-risk perception of the COVID-19 (85.02%) but declared no trust and confidence to receive the vaccine when compared to 73.50% of respondents with a high perception of the risk and who showed significant faith and enthusiasm to the COVID-19 vaccine (p < 0.05). The history of vaccination hesitancy, the history of contact with confirmed COVID-19 patients, and the exposure to the COVID-19 were without any impact on the trust and confidence in the COVID-19 vaccine (p > 0.05).
Table 5 shows a multivariable logistic regression analysis of the factors influencing the COVID-19 vaccine uptake among study participants. As the respondents were divided into two groups according to their intention to vaccinate (53.35% “Yes” vs. 46.65% “No or Not sure”), a multivariable logistic regression analysis was then conducted between these two groups to identify factors that may impact the acceptance or refusal of the vaccine uptake. Basic socio-demographic characteristics, history of vaccine hesitance, risk perception, and trust in domestic vaccinations were studied, with the refusal group of the vaccine considered as the reference group (Table 5). Respondents with a high perception of vaccination benefit in reducing the spread of the disease and control the risk of the COVID-19 are showing high intention to be vaccinated (OR: 2.27, 95% CI: 1.49–3.48). The trust in the healthcare system and confidence in its role to manage the situation in Saudi Arabia and to prevent and control the COVID-19 (OR: 3.24, 95% CI: 2.32–4.61) was found to be the significant factor affecting the decision-making of the respondents regarding the acceptance of the COVID-19 vaccine.

Table 5. Multivariable regression analysis of the influencing factors on the COVID-19 vaccine uptake among study participants.
In this study, we aimed to determine the acceptability and hesitancy toward vaccination during the second wave of the COVID-19 pandemic in Saudi Arabia, and the factors associated with these issues. We found that nearly 53.3% of adults in Saudi Arabia would be willing to receive a COVID-19 vaccine vs. 64.7% during the first phase of the pandemic (19). Socio-demographic factors, such as being married and higher educational level, were found to be associated with vaccine acceptance. Higher risk perception and higher trust in the healthcare system were found to be the significant predictors in explaining participants' intentions behind the vaccination. Our findings represent one of the first estimates of the acceptance of a COVID-19 vaccine in Saudi Arabia during the second wave of the COVID-19 pandemic.
Even though this study was conducted between January and March 2021 when the second wave of COVID-19 was approaching and the country was ready with vaccine to immunize the community, only 53.3% of the participants intended to be vaccinated. This percentage is comparably lower than that in our previous finding when there was no vaccine available in the country (19). Still, the community in Saudi Arabia has a higher rate of acceptance toward the vaccine in comparison to countries like Kuwait (23.6%) and Jordan (28.4%) (16). Even the general public had a higher acceptability to the vaccine than healthcare workers in Saudi Arabia (21). The healthcare workers reported 50.52% willing to have the COVID-19 vaccine in Saudi Arabia (21). The young adults have a lower acceptability (48.0%) of the vaccine in Saudi Arabia, as reported in a recent study (20). A study conducted among working people in Hong Kong, China, also reported a lower rate of intention in vaccination between the first wave (44.2%) and the third wave (34.8%) (17). The study highlighted that concerns over vaccine safety was found to be the factor behind the willingness to accept the COVID-19 vaccine (17).
Our study also highlighted that public trust on the healthcare system and risk perception toward the virus were the significant predictive behavior in accepting the vaccine, as stated in previous studies (20–24).
The strength of our study includes an appropriate sample size and recruitment of study participants across the country. The use of over-the-air platforms to recruit participants during the restricted environment of COVID-19 is a great strength. The major limitation of this study includes the sample recruitment and the data collection strategy; we used a snowball sampling which may have been overestimated due to selection bias. The outcome of this study may not be used as a yardstick to depict the perception of the Saudi Arabians as the study was conducted among social media users and those more educated to access the questionnaire over the air, leaving chuck of other citizens. Local COVID-19 information is also missing; sometimes people respond fast when they find the fear of spreading the disease. The urban rural differences in COVID-19 vaccine acceptance was not accounted in this study. This is a key socio-demographic determinant in vaccine hesitancy as reported by numerous studies. The study also did not record any adverse events including the psychological factors, which may be one of the causes for poor response in acceptance of the COVID-19 vaccination. Despite these limitations, to the best of our knowledge, this is the first study to report the current COVID-19 vaccine acceptance in the country while there is a vaccine available and the second wave of the pandemic is devastating the community.
This study depicts that the study participants have good knowledge of COVID-19 and vaccine developments. However, the percentage of participants with vaccination intention was only 53.3% during the second wave of the pandemic. The study highlighted that higher risk perception and higher trust in the healthcare system were found to be the main reasons for participants' intentions behind the vaccination. Policymakers should prioritize these concerns by creating awareness among the community.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethical approval was granted for the study by the institutional Research Ethics Committee (SEUREC-CHS20110) Saudi Electronic University, Riyadh, Kingdom of Saudi Arabia, and consent was taken before participation in the study. Anonymized data was used for analysis, interpretation, and reporting. The patients/participants provided their written informed consent to participate in this study.
MA-M conceptualized the study, conducted research, provided research materials, and collected and organized data and also contributed substantially for writing the manuscript. BP and SE analyzed and interpreted data and written the initial original draft of article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
2. Nicholson P, Krings T. Time for a “Second Wave” of COVID-19 data. Am J Neuroradiol. (2021) 42:262–3. doi: 10.3174/ajnr.A7020
3. Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. (2020) 395:1321–2. doi: 10.1016/S0140-6736(20)30845-X
4. Barry M, BaHammam A. COVID-19 vaccine in the Kingdom of Saudi Arabia: a true operation warp speed. J Nat Sci Med. (2021) 4:92–8. doi: 10.4103/jnsm.jnsm_8_21
5. Ministry of Health Saudi Arabia. MOH News-Al-Rabiah: Kingdom Receives First Batch of COVID-19 Vaccine (2020).
6. Ministry of Health Saudi Arabia. MOH News-MOH: Over A Million People Registered to Receive COVID-19 Vaccine (2020).
7. Ministry of Health Saudi Arabia. MOH News-MOH: COVID-19 Vaccines Are Available in all Regions of the Kingdom (2020).
8. World Health Organization. WHO Health Emergency Dashboard. (2021). Available online at: https://covid19.who.int/region/emro/country/sa.
9. Wilson K, Nguyen H, Henningsen B. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. (2011) 4:197–207. doi: 10.2147/IDR.S23174
10. Yang Y, Peng F, Wang R, Guan K, Jiang T, Xu G, et al. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmun. (2020) 109:102434. doi: 10.1016/j.jaut.2020.102434
11. Maurer J, Uscher-Pines L, Harris KM. Perceived seriousness of seasonal and A (H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among US adults: does the source of information matter? Prev Med. (2010) 51:185–7. doi: 10.1016/j.ypmed.2010.05.008
12. Schwarzinger M, Flicoteaux R, Cortarenoda S, Obadia Y, Moatti JP. Low acceptability of A/H1N1 pandemic vaccination in French adult population: did public health policy fuel public dissonance? PLoS ONE. (2010) 5:e10199. doi: 10.1371/journal.pone.0010199
13. Seale H, Heywood AE, McLaws ML, Ward KF, Lowbridge CP. Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis. (2010) 10:1–9. doi: 10.1186/1471-2334-10-99
14. Sypsa V, Livanios T, Psichogiou M, Malliori M, Tsiodras S, Nikolakopoulos I, et al. Public perceptions in relation to intention to receive pandemic influenza vaccination in a random population sample: evidence from a cross-sectional telephone survey. Eurosurveillance. (2009) 14:19437. doi: 10.2807/ese.14.49.19437-en
15. Alsubaie SS, Gosadi IM, Alsaadi BM, Albacker NB, Bawazir MA, Bin-Daud N, et al. Vaccine hesitancy among Saudi parents and its determinants. Saudi Med J. (2019) 40:1242–50. doi: 10.15537/smj.2019.12.24653
16. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. (2020) 27:225–28. doi: 10.1101/2020.08.23.20180307
17. Wang K, Wong EL, Ho KF, Cheung AW, Yau PS, Dong D, et al. Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: repeated cross-sectional surveys. Vaccines. (2021) 9:62. doi: 10.3390/vaccines9010062
18. Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. (2021) 9:632914. doi: 10.3389/fpubh.2021.632914
19. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. (2020) 13:1657–63. doi: 10.2147/JMDH.S276771
20. Almaghaslah D, Alsayari A, Kandasamy G, Vasudevan R. COVID-19 vaccine hesitancy among young adults in Saudi Arabia: a cross-sectional web-based study. Vaccines. (2021) 9:330. doi: 10.3390/vaccines9040330
21. Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med.(2021) 8: 644300. doi: 10.3389/fmed.2021.644300
22. Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. (2021) 10:2052–61. doi: 10.1159/000514636
23. Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy' among University students in Italy during the COVID-19 pandemic. Eur J Epidemiol. (2020) 35:781–3. doi: 10.1007/s10654-020-00670-z
Keywords: vaccine acceptance, vaccine hesitancy, Saudi Arabia, risk perception, trust, second wave of COVID-19
Citation: AL-Mohaithef M, Padhi BK and Ennaceur S (2021) Socio-Demographics Correlate of COVID-19 Vaccine Hesitancy During the Second Wave of COVID-19 Pandemic: A Cross-Sectional Web-Based Survey in Saudi Arabia. Front. Public Health 9:698106. doi: 10.3389/fpubh.2021.698106
Received: 20 April 2021; Accepted: 24 May 2021;
Published: 24 June 2021.
Edited by:
Chiara de Waure, University of Perugia, ItalyReviewed by:
Obasanjo Afolabi Bolarinwa, University of KwaZulu Natal, South AfricaCopyright © 2021 AL-Mohaithef, Padhi and Ennaceur. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed AL-Mohaithef, bS5hbG1vaGFpdGhlZkBzZXUuZWR1LnNh; Soukaina Ennaceur, cy5lbm5hY2V1ckBzZXUuZWR1LnNh
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.