
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health, 28 May 2021
Sec. Occupational Health and Safety
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.666442
This article is part of the Research TopicOccupational Medicine: Disease Risk Factors and Health PromotionView all 22 articles
 Luisa Dudine1*†
Luisa Dudine1*† Claudia Canaletti1†
Claudia Canaletti1† Fabiola Giudici2†
Fabiola Giudici2† Alberta Lunardelli3†
Alberta Lunardelli3† Giulia Abram1‡
Giulia Abram1‡ Ingrid Santini1‡
Ingrid Santini1‡ Vera Baroni1‡
Vera Baroni1‡ Marta Paris1†
Marta Paris1† Valentina Pesavento3§
Valentina Pesavento3§ Paolo Manganotti4§
Paolo Manganotti4§ Federico Ronchese5‡
Federico Ronchese5‡ Barbara Gregoretti6§
Barbara Gregoretti6§ Corrado Negro7§
Corrado Negro7§The aim of this study was to investigate the correlation between psychological distress and taste and sense of smell dysfunctions on healthcare workers (HCW) who contracted the COVID-19 infection in the midst of the disease outbreak. Reports of sudden loss of taste and smell which persist even after recovery from COVID-19 infection are increasingly recognized as critical symptoms for COVID-19 infections. Therefore, we conducted a cross-sectional study on COVID-19 HCW (N = 104) who adhered to respond to a phone semistructured interview addressing the virus symptoms and associated psychological distress. Data were collected from June to September 2020. Findings confirm the association between experienced taste/olfactory loss and emotional distress and suggest that dysfunctions of taste and smell correlate positively with anxiety and depression. Furthermore, their psychological impact tends to persist even after the recovery from the disease, suggesting the need for appropriate psychological interventions to prevent people from developing more serious or long-lasting psychological disorders and, as far as HCW, to reduce the risk of work-related distress.
In December 2019, an outbreak of pneumonia with unknown origin began in China's Hubei Province raising global health concerns due to the ease of transmission. After numerous studies conducted around the world, a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified and was called “coronavirus-19” (COVID-19). For the National Institutes of Health (1), several symptoms characterized this infection, ranging from asymptomatic/mild symptoms to severe illness and death. In particular, COVID-19 symptomatology included cough, fever, and shortness of breath, as well as weakness, malaise, respiratory distress, muscle pain, sore throat, loss of taste, and/or smell (2–8).
In countless studies (9–14), smell dysfunction has been demonstrated as one of the first among other neurologic manifestations of both hospitalized and mild COVID-19 patients (15).
World's pandemics are usually associated with adverse mental health consequences as reported in different studies (16–22). According to Rajkumar (23), first evidence suggests that symptoms of anxiety and depression and self-reported distress are common psychological reactions to the COVID-19 pandemic and may be associated with disturbed sleep.
However, studies on determinants of psychological distress have rarely focused on the clinical manifestation of the SARS-COV-2.
During the first wave of COVID-19 pandemic, a psychology crisis unit (coworked with the Occupational Medicine Service) kept in touch by phone calls with HCW infected with COVID-19 to prevent psychological distress, and observed an association between psychological distress and olfactory/taste dysfunctions.
Therefore, our primary aim was to determine the psychological impact of COVID-19 symptomatology and, more specifically, whether taste/olfactory dysfunctions were associated with more emotional disorders as compared with subjects not experiencing these sense symptomatologies. Indeed, it is well-known that taste and olfactory sensory dysfunctions/loss represent an early manifestation of infection (7, 10, 11, 24) that can have a negative impact on emotional well-being and quality of life (25) people with anosmia often refer feelings of loneliness, fear, and depression as well-difficulties concerning social and sexual relationship, concerns about personal hygiene. Taste disturbance or loss can also cause subjective discomfort and have a negative impact on nutrition, indeed depression subsequent to gustatory dysfunction has been described (26). In addition, in one study, Weiffenabch and Bartoshuk (27) reported how dysfunction of taste and smell can amplify psychological distress. Further analyses concerned the prevalence of smell and taste dysfunctions, how these symptoms were distributed within our sample, and at what stage of the disease they tended to emerge. Because the mental status of health professionals directly affected by the COVID-19 epidemic to our knowledge has been under-addressed, we focus on a sample of HCW who contracted the infection during the first wave of COVID-19. The purpose of the study will also investigate the distress and psychological needs and serve to better target and plan support services for healthcare professionals working in COVID-19 centers, especially focusing on work-related distress. The HCW normally represent an important sector, actually overexposed to COVID-19 consequences, that needs to be further explored and protected. This study represents a started point for future researches.
A no-profit study representing a cross-sectional investigation was conducted from June to September 2020 according to the local Ethical Committee (N.051/2020). HCW of the Trieste area in Northern Italy who contracted the COVID-19 infection in the midst of the disease outbreak were interviewed by phone by psychologists of the same healthcare service. The presence of infection was determined by the positive result of molecular swabs as established by the World Health Organization (28).
One hundred twenty-three HCW were involved in the study by occupational doctors from an Italian local network of hospitals. However, the final sample of subjects who adhered to participate to the study was composed by a total of 104 subjects (women N = 71 and men N = 33) between the ages of 23 and 65 years (mean = 43) who completed the interview and the questionnaires. At the time of the interview, participants were COVID-19 positive, COVID-19 negative with symptoms, and COVID-19 negative without symptoms (see Table 1). The inclusion criteria were age >18–<70; contraction of COVID-19 infection; good understanding of the Italian language; and those who have expressed their favorable consent to participate in the study. The exclusion criterion was inability to cooperate due to high distress at the time of the interview evaluated by the psychologist.
Subjects were reached by phone and administered a semistructured interview which involved questions concerning clinical symptoms of COVID-19 including taste and smell problems, the distress thermometer (29), and the Hospital Anxiety and Depression Scale (HADS) (30, 31). The distress thermometer (DT) is a simple self-reported tool that screens for symptoms of distress and has been found valid in measuring psychological distress in different countries, cultures, and pathological populations as confirmed by different studies (32–34). It measures the stress variable on a 0- (no distress) to 10-rating (extreme distress) scale. The DT can be considered a continuous variable, with an established cutoff of 5 indicating experience of significant distress and need for attention or can be employed to classify people with low (0–3), moderate (4–5), and high levels (>6) of stress, as reported by Grassi et al. (35).
The HADS questionnaire is a 14-item scale designed to detect emotional disturbances in non-psychiatric patients (31) in hospital settings by screening for the two most frequent disorders: anxiety and depression. Each item is rated on a 4-point scale, ranging from 0 to 3, with 3 indicating higher symptom frequency. Two separate subscales identifying anxiety and depression symptoms can be obtained as well as a total score of psychological state. Total scores for each subscale range from 0 to 21, categorized as: normal (0–7), borderline (8–10), and present disorder (≥11).
In the present study, the DT was proposed to participants considering two different periods of time: (1) COVID-DT which refers to the stress perceived during the early illness and (2) Current-DT which indicates the level of stress perceived at the time of the interview about COVID-19. The HADS score refers only to the time of the interview.
Taking into account the primary objective of the study, namely the association between olfactory and gustatory dysfunctions and a state of distress, the sample size available (n = 104) can be considered sufficient to determine a difference of 0.62 (medium Cohen's d effect size) in the outcome evaluation scale (DT) assuming a power of 80% (1-β) and a level of significance of 5% (α) (two-tailed student t test).
Categorical variables were expressed by frequencies and percentage, while continuous variables were expressed by mean [standard deviation (SD)] or median [range (min-max)], as appropriate according to data distribution verified through Shapiro Wilk normality test. Student's t test or Mann-Whitney test were used to compare continuous variables (age, DT, HADS scores) with respect to groups of interests. Independent Chi-square test or Fischer exact test (when appropriate) were performed to evaluate and investigate associations among categorical variables. Paired Wilcoxon test compared DT values perceived by the patients during COVID-19 infection with current distress. Spearman linear correlation coefficients were calculated in order to verify correlation among different psychological scores. Multivariate linear regression models were performed to identify risk factors for psychological disorders and results reported as Beta coefficient regression with 95% confidence interval. All the statistical tests were two sided, and statistical significance was defined as p-value < 0.05. Analyses were performed using statistical software R, v. 4.0.3, 2020.
Subjects' response analysis on COVID-19 symptoms revealed that only one person was asymptomatic and three workers required hospitalization, while the majority of the sample experienced mild to moderate symptomatology with an average of 7 symptoms (60.2%). The most frequent symptoms were fatigue (83%), olfactory dysfunctions (82%), and taste dysfunctions (77%) Women reported dysfunctions significantly greater than men in smell (89 vs. 67%, p = 0.007), taste (84 vs. 61%, p = 0.008), and sore throat (41 vs. 21%, p = 0.05) (see Table 1). The only correlation between age and type of symptom was found for numbness: the presence of the symptom is associated with a greater age (medians 50 vs. 43, p = 0.03).
The characteristics of taste and smell dysfunctions have been analyzed more in depth (see Table 2): temporal onset in most of the sample is, on average, 6 days after the beginning of other symptoms (smell in 62% of the group and taste in 68%); only for a few of them these disorders emerged before other symptoms (in 13% of subjects, both dysfunctions appeared on an average of 5 days before other complaints). The type of dysfunction has also been explored, considering both sensory alteration, loss, or reduction. Anosmia and ageusia are the most frequent reported dysfunction particularly in case of smell (nearly 80% olfaction vs. 51% of taste, p = 0.004). No significant differences have been found in the rate of taste/smell resolution at the time of the interview (p = 0.18), though it resulted higher in case of taste problems (67% of taste vs. 52% of smell) and persistence of sensory disorders was similar for both senses (taste 5% and smell 7%).
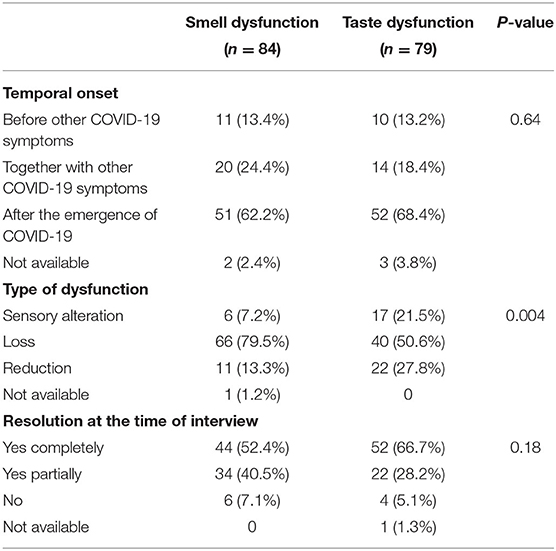
Table 2. Analysis of the characteristics of smell and taste dysfunctions: temporal onset, type of dysfunctions, and resolution.
At the time of the interview, the most frequent symptoms in the “COVID-19 negative with symptoms” group (n = 38), remained “smell dysfunction” (n = 21, 55%), and “taste dysfunction” (n = 12, 32%).
As far as the emotional state reported by subjects, the DT showed a median score of 7 out of 10 when referring to the period of the COVID-19 illness. Gender and age were not associated with DT at the period of COVID-19 positivity (COVID-DT). Eighty-six percent of the sample declared moderate to high distress, and the most frequent manifestations of psychological symptoms were anxiety, irritability, negative mood, and a sense of loneliness (see Table 3). In addition, COVID-DT correlates significantly with the presence of some COVID-19 symptoms (fatigue, diarrhea, taste loss) and patients with more than seven symptoms (median value of symptom prevalence) showed higher levels of distress (see Table 3). While the loss of smell does not appear to be related to greater distress, in patients who have lost the taste, the level of distress is significantly higher in the period of illness. This result remained confirmed in the multivariate analysis (Beta = 1.58, 95% CI:0.15; 3.00, p = 0.02, see Supplementary Table 1).
Subjects' psychological state has been specifically investigated also through the HADS. Answers to the HADS questionnaire revealed the presence of anxiety and depression in a small percentage of cases at the time of the interview (score ≥11 <13% for anxiety and 6% for depression). Age and gender were not associate with HADS scores.
Looking at the relationship between the scores on the HADS scale and the loss of taste/smell, anxiety results to be significantly higher in patients with alterations in both senses than in subjects without these disorders. On the other hand, subjects who report loss of taste constantly refer also symptoms of depression, while in case of smell loss there is only a tendency, though not significant, to report more depressive symptoms (see Tables 4a,b,c). However, in multivariate analysis, the only factor associated at the limit of significance, with anxiety/depression disorders was sex: men tend to suffer less from these disorders than women (see Supplementary Tables 2, 3).
To complete the analyses of subjects' psychological state, results from the two administration of the DT (i.e., COVID-TD and Current-DT) have been compared, as well as the HADS total score with the Current-DT. As shown in Table 5, all psychological distress scales were correlated. In particular, at the Current-DT, subjects gained scores significantly lower than those obtained in the COVID period (median DT 4 and 7, respectively, p < 0.001) even though 53 subjects (51%) reached scores of clinical interest (DT ≥4: moderate and high distress). A strong association has also been found between the CurrentpDT and the HADS questionnaire: 86% of subjects who reached a high HADS total score (HADS >13) have also gained a critical Current-DT score (DT >5), while only 29% of subjects with lower HADS scores (HADS <13) have an high DT score (p < 0.001) (see Supplementary Table 4). Accordingly, results from the administration of HADS confirm that 30 out of the all cohort (29%) would require clinical psychological intervention as shown by their overall HADS score (≥13).
This study evidences that smell and taste dysfunctions in subjects with mild to moderate COVID-19 symptoms are associated with higher levels of psychological distress compared to those not experiencing taste and smell dysfunctions [as observed by (25, 36)]. Anxiety and depressive symptoms are the most frequent responses, even though depression appears to be higher in relation to ageusia with respect to anosmia. Indeed, it is well-known that olfactory and taste sensory loss can have a negative impact on emotional well-being and quality of life, leading to feelings of loneliness, fear, and depression, as well as difficulties concerning social/sexual relationships (25, 36). Since taste and smell have always been a fundamental need in evolution and survival, psychological effects can be easily expected (25, 36–38). Consistent with other findings [e.g., (39)], women were more frequently affected by smell and taste disorders compared with men.
The COVID-19 pandemic issues such as the high risk of infection and reinfection, inadequate protection from contamination, overwork, frustration (i.e., witnessing death and feeling powerless over the levels of patient death, the delivery of patient care), discrimination, isolation, patients with negative emotions, lack of contact with families, exhaustion, the incapacity of healthcare systems to respond to the increased demand (40–43) play an important role in patients' emotional experience, the co-existence of COVID-19 symptoms however may intensify their reactions and for the most induce anxiety disorders. In addition, even when people are healed, they continue to experience high emotional distress, especially because they are worried of getting sick again. In accordance with Lima et al. (44) and Duan and Zhu (45), this suggests the need for appropriate psychological interventions under pandemic conditions to prevent people from developing more serious or long-lasting psychological disorders and, as far as HCW, to reduce the risk of work related distress (42, 46–49).
The study has some limitations. Data analysis was retrospective and did not fulfill the criteria of a randomized controlled study. Indeed, it is possible that individuals who adhered to be interviewed and completed the questionnaires were those who experienced greater psychological distress during the pandemic or who are simply more interested in psychological factors and implications. Another limitation might pertain the validity of the selected tools to investigate emotional distress related to the COVID pandemics. The DT and the HADS have been chosen as they are among the most widely used tests for screening and evaluating distress associated with organic diseases; however, they are not specifically designed for assessing emotional reactions during epidemics and/or pandemics, or for detecting their evolution over time as the pandemic continues; in addition, responses of COVID-DT can be influenced by recall bias. Finally, individuals' stress intensity has not been evaluated considering the duration of taste and smell disorders but taking into account only their presence or absence at the time of the interview. This aspect certainly deserves attention and could be investigated in-depth in future studies.
Anosmia and dysgeusia in people infected with COVID-19 are confirmed to increase psychological distress. Smell and taste dysfunctions can amplify psychological distress, and depressive symptoms are mostly associated with the loss of taste and tend to persist even after resolution of symptoms and disease. In this study, HCW reported high rates of emotional distress associated with COVID-19 infection and taste and smell dysfunctions. This highlights the importance of developing a systematic approach to identify at-risk individuals to prevent the development of more serious or long-lasting psychological disorders. Psychological interventions targeting HCW who contracted the COVID-19 infection, should be designed considering the symptom effects and job reintegration, which should take into account anxiety and depression experienced by workers who became ill. Interventions to benefit HCW, such as those suggested in the literature of psychological support, CBT, self-help strategies, and others, could be targeted to COVID-19 psychological effects. As well as the importance of collaboration in health care provider support services between occupational doctors, occupational psychologists, and clinicians to study work-related risks.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Comitato Etico Unico Regionale ARCS- FVG Nr. 0000611-P del 23/06/2020. The patients/participants provided their written informed consent to participate in this study.
LD was the main author and lead researcher. CC and AL assisted in the conception of the research, recruitment of subjects, collection of data, and contributed to the writing-up of the manuscript. FG carried out statistical analyses of results and contributed to interpretation of the final conclusions. GA, IS, VB, and MP helped in the recruitment of subjects and carried out the interviews. VP, PM, FR, BG, and CN supervised the project and discussed the findings of this work. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are grateful to Massimo Bovenzi and Alessandra Guglielmi for their diligent proofreading of the manuscript. We would like to thank also Daria Ghersetti, Sabrina Fossella, Maria Grazia Giacchin, Filomena Vella, Franco Bruni, Milena Pascotto, Francesca Valencak, and Luca Ianza for their help with health workers and interviews. Also, we thank Roberto Miceli, Andrea Miani, and Ottavia Spadola for support in the review.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.666442/full#supplementary-material
1. COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines (2019). National Institutes of Health. Available online at: https://www.covid19treatmentguidelines.nih.gov/ (accessed December 17, 2020).
2. Chow EJ, Schwartz NG, Tobolowsky FA, Zacks RLT, Huntington-Frazier M, Reddy SC, et al. Symptom screening at illness onset of health care personnel with sars-cov-2 infection in king county, Washington. JAMA. (2020) 323:2087. doi: 10.1001/jama.2020.6637
3. Clemency BM, Varughese R, Scheafer DK, Ludwig B, Welch JV, McCormack RF, et al. Symptom criteria for COVID-19 testing of heath care workers. Acad Emerg Med. (2020) 27:469–74. doi: 10.1111/acem.14009
4. Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili S.-M., et al. A comprehensive review of COVID-19 characteristics. Biol Proced Online. (2020) 22:1–10. doi: 10.1186/s12575-020-00128-2
5. Gengler I, Wang JC, Speth MM, Sedaghat AR. Sinonasal pathophysiology of SARS-CoV−2 and COVID−19: a systematic review of the current evidence. Laryngoscope Investig Otolaryngol. (2020) 5:354–9. doi: 10.1002/lio2.384
6. Gilani S, Roditi R, Naraghi M. COVID-19 and anosmia in Tehran, Iran. Med Hypotheses. (2020) 141:109757. doi: 10.1016/j.mehy.2020.109757
7. Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Oto-Rhino-Laryngology. (2020) 277:2251–61. doi: 10.1007/s00405-020-06024-5
8. Villalba NL, Maouche Y, Ortiz MBA, Sosa ZC, Chahbazian JB, Syrovatkova A, et al. Anosmia and dysgeusia in the absence of other respiratory diseases: should COVID-19 infection be considered? Eur J Case Rep Intern Med. (2020) 7:001641. doi: 10.12890/2020_001641
9. Boscolo-Rizzo P, Borsetto D, Fabbris C, Spinato G, Frezza D, Menegaldo, et al. Evolution of altered sense of smell or taste in patients with mildly symptomatic COVID-19. JAMA Otolaryngol Head Neck Surg. (2020) 146:729. doi: 10.1001/jamaoto.2020.1379
10. Lechner M, Chandrasekharan D, Jumani K, Liu J, Gane S, Lund VJ, et al. Anosmia as a presenting symptom of SARS-CoV-2 infection in healthcare workers-a systematic review of the literature, case series, and recommendations for clinical assessment and management. Rhinology. (2020) 58:394–99. doi: 10.4193/Rhin20.189
11. Lechner M, Patel ZM, Philpott C, Lund VJ. Olfactory loss of function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg. (2020) 146:872–3. doi: 10.1001/jamaoto.2020.1589
12. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. (2020) 77:683–90. doi: 10.1001/jamaneurol.2020.1127
13. Mercante G, Ferreli F, De Virgilio A, Gaino F, Di Bari M, Colombo G, et al. Prevalence of taste and smell dysfunction in coronavirus disease 2019. JAMA Otolaryngol Head Neck Surg. (2020) 146:723–8. doi: 10.1001/jamaoto.2020.1155
14. Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. (2020) 323:2089–90. doi: 10.1001/jama.2020.6771
15. Wilson MP, Jack AS. Coronavirus disease (COVID-19) in neurology and neurosurgery: a scoping review of the early literature. Clin Neurol Neurosurg. (2020) 193:105866. doi: 10.1016/j.clineuro.2020.105866
16. Wong TW, Yau JK, Chan CL, Kwong RS, Ho SM, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. (2005) 12:13–8. doi: 10.1097/00063110-200502000-00005
17. Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
18. Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. (2020) 26:1583–87. doi: 10.1111/jep.13444
19. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
20. Stuijfzand S, Deforges C, Sandoz V, Sajin CT, Jaques C, Elmers J, et al. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health. (2020) 20:1–18. doi: 10.1186/s12889-020-09322-z
21. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732. doi: 10.7150/ijbs.45120
22. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
23. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatry. (2020) 52:102066. doi: 10.1016/j.ajp.2020.102066
24. Russell B, Moss C, Rigg A, Hopkins C, Papa S, Van Hemelrijck M. (2020) Anosmia and ageusia are emerging as symptoms in patients with COVID-19: what does the current evidence say? Ecancermedicalscience. (2020) 14:ed98. doi: 10.3332/ecancer.2020.ed98
25. Tennen H, Affleck G, Mendola R. Coping with smell and taste disorder. In: Getchell TV, Doty RL, Bartoshuk LM, Snow JB, editors. Smell and Taste in Health and Disease. New York, NY: Raven Press (1991). p. 787–802.
26. Heath TP, Melichar JK, Nutt DJ, Donaldson LF. Human taste thresholds are modulated by serotonin and noradrenaline. J Neurosci. (2006) 26:12664–71. doi: 10.1523/JNEUROSCI.3459-06.2006
27. Weiffenbach JM, Bartoshuk LM. Taste and smell. Clin Geriatr Med. (1992) 8:543–56. doi: 10.1016/S0749-0690(18)30463-4
28. Public health surveillance for COVID-19: interim guidance. World Health Organization (2020). Available online at: https://www.who.int/publications/i/item/who-2019-nCoV-surveillanceguidance-2020.7 (accessed December 16, 2020).
29. Donovan KA, Grassi L, McGinty HL, Jacobsen PB. Validation of the distress thermometer worldwide: state of the science. Psychooncology. (2014) 23:241–50. doi: 10.1002/pon.3430
30. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
31. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. J Psychosom Res. (2002) 52:69–77. doi: 10.1016/S0022-3999(01)00296-3
32. Tesio V, Molinaro S, Castelli L, Andriani M, Fanelli AL, Marra S, et al. Screening of depression in cardiac patients: is the HADS an effective tool? Int J Cardiol. (2014) 172:e344–5. doi: 10.1016/j.ijcard.2013.12.308
33. Di Stasio D, Candotto V, Serpico R, Migliozzi R, Petruzzi M, Tammaro M, et al. Depression and distress in burning mouth syndrome: a case control study. J Biol Regul Homeost Agents. (2018) 32(2 Suppl. 1):91–5.
34. Canaletti C, Colombo F, Dessì A, Geccherle E, Tongiorgi A, Cai P, et al. Depressive symptoms and anxiety and their screening in IBD patients: performance of the distress thermometer in Italian IBD patients. Abstracts of the 15th Congress of ECCO—European Crohn's and Colitis Organisation, Vienna 2020(2020).
35. Grassi L, Johansen C, Annunziata MA, Capovilla E, Costantini A, Gritti P, et al. Screening for distress in cancer patients: a multicenter, nationwide study in Italy. Cancer. (2013) 119:1714–21. doi: 10.1002/cncr.27902
36. Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life—an updated review. Chem Senses. (2014) 39:185–94. doi: 10.1093/chemse/bjt072
37. Wang L, Gillis-Smith S, Peng Y, Zhang J, Chen X, Salzman CD, et al. The coding of valence and identity in the mammalian taste system. Nature. (2018) 558:127–31. doi: 10.1038/s41586-018-0165-4
38. Rolls ET. Taste and smell processing in the brain. In: Doty RL, editor. Handbook of Clinical Neurology. Amsterdam: ELSEVIER (2019). p. 97–118.
39. Printza A, Constantinidis J. The role of self-reported smell and taste disorders in suspected COVID-19. Eur Arch Oto-Rhino-Laryngology. (2020) 277:2625–30. doi: 10.1007/s00405-020-06069-6
40. Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, Lulli LG, et al. COVID-19-Related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. (2020) 17:7857. doi: 10.3390/ijerph17217857
41. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
42. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. (2020) 11:CD013779. doi: 10.1002/14651858.CD013779
43. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:1–22. doi: 10.1007/s11920-020-01166-z
44. Lima CKT, De Medeiros Carvalho PM, Lima IDAAS, de Oliveira Nunes JVA, Saraiva JS, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Research. (2020) 287:112915. doi: 10.1016/j.psychres.2020.112915
45. Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:300–2. doi: 10.1016/S2215-0366(20)30073-0
46. De Pablo GS, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J Affect Disord. (2020) 275:48–57. doi: 10.1016/j.jad.2020.06.022
47. Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
48. Magnavita N, Tripepi G, Di Prinzio. R. R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int J Environ Res Public Health. (2020) 17:5218. doi: 10.3390/ijerph17145218
Keywords: COVID-19, taste disorder, smell loss, psychological distress, healthcare workers
Citation: Dudine L, Canaletti C, Giudici F, Lunardelli A, Abram G, Santini I, Baroni V, Paris M, Pesavento V, Manganotti P, Ronchese F, Gregoretti B and Negro C (2021) Investigation on the Loss of Taste and Smell and Consequent Psychological Effects: A Cross-Sectional Study on Healthcare Workers Who Contracted the COVID-19 Infection. Front. Public Health 9:666442. doi: 10.3389/fpubh.2021.666442
Received: 10 February 2021; Accepted: 12 April 2021;
Published: 28 May 2021.
Edited by:
Nicola Mucci, University of Florence, ItalyReviewed by:
Luigi Isaia Lecca, University of Cagliari, ItalyCopyright © 2021 Dudine, Canaletti, Giudici, Lunardelli, Abram, Santini, Baroni, Paris, Pesavento, Manganotti, Ronchese, Gregoretti and Negro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luisa Dudine, bHVpc2EuZHVkaW5lQGFzdWdpLnNhbml0YS5mdmcuaXQ=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
§These authors share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.