
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 17 March 2021
Sec. Public Health Education and Promotion
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.639273
 Xun Gong1,2
Xun Gong1,2 Wenliang Zhang1,2
Wenliang Zhang1,2 Jeffrey W. Ripley-Gonzalez1
Jeffrey W. Ripley-Gonzalez1 Yuan Liu1
Yuan Liu1 Yaoshan Dun1,2,3
Yaoshan Dun1,2,3 Fan Zheng1
Fan Zheng1 Ling Qiu1
Ling Qiu1 Suixin Liu1,2*
Suixin Liu1,2*Background: Despite the benefits of cardiac rehabilitation (CR), phase II CR remains highly unavailable; the factors influential to the successful implementation and development of phase II CR programs have not been fully explored.
Methods: A cross-sectional survey was completed by 168 nationwide clinical staff. Parameters associated with the successful implementation and development of phase II CR and the factors associated with the quality of CR were explored by multivariable logistic regression.
Results: One hundred and eighteen of 168 respondents' institutions had successfully developed phase II CR programs, 41 of which delivered high-quality CR. Independent factors associated with successful implementation and development of CR were leadership support from hospital administrators, support from resident physicians, staff perception in CR increasing medical risk, and department type (cardiology vs. rehabilitation department). Independent factors associated with CR quality were the availability of “professional CR providers” and staff perceptions of CR improving physician–patient relationships. The medical system factors did not affect the development and quality of CR, including hospital level, funding type, academic type, general/specialized hospital, located city, medical insurance, the existence of a CR outpatient clinic and independent space, the availability of professional CR providers, staff structure, and the availability of regular training and standard procedure.
Conclusions: The development and quality of a phase II CR program may benefit from factors including support from administrators and resident physicians, adequately training more CR providers, without viewing medical system factors as a major issue.
Cardiovascular diseases (CVDs) are the leading cause of death worldwide (1, 2). Cardiac rehabilitation (CR) can aid in reducing morbidity and all-cause mortality, including from CVDs, and is recommended as 1A class by multinational guidelines (2, 3). CR is composed of three distinct phases. Phase II of CR offers services to patients following an acute cardiac event or hospitalization and plays a pivotal role in the whole process of CVDs treatment and rehabilitation. However, phase II CR remains highly unavailable, even in recent years. CR programs are currently carried out in ~40% of countries worldwide (4) and only 22.1% in low- and middle-income countries (5). Therefore, exploring the factors in the implementation and development of CR is conducive to accelerating its development.
To understand the barriers of phase II CR development and promote the development of CR, previous studies have been carried out on the barriers encountered by CR both in China and abroad. Studies abroad have investigated the barriers of CR delivery in already developed programs mainly focusing on exploring the factors affecting the referral rate, admission rate, and compliance of patients (6–10). These factors are multifactorial, including patient factors, those of healthcare providers, and medical system levels (9, 11–15). Few studies from China have briefly explored these issues. Although Wang et al. (16) had reported that medical system factors are a major obstacle to the development of CR programs, this study included a small sample of 18 medical staff from a single center. The above-mentioned research mainly discussed these issues in CR from the perspective of patients, CR procedure, and medical insurance policy, but there is no research focusing on CR providers themselves. In addition, there is still a lack of relevant research on the factors that determine CR quality.
China has the largest population with cardiovascular diseases; even so, there were only 216 medical institutions in China developing CR programs until 2018 (17), and many other institutions are preparing for implementation since then. At present, the development of CR programs in China is in its infancy, and the barriers encountered may be representative and of reference significance, especially for low- and middle-income developing countries. In this study, we conducted a nationwide cross-sectional study using an online questionnaire survey of in-service training medical staff. Then, we conducted the investigation and analysis of the influencing factors of phase II of CR implementation and development and further explored the factors related to the quality of CR to provide evidence for the successful implementation and development of phase II CR in China and the undeveloped districts.
A national cross-sectional design was used in the study. The investigation conforms with the principles outlined in the Declaration of Helsinki and was approved by the Medical Ethics Committee of Xiangya Hospital of Central South University (Ethics number: 202007212). In-service training clinical staff trained in the CR Center of Xiangya Hospital were contacted through telephone or messages. The online survey was sent via WeChat (a messaging/calling app) to participants with informed consent. The survey was collected from July to September 2019.
Inclusion criteria were the following: (1) in-service training clinical staff who completed the CR training in the CR Center of Xiangya Hospital; (2) 3–6 months training length; (3) undertook training between January 2013 and December 2018; (4) Passed the CR certificate exam; and (5) offered accurate contact information.
The following steps were taken to design the survey (18): (1) literature review (databases including MEDLINE, EMBASE, Google Scholar, CNKI, Wanfang Data) to identify studies reporting results of CR program surveys on a regional, national, or greater basis; (2) invited three cardiac rehabilitation specialists and eight in-service training clinical staff created a 30-item survey. The survey comprised four parts, including characteristics of in-service training clinical staff and their affiliated institutions; knowledge, perceptions, and attitudes toward CR; availability and characteristics of CR programs (19), space, equipment, and management system and human resources for CR (a version of the questionnaire translated to English is described in the Supplementary Material Methods and Survey 1).
Phase II CR programs that offered services to patients following an acute cardiac event or hospitalization were of interest. The criteria of phase II CR programs were the following: (1) initial assessment or risk assessment/stratification; (2) structured exercise training program (supervised or not); and (3) at least one other strategy to control CV risk factors (20).
Overall, 16 structure and process quality indicators were assessed to evaluate the quality of CR through the survey (20). Eight core components (structure indicators) were recorded, including initial assessment, risk assessment/stratification, exercise training, patient education, management of cardiovascular (CV) risk factors, nutrition counseling, stress management, and tobacco cessation interventions. Eight risk factors (process indicators) interventions were recorded, including blood pressure, lipids, physical inactivity, poor diet, adiposity, tobacco use, glucose/HbA1c, and depression. The CR programs providing 16 quality indicators were categorized as high-quality CR, otherwise lower quality (21, 22).
Data analysis was performed with SPSS (version 24 for Windows; IBM Corp, Armonk, New York, USA). Data are described in frequency (percentage) or mean (SD). To explore the factors associated with CR development, all cases were divided into two groups (successful implementation and development institutions, failed implementation and development institutions). Furthermore, to explore the factors associated with CR quality during implementation and development, all cases of successful implementation and development institutions were divided into either a high- or a lower-quality group (Figure 1). A chi-square test was used to compare group differences in categorical variables, and an independent-sample t test was used for quantitative variables. The factors with P < 0.05 were chosen for the next multivariable logistic regression analysis; P < 0.05 was considered statistically significant. The odds ratio (OR) and 95% confidence interval (95% CI) were also calculated. (More detailed information of “Methods” are described in Supplementary Material Methods and Survey 1).
This study enrolled 238 in-service clinical staff and received 168 responses, a response rate of 70.6% (Figure 2). One hundred and eighteen (70.2%) respondents' affiliated institutions have already developed phase II CR program.
The rate of successful CR implementation and development was higher in cardiology departments than in rehabilitation departments. Hospitals in China are designated as Primary, Secondary, or Tertiary institutions (23). The cities in which affiliated institutions are located were regrouped into five classes using the latest population-based city classifications released by the Chinese State Council (24). The located city of respondents covered 28 provinces and autonomous regions and municipalities, which consisted of 90.3% of administrative areas in mainland China. Overall, most of these characteristics showed no difference between the successful and failed implementation and development institutions, including age, academic degree, clinical title, job title, affiliated institution's level, funding type, general/specialized, academic type, and located city level (Table 1).
Concerning the benefits of CR, the successful implementation and development of phase II CR group's staff were more optimistic about “Improvement of quality of life” (98.3 vs. 90.0%, P = 0.04) and “Improvement of mental health” (94.1 vs. 82.0%, P = 0.03). Fewer of those from the successful implementation and development of phase II CR group considered “Increased medical risk” (47.5 vs. 66.0%, P = 0.03) a disadvantage. All clinical staff professionals were largely supportive of CR (≥85.7%). Resident physicians, department administrators, and hospital administrators showed more positive attitudes toward CR in successful implementation and development of phase II CR group than those in unsuccessful implementation and development of phase II CR group (91.5 vs. 72.0%; 98.3 vs. 86.0%; 93.2 vs. 70.0%, respectively) (Table 1).
Multivariable logistic regression showed that “Department type (cardiology vs. rehabilitation department),” “Resident physicians support for CR,” and “Hospital administrators support for CR” are positive independent predictors, and their OR (95% CI) values were 3.175 (1.270, 7.936), 4.313 (1.434, 12.973), and 4.783 (1.508, 15.175), respectively. “Clinical staff perception that there is increased medical risk in CR” was a negative predictor and its OR value was 0.355 (0.144, 0.878) (Figure 3).
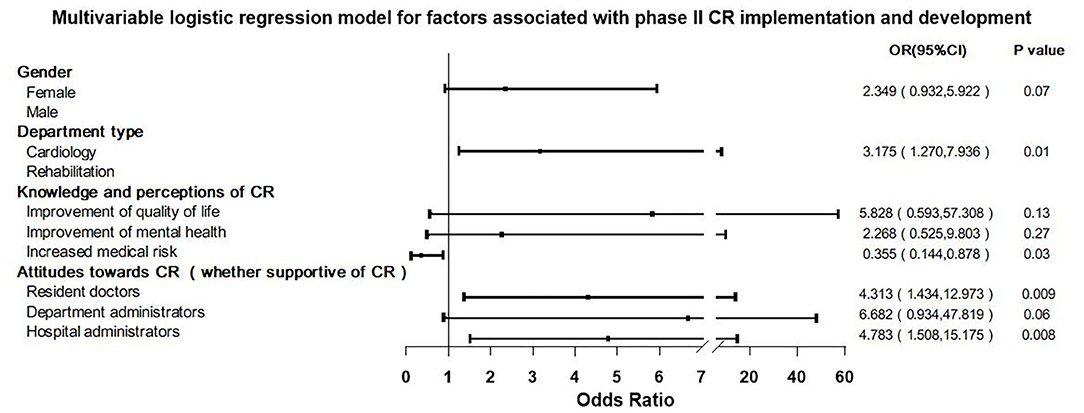
Figure 3. Multivariable logistic regression model for factors associated with phase II cardiac rehabilitation (CR) implementation and development.
The study showed that 118 (70.2%) affiliated institutions had already developed phase II CR programs, 114 provided 16 indictors about CR quality, and 41/114 (36.0%) of institutions delivered high-quality CR (Figure 4).
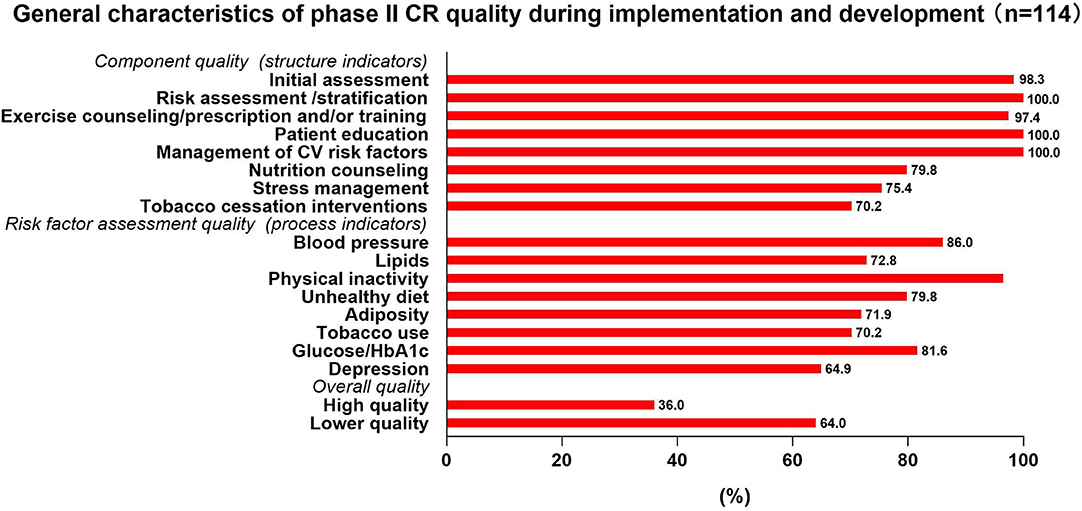
Figure 4. General characteristics of phase II cardiac rehabilitation (CR) quality during implementation and development.
There were significant differences in independent space, the availability of professional CR providers, regular CR training, and standard procedure between the two groups. Regarding staff structure in the CR team, there were differences in the composition of nurses and therapists between two groups, and a higher proportion of “both nurses and therapists” and “either nurses or therapists” (compared with “no nurses or therapists”) were observed in the high-quality group (Table 2).
There were differences in “Improvement of physician–patient relationships” and “Improvement of the clinical staff's specialized knowledge” between the two groups. There were no differences in attitudes toward CR among six types of clinical staff between the two groups (Table 2).
Multivariable logistic regression showed that availability of “Professional CR providers” and staff perception that CR improves physician–patient relationships are two independent predictors for phase II CR quality; their OR (95% CI) values were 3.880 (1.295–11.627) and 7.512 (1.853, 30.465), respectively (Figure 5).
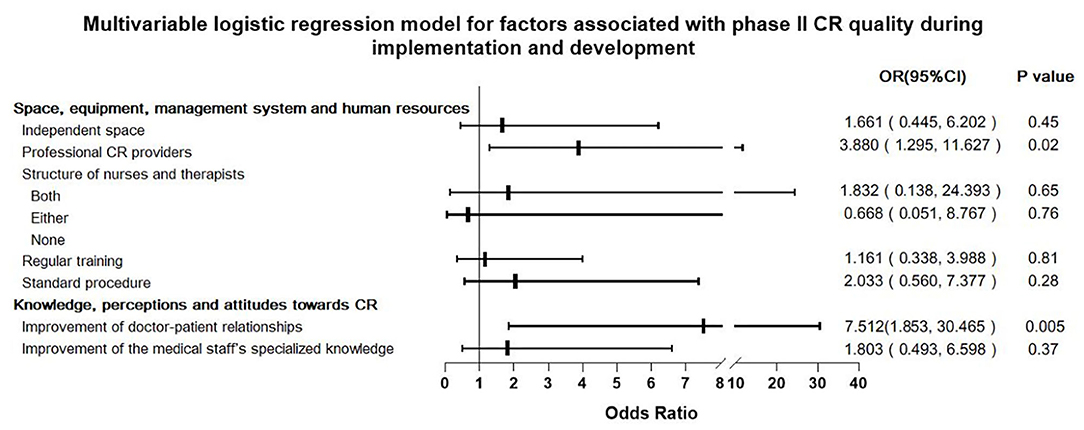
Figure 5. Multivariable logistic regression model for factors associated with phase II cardiac rehabilitation (CR) quality during implementation and development.
Phase II CR implementation continues to face many difficulties throughout the process of implementing and developing CR programs (15). This study investigated and analyzed the factors on the implementation and development of phase II CR and also was the first study to explore the factors on the quality of CR via a nationwide survey. The data showed that after clinical staff had been trained, venues had been prepared, and equipment had/soon to be purchased, nearly one-third of these medical institutions had failed in developing a CR program. Moreover, of the remaining two-thirds of the institutions, 64% of them were unsuccessful in carrying out a high-quality program. This study showed that leadership support from hospital administrators, support from resident physicians, and staff perception in CR increasing medical risk were all independently associated with phase II CR implementation and development (Figure 3). The availability of “professional CR providers” and staff perceptions of CR improving physician–patient relationships were associated with CR quality during implementation and development (Figure 5). The quality of CR was unexpectedly not associated with medical system factors, and even though the department type was a significant indicator toward initial implementation and development success, thereafter, it was not associated with the quality of CR.
When analyzing the reasons behind this, institution leadership appears to play a key role. Hospital administrators are responsible for key decisions in hospitals (25), and as such, this study found that garnered support from these administrators was significantly associated with a successful implementation and development of a phase II CR program. Furthermore, support from resident physicians also appears to be associated with successful implementation and development. Patients are more receptive to the advice of the resident in-charge, so resident physicians play a key role in CR referral, thus affecting the effective implementation and development (8). This suggests that there is a need to gain the support of those in leadership roles within the hospital before the implementation and development of a phase II CR program.
Regarding clinical staff's perception and knowledge of CR, clinical staff recognized the beneficial effects of CR but cited the medical risk involved in treating patients as their main concern with implementing CR. Currently, research has shown that if strict procedures are followed, the risks involved in CR procedures are largely controllable (26–28), and physicians should not overestimate the risks (29). The medical personnel's awareness that CR can improve the relationship between physicians and patients will positively influence the quality of CR. This may be in part due to the current medical environment in China in that physician–patient relationships are not as positive as their international counterparts (30). If the medical staff believes that the doctor–patient relationship can be improved by CR, then they are more willing to promote CR development, thereby improving quality.
Additionally, the availability of professional CR providers in phase II CR programs also appears to influence the quality of CR. The professional level of medical personnel is impactful to the overall quality of CR programs. Because of this, the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) began to conduct Certified Cardiac Rehabilitation Professional (CCRP) certifications in 2014 and requires personnel to update their knowledge and skills every 3 years (31). In phase II, the constant improvement of professional skills and knowledge is indispensable, as well as the encouragement of clinical staff including physicians, nurses, and therapists, to actively participate in CR training to reach the primary qualification level (32). Therefore, at this stage, the Cardiac Rehabilitation associations around the world strive for government support and organize personnel training, attracting more professionals to join the CR program; this may be one of the key elements to accelerating development (32, 33).
Thought also must be placed on phase II CR location within a hospital. It is commonly acknowledged that carrying out CR in rehabilitation departments would be comparatively difficult compared to cardiology departments in China. Although rehabilitation departments are less likely to carry out CR programs than cardiology departments, once the program is set up, there is no difference in the quality of care delivered. Although the cardiology department may be able to control cardiovascular events risks very well, the rehabilitation department also has its advantages, such as better understanding the concept of rehabilitation and being accustomed to the technology used there (32, 34). Therefore, this suggests that the rehabilitation department is also able to develop a phase II CR program and deliver it at a high quality.
Medical system factors tend to play an important role in affecting the implementation and development of CR, mainly including characteristics of CR facilities and characteristics of the delivery systems (12). Generally, higher-level hospitals, public hospitals, general hospitals, teaching hospitals, and hospitals in large cities attract a greater number of patients due to their reputations and skillful clinical staff in China (23). Under the principle of performance appraisal, such hospitals have better financial and human resources to develop CR than the lower-level, private, specialized, non-affiliated hospitals and hospitals in small cities. However, these medical system factors did not affect the development and quality of CR. These results indicate that each hospital can achieve the basic requirements of CR and set up the CR program according to their own situation. There is a huge gap in medical insurance policies across China (35), and preceding studies have found that a lack of medical insurance is an obstacle to CR (16, 17). However, this study shows that both the medical insurance coverage and the reimbursement rate do not affect the quality of CR. Nevertheless, the promotion of insurance is conducive to further development of CR (36); also, good cost effectiveness brought by CR programs (37) will in turn promote the investment of medical insurance.
This study is not without limitations. Although the study covered most regions in China with varying levels of development and economies, variations between populations in other countries exist and will require further studies across different populations. In addition, patient factors were not included in the present study. Lastly, the survey was not analyzed for reliability and validity, but this survey had been fully discussed and revised by three cardiac rehabilitation experts and eight in-service training clinical staff; the final version of the survey was determined after three rounds of discussion. Such method designs ensured that the items and content of the survey were relatively reasonable.
In conclusion, before the implementation and development of phase II CR, support from those in leadership roles and resident physicians is required. Improving the awareness of the benefits and risks of CR through professional training can attract more relevant professionals and medical institutions to fully engage in CR programs. Regarding quality during implementation and development, CR programs should not be limited to specific departments or hospitals, as related departments in hospitals of all levels can carry out high-quality CR programs without viewing medical system factors as a major issue. Therefore, medical institutions that are planning to develop CR programs in the future may emphasize gaining support from those in leadership roles and training more medical personnel to improve the quality of CR.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Xiangya Hospital of Central South University. Written informed consent was not provided because oral and digital informed consent was retrieved before the beginning of the survey.
SL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SL and XG contributed to the concept and design. SL, XG, WZ, JR-G, YD, YL, and LQ contributed to acquisition, analysis, or interpretation of the data. XG, JR-G, YL, and FZ contributed to drafting of the manuscript and contributed to statistical analysis. SL, XG, YL, and FZ contributed to critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.639273/full#supplementary-material
1. Cardiovascular disease in Europe 2016: an epidemiological update. Eur Heart J. (2016) 37:3182–3. doi: 10.1093/eurheartj/ehw468
2. Arnett DK, Khera A, Blumenthal RS. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: Part 1, lifestyle and behavioral factors. JAMA Cardiol. (2019) 4:1043–4. doi: 10.1001/jamacardio.2019.2604
3. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European association for cardiovascular prevention & rehabilitation (EACPR). Eur Heart J. (2016) 37:2315–81. doi: 10.1093/eurheartj/ehw106
4. Pesah E, Supervia M, Turk-Adawi K, Grace SL. A review of cardiac rehabilitation delivery around the world. Prog Cardiovasc Dis. (2017) 60:267–80. doi: 10.1016/j.pcad.2017.08.007
5. Shanmugasegaram S, Perez-Terzic C, Jiang X, Grace SL. Cardiac rehabilitation services in low- and middle-income countries: a scoping review. J Cardiovasc Nurs. (2014) 29:454–63. doi: 10.1097/JCN.0b013e31829c1414
6. Grace SL, Gravely-Witte S, Brual J, Monette G, Suskin N, Higginson L, et al. Contribution of patient and physician factors to cardiac rehabilitation enrollment: a prospective multilevel study. Eur J Cardiovasc Prev Rehabil. (2008) 15:548–56. doi: 10.1097/HJR.0b013e328305df05
7. Grace SL, Gravely-Witte S, Brual J, Suskin N, Higginson L, Alter D, et al. Contribution of patient and physician factors to cardiac rehabilitation referral: a prospective multilevel study. Nat Clin Pract Cardiovasc Med. (2008) 5:653–62. doi: 10.1038/ncpcardio1272
8. Dahhan A, Maddox WR, Krothapalli S, Farmer M, Shah A, Ford B, et al. Education of physicians and implementation of a formal referral system can improve cardiac rehabilitation referral and participation rates after percutaneous coronary intervention. Heart Lung Circ. (2015) 24:806–16. doi: 10.1016/j.hlc.2015.02.006
9. Gallagher R, Neubeck L, Du H, Astley C, Berry NM, Hill MN, et al. Facilitating or getting in the way? The effect of clinicians' knowledge, values and beliefs on referral and participation. Eur J Prev Cardiol. (2016) 23:1141–50. doi: 10.1177/2047487316630085
10. Reges O, Vilchinsky N, Leibowitz M, Khaskia A, Mosseri M, Kark JD. Systemic determinants as barriers to participation in cardiac prevention and rehabilitation services after acute coronary syndrome. Int J Cardiol. (2013) 168:4865–7. doi: 10.1016/j.ijcard.2013.07.056
11. Brown TM, Hernandez AF, Bittner V, Cannon CP, Ellrodt G, Liang L, et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: findings from the American Heart Association's Get With The Guidelines Program. J Am Coll Cardiol. (2009) 54:515–21. doi: 10.1016/j.jacc.2009.02.080
12. Gurewich D, Prottas J, Bhalotra S, Suaya JA, Shepard DS. System-level factors and use of cardiac rehabilitation. J Cardiopulm Rehabil Prev. (2008) 28:380–5. doi: 10.1097/HCR.0b013e31818c3b5b
13. Back M, Oberg B, Krevers B. Important aspects in relation to patients' attendance at exercise-based cardiac rehabilitation - facilitators, barriers and physiotherapist's role: a qualitative study. BMC Cardiovasc Disord. (2017) 17:77. doi: 10.1186/s12872-017-0512-7
14. Servio TC, Britto RR, de Melo Ghisi GL, da Silva LP, Silva LDN, Lima MMO, et al. Barriers to cardiac rehabilitation delivery in a low-resource setting from the perspective of healthcare administrators, rehabilitation providers, and cardiac patients. BMC Health Serv Res. (2019) 19:615. doi: 10.1186/s12913-019-4463-9
15. Ragupathi L, Stribling J, Yakunina Y, Fuster V, McLaughlin MA, Vedanthan R. availability, use, and barriers to cardiac rehabilitation in LMIC. Glob Heart. (2017) 12:323–34 e10. doi: 10.1016/j.gheart.2016.09.004
16. Wang W, Chair SY, Thompson DR, Twinn SF. Health care professionals' perceptions of hospital-based cardiac rehabilitation in mainland China: an exploratory study. J Clin Nurs. (2009) 18:3401–8. doi: 10.1111/j.1365-2702.2009.02876.x
17. Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. (2019) 13:31–45. doi: 10.1016/j.eclinm.2019.06.007
18. Turk-Adawi KI, Terzic C, Bjarnason-Wehrens B, Grace SL. Cardiac rehabilitation in Canada and Arab countries: comparing availability and program characteristics. BMC Health Serv Res. (2015) 15:521. doi: 10.1186/s12913-015-1183-7
19. Cortes-Bergoderi M, Lopez-Jimenez F, Herdy AH, Zeballos C, Anchique C, Santibanez C, et al. Availability and characteristics of cardiovascular rehabilitation programs in South America. J Cardiopulm Rehabil Prev. (2013) 33:33–41. doi: 10.1097/HCR.0b013e318272153e
20. Supervia M, Turk-Adawi K, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Nature of cardiac rehabilitation around the globe. EClinicalMedicine. (2019) 13:46–56. doi: 10.1016/j.eclinm.2019.06.006
21. Initiative CDQ. Evaluation Criteria for National Standardized Cardiac Rehabilitation Centre. (2020). Available online at https://www.cdqi.org.cn/CDAssessment/crc_standard.aspx?to=crc (accessed June 01, 2020).
22. National Center for Cardiovascular diseases CMA. Cardiovascular Disease Quality Initiative. (2020). Available online at: https://www.cdqi.org.cn/CDAssessment/crc_evaluation.aspx?to=crc (accessed June 01, 2020).
23. Bi Y, Zhu D, Cheng J, Zhu Y, Xu N, Cui S, et al. The status of glycemic control: a cross-sectional study of outpatients with type 2 diabetes mellitus across primary, secondary, and tertiary hospitals in the Jiangsu province of China. Clin Ther. (2010) 32:973–83. doi: 10.1016/j.clinthera.2010.05.002
24. Wang K, Liu J. The spatiotemporal trend of city parks in Mainland China between 1981 and 2014: implications for the promotion of leisure time physical activity and planning. Int J Environ Res Public Health. (2017) 14:1150. doi: 10.3390/ijerph14101150
25. Skirbekk H, Hem MH, Nortvedt P. Prioritising patient care: the different views of clinicians and managers. Nurs Ethics. (2018) 25:746–59. doi: 10.1177/0969733016664977
26. Franklin BA, Bonzheim K, Gordon S, Timmis GC. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy: a 16-year follow-up. Chest. (1998) 114:902–6. doi: 10.1378/chest.114.3.902
27. Van Camp SP, Peterson RA. Cardiovascular complications of outpatient cardiac rehabilitation programs. JAMA. (1986) 256:1160–3. doi: 10.1001/jama.1986.03380090100025
28. Pavy B, Iliou MC, Meurin P, Tabet JY, Corone S. Safety of exercise training for cardiac patients: results of the French registry of complications during cardiac rehabilitation. Arch Int Med. (2006) 166:2329–34. doi: 10.1001/archinte.166.21.2329
29. American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 10th ed. Philadelphia, PA: Wolters Kluwer Health (2016).
30. Ma S, Xu X, Trigo V, Ramalho NJ. Doctor-patient relationships (DPR) in China. J Health Organ Manag. (2017) 31:110–24. doi: 10.1108/JHOM-09-2016-0165
31. American Association of Cardiovascular and Pulmonary Rehabilitation. AACVPR Professional Certification Commission. Certification Renewal Policy. (2019). p. 1–5.
32. Grace SL, Turk-Adawi KI, Contractor A, Atrey A, Campbell NR, Derman W, et al. Cardiac rehabilitation delivery model for low-resource settings: an international council of cardiovascular prevention and rehabilitation consensus statement. Prog Cardiovasc Dis. (2016) 59:303–22. doi: 10.1016/j.pcad.2016.08.004
33. Grace SL, Turk-Adawi KI, Contractor A, Atrey A, Campbell N, Derman W, et al. Cardiac rehabilitation delivery model for low-resource settings. Heart. (2016) 102:1449–55. doi: 10.1136/heartjnl-2015-309209
34. Cowie A, Buckley J, Doherty P, Furze G, Hayward J, Hinton S, et al. Standards and core components for cardiovascular disease prevention and rehabilitation. Heart. (2019) 105:510–5. doi: 10.1136/heartjnl-2018-314206
35. Guo Q, Luo K. Concentration of healthcare resources in China: the spatial-temporal evolution and its spatial drivers. Int J Environ Res Public Health. (2019) 16:4606. doi: 10.3390/ijerph16234606
36. Moghei M, Pesah E, Turk-Adawi K, Supervia M, Jimenez FL, Schraa E, et al. Funding sources and costs to deliver cardiac rehabilitation around the globe: drivers and barriers. Int J Cardiol. (2019) 276:278–86. doi: 10.1016/j.ijcard.2018.10.089
Keywords: cardiac rehabilitation, implementation and development, independent predictors, quality, survey
Citation: Gong X, Zhang W, Ripley-Gonzalez JW, Liu Y, Dun Y, Zheng F, Qiu L and Liu S (2021) Successful Implementation and Development of a Phase II Cardiac Rehabilitation Program: A China-Wide Cross-Sectional Study Tracking In-service Training Clinical Staff. Front. Public Health 9:639273. doi: 10.3389/fpubh.2021.639273
Received: 09 December 2020; Accepted: 10 February 2021;
Published: 17 March 2021.
Edited by:
Shane Andrew Thomas, Australian National University, AustraliaReviewed by:
Warren G. McDonald, Methodist University, United StatesCopyright © 2021 Gong, Zhang, Ripley-Gonzalez, Liu, Dun, Zheng, Qiu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suixin Liu, bGl1c3VpeGluQGNzdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.