- 1Department of Nutrition, Kings College London, London, United Kingdom
- 2Department of Women and Children's Health, King's College London, London, United Kingdom
- 3Faculty of Health and Life Sciences, School of Nursing, Midwifery and Health, Coventry University, Coventry, United Kingdom
- 4UCL Social Research Institute, University College London (UCL), London, United Kingdom
Background: Women of black African heritage living in high income countries (HIC) are at risk of obesity and weight-related complications in pregnancy. This review aimed to synthesize evidence concerning attitudes to weight management-related health behaviors in pregnancy and postpartum, in women of black African ancestry, living in high-income countries.
Methods: A systematic review of the literature and thematic evidence synthesis using the Capability-Opportunity-Motivation Behavioral change theoretical model (COM-B). Databases searched included MEDLINE, EMBASE, Web of Science, and Scopus. The CASP tool was used to assess quality.
Results: Twenty-four papers met the selection criteria, most of which were from the US. Motivational factors were most commonly described as influencers on behavior. Normative beliefs about “eating for two,” weight gain being good for the baby, the baby itself driving food choice, as well as safety concerns about exercising in pregnancy, were evident and were perpetuated by significant others. These and other social norms, including a cultural acceptance of larger body shapes, and daily fast food, created a challenge for healthy behavior change. Women also had low confidence in their ability to lose weight in the postpartum period. Behavior change techniques, such as provision of social support, use of credible sources, and demonstration may be useful to support change.
Conclusions: The women face a range of barriers to engagement in weight-related health behaviors at this life-stage. Using a theoretical behavior change framework can help identify contextual factors that may limit or support behavior change.
Introduction
Obesity is a significant global health challenge (1). In most high-income countries (HIC), over 50% of women enter pregnancy with a body mass index (BMI) above the recommended range (2, 3). Excessive gestational weight gain in pregnancy is associated with postpartum weight retention (4, 5), contributing to long-term obesity risk for women (6), particularly when they have a high pre-pregnancy BMI (7, 8). It also increases their risk of gestational diabetes, complications, and mortality in pregnancy (9–12) and impacts on the future health and obesity risks of the offspring (13, 14).
In HIC, women of black African heritage are more likely to enter pregnancy overweight or obese compared with white women (8, 11). Furthermore, black women are four times more likely to remain overweight following pregnancy than white women, with excessive gestational weight gain and postpartum weight retention being key risk factors (15–17).
There is growing evidence to suggest that engagement in optimal diet and physical activity behaviors during pregnancy and the postpartum period can reduce gestational (18–21) and postpartum weight retention (22, 23). However, there is a paucity of studies focusing on modifying lifestyle behaviors in women from ethnic minorities (10, 11, 18, 24).
Improving health behaviors in minority ethnic groups requires healthcare and interventions to be culturally sensitive, taking into consideration beliefs and structural influences on access (25–27). Additionally, it is increasingly recognized that theoretically informed interventions are more likely to show increased efficacy (28), particularly for complex interventions such as those designed to change lifestyle and health behaviors (29, 30). The use of a theoretical framework leads to greater understanding of the influences on health behaviors and provides an opportunity to map these factors to appropriate behavior change techniques, in order to improve the efficacy of interventions (25, 31).
Qualitative methods are a useful approach when exploring attitudes and influences on behavior. Individual studies consider contextually shaped situations, however, they are typically small in size and are setting specific. Synthesizing qualitative studies can lead to a greater understanding of a phenomenon across settings and be of value to researchers and clinicians who are interested in the unique perspectives but who are unlikely to have time to collate all the literature themselves.
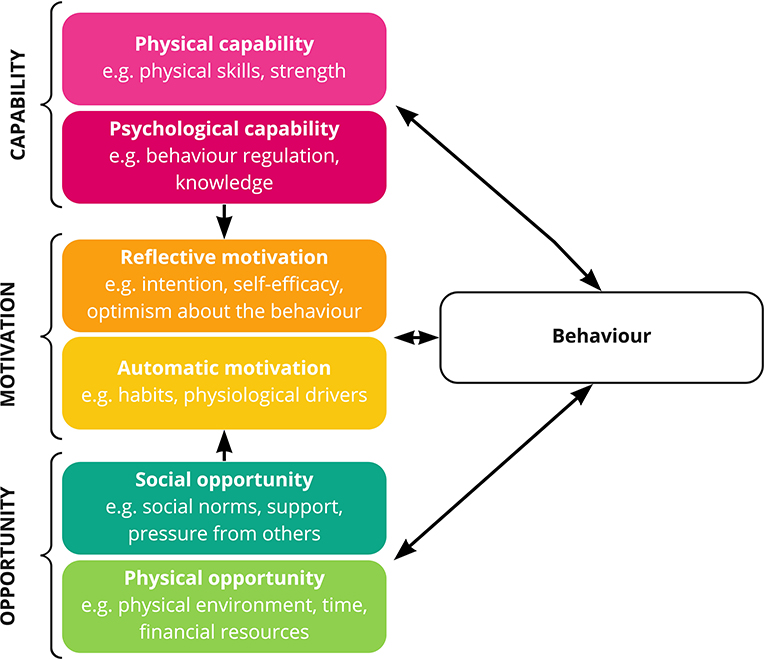
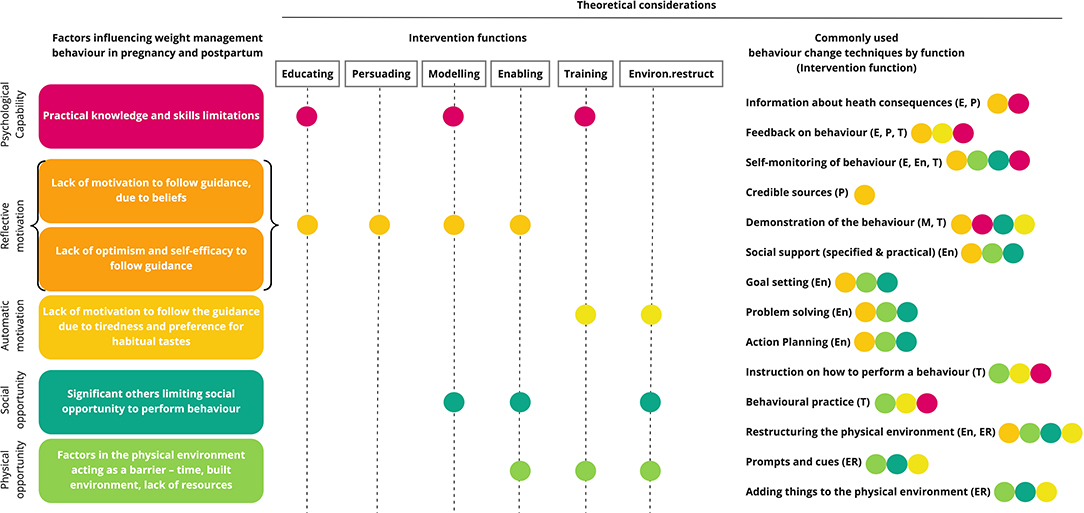
To improve the practical utility of the results, we have applied a theoretical behavioral analysis framework, the Capability-Opportunity-Motivation model of behavior change (COM-B) to our synthesis of the data. In this model the factors that influence behavior are classified according to their influence on Capability (psychological or physical), Opportunity (social or physical), or Motivation (reflective or automatic) (31) (Figure 1). The associated Behavior Change Wheel supports the mapping of the COM-B findings to evidence-based behavior change techniques, linking theory to mechanisms supporting change (32). Underpinning interventions theoretically in this way can improve efficacy and evaluation (33).
This review aims to synthesize the qualitative evidence concerning the attitudes toward and factors influencing engagement in weight management, physical activity and healthy dietary behaviors in the pregnancy and postpartum period in women of African ancestry living in HIC, where there is strong evidence of a disproportionate burden of obesity and weight-related complications associated with pregnancy. The evidence summary will be useful for researchers, healthcare practitioners as well as intervention and health promotion designers.
Methods
Reporting
This review paper has been reported in accordance with the Enhancing Transparency of Reporting the Synthesis of Qualitative Research Framework (ENTREQ) and the PRISMA guidelines and is registered on the PROSPERO database for systematic reviews (PROSPERO 2019: CRD42019143056).
Literature Search
A literature search was conducted on the following electronic databases: MEDLINE, EMBASE, Web of Science, CINAHL, PsycINFO, LILACS, Cochrane Database of Systematic Reviews (CDSR), SCOPUS, and DARE. The search strategy used MeSH index terms and keywords (Table 1, Supplementary File 1). The search strategy was devised for MEDLINE by two members of the review team (AA and AM) and was subsequently modified for the other databases. Each database was searched separately and the results combined. The searches were conducted between 29th June and 18th July 2019 and updated by search alert until 23rd November 2020.
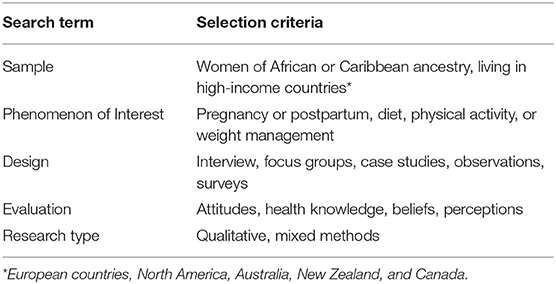
Table 1. Summary of sample, phenomenon of interest, design, evaluation, research type (SPIDER) search criteria (34).
Study Selection
For quality control, two reviewers (AM and GS1) independently screened 70% of titles and abstracts for full-text review against the inclusion/exclusion criteria and the final 30% were screened by a single reviewer (AM). Two reviewers independently selected articles for inclusion from the full texts (AA and AM); any differences between reviewers were resolved by a third reviewer (CR).
The inclusion criteria were: A qualitative study design (focus groups, ethnography, or interviews) exploring attitudes, behavior or social influences related to exercise, diet, weight management, or body image during pregnancy and postpartum; Incorporating women of black African or Caribbean ancestry (immigrants and long-term settlers (1st−4th generation); HIC setting (Europe, North America, Australia, and New Zealand); Results reporting data for black participants explicitly, or the majority of the sample was of black ethnicity (85%+). The exclusion criteria included: Survey methodology; Studies where data concerning exercise, diet, or weight-management was not explicit; Studies focusing on dietary supplement use; Studies where the population criteria or black participant reporting criteria were not met.
Eighty-five percent black participants was chosen as the cut-off by the team for quality reasons when data for black participants was not explicitly reported, such that the themes were likely to be representative of those of black ethnicity. Gestational diabetes (GDM) studies were included if detail regarding diet, physical activity or weight management were reported.
Data Extraction
Data extraction was carried out according to the published PROSPERO protocol. Information extracted included authors, year of publication, study setting, participant characteristics, data collection method, theoretical framework and author's themes and results. Study results included first- and second-order constructs that were labeled in the results section of the studies, according to reported qualitative synthesis methodology (35).
Quality Appraisal and Sensitivity Analysis
Studies were appraised for quality using the Critical Appraisal Skills Programme (CASP) tool for qualitative studies (36, 37). No studies were excluded based on the quality appraisal, but a sensitivity analysis was carried out to evaluate the contribution of the weaker studies to the overall findings.
Sensitivity analyses were conducted to assess the impact of study quality and contextual relevance to the review question on the findings (Supplementary File 2).
Data Synthesis
We employed the thematic synthesis approach as reported by Thomas, Harden et al. (35) using both deductive and inductive methods to synthesize the data. The findings from each study were imported into NVivo as well as other extracted data, e.g., population, setting, topic focus, and pregnancy stage, to allow contextual comparison as the analysis developed. The data were initially coded according to the COM-B framework (31) and then synthesized thematically (35). The coding framework is provided in Supplementary File 3.
Results
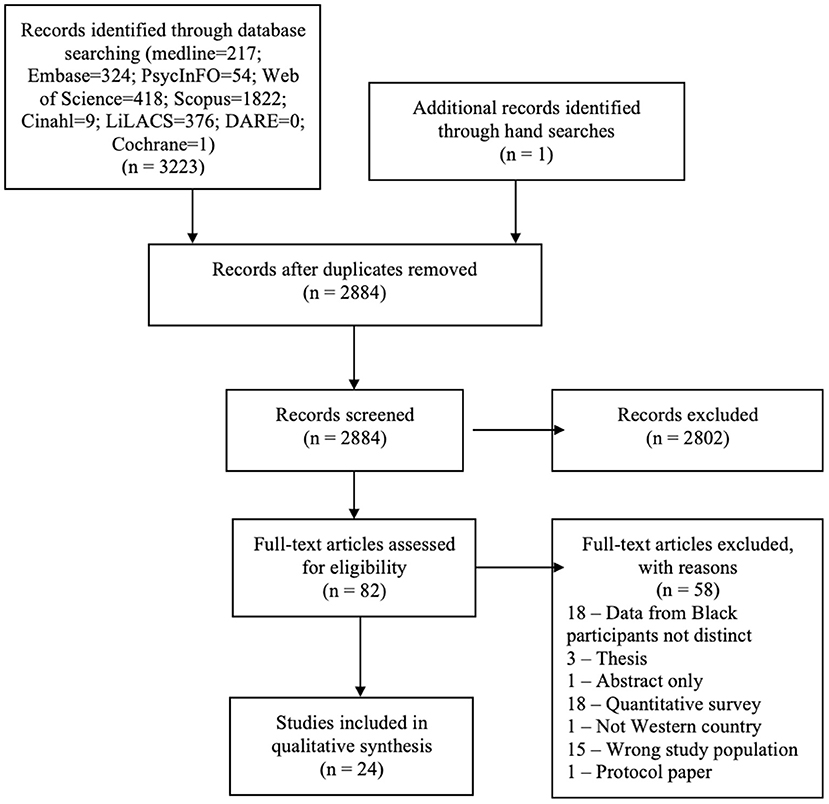
The search identified 3,223 titles (Figure 2). Following screening, 24 published papers were identified for inclusion in the review (Table 2). The search alert confirmed no further eligible papers were published between completion of the search and submission of the review for publication.
Description of Studies
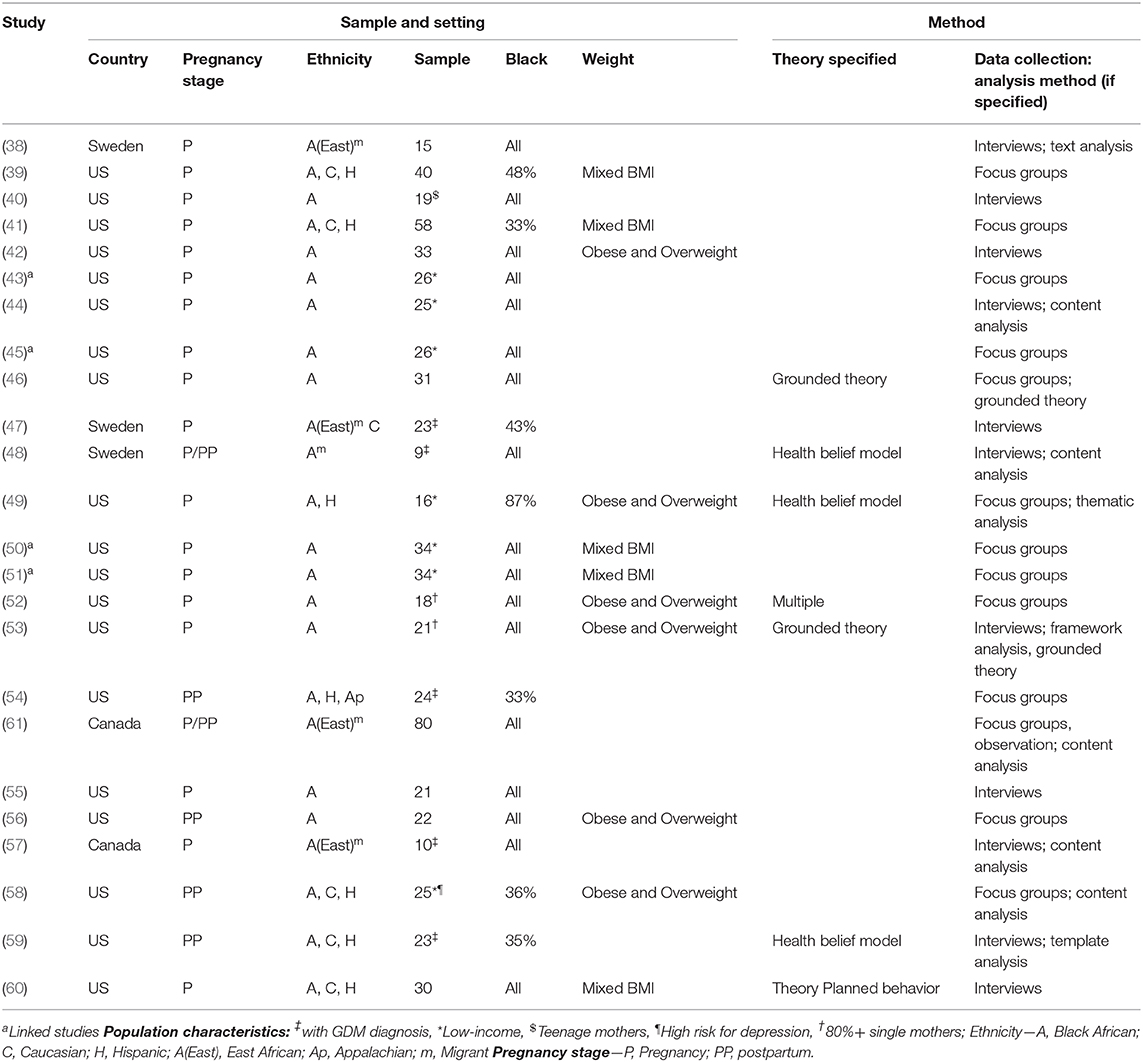
Of the 24 studies included, 19 were conducted in America (39–46, 49–56, 58–60), 3 in Sweden (38, 47, 48), and 2 in Canada (57, 61). Eighteen studies concentrated on pregnancy (38–47, 49–53, 55, 57, 60), 4 on the postpartum period (54, 56, 58, 59) and 2 on both (48, 61). Five studies exclusively comprised a sample of women who had been diagnosed with GDM (47, 48, 54, 57, 59). Across the studies, 6 papers explicitly focused on weight (45, 46, 49, 52, 53, 55), 3 on physical activity (39, 50, 51), 2 on healthy eating (44, 55), and the remainder focused on a combination of these, or lifestyle in general. Qualitative data collection included focus groups (39, 41, 43, 45, 46, 49–52, 54, 56, 58), interviews (38, 40, 42, 44, 47, 48, 53, 55, 57, 59, 60). One study included ethnographic observation in addition to focus groups (61) (Table 2).
Participant Characteristics
In total, data from 401 women were included in the analysis. The complete sample included women across all BMI categories. Six studies included only women who were overweight or obese (42, 49, 52, 53, 55, 58). Seven studies selected low-income women (43–45, 49–51, 58) and in 2 studies at least 80% of the sample were single mothers, although not chosen by purposive sampling (52, 53). Educational attainment was inconsistently reported across the studies but suggests a range of educational attainment levels. Two studies reported more than 50% of participants receiving tertiary education (41, 59) whilst five studies reported at least a quarter of participants had not proceeded beyond high school education (46, 52, 53, 55, 58). Seven studies included mixed ethnicities (39, 41, 47, 49, 54, 58, 59) and the remaining studies included only women of black African heritage. Five of the 24 studies identified the study sample as a first-generation migrant (38, 47, 48, 57, 61) and the remaining studies did not report generational status (Table 3).
Quality Appraisal
One study was considered to be of poor quality (40), one good (49) and the others fair, according to the CASP qualitative studies tool. The main reason for lower quality was an incomplete description of the data analysis process to indicate if it was sufficiently rigorous and lack of clarity in the statement of findings (Supplementary File 2).
Study Methodology Comparisons
A comparison was made across the study methodologies (focus groups, interviews, and ethnographic studies) to compare coding and contribution to thematic analysis. Each methodology contributed equally to each of the themes. However, focus groups were preferentially used for discussions of weight and weight gain. This approach generated rich discussion and conclusions about the traditional attitudes and beliefs around weight and size, which were less evident from the interview data.
Sensitivity Analysis
Sensitivity analyses were conducted to assess the impact on the finding of study quality (40) and contextual relevance to the review question (38, 39, 47, 48, 54, 57–59). After removing one study of poor quality, the sensitivity analysis did not alter the review findings.
Findings of Thematic Synthesis
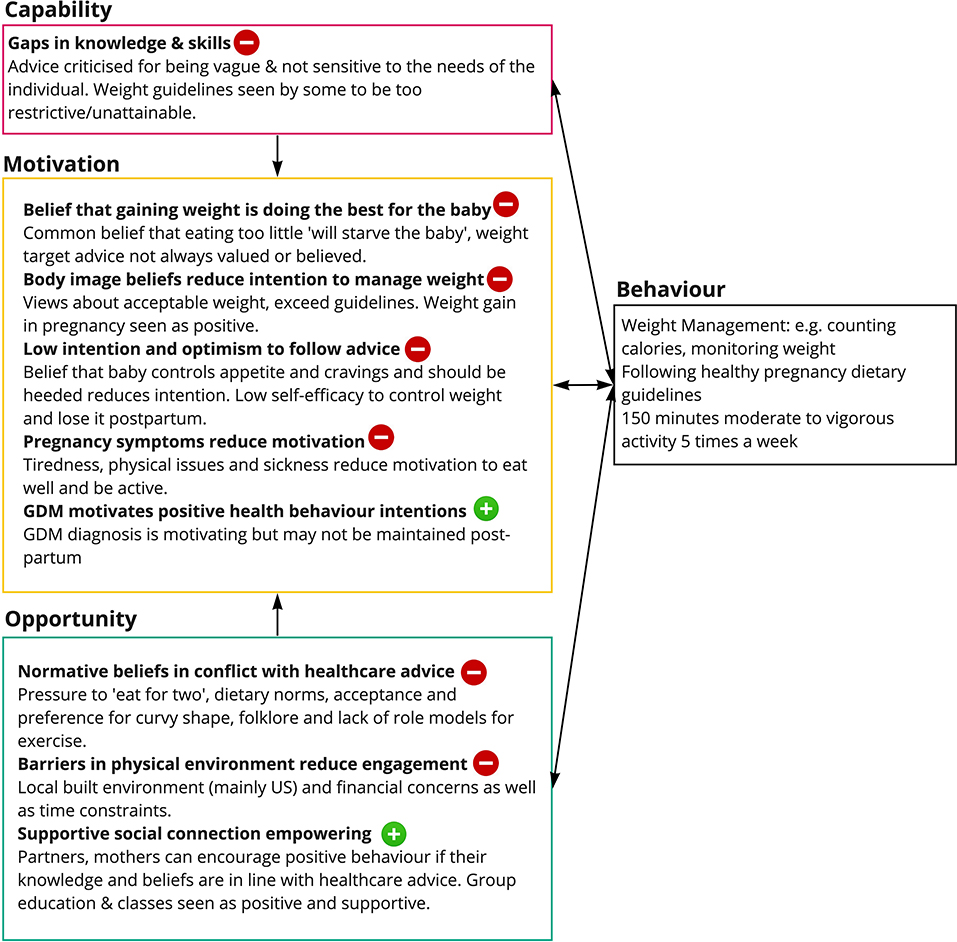
Across the domains of the COM-B framework, Motivation accounted for 54% of the coding, Opportunity for 37% (Social 28% and Physical 9%) and Capability for 9% (Figure 3).
The derivation of each theme from first and second-order constructs is detailed with verbatim examples in Supplementary File 4, together with details of the source publication. First-order constructs (participant quotes) are shown in bold italics and second-order constructs (researcher quotes) are shown in italics.
Capability
Psychological Capability
Gaps in Knowledge and Skills. Women felt healthcare advice was not as useful as it could be. Dietary advice was considered vague, negative and inconsistent, and it failed to take into account personal circumstances and cultural preferences (41, 49, 53, 57, 61). In terms of activity, women wanted to know specifically what type of exercise is safe in pregnancy and criticized health practitioners for not actively promoting physical activity (41, 50, 51). Krans et al. (50, 51) suggested that more practical advice on the duration, frequency, and the most appropriate type of exercise was needed. Gestational weight advice was generally seen as too restrictive, unattainable (46, 53, 56, 60) and inconsistent (49). However, a minority of women did find the gestational weight gain guidance useful (45, 60). Women said that to support postpartum weight loss they would like more information on calories, suggested meal plans and to learn how to cook traditional cultural foods in a healthy way (56).
Opportunity
Social Opportunity
Beliefs of Community Networks Conflicted With Healthcare Advice. Significant others offered advice that conflicted with that of healthcare practitioners (39, 40, 43, 45, 46, 49–53, 55). Pregnant women stated that they felt pressure from partners and family to “eat for two” creating conflict and resulting in stress for the mother-to-be and sometimes led to the advice being ignored (40, 44, 46, 49, 53). A social acceptance of larger body sizes and pressure from partners to retain their curvy shape resulted in women rejecting both BMI charts as an indicator of obesity and healthcare assertions of the need for weight management (45, 46, 49, 50).
Dietary norms within the community included regular consumption of fried foods, fast food and regular consumption of snacks. Women enjoyed the taste of these foods before pregnancy and consumption was perpetuated by others around them, making it difficult to change habits, even for those motivated to do so (40, 42, 43, 49, 50, 52, 56, 60). Multigenerational households were common; food choice was dictated by the primary homemaker and often did not align with recommendations (49).
Community beliefs, such as not raising your hands above your head while pregnant, created a fear of exercising during pregnancy (49, 51). In addition, there were reports of a lack of black cultural role models for women undertaking exercise in their everyday lives (50, 53).
Supportive Social Connection Was Empowering. The majority of studies reported that where family members, especially the pregnant woman's mother, understood healthy lifestyle guidance in pregnancy, it helped to improve compliance (39, 40, 42–44, 47–53, 55–58, 60, 61).
East African immigrant women described a “we culture” in their native countries. Community support meant being healthy while having a baby was a lot easier than in the HIC country (47, 61).
Building a relationship with the healthcare practitioner, feeling personally understood, and having personal circumstances acknowledged was important for women. This included practitioners tailoring advice to women's needs, understanding financial constraints, cultural dietary practices, difficulties attending appointments and being sympathetic to fluctuating motivation associated with pregnancy-related mood (41, 48, 53, 54, 56, 57, 61).
Mothers felt that learning, cooking and exercising in group classes would provide social support to help with weight loss (49, 50, 53, 56, 60). Postpartum women would like extended family to be able to join them, especially for nutrition and cooking sessions (56).
Physical Opportunity
Barriers in the Physical Environment Reduced Engagement. The physical environment, including local neighborhoods, workplaces, financial constraints, and lack of free time, were practical barriers to making positive lifestyle changes (39, 42–44, 47–50, 52, 54–58, 60, 61). In Sweden, the issues were primarily financial (47, 48). By contrast in the US and Canada, participants highlighted additional constraints of the built environment and food insecurity (39, 42, 50, 61). In the US studies, access to healthy food was described as limited while cheap unhealthy foods and fast-food shops were considered plentiful, perpetuating the consumption of less healthy alternatives (42, 44, 53, 55, 60, 61).
Healthy foods were seen as more expensive, limiting both the ability to eat healthily and limiting the desire to try new foods (44, 47, 52, 53, 55, 57, 60, 61). Women diagnosed with GDM expressed a strong need to comply with the guidance, but particular stress associated with the financial implications of doing so (47, 48, 57).
For East African women life “back home” in Africa was seen as more active, involving farming and walking, compared to life in Canada. In Canada, affordable facilities were not available and the weather was not conducive to being outdoors (61).
The need to juggle care of other children created barriers to exercise and made fast food an attractive option (39, 42–44, 49, 50, 56, 58, 60, 61).
Motivation
Reflective Motivation
Gaining Weight Was Believed to be “Doing the Best for the Baby.” Authors concluded women felt weight gain, “no matter how much” (45) was best for the baby, too little gain would “starve the baby” (46), that they were “eating for two” (53). Herring et al. (46) assert that “few women listened to their obstetric providers about IOM recommended weight gain targets”. This was echoed by comments from participants in other studies (45, 49, 60). Notably, little evidence is reported across the studies to indicate that women recognize the risks of GWG to the infant. Instead, they focus on the implications of weight gain on themselves (45, 60). Kroeger et al. explored what level of risk to the infant would curb unhealthy snacking. Women discussed issues such as “birth defects or heart problems” as being serious enough to motivate behavior change while having an obese child was not (52).
There were two notable exceptions to the main body of data. Young women at risk of having a low birthweight baby reported negativity toward weight gain and taking actions to ensure their body weight did not go up too much (40). A study of Somalian women (38) also described women restricting food intake to limit fetal growth which they felt would reduce the risk of a cesarean.
Body Image Beliefs Reduced the Intention to Manage Weight. Beliefs about body weight and what is attractive reduced the intention to manage weight. For example, Kominiarek et al. noted women “described a body image that was not in line with standard clinical recommendations” such as “200 lbs. is not that big” (49). One study reported pregnancy weight gain made women feel more attractive due to cultural preferences for a “voluptuous” shape (45). Extra weight “in the right places” (45) was welcomed, as long as it did not negatively impact on appearance or physical abilities (45, 51, 56).
Women Had Low Intention an Optimism in Their Ability to Follow Advice. Cravings are a key driver of dietary intake in pregnancy (40, 42–44, 46, 52–55, 60). Four of these studies suggest women believed that “the baby is in control,” and cravings and baby movements are linked to the baby communicating what it needs and that a pregnant woman should therefore respond to cravings (43, 46, 52, 55). Women described not having the desire to resist these cravings, which are often for “tasty” foods high in salt, fat and sugar (42, 43, 46, 52).
In general, women put off actively managing their weight during pregnancy but planned to do so after the birth whatever their starting weight (39, 45, 46, 51). However, women who enter pregnancy overweight or who have already had a child, show lower self-belief in their ability to do so (56, 59, 60).
GDM Diagnosis Motivated Positive Health Behavior Intentions. The GDM diagnosis gives women greater determination to control lifestyle in pregnancy (47, 48, 54, 57). However, Hjelm et al. (48) suggest that after pregnancy this motivation wanes.
Automatic Motivation
Pregnancy Symptoms Reduce Motivation to Engage. Tiredness, low energy, poor sleep, aches, pains, and mood swings reduced the desire to engage in physical activity in particular but also influenced increased appetite and snacking behavior (38, 39, 42, 43, 47, 49, 50, 52, 53, 55, 60).
Behavior Change Technique Mapping
Following the COM-B thematic analysis, behavior change wheel (BCW) mapping was carried out to identify potentially useful evidence-based behavior change techniques, based on the synthesized data. The BCW suggests potential intervention functions for each of the COM-B domains. These include, for example, interventions designed to educate, to persuade or to restructure the environment. For each of these intervention functions, a range of evidence-based behavior change techniques are recommended. There is a large glossary of published behavior techniques (62), these are detailed and specific, e.g., providing information about health consequences: “Provide information (e.g., written, verbal, visual) about health consequences of performing the behavior” (32). These behavior change techniques can then be incorporated into the design of intervention components. For example, using educational videos as a component to provide information about health consequences.
Based on this approach, the mapping results are presented in Figure 4.
For motivational factors—for example reluctance to manage weight due to beliefs or lack of self-efficacy, interventions designed to educate, persuade, model, train, or enable are recommended. Potential behavior change techniques include providing information about the health consequences of weight gain in pregnancy, providing evidence from credible sources, which may translate into intervention components such as including peers or faith-leaders to promote the desired behavior. Techniques from control theory have also been shown to increase self-efficacy to perform health behaviors such as goal setting, problem-solving, and action planning (63). Barriers associated with automatic drivers, such as food cravings, may be supported by the techniques adding things to the physical environment or providing instruction. Intervention components such as providing healthy snacks or providing instruction about what snacks may be the best alternatives to the foods craved would support these techniques. Motivational factors may also be influenced by changes in Capability and Opportunity (Figure 1).
For social opportunity factors—such as barriers associated with normative beliefs and habits of significant others, interventions focused on modeling and enabling, are recommended. Given the suggestion in the data that social support was beneficial, provision of social support (practical and specified) may be beneficial. This could translate for example into including the baby's father in an educational intervention, to provide support to perform healthy behaviors. Modeling may include demonstrating the behavior in a practical way; for example, cooking classes would map well to the thematic findings.
Gaps in knowledge and skills may be supported by interventions designed to educate, model, and train. Behavior change techniques mapped to these intervention functions include providing information about health consequences. As the data showed, the majority of the women had little knowledge about the implication of weight on the health of the offspring. Self-monitoring may help keep weight more uppermost in the mind of the women and demonstration of behavior, such as working out calories in a portion size, can be incorporated as an intervention component into education classes.
Physical opportunity barriers are obviously more pervasive and in many cases demand restructuring the environment, to provide financial support or safe space to exercise. However, for factors such a time restriction associated with looking after other children, practical social support may be useful, such as the provision of accessible creche facilities.
Discussion
The pregnancy and postpartum periods are potential intervention points to reduce long-term obesity risk as well as positively influence the health of offspring of women of African and Caribbean descent living in HIC. The review presents a synthesis of qualitative evidence, most of which comes from the US. Use of the theoretical COM-B framework suggests that in particular there are barriers in Motivation and Social Opportunity to performing healthy weight management behaviors, due to cultural beliefs and normative social influences. Analysis using the Behavior Change Wheel suggests that behavior change techniques such as the provision of social support, providing information about health consequences, use of credible sources, demonstration, and techniques from control theory e.g., goal setting are potential approaches to incorporate into intervention design.
Overall, the thematic synthesis indicated motivational barriers included beliefs contradictory to healthcare advice, such as maternal weight gain and responding to cravings being best for the baby and positive body image being associated with higher weight. Intention to manage weight during pregnancy was low, with women preferring to concentrate on weight management after the baby's birth; optimism in the ability to lose weight postpartum was low, particularly for women entering pregnancy overweight or obese. In addition, while social support was helpful for women, normative beliefs, and habits of significant others, driven by cultural norms could conflict with healthcare advice. This limited adherence to recommendations, even for those with positive intention. Additionally, there were evident gaps in knowledge about the risks of excessive weight gain to the fetus, the specific recommendations for physical activity and the translation of dietary advice to incorporate cultural preferences. Factors associated with the built environment such as the barriers associated with the density of fast-food and limited safe space to exercise were reported in the North American studies particularly. The five studies that specifically focus on migrant women highlight the challenges for women adjusting to the lack of support compared to “back home” (61) and the difficulties they faced due to a perceived lack of cultural saliency and healthcare sensitivity to their personal circumstances, especially the lack of financial resources (47, 57, 61). Gaps in knowledge were particularly evident amongst participants in these studies (38, 47, 48, 57) and were sometimes perpetuated by traditional cultural beliefs, such as limiting food intake to avoid a cesarean delivery (38) and stigma (57). Overall, contributions to the themes were broadly similar for migrant women and those of settled status, however three of the five studies focused on gestational diabetes and so exploration of attitudes to weight-related health behaviors was more superficial resulting in these studies contributing less to the summative findings.
The traditional cultural roots of the reported beliefs have been reflected in published literature. Studies amongst traditional African cultures identify an appreciation of a larger body size (64) and cultural taboos about the safety of exercise in pregnancy (65). The importance of responding to cravings has also been reported in West African communities; cravings were considered a signal from the fetus of what it needs and failure to respond to these signals was thought to harm the fetus (66). The presence of beliefs associated with positive benefits of pregnancy weight gain amongst women of African heritage and a low perceived risk of excessive gestational weight gain to the offspring, are supported by quantitative evidence (67). Conversely, barriers associated with tiredness and pregnancy symptoms are consistent with pregnant women in general, whatever their ethnicity (68).
Comparing the results of the analysis to current literature there is some evidence supporting the review findings. The provision of social support in lifestyle interventions, in terms of education delivered in a group setting or inclusion of a partner or family member, as part of lifestyle interventions, have been shown to be effective in African American studies (69–72). Faith-based interventions have been successful in the US setting for a number of health conditions, combining social support with endorsement from credible sources from pastors (73–76). Weight-management interventions in particular have proved successful in the faith setting (77, 78). COM-B analysis to support intervention design for type 2 diabetes education in UK African-Caribbean communities also suggested the potential of social support as a technique (79). While the gaps in knowledge were evident in the data, the access and provision of advice alone have not been conclusively shown to result in appropriate gestational weight gain (24, 80). However, the analysis suggested demonstration as a potential technique to explore, this approach could support the verbal and written advice provision; demonstration involves actively showing the behavior—such as exercise or cooking classes. In fact, Airhihenbuwa, who has contributed considerably toward understanding culturally tailored health promotion to support African Americans (81), explains how important this type of approach is, along-side written or pictorial health communication, because it sits well with the African oral traditions where seeing and listening are intertwined in knowledge development (82). The provision of information about health consequences may be helpful to improve understanding of the risks of excessive weight. However, behavior change theorists do advocate that this approach needs to be used concurrently with other techniques to increase self-efficacy, so the increased knowledge is accompanied with practical skills to alter outcomes (83). This would include use of behavior change techniques such as goal setting, action planning, and problem-solving, which have also been reported as useful in lifestyle interventions generally (63, 84). There is limited data evaluating restructuring of the physical environments as a behavior change technique, however epidemiological data suggest a link between poor accessibility to healthy foods and limited access to appropriate spaces for physical activity and excessive gestational weight gain and poorer pregnancy outcomes (80). Additionally, Physical opportunity to access to healthy foods, availability of safe spaces to exercise, and associated time and budgetary constraints all influence compliance with healthy lifestyle advice (85, 86).
COM-B and the Behavior Change Wheel framework have been developed from a synthesis of 19 theoretical frameworks across the discipline of behavior science (31). The approach has the advantage that it is an easily accessible, well-defined methodological approach, which can facilitate incorporating behavior change thinking into intervention design. However, this accessibility does, to a degree, belie the complexities of behavior science (28). In comparison, the Intervention Mapping framework, which also provides a step-by-step approach to intervention development, offers a more nuanced approach. While potentially this may lead to a more pertinent selection of behavior change techniques (87), it does require the integrated involvement of a behavior change scientist on the team, in order to inform the selection of theoretical constructs (88). As such, the approach of Michie et al. (89) may offer a pragmatic compromise to improve the mapping of theoretical constructs to behavior change techniques when a multi-disciplinary team is not an option.
This review synthesizes the available evidence in a novel and practical way to help inform intervention development to support weight-related health behaviors in pregnant and postpartum women of African heritage. The use of the COM-B framework and BCW allows researchers, health promotion planners and intervention designers to think more theoretically about how an intervention is intended to shift patterns in the performance of behavior and the data suggest potential behavior change techniques. However, while there is a reasonable body of data available and many of these factors are likely to be pertinent across the African diaspora, there is a discernable gap in the literature from across Europe. The transferability of findings to the European setting is reduced because of access issues to healthcare within the privatized medical sector in the US and because the dietary patterns of African American communities are more streamlined with the majority population than has been found in European settings such as the UK (90). In addition, it is also recommended that further participatory work would be done in any local community settings to improve salience of health promotion or intervention (26). It is also a limitation that with the exception of five studies, the majority do not report generational status, thus limiting an assessment of the influence of acculturating factors.
The findings of this review will be of particular value to healthcare providers, researchers, and designers of healthcare and health promotion interventions supporting this population. The review highlights the evidence to suggest that there are positive community assets, such as community social networks that may be leveraged to support healthful behavior and that practical demonstration and modeling of behavior may be particularly helpful to support positive change. The review also identifies the inequities and specific cultural barriers and beliefs which need to be considered. By identifying key determinants of behavior and theoretically associating these with evidence-based behavior change techniques, the findings can help contribute toward the theoretical understanding of pregnancy and postpartum weight-related health behavior in this population. The results may be of notable relevance for those supporting African American women.
Conclusion and Future Directions
Synthesized qualitative evidence suggested that cultural beliefs and social norms shape weight-related health behavior during pregnancy and the postpartum period. This potentially reduces the intention and opportunity for women of African heritage living in HIC settings to engage in optimal health behaviors. Gaps in knowledge and practical environmental factors were also evident. Potential behavior change techniques such as social support, demonstration, credible sources, and techniques that can improve self-efficacy, e.g., goal setting are suggested by analysis using the Behavior Change Wheel. There is a discernable gap in the available literature from the European setting.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
AM: study conception, search and selection, quality assessment, and drafting of the manuscript. AA: search and selection, drafting of the manuscript. AF: drafting of the manuscript. LG: study conception, search development, and drafting of the manuscript. CR: selection, quality assessment, and drafting of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector. AM is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King's College Hospital NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Grace Squires, King's College London for her contribution to the search and selection process (GS).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.637800/full#supplementary-material
Supplementary File 1. Details of the search strategy.
Supplementary File 2. Quality appraisal.
Supplementary File 3. Coding framework.
Supplementary File 4. Example verbatim quotes linking sources to themes.
Footnotes
1. ^See acknowledgments.
References
2. Royal College of Obstetricians and gynaecologists. Care of Women With Obesity in Pregnancy. RCOG, Contract No.: Green top guideline number 72 (2018).
3. Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. (2011) 377:557–67. doi: 10.1016/S0140-6736(10)62037-5
4. Rong K, Yu K, Han X, Szeto IM, Qin X, Wang J, et al. Pre-pregnancy BMI, gestational weight gain and postpartum weight retention: a meta-analysis of observational studies. Public Health Nutr. (2015) 18:2172–82. doi: 10.1017/S1368980014002523
5. Kac G, Benicio MH, Velasquez-Melendez G, Valente JG, Struchiner CJ. Gestational weight gain and prepregnancy weight influence postpartum weight retention in a cohort of brazilian women. J Nutr. (2004) 134:661–6. doi: 10.1093/jn/134.3.661
6. Amorim AR, Rossner S, Neovius M, Lourenco PM, Linne Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity (Silver Spring). (2007) 15:1278–86. doi: 10.1038/oby.2007.149
7. Restall A, Taylor RS, Thompson JM, Flower D, Dekker GA, Kenny LC, et al. Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. J Obes. (2014) 2014:148391. doi: 10.1155/2014/148391
8. Chu SY, Callaghan WM, Bish CL, D'Angelo D. Gestational weight gain by body mass index among US women delivering live births, 2004-2005: fueling future obesity. Am J Obstet Gynecol. (2009) 200:271.e1–7. doi: 10.1016/j.ajog.2008.09.879
9. Aune D, Saugstad O, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. J Am Med Assoc. (2014) 311:1536–46. doi: 10.1001/jama.2014.2269
10. Oteng-Ntim E, Kopeika J, Seed P, Wandiembe S, Doyle P. Impact of obesity on pregnancy outcome in different ethnic groups: calculating population attributable fractions. PLoS One. (2013) 8:e53749. doi: 10.1371/journal.pone.0053749
11. Nishikawa E, Oakley L, Seed PT, Doyle P, Oteng-Ntim E. Maternal BMI and diabetes in pregnancy: Investigating variations between ethnic groups using routine maternity data from London, UK. PLoS One. (2017) 12:e0179332. doi: 10.1371/journal.pone.0179332
12. Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. Vital Signs: Pregnancy-Related Deaths, United States, 2011-2015, and Strategies for Prevention, 13 States, 2013-2017. MMWR Morb Mortal Wkly Rep. (2019) 68:423–9. doi: 10.15585/mmwr.mm6818e1
13. Loring B, Robertson A. Obesity and Inequalitities: Guidance for Addressing in Equities in Overweight and Obesity. Copenhagen: World Health Organization - Europe (2014).
14. Dalrymple KV, Martyni-Orenowicz J, Flynn AC, Poston L, O'Keeffe M. Can antenatal diet and lifestyle interventions influence childhood obesity? A systematic review. Matern Child Nutr. (2018) 14:e12628. doi: 10.1111/mcn.12628
15. Waage CW, Falk RS, Sommer C, Morkrid K, Richardsen KR, Baerug A, et al. Ethnic differences in postpartum weight retention: a Norwegian cohort study. BJOG Int J Obstetr Gynaecol. (2016) 123:699–708. doi: 10.1111/1471-0528.13321
16. Keppel KG, Taffel SM. Pregnancy-related weight gain and retention: implications of the 1990 Institute of Medicine guidelines. Am J Public Health. (1993) 83:1100–3. doi: 10.2105/AJPH.83.8.1100
17. Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. (2000) 22:261–74. doi: 10.1093/oxfordjournals.epirev.a018038
18. Flynn AC, Dalrymple K, Barr S, Poston L, Goff LM, Rogozinska E, et al. Dietary interventions in overweight and obese pregnant women: a systematic review of the content, delivery, and outcomes of randomized controlled trials. Nutr Rev. (2016) 74:312–28. doi: 10.1093/nutrit/nuw005
19. Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Roseboom T, Tomlinson JW, et al. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ. (2012) 344:e2088. doi: 10.1136/bmj.e2088
20. Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med. (2012) 10:47. doi: 10.1186/1741-7015-10-47
21. Wang J, Wen D, Liu X, Liu Y. Impact of exercise on maternal gestational weight gain: an updated meta-analysis of randomized controlled trials. Medicine (Baltimore). (2019) 98:e16199. doi: 10.1097/MD.0000000000016199
22. Dalrymple KV, Flynn AC, Relph SA, O'Keeffe M, Poston L. Lifestyle interventions in overweight and obese pregnant or postpartum women for postpartum weight management: a systematic review of the literature. Nutrients. (2018) 10:1704. doi: 10.3390/nu10111704
23. van der Pligt P, Willcox J, Hesketh KD, Ball K, Wilkinson S, Crawford D, et al. Systematic review of lifestyle interventions to limit postpartum weight retention: implications for future opportunities to prevent maternal overweight and obesity following childbirth. Obes Rev. (2013) 14:792–805. doi: 10.1111/obr.12053
24. Headen IE, Davis EM, Mujahid MS, Abrams B. Racial-ethnic differences in pregnancy-related weight. Adv Nutr. (2012) 3:83–94. doi: 10.3945/an.111.000984
25. National Institute for Clinical Excellence. Promoting Health and Preventing Premature Mortality in Black, Asian and Other Minority Ethnic Groups. NICE, Report No.: QS 167 (2018).
26. Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess. (2012) 16:1–469. doi: 10.3310/hta16440
27. Davidson EM, Liu JJ, Bhopal R, White M, Johnson MR, Netto G, et al. Behavior change interventions to improve the health of racial and ethnic minority populations: a tool kit of adaptation approaches. Milbank Q. (2013) 91:811–51. doi: 10.1111/1468-0009.12034
28. Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. J Public Health Dent. (2011) 71(Suppl 1):S20–33. doi: 10.1111/j.1752-7325.2011.00223.x
29. Michie S. Designing and implementing behaviour change interventions to improve population health. J Health Serv Res Policy. (2008) 13(Suppl 3):64–9. doi: 10.1258/jhsrp.2008.008014
30. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. (2008) 337:a1655. doi: 10.1136/bmj.a1655
31. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
32. Michie S, Atkinson L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. United Kingdom: Silverback Publishing (2014).
33. Michie S, Webb TL, Sniehotta FF. The importance of making explicit links between theoretical constructs and behaviour change techniques. Addiction. (2010) 105:1897–8. doi: 10.1111/j.1360-0443.2010.03161.x
34. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. (2012) 22:1435–43. doi: 10.1177/1049732312452938
35. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:45. doi: 10.1186/1471-2288-8-45
36. Critical Appraisal Skills Programme. Qualitative Checklist. (2017). Available online at: http://www.casp-uk.net/checklists
37. Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane qualitative and implementation methods group guidance series-paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol. (2018) 97:49–58. doi: 10.1016/j.jclinepi.2017.06.020
38. Essen B, Johnsdotter S, Hovelius B, Gudmundsson S, Sjoberg NO, Friedman J, et al. Qualitative study of pregnancy and childbirth experiences in Somalian women resident in Sweden. BJOG. (2000) 107:1507–12. doi: 10.1111/j.1471-0528.2000.tb11676.x
39. Evenson KR, Moos M-K, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. Matern Child Health J. (2009) 13:364–75. doi: 10.1007/s10995-008-0359-8
40. Everette M. Gestational weight and dietary intake during pregnancy: perspectives of African American women. Matern Child Health J. (2008) 12:718–24. doi: 10.1007/s10995-007-0301-5
41. Ferrari RM, Siega-Riz AM, Evenson KR, Moos M-K, Carrier KS. A qualitative study of women's perceptions of provider advice about diet and physical activity during pregnancy. Patient Educ Counsel. (2013) 91:372–7. doi: 10.1016/j.pec.2013.01.011
42. Goodrich K, Cregger M, Wilcox S, Liu J. A qualitative study of factors affecting pregnancy weight gain in African American women. Matern Child Health J. (2013) 17:432–40. doi: 10.1007/s10995-012-1011-1
43. Groth. Low-income, pregnant, African American women's views on physical activity and diet. J Midwifery Womens Health. (2013) 58:195–202. doi: 10.1111/j.1542-2011.2012.00203.x
44. Groth SW, Simpson AH, Fernandez ID. The dietary choices of women who are low-income, pregnant, and African American. J Midwifery Womens Health. (2016) 61:606–12. doi: 10.1111/jmwh.12463
45. Groth SW. How pregnant African American women view pregnancy weight gain. JOGNN J Obstetr Gynecol Neonatal Nurs. (2012) 41:798–808. doi: 10.1111/j.1552-6909.2012.01391.x
46. Herring SJ, Henry TQ, Klotz AA, Foster GD, Whitaker RC. Perceptions of low-income African-American mothers about excessive gestational weight gain. Matern Child Health J. (2012) 16:1837–43. doi: 10.1007/s10995-011-0930-6
47. Hjelm K, Berntorp K, Apelqvist J. Beliefs about health and illness in Swedish and African-born women with gestational diabetes living in Sweden. J Clin Nurs. (2012) 21:1374–86. doi: 10.1111/j.1365-2702.2011.03834.x
48. Hjelm K, Bard K, Apelqvist J. A qualitative study of developing beliefs about health, illness and healthcare in migrant African women with gestational diabetes living in Sweden. BMC Womens Health. (2018) 18:34. doi: 10.1186/s12905-018-0518-z
49. Kominiarek MA, Gay F, Peacock N. Obesity in pregnancy: a qualitative approach to inform an intervention for patients and providers. Matern Child Health J. (2015) 19:1698–712. doi: 10.1007/s10995-015-1684-3
50. Krans E, Chang J. A Will without a way: barriers and facilitators to exercise during pregnancy of low-income, African American women. Women Health. (2011) 51:777–94. doi: 10.1080/03630242.2011.633598
51. Krans E, Chang J. Low-income African American women's beliefs regarding exercise during pregnancy. Matern Child Health J. (2012) 16:1180–7. doi: 10.1007/s10995-011-0883-9
52. Kroeger EN, Carson TL, Baskin ML, Langaigne A, Schneider CR, Bertrand B, et al. Reasons for late-night eating and willingness to change:a qualitative study in pregnant black women. J Nutr Educ Behav. (2019) 51:598–607. doi: 10.1016/j.jneb.2018.11.003
53. Nagourney EM, Goodman D, Lam Y, Hurley KM, Henderson J, Surkan PJ. Obese women's perceptions of weight gain during pregnancy: a theory-based analysis. Public Health Nutr. (2019) 22:2228–36. doi: 10.1017/S1368980019000703
54. Oza-Frank R, Conrey E, Bouchard J, Shellhaas C, Weber MB. Healthcare experiences of low-income women with prior gestational diabetes. Matern Child Health J. (2018) 22:1059–66. doi: 10.1007/s10995-018-2489-y
55. Reyes NR, Klotz AA, Herring SJ. A Qualitative Study of Motivators and Barriers to Healthy Eating in Pregnancy for Low-Income, Overweight, African-American Mothers. Journal of the Academy of Nutrition and Dietetics. (2013) 113:1175–81. doi: 10.1016/j.jand.2013.05.014
56. Setse R, Grogan R, Cooper LA, Strobino D, Powe NR, Nicholson W. Weight loss programs for urban-based, postpartum african-american women: Perceived barriers and preferred components. Maternal and Child Health Journal. (2008) 12:119–27. doi: 10.1007/s10995-007-0211-6
57. Siad FM, Fang XY, Santana MJ, Butalia S, Hebert MA, Rabi DM. Understanding the experiences of east african immigrant women with gestational diabetes mellitus. Can J Diabetes. (2018) 42:632–8. doi: 10.1016/j.jcjd.2018.01.013
58. Sterling B, Fowles E, Kim S, Latimer L, Walker LO. Ethnic-specific perceptions of altered control among American women: implications for health promotion programs after pregnancy. Health Care Women Int. (2011) 32:39–56. doi: 10.1080/07399332.2010.529353
59. Tang JW, Foster KE, Pumarino J, Ackermann RT, Peaceman AM, Cameron KA. Perspectives on prevention of Type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White Women. Matern Child Health J. (2015) 19:1526–34. doi: 10.1007/s10995-014-1657-y
60. Whitaker KM, Wilcox S, Liu J, Blair SN, Pate RR. African American and White womens to behavior change g American women: implications for health promotion programs Midwifery. (2016) 34:211–20. doi: 10.1016/j.midw.2015.11.005
61. Quintanilha M, Mayan MJ, Thompson J, Bell RC. Contrasting “back home” and “here”: how Northeast African migrant women perceive and experience health during pregnancy and postpartum in Canada. Int J Equity Health. (2016) 15:80. doi: 10.1186/s12939-016-0369-x
62. Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. (2013) 46:81–95. doi: 10.1007/s12160-013-9486-6
63. Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. (2011) 26:1479–98. doi: 10.1080/08870446.2010.540664
64. Coetzee V, Faerber SJ, Greeff JM, Lefevre CE, Re DE, Perrett DI. African perceptions of female attractiveness. PLoS One. (2012) 7:e48116. doi: 10.1371/journal.pone.0048116
65. Adinma JIB, Adinma ED, Umeononihu OS, Oguaka V, Oyedum SO. Perception and practice of exercise during pregnancy by antenatal women in Southeastern Nigeria. J Gynecol Reprod Health. (2018) 2:1–6. doi: 10.33425/2639-9342.1057
66. Phillips W. Cravings, Marks, and Open Pores: Acculturation and preservation of pregnancy-related beliefs and practices among mothers of African Descent in the United States. Ethos. (2005) 33:231–55. doi: 10.1525/eth.2005.33.2.231
67. Brooten D, Youngblut JM, Golembeski S, Magnus MH, Hannan J. Perceived weight gain, risk, and nutrition in pregnancy in five racial groups. J Am Acad Nurse Pract. (2012) 24:32–42. doi: 10.1111/j.1745-7599.2011.00678.x
68. Bauer C, Graf C, Platschek AM, Strüder HK, et al. Reasons, motivational factors, and perceived personal barriers to engagement in physical activity during pregnancy vary within the BMI classes: the Prenatal Prevention Project Germany. J Phys Act Health. (2016) 15:204–11. doi: 10.1123/jpah.2016-0563
69. Tyler KA. The impact of support received and support provision on changes in perceived social support among older adults. Int J Aging Hum Dev. (2006) 62:21–38. doi: 10.2190/5Y7P-WCL6-LE5A-F4U3
70. Wilbur J, Chandler P, Dancy B, Choi J, Plonczynski D. Environmental, policy, and cultural factors related to physical activity in urban, African American women. Women Health. (2002) 36:17–28. doi: 10.1300/J013v36n02_02
71. Wolfe WA. A review : maximizing social support-a neglected strategy for improving weight management with African-American women. Ethn Dis. (2004) 14:212–8.
72. Kumanyika SK, Wadden TA, Shults J, et al. Trial of family and friend support for weight loss in african american adults. Arch Intern Med. (2009) 169:1795–804. doi: 10.1001/archinternmed.2009.337
73. Bopp M, Peterson JA, Webb BL. A comprehensive review of faith-based physical activity interventions. Am J Lifestyle Med. (2012) 6:460–78. doi: 10.1177/1559827612439285
74. Hou SI, Cao X. A systematic review of promising strategies of faith-based cancer education and lifestyle interventions among racial/ethnic minority groups. J Cancer Educ. (2018) 33:1161–75. doi: 10.1007/s13187-017-1277-5
75. Lynch E, Emery-Tiburcio E, Dugan S, White FS, Thomason C, Jenkins L, et al. Results of alive: a faith-based pilot intervention to improve diet among african american church members. Prog Community Health Partnersh. (2019) 13:19–30. doi: 10.1353/cpr.2019.0005
76. Newlin K, Dyess SM, Allard E, Chase S, Gail D'Eramo M. A methodological review of faith-based health promotion literature: advancing the science to expand delivery of diabetes education to Black Americans. J Religion Health. (2012) 51:1075–97. doi: 10.1007/s10943-011-9481-9
77. Lancaster KJ, Carter-Edwards L, Grilo S, Shen C, Schoenthaler AM. Obesity interventions in African American faith-based organizations: a systematic review. Obesity Rev. (2014) 15:159–76. doi: 10.1111/obr.12207
78. Maynard MJ. Faith-based institutions as venues for obesity prevention. Curr Obesity Rep. (2017) 6:148–54. doi: 10.1007/s13679-017-0257-8
79. Moore AP, Rivas CA, Stanton-Fay S, Harding S, Goff LM. Designing the healthy eating and active lifestyles for diabetes (HEAL-D) self-management and support programme for UK African and Caribbean communities: a culturally tailored, complex intervention under-pinned by behaviour change theory. BMC Public Health. (2019) 19:1146. doi: 10.1186/s12889-019-7411-z
80. Rasmussen K, Yatkine A. Committee to Reexamine IOM Pregnancy Weight Guidelines. Institute of Medicine (US), National Research Council (US) (2009).
81. Iwelunmor J, Newsome V, Airhihenbuwa CO. Framing the impact of culture on health: a systematic review of the PEN-3 cultural model and its application in public health research and interventions. Ethn Health. (2014) 19:20–46. doi: 10.1080/13557858.2013.857768
83. Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
84. Williams SL, French DP. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour–and are they the same? Health Educ Res. (2011) 26:308–22. doi: 10.1093/her/cyr005
85. Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: where should we look and what should we count? Int J Behav Nutr Phys Act. (2006) 3:33. doi: 10.1186/1479-5868-3-33
86. Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. (1998) 280:1371–4. doi: 10.1126/science.280.5368.1371
87. Kok G. A practical guide to effective behavior change: how to apply theory- and evidence-based behavior change methods in an intervention. Eur Health Psychol. (2014) 16:156–70. doi: 10.31234/osf.io/r78wh
88. Batholomew L, Markham C, Ruiter R, Fernandez M, Kok G, Parcel G. Planning Health Promotion Programmes: An Intervention Mapping Approach, 4th edn. San Francisco: Jossey-Boss, John Wiley & Sons (2016).
89. Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. (2008) 57:660–80. doi: 10.1111/j.1464-0597.2008.00341.x
Keywords: pregnancy, postpartum, weight, lifestyle, black African, Caribbean, ethnicity
Citation: Moore AP, Flynn AC, Adegboye ARA, Goff LM and Rivas CA (2021) Factors Influencing Pregnancy and Postpartum Weight Management in Women of African and Caribbean Ancestry Living in High Income Countries: Systematic Review and Evidence Synthesis Using a Behavioral Change Theoretical Model. Front. Public Health 9:637800. doi: 10.3389/fpubh.2021.637800
Received: 04 December 2020; Accepted: 18 January 2021;
Published: 17 February 2021.
Edited by:
Orla Doyle, University College Dublin, IrelandReviewed by:
Ana Santos, University of Porto, PortugalRoch A. Nianogo, UCLA School of Public Health, United States
Copyright © 2021 Moore, Flynn, Adegboye, Goff and Rivas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanda P. Moore, YW1hbmRhLm1vb3JlQGtjbC5hYy51aw==
 Amanda P. Moore
Amanda P. Moore Angela C. Flynn2
Angela C. Flynn2 Amanda Rodrigues Amorim Adegboye
Amanda Rodrigues Amorim Adegboye