
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 March 2021
Sec. Family Medicine and Primary Care
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.625834
This article is part of the Research Topic The Relationship Between Cardiovascular Disease and Other Chronic Conditions View all 39 articles
 Ying-Cheng Chen1,2†
Ying-Cheng Chen1,2† Yin-Yang Chen1,3†
Yin-Yang Chen1,3† Han Wei Yeh4
Han Wei Yeh4 Tung-Ying Yeh5,6
Tung-Ying Yeh5,6 Jing-Yang Huang1,7
Jing-Yang Huang1,7 Pei-Lun Liao7
Pei-Lun Liao7 Liang-Tsai Yeh1,8
Liang-Tsai Yeh1,8 Shun-Fa Yang1,7
Shun-Fa Yang1,7 Ming-Chih Chou1,3*
Ming-Chih Chou1,3* Chao-Bin Yeh1,9,10*
Chao-Bin Yeh1,9,10*This study evaluated the association between long-term low-dose aspirin use and decreased risk of pneumonia in patients with cardio-cerebra-vascular ischemic diseases (CCVDs). This retrospective cohort study used records from Taiwan's National Health Insurance Research Database of claims made between 1997 and 2013. After propensity score matching (PSM), patients who took a low dose of aspirin for more than 90 days within 1 year of diagnosis with CCVDs were identified as the exposure group (n = 15,784). A matched total of 15,784 individuals without aspirin use were selected for the non-aspirin group. The main outcome was the development of pneumonia after the index date. Multivariable Cox regression analysis and Kaplan–Meier survival analysis were performed to estimate the adjusted hazard ratio (aHR) and cumulative probability of pneumonia. The result after PSM indicated a lower hazard ratio for pneumonia in aspirin users (aHR = 0.890, 95% confidence interval = 0.837–0.945). Therefore, patients with CCVDs who took aspirin had a lower risk of developing pneumonia than those who did not. In conclusion, this population-based cohort study demonstrated that long-term low-dose aspirin use is associated with a slightly decreased risk of pneumonia in patients with CCVDs.
Cardio-cerebra-vascular ischemic diseases (CCVDs), a class of disorders involving the heart and blood vessels, are the major leading causes of death worldwide, contributing to decreased quality of life and increased economic burden on patients. CCVDs include coronary heart disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, and pulmonary embolism (1). In Taiwan, coronary heart disease and cerebrovascular disease are the 2nd and 4th leading causes of death, respectively, with mortality rates of 48.8 and 26.1% (2). The average medical costs for the 1st year of myocardial infarction, stoke, and angina were reported to be NT$293,995, NT$141,086, and NT$60,305, respectively (3).
Moreover, CCVDs puts patients at higher risk of comorbidities such as hypertension, diabetes mellitus, pneumonia, heart failure, and arrhythmia. Among these, pneumonia is the 3rd leading cause of death in Taiwan (2). A population-based retrospective cohort study reported that patients with CCVDs had a higher risk of pneumonia than did those without [adjusted hazard ratio (aHR): 2.27, 95% confidence interval (CI): 2.01–2.56, P < 0.001) (4). The coexistence of CCVDs and pneumonia is associated with a high rate of pneumonia-associated 30-day mortality [hazard ratio (HR), 5.490, CI: 2.905–10.374, P < 0.001] (5). Prevention and early treatment of pneumonia in patients with CCVDs is crucial.
Other than lifestyle modifications, antiplatelet therapies such as aspirin play a crucial role for primary and secondary prevention of CCVDs. The cardioprotective effect of aspirin is mainly attributed to the irreversible acetylation of cyclooxygenase (COX)-1 and COX-2 in platelets, resulting in blockade of the production of thromboxane A2 and prostaglandin I2 (PGI2) and inhibiting platelet aggregation and vasoconstriction (6–9). Benefits are achieved with low-dose aspirin (75–100 mg orally daily) according to current trials (10) and guidelines (11).
The anti-infection effects of aspirin have also been studied. The mechanisms by which aspirin affects the immune system and manipulates processes involved in sepsis include the inhibition of COX (12) and nuclear factor kappa B (NF-κB) (13) and the induction of the production of nitric oxide (14) and lipoxin (15). Falcone et al. demonstrated an association between long-term use of aspirin and lower mortality rates (2.07, CI: 1.08–3.98, P = 0.029) in patients with pneumonia (16). Other studies have reported protective effects against viral infections of the respiratory tract (17), infectious endocarditis (18), and pyogenic liver abscess (19).
By contrast, Yayan's retrospective cohort study indicated that rather than exhibit significant anti-infection effects in patients with chronic obstructive pulmonary disease (COPD), aspirin use corresponded to increased infection rates (20). Eisen et al. designed the “AspiriN To Inhibit SEPSIS (ANTISEPSIS) randomized controlled trial protocol” for further research into this topic, but the final data have yet to be reported (21). Moreover, McNeil et al. demonstrated increased all-cause mortality in patient with daily low dose aspirin without indication (22). In response to the lack of consensus on the anti-infection effect of aspirin and the high mortality rate of pneumonia in patients with CCVDs, this study evaluated the association between long-term aspirin use and risk of pneumonia in patients with CCVDs in Taiwan. We hypothesized that aspirin can reduce the risk of pneumonia in patients with CCVDs.
We used the Longitudinal Health Insurance Database (LHID) 2000, which is a subset of the National Health Insurance Research Database (NHIRD), to evaluate the effect of aspirin on the risk of pneumonia. The NHIRD provides real-world evidence for exploring the risk factors or effects of an intervention for specific diseases (23). The LHID 2000 consists of the data of one million beneficiaries who were insured by the National Health Insurance program in 2000. The research timeframe in this study was the 17 years between January 1997 and December 2013. This retrospective population-based cohort study was approved by the National Health Insurance Administration and the Institutional Review Board of Chung Shan Medical University (registration number: CSMUH CS16183).
We included patients with a diagnosis of a CCVDs, including coronary artery disease and ischemic stroke (using International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 410.x to 414. × and 433. × to 436. ×), between January 1, 1997, and December 31, 2013. To reduce the false positive rate of identifying diseases with ICD-9-CM codes (24), patients were excluded if they had outpatient visit records with CCVDs only. The index date was 365 days after the date of first diagnosis with CCVDs. We excluded patients who (a) had index dates before January 2001 (for left-censored or left-truncated data) or after December 2013 (limited due to the research timeframe), (b) were missing demographic data, (c) died before the index date, or (d) developed pneumonia before the index date. In this study, the censored data including withdraw from insurance coverage, death, and end of study (December 31, 2013). Figure 1 illustrates the study framework.
Initially, 22,858 patients with CCVDs and low-dose aspirin use for more than 90 days after their first diagnosis were classified into the aspirin user group. We evaluated the dose of aspirin within 1 year after diagnosis of CCVDs, the median (Q1, Q3) duration of long-term (100 mg per day) aspirin usage was 275-day (152, 365) and the average medication possession ratio (MPR) was 0.71 in exposure group. By contrast, the median of duration was 1-day (0, 15) with average MPR of 0.03 in non-exposure group within 1 year. In addition, we identified the overall dosage during follow up, the median of duration was 807-day with average MPR of 0.58 in exposure group, and the median of duration was 26-day with average MPR of 0.08 in non-exposure group. The remaining individuals comprised the non-aspirin cohort. To reduce potential confounding bias in our results, 1:1 propensity score matching (PSM) was performed using greedy nearest neighbor, non-replacement matching with a caliper width of 0.01. PSM analysis is widely used in retrospective studies to eliminate imbalance in measured confounding factors among subjects in two study groups. The propensity score of exposure was estimated using logistic regression and covariates, including age, sex, and comorbidities (e.g., hypertension, diabetes mellitus, hyperlipidemia, chronic obstruction pulmonary disease (COPD), dementia, cancer, or major bleeding) and co-medication [including corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), proton-pump inhibitors (PPIs), calcium channel blockers (CCBs), Angiotensin-converting-enzyme inhibitors (ACEIs) and statin]. Standardized differences (SDs) were estimated to evaluate the success of balancing baseline covariates between the two study groups; a SD absolute value of <0.1 indicated that the item was balanced between the two groups (25).
Baseline demographic characteristics, such as age and sex, were recorded. Comorbidities, including hypertension, diabetes mellitus, hyperlipidemia, COPD, dementia, cancer, major bleeding, corticosteroids, NSAIDs, PPIs, CCBs, ACEIs and statin within 1 year before the index date, were documented as potential confounding factors. The study event was defined as the diagnosis of pneumonia (ICD-9-CM 480-486.) during an emergency visit or upon hospital admission. All study individuals were followed up from the index date to the study event, date of death, or end of the study (December 31, 2013).
Categorical data are presented as numbers and percentages and were compared using a chi-square test. The incidence rate ratio with corresponding CIs and crude HR were calculated using Poisson regression. After the proportional hazard assumption was tested, Cox proportional hazard model analysis was performed to estimate the HR for pneumonia and 95% CI. Statistical analysis was performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA). The significance level was set at 0.05. The cumulative probability of pneumonia was assessed using Kaplan-Meier analysis, in which statistical significance was based on a log-rank test.
We identified 48,186 patients who had received a CCVDs diagnosis during the period from 2000 to 2012. Of these, 22,858 (47.43%) were using a low dose of aspirin for secondary prevention. The aspirin group had a higher proportion of male patients (61.27%), elderly patients, and patients with comorbidities (such as hypertension, diabetes mellitus, and hyperlipidemia); however, a lower proportion of major bleeding was found in the aspirin group. After PSM, a matched aspirin cohort of 15,784 and non-aspirin cohort of the same number were established for analysis. A comparison of the characteristics of the aspirin users and the non-aspirin users is presented in Table 1. Hypertension was the comorbidity of highest prevalence in both groups, followed by hyperlipidemia and diabetes mellitus. Age, gender, comorbidities, and co-medication of corticosteroids, NSAIDs, PPIs, CCBs, ACEIs and statin were not significantly different between the propensity score matched aspirin and non-aspirin groups.
After PSM, the incidence densities of pneumonia (per 1,000 person months) were 3.60 (CI = 3.48–3.73) and 3.95 (CI = 3.82–4.07) in the aspirin and non-aspirin cohorts, respectively. A Kaplan–Meier survival analysis revealed a significantly lower cumulative incidence of pneumonia in the aspirin group (Figure 2). Compared with patients in the non-aspirin group, those with CVD in the aspirin group exhibited a decreased risk of pneumonia (aHR: 0.890, CI: 0.837–0.945). Other significant risk factors of pneumonia in patients with CCVDs included dementia, DM and COPD (Table 2). The stratified analysis showed the significant protect effect of aspirin in subgroup of male, hypertension, non-DM, COPD, non-dementia, non-cancer, and patients without major bleeding (Table 3).
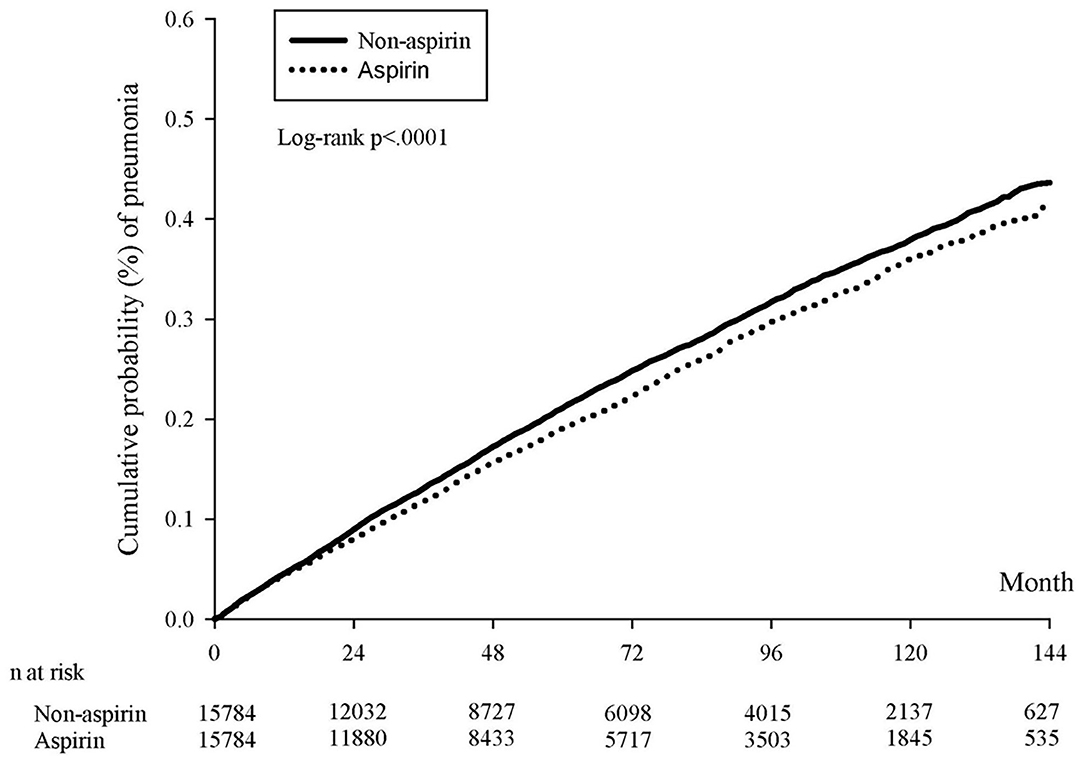
Figure 2. Kaplan–Meier curves of the cumulative proportions of pneumonia after propensity score matching.
This is the first nationwide longitudinal population-based cohort study to evaluate the effect of aspirin on pneumonia in patients with CCVDs, and the findings indicate that long-term low-dose aspirin use is associated with a slightly decreased risk of pneumonia. Aspirin is well-known for secondary prevention in patients with CCVDs and reduces the mortality and disease recurrence of CCVDs (10, 11). We discovered its further ability to reduce the incidence of pneumonia in patients with CCVDs. Nevertheless, for patients with hemorrhagic stroke, how aspirin use affects the risk of major bleeding is still under debate. Hence, we only included patients with ischemic stroke in this study population.
Our findings are consistent with those of other studies on the association between aspirin and infection. A literature review revealed the ability of aspirin to prevent infections. Eisen et al. performed a retrospective cohort study in an intensive care unit setting that showed that the administration of aspirin was associated with 14.8% lower mortality in critically ill patients with sepsis (26). Another nationwide population-based cohort study published in 2015 reported that the administration of aspirin was associated with survival benefit in patients with sepsis (27). Furthermore, a prospective cohort study published in the same year demonstrated that elderly patients with pneumonia who received a low daily dose of aspirin (100 mg/day) had a lower total mortality rate than did those who did not receive any medication (16). In our population, 47.43% of patients were treated with long-term low-dose aspirin and were predominantly male, of old age, and with comorbidities of hypertension, diabetes mellitus, or hyperlipidemia and use of PPI before PSM.
The mechanisms by which aspirin affects the immune system has three main pathways, involving tumor necrosis factor (TNF), lipid mediators, and platelets (21). First, receptors of immune cells can recognize pathogen-associated molecular patterns and modulate intracellular signaling, resulting in the activation of NFκB and the transcription of TNF, a proinflammatory cytokine. Aspirin regulates immune response by inhibiting the activation of NFκB (28). Second, lipid mediators play a part in anti-inflammation and the restoration of homeostasis (29). Low-dose aspirin use increases the number of lipid mediators of lipoxins and resolvins, which inhibit the production of proinflammatory cytokines (30). Finally, aspirin inhibits the activation and aggregation of platelets, and its role in the interaction between platelets and pathogens in immune responses and infections has recently been researched widely (31, 32). The surface receptors of platelets are involved in direct platelet–bacteria interactions, and plasma proteins promote indirect interactions, resulting in the modulation of neutrophils, Kupffer cells, and the complement system (33).
In regard to the definition of pneumonia in our study was described as follows. According to our study design, the index date was 365 days after the date of first diagnosis of CCVDs and patients with previous pneumonia diagnosis were excluded and we only included the newly diagnosis of pneumonia with ICD 9 code from emergencies or hospitalization to confirm the accuracy of diagnosis. Hence, if the diagnosis of pneumonia was made in ER or upon admission, it should represent for community-acquired pneumonia (CAP). On the contrast, if the diagnosis of pneumonia was made during the hospitalization, it could be hospital-acquired pneumonia (HAP). We could not distinguish CAP from HAP only using ICD 9 code and this is one limitation of NHIRD. However, CAP should be the majority of the diagnosis based on the clinical condition. Hence, our study included all cause of pneumonia instead of CAP only. On the other hand, for the accuracy of using ICD 9 code to claim the data of pneumonia, there is one research on this question: International classification of diseases codes showed modest sensitivity for detecting community-acquired pneumonia. Previous study concluded that ICD-9-CM codes showed modest sensitivity for detecting CAP in hospital administrative databases, leaving at least one quarter of pneumonia cases undetected (34). Therefore, sensitivity decreased with longer duration of hospital stay.
Our study demonstrated a 2-fold risk of pneumonia in patients with COPD and patients with dementia, which is in agreement with the findings of other studies. COPD was associated with a higher risk of pneumonia and an increased mortality rate (35, 36). A recent COPD cohort study showed an incidence rate of pneumonia of 22.4 (CI: 21.7–23.2) per 1,000 person years (37). Furthermore, a single center study in Taiwan demonstrated that COPD patients with CCVDs had an increased risk of pneumonia (38). However, dementia was proven to be a risk factor of pneumonia because of prolonged latency of the swallowing reflex (39). A systemic review and meta-analysis published in 2019 reported that the rate of pneumonia-associated mortality was doubled in patients with dementia compared with those without (40). Patients with COPD and dementia require adequate chest care and cautious clinical management for pneumonia prevention and improved prognoses. The non-protection effect of aspirin in COPD patients with pneumonia was consistent with a previous study mentioned, showing that aspirin was associated with higher COPD acute exacerbation and infection events (20). On the other hand, the non-protection effect of aspirin on diabetes mellitus, dementia and cancer population found in our study needs more research to confirm the relevance. The strengths and novelties of our study are as follows. First, a large population cohort with application of PSM provided a balance of selected covariates. Second, pneumonia is associated with higher mortality in CCVDs patients. Our results demonstrate the clinical benefits of aspirin for pneumonia prevention. Finally, aspirin prescriptions are made for patients with CCVDs after careful consideration of two crucial aspects: the reduced risk of death of CCVDs and the increased risk of major bleeding. The results of our study provide supporting evidence of the reduced risk of pneumonia resulting from aspirin use in patients with CCVDs.
This study had some limitations. First, the NHIRD did not contain information on the severity of CCVDs, performance status, or patients' clinical characteristics such as obesity or smoking status. Second, covariates in this study lacked information on the initial treatment of CCVDs, such as medication usage or the necessity of therapeutic or surgical intervention. Third, data on influenza and pneumococcal vaccinations was not included in this study. In Taiwan, the health policy provided annual free influenza and pneumococcal vaccination since 2001 and 2007, respectively, but with age limitation. Annual influenza vaccination was only free for people aged more than 65 years, and pneumococcal vaccination people only for aged more than 75 years, both elder and susceptible group of general population. Finally, a lack of randomization due to the observational nature of this study was an intrinsic limitation. Carefully designed and planned studies using randomized control trials are warranted for precise analysis of the benefits of aspirin.
In summary, this population-based cohort study with PSM demonstrated that long-term low-dose aspirin use is associated with a decreased risk of pneumonia in patients with CCVDs, whereas Diabetes mellitus, COPD and dementia are associated with greater risk of pneumonia. Further randomized clinical trials are required to support these findings before strategies for increasing prevalence of aspirin use among patients with CCVDs can be developed.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
This retrospective population-based cohort study was approved by the National Health Insurance Administration and the Institutional Review Board of Chung Shan Medical University (registration number: CSMUH CS16183). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Y-CC, Y-YC, M-CC, and C-BY conceived and designed the experiments. HY, T-YY, J-YH, and P-LL analyzed the data. L-TY, S-FY, and C-BY contributed reagents, materials, and analysis tools. Y-CC, Y-YC, M-CC, and C-BY wrote the paper. All authors contributed to the article and approved the submitted version.
This study was partly based on data from the NHIRD provided by the NHI Administration, Ministry of Health and Welfare, and managed by the National Health Research Institutes (registration number: NHIRD-104-148). The interpretation and conclusions contained herein do not represent those of the NHI Administration, Ministry of Health and Welfare, or National Health Research Institutes.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
aHRs, adjusted hazard ratios; CCVDs, cardio-cerebra-vascular ischemic disease; NHIRD, National Health Insurance Research Database; COPD, Chronic Obstruction Pulmonary Disease; NSAIDs, Non-steroidal anti-inflammatory drugs; PPIs, Proton-pump inhibitors; CCBs, Calcium channel blockers; ACEIs, Angiotensin-converting-enzyme inhibitors.
1. Mendis S, Puska P, Norrving B, Organization WH. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva:World Health Organization (2011).
2. Health Promotion Administration MOHAW. The Executive Yuan, Taiwan, 2018 Cause of Death Statistics. Taiwan.
3. Tang CH, Chuang PY, Chen CA, Fang YC. Medical costs of cardiovascular diseases in Taiwan. Value Health. (2014) 17:A759–60. doi: 10.1016/j.jval.2014.08.251
4. Yeh JJ, Lin CL, Kao CH. Relationship between pneumonia and cardiovascular diseases: a retrospective cohort study of the general population. Euro J Internal Med. (2019) 59:39–45. doi: 10.1016/j.ejim.2018.08.003
5. Violi F, Cangemi R, Falcone M, Taliani G, Pieralli F, Vannucchi V, et al. Cardiovascular complications and short-term mortality risk in community-acquired pneumonia. Clin Infect Dis. (2017) 64:1486–93. doi: 10.1093/cid/cix164
6. Miner J, Hoffhines A. The discovery of aspirin's antithrombotic effects. Tex Heart Inst J. (2007) 34:179–186.
7. Ittaman SV, VanWormer JJ, Rezkalla SH. The role of aspirin in the prevention of cardiovascular disease. Clin Med Res. (2014) 12:147–54. doi: 10.3121/cmr.2013.1197
8. Vane JR, Botting RM. The mechanism of action of aspirin. Thrombosis Res. (2003) 110:255–8. doi: 10.1016/S0049-3848(03)00379-7
9. Warner TD, Nylander S, Whatling C. Anti-platelet therapy: cyclo-oxygenase inhibition and the use of aspirin with particular regard to dual anti-platelet therapy. Br J Clin Pharmacol. (2011) 72:619–33. doi: 10.1111/j.1365-2125.2011.03943.x
10. Antithrombotic Trialists C. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. (2009) 373:1849–60. doi: 10.1016/S0140-6736(09)60503-1
11. Arnett Donna K, Blumenthal Roger S, Albert Michelle A, Buroker Andrew B, Goldberger Zachary D, Hahn Ellen J, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. (2019) 140:e596–646. doi: 10.1161/CIR.0000000000000678
12. Floyd CN, Ferro A. Mechanisms of aspirin resistance. Pharmacol Therap. (2014) 141:69–78. doi: 10.1016/j.pharmthera.2013.08.005
13. Weber C, Erl W, Pietsch A, Weber Peter C. Aspirin inhibits nuclear factor–κB mobilization and monocyte adhesion in stimulated human endothelial cells. Circulation. (1995) 91:1914–7. doi: 10.1161/01.CIR.91.7.1914
14. Taubert D, Berkels R, Grosser N, Schröder H, Gründemann D, Schömig E. Aspirin induces nitric oxide release from vascular endothelium: a novel mechanism of action. Brit J Pharmacol. (2004) 143:159–65. doi: 10.1038/sj.bjp.0705907
15. El Kebir D, József L, Pan W, Wang L, Petasis NA, Serhan CN, et al. 15-epi-lipoxin A4 inhibits myeloperoxidase signaling and enhances resolution of acute lung injury. Am J Respir Crit Care Med. (2009) 180:311–9. doi: 10.1164/rccm.200810-1601OC
16. Falcone M, Russo A, Cangemi R, Farcomeni A, Calvieri C, Barillà F, et al. Lower mortality rate in elderly patients with community-onset pneumonia on treatment with aspirin. J Am Heart Assoc. (2015) 4:e001595. doi: 10.1161/JAHA.114.001595
17. Glatthaar-Saalmüller B, Mair KH, Saalmüller A. Antiviral activity of aspirin against RNA viruses of the respiratory tract-an in vitro study. Influenza Other Respir Viruses. (2017) 11:85–92. doi: 10.1111/irv.12421
18. Hannachi N, Habib G, Camoin-Jau L. Aspirin effect on Staphylococcus aureus—platelet interactions during infectious endocarditis. Front Med. (2019) 6:217. doi: 10.3389/fmed.2019.00217
19. Liu J-S, Lee C-H, Chuah S-K, Tai W-C, Chang C-C, Chen F-J. Aspirin use is associated with reduced risk for recurrence of pyogenic liver abscess: a propensity score analysis. Sci Rep. (2019) 9:11511. doi: 10.1038/s41598-019-48017-3
20. Yayan J. No significant detectable anti-infection effects of aspirin and statins in chronic obstructive pulmonary disease. Int J Med Sci. (2015) 12:280–7. doi: 10.7150/ijms.11054
21. Eisen DP, Moore EM, Leder K, Lockery J, McBryde ES, McNeil JJ, et al. AspiriN to inhibit SEPSIS (ANTISEPSIS) randomised controlled trial protocol. BMJ Open. (2017) 7:e013636. doi: 10.1136/bmjopen-2016-013636
22. McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. (2018) 379:1519–28. doi: 10.1056/NEJMoa1803955
23. Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, et al. Taiwan's national health insurance research database: past and future. Clin Epidemiol. (2019) 11:349–58. doi: 10.2147/CLEP.S196293
24. Olson KL, Wood MD, Delate T, Lash LJ, Rasmussen J, Denham AM, et al. Positive predictive values of ICD-9 codes to identify patients with stroke or TIA. Am J Manage Care. (2014) 20:e27–34.
25. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stati Med. (2009) 28:3083–107. doi: 10.1002/sim.3697
26. Eisen DP, Reid D, McBryde ES. Acetyl salicylic acid usage and mortality in critically ill patients with the systemic inflammatory response syndrome and sepsis. Crit Care Med. (2012) 40:1761–7. doi: 10.1097/CCM.0b013e318246b9df
27. Tsai M-J, Ou S-M, Shih C-J, Chao P-W, Wang L-F, Shih Y-N, et al. Association of prior antiplatelet agents with mortality in sepsis patients: a nationwide population-based cohort study. Inten Care Med. (2015) 41:806–13. doi: 10.1007/s00134-015-3760-y
28. Takada Y, Bhardwaj A, Potdar P, Aggarwal BB. Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-κB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene. (2004) 23:9247–58. doi: 10.1038/sj.onc.1208169
29. Serhan CN, Chiang N. Lipid-derived mediators in endogenous anti-inflammation and resolution: lipoxins and aspirin-triggered 15-epi-lipoxins. ScientificWorldJournal. (2002) 2:169–204. doi: 10.1100/tsw.2002.81
30. Arita M, Yoshida M, Hong S, Tjonahen E, Glickman JN, Petasis NA, et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci USA. (2005) 102:7671. doi: 10.1073/pnas.0409271102
31. Assinger A. Platelets and infection - an emerging role of platelets in viral infection. Front Immunol. (2014) 5:649. doi: 10.3389/fimmu.2014.00649
32. Klinger MHF, Jelkmann W. Review: role of blood platelets in infection and inflammation. J Interferon Cytokine Res. (2002) 22:913–22. doi: 10.1089/10799900260286623
33. Deppermann C, Kubes P. Platelets and infection. Semin Immunol. (2016) 28:536–45. doi: 10.1016/j.smim.2016.10.005
34. van de Garde EM, Oosterheert JJ, Bonten M, Kaplan RC, Leufkens HG. International classification of diseases codes showed modest sensitivity for detecting community-acquired pneumonia. J Clin Epidemiol. (2007) 60:834–8. doi: 10.1016/j.jclinepi.2006.10.018
35. Restrepo MI, Sibila O, Anzueto A. Pneumonia in patients with chronic obstructive pulmonary disease. Tuberc Respir Dis. (2018) 81:187–97. doi: 10.4046/trd.2018.0030
36. Restrepo MI, Mortensen EM, Pugh JA, Anzueto A. COPD is associated with increased mortality in patients with community-acquired pneumonia. Euro Respirat J. (2006) 28:346. doi: 10.1183/09031936.06.00131905
37. Müllerova H, Chigbo C, Hagan GW, Woodhead MA, Miravitlles M, Davis KJ, et al. The natural history of community-acquired pneumonia in COPD patients: A population database analysis. Respirat Med. (2012) 106:1124–33. doi: 10.1016/j.rmed.2012.04.008
38. Lin S-H, Perng D-W, Chen C-P, Chai W-H, Yeh C-S, Kor C-T, et al. Increased risk of community-acquired pneumonia in COPD patients with comorbid cardiovascular disease. Int J Chron Obstruct Pulmon Dis. (2016) 11:3051–8. doi: 10.2147/COPD.S115137
39. Wada H, Nakajoh K, Satoh-Nakagawa T, Suzuki T, Ohrui T, Arai H, et al. Risk factors of aspiration pneumonia in Alzheimer's disease patients. Gerontology. (2001) 47:271–6. doi: 10.1159/000052811
Keywords: aspirin, pneumonia, risk, database, cardio-cerebra-vascular ischemic diseases
Citation: Chen Y-C, Chen Y-Y, Yeh HW, Yeh T-Y, Huang J-Y, Liao P-L, Yeh L-T, Yang S-F, Chou M-C and Yeh C-B (2021) Association Between Aspirin Use and Decreased Risk of Pneumonia in Patients With Cardio-Cerebra-Vascular Ischemic Disease: A Population-Based Cohort Study. Front. Public Health 9:625834. doi: 10.3389/fpubh.2021.625834
Received: 04 November 2020; Accepted: 25 February 2021;
Published: 18 March 2021.
Edited by:
Cristina Vassalle, Gabriele Monasterio Tuscany Foundation (CNR), ItalyReviewed by:
Charles Feldman, University of the Witwatersrand, South AfricaCopyright © 2021 Chen, Chen, Yeh, Yeh, Huang, Liao, Yeh, Yang, Chou and Yeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao-Bin Yeh, c2t5NWZmQGdtYWlsLmNvbQ==; Ming-Chih Chou, Y3NoeTIzNkBjc2gub3JnLnR3
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.