- Occupational, Economic and Social Psychology, University of Vienna, Vienna, Austria
With the current study, we investigate mechanisms linking sleep quality with work engagement. Work engagement is an affective-motivational state of feeling vigorous, absorbed, and dedicated while working. Drawing from both the effort-recovery model and the job demands-resources framework, we hypothesize that sleep quality should be positively related to work engagement via the replenishment of personal resources that become apparent in mental health and physical health. Because personal resources should gain salience especially in the face of job demands, we hypothesize that overtime as an indicator for job demands should strengthen the positive relationship between mental health and work engagement. We gathered data from 152 employees from diverse industries via an online survey. Results showed that sleep quality was positively related to work engagement (r = 0.20, p < 0.05), and that mental health mediated this relationship (indirect effect: β = 0.23, lower limit confidence interval = 0.13, upper limit confidence interval = 0.34). However, physical health did not serve as a mediator. Overtime turned out to be significantly and positively related to work engagement (r = 0.22, p < 0.01), replicating previous findings, but did not significantly interact with mental health or physical health in predicting work engagement. Overall, the study highlights the significance of sleep quality for employees' mental health and work engagement.
Introduction
The research on sleep and its relationship to factors in the context of work has gained growing attention over the past years. Sleep at night has been acknowledged to play an important role for employees' experiences and behavior at work (1–4). However, little is yet known about the mechanisms linking employees' sleep with their experience and behavior at work, i.e., how sleep affects an employee's experience and behavior. Among others, energetic and self-regulatory resources (5) have been proposed as mechanisms for the relationship between sleep and work engagement. Yet, in order to draw implications for practice and to highlight sleep's significance for employees' health and performance, it is important to gain an even better understanding of the ways in which sleep can influence employees' behavior. This paper aims to contribute to existing research in several ways. First, it aims to contribute to sleep research by shedding light on possible mechanisms, namely mental health and physical health, between sleep quality and well-being at work, represented through work engagement. Second, we would like to broaden the perspective on the Job Demands-Resources (JD-R) model (6, 7) and examine mental and physical health as personal, non-work resources in our conceptual model that link the non-work domain, represented through sleep, and the work domain, represented by work engagement. Also, we would like to examine if indicators of job demands can have similar effects for the relationships within the JD-R as have job demands themselves. Third, we would like to point out the opportunity sleep offers as a self-regulation strategy for improving an employee's own health and performance. E.g., organizations may offer trainings or speeches on topics like sleep hygiene and recovery after work and implement work conditions which support employees in pursuing a healthy lifestyle.
In the following sections, we derive our hypotheses on the relationships between sleep, work engagement, mental and physical health, and overtime from the Job Demands-Resources framework. Figure 1 shows the conceptual model for this study and summarizes our hypotheses. We are taking a perspective in line with the Positive Occupational Psychology framework (8, 9) focusing on positive outcomes and opportunities for promoting employees' mental and physical health and work engagement.
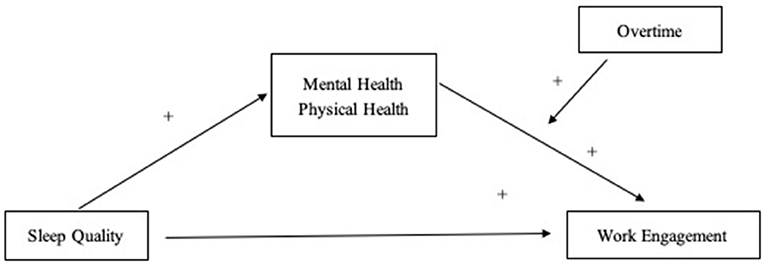
Figure 1. Conceptual model of this study. The “+” indicates that a positive relationship/moderating effect is assumed.
Sleep at Night and Work Engagement
Everybody needs sleep (10). Especially after facing cognitive or physical demands, the human body and mind need rest to restore energy and resources, e.g., self-regulatory or affective resources, and process new information (Effort-Recovery model) (11). Several studies have shown the crucial impact sleep has on mental and physical recovery processes (12–14). Sleep deprivation, on the other hand, can lead to serious consequences for health and performance (10).
Sleep quality appears to be an important predictor for employees' behavior and experience at work, including one of the key concepts in work and health research of the past decade, which is work engagement (15). Bakker, Schaufeli and Salanova (16) define work engagement as the experience of vigor, dedication and absorption at work. Work engagement takes a central role in the JD-R (6, 7) as a desirable, positive outcome being positively associated with an employee's performance (8) contrary to depletion and burnout as negative outcomes.
According to the JD-R model, the presence and availability of resources promotes work engagement. Following the Effort-Recovery model (11) sleep is responsible for restoring resources depleted during the day. Based on this theory, we assume that sleep is positively linked to work engagement via the regeneration of resources. People who sleep better should have more resources available during the day. Thus, they experience more work engagement compared to people who sleep worse. Indeed, the positive relationship between sleep quality and work engagement has already been addressed and supported in previous studies (5, 17–19). Theoretical ideas like both the JD-R framework and the Effort-Recovery model, supported by empirical results, indicate that recharging resources is a linking mechanism in this relationship. Therefore, the relationship between sleep quality and work engagement is the starting point for our hypotheses.
Hypothesis 1. The better employees sleep, the higher is their work engagement.
Sleep at Night, Mental Health, and Physical Health
Sleep at night is crucial for recovery, regenerating resources and thus, for mental and physical health (10). According to Meijman's and Mulder's Effort-Recovery model (11), especially after a demanding and resource-depleting workday, it is important to recover (load effect), i.e., to sleep well and sufficiently, in order to avoid negative load consequences, e.g., for employees' health. Several studies report health impairments after sleep deprivation (20). Reid et al. found sleep to be a significant predictor of both mental and physical health in a sample consisting of elderly people, such that poor sleep quality resulted in poor mental and physical health (21). A 30-day experiment on sleep quality and quantity and mental health showed similar results for young people and students (22). Insomnia and nightmares were found to serve as predictors of impaired mental health, such as paranoia, hallucinations, anxiety, depression, and mania (23). Equivalently, Freeman et al. showed how improving sleep through a Cognitive Behavioral Therapy sleep intervention including measures of sleep hygiene helped reducing symptoms of paranoia and hallucinations (24). Health practices like sufficient restorative sleep, physical exercise, and regular and healthy meals also help with improving the physical health status independently of age, sex, and economic status (25). According to a study on sleep's consequences for physical health, the functioning of T cells is regenerated during sleep, strengthening the immune system and the effectiveness of fighting pathogens (26).
Following our theoretical argumentation based on the effort-recovery model and supported by previous empirical findings, sleep quality should be positively related to both mental and physical health.
Hypothesis 2. The better sleep employees experience, the healthier they are (a) mentally and (b) physically.
Health as a Personal Resource That Enables the Experience of Work Engagement
The presence and accessibility of resources plays a significant role for the extent of work engagement an employee experiences (6). Those resources can be job-related or of personal nature (15). Hobfoll defines a personal resource to be anything that helps individuals to affect and control their environment in order to meet demands in their daily life (27). However, up until now, most studies building on the JD-R framework have examined job-related resources (28). Even personal resources investigated were often indirectly linked to the job context, e.g., an employee's career progression and planning (29) or organizational-based self-esteem (30). However, personal resources play at least an equally important role within the JD-R model as do job resources (15). Xanthopoulou et al. showed that personal resources are positively linked to the perception of accessible job resources (30), implying that personal resources might be even more important. Therefore, we would like to broaden the perspective on the connections within the JD-R model and propose that health is a personal, non-work-related resource and predictor of work engagement.
Health is defined by the World Health Organization (WHO) as “a resource for everyday life, not the objective of living” and “a positive concept emphasizing social and personal resources, as well as physical capacities” (31). This definition reflects the salutogenic perspective on health that has been established over the past decades. Furthermore, it provides a first hint of health being a personal resource. Health can be further regarded as mental or physical. “Mental health includes […] emotional, psychological, and social well-being” (32). Ergo, mental health makes up a significant part of psychosocial functioning (33). Physical health means “the condition of [the] body, taking into consideration everything from the absence of disease to fitness level. [It] is critical for overall well-being […]” (34). The definitions show that mental health and physical health both contribute to the overall health state in their own way, but still, they have a (psychosomatic) connection. Therefore, it is necessary to investigate both mental health and physical health when talking about overall health. Perceived mental and physical health have been found to be related to work engagement (8, 35). Similarly, poor health states can result in reduced productivity (36), job performance, and increased sickness absence, a fact that was acknowledged by developing an instrument to calculate workplace costs caused by health problems (HPQ) (37) and by initiating the annual German Report on Absence from Work (38).
Considering an employee's mental and physical health as important personal resources to draw from, according to the JD-R model, both mental and physical health should be positively linked to work engagement.
Hypothesis 3. The healthier employees are (a) mentally and (b) physically, the more work engagement they show.
One of our aims in the current study is to identify mechanisms between sleep and work engagement. More specifically, we examine how or why sleep quality affects work engagement. Therefore, we hypothesize that both mental health and physical health serve as mediators between sleep quality and work engagement based on the following arguments: First, sleep is positively linked to work engagement via the restoration of personal resources (39). Second, sleep is both responsible for restoring personal resources and maintaining mental and physical health (Hypothesis 2), which themselves are personal resources that enable the experience of work engagement (Hypothesis 3). These considerations result in Hypothesis 4.
Hypothesis 4. Employees' sleep quality is indirectly and positively related to work engagement via (a) better mental health and (b) better physical health.
Overtime as an Indicator for Job Demands
According to the JD-R model, another important aspect when explaining the experience of work engagement is the role of job demands. In the JD-R model, resources are assumed to increase work engagement in employees. Contrary to this, job demands are assumed to cause depletion and burnout (6).
Long work hours are an especially interesting factor to consider when investigating job demands, because they are an indicator for several possible job demands an employee might experience. E.g., high workload and time pressure might cause an employee to work overtime. Overtime hours have been used as an indicator for high workload in several empirical studies (40, 41). Overall, overtime and high workload have been found to have similar effects on employees' health (42): Like job demands, overtime hours can cause strain in employees, raise their cortisol levels and threaten their balance between work and non-work periods (40, 43, 44). We would like to test if overtime as an indicator for job demands with its own potential of damaging employees' health can equally serve as “job demand” within the JD-R model as do job demands themselves.
According to the JD-R theory's Coping Hypothesis, resources gain particular salience in the face of demands (7, 45). This means that job demands trigger employees to invest more resources into their work and this investment leads to even higher work engagement. We expect this to be also true for health as a personal resource and overtime as an indicator for job demands. Results of empirical studies have shown that good health conditions, such as low depression, fatigue or anxiety, good recuperation and well-being, are associated with beneficial coping behavior (46, 47). Consequently, both mental health and physical health should contribute to successfully coping with job demands, like time pressure or high workload, and therefore also with overtime hours. When confronted with job demands, health provides resources that employees can invest in the effort of coping. Hence, being confronted with job demands becoming apparent in overtime hours should cause employees to invest even more mental resources and physical energy into their work. This way, they enable themselves to deal with the demand and therefore boost the effect of good mental and physical health, resulting in even higher work engagement.
Hypothesis 5a. The relationship between mental health and work engagement is stronger for employees who work more overtime hours.
Hypothesis 5b. The relationship between physical health and work engagement is stronger for employees who work more overtime hours.
Materials and Methods
Sample and Procedure
One hundred and fifty-two employees (91 females, 61 males) from companies operating in diverse industries [the top three being services (N = 38); education (N = 24); public health/social affairs (N = 22)] participated in our study. They were recruited for a master thesis project and did not receive compensation for their participation. All subjects gave their informed consent before they participated in the study. The study was conducted in accordance with the ethical guidelines for the treatment of human subjects of the German Psychological Association (48) and the model code of ethics of the European Federation of Psychologists' Associations (49). The participants' age ranged from 19 to 69 (M = 37.91, SD = 12.35). 19.7% of the sample had children and 32.9% were in a leadership position. The sample exclusively consisted of non-shift workers. The regular weekly working hours in our sample ranged from 35 to 55 h (M = 39.44, SD = 5.47) as indicated by participants, while the actual weekly working hours ranged from 35 to 70 h (M = 43.71, SD = 6.66).
The questionnaire was provided via an online survey platform, so participants filled it in using electronic devices. The questionnaire consisted of scales or items retrieved from existing and reliable instruments that are described below.
Measures
Sleep Quality
We assessed sleep quality using a single item (“Please evaluate your overall sleep quality during the last 4 weeks”) from the Pittsburgh Sleep Quality Index (PSQI) (50). This item has been successfully used in previous studies (5, 51) because it represents the core indicator for sleep quality (52). A single item to assess sleep quality shows high correlations with the Morning Questionnaire-Insomnia (MQI) and the PSQI overall score (53). The item-total correlation of the single item assessing sleep quality with all other components of the PSQI is high (r = 0.73, p < 0.001) (54). The rating scale for the sleep quality item ranged from 1 = very bad to 5 = very good.
Work Engagement
We used the 9-item version of the Utrecht Work Engagement Scale, UWES-9 (16). The instrument contains three items for each of the three subcomponents of work engagement, vigor (e.g., “At my work, I feel bursting with energy”), absorption (e.g., “I get carried away when I am working”), and dedication (e.g., “My job inspires me”). Participants answered the items using a Likert scale ranging from 0 = never to 6 = always / every day. Cronbach's alpha was 0.94.
Mental and Physical Health
We used the German 12-item version (55) of the Short-Form Health Survey, SF-12 (56), to assess both mental and physical health. The questionnaire consists of two subscales, one for mental and one for physical health, with six items each. An example item from the mental health subscale is “Have you felt downhearted and low?,” an example item from the physical health subscale is “The following questions are about activities you might do during a typical day. Does your health limit you in these activities? If so, how much?—Climbing several flights of stairs.” Some items should be answered with regard to the last 4 weeks, others are asked in general. Scale ranges vary between two (yes / no) and six points (All of the time to none of the time). A sum score is computed from all items for each of the two subscales, resulting in scores between 0 and 100, high scores representing a good health state. Cronbach's alpha was 0.73 for the physical health subscale and 0.82 for the mental health subscale.
Overtime
Participants indicated the number of hours they actually spent at work each week, in contrast to the number of work hours per week that was agreed on by contract. The difference between the two indicators equals the number of overtime hours.
Statistical Analyses
To test Hypotheses 1 – 3 and 5, we conducted regression analyses using the software SPSS Statistics (IBM) to predict work engagement. For the analysis of Hypothesis 3, we simultaneously entered both mental health and physical health as predictors of work engagement into the regression model. We used the PROCESS macro for SPSS (57) to test for the mediation and moderation effects predicted in Hypotheses 4 and 5.
Results
Correlation Analyses
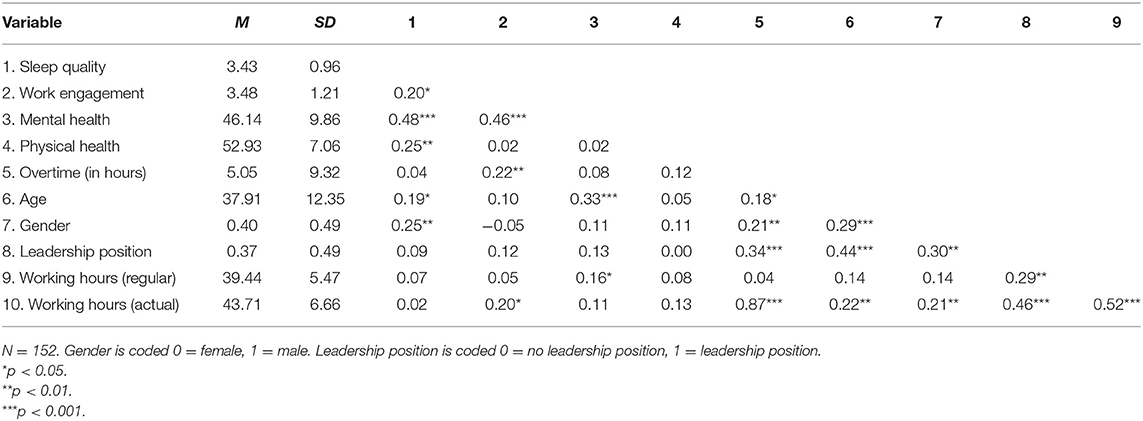
In line with our expectations, sleep quality was significantly and positively correlated with work engagement (r = 0.20, p < 0.05), mental health (r = 0.48, p < 0.001), and physical health (r =0.25, p < 0.01; see Table 1). Table 1 also shows that mental health was significantly and positively related to work engagement (r = 0.46, p < 0.01), but that physical health was not significantly related to work engagement (r = 0.02, p = 0.781). Further, overtime was significantly related to work engagement (r = 0.22, p < 0.01).
Test of Hypotheses
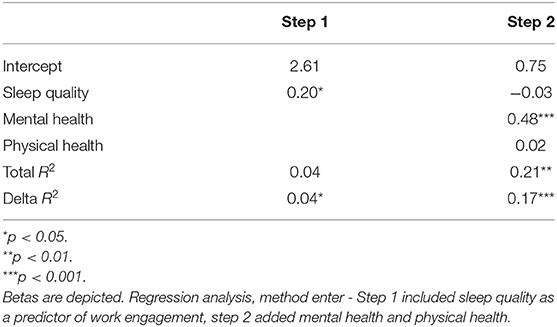
Results of regression analyses to test Hypotheses 1 – 3 and 5 are depicted in Table 2. The regression of work engagement on sleep quality showed that sleep quality was a positive and significant predictor of work engagement (β = 0.20, p < 0.05), yielding support for Hypothesis 1 (see Table 2), which stated that sleep quality should be positively related to work engagement.
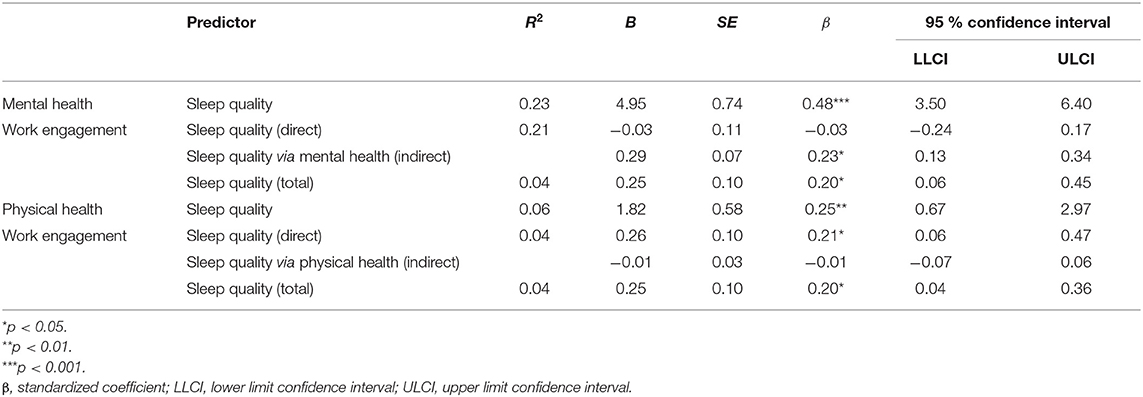
Hypothesis 2 stated a positive effect of sleep quality on mental health (2a) and physical health (2b). Results of regression analyses showed that sleep quality had a significant positive effect on both mental health (β = 0.46, p < 0.001) and physical health (β = 0.25, p < 0.01; see Table 3). These results supported Hypothesis 2.
Hypothesis 3 stated that (a) mental health and (b) physical health should be positively related to work engagement. Results are depicted in Table 2 and showed a significant positive effect of mental health (β = 0.48, p < 0.001) and no significant effect of physical health on work engagement (β = 0.02, p = 0.783). When tested separately as a single predictor, physical health was still not a significant predictor of work engagement. Thus, Hypothesis 3a was supported, while Hypothesis 3b needed to be rejected. Mental health explained a significant amount of variance in work engagement (R2 = 0.21, p < 0.001).
Hypothesis 4 stated indirect effects of sleep quality on work engagement via mental and physical health. Table 3 shows the results of indirect effect models for Hypothesis 4. The indirect effect of sleep quality on work engagement via mental health was significant (β = 0.23, LLCI = 0.13, ULCI = 0.34), i.e., mental health was a mediator in the relationship between sleep quality and work engagement, confirming Hypothesis 4a. The direct effect of sleep quality on work engagement was not significant when mental health was included in the regression model (β = −0.03, LLCI = −0.24, ULCI = 0.17). Furthermore, it was not significantly different from zero, so we could assume that the present mediation was a full one. The indirect effect of sleep quality on work engagement via physical health was not significant (β = −0.01, LLCI = −0.07, ULCI = 0.06), i.e., physical health was not a mediator in the relationship between sleep quality and work engagement, so Hypothesis 4b needed to be rejected. The model consisting of sleep quality as a predictor, mental and physical health as mediators, and work engagement as the criterion explained 21% of data variance in the mediation model.
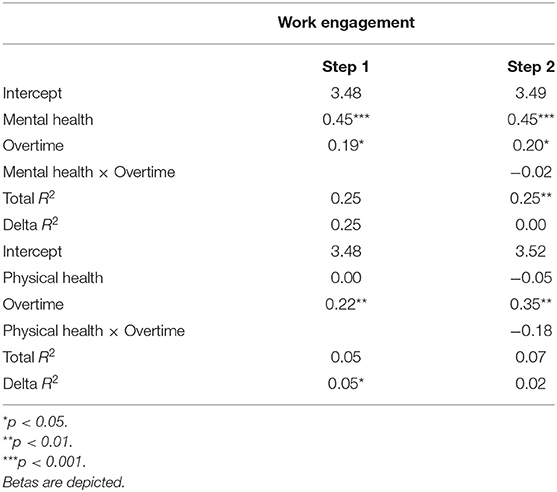
Hypothesis 5 stated overtime hours to moderate the relationship between (a) mental health and (b) physical health and work engagement. Results are depicted in Table 4. The interaction term between mental health and overtime was not significant in predicting work engagement (Mental Health × Overtime: Estimate = −0.02, SE = 0.12, t = −0.22, p = 0.829). We found the same result for the interaction term between physical health and overtime (Physical Health × Overtime: Estimate = −0.18, SE =0.18, t = −1.67, p = 0.097). Consequently, we had to reject Hypothesis 5.
Robustness Checks and Additional Analyses
Following recommendations for correlational and cross-sectional studies (58–60), we repeated all analyses controlling for age, gender, leadership position, and regular and actual weekly working hours. More specifically, we included these variables in the regression analyses testing Hypotheses 1 – 3 as main effects (see Supplementary Table 1). Taking into account employees' age, gender, leadership position, and regular and actual weekly working hours as control variables did not affect our results regarding acceptance or rejection of hypotheses.
Moreover, we also tested gender, leadership position, age, and weekly working hours as moderator(s) of the relationships between sleep, mental health, and work engagement. That is, we investigated if certain relationships were different for, e.g., men vs. women or if certain relationships only existed for a certain group of participants, e.g., only for older participants. Interaction analyses revealed no significant interaction effects between the control variables and any of the predictor variables on any of the outcome variables. This means that the results equally apply to both men and women, employees in leadership positions and in non-leadership positions, older and younger employees, as well as employees working more or less hours. However, leadership position was significantly related to overtime hours and work engagement and that including leadership position as a covariate in the regression analyses erased the effect of overtime hours on work engagement.
Because mental health increases and physical health decreases with age, it is important to consider age-specific norms when interpreting scores on the SF-12 physical health and mental health subscales (61). Thus, we repeated all analyses once more, using the age-corrected difference scores for mental health and physical health (see Supplementary Table 2). Difference scores were calculated comparing each participant's index to the mean index for their age group. The analyses in which we used the age-corrected difference scores did not change the interpretation of the findings.
Discussion
Summary and Discussion of Results
The results largely support our conceptual model and highlight the relevance of sleep and health for employees' work engagement. In line with our predictions derived from the JD-R framework and the Effort-Recovery model, employees' sleep quality was indirectly and positively related to their work engagement via their mental health. The results of the current study thus suggest that (a) mental health does serve as a personal resource and that (b) both mental health and sleep quality can trigger motivational processes in line with the JD-R model. This highlights how valuable good sleep and mental health are for indicators of interest in the context of work, such as work engagement, a desirable experience for employees. Since work engagement is closely related to work performance, sleep and mental health might also boost work performance (15). Furthermore, the results allow a broader perspective on the JD-R model, since they provide a first hint of mental health's role as a personal, non-work resource in the context of the model, which has not received attention thus far.
Contrary to expectations, physical health did not serve as a link between sleep quality and work engagement. While sleep quality and physical health were significantly connected, physical health and work engagement were not. This result suggests that physical health does not serve as a relevant personal resource in the current study.
A possible explanation for why mental health turned out to serve as a personal resource in this context, while physical health did not, is that we investigated our model in a sample of white-collar workers. White-collar workers report higher psychological demands, whereas blue-collar workers report higher physical demands and more physical health complaints (62). Consequently, for white-collar workers, mental health should be more relevant for the affective-motivational state of work engagement (16, 63) than physical health. Equivalently, physical health should be more relevant for blue-collar workers. This assumption coincides with de Jonge's and Dormann's Triple-Match Principle (63) (see below for more details). In a different sample consisting of blue-collar workers, physical health might fit better into the JD-R model and our conceptual model. Thus, future studies might want to investigate physical health as a resource in a sample of blue-collar employees.
Based on the observation that our sample consists of white-collar workers arises another possible explanation for the fact that we could not find similar effects on work engagement for mental health and physical health. Since we excluded shift workers and blue-collar workers, our sample might be rather homogeneous regarding the physical health status. Low variance in our data regarding the physical health component of the SF-12 score could explain the lack of a connection between physical health and work engagement. The SF-12 is composed in a way that allows to compare individual scores to the norm mean index of 50.0 (SD = 10.0) (61). The mean index in our sample was M = 52.93, SD = 7.06, implying that participants were healthier than average, and their health status was relatively homogeneous. Therefore, we cannot rule out this argument as a possible explanation.
According to the JD-R model, overtime and mental health or physical health should have interacted in their prediction of work engagement due to their nature as personal resources and indicator for job demands, which they did not. Following the Triple-Match Principle (63), one possible reason for the rejection of this assumption is that health is not the appropriate resource to cope with overtime or job demands causing overtime. The Triple-Match Principle states that the more demands, resources and outcome variable match one another (triple match), the likelier there will be an interaction between demands and resources in predicting the outcome variable. In order to make a match, variables must be classified as belonging to the same category. For example, emotional demands and emotional resources likely predict emotional outcomes, whereas cognitive demands and cognitive resources likely predict cognitive outcomes. The likelihood for a joint prediction will decrease for a double, single or no match. If, in this case, there is no triple or double match between overtime, health, and work engagement, this could possibly explain why there was no interaction between overtime and health in predicting work engagement. Another explanation could be that physical health operates as a hygiene criterion for work engagement (e.g., like safety at work does for job satisfaction) (64): Physical health's absence could cause work engagement to decline, but its presence is not a booster for work engagement in the face of a job demand or its indicator, i.e., overtime. Finally, one more explanation might be that overtime as an indicator for job demands simply does not work for the JD-R model in the same way as do job demands themselves.
It should be noted that mental health and physical health turned out to be unrelated to each other (r = 0.02, p > 0.05). This means that, in our sample, mentally healthy employees were not physically healthy as well, even though theories of psychosomatic links (10) and results of empirical research (65) suggest that mental and physical health do have a connection. This finding reveals a particularity of our sample.
Interestingly, overtime as an indicator for job demands was positively related to work engagement. This might be a hint at the nature of job demands represented by overtime. Time pressure and high workload, two job demands potentially causing employees to work overtime, have been identified as challenge job demands rather than hindrance job demands (66–68). Challenge demands and resources can have similar effects on work engagement (69). However, when conducting robustness analyses considering age, gender, and leadership position as control variables, the positive relationship between overtime and work engagement disappeared. Further investigations revealed that leadership position was the variable responsible for the effect to disappear, showing that employees in a leadership position report more overtime hours and also more work engagement than employees in non-leadership positions.
Limitations
Our study was designed as a cross-sectional study. Future researchers conducting studies on this topic might want to choose a longitudinal diary design to be able to explore the links between day-to-day fluctuations in sleep and employee experiences and behavior. They might even consider long-term studies to test for long-term effects of sleep quality on changes in health status and changes in work engagement. This might add useful insights to the results from our “momentary snapshot” study.
Another limitation resulting from our study design concerns the monocausal direction of the investigated relationship between sleep quality, health, and work engagement. Sleep quality, health, and work engagement might as well be reciprocally related: Work engagement might depend on sleep quality and mental health and, at the same time, predict sleep quality and mental health. Indeed, previous research provides some support for this idea, showing that work engagement can foster sleep quality. People experiencing more work engagement have less unfinished tasks and lower rumination and subsequently sleep better (70).
Subjective sleep quality has not been sharply defined and correlations with subjective sleep quality indicators, like wake after sleep onset or total sleep time, are medium to low (52). Also, subjective and objective measures for sleep quality do not correlate strongly (52, 71). Therefore, we chose to assess sleep quality using a widely accepted method, which is a single item retrieved from the PSQI (50). This single item is endorsed by Krystal and Edinger (52) in their article about sleep assessments. Still, in future studies, objective measures such as wrist actimetry might be utilized to triangulate the assessment of sleep quality.
Practical Implications
Our study's results reveal some practical implications in the sense of prevention measures aimed at both environmental and behavioral change to be implemented. First, the results suggest that sleep quality is crucial for an employee's mental and physical health and their affective-motivational state at work, represented by work engagement.
Therefore, to foster work engagement, sleep quality may be enhanced. There are several possibilities to achieve better sleep quality, e.g., practicing sleep hygiene strategies (72), like avoiding exposure to blue light before going to bed, i.e., not watching TV or using a smartphone, or strategies for better recovery after work (73). A strategy for better recovery after work is fostering recovery experiences, i.e., mastery of challenging goals, mental detachment from work, relaxation and experience of control in leisure time. Research has shown that employees engaging in sleep hygiene practices experience higher self-regulatory capacity and higher work engagement (17), supporting this recommendation. Organizations may offer talks and speeches on these and other health-related issues (e.g., coping with stress) in order to help employees to promote their sleep quality.
Caring for their own sleep quality offers an opportunity to foster employees' self-regulation that should be supported and trained. Enabling employees to actively and consciously improve their sleep leads to creating more productive employees (74). Therefore, human resource departments that address personnel development should offer trainings and workshops aiming at employees' consciousness and awareness for the topic and at their self-regulation skills. Still, apart from providing possibilities for employees to become active agents for their health, organizations and leaders need to ensure that job characteristics allow employees to get enough restorative sleep. For example, previous research has found demands like time pressure, effort-reward imbalance and unfinished tasks to significantly affect sleep quality negatively via rumination (75). High performance expectations by leaders aggravate this effect (39). Therefore, not only should employees be trained to practice sleep-promoting skills, but also should leaders' awareness for the effects of their actions be raised.
Second, another topic that employees should be aware of is taking care of their own mental health. Mentally healthy employees turned out to experience significantly more work engagement in this study, so enabling employees to improve their own mental health might be beneficial for organizations. Raising employees' awareness by offering relevant health-oriented programs or conveying concrete self-care skills via coaching are two possible strategies to foster employees' mental health. Corporate health management and corporate health promotion are important approaches to create a basis for offering such programs. This study also revealed that promoting sleep quality is one of the basic preconditions for a healthy mind. Further, health-oriented leadership and other employee-oriented leader behavior should be encouraged among supervisors (76) in order to create a healthy work atmosphere and healthy work conditions for employees. Previous research has shown how transformational leadership supports employees in pursuing a healthy lifestyle, e.g., by fostering their work-life-balance (77).
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JK made contributions to the conception and design of the study. RS conceptualized the model, analyzed, interpreted the data, and drafted the manuscript. RS and JK revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Antonia Lorenz for contributing to the conception and design of the study and for collecting the data.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.592850/full#supplementary-material
References
1. Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res. (2002) 53:741–8. doi: 10.1016/S0022-3999(02)00333-1
2. Barling J, Barnes CM, Carleton EL, Wagner DT. Work and Sleep—Insights for the Workplace. New York City, NY: Oxford University Press (2016). doi: 10.1093/acprof:oso/9780190217662.001.0001
3. Barnes CM. Working in our sleep: sleep and self-regulation in organizations. Organ Psychol Rev. (2012) 2:234–57. doi: 10.1177/2041386612450181
4. Kühnel J, Bledow R, Feuerhahn N. When do you procrastinate? Sleep quality and social sleep lag jointly predict self-regulatory failure at work. J Organ Behav. (2016) 37:983–1002. doi: 10.1002/job.2084
5. Kühnel J, Zacher H, de Bloom J, Bledow R. Take a break! Benefits of sleep and short breaks for daily work engagement. Eur J Work Organ Psychol. (2016) 4:481–91. doi: 10.1080/1359432X.2016.1269750
6. Bakker AB, Demerouti E. The job demands-resources model: state of the art. J Manag Psychol. (2007) 22:309–28. doi: 10.1108/02683940710733115
7. Bakker AB, Demerouti E. Job demands-resources theory. In: Chen PY, Cooper CL, editors, Work and Wellbeing: Wellbeing: A Complete Reference Guide (Vol. III). Chichester: Wiley-Blackwell (2014). p. 37–64. doi: 10.1002/9781118539415.wbwell019
8. Schaufeli WB. Work engagement: a key concept of a positive health psychology? In: Proceedings of the Wellness in the Workplace Conference. Bloemfontein (2011).
9. Sonnentag S, Binnewies C, Mojza EJ. Did you have a nice evening? a day-level study on recovery experiences, sleep, and affect. J Appl Psychol. (2008) 93:674–84. doi: 10.1037/0021-9010.93.3.674
10. Higgs S, Cooper A, Lee J. Sleep disturbances and implications for health. In: Higgs S, Cooper A, Lee J, editors, Biological Psychology. 2nd ed. London: Sage (2019).
11. Meijman TF, Mulder G. Psychological aspects of workload. In: Drenth PJD, Thierry H, de Wolff CJ, editors, Handbook of Work and Organizational Psychology: Work Psychology. Hove: Psychology Press (1998). p. 5–28.
12. Åkerstedt T, Nilsson PM, Kecklund G. Sleep and recovery. In: Sonnentag S, Perrewé PL, Ganster DC, editors, Research in Occupational Stress and Well-Being: Current Perspectives on Job-Stress Recovery (Vol. 7). Bingley: JAI Press/Emerald Group Publishing (2009). p. 205–47. doi: 10.1108/S1479-3555(2009)0000007009
13. Fritz C, Crain T. Recovery from work and employee sleep: understanding the role of experiences and activities outside of work. In: Barling J, Barnes CM, Carleton EL, Wagner T, editors, Work and Sleep—Insights for the Workplace. New York City, NY: Oxford University Press (2016). p. 55–76. doi: 10.1093/acprof:oso/9780190217662.003.0004
14. Nägel IJ, Sonnentag S. Exercise and sleep predict personal resources in employees' daily lives. Appl Psychol. (2013) 5:348–86. doi: 10.1111/aphw.12014
15. Schaufeli WB, Taris TW. A critical review of the Job Demands-Resources Model: implications for improving work and health. In: Bauer GF, Hämmig O, editors, Bridging Occupational, Organizational and Public Health. Dordrecht: Springer (2014). p. 43–68. doi: 10.1007/978-94-007-5640-3_4
16. Bakker AB, Schaufeli WB, Salanova M. The measurement of work engagement with a short questionnaire: a cross-national study. Educ Psychol Meas. (2006) 66:701–16. doi: 10.1177/0013164405282471
17. Barber L, Grawitch MJ, Munz DC. Are better sleepers more engaged workers? A self-regulatory approach to sleep hygiene and work engagement. Stress Health. (2013) 29:307–16. doi: 10.1002/smi.2468
18. Diestel S, Rivkin W, Schmidt KH. Sleep quality and self-control capacity as protective resources in the daily emotional labor process: results from two diary studies. J Appl Psychol. (2015) 100:809–27. doi: 10.1037/a0038373
19. Yuan Z, Boyd E, Shockley KM. Did you sleep well? A diary study on sleep, work engagement, and family satisfaction. Acad Manag Proc. (2017) 2015:11558. doi: 10.5465/ambpp.2015.11558abstract
20. Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. Int J Clin Med. (2007) 3:519–28. doi: 10.5664/jcsm.26918
21. Reid KJ, Martinovich Z, Finkel S, Statsinger J, Golden R, Harter K, et al. Sleep: a marker of physical and mental health in the elderly. Am J Geriatr Psychiatry. (2006) 14:860–6. doi: 10.1097/01.JGP.0000206164.56404.ba
22. Sano A, Phillips AJ, Yu AZ, McHill AW, Taylor S, Jaques N, et al. Recognizing academic performance, sleep quality, stress level, and mental health using personality traits, wearable sensors and mobile phones. In: Proceedings of the IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN). Cambridge, MA (2015). doi: 10.1109/BSN.2015.7299420
23. Sheaves B, Porcheret K, Tsanas A, Espie CA, Foster RG, Freeman D, et al. Insomnia, nightmares and chronotype as markers of risk for severe mental illness. Sleep. (2016) 39:173–81. doi: 10.5665/sleep.5342
24. Freeman D, Sheaves B, Goodwin G, Yu LM, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Psychiatry. (2017) 4:749–58. doi: 10.1016/S2215-0366(17)30328-0
25. Belloc NB, Breslow L. Relationship of physical health status and health practices. Prev Med. (1972) 1:409–21. doi: 10.1016/0091-7435(72)90014-X
26. Dimitrov S, Lange T, Gouttefangeas C, Jensen ATR, Szczepanski M, Lehnnolz J, et al. Gαs-coupled receptor signaling and sleep regulate integrin activation of human antigen-specific T cells. J Exp Med. (2019) 216:517. doi: 10.1084/jem.20181169
27. Hobfoll SE. Social and psychological reesources and adaptations. Rev Gen Psychol. (2002) 6:302–24. doi: 10.1037/1089-2680.6.4.307
28. Lee JY, Rocco TS, Shuck B. What is a resource: toward a taxonomy of resources for employee engagement. Hum Resour Dev Rev. (2019) 2019:1–34. doi: 10.1177/1534484319853100
29. Goel AK, Gupta N, Rastogi R. Measuring the level of employee engagement: a study from Indian automobile sector. Int J Indian Cult Bus Manag. (2013) 6:5–21. doi: 10.1504/IJICBM.2013.050710
30. Xanthopoulou D, Bakker AB, Demerouti E, Schaufeli WB. The role of personal resources in the job demands-resources model. Int J Stress Manag. (2007) 12:121–41. doi: 10.1037/1072-5245.14.2.121
31. World Health Organization. The Ottawa Charter for Health Promotion. (1986). Available online at: https://www.who.int/healthpromotion/conferences/previous/ottawa/en/ (accessed March 5, 2021).
32. U.S. Department of Health and Human Services. What Is Mental Health? (2019). Available online at: https://www.mentalhealth.gov/basics/what-is-mental-health (accessed March 5, 2021).
33. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
34. European Patients' Academy. Physical Health. (2015). Available online at: https://www.eupati.eu/glossary/physical-health/ (accessed March 5, 2021).
35. Bakker AB, Schaufeli WB, Leiter MP, Taris TW. Work engagement: an emerging concept in occupational health psychology. Work Stress. (2008) 22:187–200. doi: 10.1080/02678370802393649
36. Alavinia SM, Molenaar D, Burdorf A. Productivity loss in the workforce: associations with health, work demands, and individual characteristics. Am J Ind Med. (2008) 52:ajim.20648. doi: 10.1002/ajim.20648
37. Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The world health organization health and work performance questionnaire (HPQ). J Occup Environ Med. (2003) 45:156–74. doi: 10.1097/01.jom.0000052967.43131.51
38. Badura B, Ducki A, Schröder H, Klose J, Meyer M. Fehlzeiten-Report 2018: Sinn erleben – Arbeit und Gesundheit. Heidelberg: Springer (2018). doi: 10.1007/978-3-662-57388-4
39. Syrek C, Antoni CH. Unfinished tasks foster rumination and impair sleeping – particularly if leaders have high performance expectations. J Occup Health Psychol. (2014) 19:490–9. doi: 10.1037/a0037127
40. Lundberg U, Hellström B. Workload and morning salivary cortisol in women. Work Stress. (2002) 16:356–63. doi: 10.1080/0267837021000064427
41. Krantz G, Lundberg U. Workload, work stress, and sickness absence in Swedish male and female white-collar employees. Scand J Public Health. (2006) 34:238–46. doi: 10.1080/14034940500327372
42. Burke RJ, Fiksenbaum L. Work hours, work intensity, and work addiction: costs and benefits. In: Burke RJ, Cooper CL, editors, The Long Work Hours Culture – Causes, Consequences and Choices. Bingley: Emerald Group Publishing (2008). p. 3–36. doi: 10.1093/oxfordhb/9780199211913.003.0012
43. Albertsen K, Rafnsdóttir GL, Grimsmo A, Tomasson K, Kauppinen K. Workhours and worklife balance. Scand J Work Env Hea. (2008) 5:14–21.
44. Hsu YY, Bai CH, Yang CM, Huang YC, Lin TT, Lin CH. Long hours' effects on work-life balance and satisfaction. BioMed Res Int. (2019) 2019:5046934. doi: 10.1155/2019/5046934
45. Bakker AB, Hakanen JJ, Demerouti E, Xanthopoulou D. Job resources boost work engagement, particularly when job demands are high. J Educ Psychol. (2007) 99:274–84. doi: 10.1037/0022-0663.99.2.274
46. Astvik W, Melin M. Coping with the imbalance between job demands and resources: a study of different coping patterns and implications for health and quality in human service work. J Soc Work. (2012) 13:337–60. doi: 10.1177/1468017311434682
47. Mark G, Smith AP. Occupational stress, job characteristics, coping, and the mental health of nurses. Br J Health Psychol. (2012) 17:505–21. doi: 10.1111/j.2044-8287.2011.02051.x
48. Föderation deutscher Psychologenvereinigungen. Berufsethische Richtlinien. (2016). Available online at: https://www.dgps.de/fileadmin/documents/Empfehlungen/ber-foederation-2016.pdf (accessed March 5, 2021).
49. European Federation of Pychologists' Associations Board of Ethics. Model Code of Ethics. (2015). Available online at: http://ethics.efpa.eu/metaand-model-code/model-code/ (accessed March 5, 2021).
50. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
51. Hülsheger UR, Lang JW, Depenbrock F, Fehrmann C, Zijlstra FR, Alberts H. The power of presence: the role of mindfulness at work for daily levels and change trajectories of psychological detachment and sleep quality. J Appl Psychol. (2014) 99:1113–28. doi: 10.1037/a0037702
52. Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. (2008) 9:10–7. doi: 10.1016/S1389-9457(08)70011-X
53. Snyder E, Cai B, DeMuro C, Morrison MF, Ball W. A new single-item sleep quality scale: results of psychometric evaluation in patients with chronic primary insomnia and depression. J Clin Sleep Med. (2018) 14:1849–57. doi: 10.5664/jcsm.7478
54. Hahn VC, Binnewies C, Sonnentag S, Mojza EJ. Learning how to recover from job stress: effects of a recovery training program on recovery, recovery-related self-efficacy, and well-being. J Occup Health Psychol. (2011) 16:202–16. doi: 10.1037/a0022169
55. Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 health survey. Z Gesundheitswiss. (1995) 3:21–36. doi: 10.1007/BF02959944
56. Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
57. Hayes AF. Process: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling. (2012). Available online at: http://www.afhayes.com/ public/process2012.pdf (accessed March 5, 2021).
58. Spector PE, Brannick MT. Methodological urban legends: the misuse of statistical control variables. Organ Res Methods. (2010) 14:1–19. doi: 10.1177/1094428110369842
59. Becker TE, Atinc G, Breaugh JA, Carlson KD, Edwards JR, Spector PE. Statistical control in correlational studies: 10 essential recommendations for organizational researchers. J Organ Behav. (2018) 37:157–67. doi: 10.1002/job.2053
60. Spector PE. Do not cross me: optimizing the use of cross-sectional designs. J Bus Psychol. (2019) 34:125–37. doi: 10.1007/s10869-018-09613-8
61. Utah Department of Health. Utah Health Status Survey. (2001). Available online at: http://health.utah.gov/opha/publications/2001hss/sf12/SF12_Interpreting.pdf (accessed March 5, 2021).
62. Schreuder KJ, Roelen CA, Koopmans PC, Groothoff JW. Job demands and health complaints in white and blue collar workers. Work. (2008) 31:425–32.
63. de Jonge J, Dormann C. Stressors, resources, and strain at work: a longitudinal test of the Triple-Match Principle. J Appl Psychol. (2006) 91:1359–74. doi: 10.1037/0021-9010.91.5.1359
65. Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: a mediation analysis. Soc Sci Med. (2017) 195:42–9. doi: 10.1016/j.socscimed.2017.11.008
66. Baethge A, Vahle-Hinz T, Schulte-Braucks J, van Dick R. A matter of time? Challenging and hindering effects of time pressure on work engagement. Work Stress. (2018) 32:228–47. doi: 10.1080/02678373.2017.1415998
67. Van den Broeck A, De Cuyper N, De Witte H, Vansteenkiste M. Not all job demands are equal: job hindrances and job challenges in the Job Demands-Resources Model. Eur J Work Organ Psychol. (2010) 19:735–59. doi: 10.1080/13594320903223839
68. Sonnentag S, Casper A, Pinck AS. Job stress and sleep. In: Barling J, Barnes, CM, Carleton, EL, Wagner T, editors, Work and Sleep – Insights for the Workplace. New York City, NY: Oxford University Press (2016). p. 77–100. doi: 10.1093/acprof:oso/9780190217662.003.0005
69. Crawford ER, LePine JA, Rich BL. Linking job demands and resources to employee engagement and burnout: a theoretical extension and meta-analytic test. J Appl Psychol. (2010) 95:834–48. doi: 10.1037/a0019364
70. Syrek CJ, Weigelt O, Peifer C, Antoni C. Zeigarnik's sleepless nights: how unfinished tasks at the end of the week impair employee sleep on the weekend through rumination. J Occup Health Psychol. (2017) 22:225–38. doi: 10.1037/ocp0000031
71. Boudebesse C, Geoffroy PA, Bellivier F, Henry C, Folkard S, Leboyer M, et al. Correlations between objective and subjective sleep and circadian markers in remitted patients with bipolar disorder. Chronobiol Int. (2014) 31:698–704. doi: 10.3109/07420528.2014.895742
72. Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med. (2006) 29:223–7. doi: 10.1007/s10865-006-9047-6
73. Sonnentag S, Fritz C. The recovery experience questionnaire: development and validation of a measure for assessing recuperation and unwinding from work. J Occup Health Psychol. (2007) 12:204–21. doi: 10.1037/1076-8998.12.3.204
74. Rosekind MR, Gregory B, Mallis MM, Brandt SL, Seal B, Lerner D. The cost of poor sleep: workplace productivity loss and associated costs. J Occup Environ Med. (2010) 52:91–8. doi: 10.1097/JOM.0b013e3181c78c30
75. Berset M, Elfering A, Lüthy S, Lüthi S, Semmer NK. Work stressors and impaired sleep: rumination as a mediator. Stress Health. (2011) 27:e71–82. doi: 10.1002/smi.1337
76. Franke F, Felfe J. Diagnose gesundheitsförderlicher Führung – Das Instrument “Health-oriented Leadership.” In: Badura B, Ducki A, Schröder H, Klose J, Macco K, editors, Fehlzeiten-Report, Vol. 2011. Berlin, Heidelberg: Springer (2011). p. 3–13. doi: 10.1007/978-3-642-21655-8_1
Keywords: sleep, work engagement, mental health, job demands - resources model, resources
Citation: Schleupner R and Kühnel J (2021) Fueling Work Engagement: The Role of Sleep, Health, and Overtime. Front. Public Health 9:592850. doi: 10.3389/fpubh.2021.592850
Received: 12 August 2020; Accepted: 28 April 2021;
Published: 20 May 2021.
Edited by:
Daniel P. Bailey, Brunel University London, United KingdomReviewed by:
Catherine Bodeau-Pean, Independent Researcher, Paris, FranceJens Brandt, International School of Management, Germany
Copyright © 2021 Schleupner and Kühnel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ricarda Schleupner, cmljYXJkYS5zY2hsZXVwbmVyQHVuaXZpZS5hYy5hdA==
 Ricarda Schleupner
Ricarda Schleupner Jana Kühnel
Jana Kühnel