
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 09 December 2021
Sec. Public Mental Health
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.590458
This article is part of the Research TopicSystem level Interventions, Prevention Strategies, Mitigation Policies and Social Responses during COVID-19 that Improve Mental Health Outcomes: Evidence from Lower- and Middle-Income Countries (LMICs)View all 32 articles
 Victor Archibong1*
Victor Archibong1* Ibe Michael Usman2*
Ibe Michael Usman2* Keneth Iceland Kasozi3*
Keneth Iceland Kasozi3* Eric Osamudiamwen Aigbogun Jr.2
Eric Osamudiamwen Aigbogun Jr.2 Ifie Josiah2
Ifie Josiah2 Ann Lemuel Monima1
Ann Lemuel Monima1 Robinson Ssebuufu4
Robinson Ssebuufu4 Gaudencia Chekwech5
Gaudencia Chekwech5 Swase Dominic Terkimbi2
Swase Dominic Terkimbi2 Okon Owoisinke6
Okon Owoisinke6 Ngala Elvis Mbiydzenyuy7
Ngala Elvis Mbiydzenyuy7 Azeez Adeoye2
Azeez Adeoye2 Joshua Ojodale Aruwa2
Joshua Ojodale Aruwa2 Adam Moyosore Afodun8
Adam Moyosore Afodun8 Saidi Odoma9
Saidi Odoma9 Fred Ssempijja2
Fred Ssempijja2 Emmanuel Tiyo Ayikobua10
Emmanuel Tiyo Ayikobua10 John Tabakwot Ayuba2
John Tabakwot Ayuba2 Viola Nankya11
Viola Nankya11 Comfort Onongha11
Comfort Onongha11 Sussan Henry11
Sussan Henry11 Kevin Matama9
Kevin Matama9 Helen Yusuf12
Helen Yusuf12 Halima Nalugo13
Halima Nalugo13 Ewan MacLeod3
Ewan MacLeod3 Susan Christina Welburn3,14*
Susan Christina Welburn3,14*Background: Low-income earners are particularly vulnerable to mental health, consequence of the coronavirus disease 2019 (COVID-19) lockdown restrictions, due to a temporary or permanent loss of income and livelihood, coupled with government-enforced measures of social distancing. This study evaluates the mental health status among low-income earners in southwestern Uganda during the first total COVID-19 lockdown in Uganda.
Methods: A cross-sectional descriptive study was undertaken amongst earners whose income falls below the poverty threshold. Two hundred and fifty-three (n = 253) male and female low-income earners between the ages of 18 and 60 years of age were recruited to the study. Modified generalized anxiety disorder (GAD-7), Spielberger's State-Trait Anger Expression Inventory-2 (STAXI-2), and Beck Depression Inventory (BDI) tools as appropriate were used to assess anxiety, anger, and depression respectively among our respondents.
Results: Severe anxiety (68.8%) followed by moderate depression (60.5%) and moderate anger (56.9%) were the most common mental health challenges experienced by low-income earners in Bushenyi district. Awareness of mental healthcare increased with the age of respondents in both males and females. A linear relationship was observed with age and depression (r = 0.154, P = 0.014) while positive correlations were observed between anxiety and anger (r = 0.254, P < 0.001); anxiety and depression (r = 0.153, P = 0.015) and anger and depression (r = 0.153, P = 0.015).
Conclusion: The study shows the importance of mental health awareness in low resource settings during the current COVID-19 pandemic. Females were identified as persons at risk to mental depression, while anger was highest amongst young males.
COVID-19 emerged in Africa on February 14th, 2020 with the first case reported in Egypt. To date 54 countries on the African sub-continent have now reported cases of COVID-19 (1). Uganda reported its first confirmed case on 22 March 2020, from a 36-year-old male who had traveled from Dubai (2, 3). On 18th March 2020, the President of Uganda announced the first total national lockdown which included the international border closures; the closing of schools, private offices and banned public gatherings at places of worships/social events, initially for a period of 32 days (4). Efforts to prevent the spread of COVID-19, effectively closed off most sources of income for the majority of low-income earners, who were forced to stay at home. The resulting decrease in household income impacted on food security and hunger and boredom have impacted on mental health and well-being, complicating adjustment to existence under the COVID-19 lockdown (5). Social distancing measures proposed by health experts and adopted by government lead to social isolation, especially in low-income settings where resources are limited and social networks are cut off by a lack of disposable income. Incidence of domestic violence has increased under conditions of social lockdown, exacerbated by economic uncertainty and stress; reports of domestic violence have been reported as tripling in some countries following previously reported increased rates of child abuse, neglect, and exploitation during previous public health emergencies, for example during the 2014–2016 Ebola outbreak in West Africa (5).
Mental health illnesses and drug abuse are common consequences observed during infectious disease outbreaks because of psychological distress, frustration, and unemployment (6, 49). There are concerns that the COVID-19 pandemic will lead to a mental health crisis, especially in countries with high disease burden (7). Unpredictability, uncertainty, disease severity, misinformation, and social isolation all contribute to stress and mental morbidity (8). Asmundson and Taylor (9, 10) and Xiao et al. (11) reported anxiety to be the most common of individual mental health symptoms, associated with impaired sleep. Mitsuishi and Ries (12) reported that stigmatization from an infectious disease such as COVID-19 could lead to depression in those afflicted.
Elevated levels of stress or anxiety as a function of disruption of livelihoods that lead to an increase in levels of depression, loneliness, harmful alcohol use, self-harm, or suicidal behavior which interferes with how people adjust in difficult situations in this era of the pandemic (1). Studies assessing the mental health status of respondents in developing countries are however, scarce. Common stressors include the risk of being infected and infecting others, health anxiety manifesting in form of mistaking common symptoms of other health problems such as fever for COVID-19, leading to fear of infection (13, 14).
Constant fear, worry and uncertainty combined with individual stressors within the population is likely to have long-term consequences within communities, families and vulnerable individuals. This manifests in the form of possible higher emotional state, anger and aggression against government, frontline workers, partners, and children (13, 14) and sometimes, fear and behaviors are modeled by ignorance, and misinformation (13, 14).
Low-income earners are defined as individuals in work whose income falls below the poverty line and an average Ugandan survives on < $1 US per day (15). Economic pressure associated with the pandemic has not been explored in low resource settings, thus undermining the mental health status of most Africans. This is important since persons in these communities work longer hours, earn less, and have a high dependent-income ratio (16). This study aimed to assess the mental health status among low income earners in Bushenyi district of southwestern Uganda during the first total COVID-19 lockdown.
This was a cross-sectional study conducted amongst low-income earners i.e., boda-boda riders, taxi drivers, taxi turn-boys in the taxi-park, market sellers, barbers, hairdressers, photocopier attendants, and street food sellers in Bushenyi district (Figure 1).
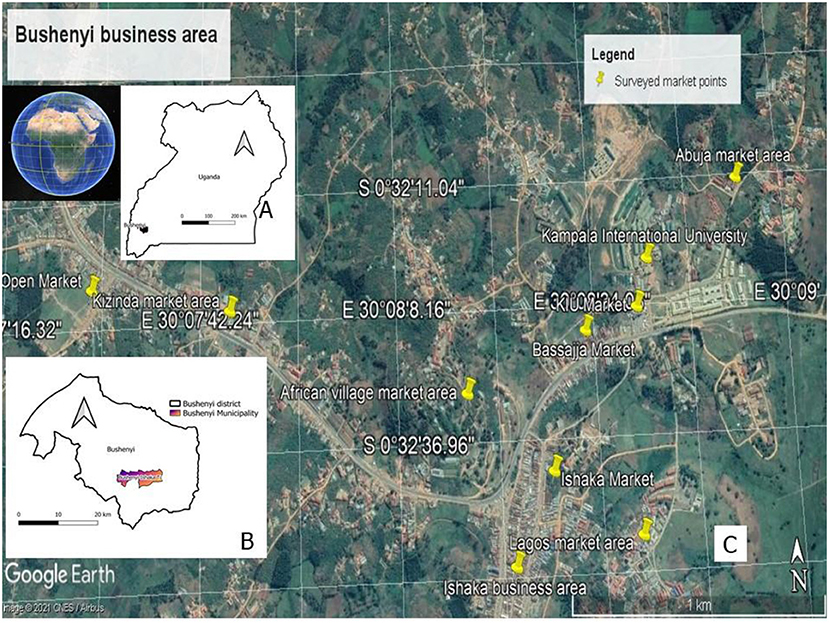
Figure 1. Description of the study area. The study was conducted in Uganda (A) which is an East African country. In particular, the surveyed participants where located in Bushenyi Municipality (B), covering a total of 10 market areas (C). Market areas visited included: Kizinda market area, Kizinda open market, African village market area, Ishaka business area, Ishaka open market, Bassajja market, Kampala International University (KIU), KIU open market, Lagos market area, and Abuja market areas (C).
The study population consisted of males and females (n = 253) above 18 years of age, who have resided in the region for the past 12 months. This was important since these had permanent businesses and were residents in the area, thus able to assess how the pandemic has changed their work routine.
Individuals who refused to participate in the study or casual laborers and those not involved in the financial management of the business. In addition, individuals who owned other businesses outside the study area, although residents in the area were excluded from the survey.
An electronic questionnaire was shared with participants to assess their mental health, anger, anxiety, and depression status. Awareness of mental health care was assessed using simple questions and each of the options provided were assigned scores. Anxiety was assessed using a modified generalized anxiety disorder (GAD-7) item tool (17). Each of the responses attracted scores. Anger was assessed using a modified Spielberger's State-Trait Anger Expression Inventory-2 (STAXI-2) (18). Responses for each question were assigned scores. Depression was assessed using a modified Beck Depression Inventory (BDI) (19). Responses for each of the questions were assigned scores. The questionnaire consisted of multiple-choice unambiguous questions, and respondents who could not understand the questions had the questions interpreted in the local language for them by team members who could communicate effectively in the local vernacular. A Google format of the questionnaire was used to minimize physical contact and maintain social distancing according to the guidelines by WHO and the Ministry of Health in Uganda (Supplementary Material 1).
Data from the survey was entered into Microsoft Excel (2016) and scores were assigned to each option as follows: Mental Health Care Awareness (Q5 – Q10): Numerical values – Mental Health Awareness [Correct response = 1, Incorrect response = 0]. Modified GAD Assessment of Anxiety (Q11 – Q16): Numerical values – Multiple response [For each option selected = 1, indifferent = 0].Modified STAXI-2 Assessment for Anger (Q17 – Q23): Numerical values – Multiple response [For each option selected = 1, indifferent = 0].Modified BDI Assessment for Depression (Q24 – Q30): Numerical values – Single graded response [Highest grade of 3, indifferent = 0].
Anxiety, Anger, and Depression were the mental health concerns of interest, while awareness was an influence variable of significant interest. These variables were obtained using interviewer-based questionnaires. The data were assessed for completeness and responses failing to meet the 75% cut-off (on all valid questions) were excluded. Scores of the multiple options for the modified GAD, and STAXI-2 were obtained by assigning one (1) mark per response, and the averages were obtained by summing all scores (qt) and dividing the number of questions (n). While BDI had four (4) options graded as 3, 2, 1, and 0 (for indifferent). For specific graded questions (yes, sometimes, or no), scores; 2, 1, 0 were assigned and all questions in this form were cumulated (per row), added, then divided by the maximum assigned weight (w) and the distribution (n). This provided the score (Level-score), which is then rated (name of condition; awareness, anxiety, depression, or anger) using cut-offs. To determine the level of awareness and mental state, the composite scores were grade; awareness (no; <0.3, low; 0.30–0.69, high; ≥70) and mental state (no/mild; <0.20, moderate; 20–0.49 or severe; ≥50). This scoring and grading system allows for both linear and uni/multivariate logistic regression analysis.
Data was transferred to Minitab® 18.1 (Minitab, Inc. 2017, Pennsylvania, USA) and all relevant analysis was carried out. The data was not uniformly distributed and principal component analysis (PCA) was used to observe the uncorrelatedness of the dependent variables and determine how they account for differences and separated the socio-demographic variables into components. Spearman Rho correlation was used to observe the relationship between age, awareness, anxiety, anger, and depression, then all significant correlates were regressed using a system-assisted regression model. All analyses were performed at a 95% confidence level and p-values < 0.05 were taken to be significant.
The study comprised of 150 males (59.3%) and 103 females (40.7%), with more middle-aged adults (170/253; 67.2%) compared to younger (65/253; 25.7%) and older (18/253; 7.1%) adults. The proportion of low-income earners in western Uganda with awareness of mental health care was 126/253 (49.8%). A high proportion of low-income earners reported to have experienced severe anxiety 174/253 (68.8%), moderate depression 144/253 (56.9) and moderate anger 153/253 (60.5) (Table 1).
The mean percentage score for awareness in male and female respondents were 63.8 and 63.2%, respectively. Female respondents reported anxiety, anger, and depression of 43.6, 56.5, and 27.5%, respectively, while male respondents reported anxiety, anger, and depression of 43.4, 54.5, and 25.4%, respectively (Figure 2).
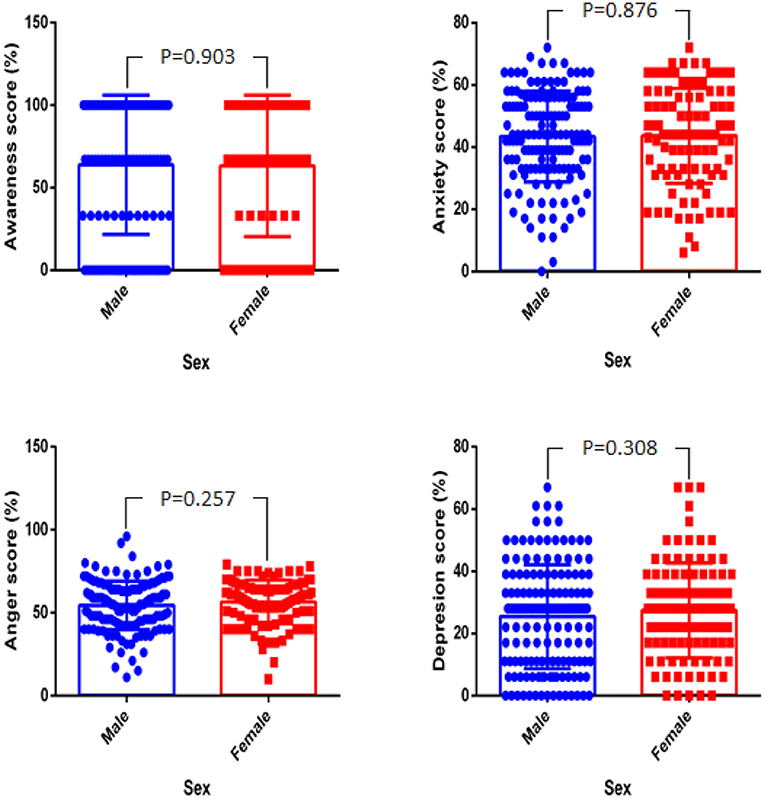
Figure 2. Percentage score difference for awareness, anxiety, anger, and depression between male and female.
The study also showed that older adults had higher awareness of mental health, lower anxiety, anger, and depression than middle-aged and younger adults (Figure 3); however, the difference in the scores was only significant for depression (P = 0.03).
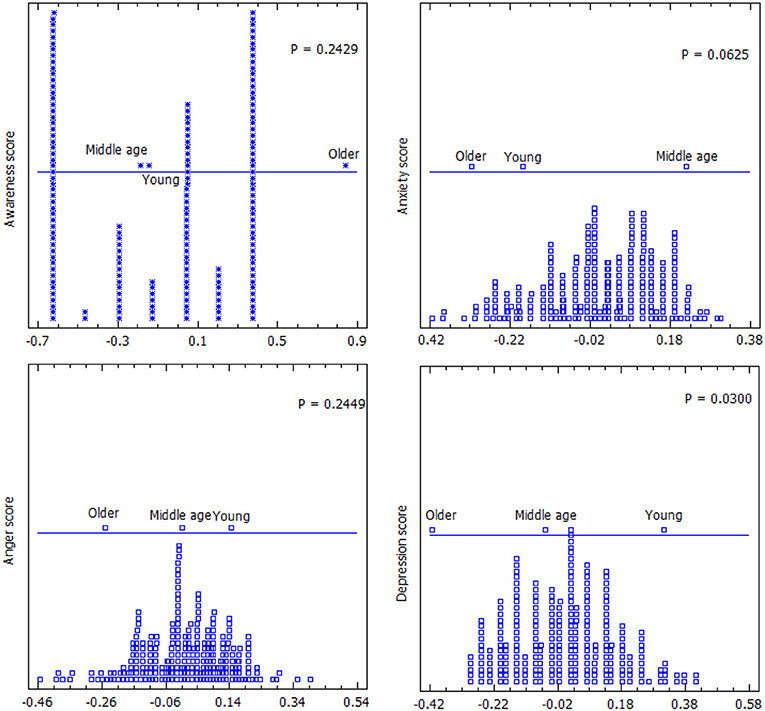
Figure 3. Composite score difference for awareness, anxiety, anger, and depression between the different age groups.
The correlation analysis of the study variables was presented in Table 2. There was a negative relationship between age and depression (r = −0.154, P = 0.014), while a positive relationship was observed between anxiety and anger (r = 0.254, P < 0.001), anxiety and depression (r = 0.153, P = 0.015) and anger and depression (r = 0.153, P = 0.015).
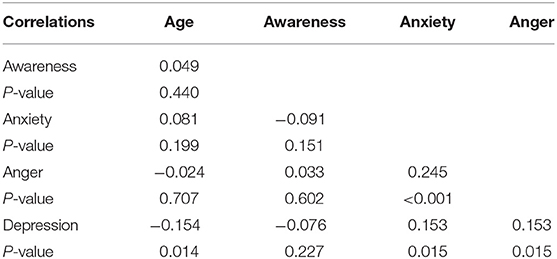
Table 2. Spearman Rho correlation of age, awareness, anxiety, and anger on COVID-19 amongst low-income Ugandans.
The study also showed that there were relationships in participants anger score however all other variables were not related in both sexes (Figure 4).
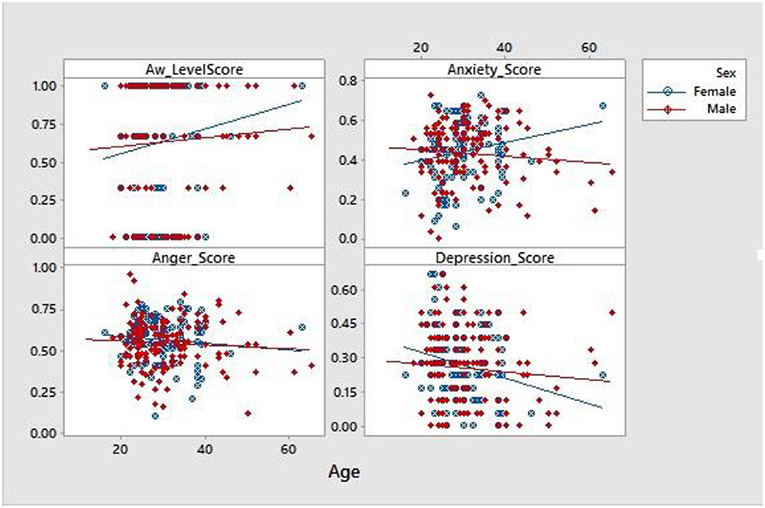
Figure 4. Scatter plot of Sex influence on age associated changes in awareness, anxiety, anger, and depression.
Survivors of natural disasters as exemplified by the current COVID-19 pandemic often suffer from traumatic experiences, anxiety disorders (GAD), depression, panic disorders and substance abuse (20–22). The study provided evidence that generally the Ugandan population was aware of mental health issues and this was in agreement with previous studies amongst healthcare workers (23) and market workers (24).
Females who demonstrated severe anxiety, moderate anger and depression probably due to their relatively low knowledge as compared to males on COVID-19. Social-economic barriers in several developing countries have continued to predispose women to apathy, segregation and mistreatment at the hands of their men counterparts in several rural communities in Africa, thus accounting for the severe discrepancies in knowledge between the two sexes. The WHO has identified women as vulnerable persons in Africa who should be supported in response programs against COVID-19 (25) and this is re-emphasized by the current study. Findings in the study were elderly persons showed a keen awareness and interest on mental healthcare demonstrated their keen interest to improve on their lifestyle, contrary to young adults in this population.
Anxiety also increased with age amongst females due to the inherent responsibilities associated with women in African communities. A majority of homes in Africa are managed by single mothers, and elderly women taking care of orphaned grandchildren, thus social pressures associated with COVID-19 were amplified in this population group than in their male counterparts who generally live more reckless lifestyles (i.e., alcoholism, polygamy, and crime, vices not common with African women).
Anger and depression decreased with an increase in age in the study population. These findings though perplexing, help to demonstrate the fluidity associated with community health response projects, and the need for flexibility while dealing with different age populations. Generally, Africa has a young vibrant population and these findings may not be applicable in the global context. Females were found to be more depressed probably due to the associated pressures of lost time due to the total lockdown which led to a closure of all academic centers of learning, forcing many young girls into early marriage and teenage pregnancies, thus derailing their academic goals (25). In addition, the study identifies Ugandan females as vulnerable persons to depression and in great need of guidance and counseling services for the promotion of better public health policies (26, 48). Generally, females experience more stress than males on a monthly basis as a result of physiological processes associated with their gender, thus offering a foundation for the increased anxiety attacks common in the gender (27, 28). Furthermore, neurophysiology studies have revealed that there are structural and functional differences in the brain relevant to anxiety in males and females (29–31) and blood pressure and pulse have been reported to be more reactive to anxiety in females compared to males (32), although these were not investigated in the current study.
A strong relationship between anxiety and anger was found amongst the young study participants probably due to frustrations associated with the lockdown and the fact that a majority of the youth in Uganda are under/unemployed. Our findings are in agreement with Walsh et al. (47) who reported a similar relationship between anxiety and anger in younger people. Poverty amongst the young and the on-going presidential elections were COVID-19 guidelines are enforced by the police against the opposition parties could have played a role in saturating a hateful atmosphere (personal communication). Amongst the youth, anger is a psychological and physical health predictor (33), demonstrating a need for policymakers to work closely with this age group.
Anger refers to a basic and universal emotional state brought forth by a perception of threat and it is associated with cognitions centered on others' transgressions (34). In contrast, irritability is a physiological state which is characterized by a lowered threshold for responding with negative affect to stimuli, often with anger and aggression (35, 44). Anger has not been included as a feature or symptom associated with anxiety disorders during the diagnostic process, however, irritability has been included as part of generalized anxiety disorders (GAD) diagnosis. Evidence has emerged in samples of adults with anxiety disorders that the rate and intensity of anger are elevated when compared to healthy individuals and this is common during severe anxiety (36). Anger may be expressed differently depending on anxiety diagnosis. For instance, it was observed that individuals with GAD may experience angry feelings but suppress them more than healthy controls, leading to higher levels of anxiety severity in adulthood (37, 46). This simply means that younger people express anger more than adults because they cannot suppress it, while adults tend to suppress anger and this increases anxiety. In addition, the initial increase in anger-score may be due to the inability or difficulty for younger persons to rate anger and anxiety as distinct constructs. This supports the study done by Walsh et al. (47) which reported that younger people confused physical symptoms of anxiety which mimic some physical symptoms of anger for anger and this led to difficulty in rating anger and anxiety as separate constructs.
A positive relationship was found between anxiety and depression in the study showing that younger persons (20 years of age) experienced depression as anxiety score increased more than adults (40–60 years of age) in the study. This supports the statistics from the Substance Abuse and Mental Health Services Administration (SAMHSA) of 2017 which estimated depressive disorder to be 7.1% for adults and 13.3% for adolescents/teens (45). Anxiety disorders and major depression occur during development with anxiety disorders beginning during pre-adolescence and early adolescence, while major depression tends to emerge during adolescence and early to mid-adulthood (38–40). Further studies have shown that anxiety disorders generally precede the presentation of major depressive disorder (39). Previous studies done in the USA revealed that depression is on the rise amongst teenagers and that females were three times more likely to experience depression compared to males. A 10-year study between 2007 and 2017 in the US revealed that the number of teenagers who experienced depression had increased by 59% and the rate was faster for females (66%) than males (44%) (41); the number of adults who experienced depression increased by 7% within the same period. Academic and social pressures were cited by experts as the reasons behind the increase in depression among the teens recruited in that study. About six out of 10 (61%) of the teens reported they felt a lot of pressure to get good grades while 29% of the teens reported they felt a lot of pressure to look good and 28% of the teens reported they felt pressured to fit socially (41). The results from our study showed that people at 20 years of age (this age bracket captures teens), had a depression score which increased as anxiety score increased. In Bushenyi district (Uganda), some of the students within the 20 years of age group do engage in low-income jobs after school hours and this may affect their academic performances or social life resulting in depression if not monitored and this observation is in agreement with postulations by Geiger and Leslie (41).
There was a positive relationship between anger score and depression score in our study. It was observed that as anger score increased depression score tends to increase. Anger is one of the ways that depression manifests and there is an association between the level of anger that people experience and the severity of depression (50). According to the Anxiety and Depression Association of America (ADAA), depression is expressed in different ways by different people. Females with depression tend to feel sad or guilty while males with depression are more likely to feel irritable and angry (ADAA). However, there is limited research available to support or show that anger can cause depression.
A general observation from our study showed that awareness of mental health care was high (49.8%) across the sample population (n = 253) and an increase in age-related to high awareness. 24.5% of the respondents had low awareness and 25.7% had no awareness of mental health care. 68.8% of the respondents experienced severe anxiety due to the COVID-19 lockdown and 29.2% experienced moderate anxiety while 2.0% experience no/mild anxiety based on anxiety score scale using a modified GAD-7 item tool. Also, 33.9% of the respondents experienced severe anger due to the COVID-19 lockdown, and 56.9% experienced moderate anger while 9.5% experienced no/mild anger based on the anger-score grading scale using a modified STAXI-2 item tool. About 4.7% of the respondents experienced severe depression due to the COVID-19 lockdown and 60.5% experienced moderate depression while 34.8% experienced no depression based on the depression score grading scale using a modified BDI. Other studies done elsewhere have reported different figures due to the variations in the study population and sample size. Wang et al. (42), in their study of mental health status related to COVID-19 among the general population (n = 1,210) in China reported that 16.5% experienced moderate to severe depression symptoms, 28.8% experienced moderate to severe anxiety symptoms and 8.1% experienced moderate to severe stress. The variation in statistics from our study in Uganda and Wang et al. (42) in China maybe because we targeted low-income earners which are persons who depend on day-to-day-business to make ends meet, tools used for assessment, and sample size. However, our study indicates that anxiety was the most common mental health challenge and this supports the study by Wang et al. (42), which also identified anxiety as the most common mental health challenge in their study. Other studies have reported increased traumatization related to COVID-19 among the public and non-front-line nurses in China (43). Xiao et al. (11), targeted individuals (n = 170) observing COVID-19 self-isolation for 14 days in China, and they reported that anxiety positively correlated with stress and negatively with sleep quality and social capital and social capital positively correlated with sleep quality. This indicates that COVID-19 lockdown, without doubt, affects the mental health status of individuals.
The study showed that pandemic mental health is a realistic public health concern which needs to be addressed. Poor and low knowledge on the pandemic precipitates anxiety which leads to a depressed population. In particular, females and the elderly were identified as vulnerable persons who should be prioritized in any community extension activities. The authors could not include the COVID-19 status of the respondents due to absence of clinical data at the time of the study (early COVID-19 period and no community testing was in place). We also did not have access to population data to access clinical mental status of study participants prior to the pandemic. Further studies to generate information on the impact of the pandemic in the general population could help guide policymakers draft community-practical policies which address mental health amongst the vulnerable communities of Uganda.
Data files can be accessed at https://figshare.com/s/88a0cf974d67f2654816.
The studies involving human participants were reviewed and approved by Kampala International Ethical Review Board Kampala International University, Uganda. The patients/participants provided their written informed consent to participate in this study.
VA and IU conceptualized the study. IU, KK, FS, and SW designed the study. VA, IU, RS, AM, ETA, VN, JTA, and FS collected the data. VA, IU, and EOA conducted statistical analysis. VA, IU, KK, EOA, IJ, SH, EM, HN, and SW conducted data interpretation. VA, IU, and KK drafted the initial manuscript while EOA, IJ, AM, RS, GC, ST, OO, NM, AA, JOA, AMA, SO, FS, ETA, JTA, VN, HY, CO, SH, EM, HN, and SW reviewed it for intellectual content. All authors approved the final version for publication and remain in agreement to ensure that questions related to the integrity of any part of the work are resolved.
This work was supported by Zhejiang University Education Foundation Emergency Research Fund (SW and KK); Global Challenges Research Fund and the University of Edinburgh.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Authors are grateful to colleagues who offered positive criticism and are not on the paper.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.590458/full#supplementary-material
Supplementary Material 1. The questionnaire.
1. World Health Organization. World Health Organization Report on 7 April, 2020. Covid19 Cases Top 10,000 in Africa. WHO/2020 Report in Brazzaville/Cairo. (2020). Available online at: https://www.afro.whoint.news (accessed April 12, 2020).
2. Obulutsa G. Angola, Eritrea, Uganda Confirm First Cases as Coronavirus Spreads in Africa. (2020). Available online at: https://www.reuters.com/article/us-health-coronavirus-africa-idUSKBN2180P4 (accessed March 22, 2020).
3. Ministry of Health-Uganda. Uganda Confirms 1st Case of COVID-19. Ministry of Health Uganda. (2020). Available online at: https://www.health.go.ug/covid/2020/03/23/uganda-confirms-1st-case-of-covid-19-saturday-21-march-2020/ (accessed March 22, 2020).
4. Javira S. Full Speech: Uganda Bans Travellers From COVID-19Hit Countrises. PML Daily. (2020). Available online at: https://www.pmldaily.com/features/tours-travel/2020/03/full-speech-uganda-bans-travellers-from-Covid-19-hit-countries.html (accessed May 10, 2020).
5. Lee J. Mental Health Effects of School Closures During COVID-19. (2020). Available online at: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642%2820%2930109-7/fulltext (accessed April 20, 2020).
6. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 22:e37–8. doi: 10.1016/S0140-6736(20)30309-3
7. Dong L, Bouey J. Public mental health crisis during COVID-19pandemic, China. Emerg Infect Dis. (2020) 23. doi: 10.3201/eid2607.202407
8. Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. (2020) 51:101990. doi: 10.1016/j.ajp.2020.101990
9. Asmundson GJG, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J Anxiety Disord. (2020) 71:102211. doi: 10.1016/j.janxdis.2020.102211
10. Asmundson GJG, Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J Anxiety Disord. (2020) 70. doi: 10.1016/j.janxdis.2020.102196
11. Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. (2020) 26:e923921. doi: 10.12659/MSM.923921
12. Mitsuishi F, Ries J. COVID-19 Can Have Serious Effects on People with Mental Health Disorders. (2020). Available online at: https://www.healthline.com/health-news/Covid-19-serious-effects-people-with-mental-health-disorders (accessed April 20, 2020).
13. International Federation of Red Cross and Red Crescent Societies. Mental Health and Psychosocial Support for Staff Volunteers and Communities in an Outbreak of Novel Coronavirus. Hong Kong: IFRC (2020).
14. Inter-Agency Standing Committee,. Interim Briefing Note Addressing Mental Health Psychosocial Aspects of COVID-19 Outbreak. IASC. (2020). Available online at: https://interagencystandingcommittee.org/system/files/2021-03/IASC%20Interim%20Briefing%20Note%20on%20COVID-19%20Outbreak%20Readiness%20and%20Response%20Operations%20-%20MHPSS.pdf (accessed March 20, 2020).
15. Sykes J, Križ K, Edin K, Halpern-Meekin S. Dignity and dreams: what the earned income tax credit (EITC) means to low-income families. Am Sociol Rev. (2015) 80:243–67. doi: 10.1177/0003122414551552
16. Chowa G, Masa R, Ansong D. Determinants of saving among low-income individuals in rural uganda: evidence from assets Africa. Adv Appl Sociol. (2012) 2:280–91. doi: 10.4236/aasoci.2012.24037
17. Bystritsky A, Kerwin L, Feusner JD. A pilot study of Rhodiola rosea (Rhodax®) for generalized anxiety disorder (GAD). J Alternat Complement Med. (2008) 14:175–80. doi: 10.1089/acm.2007.7117
18. Trotter SE. Review of the state-trait anger expression inventory. In: BS Plake, JC Impara, editors, The Fourteenth Mental Measurements Yearbook. Lincoln, NE: Buros Institute of Mental Measurements (2001). p. 1183–4.
19. Steer RA, Rissmiller DJ, Beck AT. Use of the beck depression inventory with depressed geriatric patients. Behav Res Ther. (2000) 38:311–8. doi: 10.1016/S0005-7967(99)00068-6
20. Mason V, Andrews H, Upton D. The psychological impact of exposure to floods. Psychol Health Med. (2010) 15:61–73. doi: 10.1080/13548500903483478
21. Aciemo R, Ruggieri KJ, Galea S, Resnick HS, Koenen K, Roitzsch J, et al. Psychological sequalae resulting from the 2004 Florida Hurricanes: implications for post disaster intervention. Am J Public Health. (2007) 97:S103–8. doi: 10.2105/AJPH.2006.087007
22. Norris FH. Range magnitude and duration of the effects of disasters on mental health: review update. Res Educ Disaster Ment Health. (2005) 1–23. Available online at: https://medipe2.psu.ac.th/~disaster/disasterlast/FranNorris_Tsunami.pdf
23. Olum R, Chekwech G, Wekha G, Nassozi DR, Bongomin F. Coronavirus disease-2019: knowledge, attitude, and practices of health care workers at makerere university teaching hospitals, Uganda. Front Public Health. (2020) 8:181. doi: 10.3389/fpubh.2020.00181
24. Usman IM, Ssempijja F, Ssebuufu R, Lemuel AM, Archibong VB, Ayikobua ET, et al. Community drivers affecting adherence to WHO guidelines against COVID-19 amongst rural Ugandan Market Vendors. Front Public Health. (2020) 2020:340. doi: 10.3389/fpubh.2020.00340
25. Kasozi KI, MacLeod E, Ssempijja F, Mahero MW, Matama K, Musoke GH, et al. Misconceptions on COVID-19 risk among ugandan men: results from a rapid exploratory survey, April 2020. Front Public Health. (2020) 8:416. doi: 10.3389/fpubh.2020.00416
26. Beane ML, Cole MA, Spencer RL, Rudy JW. Neonatal handling enhances contextual fear conditioning and alter corticosterone stress responses in young rats. HormBehav. (2002) 41:33–40. doi: 10.1006/hbeh.2001.1725
27. Premier Health. Your Gender May Be Causing Your Worries. (2017). Available online at: https://www.premierhealth.com/your-health/articles/women-wisdom-wellness-/your-gender-may-be-causing-your-worries (accessed July 7, 2020).
28. McHenry J, Carrier N, Hull E, Kabbaj M. Gender differences in anxiety and depression: role of testosterone. Front Neuroendocrinol. (2014) 35:42–57. doi: 10.1016/j.yfrne.2013.09.001
29. Lebron-Milad K, Milad MR. Sex differences, gonadal hormones and the fear extinction network: implications for anxiety disorders. Biol Mood Anxiety Disord. (2012) 2012:2. doi: 10.1186/2045-5380-2-3
30. Segalas C, Alonso P, Labad J, Real E, Pertusa A, Jaurrieta N, et al. A case-control study of sex differences in strategic processing and episodic memory in obsessive-compulsive disorders. Comprehens Psychiatry. (2010) 51:303–11. doi: 10.1016/j.comppsych.2009.05.008
31. Lochner C, Hemmings SMJ, Kinnear CJ, Moolman-Smook JC, Corfield VA, Knowles JA, et al. Gender in obsessive-compulsive disorder clinical and genetic findings. Eur Neuropsychopharmacol. (2004) 14:105–13. doi: 10.1016/S0924-977X(03)00063-4
32. Altemus M. Sex differences in depression and anxiety disorders: potential biological determinants. Hormon Behav. (2006) 50:534–8. doi: 10.1016/j.yhbeh.2006.06.031
33. Kerr MA, Schneider BH. Anger expression in children and adolescents: a review of the empirical literature. Clin Psychol Rev. (2008) 28:559–77. doi: 10.1016/j.cpr.2007.08.001
34. Deater-Deckard K, Wang Z. Anger and irritability. In: M Zentner, RL Shiner, editors, Handbook of Temperament. New York, NY: Guilford Press (2012). p. 124–44. doi: 10.1093/obo/9780199828340-0016
35. Stoddard J, Stringaris A, Brotman MA, Montville D, Pine DS, Leibenluft E. Irritability in child and adolescent anxiety disorders. Depress Anxiety. (2014) 31:566–73. doi: 10.1002/da.22151
36. Hawkins KA, Cougle JR. Anger problems across the anxiety disorders: findings from a population-based study. Depress Anxiety. (2011) 28:145–52. doi: 10.1002/da.20764
37. Fracalanza K, Koerner N, Deschênes SS, Dugas MJ. Intolerance of uncertainty mediates the relation between generalized anxiety disorder symptoms and anger. Cogn Behav Ther. (2014) 43:122–32. doi: 10.1080/16506073.2014.888754
38. Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. (2009) 32:483–524. doi: 10.1016/j.psc.2009.06.002
39. Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. (2008) 29:115–29. doi: 10.1146/annurev.publhealth.29.020907.090847
40. Ohayon MM, Schatzberg AF. Social phobia and depression: prevalence and comorbidity. J Psychosom Res. (2010) 68:235–43. doi: 10.1016/j.jpsychores.2009.07.018
41. Geiger AW, Leslie D. A Growing Number of American Teenagers – Particularly Girls – Are Facing Depression. (2019). Available online at: https://www.pewresearch.org/fact-tank/2019/07/12/a-growing-number-of-american-teenagers-particularly-girls-are-facing-depression/ (accessed July 8, 2020).
42. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:E1729. doi: 10.3390/ijerph17051729
43. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
44. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
45. Substance Abuse Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, SAMHSA (2018). Available online at: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm
46. Deschênes SS, Dugas MJ, Fracalanza K, Koerner N. The role of anger in generalized anxiety disorder. Cogn Behav Ther. (2012) 41:261–71. doi: 10.1080/16506073.2012.666564
47. Walsh LM, Wolk CB, Becker Haimes EM, Jensen-Doss A, Beidas RS. The relationship between anger and anxiety symptoms in youth with anxiety disorder. J Child AdolescCouns. (2018) 4:117–33. doi: 10.1080/23727810.2017.1381930
48. Papaioannou A, Gerozissis K, Prokopiou A, Solaris S, Stylianopoulou F. Sex differences in the effects of neonatal handling on the animal's response to stress and the vulnerability for depressive behaviour. Behav Brain Res. (2002) 129:131–9. doi: 10.1016/S0166-4328(01)00334-5
49. Simon-Morton B, Chen R, Abram SK, Haynie DC. Latent growth curve analysis of peers and parents influence on smoking progression among early adolescent healthy. Psychology. (2014) 23:612–21. doi: 10.1037/0278-6133.23.6.612
50. Timothy J, Rachell N. What Is the Link Between Depression Anger? (2020). Available online at: https://www.medicalnewstoday.com/articles/327408 (accessed July 7, 2020).
Keywords: COVID-19 response in Africa, socio-economic impacts of COVID-19, COVID-19 outcomes, psychosocial impacts of COVID-19, hunger and COVID-19, COVID-19 hits poor harder, women dangers in COVID-19
Citation: Archibong V, Usman IM, Kasozi KI, Aigbogun EO Jr, Josiah I, Monima AL, Ssebuufu R, Chekwech G, Terkimbi SD, Owoisinke O, Mbiydzenyuy NE, Adeoye A, Aruwa JO, Afodun AM, Odoma S, Ssempijja F, Ayikobua ET, Ayuba JT, Nankya V, Onongha C, Henry S, Matama K, Yusuf H, Nalugo H, MacLeod E and Welburn SC (2021) Anxiety, Anger and Depression Amongst Low-Income Earners in Southwestern Uganda During the COVID-19 Total Lockdown. Front. Public Health 9:590458. doi: 10.3389/fpubh.2021.590458
Received: 01 August 2020; Accepted: 14 October 2021;
Published: 09 December 2021.
Edited by:
Joanna Lai, UNICEF United Nations International Children's Emergency Fund, United StatesReviewed by:
Herbert Ainamani, Kabale University, UgandaCopyright © 2021 Archibong, Usman, Kasozi, Aigbogun, Josiah, Monima, Ssebuufu, Chekwech, Terkimbi, Owoisinke, Mbiydzenyuy, Adeoye, Aruwa, Afodun, Odoma, Ssempijja, Ayikobua, Ayuba, Nankya, Onongha, Henry, Matama, Yusuf, Nalugo, MacLeod and Welburn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Victor Archibong, dmljdG9yYXJjaGlib25nM0BnbWFpbC5jb20=; Ibe Michael Usman, Z29wYW1hMTNAZ21haWwuY29t; Keneth Iceland Kasozi, a2ljZWxhbmR5QGdtYWlsLmNvbQ==; Susan Christina Welburn, c3VlLndlbGJ1cm5AZWQuYWMudWs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.