- 1Youth Health Care Division, Regional Public Health Service South Limburg, Heerlen, Netherlands
- 2Department of Social Medicine, Care and Public Health Research Institute, School for Public Health and Primary Care, Maastricht University, Maastricht, Netherlands
- 3King's Health Partners, Department of Psychosis Studies, Institute of Psychiatry, King's College London, London, United Kingdom
- 4Department of Psychiatry and Psychology, MHeNS School for Mental Health and NeuroScience, Maastricht University Medical Centre, Maastricht, Netherlands
- 5Department Psychiatry, Brain Center Rudolf Magnus, Utrecht University Medical Centre, Utrecht, Netherlands
Background: Adverse communication development in preschool children is a risk factor influencing child health and well-being with a negative impact on social participation. Language and social skills develop and maintain human adaptability over the life course. However, the accuracy of detecting language problems in asymptomatic children in primary care needs to be improved. Therefore, it is important to identify concerns about language development as a risk factor for child health. The association between parental and professional caregivers' concerns about language development and the level of preschool social participation was assessed, as well as the possible mediating/moderating effect of the perception of social competence. In addition, validity and predictive value of parental and professional caregivers' concerns about language development were tested.
Methods: To identify emerging concerns about development and social participation, a community sample of 341 preschool children was systematically assessed with a comprehensive preventive child health care “toolkit” of instruments, including parent-completed tools like the Parents' Evaluation of Developmental Status (PEDS) and child competence Visual Analog Scales (VAS). At baseline, children were aged 3 years and at follow-up ~4 years.
Results: There was a statistically significant association between parental and professional caregivers' concerns about language development and the level of preschool social participation, with a mediating effect of child social competence at the age of 3 years as well as 4 years. Negative predictive value of parental and professional caregiver language concerns at the age of 3 and 4 years were 99 and 97%, respectively. Furthermore, this article showed that while some preschool children grow out of language problems, others may develop them.
Conclusion: Short but valid pediatric primary care tools like the PEDS and child competence VAS can support monitoring and early identification of concerns about language development and social competence as a risk factor for preschool social participation. Personalized health care requires continued communication between parents, professional caregivers and preventive child health care about parental and professional caregiver perceptions concerning preschool language development as well as the perception of a child's social competence.
Introduction
Poor communication is a risk factor influencing child health and well-being with adverse consequences for behavior, literacy, learning, mental health, future employment, parenting, the next generation, and social inequalities (1, 2).
Effective communication is fundamental to the initiation and maintenance of successful peer relations (3, 4). The ability to interact with others and to establish relationships is of great influence on learning and development, and successful social adaptation and participation. From a dynamic perspective, health can be seen as the ability to adapt and self-manage in the face of social, physical, and emotional challenges (5). For this, language and social skills are needed; they develop and maintain human adaptability over the life course (6, 7).
From a public health perspective, preschool children represent an important group (8, 9). The preschool period is a sensitive period in language development (7, 10). Developmental growth in language skills is an important parameter of overall communication development (11). Language problems are often the first presenting symptoms of delay in the development of multiple basic functions including socialization and communication (3, 12). Early expressive and receptive language problems and behavioral problems may have long-term consequences (13). In particular, early receptive language problems are a significant risk factor for adult mental health (1).
However, the accuracy of detecting language problems in asymptomatic children in primary care is inadequate (14). Early recognition of adverse language development is challenging, given that normal development in young children is highly variable and all growth and development takes place in interaction with the environment (15–17). Differentiating between speech language delays and disorders is complicated, children with concerns about language development are a heterogeneous group with different individual and environmental characteristics. On the other hand, many children whose language development is delayed may catch up over the next few years and do not require interventions (18). Prevalence of language problems varies widely (2–25%) due to a lack of consistent definitions, the nature of the population, the diagnostic method that is utilized, and whether data were collected in a clinical sample or in the general population (19–21).
From a personalized health care “growing into deficit” model (Figure 1), prevention of language developmental problems requires a focus on concerns, emerging problems and symptoms at an early stage where signs and symptoms do not yet meet diagnostic criteria for a disorder (13, 22, 23). For early identification of language needs, it is important to understand the pervasive nature of language development (8, 13, 19). It is assumed that differences in young children's language development reflect differences in experience and in creating interactive routines, next to their biologically mediated genetic potential (24). If needed, early intervention has to be personalized; standard intervention programs have limited added value (25).
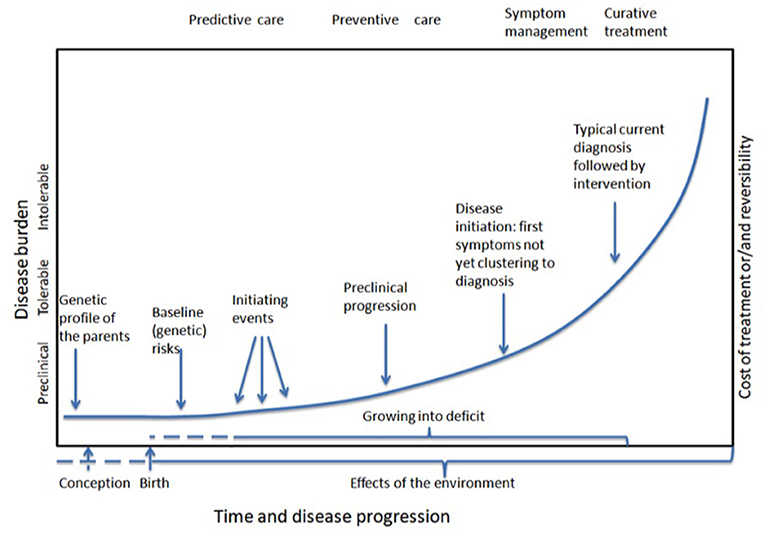
Figure 1. Modification of Syurina's adaptation of Snyderman's curve representing the timelines of “growing into deficit” and developing common complex diseases.
Previous research has shown that there is an association between language difficulties, behavioral difficulties, and social participation (26, 27). Language impairment in childhood may be related to problems with activities and social participation as defined by the International Classification of Functioning Disability and Health—Children and Youth (ICF-CY) (19, 28). Social participation is a broad concept including the objective state and the subjective experience of involvement in society. This concept has to be understood in the light of social roles (6). For young children, play is an important social activity.
Social competence development is linked with both language development and social participation. Social competence is affected when abilities or skills that are required to engage in socio-cognitive processes and to display social behaviors are limited (7). For example, not only expressive and receptive language, but also the ability to grasp non-linguistic signals is important for optimal social interaction and participation. Toddler's play has been associated with their language proficiency (4). However, this same study also showed that the child's functioning in play was better explained by their social competence than by their language skills. From a dynamic transactional developmental perspective (29), it is hypothesized that language development is mediated by social competence and social participation, and vice versa. Language development, social competence, and social participation are seen as dynamic skills simultaneously developing during the preschool period, suggesting a reciprocal model (30).
A community-based approach with a focus on personalized health care requires cooperation and communication within a public health framework (8, 22). According to a bio ecological model of development-in-context, it is important to obtain child context-specific information (20). Teachers, employees from childcare, kindergarten, preschool or primary school (hereafter: professional caregivers) as well as parents and Preventive Child Health Care (PCHC) professionals are important perceivers with expert knowledge on child development from different perspectives.
PCHC is synonymous with Pediatric Preventive Primary Care. All children in the area are regularly invited to visit the PCHC. The Dutch PCHC system includes preventive health care doctors and has a high level of population compliance. It is a public health endeavor to provide ongoing monitoring up to the age of 18 years (31, 32). This way, the early conditions that place children at risk for less than optimal development and successful social participation can be improved (33–36). To deal with emerging problems and symptoms at an early stage where signs and symptoms do not yet meet diagnostic criteria for a disorder, systematically exploring parental as well as other caregivers' concerns is a main component in PCHC for family-centered practice and personalized health care. Knowledge and understanding of the true epidemiology of genetic and environmental risk and protective factors and their early phenotypes can help in prevention of “growing into deficit” (23, 37).
In order to document children's development over time, monitoring development at multiple time points, across informants, instruments and contexts, is more valid and accurate than a single assessment (16, 38–41). For early identification of developmental problems, special attention should be given to the validity of instruments about the perceived impact of concerns as concurrent and long-term predictors, and outcome domains such as health, well-being and social participation (42). In a PCHC setting, monitoring instruments should: (1) easily obtain information in every day PCHC setting; (2) carry out dimensional assessment of symptoms and behavior; (3) measure the progress of development of young children and their possible determinants of influence; (4) identify general signals and symptoms indicating a possible disruption or imbalance of the educational/parent-child system, not yet related to a specific diagnosis; (5) support communication between PCHC, parents and professional caregivers about their perceptions on health and development; (6) connect to needs and demands of the child and the social system around the child; and (7) promote shared decision making (43, 44). Short instruments with a high negative predictive value are preferred; it ensures that most children who pass the developmental assessment are truly healthy. Follow-up consultations are no problem, these children can benefit from additional preventive monitoring (45).
Research has shown that parent-completed tools are highly accurate in detecting true problems, are relatively inexpensive, and promote a dialogue about concerns, needs and demands between parents and other caregivers (46–48). Therefore, incorporating tools utilizing a parent—and professional caregivers—report assessment like the Parents' Evaluation of Developmental Status (PEDS), child competence Visual Analog Scales (VAS) and the Strengths and Difficulties Questionnaire (SDQ) into a routine child monitoring toolkit could improve the rate of early identification of concerns about language development, social competence and social participation (43, 49). In this article, the concept social participation was operationalized using instruments to assess early emerging concerns about factors underlying preschool competence and social participation: a child's general competence at day care, kindergarten and preschool, the impact of distress and the total amount of concerns about child development and behavior.
This article investigates (1) the validity of the Parents' Evaluation of Developmental Status (PEDS) to assess language development concerns; (2) the cross-sectional association of language development concerns with social participation; (3) the longitudinal association of language development concerns with social participation, and (4) the possible mediating effect of social competence on the association between language development and social participation at the ages of 3 and 4 years.
Methods
The present study was performed as part of the Monitoring Outcome Measurements of child development (MOM) study, a prospective observational study within PCHC practice. A community-based sample of 346 children was systematically assessed with a comprehensive PCHC “toolkit” of instruments using a multisource and cross-informant repeated measures design to identify developmental pathways impacting school readiness as an outcome of social participation. Children were aged 3 years at baseline and 4 years at follow up.
The Maastricht University Medical Center Medical Ethics Committee approved the MOM-study protocol under registration number MEC 09-04-018/P. Therefore, this study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participating parents gave their informed consent prior to their inclusion in the study.
Data Collection and Instruments
For this article, data of parents, professional caregivers and PCHC professionals of 341 children were analyzed. At baseline, children were aged 3 years and at follow-up ~4 years. To assess emerging problems, signs and symptoms, perceptions, demands and concerns about development and social participation, various short instruments like the Parents' Evaluation of Developmental Status (PEDS), the Strengths and Difficulties Questionnaire (SDQ) and child competence Visual Analog Scales (VAS) were included in this study. PCHC professionals provided information about, for example, background factors, family history, child health, and development and interventions.
Language Concerns
Parents as well as professional caregivers completed the PEDS, a 10-item standardized semi-structured questionnaire to elicit concerns regarding child development for children aged <8 years in the general population and clinical samples (40). Ten questions explore concerns in various domains: expressive and receptive language, fine motor, gross motor, behavior, socialization, self-care and learning. The PEDS-question could be answered on a trichotomous scale: “no,” “a little,” “yes.” Subsequently, an open-ended field provides more information. The PEDS is validated for clinical samples and general population samples aged between 0 and 8 years, and is available in multiple languages. In recent validation studies from the USA for the accuracy of parental concerns in detecting children at high and/or moderate developmental risk, the PEDS has a sensitivity of 91–97% and specificity of 73–86% (50). The PEDS is less time-consuming than other instruments, emphasis is on parental and other professional caregivers' opinions, and has reasonable test characteristics for developmental screening in primary care settings (51). Furthermore, the PEDS has shown to be reliable, valid and useful as brief monitoring tools in daily Dutch PCHC practice (43, 51). This suggests that the PEDS is an accurate tool for use as an initial screening and monitoring tool in Dutch PCHC, where professionals have to deal with the time constraints of daily practice.
For the current paper, dichotomous “parental concerns” and “professional caregiver concerns” variables about expressive and/or receptive language (any concern yes/no) were constructed for use in the analyses, if any of the parents or professional caregivers scored “yes” or “a little,” the answer was recoded as “yes.”
Child Competence
To address the issue of the child's functional adaptation, professional caregivers were asked to indicate on 2 VAS, the degree of the child's general competence and the child's social competence (0 = not competent, 100 = very competent).
Participation
The child's general competence as described above is one of the instruments to assess the broad construct of participation. Other instruments are SDQ total score and SDQ impact.
The Dutch version of the SDQ was completed by parents as well as by professional caregivers to assess the child's behavior (46, 52–54). The SDQ is a brief behavioral screening questionnaire for children aged 3–16 years. It also includes items that identify the impact of the behavioral problems of the child. The SDQ is considered valid and reliable as a research instrument in community samples (49). For this article, the “SDQ total sum score” and the “SDQ impact of distress score” of both parents and professional caregivers were used. If any of the parents or professional caregivers scored “yes” on the impact probe question, the dichotomous overall distress variable was set at “yes.”
Van Wiechen Developmental Test
In addition to the validation of the overall PEDS, validity of the PEDS language items was assessed, using the Van Wiechen developmental test as reference standard (43, 55–57). This Dutch instrument is a modification of the Gesell test and is routinely used by all PCHC Centers in the Netherlands and Belgium to monitor the development of all children from birth to the age of 4 years. It consists of a set of 57 developmental indicators to assess motor behavior, speech, communication, and social skills based on physicians' observations and interviewing the parents. A total of 23 indicators cover language development and communication and are called language milestones. All PCHC professionals are trained to asses and register mile stones in the PCHC system according to a uniform protocol. For this paper, the Van Wiechen communication and language items were used. In a large community-based sample of Dutch children, test characteristics of the Van Wiechen language items for the age group 36–48 months showed an Area Under the Curve (AUC) of 0.83%, with an average sensitivity of 66.1%, specificity of 87.5%, positive predictive value (PPV) of 29.2%, and a negative predictive value (NPV) of 98.8% (58).
In a study in Australia, agreement between ratings of parental PEDS language concerns and clinical assessment was high (86–90%); agreement between teacher PEDS language concerns and clinical assessment was lower and more varied (63–80%) (59). In this study, parental and professional caregiver PEDS language concerns were combined to provide complementary information and capture all possible language concerns of a specific child. Subsequently this combined concerns variable was validated; reference standard was the Van Wiechen developmental test, communication and language items (see above) (60, 61). For this study, the PCHC professionals were asked to judge the Van Wiechen language and communication items as “sufficient” or “not sufficient,” at the age of 3 years and a year later.
Other Variables
As an indicator of socioeconomic status, the level of maternal and paternal education was assessed across three categories: low (primary education, junior vocational education), middle (general secondary education, senior vocational education) and high (preparatory university education and university education). The parent with the highest level of education determined parental educational level.
Statistical Analyses
All analyses were performed using Stata Statistical Software, version 15 (62). First, to assess the validity of the PEDS language items, positive predictive value (PPV) and negative predictive value (NPV) were obtained at the age of 3 years and at the age of 4 years. PPV and NPV were then assessed as measures of predictive validity of language concerns at the age of 3 years, using the Van Wiechen developmental test at age 4 years as reference standard. Second, logistic and linear regression analyses were performed. In the cross-sectional analyses at both ages 3 and 4 years and in the longitudinal analyses, the independent variable (X) was concerns about language development. The dichotomous dependent variable (Y) to index social participation, used in the logistic regression analyses, was SDQ impact of distress score. Continuous dependent variables (Y) to index social participation, used in the linear regression analyses, were: SDQ total score, the child's general competence VAS and the child's social competence VAS. Analyses were adjusted a priori for age, sex, and parental educational status.
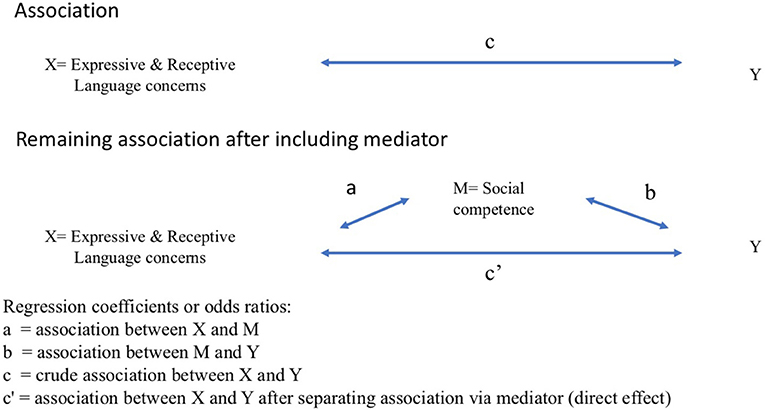
Finally, to analyze the fourth research question, the child's social competence was included as a mediator (M) in the association between independent (X) and dependent (Y) variable. Mediation was assessed by analyzing a regression model with and without the mediator. The question was whether the association between X and Y after including the mediator is zero or substantially smaller than the direct association between X and Y. This is visualized in Figure 2. The arrows a, b, c and c' present regression coefficients or odds ratios: a represents the association between independent variable (X) and mediator (M); b represents the association between the mediator (M) and the dependent variable (Y); c represents the crude association between independent variable (X) and dependent variable (Y); and c' represents the association between X and Y after including the mediator (M) in the regression model. When the hypothesis that there can be mediation is plausible and c shows an association while c' is smaller or close to zero, there is evidence for partial or full mediation, respectively.
Results
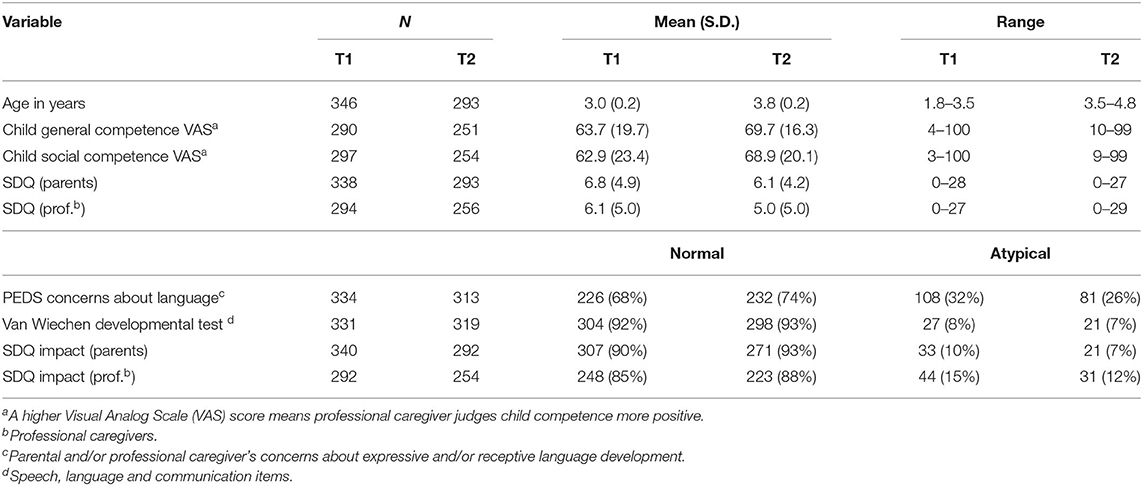
Parents of 346 children agreed to participate in the MOM study. At baseline, parents of 341 children and professional caregivers of 301 children completed the questionnaires. The mean age of the children was 3.0 years (SD 0.2, Table 1). For 296 of these children (86%), information from both informants was available. In the follow up, at the age of ~4 years (mean age 3.8; SD 0.2, Table 1), information of both informants was available for 236 children (68%). For 32 children (9%) there was no information available from parents or professional caregivers because they did not return the questionnaire. At baseline, the total sample of children consisted of 166 boys (48%) and 180 girls (52%). Of the participating children, 60% (n = 207) were resident in the municipality of Maastricht, while 40% (n = 139) lived in the surrounding areas. At baseline, parents and/or professional caregivers of 108 (32%) of 334 children had concerns about expressive and/or receptive language development (12 missings on the PEDS). In the follow up, at the age of 4 years, the total number of children with concerns about language development was 81 (26%) of 313 children (Table 1).
In order to test representativeness, 40% of non-responders were randomly sampled to manually collect data on parental education from the medical files. The distribution in non-responders was minimally different from distribution in responders (responders 63, 27, and 10% and non-responders 55, 33, and 12% having high, intermediate and low parental education, respectively).
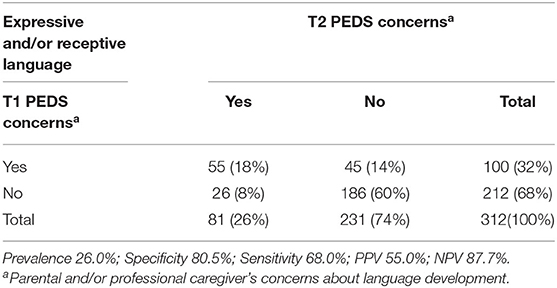
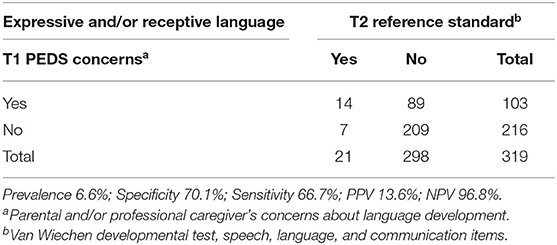
Validity of the PEDS Language Items
The prevalence of PCHC language concerns was 8% at the age of 3 and 7% one year later (Table 2). At the age of 3 years, PEDS language concerns had a PPV of 23% and NPV of 99%. At the age of 4, the PPV and NPV of PEDS language concerns were 19 and 97% respectively (Table 2). Table 3 shows the stability of language developmental concerns at the age of 3 and 4 years. The predictive validity of the PEDS at the age of 3 years was: PPV of 14% and NPV of 97% (Table 4).
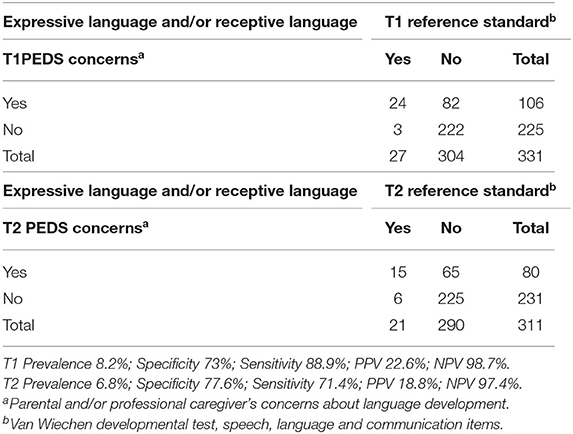
Table 2. Prevalence, Positive, and Negative Predictive Value of PEDS concerns about language development at the age of 3 and 4 years.
Association Between Language Development Concerns and Preschool Social Participation
When assessing parental SDQ impact at the age of 3 years, children with receptive language concerns had an OR of 7.3 and children with expressive language concerns had an OR of 2.4. However, confidence intervals were overlapping (Table 5).
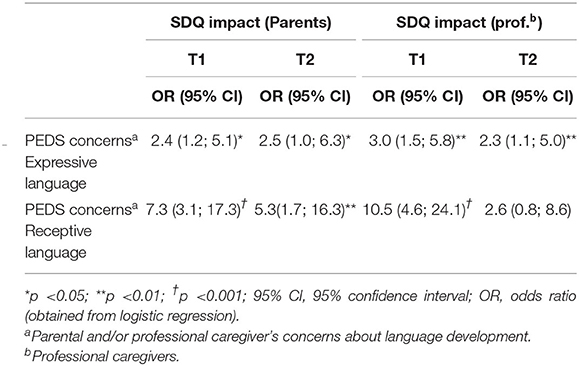
Table 5. Logistic regression analysis (significant interaction with one or both risk factors): association between PEDS concerns about expressive and receptive language development and SDQ impact according to parents and professional caregivers at the age of 3 and 4 years; odds ratios (OR) and 95% confidence intervals (CI).
According to professional caregivers, the association between receptive language concerns and outcomes was stronger than the association between expressive language and outcomes (e.g., general competence VAS: B = −21.3, p < 0.001; Table 6). In addition, both professional caregivers and parents reported more behavioral problems when there were receptive language concerns (SDQ total score B = 4.5, p < 0.001; B = 4.5, p < 0.001, respectively). A year later, the association between language concerns, competence and behavior was less strong but still significant, except for PEDS expressive language concerns and the parental perception of child behavior (Table 6).
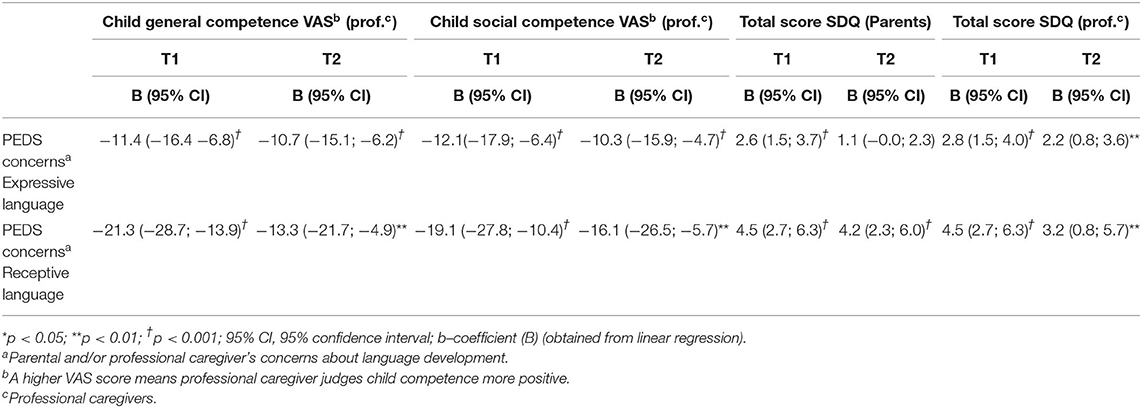
Table 6. Linear regression analysis: association between PEDS concerns about expressive and receptive language development and child general competence, child social competence, and total score SDQ according to parents and professional caregivers at the age of 3 and 4 years; b- coefficient (B) and 95% confidence intervals (CI).
Mediating Effect of Social Competence
At baseline and at follow up a year later, there was a significant association between social competence and social participation, but also a direct association between concerns about expressive and/or receptive language development and social competence. For example, according to the professional caregiver, at age 3 years there was a significant association between language concerns and social participation (SDQ impact B = 4.3, p < 0.001; SDQ total score B = 3.0, p < 0.001) and a significant association between social competence and social participation (SDQ impact B = 0.9, p < 0.001; SDQ total score B = −0.1, p < 0.001) (Tables 7, 8). There was a mediating effect of social competence: after inclusion of social competence in the regression model, the remaining association between language concerns and social participation was less strong (SDQ impact B = 2.8, p = 0.014; SDQ total score B = 1.2, p = 0.016). A year later, at the age of 4 years, the mediating effect of social competence was even stronger with non-significant regression coefficients (B = 1.1, p = 0.884 and B = 0.8, p = 0.198, respectively). When tested separately, the mediating effect was found both for expressive and receptive language concerns (data not shown). Mediating effects of social competence were also found between language concerns and general competence (data not shown).
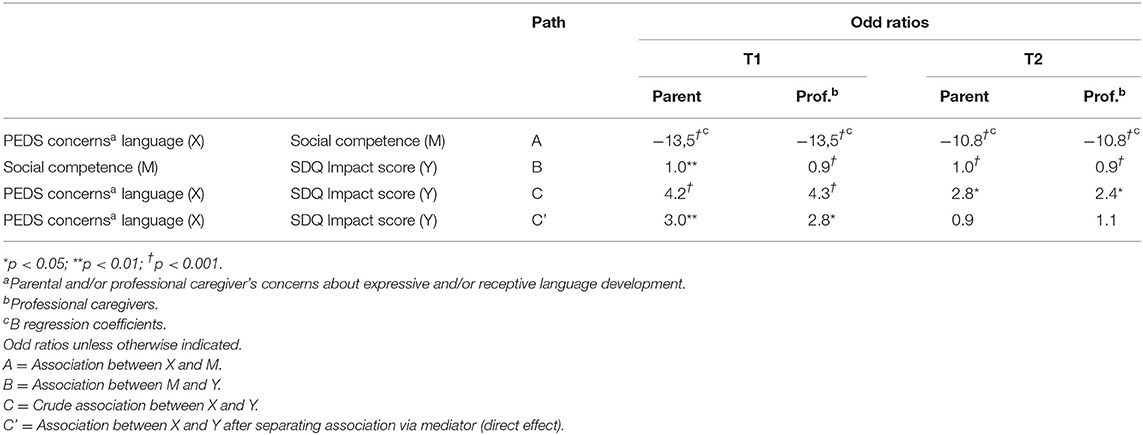
Table 7. Mediating effect of social competence on the association of PEDS concerns about language development with SDQ impact score at T1 and T2.
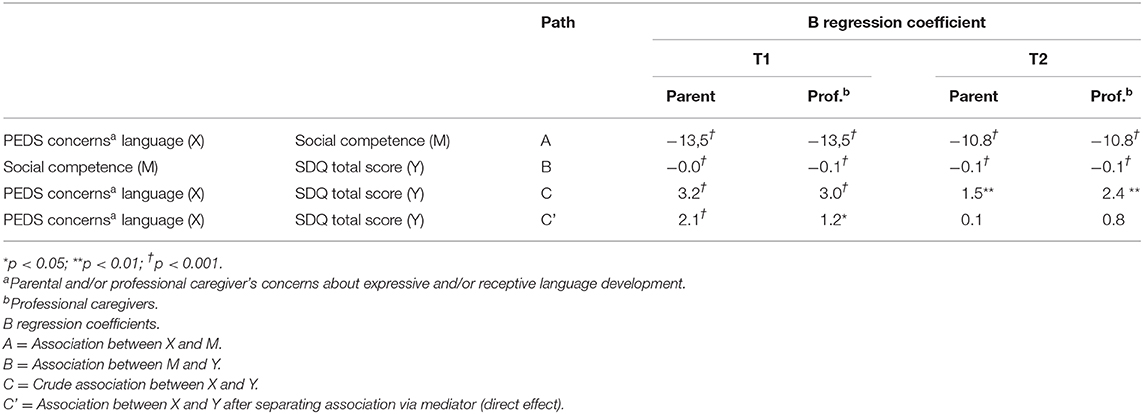
Table 8. Mediating effect of social competence on the association of PEDS concerns about language development with SDQ total score at T1 and T2.
Discussion
The results in this paper suggest concurrent and predictive validity of the PEDS to assess parental and professional caregivers' language development concerns, as well as the mediating effect of professional caregivers' perception of the child's social competence in the association between these concerns and social participation at the age of 3 years as well as the age of 4 years.
Validity of Preschool Language Development Concerns
Prevalence of language delay (7–8%) in the present study is within the international reported range of prevalence of atypical language delay (7–15%) (20, 21, 38). In addition, the association between parental and professional caregiver concerns on the one hand, and not meeting the expected milestones for language on the other, was statistically significant. These results are in line with other studies where parental concerns were consistently associated with preschool language development (40, 58, 63). Moreover, this confirms the value of including parents' and professional caregivers' expert knowledge in the assessment and clinical decision-making process for personalized support (28, 59). The high NPV of parental and professional caregiver language concerns validate a strategy of exclusion of children without concerns from extra monitoring. The PEDS language screening items appear to be very good in identifying children who do not have any language delay. Current assessment tools are still not sufficiently specific to discriminate between delayed language that will resolve naturally and delayed speech or language that will develop into persistent problems. The relatively low PPV in the present study implies a high percentage of false positives. Earlier research has shown that children with false positive screening results differ from children with true negative scores. These children had more risk factors and their performance on diagnostic measures was less (45). As confirmed by other population studies (17, 18, 26, 64), this article showed that while some preschool children grow out of language problems, others may develop them (Table 3). From a classical screening point of view, children crossing back and forth over the threshold would impact sensitivity and specificity. However, PCHC repeated monitoring concerns of language development and if necessary, extra follow up can make a distinction between children “growing into or out of deficit.”
So, PCHC monitors the true positives as well as the false positives and refers when needed, even if the child did not score on the reference standard. Language tests may not capture important aspects of everyday communication. In addition, a language problem may not always look like a language problem: underlying comprehension impairment can present as poor academic attainment, impaired social interaction, or behavioral difficulties (12, 65). Furthermore, due to the variation in the cut-off points of different “reference standard” measures in research, interpretation of parents' and professional caregivers' information is complicated. In addition, there is no agreement on different definitions of language disorders and what proportion of the population should be considered cases that need intervention (65).
Prediction of Preschool Social Participation: Mind the Communication
Parental and professional caregiver concerns were associated with altered social participation at home as well as in preschool. This association was seen both in cross-sectional and in longitudinal analyses.
Language concerns seem to be predictive for altered social participation as early as in preschool. Earlier research showed that especially children who experienced language impairment that persisted into the school years are at risk for adult mental health problems and substandard social participation (66). The strongest association was seen between receptive language delay concerns and behavioral problems. Odds ratio confidence intervals of children with receptive and expressive language concerns were overlapping, thus were not statistically significant, except for the association with parental SDQ total score at the age of 4 years (Table 5). From PCHC practice it is recognizable that receptive and expressive language development are closely linked, with more problems in social participation because of language comprehension problems. This confirms the observation that needs of children with receptive language problems are complex and call for extra monitoring of the child's developmental pathway (1). Listening to parental and professional caregivers' concerns with avoidance of diagnostic labels is an important aspect of PCHC clinical judgement and pre-screening. It may identify other developmental problems without potential stigmatization (23, 37). Avoidance of diagnostic labels is not the same as denying any role of biological risk factors in causing health problems; children vary in their biological as well in their social backgrounds and life events (65).
Mediating Effect of Social Competence
Language delay in itself may not be a risk factor for later behavioral and emotional disturbances (67). The present results showed that concerns about language development may reflect the effect of other developmental problems (68). There was a mediating effect of child social competence on the association between receptive and expressive language concerns and social participation at the age of 3 and 4. While at age 3 years social competence was a partial mediator, at age 4 it was a full mediator. So, at age 4, social competence seems to play a more important role in the association between concerns and participation. After inclusion of social competence score, language concerns seem to lose their predictive value but these factors might be related to each other.
The expansion of this mediating effect between ages 3 and 4 years emphasizes once again that all children with language concerns can benefit from additional monitoring to prevent “growing into deficit,” especially concerning interpersonal relationships. There is a role for enhanced monitoring in which the primary care professional responds to parental concerns about language development and social skills (3, 6, 23). The group of children with symptoms of mental problems may be twice as large as the group of children meeting formal diagnostic criteria for a mental disorder (69–77). Inefficiency can arise if educational and medical support is restricted to those who meet arbitrary cut-offs as a result of discrepancy in criteria used for diagnostic labels (65). Therefore, a PCHC “toolkit” with short instruments for regular short parental and professional caregivers' reports can serve as a first step in PCHC monitoring procedures to select children who require further support in the form of a “watch and wait” strategy, assessment of other developmental domains, or referral to a specialist. Professional support can then be tailored to the needs, conform the child's development.
PCHC professionals have to deal with emerging problems and symptoms at a stage where signs and symptoms do not yet meet diagnostic criteria, but already give rise to early impairment and distress for both the children and their context, at home as well as in preschool. Both parental and professional caregiver concerns are relevant for early detection of problems, because they both know the child and their perception is from a different perspective (41). The PEDS: (1) facilitates monitoring of parental and professional caregivers concerns; (2) identify general signals and symptoms not yet related to a specific diagnosis; (3) support communication between PCHC, parents and professional caregivers about their perceptions on health and development; and (4) promote shared decision making (23, 44).
Methodological Issues
Strength of the study is that a community sample of preschool children was systematically assessed using a comprehensive PCHC “toolkit” of instruments designed for the purpose of monitoring in a public health setting. The study was integrated in real life practice. No children were excluded for not meeting inclusion criteria. In addition, the child's development and participation was evaluated across different settings with cross-sectional and longitudinal information from different instruments and multiple informants. With emphasis on their perception, information was obtained through hetero-anamnesis of parents and professional caregivers (78). PCHC professionals provided data as well; with exception of the Van Wiechen developmental test, these data were not used in the present paper. Furthermore, the Van Wiechen language milestones were collected in a uniform manner by trained professionals.
The present paper has some limitations. First, response rates were difficult to establish. In the MOM region over the study period, 1,692 children were born and, therefore, were within the caseload of the PCHC professionals participating in the MOM study. However, not all PCHC professionals participated in MOM. Consequently, parents of non-participating PCHC doctors were asked to participate by another PCHC doctor (BD), who did not know these families. During the baseline inclusion, the number of participating PCHC professionals increased. Response from one PCHC doctor who participated from the beginning (BD) was 70%. Because response in participating doctors was relatively high and because distribution in socio-economic status was comparable, results presented in this article can be considered approximately representative for the general population. If the PEDS and different VAS are implemented in general PCHC practice, a response rate higher than 70% is expected, because a possible barrier for parents to participate in MOM was the number of questions added for research purposes (e.g., additional instruments for the purpose of validation of VAS). Usually, short form questionnaires collected in PCHC have response rates between 80 and 90% (79).
Second, the MOM data are limited to the city of Maastricht and surrounding areas. This part of the Netherlands is quite similar to the rest of the country. However, there are some differences. In Maastricht, the proportion of non-European inhabitants (about 10%) is less than in the larger cities in the north west of the country (about 30%) (80). In addition, the proportion of highly educated parents participating the MOM is quite large (63%). For this reason, the MOM study findings may not necessarily be valid for large cities with ethnically mixed populations and areas with a larger proportion of low educated parents.
Third, assessment tools were general in nature and did not reveal specific information to assist with remediation of deficits. The measures find general delay and it is not necessarily clear that the delays are clinically significant. PCHC professionals must remain aware they have to deal with emerging problems and symptoms at a stage where signs and symptoms do not yet meet diagnostic criteria. Although each type of parental concern can be associated with validated tests on the same developmental domain, studies about the validity of the PEDS showed that parents often have concerns in seemingly unrelated domains [i.e., parents often reflect on not just the apparent problem but also its impact on other aspects of development (40)]. Revelation of parental and professional caregivers' concerns are a first step in PCHC monitoring procedures to select children who require further assessment of other developmental domains, or referral to a specialist.
Fourth, social competence was included as a mediator and this was based on judgement of the professional caregiver. However, if a similar instrument was available from the parents, we would expect to find similar mediating effects.
Finally, because of the small sample size, analyses were not adjusted for risk factors (e.g., family history of language or literacy problems, health or developmental problems).
Conclusions
The individual's social and educational environment, including interpersonal relationships, is hypothesized to be instrumental for PCHC professionals wishing to provide personalized preventive public health care for successful participation for all children (31). In order to identify emerging problems at an early stage where signs and symptoms do not yet meet diagnostic criteria for a disorder, short but valid PCHC monitoring tools like the PEDS and different VAS are required (43). Within this PCHC “toolkit,” parental and professional caregivers' perception and concerns about language development take an important position. Language development can be seen as the outcome of the mental processes set in motion when the child meets the social and linguistic world (24, 81). The analyses presented here uncovered significant associations between parental and professional caregiver concerns about language development, the child's social competence and the level of preschool social participation. Therefore, pediatric primary care professionals may productively use parental and professional caregiver perceptions concerning preschool language development in clinical practice. Equally important is the perception of a child's social competence. In children not meeting the expected milestones for language development, a comprehensive developmental evaluation and additional monitoring of child development may be required, particularly concerning interpersonal relationships. Consequently, personalized health care requires cooperation within the public health frame. Monitoring of language and social competence development in preschool children can profit from continued communication between parents, professional caregivers and preventive child health care.
Data Availability Statement
The datasets for this article are not publicly available to conform with the General Data Protection Regulation, a European regulation regarding the processing of personal data. Requests to access the datasets should be directed to Bernice Doove, MD, YmVybmljZS5kb292ZUBnZ2R6bC5ubA==.
Ethics Statement
The Maastricht University Medical Center Medical Ethics Committee approved the MOM-study under registration number MEC 09-04-018/P. Therefore, this study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author's Note
Underlying research materials related to this paper are available on request by the corresponding author.
Author Contributions
BD drafted the initial manuscript. FF, JO, and MD reviewed and revised the manuscript. All authors approved the final manuscript as submitted, agreed to be accountable for all aspects of the work, and conceptualized and designed the study.
Funding
ZonMw, the Netherlands Organization for Health Research and Development, funded this study (No. 7125.0001).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Parents, professional caregivers, and colleagues are kindly thanked for their participation. Thanks to Frances Page Glascoe for permission to use the PEDS.
Abbreviations
PCHC, Preventive Child Health Care; PEDS, Parents' Evaluation of Developmental Status; SDQ, Strengths and Difficulties Questionnaire; Stata, Statistical Software Package; VAS, visual analog scale.
References
1. Schoon I, Parsons S, Rush R, Law J. Children's language ability and psychosocial development: a 29-years follow-up study. Pediatrics. (2010) 126:e73–80. doi: 10.1542/peds.2009-3282
2. Schoon I, Parsons S, Rush R, Law J. Childhood language skills and adult literacy: a 29-years follow-up study. Pediatrics. (2010) 125:e459–66. doi: 10.1542/peds.2008-2111
3. Mok PL, Pickles A, Durkin K, Conti-Ramsden G. Longitudinal trajectories of peer relations in children with specific language impairment. J Child Psychol Psychiatry. (2014) 55:516–27. doi: 10.1111/jcpp.12190
4. Stangeland EB. The impact of language skills and social competence on play behaviour in toddlers. Eur Early Childh Educ Res J. (2017) 25:106–21. doi: 10.1080/1350293X.2016.1266224
5. Huber M, Knottnerus JA, Green L, van der Horst H, Jadad AR, Kromhout D, et al. How should we define health? BMJ. (2011) 343:d4163. doi: 10.1136/bmj.d4163
6. Zubrick SRT, Catherine L, Lawrence D, Mitrou F, Christensen D, Dalby R. The development of human capability across the lifecourse: perspectives from childhood. Australasian Epidemiol. (2009) 16:6–10.
7. Beauchamp MH, Anderson V. SOCIAL: an integrative framework for the development of social skills. Psychol Bull. (2010) 136:39–64. doi: 10.1037/a0017768
8. Law J, Reilly S, Snow PC. Child speech, language and communication need re-examined in a public health context: a new direction for the speech and language therapy profession. Int J Lang Commun Disord. (2013) 48:486–96. doi: 10.1111/1460-6984.12027
9. Jones DE, Greenberg M, Crowley M. Early social-emotional functioning and public health: the relationship between kindergarten social competence and future wellness. Am J Public Health. (2015) 105:2283–90. doi: 10.2105/AJPH.2015.302630
10. Cunningham BJ, Rosenbaum PL. A Bioecological framework to evaluate communicative participation outcomes for preschoolers receiving speech-language therapy interventions in Ontario, Canada. Int J Lang Commun Disord. (2015) 50:405–15. doi: 10.1111/1460-6984.12145
11. Goorhuis-Brouwer SM, Knijff WA. Efficacy of speech therapy in children with language disorders: specific language impairment compared with language impairment in comorbidity with cognitive delay. Int J Pediatr Otorhinolaryngol. (2002) 63:129–36. doi: 10.1016/S0165-5876(02)00004-6
12. O'Hare Bremner L. Management of developmental speech and language disorders: part 1. Arch Dis Child. (2016) 101:272–7. doi: 10.1136/archdischild-2014-307394
13. Hawa VV, Spanoudis G. Toddlers with delayed expressive language: an overview of the characteristics, risk factors and language outcomes. Res Dev Disabil. (2014) 35:400–7. doi: 10.1016/j.ridd.2013.10.027
14. Siu AL, Force USPST. Screening for speech and language delay and disorders in children aged 5 years or younger: US preventive services task force recommendation statement. Pediatrics. (2015) 136:e474–81. doi: 10.1542/peds.2015-1711
15. Masten AS. Global perspectives on resilience in children and youth. Child Dev. (2014) 85:6–20. doi: 10.1111/cdev.12205
16. Rutter M. Resilience as a dynamic concept. Dev Psychopathol. (2012) 24:335–44. doi: 10.1017/S0954579412000028
17. Taylor CL, Zubrick SR. Predicting children's speech, language and reading impairment over time. Int J Speech Lang Pathol. (2009) 11:341–3. doi: 10.1080/17549500903161561
18. Ukoumunne OC, Wake M, Carlin J, Bavin EL, Lum J, Skeat J, et al. Profiles of language development in pre-school children: a longitudinal latent class analysis of data from the Early Language in Victoria Study. Child Care Health Dev. (2012) 38:341–9. doi: 10.1111/j.1365-2214.2011.01234.x
19. McCormack JMS, Mc Allister L, Harrison L. A systematic review of the association between childhood speech impairment and participation across the lifespan. Int J Speech-Language Pathol. (2009) 2:155–70. doi: 10.1080/17549500802676859
20. McLeod S, Harrison LJ. Epidemiology of speech and language impairment in a nationally representative sample of 4 to 5 years old children. J Speech Language Hearing Res. (2009) 52:1213–29. doi: 10.1044/1092-4388(2009/08-0085)
21. Tomblin JB, Records NL, Buckwalter P, Zhang X, Smith E, O'Brien M. Prevalence of specific language impairment in kindergarten children. J Speech Lang Hear Res. (1997) 40:1245–60. doi: 10.1044/jslhr.4006.1245
22. Snyderman R. Personalized health care: from theory to practice. Biotechnol J. (2012) 7:973–9. doi: 10.1002/biot.201100297
23. Syurina E, Hens K, Feron F. Literature review: use of family history for primary paediatric care as the next step towards use of genomics in healthcare. Curr Pediatr Rev. (2013) 9:353–72. doi: 10.2174/157339630904131223112559
24. Hoff E. How social contexts support and shape language development. Dev Rev. (2006) 26:55–88. doi: 10.1016/j.dr.2005.11.002
25. Fukkink R, Jilink L, Oostdam R. A meta-analysis of the impact of early childhood interventions on the development of children in the Netherlands: an inconvenient truth? Eur Early Childh Educ Res J. (2017) 25:656–66. doi: 10.1080/1350293X.2017.1356579
26. Levickis P, Sciberras E, McKean C, Conway L, Pezic A, Mensah FK, et al. Language and social-emotional and behavioural well-being from 4 to 7 years: a community-based study. Eur Child Adolesc Psychiatry. (2018) 27:849–59. doi: 10.1007/s00787-017-1079-7
27. Conway LJ, Levickis PA, Mensah F, McKean C, Smith K, Reilly S. Associations between expressive and receptive language and internalizing and externalizing behaviours in a community-based prospective study of slow-to-talk toddlers. Int J Lang Commun Disord. (2017) 52:839–53. doi: 10.1111/1460-6984.12320
28. McCormack J, McLeod S, Harrison LJ, McAllister L. The impact of speech impairment in early childhood: investigating parents' and speech-language pathologists' perspectives using the ICF-CY. J Commun Disord. (2010) 43:378–96. doi: 10.1016/j.jcomdis.2010.04.009
29. Sameroff A. A unified theory of development: a dialectic integration of nature and nurture. Child Dev. (2010) 81:6–22. doi: 10.1111/j.1467-8624.2009.01378.x
30. Pakarinen E, Salminen J, Lerkkanen M, Von Suchodoletz A. Reciprocal associations between social competence and language and pre-literacy skills in preschool. J Early Childh Educ Res. (2018) 7:207–34.
31. Williams PG AAP Council on Early Childhood and AAP Council on School Health. The pediatrician's role in optimizing school readiness. Pediatrics. (2016) 138:2293. doi: 10.1542/peds.2016-2293
32. van Esso D, del Torso S, Hadjipanayis A, Biver A, Jaeger-Roman E, Wettergren B, et al. Primary-Secondary Working Group of European Academy of Paediatric primary care in Europe: variation between countries. Arch Dis Child. (2010) 95:791–5. doi: 10.1136/adc.2009.178459
33. Garner AS. Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics. (2013) 132(Suppl.2):S65–73. doi: 10.1542/peds.2013-1021D
34. Kuo AA, Etzel RA, Chilton LA, Watson C, Gorski PA. Primary care pediatrics and public health: meeting the needs of today's children. Am J Public Health. (2012) 102:e17–23. doi: 10.2105/AJPH.2012.301013
35. Gan SM, Tung LC, Yeh CH, Chang HY, Wang CH. The ICF-CY-based structural equation model of factors associated with participation in children with autism. Dev Neurorehabil. (2014) 17:24–33. doi: 10.3109/17518423.2013.835357
36. Theunissen MHC. The Early Detection of Psychosocial Problems in Children Aged 0–6 Years by Dutch Preventive Child Health Care: Professionals and Their Tools. Groningen: University of Groningen (2013).
37. Syurina EV, Feron FJM. Advances in genetics and neuroscience: A challenge for personalizing child and youth health care? In: Hens K, Cutas D, Horstkötter D editors. Parental Responsibility in the Context of Neuroscience and Genetics. Maastricht: Springer International Publishing (2017). p. 55–72.
38. Reilly S, McKean C, Morgan A, Wake M. Identifying and managing common childhood language and speech impairments. BMJ. (2015) 350:h2318. doi: 10.1136/bmj.h2318
39. van der Vleuten CP, Schuwirth LW, Driessen EW, Govaerts MJ, Heeneman S. 12 Tips for programmatic assessment. Med Teach. (2015) 37:641–6. doi: 10.3109/0142159X.2014.973388
40. Glascoe FP. Collaborating with Parents: Using Parents' Evaluation of Developmental Status (PEDS) to Detect and Address Developmental and Behavioural Problems. Nolensville, TN: Pedstest (2013).
41. Kaurin A, Egloff B, Stringaris A, Wessa M. Only complementary voices tell the truth: a reevaluation of validity in multi-informant approaches of child and adolescent clinical assessments. J Neural Transm. (2016) 123:981–90. doi: 10.1007/s00702-016-1543-4
42. Thompson EJ, Beauchamp MH, Darling SJ, Hearps SJC, Brown A, Charalambous G, et al. Protocol for a prospective, school-based standardisation study of a digital social skills assessment tool for children: the Paediatric Evaluation of Emotions, Relationships, and Socialisation (PEERS) study. BMJ Open. (2018) 8:e016633. doi: 10.1136/bmjopen-2017-016633
43. Doove B, Feron J, Feron F, van Os J, Drukker M. Validation of short instruments assessing parental and caregivers' perceptions on child health and development for personalized prevention. Clin Child Psychol Psychiatry. (2019) 24:608–30. doi: 10.1177/1359104518822673
44. Marks KP, Glascoe FP, Macias MM. Enhancing the algorithm for developmental-behavioral surveillance and screening in children 0 to 5 years. Clin Pediatr. (2011) 50:853–68. doi: 10.1177/0009922811406263
45. Glascoe FP. Are overreferrals on developmental screening tests really a problem? Arch Pediatr Adolesc Med. (2001) 155:54–9. doi: 10.1001/archpedi.155.1.54
46. Theunissen MHC, Vogels AG, de Wolff MS, Crone MR, Reijneveld SA. Comparing three short questionnaires to detect psychosocial problems among 3 to 4-years olds. BMC Pediatr. (2015) 15:84. doi: 10.1186/s12887-015-0391-y
47. Potijk MR, de Winter AF, Bos AF, Kerstjens JM, Reijneveld SA. Co-occurrence of developmental and behavioural problems in moderate to late preterm-born children. Arch Dis Child. (2016) 101:217–22. doi: 10.1136/archdischild-2015-308958
48. Kerstjens JM, Bos AF, ten Vergert EM, de Meer G, Butcher PR, Reijneveld SA. Support for the global feasibility of the Ages and Stages Questionnaire as developmental screener. Early Hum Dev. (2009) 85:443–7. doi: 10.1016/j.earlhumdev.2009.03.001
49. Sim F, Thompson L, Marryat L, Ramparsad N, Wilson P. Predictive validity of preschool screening tools for language and behavioural difficulties: a PRISMA systematic review. PLoS ONE. (2019) 14:e0211409. doi: 10.1371/journal.pone.0211409
50. Woolfenden S, Eapen V, Williams K, Hayen A, Spencer N, Kemp L. A systematic review of the prevalence of parental concerns measured by the Parents' Evaluation of Developmental Status (PEDS) indicating developmental risk. BMC Pediatr. (2014) 14:231. doi: 10.1186/1471-2431-14-231
51. Limbos MM, Joyce DP. Comparison of the ASQ and PEDS in screening for developmental delay in children presenting for primary care. J Dev Behav Pediatr. (2011) 32:499–511. doi: 10.1097/DBP.0b013e31822552e9
52. Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. (2001) 40:1337–45. doi: 10.1097/00004583-200111000-00015
53. van Widenfelt BM, Goedhart AW, Treffers PD, Goodman R. Dutch version of the Strengths and Difficulties Questionnaire (SDQ). Eur Child Adolesc Psychiatry. (2003) 12:281–9. doi: 10.1007/s00787-003-0341-3
54. Stone LL, Otten R, Engels RC, Vermulst AA, Janssens JM. Psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire for 4- to 12-years-olds: a review. Clin Child Fam Psychol Rev. (2010) 13:254–74. doi: 10.1007/s10567-010-0071-2
55. Laurent di Angulo MS. Ontwikkelingsonderzoek in de jeugdgezondheidszorg. Van Gorcum: Assen (2008).
56. Jacobusse G, van Buuren S, Verkerk PH. An interval scale for development of children aged 0–2 years. Stat Med. (2006) 25:2272–83. doi: 10.1002/sim.2351
57. van Buuren S. Growth charts of human development. Stat Methods Med Res. (2014) 23:346–68. doi: 10.1177/0962280212473300
58. van Agt HM, van der Stege HA, de Ridder-Sluiter JG, de Koning HJ. Detecting language problems: accuracy of five language screening instruments in preschool children. Dev Med Child Neurol. (2007) 49:117–22. doi: 10.1111/j.1469-8749.2007.00117.x
59. Harrison LJ, McLeod S, McAllister L, McCormack J. Speech sound disorders in preschool children: correspondence between clinical diagnosis and teacher and parent report. Austr J Learn Difficult. (2017) 22:35–48. doi: 10.1080/19404158.2017.1289964
60. Diepeveen FB, Dusseldorp E, Bol GW, Oudesluys-Murphy AM, Verkerk PH. Failure to meet language milestones at 2 years of age is predictive of specific language impairment. Acta Paediatr. (2016) 105:304–10. doi: 10.1111/apa.13271
61. Diepeveen FB, van Dommelen P, Oudesluys-Murphy AM, Verkerk PH. Concise tool based on language milestones identifies children with specific language impairment at 24–45 months of age. Acta Paediatr. (2018) 107:2125–30. doi: 10.1111/apa.14596
62. StataCorp., Stata Statistical Software: Release 15. TX: StataCorp LP, College Station, Texas (2017).
63. Klee T, Pearce K, Carson DK. Improving the positive predictive value of screening for developmental language disorder. J Speech Lang Hear Res. (2000) 43:821–33. doi: 10.1044/jslhr.4304.821
64. Roulstone S, Peters TJ, Glogowska M, Enderby P. A 12-months follow-up of preschool children investigating the natural history of speech and language delay. Child Care Health Dev. (2003) 29:245–55. doi: 10.1046/j.1365-2214.2003.00339.x
65. Bishop DV. Ten questions about terminology for children with unexplained language problems. Int J Lang Commun Disord. (2014) 49:381–415. doi: 10.1111/1460-6984.12101
66. Snowling MJ, Bishop DV, Stothard SE, Chipchase B, Kaplan C. Psychosocial outcomes at 15 years of children with a preschool history of speech-language impairment. J Child Psychol Psychiatry. (2006) 47:759–65. doi: 10.1111/j.1469-7610.2006.01631.x
67. Whitehouse AJ, Robinson M, Zubrick SR. Late talking and the risk for psychosocial problems during childhood and adolescence. Pediatrics. (2011) 128:e324–32. doi: 10.1542/peds.2010-2782
69. Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children's social-emotional development and psychopathology: recent advances and recommendations for practice. J Child Psychol Psychiatry. (2004) 45:109–34. doi: 10.1046/j.0021-9630.2003.00316.x
70. Hielkema M, de Winter AF, de Meer G, Reijneveld SA. Effectiveness of a family-centered method for the early identification of social-emotional and behavioral problems in children: a quasi experimental study. BMC Public Health. (2011) 11:636. doi: 10.1186/1471-2458-11-636
71. Spijkers W, Jansen DE, de Meer G, Reijneveld SA. Effectiveness of a parenting programme in a public health setting: a randomised controlled trial of the positive parenting programme (Triple P) level 3 versus care as usual provided by the preventive child healthcare (PCH). BMC Public Health. (2010) 10:131. doi: 10.1186/1471-2458-10-131
72. Lavigne JV, Binns HJ, Christoffel KK, Rosenbaum D, Arend R, Smith K, et al. Behavioral and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians' recognition. Pediatric Practice Research Group. Pediatrics. (1993) 91:649–55.
73. Lavigne JV, Lebailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-years-olds. J Clin Child Adolesc Psychol. (2009) 38:315–28. doi: 10.1080/15374410902851382
74. American Academy of Pediatrics. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. (2006) 118:405–20. doi: 10.1542/peds.2006-1231
75. Luby JL, Gaffrey MS, Tillman R, April LM, Belden AC. Trajectories of preschool disorders to full DSM depression at school age and early adolescence: continuity of preschool depression. Am J Psychiatry. (2014) 171:768–76. doi: 10.1176/appi.ajp.2014.13091198
76. Gill AM, Hyde LW, Shaw DS, Dishion TJ, Wilson MN. The Family Check-Up in early childhood: a case study of intervention process and change. J Clin Child Adolesc Psychol. (2008) 37:893–904. doi: 10.1080/15374410802359858
77. Bayer JK, Rapee RM, Hiscock H, Ukoumunne OC, Mihalopoulos C, Wake M. Translational research to prevent internalizing problems early in childhood. Depress Anxiety. (2011) 28:50–7. doi: 10.1002/da.20743
78. Wolraich ML, Felice ME, Drotar D. The Classification of Child and Adolescent Mental Diagnosis in Primary Care: Diagnostic and Statistical Manual for Primary Care (DSM-PC) Child and Adolescent Version. Elk Grove Village, IL: American Academy of Pediatrics (1996).
79. de Wolff MS, Theunissen MH, Vogels AG, Reijneveld SA. Three questionnaires to detect psychosocial problems in toddlers: a comparison of the BITSEA, ASQ:SE, and KIPPPI. Acad Pediatr. (2013) 13:587–92. doi: 10.1016/j.acap.2013.07.007
80. Tjin-A-Tsoi TBPM. Jaarrapport integratie 2016. Den Haag: Centraal Bureau voor de Statistiek (2016).
Keywords: preschool social participation, social competence, communication, early identification, language concerns, PEDS, personalized health care, monitoring
Citation: Doove BM, Feron FJM, van Os J and Drukker M (2021) Preschool Communication: Early Identification of Concerns About Preschool Language Development and Social Participation. Front. Public Health 8:546536. doi: 10.3389/fpubh.2020.546536
Received: 28 March 2020; Accepted: 31 December 2020;
Published: 22 January 2021.
Edited by:
Daniel Holzinger, Hospitaller Brothers of Saint John of God Linz, AustriaReviewed by:
Laura Nabors, University of Cincinnati, United StatesDavid Saldaña, Sevilla University, Spain
Copyright © 2021 Doove, Feron, van Os and Drukker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernice M. Doove, YmVybmljZS5kb292ZUBnZ2R6bC5ubA==; YmVybmljZS5kb292ZUBtYWFzdHJpY2h0dW5pdmVyc2l0eS5ubA==; orcid.org/0000-0002-3189-4276
 Bernice M. Doove
Bernice M. Doove Frans J. M. Feron
Frans J. M. Feron Jim van Os
Jim van Os Marjan Drukker
Marjan Drukker