
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 07 August 2020
Sec. Health Economics
Volume 8 - 2020 | https://doi.org/10.3389/fpubh.2020.00310
Background: Stomach cancer is a huge threat to the health of Chinese people. However, few studies have looked into the expenditure and financial burden due to stomach cancer in China.
Methods: To estimate the direct (medical and non-medical) and indirect expenditure for diagnosis and treatment for stomach cancer patients in China, a multicenter survey was conducted in 37 tertiary hospitals in 13 provinces across China from 2012 to 2014. Each enrolled patient was interviewed through a structured questionnaire. The medical and non-medical expenditure at different clinical stages, the composition of non-medical expenditure, and the time loss for the cancer patient and their family were assessed. All expenditure data were inflated to the 2014 Chinese Yuan [CNY; 1 CNY = 0.163 USA dollar (USD)].
Results: A total of 2,401 stomach cancer patients with a mean age of 58.1 ± 11.4 years were included, predominately male. The overall average direct expenditure per patient was estimated to be US $9,899 (medical expenditure 91.2%, non-medical expenditure 8.8%), and the expenditures for stage I, II, III, and IV were $8,648, $9,004, $9,810, and $10,816, respectively; expenditure in stage III and IV was significantly higher than that in stages I and II (p < 0.05). One-year out-of-pocket expenditure of a newly diagnosed patient with stomach cancer was $5,368, accounting for 63.8% of their previous-year household income, which led to 79.2% families suffering an unmanageable financial burden. The average loss of time for patients and caregivers was $996.
Conclusions: This study indicated that the economic burden of stomach cancer in urban China was onerous. Effective intervention is necessary to reduce the financial burden by reducing the personal payment ratio and increasing the reimbursement ratio.
Stomach cancer incidence and mortality have declined significantly worldwide over the past 4-5 decades, but it remains a global health problem as the fifth most common cancer and the third most common cause of cancer-related deaths worldwide (1). Even today, stomach cancer incidence and mortality remain extremely high in China, which is responsible for 42.6% of the new cases and 45.0% of the death cases in the world (2). In 2015, it was estimated that 679,100 new cases and 498,000 deaths occurred in China (3). Moreover, due to a lack of awareness of physical examination and screening, most patients with stomach cancer have developed to the late stage, missing the optimal treatment time period. Thus, the current status of the stomach cancer epidemic in China dramatically affects people's health and imposes a large financial burden on both the family and society.
Given the growing trend of diagnostic and therapeutic technologies and changes in lifestyles and in people's expectations of the health system, the cost of the healthcare system and the out-of-pocket costs for patients' families are increasingly growing (4). Moreover, many studies have indicated that both cancer patients and their family members suffer a financial burden (4–8). Timely estimation of the costs of care for cancer patients assesses the general status of a population's health under the current healthcare system, which is a vital component of national programs and policies for cancer (9); thus, it enables the development of optimal policies in order to relieve the burden on family and society.
Numerous studies have been carried out on the financial burden of cancer worldwide but rarely on stomach cancer (10–12). Additionally, the majority of them concentrate mainly on the medical expenditure that is documented on hospital information systems; few studies focus on the non-medical expenditure (12–14). Only one multicenter study (five rural and two urban areas) reported direct and indirect expenditure until now (15).
In consideration of the context of the high prevalence of stomach cancer and limited evidence concerning the economic evaluation of stomach cancer in China (12), the study of direct (medical and non-medical) and indirect expenditure of stomach cancer is extremely necessary and meaningful.
In October 2012, the National Health and Family Planning Commission of China initiated the population-based Cancer Screening Program in Urban China (CanSPUC) (16, 17), targeting five types of cancer that are most prevalent in urban areas, i.e., upper digestive tract cancer (stomach cancer and esophageal cancer), lung cancer, breast cancer, liver cancer, and colorectal cancer. Eligible participants are recruited in the communities of the study regions and invited to undertake cancer screening free of charge. As a part of the health economic evaluation research of the CanSPUC, the objective of the study is to estimate both medical and non-medical expenditures overall and for subgroups of stomach cancer patients, to identify the subsequent financial burdens imposed on patient families, and to assess whether the screening strategies involved in the uninterrupted CanSPUC are cost-effective at the current scale or an expanded scale in the future.
We conducted a multicenter, hospital-based, cross-sectional study in 21 cities from 13 provinces (Shandong, Beijing, Jiangsu, Guangdong, Zhejiang, Hebei, Liaoning, Hunan, Heilongjiang, Henan, Xinjiang, Gansu, and Chongqing) in the east, west, south, and north of China between September 2012 and December 2014, which covered the first 2 years after the CanSPUC startup. A total of 37 tertiary hospitals (23 general hospitals and 14 specialized hospitals) were involved, which is the leading medical hub providing standard and advanced medical care. The details for the 13 provinces concerning population size, gross domestic product (GDP) per capita in 2014 based on the China Statistical Yearbook 2015 (18), number of cities, and general and specialized hospitals are shown in Table S1. The survey was approved by the Institutional Review Board of the Cancer Hospital of the Chinese Academy of Medical Sciences. All patients provided written informed consent.
A total of 2,401 stomach cancer patients were expected from the 13 study provinces. Briefly, according to a uniform design scheme, a stratified convenience sampling approach was used for selecting 240 stomach patients from each province. To reach a sufficient power for subgroup analyses, we tried to balance sample sizes among gender (maximum 60% for either gender) and cancer stage (19) (~25% for all clinical stages). All respondents were interviewed face to face using a structured questionnaire at the time of discharge, when most treatment expenses had already been incurred. Family members or caregivers helped with the interview for patients in poor physical condition; otherwise, the patients themselves gave the interview.
During the survey process, the subjects were interviewed face to face by trained investigators using a unified questionnaire designed by health economics experts for data collection. The questionnaire included five sections that are introduced briefly as follows (17): (1) demographic and societal information; (2) clinical information; (3) expenditure information for the whole course of illness to date; (4) time loss due to the whole course of clinical visits to date; and (5) quality control. Only if the first four sections were evaluated as of excellent or good reliability would the record be regarded as high quality; otherwise, it was deemed to be low quality, and the subject was excluded from our study. With regard to the inclusion criteria, each patient aged 40–69 years was diagnosed pathologically with primary stomach cancer, primarily underwent treatment at a hospital affiliated with the CanSPUC project, could understand the survey process, and provided informed consent.
The overall expenditure of each patient during the whole course of illness was estimated, which included both medical (amount spent for diagnosis or treatment of stomach cancer) and non-medical (including meals, accommodation, transportation, nutrition, and employee escort fees) expenditures. Medical expenditures were paid in part by the insurers, while non-medical expenditures were paid completely by the patients. Expenditure data indicated the estimates for the whole course of the disease where not specified otherwise. A newly diagnosed course was defined as 2 months before diagnosis and 10 months after diagnosis, which is not completely the same as the commonly used definition (1 year after diagnosis) on the grounds that a great amount of money, in China, is usually spent on diagnosis before the confirmation of the pathological pattern. All patient-paid medical expenditure items and non-medical expenditure of a newly diagnosed course were defined as out-of-pocket expenditure. With the exception of calculating the proportional breakdown of non-medical expenditures, all expenditure data were converted to the 2014 Chinese Yuan (CNY; 1 CNY = 0.163 USD) using the year-specific healthcare consumer price index of China (20).
The indicator of the expense-income ratio, equal to the average out-of-pocket expense of a newly diagnosed course divided by the average previous-year household income, was used to objectively reflect the financial burden. Financial catastrophe, using this threshold, occurs with an expense-income ratio equal to or >40% of total household income (21). Furthermore, to further access financial pressure, we asked the patient, “Which of the following accurately describes the financial pressure on your family from your disease?” and offered four response options: “None at all,” “Some, but manageable,” “Heavy,” and “Overwhelming.” “Not at all” and “Some, but manageable” were classified as manageable burdens and the other two responses as unmanageable burdens.
First, the questionnaire was designed by an experienced expert committee. Second, all well-trained investigators were required to check each questionnaire before completing the survey, and within 2 days, another member of the research staff would subsequently double-check each questionnaire. Third, a data administrator from the National Cancer Center of China would perform a logical test.
All data were double-entered into EpiData 3.1 software (EpiData Association, Odense, Denmark), and data analysis was performed using SAS 9.2 statistical software (SAS Institute, Cary/NC, USA).
Subgroup analyses of overall expenditure, expense-income ratio, financial pressure, and time loss were conducted. Overall expenditure after logarithm transition, expense-income ratio, and time loss were compared using the two-sample Student's t-test for a two-group comparative analysis or ANOVA for more than two groups; the SNK-q test was used for multiple comparisons. The χ2-test was used to determine financial pressure. All statistical tests were two-sided, and p < 0.05 was considered statistically significant.
A total of 2,401 stomach patients with a mean age at diagnosis of 58.1 ± 11.4 years old were finally included. Out of these patients, 607 (25.3%) came from general hospitals and 1,794 (74.7%) from specialized hospitals; 1,677 (69.8%) were men, over twice as many as women (724, 30.2%); the largest numbers of the patients had had primary-school eduction or lower (912, 38.0%) and were farmers (1,066, 44.4%). The mean of previous-year household income and income per patient in the last 5 years were US $8,415 ± $7,863 and $4,476 ± $4,327, respectively. The most common healthcare insurance type was the new rural cooperative medical scheme (1,136, 47.3%), followed by urban employee basic medical insurance (803, 33.4%), and urban resident basic medical insurance (404, 16.8%). The percentages of clinical stage I, II, III, and IV disease were 17.5, 14.4, 27.5, and 38.9%, respectively. More detailed information about the questionnaire results is shown in Table 1.
In 13 provinces, overall expenditure ranged from $6,633 (Chongqing) to $14,352 (Shandong) (Table S1). Spearman correlation analysis indicated that the overall expenditure was not associated with the economy of each site (r = 0.154, p = 0.616; Table S1). We, therefore, did not use the GDP per capita in the later univariate and multivariate analyses.
When we conducted the univariate analysis to identify subgroups associated with overall expenditure (Table 2), the age at diagnosis (p = 0.744) and gender (p = 0.177) showed no significant differences; patients in specialized hospitals (p < 0.025) or those who were well-educated (undergraduate or higher) (p < 0.001) spent more compared with their control groups; farmer patients (p < 0.001), those on the new rural cooperative medical scheme (p = 0.027), those with a lower household income (p = 0.045), or those who were diagnosed with adenocarcinoma (p < 0.001) spent less. Multivariate analysis was conducted and showed that patients who were diagnosed at stages IV (p < 0.001) and III (p < 0.008), with undergraduate or higher eduction (p < 0.001) or were retired (p < 0.003) and public-sector employees (p < 0.003) spent more compared with their control groups. Tables 3, 4 showed the expenditure details.
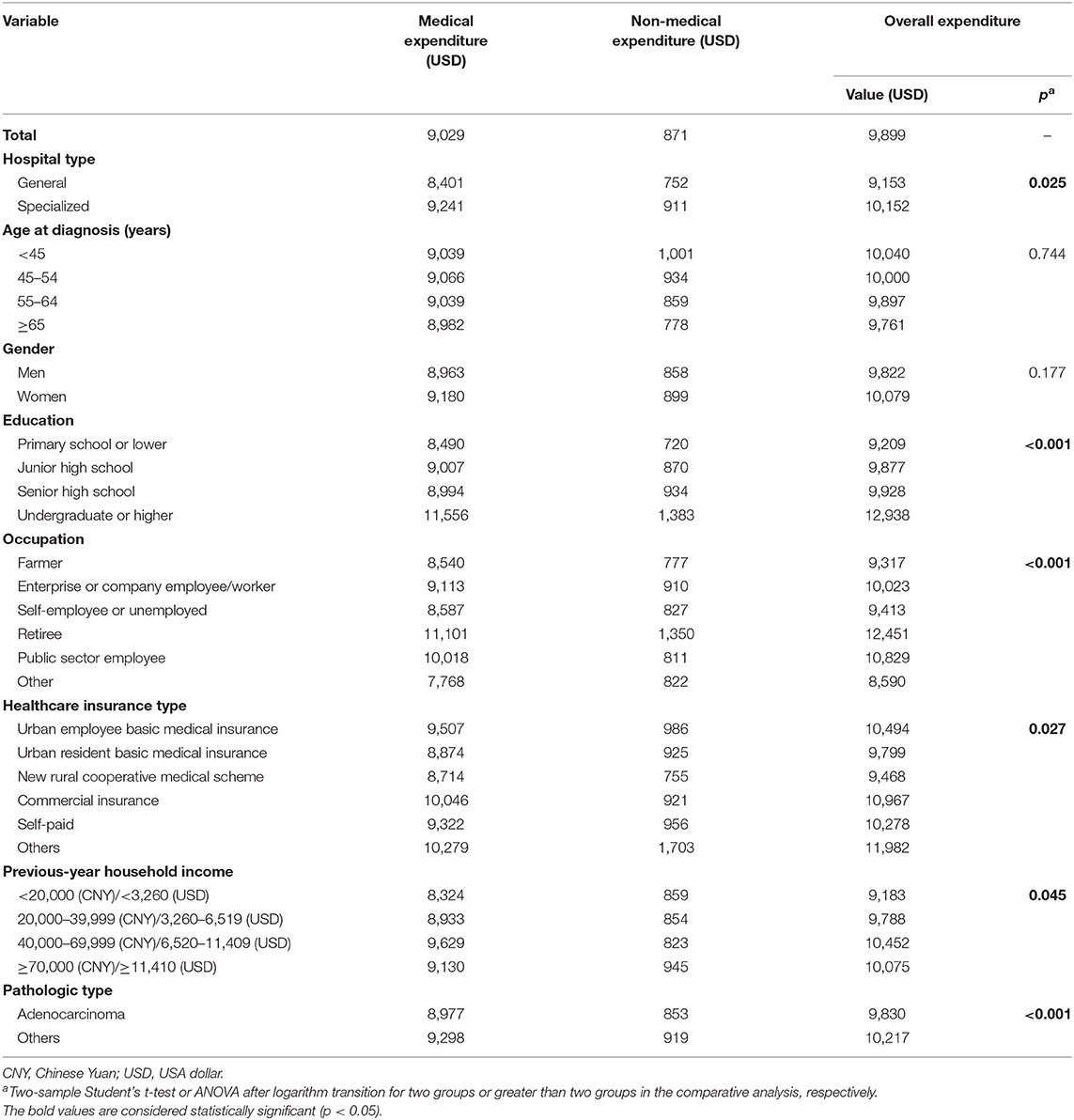
Table 2. Univariate analysis of expenditure for diagnosis and treatment of 2,401 patients with stomach cancer.
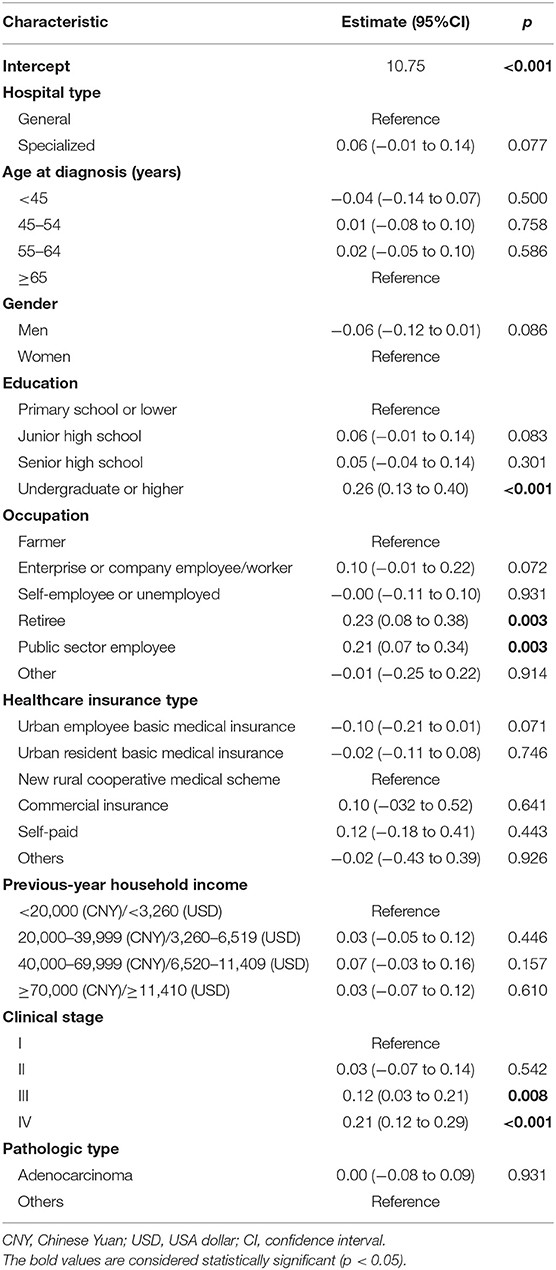
Table 3. Multivariate analysis of overall expenditure for diagnosis and treatment of 2,401 patients with stomach cancer.
Overall the mean expenditure of each stomach cancer patient was $9,899, with 91.2% ($9,029) being accounted for by medical expenditure and 8.8% ($871) by non-medical expenditure (Table 2). The overall, medical, and non-medical expenditures all showed a dramatic rise with progression of the disease (all p < 0.001; Figure 1).
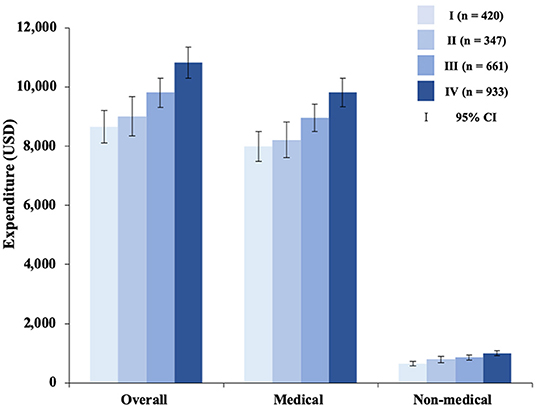
Figure 1. Medical and non-medical expenditure for stomach cancer diagnosis and treatment by clinical stage. Of the 2,361 patients included, 40 supplied no information on clinical stage. USD, USA dollar; CI, confidence interval.
When we made multiple comparisons for clinical stages in terms of overall, medical, and non-medical expenditures, stages I and III, I–IV, II–III, and II–IV diseases showed significant differences in both overall and medical expenditure (p < 0.05); stages I–II, I–III, I–IV, and II–IV showed significant differences in non-medical expenditure (p < 0.05). Overall expenditure ranged from $8,648 (95% CI $8,098–$9,198) for stage I disease, to $9,810 CNY (95% CI $9,318–$10,303) for stage III disease, with a 13.4% growth rate, to $10,816 CNY (95% CI $10,290–$11,342) for stage IV disease, with a 25.1% growth rate; medical expenditure ranged from $7,992 (95% CI $7,480–$8,505) for stage I disease, to $8,957 (95% CI $8,505–$9,409) for stage III disease, with 12.1% a growth rate, to $9,816 (95% CI $9,336–$10,296) for stage IV disease, with a 22.8% growth rate; non-medical expenditure ranged from $656 (95% CI $583–$729) for stage I disease, to $854 (95% CI $775–$932) for stage III disease, with 30.2% a growth rate, to $1,000 (95% CI $919–$1,081) for stage IV disease, with a 52.5% growth rate (Figure 1).
In non-medical expenditure, additional meals accounted for the largest proportion ($248, 28.5%), followed by transportation ($179, 20.6%) and additional nutrition ($171, 19.7%). Detailed information about non-medical expenditure is shown in Figure 2.
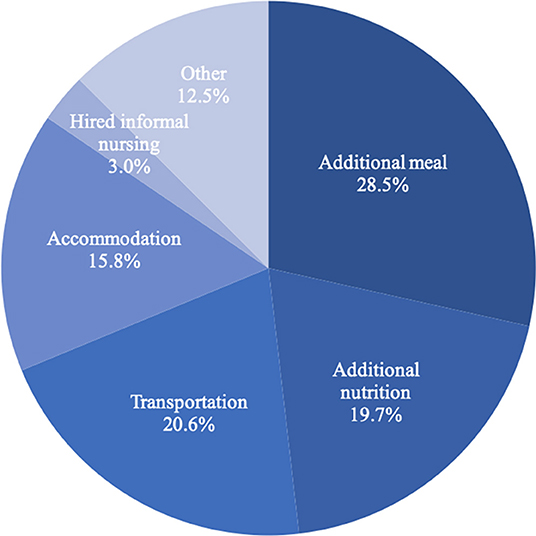
Figure 2. The proportional breakdown of non-medical expenditure for stomach cancer diagnosis and treatment.
The overall expenditure of a newly diagnosed illness course was $9,155, which was responsible for 92.5% ($9,899) of the total expenditure of the whole course of illness. The self-reported predicted reimbursement ratio was 43.0%; out-of-pocket expenditure ($5,368) accounted for 63.8% of the previous-year household income ($8,415). Of all patient families, 79.2% of the families felt an unmanageable burden (29.7% heavy, 49.5% overwhelming), 16.1% felt some burden but considered it manageable, and only 4.7% felt no burden at all.
Patients who were diagnosed at a younger age (≤54 years) felt more of an unmanageable burden than those diagnosed at an older age (p < 0.001). The expense-income ratio for patients with poor education (primary school or lower) was 0.76; the patients feeling an unmanageable burden accounted for 84.1% (28.7% heavy, 55.4% overwhelming), which was higher than for well-educated patients (p < 0.001). The expense-income ratio for patients who were farmers was 0.89, which was the highest in all occupations; 88.2% the farmer patients considered the burden unmanageable, and they felt a higher financial burden than any other occupation group (p < 0.001).
Patients who had the new rural cooperative medical scheme insurance spent 88.0% of their household income. However, 90% (23.3% heavy, 66.7% overwhelming) self-pay patients experiencing unmanageable financial pressure, which is higher than other healthcare insurance types, although the out-of-pocket expenditure of self-pay patients accounted for only 61% of the previous-year household income. Just as we expected, patients with lower household income (<20,000 CNY/<3,260 USD) experienced dramatic financial pressure, and they had spent more than 3.5 times the previous-year household income, making 95.5% (18.8% heavy, 76.7% overwhelming) of these families unable to afford treatment. We still found that families of stage I stomach cancer patients suffered the lowest pressure (76.9%), but it was not small. Financial pressure did not show significant differences with Hospital type (p = 0.056) and gender (p = 0.995). More information about the financial burden of overall expenditure is shown in Table 4.
Mean overall time loss totaled 88.1 person-days, including 48.8 person-days (55.4%) for patients and 39.3 person-days (44.6%) for caregivers. The average value of loss of time was $996.
Patients whose previous-year household income was <20,000 CNY (<3,260 USD) (p < 0.001) or those who were diagnosed with adenocarcinoma (p = 0.018) suffered relatively more time loss than patients who had higher income or those who were diagnosed with other pathologic types; on the other hand, patients who were diagnosed with stage I–II disease (p < 0.021) suffered less than their corresponding control groups, whereas stratified by the other subgroups hospital type (p = 0.808), age at diagnosis (p = 0.251), gender (p = 0.393), education (p = 0.588), occupation (p = 0.514), or healthcare insurance type (p = 0.085), there was no difference (Table 5).
In China, stomach cancer is the second most commonly diagnosed cancer in men and the third most common in women. Unlike other countries, the incidence and mortality rate continue to increase or are stable. Almost half of the new cases in 2012 occurred in China (2). Moreover, the hospitalization expense of treatment for stomach cancer increased by 49.5% from 2011 to 2015 after adjusting for purchasing power in China (22), indicating that the financial burden is heavy. Given that there is a lack of evidence on direct (medical and non-medical expenditure) and indirect expenditure in China, our investigation is therefore crucial for the medical security system and policy-making.
The study first reported multicenter data from more than 10 provinces in China concerning the direct and indirect medical expenditure of patients with stomach cancer. A total of 2,041 stomach patients from 13 provinces were included, most of whom were diagnosed and treated in specialized hospitals (74.7%). The number of men was more than double that of women, which was almost the same as the study by the National Central Cancer Registry: estimated new male and female cancer patients in China was 70.3 and 29.7%, respectively (2).
The average overall expenditure per patient was calculated to be $9,899 (medical expenditure $9,029, non-medical expenditure $871), and the overall expenditure was not associated with the economy of each province on the basis of Spearman correlation analysis (r = 0.154, p = 0.616). The amount is far higher than that reported by Zhao et al. (23) in Anhui province, China (overall expenditure $2,586, medical expenditure $2,384, and non-medical expenditure $201), those reported by Xu et al. (24) in Xinjiang province, China ($794 medical expenditure, accounting for 92.4%; $65 non-medical expenditure, accounting for 7.6%), and those reported by Sun et al. (14) from 13 provinces in China (medical expenditure $7,050, but non-medical expenditure not included), but lower than the study by Li et al. in Taiwan province ($10,780 for initial care of per patient with stomach cancer) (25). Looking at foreign countries, total medical costs for a patient with stomach cancer were $6,500 in Iran in 2015, which was lower than found in our study (4).
In our multicenter study, medical expenditure for late-stage cancer (III and IV) was higher than for care for early-stage cancer (I and II), which was consistent with previous studies (4, 26). It is well-known that late-stage patients have longer hospitalizations and more expensive therapy, such as radiotherapy, chemotherapy, and targeted therapy, which are almost never used for those patients in the early stage, and this is linked with higher cost. On the other hand, the early-stage patients tend to undergo surgery, the cost of which is less. This indicated that the high prevalence and diagnosis of disease at advanced stages of disease impose great costs on the patients and the health system. However, a multicenter study in China showed the opposite result in urban areas (15). The possible cause of this discrepancy is that in their study, the cases mainly came from cites with low GDP, where advanced patients are likely to forego expensive treatment due to their low incomes.
Although we attempted to balance stage-specific cases, only 17.5% of all cases were stage I, while 66.4% (27.5% in stage III and 38.9 in stage IV) were late-stage, which reflects the epidemic status of stomach cancer where most detected patients are late stage and there is a lack early diagnosis and treatment. Moreover, both in terms of medical and non-medical expenditures and of financial burden and time loss, late-stage patients paid more. Therefore, early diagnosis through screening and selecting an appropriate treatment method might substantially ameliorate the economic burden of the disease.
In addition, non-medical expenditure for the diagnosis and treatment of stomach cancer constituted a significant component, reaching 8.8% of the overall expenditure (additional meals, 28.5%; transportation, 20.6%; nutrition, 19.7%), which was higher than reported in the previous relevant study in China (only 5.5%) (24). In detail, transportation, nutrition and other non-medical expenditures accounted for 40.3, 17.5, and 42.2%, respectively. Moreover, the non-medical expenditure for late-stage cancer (III and IV) was also higher than that for early-stage cancer (I and II), possibly because patients with late-stage cancer need to go to and from the hospital more times and also need more nutrients.
Concerning financial burden, patients spent 63.8% of their household income for 1 year of stomach cancer diagnosis and treatment, and 79.2% of the families perceived the financial burden as unmanageable. We used the threshold proposed by Xu et al. that financial catastrophe occurs with health care payments at or exceeding 40% of a household's income each year (21); this indicates that the expenditure of our patients was catastrophic. Our result was the same as that of the study by Li et al. (27), which found that out-of-pocket cost per hospitalization accounted for 79% of per capita disposable income in Hua country in 2011. In the United States, in contrast, 25.0% of beneficiaries with the largest burden spent at least 29.9% of their annual income on healthcare (28). This indicated that the economic burden imposed by stomach cancer was relatively high for individual patients' families in China, especially for low-income families.
The loss of time of patients and their families due to the lack of a normal work schedule as a result of illness and treatment, including spending traveling to and from care, waiting for appointments, and so forth, was considered as an indirect economic impact. Time loss therefore represents an essential component of the burden of illness for patients and caregivers. However, few studies have estimated the time costs of patients with stomach cancer. In this study, the average loss of time was estimated at 88.1 days, equaling $996, which is 12.9% of per capita GDP, which crudely converted to a minimum wage loss of $254 in Beijing in 2014. In the USA, data from Surveillance, Epidemiology, and End Results linked to Medicare claims (SEER-Medicare) showed that the mean patient time cost was $5,348 (351.3 days, 12.1% GDP) in initial phase (29). Although the cost is higher than in our study, the proportion of GDP was lower, suggesting that our burden of stomach cancer was heavier. Furthermore, patients with late-stage cancer spent significantly more through time loss than those in the earlystage, not only in patients but also in caregivers. Thus, it is essential to reduce indirect costs through early diagnosis and treatment.
The study had several limitations. First, we only counted the expenditure data within the study hospitals, and it is possible that some patients had received diagnosis and therapy from other hospitals in China, indicating that we probably underestimated the economic burden. Future study needs to overcome this. Second, the retrospective nature of the questionnaire with face-to-face interview may contribute to recall bias. Third, the majority of patients being from specialized hospitals may mean that there is selection bias; nevertheless, considering that most cancer patients prefer to choose and transfer specialized hospitals, the bias can be regarded as tiny.
In conclusion, our study has directive significance in the development of optimal policies of the healthcare system. This study indicated that direct and indirect expenditures for stomach cancer in China were onerous. It is essential that effective measures be taken in order to reduce the financial burden by decreasing the personal payment ratio and increasing the reimbursement ratio. Cancer screening is cost-effective due to the fact that early detection and therapy of stomach cancer can dramatically reduce costs. Studies on the financial burden of stomach cancer in China are still rare, especially multicenter studies, and more research is sorely needed in the future.
All datasets generated for this study are included in the article/Supplementary Material.
The studies involving human participants were reviewed and approved by this survey was approved by the Institutional Review Board of the Cancer Hospital of the Chinese Academy of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
KZ, JY, JS, and MD: study concepts and study design. HH, JY, LW, and LG: data acquisition, analysis, interpretation, and statistical analysis. JY and KZ: manuscript preparation and editing. KZ, HH, JS, and MD: manuscript review. All authors read and approved the final manuscript.
This study was supported by grants from the CAMS Innovation Fund for Medical Sciences (2017-I2M-1-006) and the National Key R&D Program of China (Grant No. 2017YFC0907900).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank all of our colleagues from the Health Economic Evaluation Working Group, Cancer Screening Program in Urban China (CanSPUC).
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00310/full#supplementary-material
1. Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology. (2015) 148:719–31.e3. doi: 10.1053/j.gastro.2015.01.040
2. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. (2015) 136:E359–86. doi: 10.1002/ijc.29210
3. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
4. Izadi A, Sirizi MJ, Esmaeelpour S, Barouni M. Evaluating direct costs of gastric cancer treatment in iran - case study in Kerman City in 2015. Asian Pac J Cancer Prev. (2016) 17:3007–13.
5. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. (2017) 3:524–48. doi: 10.1001/jamaoncol.2016.5688
6. Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. (2009) 27:2758–65. doi: 10.1200/JCO.2008.20.8983
7. Haga K, Matsumoto K, Kitazawa T, Seto K, Fujita S, Hasegawa T. Cost of illness of the stomach cancer in Japan - a time trend and future projections. BMC Health Serv Res. (2013) 13:283. doi: 10.1186/1472-6963-13-283
8. Majidi A, Salimzadeh H, Beiki O, Delavari F, Majidi S, Delavari A, et al. Cancer research priorities and gaps in Iran: the influence of cancer burden on cancer research outputs between 1997 and 2014. Public Health. (2017) 144:42–7. doi: 10.1016/j.puhe.2016.11.002
9. Yabroff KR, Lamont EB, Mariotto A, Warren JL, Topor M, Meekins A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. (2008) 100:630–41. doi: 10.1093/jnci/djn103
10. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. (2017) 109:djw205. doi: 10.1093/jnci/djw205
11. Girgis A, Lambert S, Johnson C, Waller A, Currow D. Physical, psychosocial, relationship, and economic burden of caring for people with cancer: a review. J Oncol Pract. (2013) 9:197–202. doi: 10.1200/JOP.2012.000690
12. Yao F, Shi CL, Liu CC, Wang L, Song SM, Ren JS, et al. [Economic burden of stomach cancer in China during 1996-2015: a systematic review]. Zhonghua Yu Fang Yi Xue Za Zhi. (2017) 51:756–62. doi: 10.3760/cma.j.issn.0253-9624.2017.08.018
13. Shi JF, Shi CL, Yue XP, Huang HY, Wang L, Li J, et al. [Economic burden of cancer in China during 1996-2014: a systematic review]. Zhonghua Zhong Liu Za Zhi. (2016) 38:929–41. doi: 10.3760/cma.j.issn.0253-3766.2016.12.010
14. Sun XJ, Shi JF, Guo LW, Huang HY, Yao NL, Gong JY, et al. Medical expenses of urban Chinese patients with stomach cancer during 2002-2011: a hospital-based multicenter retrospective study. BMC Cancer. (2018) 18:435. doi: 10.1186/s12885-018-4357-y
15. Yang Z, Zeng H, Xia R, Liu Q, Sun K, Zheng R, et al. Annual cost of illness of stomach and esophageal cancer patients in urban and rural areas in China: a multi-center study. Chin J Cancer Res. (2018) 30:439–48. doi: 10.21147/j.issn.1000-9604.2018.04.07
16. Liao XZ, Shi JF, Liu JS, Huang HY, Guo LW, Zhu XY, et al. Medical and non-medical expenditure for breast cancer diagnosis and treatment in China: a multicenter cross-sectional study. Asia Pac J Clin Oncol. (2018) 14:167–78. doi: 10.1111/ajco.12703
17. Huang HY, Shi JF, Guo LW, Bai YN, Liao XZ, Liu GX, et al. Expenditure and financial burden for the diagnosis and treatment of colorectal cancer in China: a hospital-based, multicenter, cross-sectional survey. Chin J Cancer. (2017) 36:41. doi: 10.1186/s40880-017-0209-4
18. Dai M, Shi JF, Li N. Cancer Screening Program in Urban China: the program design and the expectancies. Chin J Prev Med. (2013) 47:179–82. doi: 10.3760/cma.j.issn.0253-9624.2013.02.018
19. UICC International Union Against Cancer. TNM Classification of Malignant Tumors. 7th ed. Berlin; Heidelberg; New York, NY; London; Paris; Tokyo: Springer-Verlag (2009).
20. National Bureau of Statistics of China. China Statistical Yearbook, 2015 Available online at: http://www.stats.gov.cn/tjsj/ndsj/2015/indexch.htm (accessed June 5, 2016).
21. Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff. (2007) 26:972–83. doi: 10.1377/hlthaff.26.4.972
22. Cai Y, Xue M, Chen W, Hu M, Miao Z, Lan L, et al. Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. (2017) 29:253–62. doi: 10.21147/j.issn.1000-9604.2017.03.11
23. Zhao T, Cheng J, Chai J, Feng R, Liang H, Shen X, et al. Inpatient care burden due to cancers in Anhui, China: a cross-sectional household survey. BMC Public Health. (2016) 16:308. doi: 10.1186/s12889-016-2995-z
24. Xu W, Shi W, Chen P. Analysis of economic burden of malignant tumor in-patients in Xinjiang. Disease Surveill. (2006) 21:38–40. doi: 10.3784/j.issn.1003-9961.2006.01.016
25. Li TY, Hsieh JS, Lee KT, Hou MF, Wu CL, Kao HY, et al. Cost trend analysis of initial cancer treatment in Taiwan. PLoS ONE. (2014) 9:e108432. doi: 10.1371/journal.pone.0108432
26. Kim SY, Kim SG, Park JH, Park EC. [Costs of initial cancer care and its affecting factors]. J Prev Med Public Health. (2009) 42:243–50. doi: 10.3961/jpmph.2009.42.4.243
27. Li X, Cai H, Wang C, Guo C, He Z, Ke Y. Economic burden of gastrointestinal cancer under the protection of the New Rural Cooperative Medical Scheme in a region of rural China with high incidence of oesophageal cancer: cross-sectional survey. Trop Med Int Health. (2016) 21:907–16. doi: 10.1111/tmi.12715
28. Neuman P, Cubanski J, Desmond KA, Rice TH. How much 'skin in the game' do medicare beneficiaries have? The increasing financial burden of health care spending, 1997-2003. Health Aff. (2007) 26:1692–701. doi: 10.1377/hlthaff.26.6.1692
Keywords: stomach cancer, direct expenditure, indirect expenditure, financial burden, medical expenditure, non-medical expenditure
Citation: Zhang K, Yin J, Huang H, Wang L, Guo L, Shi J and Dai M (2020) Expenditure and Financial Burden for Stomach Cancer Diagnosis and Treatment in China: A Multicenter Study. Front. Public Health 8:310. doi: 10.3389/fpubh.2020.00310
Received: 06 December 2019; Accepted: 08 June 2020;
Published: 07 August 2020.
Edited by:
Nemanja Rancic, Faculty of Medicine, Military Medical Academy, SerbiaReviewed by:
Tanja Pekez, Private Practitioner, Kutina, CroatiaCopyright © 2020 Zhang, Yin, Huang, Wang, Guo, Shi and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai Zhang, a2FpODc5NjhAc2luYS5jb20=; Min Dai, ZGFpbWluMjAwMkBob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.