- 1Independent Researcher, Ormond Beach, FL, United States
- 2Auckland University of Technology, Auckland, New Zealand
The previously described overfat pandemic, estimated to be 62–76% worldwide, is comprised of individuals with excess body fat sufficient to impair health. The overfat condition is common in those who are overweight and obese, and can also occur in significant numbers of normal-weight non-obese individuals. Being overfat increases the risk for a wide spectrum of common cardiovascular and metabolic (cardiometabolic) abnormalities, chronic diseases and physical impairment. In some ethnicities, up to 40% or more of those who are normal-weight and non-obese may be overfat, a figure twice that used in the original global overfat estimates. In addition to the rates of overfat outpacing overweight and obesity, non-White populations outnumber Whites 6:1, with the recently estimated overfat prevalence being low when considering ethnicities such as Asians, Chinese, Africans and Latin Americans, including these individuals living among predominantly White populations. An awareness of the extent of the overfat pandemic is important because excess body fat can precede cardiometabolic risk factors, chronic diseases, and physical disabilities, and can reduce quality of life and increase healthcare expenditure. The purpose of this Perspective is to demonstrate that the global overfat prevalence of 62–76% may be considerably underestimated.
Introduction
The term overfat was defined as excess body fat that impairs health (1). The problem can occur in those who are overweight, obese, and include significant numbers of normal-weight non-obese individuals (2, 3). Excess body fat can contribute to cardiovascular and metabolic (cardiometabolic) health impairment including various risk factors such as abnormal blood glucose, high-density lipoprotein cholesterol (HDL), triglycerides and blood pressure, and progress to a variety of diseases including type 2 diabetes, non-alcoholic fatty liver, cancers, Alzheimer's and cardiovascular diseases (4–6), including physical impairments (7). As such, the overfat pandemic has created a major global economic burden (8, 9).
As a subcategory of overfat, measured by waist circumference, the prevalence of abdominal obesity, which poses a greater cardiometabolic risk than excess fat elsewhere in the body, is increasing dramatically worldwide (10–12). The increasing number of people who are normal-weight and non-obese but overfat was first described by Ruderman et al. (2) as metabolically-obese, normal weight individuals (2, 13), with the overfat prevalence in this population estimated at ~20%. More recently, Gujral et al., referred to the problem as metabolic abnormality but normal weight (MAN), showing a wide variety in the overfat prevalence between various ethnicities, with excess body fat in normal-weight non-obese individuals exceeding 40% in some ethnic groups (3). In a US population, MAN was defined as a BMI of 18.5 to 24.9 kg/m2 for White, African American, and Hispanics or a BMI of 18.5 to 22.9 kg/m2 for South Asian and Chinese Americans, along with ≥2 cardiometabolic abnormalities.
As a surrogate measure of body fat, the body mass index (BMI) can misclassify many individuals who are normal-weight and non-obese, but overfat, and therefore miss an opportunity to prevent or treat excess body fat and its associated cardiometabolic and physical impairments. (14, 15). In the U.S., data shows that a high percent body fat can exist even in lower BMI categories (16). One reason is ethnicity, where a BMI cut point of 30 kg/m2 in Whites is equivalent to lower BMI levels for other ethnicities including South Asians, Chinese Americans, and African Americans with cardiometabolic impairment (3, 17, 18). BMI fails to consider whole body fat distribution, in particular abdominal fat, which is associated with excess around the heart, liver and kidneys, that can be more pathogenic than general obesity (19). While BMI is a screening tool for overweight and obesity, it has limitations. Many researchers and clinicians regularly use it, with continued recommendations made by healthcare organizations such as the U.S. Preventive Services Task Force (20).
Instead of BMI, the waist-to-height ratio (WHtR), an indirect measure of body fat, is more strongly related to excess body fat and cardiometabolic impairment, and is an easier measurement to obtain (21, 22). Epidemiologic studies demonstrate that increased abdominal fat assessed through WHtR can predict adiposity-related risk, although, like BMI, it does not accurately estimate body fat percentage (15). WHtR may be the most convenient, inexpensive, and valuable clinical indicator of health and overfat risk for use in all ethnic groups of adults and children, with a simple recommendation that the waist should be less than half of a person's height (15, 22–25). Unfortunately, the various methods for measuring body fat, including bioelectrical impedance, dual-energy X-ray absorptiometry (DXA), waist and WHtR, BMI, and others, makes comparison across studies difficult, contributing to the difficulty of estimating overfat prevalence.
The overfat condition can have an inverse relationship with physical activity, as increased body fat can develop despite increased rates of exercise (26). This paradox appears to include the general population, and is also evident in athletes (27, 28) and the military (29).
Global populations share a common risk factor—the increased consumption of processed carbohydrates, especially sugar, which may be the largest contributing lifestyle factor to the overfat pandemic (30). Sugar-sweetened beverages are the single largest source of added sugar and the top source of energy intake in the U.S. diet (31–33). However, their increased consumption in developing nations is significant too (34), with sugar-sweetened beverages strongly associated with chronic illness (35). In India, for example, annual sugar sweetened beverage consumption increased from 2 L per capita in 2000 to over 11 liters per capita in 2013 (36, 37).
While the global overfat prevalence was previously estimated to between 62 and 76%, this may have been considerably underestimated due to a number of factors discussed in this perspective.
Rising Rates of Overfat
Since the first estimation of global overfat prevalence was written in 2016 (published in 2017) (1, 38), a number of factors appear to indicate this estimation is low. In addition to emerging evidence regarding overfat outpacing overweight and obesity noted above, it includes the significantly higher percentage of normal-weight non-obese non-White overfat populations, especially in the two most populated regions, South Asia and China.
Ethnicities
While studies demonstrating ethnic differences in body fat content with differences in BMI cut-offs have appeared for some time (reviewed by Shah (18), a growing consensus shows there is a much higher rate of excess body fat in normal-weight non-obese non-White individuals. Compared with Whites, Asians, Hispanics, and Blacks may have a significantly higher overfat prevalence, which is not explained by factors such as demographics and behavior (3). These studies help confirm previous works that a BMI cut point of 30 kg/m2 in Whites was equivalent to lower BMI cut points for South Asians, Chinese, Blacks, and Aboriginal Canadians in terms of body fat, cardiometabolic impairment and chronic disease (17, 18, 39, 40).
Reasons for such significant growth of overfat populations in developing areas could be multifactorial, including genetics and lifestyle. The adiposity rebound is a condition of low weight and thinness at 1 to 2 years of age, often accompanied by low birth weights, developing into excess body fat and impaired glucose tolerance and diabetes in adulthood (41), a phenomenon also demonstrated in individuals growing up in post-World War II Finland (42). The nutritional transition occurring in developing populations in Asia and Africa may also have impacted the overfat prevalence. As the second most primarily non-White populated continent behind Asia's 4.5 billion people, Africa's population of 1.2 billion also shares a growing common cardiometabolic risk factor: overfat.
While non-Whites outnumber Whites significantly worldwide by ~6:1, in many developed nations that are primarily White, there are also modest numbers of other ethnicities at high risk of being overfat. For example, in a U.S. population, Gujral et al. (3) showed that, like their counterparts in developing countries, significantly higher percentages of normal-weight non-obese overfat individuals occurs in Asians, Hispanics and Blacks compared to Whites (see Table 1). This trend was also previously shown in South Asians who move to Western countries (43). The United Nations estimates that there are over 370 million aboriginal, native or indigenous people worldwide.
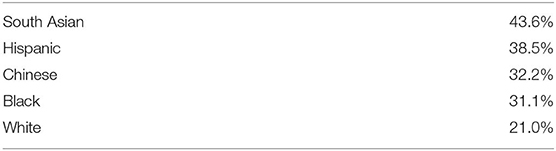
Table 1. Percentage of combined cardiometabolic abnormalities and excess body fat in normal-weight non-obese mixed U.S. population [from Gujral et al. (3)].
South Asia
India, Pakistan, Bangladesh, Bhutan and other South Asian countries have a significant and increasing prevalence of excess body fat, cardiometabolic impairment, and high burden of disease associated with insulin resistance and diabetes, hypertension, hypertriglyceremia and low serum levels of high density lipoprotein (HDL) (44, 45). For the same BMI, body fat is 7–8% higher for Indians compared to Whites (46). South Asia also has a population of ~1.92 billion people, with the highest percentage of overfat individuals in the normal-weight non-obese category, recently estimated at 44 and 41% (3, 47).
China
China was considered the largest overweight population in the world in 2014 with about 26% of adults representing about 364 million people (48). However, a recent study showed the prevalence of overfat Chinese adolescents from bioelectrical impedance to be 36% in girls and 24% in boys (49). These overfat adolescents can become overfat adults with increased risk of chronic disease and physical impairment (50). In adults, the age-adjusted prevalence of abdominal obesity measured by waist circumference was 52% in men and 35% in women in 2011, increasing dramatically from 17 to 39% between 1997 and 2009 (51, 52). Like other developing nations, China's leading cause of death is now chronic disease, particularly cardiometabolic impairment, having surpassed infectious diseases (53). Hypertension, for example, is not uncommon; using the recent definition of hypertension being blood pressure >130/80 mm Hg would estimate that 267 million Chinese in the 45–75 age group would be hypertensive (54). Over a 5-year period between 2002 and 2007, the prevalence of one or more cardiometabolic abnormalities in normoweight Taiwanese people (39% male) 16 to 45 y significantly increased from ~30 to ~40% (55).
The Continuing Overfat Trend
In addition to the increasing prevalence of overfat populations in Asia and Africa, developed nations continue leading the way. In the US, for example, between 2013 and 2016 the estimated overfat prevalence in adults increased from 87% (38, 56) to 91% with the estimated prevalence of overfat U.S. children increasing from 52 to 69% (26, 57). In addition, developed populations have modest numbers of non-Whites with significant numbers of normal-weight non-obese ethnicities who are overfat (Table 1).
Considering these factors, especially higher percentages of overfat in normal-weight non-obese non-White populations, overfat rates may be outpacing more modest increases in overweight and obesity (56–58).
Discussion
The next generation of obesity research may focus less on overweight and obesity and more on body fat, as the latter is more relevant to the development of cardiometabolic risk factors, chronic disease, and physical impairment; all significant sources of rising healthcare costs in both developed and developing nations. Rather than relying on BMI, measurements of body fat through direct or indirect methods, such as DXA or WHtR, respectively, can provide valuable data for researchers and clinicians. For home use, WHtR is a simple and accurate method for individuals to help manage health.
Previous estimates of global overfat prevalence were primarily based on overweight and obesity rates, plus ~20% of normal-weight non-obese individuals. As updated research reveals significant overfat conditions in non-White ethnicities at lower BMI ranges, especially in large populated areas such as Asia and Africa, and considering that the world population of non-Whites is about six times greater than Whites (see Table 2), the recent global overfat prevalence of between 62 and 76% may have been significantly underestimated.
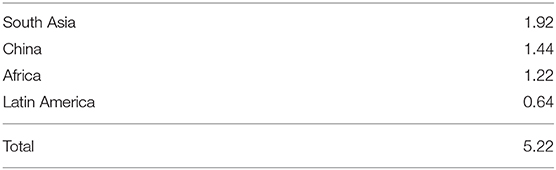
Table 2. Estimated non-white populations in billions in selected regions of the world (Global population of whites account for <1 billion; estimated world population of 7.7 billion).
Estimating the number of overfat people in the world is important because excess body fat can significantly affect quality of life, precede chronic disease and physical disability, and dramatically increase healthcare expenditure. A variety of lifestyle issues, including dietary, environmental, exercise, stress, along with epigenetic factors, must be considered in the assessment, treatment and prevention of this condition.
Even defined within the discussion of this paper, there is further risk of missing many people who are in the early stages of being overfat as they may not have obvious disease risk, i.e., one cardiometabolic risk factor. This is another missed opportunity for prevention, best implemented sooner rather than waiting for more obvious excess fat or additional cardiometabolic impairment. As such, a modified definition of overfat was previously presented and emphasized here: excess adiposity indicted by direct (DXA) or indirect (WHtR) measures combined with at least one additional measurable risk factor of impaired cardiometabolic or physical health (26). Universal public health guidelines addressing the overfat pandemic will require far more emphasis on reducing the consumption of refined carbohydrates, including added sugars (25), with taxation being one effective intervention (59).
As important as making overfat estimations, both public health officials and clinicians worldwide have sufficient, cost-effective assessment and treatment tools available to reverse this preventable condition, and the overfat pandemic.
Conclusion
Case definitions for overweight and obesity have long been developed and researched, with the awareness that excess body fat poses significant health risks to all individuals. As previously described, excess body fat that impairs health is defined as overfat. The total prevalence of overfat equals those who are overweight, plus those who are obese, plus normal-weight non-obese individuals with excess body fat. Future studies associated with overweight and obesity should also consider the overfat condition.
Determining the global overfat prevalence is not the purpose of this paper, but is instead to demonstrate that the recent estimation of 62–76% may have been significantly underestimated. This makes the overfat pandemic a serious condition requiring interventions to address the problem by governments, healthcare agencies and clinicians, including education of the public.
Author Contributions
PM wrote the initial manuscript. PL reviewed and edited the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat and underfat: new terms and definitions long overdue. Front Public Health. (2016) 4:279. doi: 10.3389/fpubh.2016.00279
2. Ruderman NB, Schneider SH, Berchtold P. The “metabolically-obese,” normal-weight individual. Am J Clin Nutr. (1981) 34:1617–21. doi: 10.1093/ajcn/34.8.1617
3. Gujral UP, Vittinghoff E, Mongraw-Chaffin M, Vaidya D, Kandula NR, Allison M, et al. Cardiometabolic abnormalities among normal-weight persons from five racial/ethnic groups in the United States: a cross-sectional analysis of two cohort studies. Ann Intern Med. (2017) 166:628–36. doi: 10.7326/M16-1895
4. Magnussen CG, Smith KJ. Pediatric blood pressure and adult preclinical markers of cardiovascular disease. Clin Med Insights Blood Disord. (2016) 9:1–8. doi: 10.4137/CMBD.S18887
5. Scappaticcio L, Maiorino MI, Bellastella G, Giugliano D, Esposito K. Insights into the relationships between diabetes, prediabetes, and cancer. Endocrine. (2017) 56:231–9. doi: 10.1007/s12020-016-1216-y
6. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K, et al. Body fatness and cancer–viewpoint of the IARC working group. N Engl J Med. (2016) 375:794–8. doi: 10.1056/NEJMsr1606602
7. Lean ME, Han TS, Seidell JC. Impairment of health and quality of life in people with large waist circumference. Lancet. (1998) 351:853–6. doi: 10.1016/S0140-6736(97)10004-6
8. Martin AB, Hartman M, Whittle L, Catlin A, National Health Expenditure Accounts T. National health spending in 2012: rate of health spending growth remained low for the fourth consecutive year. Health Aff . (2014) 33:67–77. doi: 10.1377/hlthaff.2013.1254
9. Chen Y, Peng Q, Yang Y, Zheng S, Wang Y, Lu W. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: a repeated cross-sectional study. BMC Public Health. (2019) 19:1293. doi: 10.1186/s12889-019-7633-0
10. Ford ES, Maynard LM, Li C. Trends in mean waist circumference and abdominal obesity among US adults, 1999-2012. JAMA. (2014) 312:1151–3. doi: 10.1001/jama.2014.8362
11. Yoo S, Cho HJ, Khang YH. General and abdominal obesity in South Korea, 1998–2007: gender and socioeconomic differences. Prev Med. (2010) 51:460–5. doi: 10.1016/j.ypmed.2010.10.004
12. Lilja M, Eliasson M, Stegmayr B, Olsson T, Soderberg S. Trends in obesity and its distribution: data from the Northern Sweden MONICA survey, 1986–2004. Obesity. (2008) 16:1120–8. doi: 10.1038/oby.2008.8
13. Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S. The metabolically obese, normal-weight individual revisited. Diabetes. (1998) 47:699–713. doi: 10.2337/diabetes.47.5.699
14. Tomiyama AJ, Hunger JM, Nguyen-Cuu J, Wells C. Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005-2012. Int J Obes. (2016) 40:883–6. doi: 10.1038/ijo.2016.17
15. Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F. The concept of normal weight obesity. Prog Cardiovasc Dis. (2014) 56:426–33. doi: 10.1016/j.pcad.2013.10.003
16. St-Onge MP. Are normal-weight Americans over-fat? Obesity. (2010) 18:2067–8. doi: 10.1038/oby.2010.103
17. Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV. Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care. (2011) 34:1741–8. doi: 10.2337/dc10-2300
18. Shah AD, Kandula NR, Lin F, Allison MA, Carr J, Herrington D, et al. Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes. (2016) 40:639–45. doi: 10.1038/ijo.2015.219
19. Bener A, Yousafzai MT, Darwish S, Al-Hamaq AO, Nasralla EA, Abdul-Ghani M. Obesity index that better predict metabolic syndrome: body mass index, waist circumference, waist hip ratio, or waist height ratio. J Obes. (2013) 2013:269038. doi: 10.1155/2013/269038
20. Siu AL, Force USPST. Screening for abnormal blood glucose and type 2 diabetes mellitus: U.S. Preventive services task force recommendation statement. Ann Intern Med. (2015) 163:861–8. doi: 10.7326/M15-2345
21. Zhu S, Heo M, Plankey M, Faith MS, Allison DB. Associations of body mass index and anthropometric indicators of fat mass and fat free mass with all-cause mortality among women in the first and second National Health and Nutrition Examination Surveys follow-up studies. Ann Epidemiol. (2003) 13:286–93. doi: 10.1016/S1047-2797(02)00417-9
22. Hetherington-Rauth M, Bea JW, Lee VR, Blew RM, Funk J, Lohman TG, et al. Comparison of direct measures of adiposity with indirect measures for assessing cardiometabolic risk factors in preadolescent girls. Nutr J. (2017) 16:15. doi: 10.1186/s12937-017-0236-7
23. Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. (2005) 56:303–7. doi: 10.1080/09637480500195066
24. Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord. (2000) 24:1453–8. doi: 10.1038/sj.ijo.0801401
25. Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. (2010) 91:1020–6. doi: 10.3945/ajcn.2009.28589
26. Maffetone PB, Laursen PB. The prevalence of overfat adults and children in the US. Front Public Health. (2017) 5:290. doi: 10.3389/fpubh.2017.00290
27. Klungland Torstveit M, Sundgot-Borgen J. Are under- and overweight female elite athletes thin and fat? A controlled study. Med Sci Sports Exerc. (2012) 44:949–57. doi: 10.1249/MSS.0b013e31823fe4ef
28. Yamamoto JB, Yamamoto BE, Yamamoto PP, Yamamoto LG. Epidemiology of college athlete sizes, 1950s to current. Res Sports Med. (2008) 16:111–27. doi: 10.1080/15438620802103320
29. Hruby A, Bulathsinhala L, McKinnon CJ, Hill OT, Montain SJ, Young AJ, et al. Body mass index at accession and incident cardiometabolic risk factors in US army soldiers, 2001–2011. PLoS ONE. (2017) 12:e0170144. doi: 10.1371/journal.pone.0170144
30. Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. (2013) 14:606–19. doi: 10.1111/obr.12040
31. de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. (2012) 367:1397–406. doi: 10.1056/NEJMoa1203034
32. Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. (2012) 367:1407–16. doi: 10.1056/NEJMoa1203388
33. Maersk M, Belza A, Stodkilde-Jorgensen H, Ringgaard S, Chabanova E, Thomsen H, et al. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr. (2012) 95:283–9. doi: 10.3945/ajcn.111.022533
34. Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med. (2012) 367:1387–96. doi: 10.1056/NEJMoa1203039
35. Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. (2010) 121:1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185
36. Gulati S, Misra A. Sugar intake, obesity, and diabetes in India. Nutrients. (2014) 6:5955–74. doi: 10.3390/nu6125955
37. Basu S, Vellakkal S, Agrawal S, Stuckler D, Popkin B, Ebrahim S. Averting obesity and type 2 diabetes in India through sugar-sweetened beverage taxation: an economic-epidemiologic modeling study. PLoS Med. (2014) 11:e1001582. doi: 10.1371/journal.pmed.1001582
38. Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat adults and children in developed countries: the public health importance of identifying excess body fat. Front Public Health. (2017) 5:190. doi: 10.3389/fpubh.2017.00190
39. Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. (2007) 115:2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011
40. Bhopal RS. A four-stage model explaining the higher risk of Type 2 diabetes mellitus in South Asians compared with European populations. Diabet Med. (2013) 30:35–42. doi: 10.1111/dme.12016
41. Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. (2004) 350:865–75. doi: 10.1056/NEJMoa035698
42. Eriksson JG, Forsen T, Tuomilehto J, Osmond C, Barker DJ. Early adiposity rebound in childhood and risk of Type 2 diabetes in adult life. Diabetologia. (2003) 46:190–4. doi: 10.1007/s00125-002-1012-5
43. McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. (1991) 337:382–6. doi: 10.1016/0140-6736(91)91164-P
44. Enas EA, Singh V, Munjal YP, Gupta R, Patel KC, Bhandari S, et al. Recommendations of the second Indo-U.S. health summit on prevention and control of cardiovascular disease among Asian Indians. Indian Heart J. (2009) 61:265−74.
45. Hiremath S, Vala DR, Roy T, Khera P, Kaul U. Changing patterns in the prevalence and management of cardiovascular risk factors in India and their comparison with the rest of the world along with clinical outcomes at 5-year: an analysis of stable coronary artery disease patients from The Prospective Observational Longitudinal Registry of patients with stable coronary artery disease (CLARIFY) registry. Indian Heart J. (2018) 70 (Suppl. 3):S36–42. doi: 10.1016/j.ihj.2018.04.003
46. Jackson AS, Ellis KJ, McFarlin BK, Sailors MH, Bray MS. Body mass index bias in defining obesity of diverse young adults: the Training Intervention and Genetics of Exercise Response (TIGER) study. Br J Nutr. (2009) 102:1084–90. doi: 10.1017/S0007114509325738
47. Maffetone PB. The overfat pandemic in India. Glob Epidemic Obes. (2018) 6:1–7. doi: 10.7243/2052-5966-6-2
48. Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. (2016) 387:1377–96. doi: 10.1016/S0140-6736(16)30054-X
49. Chen Y, Zhang Y, Wang L. Low diagnostic accuracy of body mass index-based and waist circumference-based references of childhood overweight and obesity in identifying overfat among chinese children and adolescents. Biomed Res Int. (2018) 2018:4570706. doi: 10.1155/2018/4570706
50. Krassas GE, Tzotzas T. Do obese children become obese adults: childhood predictors of adult disease. Pediatr Endocrinol Rev. (2004) 1(Suppl. 3):455−9.
51. Qian X, Su C, Zhang B, Qin G, Wang H, Wu Z. Changes in distributions of waist circumference, waist-to-hip ratio and waist-to-height ratio over an 18-year period among Chinese adults: a longitudinal study using quantile regression. BMC Public Health. (2019) 19:700. doi: 10.1186/s12889-019-6927-6
52. Du P, Wang HJ, Zhang B, Qi SF, Mi YJ, Liu DW, et al. Prevalence of abdominal obesity among Chinese adults in 2011. J Epidemiol. (2017) 27:282–6. doi: 10.1016/j.je.2017.03.001
53. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
54. Bakris G, Ali W, Parati G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J Am Coll Cardiol. (2019) 73:3018–26. doi: 10.1016/j.jacc.2019.03.507
55. Bintoro BS, Fan YC, Chou CC, Chien KL, Bai CH. Metabolic unhealthiness increases the likelihood of having metabolic syndrome components in normoweight young adults. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16183258
56. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013:a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
57. CDC. Disability and Risk Factors: Obesity and Overweight. Centers for disease control and prevention (2016). Available online at: https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
58. (NCHS) NCfHS. Health, United States: With Special Feature on Racial and Ethnic Disparities. Hyattsville, MD: Centers for Disease Control (2016). Available online: https://www.cdc.gov/nchs/data/hus/hus15.pdf
Keywords: overweight, obesity, cardiometabolic, chronic disease, healthcare costs
Citation: Maffetone PB and Laursen PB (2020) Revisiting the Global Overfat Pandemic. Front. Public Health 8:51. doi: 10.3389/fpubh.2020.00051
Received: 22 October 2019; Accepted: 11 February 2020;
Published: 25 February 2020.
Edited by:
Allen C. Meadors, Independent Researcher, Seven Lakes, NC, United StatesReviewed by:
Cherry Maynor Beasley, University of North Carolina at Pembroke, United StatesDiane D. Stadler, Oregon Health & Science University, United States
Timothy Lynn Taylor, Independent Researcher, Welton, United States
Copyright © 2020 Maffetone and Laursen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip B. Maffetone, cGhpbG1hZmZldG9uZUBnbWFpbC5jb20=
 Philip B. Maffetone
Philip B. Maffetone Paul B. Laursen
Paul B. Laursen