- 1Department of Family Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, United States
- 2Department of Family Medicine, University of California Los Angeles (UCLA), Los Angeles, CA, United States
- 3School of Nursing, Charles R. Drew University of Medicine and Science, Los Angeles, CA, United States
Background: While financial difficulties correlate with mental and physical health status, less is known about these associations among economically disadvantaged African-American (AA) older adults.
Objective: This study explored mental and physical health correlates of financial difficulties among AA older adults in low-income areas of south Los Angeles.
Methods: A cross-sectional study on 740 AA older adults (age ≥ 55 years) conducted in South Los Angeles between 2015 and 2018. Independent variable was financial difficulties. Outcomes were depressive symptoms, chronic pain, chronic medical conditions, self-reported health, and sick days. Age, gender, educational attainment, living alone, marital status, smoking, and drinking were also measured. Zero order (unadjusted) and partial (adjusted) correlates of financial difficulties were calculated for data analysis. Adjusted (partial) bivariate correlations controlled for age, gender, education, marital status, living alone, and health insurance.
Results: In adjusted analyses, financial difficulties were positively associated with chronic pain, chronic medical conditions, self-rated health, sick days, and depressive symptoms.
Conclusion: Financial difficulties seem to be linked to chronic pain, chronic medical conditions, self-rated health, sick days, and depressive symptoms. The results advocate for evaluation of social determinants of health in providing health care of AA older adults. Addressing financial difficulties may help with the health promotion of low-income AA older adults in urban areas.
Introduction
Socioeconomic as well as racial/ethnic disparities are widely acknowledged in the United States. The median household income of Whites in the United States is $65,041 compared to the median income of African American (AA) households at $39,490 (1). Furthermore, 22% of the AA population live below the poverty line compared to 11% of Whites. (1). Additionally, AA populations suffer disproportionately from health issues such as chronic medical conditions (CMCs) and chronic pain (2–5). While research has measured the relationship between financial difficulties and a variety of individual health outcomes (6–8), there is still much to be understood about the role of financial difficulties in the mental and physical health of older adults and racial/ethnic minority populations. Considering the economic and health disparities facing AA populations, it is crucial to understand how a variety of health outcomes relate to experiences of financial difficulties in AA populations. The current study seeks to add to the literature by exploring multiple mental and physical health correlates of financial difficulties in older AA adults, while controlling for relevant demographic and social factors.
Mental and Physical Correlates of Financial Difficulties
For certain health behaviors, such as drinking alcohol, financial difficulties appear to be associated with increased risk. A meta-analysis and systematic review of the literature reveals that debt is related to an increased odds of problem drinking (8). Additionally, research indicates chronic financial difficulties have a direct positive effect on drinking as a coping mechanism, which in turn has a direct effect on alcohol consumption and alcohol-related problems, such as binge drinking (8, 9). Furthermore, this research found that the relationship between drinking to cope was more strongly associated with alcohol consumption and related problems for AAs compared to non-AAs (9). Research among the elderly has found that although greater health problems are related to abstinence from alcohol, financial difficulties have the opposite effect, increasing odds of alcohol use among older adults (10).
A systematic review of the literature by Richardson and colleagues revealed a number of findings indicating a relationship between financial concerns and the likelihood to smoke (8). Recent findings indicate financial difficulties increase the risk of tobacco/nicotine use, and this relationship is especially strong for AA populations (11). Furthermore, financial difficulties can influence smoking cessation such that pre-quit financial difficulties are associated with more severe withdrawal symptoms which in turn reduces the likelihood of smoking abstinence (12, 13). Overall, the research indicates smoking is likely associated with financial difficulties in a way that may be especially strong for AA samples and therefore this health behavior is included in our current model of determinants.
Depressive symptoms have also been associated with financial difficulties, which can vary by race/ethnicity (14). A meta-analysis of the literature revealed more severe debt is associated with increased odds of depression (8). Furthermore, research specifically on AA populations has also found financial difficulties are associated with greater depressive symptoms (15, 16). Financial difficulties are more strongly related to major depressive episodes for AA adults rather than Whites (14). Furthermore, there may be an increased risk for older adults, considering research demonstrating disparities in depression across SES levels seems to widen across the lifespan, indicating an increased risk of low-income older adults to develop symptoms (17). Therefore, it is imperative that we include depressive symptoms as a correlate of financial difficulties in our sample of older AA adults.
Physical health may be measured through a variety of variables including chronic pain, CMCs, self-rated health (SRH), and sick days. Each of these health factors may be important correlates of financial difficulties within an older AA adult sample.
Chronic pain has been associated with financial difficulties in a variety of studies. Greater disability and distress from chronic pain is associated with living in low socioeconomic areas (18). Research has also demonstrated that greater severity and disability due to pain (19, 20) as well as greater risk of chronic pain following injuries (21) are related to low income levels. The incidence of chronic pain is also associated with financial difficulties (22). Demonstrating the relationship between SES and chronic pain, Dorner et al. found evidence that individuals in low SES groups, determined by measures including income, felt two to three times more disabled by the same level of severity of pain than those in the highest SES group (19).
In addition to chronic pain, it appears financial difficulties and CMCs may be related as well. In AA samples, financial difficulties have been linked to the increased risk of diagnosis of certain CMCs, such as Type 2 diabetes (23). Additionally, a study of older women found that those reporting financial difficulties were about 60% more likely to die within the next 5 years (24). Not only do financial difficulties predict morbidity and mortality, but CMCs can in turn also increase risk of financial difficulties, as research on those affected by cancer showed that about a third of participants lost all or most of their savings (25).
In terms of SRH, a study of older adults showed poorer SRH was related to living in a neighborhood with a higher proportion of people below the poverty line, regardless of race/ethnicity (26). Studies of AA samples and low-income samples have also found financial difficulties are associated with poorer SRH (27, 28). Furthermore, in older adults, poor SRH can increase the likelihood of future financial strain (29).
Research has also indicated a relationship between financial difficulties and work absenteeism (30). Considerable research has indicated sick days as related to stressors, such as experiencing financial difficulties for both women (31) and men (32). Research has suggested that financial strain may mediate the link between depression and sick days (33). Based on this literature, chronic pain, CMCs, SRH, and sick days may all be important health indicators related to financial difficulties. The current study explores the relationship between financial difficulties and a variety of demographic, social, behavioral, and health factors, as well as specifically examines the mental and physical health correlates of financial difficulties in older AA adults living in low-income areas of south Los Angeles.
Demographic, Social, and Behavioral Factors
Gender, like race/ethnicity, is another factor related to gaps in financial difficulties. In 2016, the female-to-male earnings ratio in the United States was 80.5%, and the median income for men was $51,640 compared to women at $41,554 (1). Furthermore, gender and financial difficulties may have a stronger relationship among AA populations. Recent data from the U.S. Census Bureau indicates 55% of AA children are in single-parent households, with the vast majority being led by single mothers (34). Data on AA single-mother households shows 43% were below the poverty line in 2012, compared to 22% of AA single-father households and 9% of married family households of any race/ethnicity (34). In recent decades, older African Americans, especially women, have emerged as custodial parents to their grandchildren, leading to worsening of health, social, and financial status and threatening their well-being (35, 36). Adding parental responsibilities in the later age can lead to added costs and burdens, especially if the child has chronic health issues (37) or if there is only one caregiving grandparent (38). Thus, in this study it is imperative to control for this factor when examining the relationship between mental and physical health factors and financial difficulties.
Age may also be related to financial difficulties in a variety of ways. Research indicates that especially for older AA women, financial difficulties predict mortality (24). Age can increase risk of health issues, such as cancer, which can also lead to increased financial difficulties (25). Additionally financial difficulties, such as health expenditures, can accumulate over the life-course, taking a toll on those at older ages (7). Furthermore, financial exploitation of older adults can be a common problem and being AA or residing in high-poverty areas places certain older adults at increased risk (6). Overall, age and gender appear to play a role in the risk for and consequences of financial difficulties, especially for AA populations, and therefore it is imperative to include these factors in our model and control for this demographic factor in our adjusted analysis.
Similar to the disparities in other SES indicators, educational attainment varies by race/ethnicity, which may be largely impacted by financial difficulties. While family assets positively impact the chances of college graduation for AA and White students, family debt is more detrimental to AA students likelihood of graduating than White students (39). Research from a national sample of low- and middle-income households found that, for AA students, the odds of student loan indebtedness is twice as high as it is for White students, and this disparity persists even after accounting for degree completion and other SES factors (40). The financial burdens of education are greater for AA students and their college attendance is significantly lower (41). Even though education is typically associated with increases in SES, recent research found that educational attainment is associated with increases in future income and emotional well-being for Whites but not AAs (42). Therefore, there is more to be parsed concerning the role of educational attainment in reducing financial difficulties in AA samples.
Data from the U.S. Census Bureau indicates an upward trend in living alone, especially among older adults, with 36.1% of women and 18.9% of men living alone over the age of 65 (34). While there appears to be much research indicating the link between living alone and psychological distress (43–45), our review of the literature indicates a gap in research on living alone and financial difficulties in the U.S., especially for older adults or racial/ethnic minorities (46, 47). Those who live alone may have sufficient income to support themselves, negating the need to live with others, or conversely those who live with others may be able to afford a higher standard of living than those living alone through combined income and resources. Given conflicting past research and current data, the current study aims to control for this potential confounding variable.
Marital status, on the other hand, has more often been studied in relation to financial difficulties. Living with a spouse is associated with decreased risk of financial exploitation for older adults (6). Even though research from a nationally representative sample indicates married people are less likely to declare bankruptcy than divorced or separated people, never-married people were the least likely (48). While marital status may be protective against some forms of financial stress, financial difficulties can also take a toll on relationship quality and increase risk of divorce (49). Among AA samples, couples who experience financial difficulties are less likely to act supportively toward their partners (50) and are at higher risk for decreased effective communication, relationship satisfaction, and relationship confidence (51). Considering the bidirectional relationship between marriage and financial difficulties, marital status should be included and controlled for in any study on mental and physical health correlates of financial difficulties.
Aim
This study explored the relationship between financial difficulties and mental and physical health factors for this high-risk sample. The above literature review on mental and physical health as well as demographic, social, and behavioral correlates of financial difficulties was mainly derived from research performed in general population. We sought to extend this literature by exploring correlates of financial difficulties in economically disadvantaged older AA adults who have heightened risk for financial difficulties and health issues. In our analysis, we controlled for demographic and social factors.
Methods
Institutional Review Board (IRB)
Charles R. Drew University of Medicine and Science (CDU) Institutional Review Board (IRB) approved the study protocol. All participants signed a written informed consent prior to their enrollment and received financial incentive.
Data Source
Between 2015 and 2018, a cross-sectional survey was conducted among older AA adults from low-income areas in south Los Angeles. We used convenience sampling from economically disadvantaged areas of south Los Angeles to recruit older AA adults from 16 predominantly AA churches, 11 senior residential units, and low-income public housing projects. Church leaders and apartment managers facilitated recruitment by encouraging eligible adults in their community to participate in this comprehensive health evaluation which would include collecting their demographic, social, behavioral, and health information. As part of the primary study, a comprehensive evaluation of each participant's medication was performed but this was not included in the current study.
Eligibility was restricted to those adults who were AA, 55 years or older, able to complete an interview in English, and resided in Service Planning Area 6 (SPA 6), one of the most economically disadvantaged urban areas in Los Angeles county as well as the highest percentage of AAs (27.4%) of the SPAs in Los Angeles (52). SPA6 has the highest unemployment rate (13.65%) as well as the highest percentage of household incomes <100% of the Federal Poverty Level (33.6%) of the SPAs in Los Angeles (52, 53). Those adults who were institutionalized, enrolled in other clinical trials, or had poor cognitive performance were excluded. The sample was 740 AA adults aged 55 or older.
Measures
The current study collected data through structured face-to-face interviews using several pages of checklist-style questionnaires created by the investigator based on standard validated measures and previous research. Interviews took place over several hours and collected information concerning gender, age, educational attainment, living alone, marital status, health behaviors (smoking and drinking), depressive symptoms, chronic pain, CMCs, SRH, sick days, and financial difficulties.
Dependent Variable
Demographic factors
Gender was treated as a dichotomous variable (1 female, 0 male), and age was operationalized as an interval variable.
Educational attainment
Educational attainment was treated as an interval variable (years of schooling), with more years reflecting higher educational attainment.
Living arrangement and marital status
Living arrangements and marital status were treated as dichotomous variables (1 living alone, 0 living with someone else; 1 married, 0 not-married).
Smoking
Participants reported their current smoking status, by answering the question “How would you describe your cigarette smoking habits?.” Responses included current smoker, previously smoked, or never smoke. This variable was treated as a dichotomous variable (1 ever smoker, 0 never smoker).
Binge drinking
Participants reported their drinking status by answering questions such as “Do you drink alcohol?,” “Do you ever drink five or more drinks on one occasion?,” “In the past 30 days, how many times did you have five or more drinks on one occasion?” Responses to the first and second question were yes or no. Using these items, we defined a dichotomous variable that indicated any binge drinking.
Depressive symptoms
Depressive symptoms were measured using the 15 item- Short Geriatric Depression Scale (GDS) (54, 55). Responses were on a “yes” or “no” scale. Summary scores were calculated, ranging between 0 and 15, with higher scores reflecting more depressive symptoms. The GDS-Short form has been used extensively among older adults in community and clinical settings to measure depression and has shown excellent reliability and validity (54, 55).
Chronic pain
Chronic pain was measured using four subscales of the McGill Pain Questionnaire–Short Form 2 (MPQ-SF-2) (56–59). Over 22 items, participants rated the extent of their past-week experience of various types of pain on an 11-point numeric scale (0 none to 10 worst possible). The subscales of the MPQ-SF-2 include: (a) continuity (throbbing, cramping, gnawing, aching, heavy, and tender pain), (b) intermittence (shooting, stabbing, sharp, splitting, electric-shock, and piercing pain), (c) neuropathic nature (hot-burning, cold-freezing, itching, tingling or “pins and needles,” light touch, and numbness pain), and (d) affective domain (tiring-exhausting, sickening, fearful, and punishing-cruel pain). Based on the average responses to all questions, a total pain score was calculated (56–59), and a higher score reflected more chronic pain.
Number of CMCs
Participants reported whether a physician has ever told them that they have any of the following CMCs: hypertension, heart disease, diabetes, lipid disorder/hypercholesterolemia, cancer, asthma, osteoarthritis, thyroid disorder, chronic obstructive pulmonary disease, rheumatoid arthritis, and gastrointestinal disease. Although self-reports provide valid information regarding CMCs, some level of measurement bias is expected (60).
Self-rated health (SRH)
This study measured SRH by the question, “Would you say your health in general is excellent, very good, good, fair, or poor?” Responses included excellent (1), very good (2), good (3), fair (4), and poor (5). SRH was treated as a continuous variable with higher scores indicating worse health. Poor SRH has been demonstrated to be a strong predictor of mortality across settings (61). The Institute of Medicine suggests that SRH be used as a tool for monitoring the health of people in the United States in national studies (62).
Sick days
Sick days were measured through a single item which asks, “In the past 12 months, how frequently have you been sick?” Responses included never (1), rarely (2), sometimes (3), most of the time (4), and always (5). Sick days were treated as an interval variable, with a higher score indicating more sick days. Frequency of sick days is commonly used as a proxy for health status (63, 64).
Health insurance
Health insurance was also measured through a single item which asks, “Do you have health insurance?” and the type of insurance was also noted. Responses were treated as a dichotomous variable (yes or no). This variable was not included in the analysis, however, as 98.8% of participants had health insurance.
Independent Variables
Financial difficulties
We measured financial difficulties using three items (α = 0.9) that asked how often participants lacked enough money for necessities, such as food, rent/mortgage, clothes, and utility bills. Responses for each item were given on a 5-point Likert- scale (1 never to 5 always) and a sum score was built ranging between 3 and 15, with higher scores reflecting more financial difficultie (lower SES).
Statistical Analysis
We used SPSS 22.0 (SPSS Inc., Chicago, IL, USA) to conduct the data analysis. Frequency (%) and mean (SD) were reported describing the sample. Bivariate correlations in the overall sample were calculated using Pearson's correlation. Linear regression models were applied with financial difficulties as the outcome, and the independent variables were gender, age, educational attainment, living alone, marital status, smoking, drinking, depressive symptoms, chronic pain, CMCs, SRH, and sick days. The list of variables was determined based on the literature review. Adjusted bivariate correlations controlled for gender, age, educational attainment, living alone, marital status, and health insurance as these variables fell under the category of demographic, social, and behavioral factors that had currently or in previous research demonstrated a relationship with financial difficulties. We controlled for these confounding variables in order to see the unique relationship between financial difficulties and mental and physical health outcomes. Smoking could not be included in the adjusted analysis as the linear regression included only continuous variables and smoking was measured as a dichotomous variable. We reported correlation coefficients (b), standard error (SE), 95% confidence intervals (95% CI), and p-values.
Results
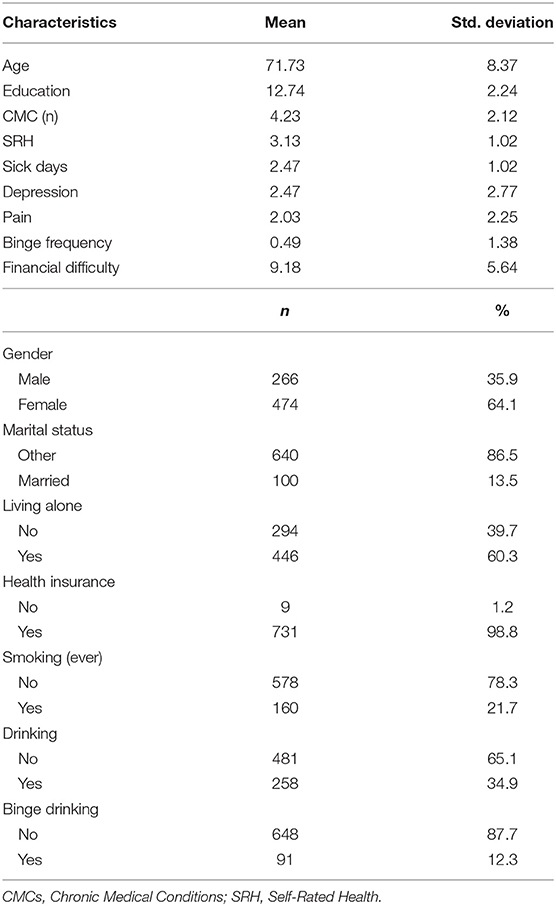
740 AA older adults who were at least 55 years old entered this study. Participants were on average 72 years old, with four CMCs. On average, they had considerable financial difficulty (9.18). They were mostly women (64%) and unmarried (86.5%). Most participants had never smoked and were not drinking alcohol (Table 1).
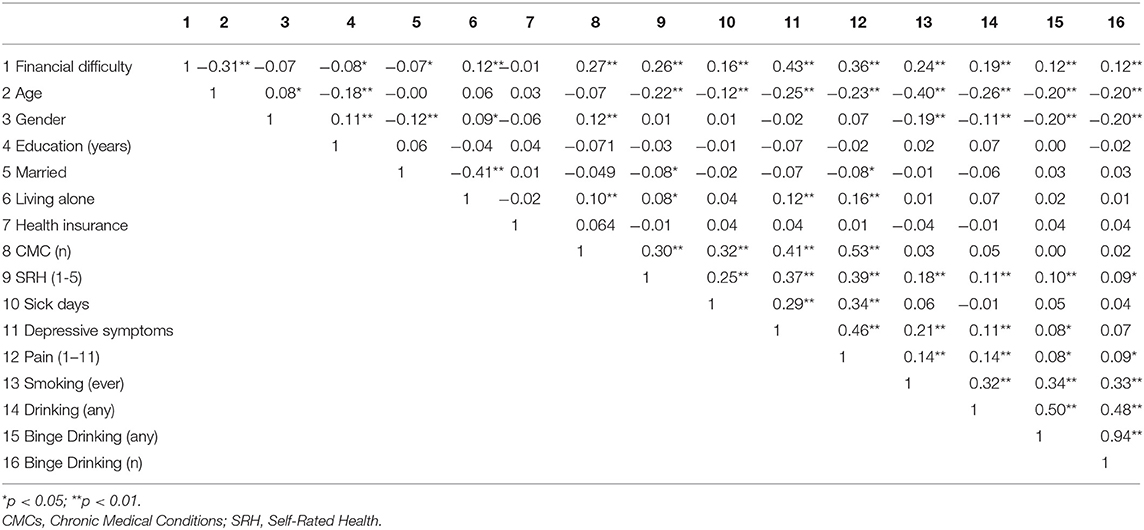
Unadjusted Correlates of Financial Difficulty
Table 2 shows the unadjusted (zero order) bivariate correlations between the study variables. Financial difficulty was inversely correlated with age, education, and marital status. Financial difficulty was positively correlated with CMCs (n), SRH (worse), sick days, depressive symptoms, chronic pain, smoking, drinking, any binge drinking, and number of binge drinking (Table 2).
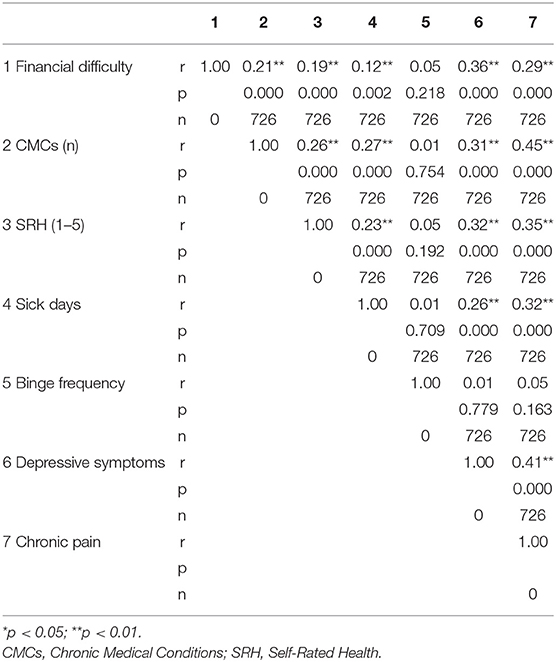
Adjusted Correlates of Financial Difficulty
Table 3 shows the adjusted (partial) bivariate correlations between financial difficulty, CMCs (n), SRH (1–5), sick days, binge drinking, and depressive symptoms. In these correlations, age, gender, education, marital status, insurance, and living alone were controlled. Financial difficulty was positively correlated with CMCs (n), SRH (worse), sick days, depressive symptoms, and chronic pain (Table 3).
Discussion
The current study sought to understand mental and physical health correlates of financial difficulties in older AA adults living in economically disadvantaged areas of Los Angeles. The adjusted analysis, controlling for age, gender, education, marital status, living alone, and health insurance, showed that financial difficulties are correlated with depressive symptoms, chronic pain, number of CMCs, worse SRH, and sick days.
Adjusted Correlates of Financial Difficulties
In the adjusted partial correlation analysis, we controlled for gender, age, education, marital status, living alone, and health insurance. Considering that health insurance is the gateway to healthcare and these demographic and SES factors are commonly correlated with health status (18, 43, 65–67), these variables were selected in order to analyze the unique relationship between financial difficulties and continuous mental and physical health variables. While much of the previous research would suggest that binge drinking is positively associated with financial difficulties, especially for AA samples (8, 9, 11), the findings did not indicate an association between financial difficulties and binge drinking. This may be due to the high percentage of participants who did not drink at all in our sample (65.1%). Considering the study environment is situated in economically disadvantaged areas, liquor store density is usually high and the influence of a substance use environment is evidenced to be stronger in the AA population (68). However, our convenience sample may have been skewed to include those who were more advantaged in the area rather than those who may have been more financially deprived or dealing specifically with substance use issues. Furthermore, those who binge drink more frequently are at an increased risk of earlier morbidity and therefore may not be included in our sample of older adults. Future research should explore whether this finding extends to other older AA adult samples and the possibility of age being a protective factor within this group.
Financial difficulties were also positively related to depressive symptoms. Much of the previous research has supported this relationship, showing a significant relationship between financial difficulties and the risk for depression as well as the severity of depressive symptoms (8, 14–16). Furthermore, research has found this relationship in AA samples and shown an increased risk among AAs and older adults (14–17). Considering the toll depressive symptoms take and the stress financial difficulties bring, it is understandable that these two variables are related, especially among a population that experiences disparities in income and mental health care (1, 69, 70). The current findings therefore align with the literature demonstrating a significant relationship between depressive symptoms and financial difficulties in older AA adults, and demonstrates that this relationship remains significant even after controlling for age, gender, education, marital status, living alone, and health insurance.
After controlling for the demographic and SES variables, financial difficulties were still positively associated with chronic pain in our sample. This aligns with much of the existing research which has shown that low SES is related to higher risk for incidence of pain, greater severity of pain, as well as, greater disability and distress from pain (18–22). While the previous research demonstrated the relationship between financial difficulties and several aspects of pain, the current study shows this relationship holds for AA samples specifically, who are especially at risk for pain mismanagement or under-treatment (71–74).
Additionally, after the adjusted analyses, financial difficulties were significantly positively associated with the number of CMCs. This finding aligns with past research indicating a link between financial difficulties and CMCs (23, 25). CMCs not only lead to increase medical costs but they detract from one's ability to work (25). Simultaneously, financial distress can take a toll on one's health physically, leading to an increased risk of CMCs (23). While we cannot make directional causal assumptions based on this analysis, these may be some of the underlying mechanisms behind the relationship between these two variables. These findings importantly demonstrate this association in an older AA sample, who have heightened rates of both financial difficulties and CMCs (1–4).
Furthermore, adjusted analyses revealed that financial difficulties were related to poorer SRH. This aligns with previous research revealing a relationship between financial difficulties or low-SES and SRH (26–29). While previous research has found this relationship in distinct low-income (28), AA (27), or older adult (29) samples, the current study provides evidence for this correlation among a sample with all of those characteristics. This provides more evidence for the relationship between financial difficulties and health variables like SRH for older AA adults, which is especially relevant given the limited health resources in low-income urban areas.
In addition, financial difficulties were positively associated with sick days. As suggested by limited previous research, financial difficulties and sickness absenteeism appear to be positively correlated in some populations (30–32). Given that taking sick days may lead to strains at work and thus financial difficulties, or that financial difficulties may take a toll on one's health leading to sick days, it is understandable that these two variables may be related although we cannot make directional causal assumptions based on the current analysis. Among this older population, managing multiple comorbidities may lead to several sick days when ill compared to younger populations who are usually healthier (75). Experiencing sick days can lead to multiple hospitalizations and visits, additional prescribed medications, and potential loss of income, if still employed (25). This can be overwhelmingly problematic for this AA population, especially if on a fixed income with costly health expenditures (76). Even if there is an acute period of a few sick days in an entire month, it can have a devastating effect on future financial outlooks for elderly individuals and their households (77).
These results are suggestive of a significant relationship between financial difficulties and various domains of mental and physical health (i.e., depression, chronic pain, CMCs, SRH, and sick days) of low-income AA older adults.
Limitations
The findings of this study must be viewed within the context of its limitations. Due to the cross-sectional design, causal associations cannot be inferred. For both methodological and ethical reasons, it would be inaccurate to suggest financial difficulties are due to poor health or health behaviors in this population rather than entrenched societal inequalities. Although not studied here, financial difficulties in AA communities have historical and current links to institutionalized racism and systematic marginalization. Claims about the mechanisms underlying the associations identified here require more nuanced data and measurements collected over the life course to more adequately test the causal role of contextual and societal factors that may explain the observed associations.
Additionally, we did not have access to the clinical records of the participants to verify CMCs or mental health diagnosis nor did we have data on area level SES factors such as neighborhood income. We also did not have data on history of depression or other psychiatric disorders. Our results may be affected by self-report measurement bias. Future research should utilize administrative data or medical chart review when attempting to replicate these findings. Additionally, due to our non-random sampling, we cannot generalize our results to all AA communities. Despite these limitations, the current study furthers our understanding of mental and physical health correlates of financial difficulties among older AA adults in economically disadvantaged urban settings.
Conclusions
The current study examined mental and physical health correlates of financial difficulties in a sample of older AA adults who were residing in low-income areas of South Los Angeles. After controlling for age, gender, education, marital status, living alone, and health insurance, financial difficulties were correlated with depressive symptoms, chronic pain, CMCs, SRH, and sick days. The findings shed light on the importance of screening for financial difficulties in addressing mental and physical health of older AA adults. Given that AA populations in similar settings (low-income areas) are facing economic disparities, the current study highlights that financial difficulties should be addressed in interventions designed to promote mental and physical health of AA older adults.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) Charles R. Drew University of Medicine and Science (CDU). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
ME prepared the first draft and revised the paper. MB designed the study, secured the funding, conducted the study, collected the data, and revised the manuscript. SA analyzed the data, conceptualized this report, and contributed to the revision of the paper. All authors contributed to the revision of the paper and approved the final draft.
Funding
This study was supported by the Center for Medicare and Medicaid Services (CMS) Grant 1H0CMS331621 to Charles R. Drew University of Medicine and Science (PI: MB). Additionally, MB and SA were supported by the NIH under Awards # 54MD008149, # R25 MD007610, 2U54MD007598, and U54 TR001627. SA was also supported by the National Cancer Institute (NCI) grant CA201415-02 (Co-PI = R. Mistry).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Semega JL, Fontenot KR, Kollar MA. Income and Poverty in the United States: 2016. Current Population Reports. Washington, DC: U.S. Census Bureau (2017).
2. Kim EJ, Kim T, Conigliaro J, Liebschutz JM, Paasche-Orlow MK, Hanchate AD. Racial and ethnic disparities in diagnosis of chronic medical conditions in the USA. J Gener Inter Med. (2018) 33:1116–23. doi: 10.1007/s11606-018-4471-1
3. Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among blacks or African Americans—United States, 1999–2015. MMWR Morb Mortal Wkly Rep. (2017) 66:444–56. doi: 10.15585/mmwr.mm6617e1
4. Fairley TL, Tai E, Townsend JS, Stewart SL, Steele CB, Davis SP, et al. Racial/ethnic disparities and geographic differences in lung cancer incidence-38 States and the District of Columbia, 1998–2006. Morbidity Mortality Weekly Rep. (2010) 59:1433–8.
5. Green CR, Ndao-Brumblay SK, Nagrant AM, Baker TA, Rothman E. Race, age, and gender influences among clusters of African American and white patients with chronic pain. J Pain. (2004) 5:171–82. doi: 10.1016/j.jpain.2004.02.227
6. Peterson JC, Burnes DPR, Caccamise PL, Mason A, Henderson CR Jr, Wells MT, et al. Financial exploitation of older adults: a population-based prevalence study. J Gener Inter Med. (2014) 29:1615–23. doi: 10.1007/s11606-014-2946-2
7. Kahn JR, Fazio EM. Economic status over the life course and racial disparities in health. J Gerontol S B Psychol Sci Soc Sci. (2005) 60(Suppl. 2):76–84. doi: 10.1093/geronb/60
8. Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and fina and physical health: a systematic review and meta-analysis. Clin Psychol Rev. (2013) 33:1148–62. doi: 10.1016/j.cpr.2013.08.009
9. Peirce RS, Frone MR, Russell M, Cooper ML. Relationship of financial strain and psychosocial resources to alcohol use and abuse: the mediating role of negative affect and drinking motives. J Health Soc Behav. (1994) 35:291–308. doi: 10.2307/2137211
10. Krause N. Stress, religiosity, and abstinence from alcohol. Psychol Aging. (1991) 6:134–44. doi: 10.1037/0882-7974.6.1.134
11. Rogers CJ, Forster M, Unger JB. Ethnic variations in the relationship between multiple stress domains and use of several types of tobacco/nicotine products among a diverse sample of adults. Add Behav Rep. (2018) 7:96–102. doi: 10.1016/j.abrep.2018.03.006
12. Kendzor DE, Businelle MS, Waters AF, Frank SG, Hébert ET. Financial strain indirectly influences smoking cessation through withdrawal symptom severity. Drug Alcohol Depend. (2018) 183:55–61. doi: 10.1016/j.drugalcdep.2017.10.027
13. Kendzor DE, Businelle MS, Costello TJ, Castro Y, Reitzel LR, Cofta-Woerpel LM, et al. Financial strain and smoking cessation among racially/ethnically diverse smokers. Am J Public Health. (2010) 100:702–6. doi: 10.2105/AJPH.2009.172676
14. Assari S. Race, depression, and financial distress in a nationally representative sample of American adults. Brain Sci. (2019) 9:29. doi: 10.3390/brainsci9020029
15. Bazargan M, Hamm-Baugh VP. The relationship between chronic illness and depression in a community of urban black elderly persons. J Gerontol Ser B Psychol Sci Soc Sci. (1995) 50:S119–27. doi: 10.1093/geronb/50B.2.S119
16. Lincoln KD, Chatters LM, Taylor RJ. Social support, traumatic events, and depressive symptoms among African Americans. J Marr Family. (2005) 67:754–66. doi: 10.1111/j.1741-3737.2005.00167.x
17. Green MJ, Benzeval M. The development of socioeconomic inequalities in anxiety and depression symptoms over the lifecourse. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1951–61. doi: 10.1007/s00127-013-0720-0
18. Brekke M, Hjortdahl P, Kvien TK. Severity of musculoskeletal pain: relations to socioeconomic inequality. Soc Sci Med. (2002) 54:221–8. doi: 10.1016/S0277-9536(01)00018-1
19. Dorner TE, Muckenhuber J, Stronegger WJ, Ràsky E, Gustorff B, Freidl W. The impact of socio-economic status on pain and the perception of disability due to pain. Eur J Pain. (2011) 15:103–9. doi: 10.1016/j.ejpain.2010.05.013
20. Rios R, Zautra AJ. Socioeconomic disparities in pain: the role of economic hardship and daily financial worry. Health Psychol. (2011) 30:58–66. doi: 10.1037/a0022025
21. Herrera-Escobar JP, Seshadri AJ, Rivero R, Toppo A, Al Rafai SS, Scott JW, et al. Lower education and income predict worse long-term outcomes after injury. J Trauma Acute Care Surg. (2019) 87:104–10. doi: 10.1097/TA.0000000000002329
22. Thomtén J, Soares Joaquim JF, Sundin Ö. Pain among women: associations with socio-economic factors over time and the mediating role of depressive symptoms. Scand J Pain. (2012) 3:62–7. doi: 10.1016/j.sjpain.2011.12.003
23. Cutrona CE, Abraham WT, Russell DW, Beach SRH, Gibbons FX, Gerrard M, et al. Financial strain, inflammatory factors, and haemoglobin A1c levels in African American women. Br J Health Psychol. (2015) 20:662–79. doi: 10.1111/bjhp.12120
24. Szanton SL, Allen JK, Thorpe RJ Jr, Seeman T, Bandeen-Roche K, Fried LP. Effect of financial strain on mortality in community-dwelling older women. J Gerontol Ser B Psychol Sci Soc Sci. (2008) 63:S369–74. doi: 10.1093/geronb/63.6.S369
25. Cagle JG, Carr DC, Hong S, Zimmerman S. Financial burden among US households affected by cancer at the end of life. Psycho Oncol. (2016) 25:919–26. doi: 10.1002/pon.3933
26. Ko J, Jang Y, Park N, Rhew S, Chiriboga D. Neighborhood effects on the self-rated health of older adults from four racial/ethnic groups. Soc Work Pub Health. (2014) 29:89–99. doi: 10.1080/19371918.2013.829760
27. Savoy EJ, Reitzel LR, Nguyen N, Advani PS, Fisher FD, Wetter DW, et al. Financial strain and self-rated health among black adults. Am J Health Behav. (2014) 38:340–50. doi: 10.5993/AJHB.38.3.3
28. Tucker-Seeley RD, Harley AE, Stoddard AM, Sorensen GG. Financial hardship and self-rated health among low-income housing residents. Health Edu. Behav. (2013) 40:442–8. doi: 10.1177/1090198112463021
29. Kim H, Lyons AC. No pain, no strain: impact of health on the financial security of older Americans. J Consumer Affairs. (2008) 42:9–36. doi: 10.1111/j.1745-6606.2007.00092.x
30. Kim J, Garman ET. Financial Stress and absenteeism: an empirically. derived model. J Financ Counsel Plan. (2003) 14:31.
31. Suominen S, Vahtera J, Korkeila K, Helenius H, Kivimäki M, Koskenvuo M. Job strain, life events, and sickness absence: a longitudinal cohort study in a random population sample. J Occupat Environ Med. (2007) 49:990–6. doi: 10.1097/JOM.0b013e3181343e2b
32. Kivimäki M, Vahtera J, Elovainio M, Lillrank B, Kevin MV. Death or illness of a family member, violence, interpersonal conflict, and financial difficulties as predictors of sickness absence: longitudinal cohort study on psychological and behavioral links. Psychoso Med. (2002) 64:817–25. doi: 10.1097/00006842-200209000-00015
33. Sutton JP, Dunstan DA. Financial strain and loss of psychosocial benefits of work mediate the relationship between sickness absence and depression among people with work disability. Aus J Rehabil Counsel. (2012) 18:71–88. doi: 10.1017/jrc.2012.11
34. Vespa J, Lewis J, Kreider R. America's Families and Living Arrangements: 2012. Washington, DC: US Census Bureau (2013).
35. Whitley DM, Kelley SJ, Lamis DA. Depression, social support, and mental health: a longitudinal mediation analysis in African American custodial grandmothers. Int J Aging Hum Dev. (2016) 82:166–87. doi: 10.1177/0091415015626550
36. Clottey EN, Scott AJ, Alfonso ML. Grandparent caregiving among rural African Americans in a community in the American South: challenges to health and wellbeing. Rural Remote Health. (2015) 15:3313. Available online at: www.rrh.org.au/journal/article/3313
37. Samuel PS, Marsack CN, Johnson LA, LeRoy BW, Lysack CL, Lichtenberg PA. Impact of grandchild caregiving on African American grandparents. Occupat Therap Health Care. (2017) 31:1–19. doi: 10.1080/07380577.2016.1243821
38. Whitley DM, Fuller-Thomson E. African-American solo grandparents raising grandchildren: a representative profile of their health status. J Commun Health. (2017) 42:312–23. doi: 10.1007/s10900-016-0257-8
39. Zhan M, Lanesskog D. The impact of family assets and debt on college graduation. Child Youth Serv Rev. (2014) 43:67–74. doi: 10.1016/j.childyouth.2014.04.011
40. Grinstein-Weiss M, Perantie DC, Taylor SH, Guo S, Raghavan R. Racial disparities in education debt burden among low- and moderate-income households. Child Youth Serv Rev. (2016) 65:166–74. doi: 10.1016/j.childyouth.2016.04.010
41. Kim J, Chatterjee S, Young J, Moon UJ. The cost of access: racial disparities in student loan burdens of young adults. College Student J. (2016) 51:99–114.
42. Assari S. Life expectancy gain due to employment status depends on race, gender, education, and their intersections. J Racial Ethn Health Disparit. (2018) 5:375–86. doi: 10.1007/s40615-017-0381-x
43. Dean A, Kolody B, Wood P, Matt GE. The influence of living alone on depression in elderly persons. J Aging Health. (1992) 4:3–18. doi: 10.1177/089826439200400101
44. Mohebbi M, Agustini B, Woods RL, McNeil JJ, Nelson MR, Shah RC, et al. Prevalence of depressive symptoms and its associated factors among healthy community-dwelling older adults living in australia and the united states. Int J Geriatr Psychiatr. (2019) 34:1208–16. doi: 10.1002/gps.5119
45. Xiu Ying H, Qian C, Peng X-d, Zhang X-m, Quan H-C. Living arrangements and risk for late life depression: a meta-analysis of published literature. Int J Psychiatr Med. (2012) 43:19–34. doi: 10.2190/PM.43.1.b
46. Temple JB. Correlates of housing affordability stress among older Australians. Aus J Ageing. (2008) 27:20–5. doi: 10.1111/j.1741-6612.2007.00268.x
47. Chou K-L, Chi I. Comparison between elderly Chinese living alone and those living with others. J Gerontol Soc Work. (2000) 33:51–66. doi: 10.1300/J083v33n04_05
48. Caputo RK. Marital status and other correlates of personal bankruptcy, 1986-2004. Marr Family Rev. (2008) 44:5–31. doi: 10.1080/01494920802184952
49. Bryant CM, Wickrama KAS, Bolland J, Bryant BM, Cutrona CE, Stanik CE. Race matters, even in marriage: identifying factors linked to marital outcomes for African Americans. J Family Theory Rev. (2010) 2:157–74. doi: 10.1111/j.1756-2589.2010.00051.x
50. Clavél FD, Cutrona CE, Russell DW. United and divided by stress: how stressors differentially influence social support in African American couples over time. Personal Soc Psychol Bull. (2017) 43:1050–64. doi: 10.1177/0146167217704195
51. Barton AW, Bryant CM. Financial strain, trajectories of marital processes, and African American newlyweds' marital instability. J Family Psychol. (2016) 30:657–64. doi: 10.1037/fam0000190
52. Los Angeles County Department of Public Health. Key Indicators of Health by Service Planning Area 2017. Los Angeles, CA: Los Angeles County Department of Public Health (2017).
53. County of Los Angeles Department of Public Health. Community Health Assesssment. Los Angeles, CA: County of Los Angeles Department of Public Health (2015).
54. Greenberg SA. How to try this: the geriatric depression scale: short form. Am J Nursing. (2007) 107:60–9. doi: 10.1097/01.NAJ.0000292204.52313.f3
55. Burke WJ, Roccaforte WH, Wengel SP. The short form of the geriatric depression scale: a comparison with the 30-item form. Topics Geriatr. (1991) 4:173–8. doi: 10.1177/089198879100400310
56. Kachooei AR, Ebrahimzadeh MH, Erfani-Sayyar R, Salehi M, Salimi E, Razi S. Short form-mcgill pain questionnaire-2 (SF-MPQ-2): a cross-cultural adaptation and validation study of the persian version in patients with knee osteoarthritis. Arch Bone Joint Surg. (2015) 3:45–50.
57. Ortner CM, Turk DC, Theodore BR, Siaulys MM, Bollag LA, Landau R. The short-form mcgill pain questionnaire-revised to evaluate persistent pain and surgery-related symptoms in healthy women undergoing a planned cesarean delivery. Reg Anesthes Pain Med. (2014) 39:478–86. doi: 10.1097/AAP.0000000000000158
58. Droz J, Howard FM. Use of the short-form mcgill pain questionnaire as a diagnostic tool in women with chronic pelvic pain. J Mini Invasive Gynecol. (2011) 18:211–7. doi: 10.1016/j.jmig.2010.12.009
59. Strand LI, Ljunggren AE, Bogen B, Ask T, Johnsen TB. The short-form mcgill pain questionnaire as an outcome measure: test-retest reliability and responsiveness to change. Eur. J Pain. (2008) 12:917–25. doi: 10.1016/j.ejpain.2007.12.013
60. Gross R, Bentur N, Elhayany A, Sherf M, Epstein L. The validity of self-reports on chronic disease: characteristics of underreporters and implications for the planning of services. Pub Health Rev. (1996) 24:167–82.
61. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. (1997) 38:21–37. doi: 10.2307/2955359
62. Institute of Medicine. State of the USA Health Indicators: Letter Report. Washington, DC: The National Academies Press (2009). doi: 10.17226/12534
63. Barnes C, Cauvin E, Duran-Kim M, Montalbano L, Londrigan M. A systematic review of the effectiveness of patient-centred care on emergency room visits, hospitalizations, unscheduled sick clinic visits, and missed school days for children with asthma. JBI Database Syst Rev Implemen Rep. (2011) 9:1–12. doi: 10.11124/01938924-201109481-00017
64. Linder LA, Bratton H, Nguyen A, Parker K, Phinney S. Comparison of good days and sick days of school-age children with cancer reflected through their drawings. Qual Life Res. (2017) 26:2729–38. doi: 10.1007/s11136-017-1621-6
65. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. (2009) 10:447–85. doi: 10.1016/j.jpain.2008.12.001
66. Schaakxs R, Comijs HC, Lamers F, Kok RM, Beekman ATF, Penninx BWJH. Associations between age and the course of major depressive disorder: a 2-year longitudinal cohort study. Lancet Psychiatr. (2018) 5:581–90. doi: 10.1016/S2215-0366(18)30166-4
67. Bulloch AGM, Williams JVA, Lavorato DH, Patten SB. The depression and marital status relationship is modified by both age and gender. J Affect Disord. (2017) 223:65–8. doi: 10.1016/j.jad.2017.06.007
68. Theall KP, Lancaster BP, Lynch S, Haines RT, Scribner S, Scribner R, et al. The neighborhood alcohol environment and at-risk drinking among African-Americans. Alcohol Clin Experi Res. (2011) 35:996–1003. doi: 10.1111/j.1530-0277.2010.01430.x
69. Alegría M, Chatterji P, Wells K, Cao Z, Chen C-n, Takeuchi D, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. (2008) 59:1264–72. doi: 10.1176/ps.2008.59.11.1264
70. Das AK, Olfson M, McCurtis HL, Weissman MM. Depression in African Americans: breaking barriers to detection and treatment. J Family Pract. (2006) 55:30–9.
71. Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer: the eastern cooperative oncology group minority outpatient pain study. Ann Inter Med. (1997) 127:813–6. doi: 10.7326/0003-4819-127-9-199711010-00006
72. Shavers VL, Bakos A, Sheppard VB. Race, ethnicity, and pain among the US adult population. J Health Care Poor Underser. (2010) 21:177–220. doi: 10.1353/hpu.0.0255
73. Yazdanshenas H, Bazargan M, Smith J, Martins D, Motahari H, Orum G. Pain treatment of underserved older African Americans. J Am Geriatr Soc. (2016) 64:2116–21. doi: 10.1111/jgs.14302
74. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA. (2016) 113:4296–301. doi: 10.1073/pnas.1516047113
75. Chlebowy DO, Kubiak N, Myers J, Jorayeva A. The relationships of demographic characteristics with diabetes biomarkers and physical activity adherence in African American adults. J Racial Ethnic health Disparit. (2016) 3:240–4. doi: 10.1007/s40615-015-0133-8
76. Byhoff E, Harris JA, Langa KM, Iwashyna TJ. Racial and ethnic differences in end-of-life medicare expenditures. J Am Geriatri Soc. (2016) 64:1789–97. doi: 10.1111/jgs.14263
Keywords: race/ethnicity, African Americans, ethnic groups, depressive symptoms, self-rated health, chronic medical conditions, financial difficulties, older adults
Citation: Evans MC, Bazargan M, Cobb S and Assari S (2020) Mental and Physical Health Correlates of Financial Difficulties Among African-American Older Adults in Low-Income Areas of Los Angeles. Front. Public Health 8:21. doi: 10.3389/fpubh.2020.00021
Received: 22 September 2019; Accepted: 23 January 2020;
Published: 12 February 2020.
Edited by:
Rasmus Hoffmann, University of Rostock, GermanyReviewed by:
Ivana Kulhánová, Charles University, CzechiaGwenn Menvielle, Institut National de la Santé et de la Recherche Médicale (INSERM), France
Copyright © 2020 Evans, Bazargan, Cobb and Assari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shervin Assari, YXNzYXJpQHVtaWNoLmVkdQ==
 Meghan C. Evans
Meghan C. Evans Mohsen Bazargan1,2
Mohsen Bazargan1,2 Shervin Assari
Shervin Assari