- 1Division of Gynecologic Surgical Subspecialties, Department of Obstetrics, Gynecology, and Women’s Health, Center for Endometriosis, Saint Louis University, St. Louis, MO, USA
- 2School of Medicine, Saint Louis University, St. Louis, MO, USA
- 3Department of Obstetrics, Gynecology, and Women’s Health, Saint Louis University, St. Louis, MO, USA
Objective: The purpose of this study was to examine if deep retraction pockets (DRPs) in the posterior cul-de-sac and uterosacral ligaments could be a manifestation of endometriosis and if excision of these pockets improves pain symptoms and quality of life.
Study design: Prospective cohort study Canadian Task Force Classification, II-3.
Materials and methods: Preoperative data, operative data, and follow-up data were collected prospectively at the Center for Endometriosis at Saint Louis University, a referral center for the surgical management of endometriosis.
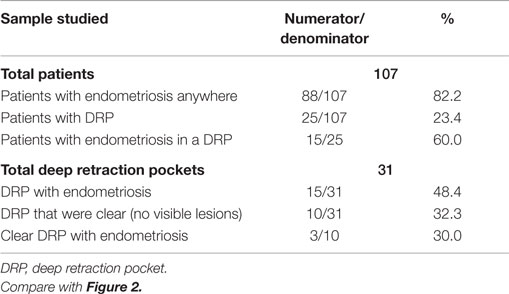
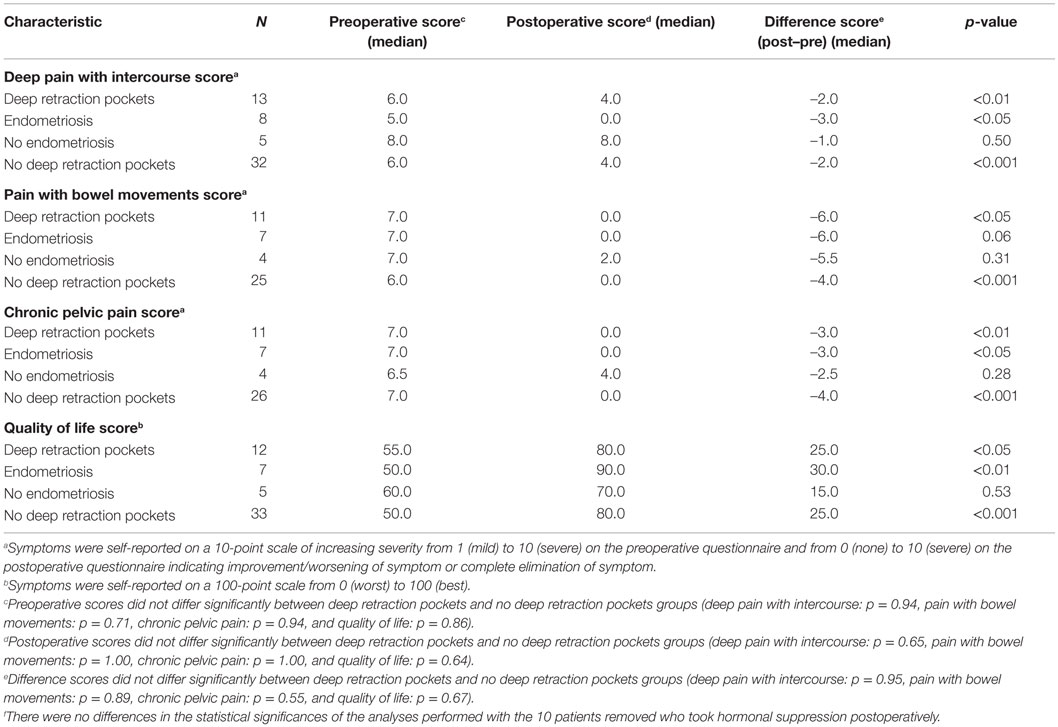
Results: The 107 consecutive patients who presented with preoperative deep dyspareunia were included in the study, and the median postoperative follow-up was 13 months. Endometriosis was confirmed histologically in any location excised in 88/107 (82.2%) of the women, and 31 DRPs were excised from 25 women with DRPs in the posterior cul-de-sac or uterosacral ligaments, of which 15/31 (48.4%) had endometriosis. Of the 10 DRPs without visible surface lesions, 3 (30.0%) had endometriosis on histology. Pain symptoms and quality of life significantly improved after excision surgery, whether or not DRPs were present. Women who had endometriosis in their DRP also had significant improvement in deep dyspareunia and chronic pelvic pain and quality of life. Results did not differ when patients who took postoperative hormonal suppression were removed from the analyses.
Conclusion: Patients had significantly improved pain symptoms and quality of life after excision surgery, whether or not DRPs were present. This study demonstrated that a DRP may be a manifestation of endometriosis (even with a clear surface of the pocket), so that DRPs should be excised to achieve optimal excision of endometriosis.
Introduction
A pelvic peritoneal pocket (or Allen-Masterson pocket) in association with endometriosis (Figure 1) was first described by Sampson (1). Chatman (2), Chatman and Zbella (3), and Redwine (4) later demonstrated the importance of recognizing peritoneal pockets as a potential manifestation of endometriosis, as endometriosis in such structures in women with pelvic pain otherwise could remain undiagnosed and untreated.
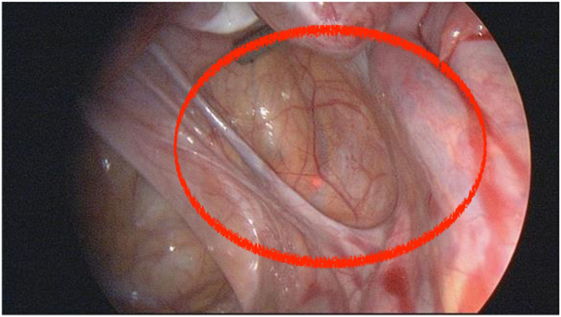
Figure 1. This annotated photo shows the appearance of a deep retraction pocket, with a visible manifestation of endometriosis, seen at laparoscopy for pelvic pain. There are abnormal red and white lesions suspicious for endometriosis at the base of the pocket.
Vercellini et al. (5) showed a poor correlation between location of pain and location of superficial disease. Hsu et al. (6) showed a stronger correlation between location of pain and location of deep disease.
The purpose of this study was to examine if deep retraction pockets (DRPs) in the posterior cul-de-sac and uterosacral ligaments could be a manifestation of endometriosis, and if excision of these pockets improves pain symptoms and quality of life.
Study Design
Prospective cohort study Canadian Task Force Classification, II-3.
Materials and Methods
Consecutive patients seen for pelvic pain at the Center for Endometriosis at Saint Louis University (SLU), a referral center for the surgical management of endometriosis, were recruited for the study. Patients included in this study were those who described deep dyspareunia on a standard of care preoperative questionnaire and who underwent laparoscopic excision surgery to relieve pain symptoms. All patients underwent optimal or complete excision of all visible manifestations of endometriosis, including peritoneal retraction pockets.
Preoperative data, operative data, and follow-up data were collected prospectively as part of an on-going database approved by the SLU Institutional Review Board (IRB). Symptom data were collected on deep dyspareunia and dyschezia by a 10-point visual analog scale (VAS) and on quality of life by a simple 100-point scale (7) before and after excision surgery. Operative data collected included location of abnormal peritoneum and DRPs (defined as estimated to be greater than 0.5 cm), phenotype or color of lesions excised, and diagnosis of endometriosis by histology. Patients were not specifically recommended to take hormonal suppression after surgery, though they were free to do so for contraception or to induce amenorrhea.
Differences in demographic characteristics, surgical characteristics, baseline severe pain symptoms (≥7 versus <7), and baseline quality of life (≥70 versus <70) between women with and without DRP were assessed using chi-square test and Fisher’s Exact test for categorical variables. Independent Student’s t-test or the Kolmogorov–Smirnov test was used for continuous variables depending on the normality of the distributions. Changes in pain symptoms and quality of life from before surgery to after surgery for women with DRP and women without DRP were assessed using paired t-tests or the Wilcoxon signed-rank test depending on distribution normality. Preoperative, postoperative, and rate of change of pain scores, and quality of life between women with and without DRP were compared using the independent Student’s t-test or the Kolmogorov–Smirnov test. A p-value of <0.05 was used to denote statistical significance. All analyses were performed using SPSS version 23.0 for Windows.
Results
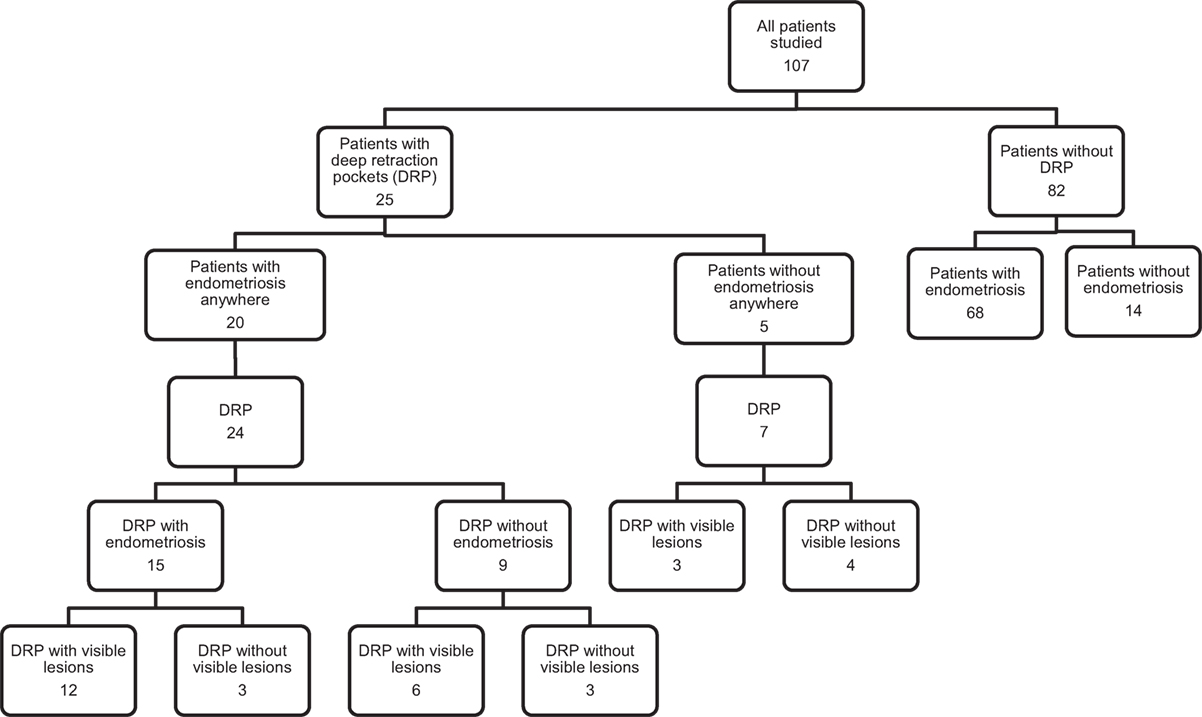
The 107 consecutive patients who presented with preoperative deep dyspareunia from February 20, 2012 to July 16, 2013 were included in the study (Table 1; Figure 2). The postoperative questionnaire was completed by 53/107 (49.5%) of the women at a median time after surgery of 13 months and a range of 12–25 months.
Endometriosis was confirmed histologically in any location excised in 88/107 (82.2%) of the women (Table 1; Figure 2). Twenty-five of the 107 women (23.4%) had DRP in the posterior cul-de-sac or uterosacral ligaments, of whom 15/25 (60.0%) had endometriosis confirmed in at least one DRP. Of the women with confirmed endometriosis anywhere, 20/88 (22.7%) had DRP, and of the women without confirmed endometriosis, 5/19 (26.3%) had DRP. Of the 15 women with endometriosis in DRP, 13/15 (86.7%) had Stage II endometriosis and 2/15 (13.3%) had Stage III endometriosis by the r-ASRM classification. Of the women with endometriosis anywhere who completed the postoperative questionnaire, 9/44 (20.5%) took hormonal suppression after surgery. Of the women with deep dyspareunia who completed the postoperative questionnaire, 1/9 (11.1%) of women with DRP and 9/39 (23.1%) of women without DRP (p = 0.66) took hormonal suppression after surgery.
A total of 31 DRPs were excised from the 25 women with DRP in the posterior cul-de-sac or uterosacral ligaments, of which 15/31 (48.4%) had endometriosis (Table 1). Ten of the 31 (32.3%) DRPs had no visible lesion on the surface of the pocket. Of these 10 DRPs without visible surface lesions, 3 (30.0%) had endometriosis on histology. The DRP locations where endometriosis most commonly occurred were the left and right uterosacral ligaments, being present in 9/31 (29.0%) DRP for each.
Women with DRP did not differ significantly from women without DRP on age, severe baseline pain symptoms (≥7 for deep dyspareunia, dyschezia, and chronic pelvic pain), or baseline quality of life (Table 2). The two groups did differ significantly in that women without DRP had a higher mean BMI (27.9 ± 7.5 versus 24.6 ± 6.8, p < 0.05), higher proportions of Stage I disease (35.8 versus 0.0%, p < 0.001) and Stage IV disease (32.1 versus 8.0%, p < 0.05), and a lower proportion of Stage II disease (24.7 versus 72.0%, p < 0.001) than women with DRP (Table 2).
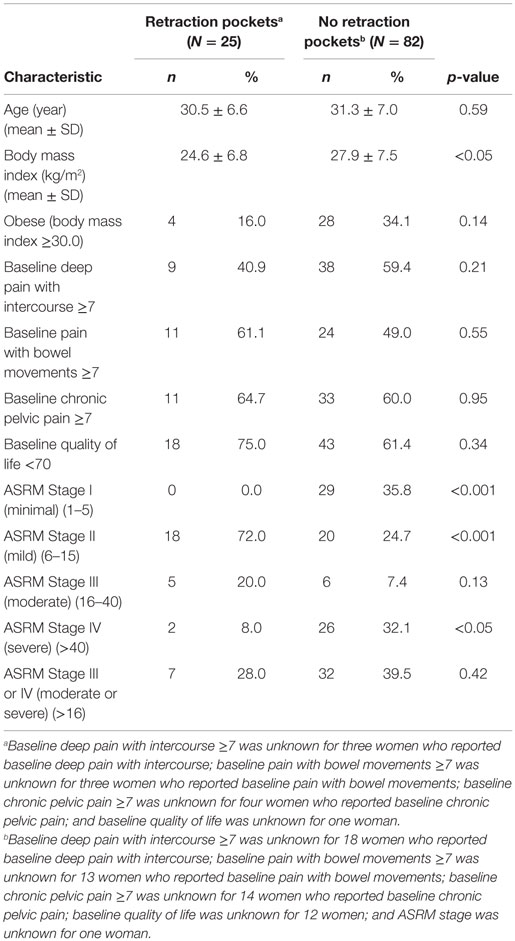
Table 2. Baseline and surgical characteristics and pain data for 107 women by deep retraction pockets.
Respondents and non-respondents to the postoperative questionnaire did not differ significantly on age, severe baseline pain symptoms, or baseline quality of life (Table 3). Non-respondents had a significantly higher mean BMI (29.1 ± 8.6 versus 25.1 ± 5.4, p < 0.01) and a higher rate of obesity (40.7 versus 18.9%, p < 0.05) than respondents.
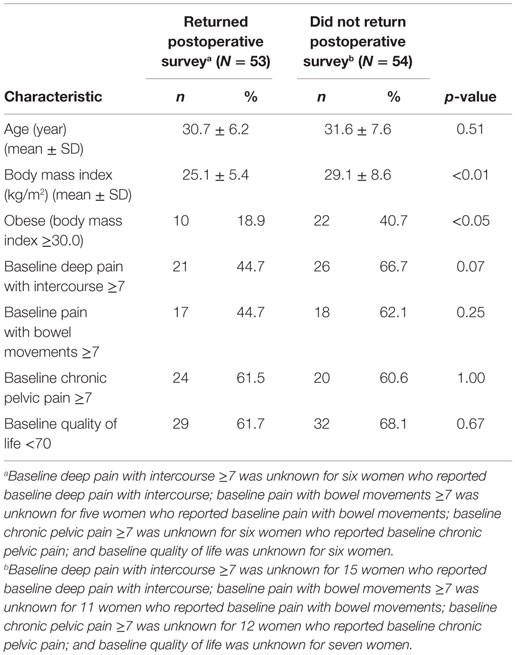
Table 3. Baseline demographic, pain, and quality of life data for 107 women by postoperative survey.
Women with DRP and women without DRP both had significant improvement in deep dyspareunia, dyschezia, and chronic pelvic pain after excision surgery (Table 4). Women who had endometriosis in their DRP also had significant improvement in deep dyspareunia and chronic pelvic pain. Quality of life significantly improved after excision surgery, whether or not DRPs were present, and in women who had endometriosis in their DRP. All significant improvements in pain symptoms and quality of life remained after women who reported hormonal suppression after surgery were removed from the analyses (data not shown).
Discussion
This study confirms the association of DRP, also called Allen-Masterson windows (2), and endometriosis. In our study, 25/107 (23.4%) of the women with deep dyspareunia had DRP within the posterior cul-de-sac or uterosacral ligaments, the majority of whom (15/25, 60%) had endometriosis diagnosed by histology in the pocket [Vilos (8) and Moen (9), only 12%]. These results are comparable to those of other studies looking at the association of retraction pockets and endometriosis, including Chatman (3) (17%) and Redwine (4) (18%). Our study adds the observation that even a clear pocket, a DRP without a visible surface lesion inside the pocket, can be associated with endometriosis up to 3/10 (30%) of the time. Thus, the retraction pocket itself, with or without visible surface lesions, can be a manifestation of endometriosis and should be treated.
The origin of retraction pockets has been postulated to result from peritoneal irritation or invasion by endometriosis, with resultant scarring and retraction of the peritoneum (2, 3). It also has been suggested that a retraction pocket may be a cause of endometriosis, where the disease presumably settles in a previously altered peritoneal surface (10). Since 16/31 (51.6%) of DRP did not have endometriosis in our study, it seems more likely that retraction pockets represent a primary developmental formation defect of the pelvic peritoneum. Since the rate of DRP was similar in patients with endometriosis 20/88 (22.7%) and patients without endometriosis 5/19 (26.3%), our study also does not support the postulate that endometriosis causes DRP (4). It is possible that endometriosis and DRP are unrelated in their origins.
Since endometriosis can be present (by histology) even if the surface of a DRP is clear, and given that quality of life improves when all manifestations of endometriosis are excised, including DRP, we recommend that DRP be removed at the time of excision surgery in patients with deep dyspareunia. Our patients had significantly improved quality of life after excision surgery, whether or not DRPs were present. Given that this study demonstrated that a DRP may be a manifestation of endometriosis (with or without visible lesions on the surface of the pocket), DRP also should be excised since the rate of recurrence or persistence of endometriosis has been shown to be very low after optimal excision of all possible visible manifestations of endometriosis (11). Since DRPs always were excised when present, further studies comparing outcomes after excision of DRP versus not excising DRP are needed to confirm this recommendation.
Limitations of our study include the lack of complete follow-up data (49.5% completion rate), lack of validated sexual functioning scales in measuring patient outcomes, lack of more detailed quality of life measures, and the lack of a comparison group where DRPs were seen but not treated. Strengths of our study include the prospective data collection of symptoms, quality of life before and after surgery and of the operative data, and consistency in patient treatment by a single surgeon committed to optimal excision.
Medical therapy has been shown to improve deep dyspareunia and quality of sex life (12). The majority of patients in our study did not take postoperative hormonal suppression. Future research also should compare medical and surgical therapies for deep dyspareunia and quality of life. Again, we recommend that validated sexual functioning questionnaires be used to assess patient outcomes in such studies.
Ethics Statement
The authors declare that the research was conducted in compliance with ethical standards.
Author Contributions
PY: project development, manuscript writing, and final approval of manuscript. IL: data collection and data management. JG: data management, data analysis, manuscript writing, and final approval of manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Special thanks to Erica Sher, medical student at Saint Louis University School of Medicine, for assistance in preparing a poster that was presented at the 12th World Congress on Endometriosis, São Paulo, Brazil, in April, 2014, to Jim Rice for maintenance of the database, and to Collin Miller for creation of the tables and figures. Jim Rice and Collin Miller are from the Division of Research, Department of Obstetrics, Gynecology, and Women’s Health, Saint Louis University School of Medicine.
References
1. Sampson JA. Metastatic or embolic endometriosis, due to the menstrual dissemination of endometrial tissue into the venous circulation. Am J Pathol (1927) 3:93–110.143.
2. Chatman DL. Pelvic peritoneal defects and endometriosis: Allen-Masters syndrome revisited. Fertil Steril (1981) 36:751–6.
3. Chatman DL, Zbella EA. Pelvic peritoneal defects and endometriosis: further observations. Fertil Steril (1986) 46:711–4.
4. Redwine DB. Peritoneal pockets and endometriosis. Confirmation of an important relationship, with further observations. J Reprod Med (1989) 34:270–2.
5. Vercellini P, Trespidi L, De Giorgi O, Cortesi I, Parazzini F, Crosignani PG. Endometriosis and pelvic pain: relation to disease stage and localization. Fertil Steril (1996) 65:299–304.
6. Hsu AL, Sinaii N, Segars J, Nieman LK, Stratton P. Relating pelvic pain location to surgical findings of endometriosis. Obstet Gynecol (2011) 118:223–30. doi: 10.1097/AOG.0b013e318223fed0
7. de Boer AG, van Lanschot JJ, Stalmeier PF, van Sandick JW, Hulscher JB, de Haes JC, et al. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res (2004) 13:311–20. doi:10.1023/B:QURE.0000018499.64574.1f
8. Vilos GA, Vilos AW, Haebe JJ. Laparoscopic findings, management, histopathology, and outcome of 25 women with cyclic leg pain. J Am Assoc Gynecol Laparosc (2002) 9:145–51. doi:10.1016/S1074-3804(05)60122-3
9. Moen MH, Halvorsen TB. Histologic confirmation of endometriosis in different peritoneal lesions. Acta Obstet Gynecol Scand (1992) 71:337–42. doi:10.3109/00016349209021069
10. Batt RE. Allen-Masters syndrome is caused by trauma, not by endometriosis. J Am Assoc Gynecol Laparosc (1995) 2:245–7. doi:10.1016/S1074-3804(05)80027-1
11. Yeung P Jr, Sinervo K, Winer W, Albee RB Jr. Complete laparoscopic excision of endometriosis in teenagers: is postoperative hormonal suppression necessary? Fertil Steril (2011) 95:1909–12. doi:10.1016/j.fertnstert.2011.02.037
Keywords: deep dyspareunia, quality of life, endometriosis, excision surgery, peritoneal window, retraction pocket, Allen-Masterson window, atypical endometriosis
Citation: Yeung PP Jr., Logan I and Gavard JA (2016) Deep Retraction Pockets, Endometriosis, and Quality of Life. Front. Public Health 4:85. doi: 10.3389/fpubh.2016.00085
Received: 18 December 2015; Accepted: 20 April 2016;
Published: 09 May 2016
Edited by:
Joseph B. Stanford, University of Utah, USAReviewed by:
Michael D. Manhart, Couple to Couple League, USAKyle Beiter, Saint Peters University Hospital, USA
Copyright: © 2016 Yeung, Logan and Gavard. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patrick P. Yeung Jr., cHlldW5nMUBzbHUuZWR1
 Patrick P. Yeung Jr.
Patrick P. Yeung Jr. Ian Logan2
Ian Logan2