- 1Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
- 2Center for Research on Ethnicity, Culture, and Health, School of Public Health, University of Michigan, Ann Arbor, MI, USA
- 3Medicine and Health Promotion Institute, Tehran, Iran
Purpose: Although the link between education and alcohol consumption is known, limited information exists on racial differences in this link. We conducted the current study to test Black–White differences in the association between education and alcohol consumption among older adults in the U.S.
Methods: This cross-sectional survey enrolled 1,493 Black (n = 734) and White (n = 759) older adults (age 66 or more) in U.S. Data came from the Religion, Aging, and Health Survey, 2001. Race, demographics, socioeconomics, and alcohol consumption were measured. Independent variable was education level. Outcome was alcohol consumption. Race was the focal moderator. Logistic regression was used for data analysis.
Results: Education was positively associated with ever drinking in the pooled sample. However, race interacted with education level on drinking, suggesting a smaller effect of education on drinking for Blacks compared to Whites. Among Whites, high-school graduation and college graduation were associated with increased odds of ever drinking, net of covariates. Among Blacks, high-school graduation, but not college graduation, was associated with ever drinking.
Conclusion: Blacks and Whites differ in how socioeconomic status (i.e., education) shapes behaviors, especially health behaviors (i.e., drinking). How race modifies consequences and correlates of social determinants of health is not yet clear. College graduation may result in the same level of change to the social network and income of race group members. Weaker effect of education on health of Blacks may be due to the structural role of race and racism that has resulted in lower job availability and pay for Blacks.
Introduction
Alcohol research literature has shown a U-shaped relationship between alcohol consumption and mortality risk, suggesting that alcohol consumption is associated with desired and undesired health outcomes, depending on the pattern of use. While compared with those who rarely or never drink, consuming up to one drink per day reduces the mortality risk (1); heavy alcohol use is a major risk factor for premature mortality (2, 3). Among older adults, low-to-moderate alcohol consumption also reduces overall mortality (4). By documenting the most favorable mortality profile for the individuals who consume two to six drinks per week and the most unfavorable mortality profile for those who consume two or more drinks per day, Camargo et al. concluded that “the difference between consumption of small and large amounts of alcohol consumption means the difference between preventing and causing excess mortality” (5).
Alcohol-related mortality is more common among lower socioeconomic status (SES) groups (2). Alcohol-related deaths are in fact major contributors to the SES disparities in premature mortality (3, 6). As differences between SES groups in alcohol-related mortality are larger than the differences in the pattern of use, SES is believed to be a vulnerability factor for the effects of alcohol use (7). That is low SES populations have higher vulnerability to the undesired outcomes associated with excessive alcohol use (7).
Drinking patterns and drinking outcomes are both shaped by the individuals’ SES (8–10). Education (11), employment (12), and financial capacity (13) determine pattern and frequency of alcohol use. Most studies have documented positive effects of education and income on risk of being an ever or current drinker. Compared to abstainers and heavy drinkers, moderate drinkers tend to enjoy higher SES and less frequently suffer alcohol-related problems (8–13).
Similar to many other parts of the world, SES is a major social determinant of drinking in American society (14, 15). In the U.S., the proportion of current drinkers increases with education and income (15), with some research reporting a U-shaped relationship between income and average daily alcohol consumption (16). Compared with consistent drinkers, consistent abstainers have lower educational levels, and lower incomes are more often unemployed. Greater alcohol consumption is also associated with having a higher educational level and having a higher income (17). Lower income predicts a larger decline in drinking levels over time among Americans (17). In the college sample, educational achievement is positively associated with drinking (18). While inconsistent findings have been also reported (16), most studies suggest that lower SES groups drink heavier quantities, while higher SES groups drink more frequently but less quantity (10).
Race and ethnicity also influences the pattern of alcohol use in the U.S. (14). While Blacks begin regular alcohol use later than Whites, they move more rapidly from initiation of regular alcohol use to problem use, a phenomenon called telescoping (14). In the U.S., the proportion of current drinkers is lower than average among Black adults (15). While consistent abstainers are more frequently Blacks, more Whites are consistent drinkers than Blacks (19). According to a study in the U.S. compared to Blacks, Whites have a higher tendency to drink at restaurants, bars, clubs, or organizational meetings. Blacks more frequently than Whites drink in public settings such as parks, streets, and parking lots (20). Latent class analysis of 4,646 older current drinkers from the National Epidemiologic Survey on Alcohol and Related Conditions showed that Blacks had lower prevalence of being a moderate-risk drinker (21). At the same time, Blacks are more likely to be in the high-risk drinking class, if they drink (21), and older Black alcoholics suffer greater undesired medical and psychosocial outcomes (22).
In the U.S., race is one of the main determinants of employment opportunities and employer choices (23–25). Structural inequalities due to race exist in the labor market preferences in the U.S. (26). Sociology and economics literature has shown wage inequality (27) and occupational segregation based on race. Particularly for individuals with the highest levels of education, differences in average income of Blacks and Whites reflect a huge racial gap in how education is being translated to health of minorities in the U.S. (28).
In addition to different employment opportunity, profits for equal jobs are different for Blacks and Whites, a phenomenon called Black–White pay gaps (29). Some of the limited job opportunities for Blacks are also due to racial residential segregation, which is against job proximity for Black neighborhoods (30). Lower school quality where Blacks live is another cause for differential effect of schooling on wages and employment opportunities (31). For example, in 2006, Black men with a master’s degree earned $27,000 less than Whites with the same education (28).
The protective effect of education on health is conditional on the availability of other resources – such as income and wealth – which are under influence of race (32–34).1 The ability of an individual to translate their socioeconomic resources into better health depends on demographic characteristics such as race (35–38). In other words, race and social class alter the health gain associated with education attainment (35–39).
Race changes the health effects of education (40). Williams argued that the effects of race and SES on mortality are not additive, but multiplicative (35). Thus, health should be conceptualized as the outcome of the interaction between race and a wide range of factors, such as education and income, that almost always place Blacks at more social and economic disadvantages (35). Our findings showed that race changes the effect of education on drinking, which in line with previous research suggests that the effects of race and SES are multiplicative other than additive.1
Based on the differential effect hypothesis (41), correlates of psychosocial and behaviors factors – that ultimately shape health and illness of population – are not universal but specific to populations. According to this theory, effects of risk and protective factors are shaped by a wide range of contextual factors such as race, ethnicity, gender, and place. Similar to other behaviors, drinking also has group-specific antecedents and consequences, which vary among Whites and Blacks (42–51). Using this conceptual model, we conducted the current study to compare Blacks and Whites for the association between education attainment and drinking behavior of older adults. To provide results that are generalizable to the U.S., we used a nationally representative cohort of older Americans.
Materials and Methods
Design and Setting
This was a cross-sectional study with 3 years of follow-up data. Data came from Wave 1 of the Religion, Aging, and Health Survey, 2001, a nationally representative household survey of Black and White older adults in the U.S. (52).
Ethics
The study protocol was approved by the University of Michigan Institutional Review Board (IRB). All participants provided consent. Data were collected anonymously.
Sampling and Participants
The study only included White or Black older adults. All participants were non-institutionalized English-speaking people of age more than 65 years. The study population was limited to Christians or those who were never associated with any faith. Older Blacks were oversampled in the survey.
Measures
Age (continuous measure), gender (female = 1, male = 0), race (Blacks = 1, Whites = 0), income (continuous measure), education (a three-level ordinal variable), and drinking (binary outcome) were measured.
Education
Following items were used to measure education: (1) did you get a high-school diploma or pass the high-school equivalency test? and (2) did you graduate from college and receive a bachelor’s degree? We treated our education variable as a three-level categorical variable: (0) less than high-school diploma [reference group], (1) completed high-school diploma, and (2) graduated from college.
Income
Participants were asked: here is a card showing amounts of yearly income. Into which of these groups did (your/your family’s) total income, from all sources, fall last year, 2000, before taxes? Responses included (1) less than $5,000, (2) $5,001–$9,999, (3) $10,000–$14,999, (4) $15,000–$19,999, (5) $20,000–$24,999, (6) $25,000–$29,999, (7) $30,000–$39,999, (8) $40,000–$59,999, (9) 60,000–$79,999, and (10) $80,000+. This variable was operationalized as a continuous measure, ranging from 1 to 10.
Drinking
Three items were used to assess drinking behavior. Items included (1) do you ever drink beer, wine, or liquor?, (2) during the last month, on how many days did you drink beer, wine, or liquor?, and (3) on the days you drink, how many cans of beer, glasses of wine, or drinks of liquor do you usually have? Our main outcomes were ever drinking, current drinking (last month), and problem drinking (5+ drinks per day), treated as three separate binary outcomes. Similar items have been shown to provide valid and reliable measures to study drinking patterns (53–55).
Statistical Analysis
We used SPSS 20.0 for data analysis. We fitted logistic regressions in the pooled sample (IBM Inc., Armonk, NY, USA), and specific to race, with education (socioeconomics) as the independent variable, ever drinking as the outcome, demographics (age and gender) as the covariates, and race as the focal moderator. We did not fit models for problem drinking as outcome, due to very limited number of individuals who reported five or more drinks per day. Odds ratios with 95% confidence intervals (CI) were reported.
Results
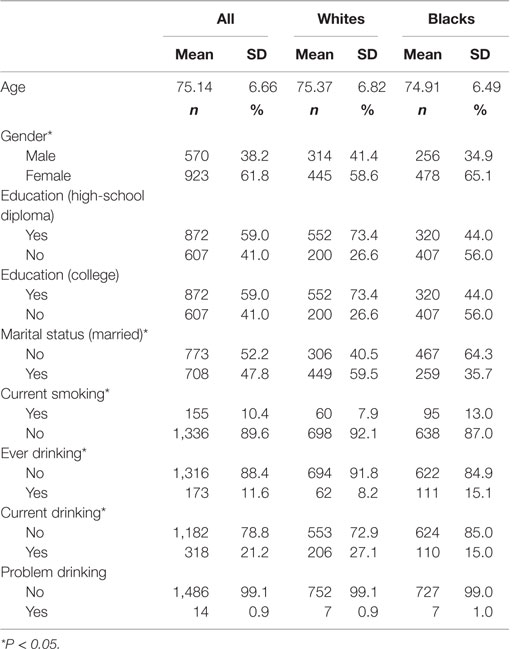
The study enrolled 1,493 older individuals (age 65 or more). This number is composed of Blacks (n = 734) and Whites (n = 759). Table 1 presents descriptive statistics overall and also based on race. While age was not significantly different between Blacks and Whites, Blacks were more likely female, had lower education, were less frequently married, more frequently smoked, and less frequently reported ever drinking.
Table 2 shows the results of logistic regressions in the pooled sample, with and without the interaction terms. Higher education was associated with higher odds of ever drinking. We also found a significant interaction between race and education level on odds of ever drinking, suggesting a smaller effect of higher education on drinking for Blacks compared to Whites.
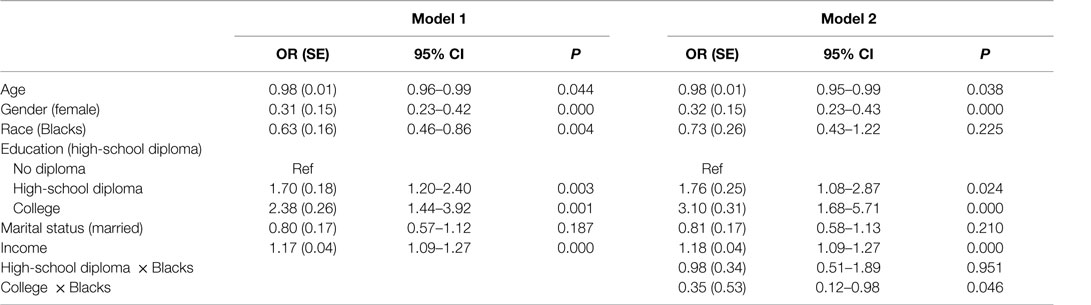
Table 2. The association between baseline high-school graduation and college graduation with drinking in the pooled sample (n = 1,439).
Table 3 provides a summary of the associations between education and ever drinking among Blacks and Whites. Among Whites, high-school graduation and college graduation were both associated with increased odds of ever drinking, net of covariates. Compared to lowest education level, high-school graduation was associated with higher odds of ever drinking. The same association could not be found for college graduation among Blacks (Table 3).
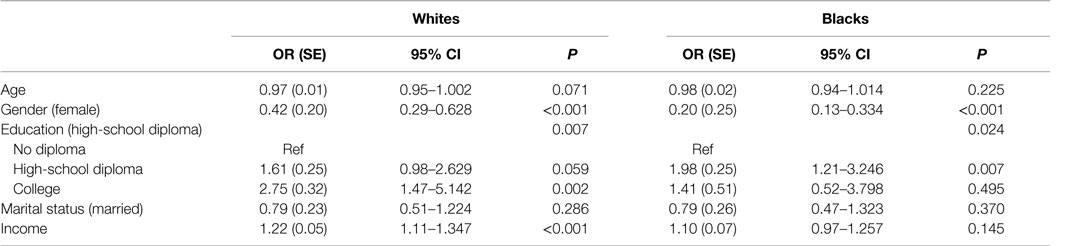
Table 3. The association between baseline high-school graduation and college graduation with drinking among Whites (n = 759) and Blacks (n = 734).
Discussion
Higher education was associated with higher odds of ever drinking among American older adults. Education level interacted with race on odds of ever drinking, suggesting a smaller effect of highest education level on ever drinking for Blacks compared to Whites. While among Whites, high-school graduation and college graduation were both associated with increased odds of ever drinking, high-school graduation, but not college graduation, was associated with higher odds of ever drinking among Blacks.
Although Mirowsky and Ross have described the effect of education on health as “enduring, consistent, and growing” (56), there are Black–White differences in the effect of education on health. In a study by Hayward et al., Whites showed an effect of education on mortality, while there was almost no association for Blacks (57). Backlund et al. found that while for Whites, each additional year of education had a stronger effect on decreasing mortality for those with a high-school diploma, for Blacks, there were step reductions in mortality at 12 and 16 years of education, with constant slopes between the steps (58). Everett et al. also showed race differences in the effect of education on mortality (37).
Findings of the current study on the stronger association between highest level of education and ever drinking for White compared to Black older adults may be due to the labor market preference for Whites, which lowers the effects of education in changing life style, behaviors, social network, and social norms of Blacks (59), which is in part due to unequal opportunities in education and employment (60). Labor market discrimination against Blacks, particularly Black men, is well known (61). According to the dual market theory, jobs are roughly divided into two groups: primary jobs are those with relatively high wages, good working conditions and opportunities for advancement into higher paying jobs; secondary jobs are those with low wages, bad working conditions, unstable employment, and minimal opportunity for advancement (62). Most Blacks and other minorities work on secondary jobs, if they obtain any employment (63).
Diminishing returns hypothesis suggests that racial disparity is largest at the highest SES levels, because with each level of increase in SES level, Blacks gain less improvement in health than Whites (64). Racial differences are not the same at low versus high SES levels (65). College attendance has shown to have a smaller effect on changing the life circumstances and behaviors of Blacks, as they less frequently afford to leave town to go to college (66). Similar to the previous research (32–34, 67) showing group differences in the health benefits of education, Assari et al. and others (40) found that the protective effects of education against mortality may not be uniform across population groups.
This study helps us understand how race and ethnicity alter how SES, behaviors, and health cluster (41–51). A growing literature has documented weaker role of a number of psychosocial factors, such as depressive symptoms, SRH, hostility, and other psychosocial outcomes on risk of mortality of Blacks compared to Whites (68–70). Previous research has shown that race and ethnicity alter the effects of SES on mortality (71–73). Race-specific role of SES may be a consequence of racial differences in distribution of risk and protective factors that influence physical health and mental health. Thus, SES may differently represent vulnerabilities to the effects of risk and protective factors (68–71). In addition, contextual factors, such as race and ethnicity, shape additive effects of SES, depression, and physical health even when their separate effects are similar (49, 74). Finally, psychosocial and subjective health indicators do not necessarily reflect same aspects of health across populations (74, 75).
Our study is subject to a number of limitations. First, we used a cross-sectional design, which does not allow causal inferences. There is a need for additional longitudinal studies that follow individuals over time. Second, drinking was measured using three single-item measures, not a standardized scale. We do not have information on alcohol use-related disorders (e.g., abuse or dependence) that require diagnosis by a clinician or detailed structured interview. Third, although some covariates were controlled, we did not control for other potential covariates, including health, function, mood, and access to medical care. Lack of data on cognitive function was another limitation. This is particularly important given the protective effects of light-to-moderate alcohol consumption against dementia and cognitive decline in older adults (76–78). Despite the above limitations, this is one of the first studies to document Black–White differences in the role of SES on drinking behavior of older adults in the U.S. Using a representative sample was the other strength of this study. Our findings have implications for racial health disparities in the U.S., given the higher burden of alcohol-related problems among Blacks (79).
Overall, our findings suggest that Black–White differences exist in the association between college graduation and drinking among older adults in the U.S. Further research is needed to better understand the mechanisms behind race and ethnic differences in behavioral correlates of SES.
Ethics
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants who were included in the study. University of Michigan Institutional Review Board (IRB) approved the study protocol.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants who were included in the study.
Author Contributions
SA designed and analyzed this work, and contributed to draft and revision. ML contributed to design and revised the paper. All authors confirmed the last version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
SA is supported by the Heinz C. Prechter Bipolar Research Fund and the Richard Tam Foundation at the University of Michigan Depression Center.
Funding
The Religion, Aging, and Health Survey was supported by National Institute on Aging (R01 AG014749, PI: Neal Krause), and per the NIH Public Access Policy requires that peer-reviewed research publications generated with NIH support are made available to the public through PubMed Central. NIH is not responsible for the data collection or analyses represented in this article. Data was accessed through The Inter-university Consortium for Political and Social Research (ICPSR), the Institute of Social Research, University of Michigan.
Footnote
- ^Assari S, Racial disparities in the link between education and mortality in United States. JAMA. (Under review, 2016).
References
1. Gaziano JM, Gaziano TA, Glynn RJ, Sesso HD, Ajani UA, Stampfer MJ, et al. Light-to-moderate alcohol consumption and mortality in the Physicians’ Health Study enrollment cohort. J Am Coll Cardiol (2000) 35(1):96–105. doi: 10.1016/S0735-1097(99)00531-8
2. Rehm J, Taylor B, Patra J. Volume of alcohol consumption, patterns of drinking and burden of disease in the European region 2002. Addiction (2006) 101:1086–95. doi:10.1111/j.1360-0443.2006.01491.x
3. Hemström Ö. Alcohol-related deaths contribute to socioeconomic differentials in mortality in Sweden. Eur J Public Health (2002) 12:254–62. doi:10.1093/eurpub/12.4.254
4. Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW Jr, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med (1997) 337(24):1705–14. doi:10.1056/NEJM199712113372401
5. Camargo CA Jr, Hennekens CH, Gaziano JM, Glynn RJ, Manson JE, Stampfer MJ. Prospective study of moderate alcohol consumption and mortality in US male physicians. Arch Intern Med (1997) 157(1):79–85. doi:10.1001/archinte.157.1.79
6. Mäkelä P, Paljärvi T. Do consequences of a given pattern of drinking vary by socioeconomic status? A mortality and hospitalisation follow-up for alcohol-related causes of the Finnish Drinking Habits Surveys. J Epidemiol Community Health (2008) 62(8):728–33. doi:10.1136/jech.2007.065672
7. Mäkelä P, Koskinen S, Keskimäki I, et al. What underlies the high alcohol-related mortality of the disadvantaged: high morbidity or poor survival? J Epidemiol Community Health (2003) 57:981–6. doi:10.1136/jech.57.12.981
8. Marmot M. Inequality, deprivation and alcohol use. Addiction (1997) 92(Suppl):s13–20. doi:10.1080/09652149738123
9. Shimotsu ST, Jones-Webb RJ, Lytle LA, MacLehose RF, Nelson TF, Forster JL. The relationships among socioeconomic status, fruit and vegetable intake, and alcohol consumption. Am J Health Promot (2012) 27(1):21–8. doi:10.4278/ajhp.110311-QUAN-108
10. Huckle T, You RQ, Casswell S. Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction (2010) 105(7):1192–202. doi:10.1111/j.1360-0443.2010.02931.x
11. Droomers M, Schrijvers CTM, Stronks K, van de Mheen D, Mackenbach JP. Educational differences in excessive alcohol consumption: the role of psychosocial and material stressors. Prev Med (1999) 29:1–10. doi:10.1006/pmed.1999.0496
12. Hemmingsson T, Lundberg I, Romelsjö A, Alfredsson L. Alcoholism in social classes and occupations in Sweden. Int J Epidemiol (1997) 26:584–91. doi:10.1093/ije/26.3.584
13. Brinkley GL. The causal relationship between socioeconomic factors and alcohol consumption: a granger-causality time series analysis, 1950–1993. J Stud Alcohol (1999) 60:759–68. doi:10.15288/jsa.1999.60.759
14. Johnson PB, Richter L, Kleber HD, McLellan AT, Carise D. Telescoping of drinking-related behaviors: gender, racial/ethnic, and age comparisons. Subst Use Misuse (2005) 40(8):1139–51. doi:10.1081/JA-200042281
15. Dawson DA, Grant BF, Chou SP, Pickering RP. Subgroup variation in U.S. drinking patterns: results of the 1992 national longitudinal alcohol epidemiologic study. J Subst Abuse (1995) 7(3):331–44. doi:10.1016/0899-3289(95)90026-8
16. Keyes KM, Hasin DS. Socio-economic status and problem alcohol use: the positive relationship between income and the DSM-IV alcohol abuse diagnosis. Addiction (2008) 103(7):1120–30. doi:10.1111/j.1360-0443.2008.02218.x
17. Brennan PL, Schutte KK, Moos RH. Patterns and predictors of late-life drinking trajectories: a 10-year longitudinal study. Psychol Addict Behav (2010) 24(2):254–64. doi:10.1037/a0018592
18. Slutske WS. Alcohol use disorders among US college students and their non-college-attending peers. Arch Gen Psychiatry (2005) 62:321–7. doi:10.1001/archpsyc.62.3.321
19. Moore AA, Gould R, Reuben DB, Greendale GA, Carter MK, Zhou K, et al. Longitudinal patterns and predictors of alcohol consumption in the United States. Am J Public Health (2005) 95(3):458–65. doi:10.2105/AJPH.2003.019471
20. Caetano R, Herd D. Drinking in different social contexts among white, black, and Hispanic men. Yale J Biol Med (1988) 61(3):243–58.
21. Sacco P, Bucholz KK, Spitznagel EL. Alcohol use among older adults in the National Epidemiologic Survey on Alcohol and Related Conditions: a latent class analysis. J Stud Alcohol Drugs (2009) 70(6):829–38. doi:10.15288/jsad.2009.70.829
22. Gomberg ESL, Nelson BW. Black and white older men: alcohol use and abuse. In: Beresford TP, Gomberg E, editors. Alcohol and Aging. New York: Oxford University Press (1995). p. 307–23.
23. Spalter-Roth R. Race and ethnicity in the labor market; employer practices and worker strategies. In: Hernan V, Feagin JR, editors. Handbooks of the Sociology of Racial and Ethnic Relations. USA: Springer (2007). p. 263–83.
24. Altonji JG, Blank RM. Race and gender in the labor market. In: Ashenfelter O, Card D, editors. Handbook of Labor Economics. Vol. 3C. Amsterdam: Elsevier Science (1999). p. 3143–259.
25. Proudford KL, Nkomo S. Race and ethnicity in organizations. In: Konrad A, Prasad P, Pringle J, editors. Handbook of Workplace Diversity. London: SAGE (2006). p. 323–44.
26. Grodsky E, Pager D. The structure of disadvantage: individual and occupational determinants of the black-white wage gap. Am Sociol Rev (2001) 66(4):542–67. doi:10.2307/3088922
27. Huffman ML, Cohen PN. Racial wage inequality: job segregation and devaluation across US labor markets. AJS (2004) 109(4):902–36. doi:10.1086/378928
28. IWPR. Importance of Social Security by Gender, Race/Ethnicity, and Marital Status. The Institute for Women’s Policy Research (IWPR) (2010). [accessed March 2016]. Available from: http://www.iwpr.org/publications/pubs/importance-of-social-security-by-gender-race-ethnicity-and-marital-status-2010
29. Tomaskovic-Devey D. The gender and race composition of jobs and the male/female, white/black pay gaps. Soc Forces (1993) 72(1):45–76. doi:10.1093/sf/72.1.45
30. Jencks C, Mayer SE. Residential Segregation, Job Proximity, and Black Job Opportunities. Inner-City Poverty in the United States. Washington, DC: National Academy Press (1990). p. 187–222.
31. Grogger J. Does school quality explain the recent black/white wage trend? J Labor Econ (1996) 14(2):231–53. doi:10.1086/209810
32. Montez JK, Hayward MD, Brown DC, Hummer RA. Why is the educational gradient of mortality steeper for men? J Gerontol B Psychol Sci Soc Sci (2009) 64(5):625–34. doi:10.1093/geronb/gbp013
33. Zajacova A, Hummer RA. Gender differences in education effects on all-cause mortality for white and black adults in the United States. Soc Sci Med (2009) 69(4):529–37. doi:10.1016/j.socscimed.2009.06.028
34. Amin V, Behrman JR, Spector TD. Does more schooling improve health outcomes and health related behaviors? Evidence from U.K. twins. Econ Educ Rev (2013) 35:134–48. doi:10.1016/j.econedurev.2013.04.004
35. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci (2010) 1186(1):69–101. doi:10.1111/j.1749-6632.2009.05339.x
36. Crimmins EM, Hayward MD, Seeman TE. Race/ethnicity, socioeconomic status, and health. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press (2004). p. 310–52.
37. Everett BG, Rehkopf DH, Rogers RG. The nonlinear relationship between education and mortality: an examination of cohort, race/ethnic, and gender differences. Popul Res Policy Rev (2013) 32(6):893–917. doi:10.1007/s11113-013-9299-0
38. Montez JK, Hummer RA, Hayward MD, Woo H, Rogers RG. Trends in the educational gradient of US adult mortality from 1986 through 2006 by race, gender, and age group. Res Aging (2011) 33(2):145–71. doi:10.1177/0164027510392388
39. Mackenbach JP, Kulhánová I, Bopp M, Deboosere P, Eikemo TA, Hoffmann R, et al. Variations in the relation between education and cause-specific mortality in 19 European populations: a test of the “fundamental causes” theory of social inequalities in health. Soc Sci Med (2015) 127:51–62. doi:10.1016/j.socscimed.2014.05.021
40. Annang L, Walsemann KM, Maitra D, Kerr JC. Does education matter? Examining racial differences in the association between education and STI diagnosis among black and white young adult females in the U.S. Public Health Rep (2010) 125(Suppl 4):110–21.
41. Assari S. Race and ethnic differences in additive and multiplicative effects of depression and anxiety on cardiovascular risk. Int J Prev Med (2016) 7(1):22. doi:10.4103/2008-7802.173931
42. Watkins DC, Assari S, Johnson-Lawrence V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. J Racial Ethn Health Disparities (2015) 2(3):385–94. doi:10.1007/s40615-015-0085-z
43. Assari S, Sonnega A, Pepin R, Leggett A. Residual effects of restless sleep over depressive symptoms on chronic medical conditions: race by gender differences. J Racial Ethn Health Disparities (2016). doi:10.1007/s40615-015-0202-z
44. Assari S, Lankarani MM, Burgard S. Black-white difference in long-term predictive power of self-rated health on all-cause mortality in United States. Ann Epidemiol (2016) 26(2):106–14. doi:10.1016/j.annepidem.2015.11.006
45. Assari S, Burgard S. Black-White differences in the effect of baseline depressive symptoms on deaths due to renal diseases: 25 year follow up of a nationally representative community sample. J Renal Inj Prev (2015) 4(4):127–34. doi:10.12861/jrip.2015.27
46. Assari S, Lankarani MM. The association between obesity and weight loss intention weaker among Blacks and men than Whites and women. J Racial Ethn Health Disparities (2015) 2(3):414–20. doi:10.1007/s40615-015-0115-x
47. Lankarani MM, Assari S. Association between number of comorbid medical conditions and depression among individuals with diabetes; race and ethnic variations. J Diabetes Metab Disord (2015) 7(14):56. doi:10.1186/s40200-015-0171-0
48. Assari S. Chronic medical conditions and major depressive disorder: differential role of positive religious coping among African Americans, Caribbean Blacks and Non-Hispanic Whites. Int J Prev Med (2014) 5(4):405–13.
49. Assari S. Separate and combined effects of anxiety, depression and problem drinking on subjective health among Black, Hispanic and Non-Hispanic White Men. Int J Prev Med (2014) 5(3):269–79.
50. Assari S, Lankarani MM, Lankarani RM. Ethnicity modifies the additive effects of anxiety and drug use disorders on suicidal ideation among Black adults in the United States. Int J Prev Med (2013) 4(11):1251–7.
51. Assari S, Burgard S, Zivin K. Long-term reciprocal associations between depressive symptoms and number of chronic medical conditions: longitudinal support for Black-White health paradox. J Racial Ethn Health Disparities (2015) 2(4):589–97. doi:10.1007/s40615-015-0116-9
52. Krause N. Religion, Aging, and Health Survey, 2001, 2004 [United States]. ICPSR03255-v2. Ann Arbor, MI: Inter-University Consortium for Political and Social Research [Distributor] (2006).
53. Barry AE, Chaney BH, Stellefson ML, Dodd V. Validating the ability of a single-item assessing drunkenness to detect hazardous drinking. Am J Drug Alcohol Abuse (2013) 39(5):320–5. doi:10.3109/00952990.2013.810745
54. Smith PC, Cheng DM, Allensworth-Davies D, Winter MR, Saitz R. Use of a single alcohol screening question to identify other drug use. Drug Alcohol Depend (2014) 139:178–80. doi:10.1016/j.drugalcdep.2014.03.027
55. Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med (2009) 24(7):783–8. doi:10.1007/s11606-009-0928-6
57. Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and U.S. adult mortality: implications for understanding education’s causal influence. Soc Sci Med (2015) 127:8–18. doi:10.1016/j.socscimed.2014.11.024
58. Backlund E, Sorlie PD, Johnson NJ. A comparison of the relationships of education and income with mortality: the National Longitudinal Mortality Study. Soc Sci Med (1999) 49(10):1373–84. doi:10.1016/S0277-9536(99)00209-9
59. Rosenfeld J, Kleykamp M. Organized labor and racial wage inequality in the United States. AJS (2012) 117(5):1460–502.
60. Annie E. Casey Foundation. Race Matters: Unequal Opportunities in Education (2006). Available from: http://www.aecf.org/resources/race-matters-1/
61. Reimers CW. Labor market discrimination against Hispanic and Black men. Rev Econ Stat (1983) 1:570–9. doi:10.2307/1935925
62. Doeringer PB, Piore MJ. Internal Labor Markets and Manpower Analysis. Lexington: Mass Health (1971).
64. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med (2005) 60(1):191–204. doi:10.1016/j.socscimed.2004.04.026
65. Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health (2004) 94(2):269–78. doi:10.2105/AJPH.94.2.269
66. Paschall MJ, Bersamin M, Flewelling RL. Racial/ethnic differences in the association between college attendance and heavy alcohol use: a national study. J Stud Alcohol (2005) 66(2):266–74. doi:10.15288/jsa.2005.66.266
67. Conti G, Heckman J, Urzua S. The education-health gradient. Am Econ Rev (2010) 100(2):234–8. doi:10.1257/aer.100.2.234
68. Ferraro KF, Kelley-Moore JA. Self-rated health and mortality among black and white adults: examining the dynamic evaluation thesis. J Gerontol B Psychol Sci Soc Sci (2001) 56(4):S195–205. doi:10.1093/geronb/56.4.S195
69. Lee SJ, Moody-Ayers SY, Landefeld CS, Walter LC, Lindquist K, Segal MR, et al. The relationship between self-rated health and mortality in older black and white Americans. J Am Geriatr Soc (2007) 55(10):1624–9. doi:10.1111/j.1532-5415.2007.01360.x
70. Dowd JB, Zajacova A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol (2007) 36(6):1214–21. doi:10.1093/ije/dym214
71. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA (2013) 309(1):71–82. doi:10.1001/jama.2012.113905
72. Patel AV, Hildebrand JS, Gapstur SM. Body mass index and all-cause mortality in a large prospective cohort of white and black US Adults. PLoS One (2014) 9(10):e109153. doi:10.1371/journal.pone.0109153
73. Capistrant BD, Gilsanz P, Moon JR, Kosheleva A, Patton KK, Glymour MM. Does the association between depressive symptoms and cardiovascular mortality risk vary by race? Evidence from the Health and Retirement Study. Ethn Dis (2013) 23(2):155.
74. Assari D, Dejman M, Neighbors HW. Ethnic differences in separate and additive effects of anxiety and depression on self rated mental health among Blacks. J Racial Ethn Health Disparities (2015). doi:10.1007/s40615-015-0154-3
75. Assari S, Moazen Zadeh E, Lankarani MM, Micol-Foster V. Race, depressive symptoms, and all-cause mortality in United States. Front Public Health (2016) 4:40. doi:10.3389/fpubh.2016.00040
76. Hendrie HC, Gao S, Hall KS, Hui SL, Unverzagt FW. The relationship between alcohol consumption, cognitive performance, and daily functioning in an urban sample of older black Americans. J Am Geriatr Soc (1996) 44(10):1158–65. doi:10.1111/j.1532-5415.1996.tb01364.x
77. Bachman DL, Green RC, Benke KS, Cupples LA, Farrer LA; MIRAGE Study Group. Comparison of Alzheimer’s disease risk factors in white and African American families. Neurology (2003) 60(8):1372–4. doi:10.1212/01.WNL.0000058751.43033.4D
78. Panza F, Frisardi V, Seripa D, Logroscino G, Santamato A, Imbimbo BP, et al. Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry (2012) 27(12):1218–38. doi:10.1002/gps.3772
Keywords: population groups, ethnic groups, African-Americans, socioeconomics, education, alcohol, drinking
Citation: Assari S and Lankarani MM (2016) Education and Alcohol Consumption among Older Americans; Black–White Differences. Front. Public Health 4:67. doi: 10.3389/fpubh.2016.00067
Received: 23 February 2016; Accepted: 28 March 2016;
Published: 21 April 2016
Edited by:
Haichang Xin, University of Alabama at Birmingham, USAReviewed by:
Francesco Panza, University of Bari Aldo Moro, ItalyHope Landrine, East Carolina University, USA
Copyright: © 2016 Assari and Lankarani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shervin Assari, YXNzYXJpQHVtaWNoLmVkdQ==
 Shervin Assari
Shervin Assari Maryam Moghani Lankarani
Maryam Moghani Lankarani