- 1Department of Epidemiology and Biostatistics, School of Public Health, Texas A&M Health Science Center, College Station, TX, USA
- 2Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, USA
- 3Department of Statistics, Texas A&M University, College Station, TX, USA
- 4Division of Health Systems Management and Policy, School of Public Health, The University of Memphis, Memphis, TN, USA
- 5Department of Health Promotion and Community Health Sciences, School of Public Health, Texas A&M Health Science Center, College Station, TX, USA
- 6National Council on Aging, Washington, DC, USA
- 7Stanford Patient Education Research Center, Department of Medicine, Stanford School of Medicine, Palo Alto, CA, USA
Background: The Chronic Disease Self-Management Program (CDSMP) has been widely disseminated among various racial and ethnic populations. In addition to the six required CDSMP workshop sessions, the delivery sites have the option to offer a Session Zero (or zero class), an information session offered prior to Session One as a marketing tool. Despite assumptions that a zero class is helpful, little is known about the prevalence of these additional sessions or their impact on retaining participants in CDSMP workshops. This study aims to describe the proportion of CDSMP workshops that offered Session Zero and examine the association between Session Zero and workshop completion rates.
Methods: Data were analyzed from 80,987 middle-aged and older adults collected during a two-year national dissemination of CDSMP. Generalized estimating equation regression analyses were conducted to assess the association between Session Zero and successful workshop completion (attending four or more of the six workshop sessions).
Results: On average, 21.04% of the participants attended workshops that offered Session Zero, and 75.33% successfully completed the CDSMP workshop. The participants of the workshops that offered Session Zero had significantly higher odds of completing CDSMP workshops than those who were not offered Session Zero (OR = 1.099, P = <0.001) after controlling for participants’ demographic characteristics, race, ethnicity, living status, household income, number of chronic conditions, and workshop delivery type.
Conclusion: As one of the first studies reporting the importance of an orientation session for participant retention in chronic disease management intervention projects, our findings suggest offering an orientation session may increase participant retention in similar translational efforts.
Introduction
In recent years, an increasing number of interventions have been deemed highly efficacious in the prevention and management of chronic diseases in randomized clinical trials (1). To disseminate the findings of those clinical trials, the critical next step is to examine whether the research-based studies can be translated into effective community-based programs that can recruit and retain large numbers of participants with various chronic diseases. Program retention is often a challenge in controlled clinical studies (2), but it can be even more pronounced in large-scale implementation efforts of community-based interventions (3–5). Participant attrition not only threatens the internal validity and statistical power of a project, but also compromises the intervention benefits received by participants because of the lack of adequate intervention dose (6, 7). Less rigorously controlled than clinical trials, translational efforts pose special challenges for participant engagement. For example, grand-scale translational intervention efforts typically allocate fewer resources to intensively track and follow-up with participants over time, which may impact retention success.
To address problems associated with participant attrition, a wide range of studies have investigated factors related to retaining participants in clinical trials and observational studies (8–15). A previous meta-analysis identified 12 basic themes for successful retention in longitudinal studies, which include community involvement, contact and scheduling methods, and financial incentives (16). To date, however, the strategies for successful retention in translational initiatives remain underexplored (17, 18).
The Chronic Disease Self-Management Program (CDSMP) has been introduced and widely disseminated into US communities as a method to empower patients to deal with their chronic conditions by enhancing their self-management skills (19). Drawing upon Social Learning Theory (20), CDSMP is an evidence-based, peer-led intervention consisting of six highly participative classes held for 2.5 h each, once a week, for six consecutive weeks (19). In addition to the six workshop sessions, some delivery sites are offering a Session Zero (or zero class), an information session offered prior to Session One as a marketing tool (21). The primary purpose of Session Zero is to provide an overview of the workshop, explain expectations for workshop participation, and confirm commitment of those who are interested in or have already registered for a workshop. This additional session also serves as an opportunity to collect baseline data from participants to alleviate administrative burden on workshop instructors and ensure time is not taken away from Session One of the workshop. Although designed as a recruitment tool, we believe that incorporating a Session Zero to CDSMP workshops may boost participant retention rates because those who were not firmly committed to the workshop might decide to opt out of the program at this time. The goals of the current study are to (1) describe the proportion of CDSMP workshops that offered Session Zero and (2) examine the association between Session Zero and workshop completion rates.
Materials and Methods
Data Source and Study Population
Data for this study were obtained from a two-year nationwide delivery of CDSMP as part of the American Recovery and Reinvestment Act of 2009 (i.e., Recovery Act) Communities Putting Prevention to Work: Chronic Disease Self-Management Program Initiative (22). The U.S. Administration on Aging led this initiative in collaboration with the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS) to support the translation of CDSMP in 45 states, Puerto Rico, and the District of Columbia (23). This initiative was executed between 2010 and 2012 to embed CDSMP delivery structures into statewide systems (22). Within the first two years of this initiative, more than 100,000 adults participated in 9305 workshops in 1234 U.S. counties (22). For this study, administrative records were utilized to determine whether or not a Session Zero was held. Data were analyzed from 80,987 participants aged 50 years or older whose programmatic records contained data about Session Zero attendance.
Measures
Dependent Variable
CDSMP workshop attendance was the dependent variable for this study. As defined by the program developers and used in a variety of studies (24, 25), successful completion was defined as when CDSMP participants attended four or more of the six workshop sessions (22, 26), excluding Session Zero.
Independent Variables
Whether or not a workshop offered a Session Zero was recorded administratively and included in the database along with workshop attendance. Participants’ actual attendance of a Session Zero was not recorded. If offered, the Session Zero was usually offered 1–4 weeks prior to the workshop and targeted those who had already registered or who might have shown an interest in the workshop. This orientation session was also used to recruit acquaintances and/or family members of those who already registered for the workshop. The specific content of Session Zero varied by site; however, all of them should have provided an overview of the CDSMP workshop and its expectations for participation. Session Zero may also be used to collect baseline data to reduce interference with Session One of the workshop.
Workshop delivery sites included area agencies on aging (AAAs), healthcare organizations, residential facilities, community or multipurpose centers, faith-based organizations, educational institution, county health department, tribal center, workplace, and other (e.g., recreational center).
Socio-demographic factors included age (in years), sex (male vs. female), median household income (in $10,000 units), and living arrangement (living with others vs. living alone). Participants’ health status was measured by their number of self-reported chronic conditions (i.e., arthritis, cancer, depression, diabetes, heart disease, hypertension, lung disease, stroke, osteoporosis, and other chronic conditions).
Statistical Analysis
To compare the characteristics of the participants who attended workshops with a Session Zero and those who attended workshops without a Session Zero, we used χ2 tests for categorical variables and two-sample t-tests for continuous variables. Because the participants were nested in workshops, generalized estimating equation (GEE) regression models were employed to investigate the association between successful workshop completion and Session Zero attendance. Specifically, the dependent variable of these regression models was successful workshop completion, while the independent variables were participant-level demographic and health characteristics. Furthermore, delivery site type was also included as an independent variable in the second GEE regression model. All the models included an exchangeable working covariance to account for the intraclass correlation among participants from the same workshop. Because the dependent variable is a binary variable; GEE analyses were conducted using SAS GENMOD procedure with a logit link function (SAS 9.3, SAS Institute, Inc., Cary, NC, USA).
Results
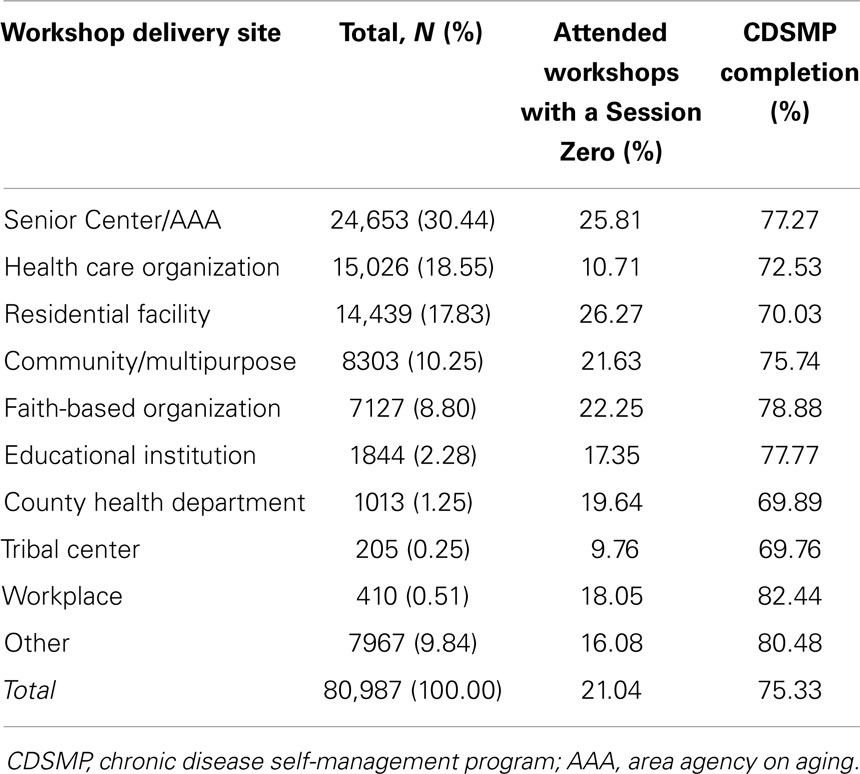
Table 1 shows the proportions of participants who attended Session Zero and the workshop completion rates among the 10 types of delivery sites. Overall, 21.04% of the participants attended workshops with a Session Zero and 75.33% of participants successfully completed the CDSMP workshop. Among the 10 different types of delivery sites, the largest proportion of participants attending workshops with a Session Zero were at residential facilities (26.27%), while the smallest proportion of participants attending workshops with a Session Zero were at tribal centers (9.76%). With respect to workshop completion rates, workplaces had the highest completion rate (82.44%) and tribal center had the lowest completion rate (69.76%).
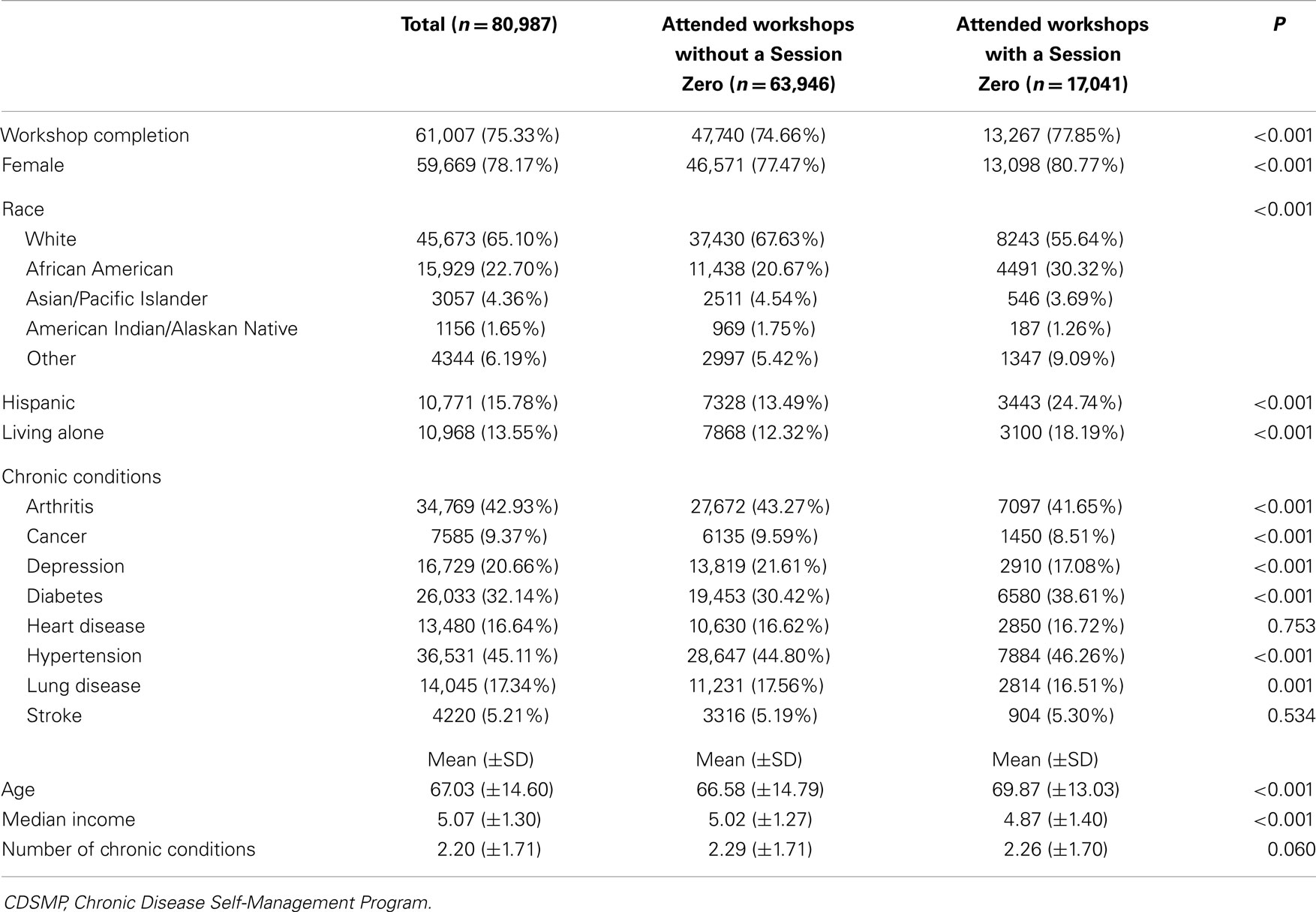
As presented in Table 2, CDSMP participants who attended workshops with a Session Zero had significantly higher workshop completion rate than those who attended workshops without a Session Zero (77.85% vs. 74.66%, P < 0.001). Participants who attended workshops with a Session Zero were more likely to be female, African American or other race group, Hispanic, and live alone. In terms of chronic conditions, they were more likely to have diabetes and hypertension, but less likely to have arthritis, cancer, depression, and lung disease. The average numbers of chronic conditions were not significantly different based on Session Zero status. Finally, the participants who attended workshops with a Session Zero were significantly older and had lower household incomes.
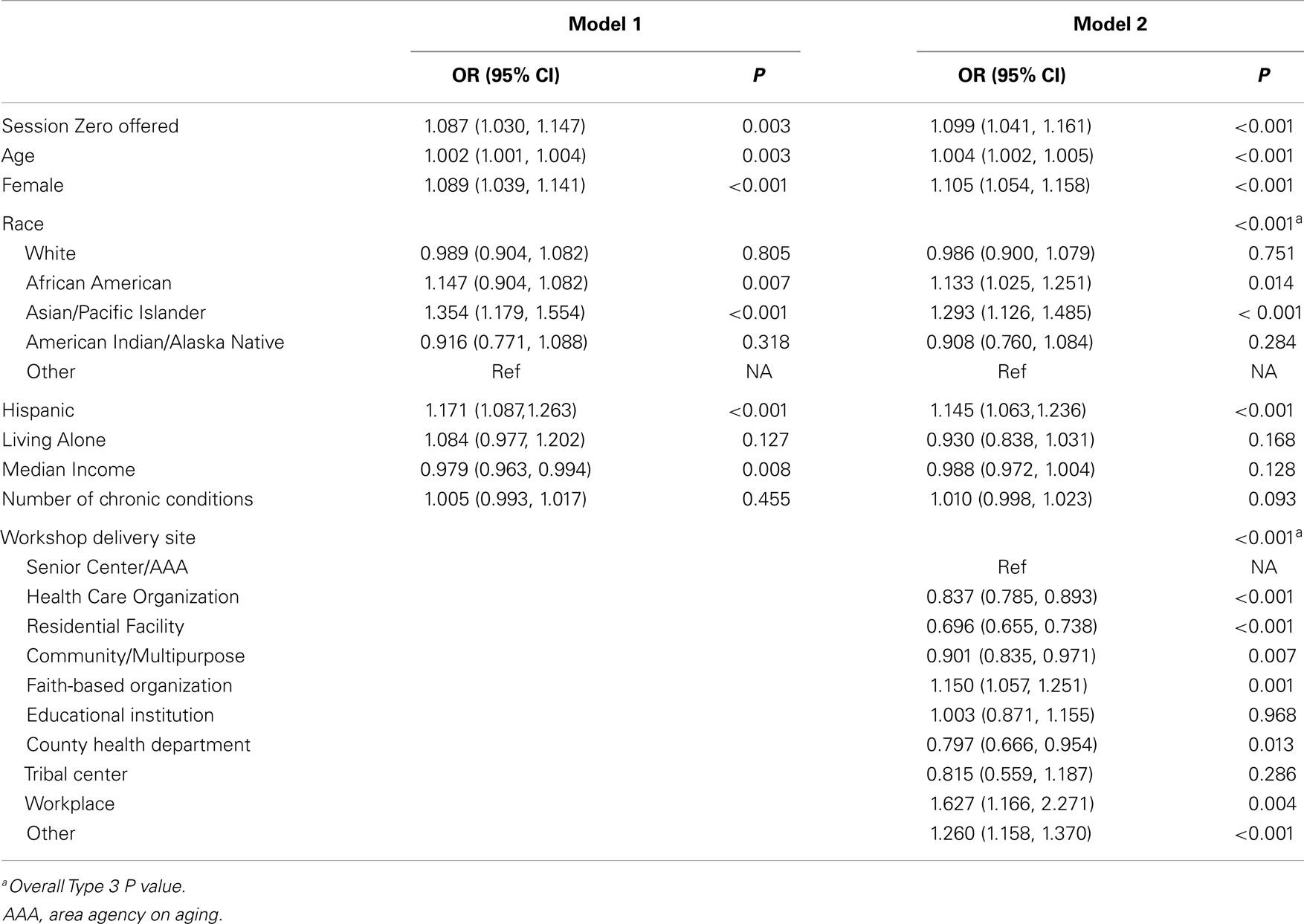
Table 3 illustrates the results of GEE regressions for workshop completion. As seen in Model 1, the participants of the workshops that offered Session Zero had significantly higher odds of completing CDSMP workshops than those who participated the workshops that did not offer a Session Zero (odds ratio [OR] = 1.087, P = 0.003). In addition, the likelihood of completing CDSMP workshops was higher among older participants (OR = 1.002, P = 0.003), females (OR = 1.089, P < 0.001), African Americans (OR = 1.147, P = 0.007), Asians and Pacific Islanders (OR = 1.354, P < 0.001), and Hispanics (OR = 1.171, P < 0.001). Conversely, the likelihood of completing the workshop was lower among those with higher household incomes (OR = 0.979, P = 0.008).
After adding types of delivery site into the GEE regression model (Model 2), we found participants of the workshops that offered Session Zero still had significantly higher odds of completing CDSMP workshops (OR = 1.099, P < 0.001). Furthermore, the average workshop completion rates were significantly different among different delivery site types (P < 0.001), with residential facility had the lowest likelihood of completing the workshop (OR = 0.696, P < 0.001) while workplace had the highest likelihood (OR = 1.627, P = 0.004).
Discussion
The results of the current study show about one in five CDSMP workshops in this national initiative offered a Session Zero. Among the 10 delivery site types, senior centers/AAAs and residential facilities had the highest rates of offering a Session Zero, while tribal centers and healthcare organizations had the lowest rates. These differences might be related to variation in population subgroups served by each delivery site type (27, 28), as well as site staff availability and facility constraints (e.g., space, time, competing commitments).
As suggested in a review of lessons learned from the National Institute of Aging’s Behavior Change Consortia (21), this study also demonstrates that participants who were offered orientation sessoins were more likely to complete intervention protocols. This finding indicates offering a Session Zero may not only facilitate participant recruitment, but also increase participant retention in grand scale community-based program dissemination efforts. Participants attending workshops with a Session Zero before the formal start of the workshop might have developed more support for and positive views of the program because they were given an opportunity to better understand the purpose, content, and expectations of the workshop. Meanwhile, attending a Session Zero may have given individuals who were not fully committed to the program a chance to re-evaluate their intention and opt out of the program if they felt they were not completely ready for it or thought it might not be beneficial for their preferences/needs. Therefore, the functions of a Session Zero with respect to retention might be twofold: (1) to strengthen the commitment of the participants by providing relevant information in advance and (2) to serve as a screening tool to identify those who are truly interested in the program and ready to participate. Future studies are warranted to study the details of these two potential functions of Session Zero.
Our results regarding the relationships between participants’ demographic characteristics and retention are consistent with the existing literature (11–13, 29–32). Specifically, we found that older participants and females had higher workshop completion rates. The relationship between race/ethnicity and participant retention in previous studies are mixed, although most report minority populations were harder to retain (33), some have reported relatively lower attrition rates among Hispanic participants (8, 10, 34). Here, we found that African American, Asian Pacific Islanders, and Hispanic participants had higher likelihood of completing the workshop successfully. Differences in CDSMP workshop attendance rates by participant demographics may have been reflective of the type of delivery site at which workshops were attended. Other studies have shown that certain delivery sites attract and serve different community subgroups (22, 27, 28). For example, better workshop attendance among older participants may reflect that larger proportions of older participants attend CDSMP workshops at residential facilities (also with higher attendance rates).
The strengths of this study include a large sample size and diverse race and ethnicity representation included in the analysis. The large sample not only allowed us to have high power to detect relatively small differences and associations, but also implies potential good generalizability of our findings. Furthermore, the study sample included 16% Hispanics, 23% African Americans, 4% Asian and Pacific Islanders, and 2% American Indian and Alaskan Natives. The substantial diversity of the sample composition further supports the generalizability of these study results.
Despite the study’s evident strengths, our findings need to be carefully interpreted in light of a few limitations. First, while data were collected that indicated whether or not workshops offered a Session Zero, participant attendance in these zero class sessions was not recorded. This means that participant attendance in a Session Zero could not be directly linked to their workshop attendance data. Second, these results were based on observational data, which limit our ability to determine a causal relationship between Session Zero attendance and CDSMP completion. Third, the number of variables collected at baseline was relatively small; therefore, although we were able to control for several important participant characteristics in the regression analyses, the identified associations in this study may be confounded by other unmeasured variables. Last, we were not able to investigate the relationship between Session Zero attendance and changes in health- and healthcare-related outcomes among these CDSMP participants because outcome measures were not available in this data collection effort.
In summary, including a Session Zero when delivering CDSMP workshops may be an important strategy for participant retention. Our findings suggest hosting a Session Zero may have implications for workshop attendance in similar translational efforts involving evidence-based programs for older adults. Given potential challenges associated with retaining participants in grand scale community-based interventions, offering a Session Zero before the formal start of the intervention might represent a feasible and efficient two-prong approach to help with participant retention in future translational projects.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This paper is included in the Research Topic, “Evidence-Based Programming for Older Adults.” This Research Topic received partial funding from multiple government and private organizations/agencies; however, the views, findings, and conclusions in these articles are those of the authors and do not necessarily represent the official position of these organizations/agencies. All papers published in the Research Topic received peer review from members of the Frontiers in Public Health (Public Health Education and Promotion section) panel of Review Editors. Because this Research Topic represents work closely associated with a nationwide evidence-based movement in the US, many of the authors and/or Review Editors may have worked together previously in some fashion. Review Editors were purposively selected based on their expertise with evaluation and/or evidence-based programming for older adults. Review Editors were independent of named authors on any given article published in this volume.
Acknowledgments
This work was supported by the Administration on Aging [90OP0001/03] and the National Institute of Child Health and Human Development [R01HD047143].
References
1. Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and healthcare utilization outcomes of the chronic disease self-management program. Prev Chronic Dis (2013) 10:120112. doi:10.5888/pcd10.120112
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
2. Warner ET, Glasgow RE, Emmons KM, Bennett GG, Askew S, Rosner B, et al. Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: results and lessons learned. BMC Public Health (2013) 13:192. doi:10.1186/1471-2458-13-192
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
3. Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: findings from the women on the move study. Ethn Dis (2002) 12(2):242–51.
4. Coday M, Boutin-Foster C, Goldman Sher T, Tennant J, Greaney ML, Saunders SD, et al. Strategies for retaining study participants in behavioral intervention trials: retention experiences of the NIH behavior change consortium. Ann Behav Med (2005) 29(Suppl):55–65. doi:10.1207/s15324796abm2902s_9
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
5. Glasgow RE, Nelson CC, Kearney KA, Reid R, Ritzwoller DP, Strecher VJ, et al. Reach, engagement, and retention in an Internet-based weight loss program in a multi-site randomized controlled trial. J Med Internet Res (2007) 9(2):e11. doi:10.2196/jmir.9.2.e11
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
6. Mody L, Miller DK, McGloin JM, Freeman M, Marcantonio ER, Magaziner J, et al. Recruitment and retention of older adults in aging research. J Am Geriatr Soc (2008) 56(12):2340–8. doi:10.1111/j.1532-5415.2008.02015.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
7. King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. Am J Prev Med (1998) 15(4):316–33. doi:10.1016/S0749-3797(98)00085-3
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
8. Hessol NA, Schneider M, Greenblatt RM, Bacon M, Barranday Y, Holman S, et al. Retention of women enrolled in a prospective study of human immunodeficiency virus infection: impact of race, unstable housing, and use of human immunodeficiency virus therapy. Am J Epidemiol (2001) 154(6):563–73. doi:10.1093/aje/154.6.563
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Williams PL, Van Dyke R, Eagle M, Smith D, Vincent C, Ciupak G, et al. Association of site-specific and participant-specific factors with retention of children in a long-term pediatric HIV cohort study. Am J Epidemiol (2008) 167(11):1375–86. doi:10.1093/aje/kwn072
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. McGuigan WM, Katzev AR, Pratt CC. Multi-level determinants of retention in a home-visiting child abuse prevention program. Child Abuse Negl (2003) 27(4):363–80. doi:10.1016/S0145-2134(03)00024-3
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
11. O’Brien RA, Moritz P, Luckey DW, McClatchey MW, Ingoldsby EM, Olds DL. Mixed methods analysis of participant attrition in the nurse-family partnership. Prev Sci (2012) 13(3):219–28. doi:10.1007/s11121-012-0287-0
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
12. Anderson RT, Ory M, Cohen S, McBride JS. Issues of aging and adherence to health interventions. Control Clin Trials (2000) 21(5 Suppl):171S–83S. doi:10.1016/S0197-2456(00)00075-1
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
13. Brown DR, Fouad MN, Basen-Engquist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol (2000) 10(8 Suppl):S13–21. doi:10.1016/S1047-2797(00)00197-6
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
14. Manson SM, Jiang L, Zhang L, Beals J, Acton KJ, Roubideaux Y. Special diabetes program for Indians: retention in cardiovascular risk reduction. Gerontologist (2011) 51(Suppl 1):S21–32. doi:10.1093/geront/gnq083
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
15. Jiang L, Manson SM, Dill EJ, Beals J, Johnson A, Huang H, et al. Participant and site characteristics related to participant retention in a diabetes prevention translational project. Prev Sci (2014). doi:10.1007/s11121-013-0451-1
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
16. Robinson KA, Dennison CR, Wayman DM, Pronovost PJ, Needham DM. Systematic review identifies number of strategies important for retaining study participants. J Clin Epidemiol (2007) 60(8):757–65. doi:10.1016/j.jclinepi.2006.11.023
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
17. Rosal MC, White MJ, Borg A, Scavron J, Candib L, Ockene I, et al. Translational research at community health centers: challenges and successes in recruiting and retaining low-income Latino patients with type 2 diabetes into a randomized clinical trial. Diabetes Educ (2010) 36(5):733–49. doi:10.1177/0145721710380146
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
18. Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials (2009) 30(1):63–70. doi:10.1016/j.cct.2008.09.007
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
19. Lorig K, Holman H, Sobel D, Laurent D. Living a Healthy Life with Chronic Conditions: Self Management of Heart Disease, Arthritis, Diabetes, Asthma, Bronchitis, Emphysema and Others. 3rd ed. Boulder, CO: Bull Publishing Company (2006).
20. Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process (1991) 50(2):248–87. doi:10.1016/0749-5978(91)90022-L
21. Frank JC, Coviak CP, Healy TC, Belza B, Casado BL. Addressing fidelity in evidence-based health promotion programs for older adults. J Appl Geron (2008) 27(1):14–33. doi:10.1177/1090198114543007
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
22. Ory MG, Smith ML, Patton K, Lorig K, Zenker W, Whitelaw N. Self-management at the tipping point: reaching 100,000 Americans with evidence-based programs. J Am Geriatr Soc (2013) 61(5):821–3. doi:10.1111/jgs.12239
23. U.S. Department of Health and Human Services Administration on Aging. ARRA – Communities Putting Prevention to Work: Chronic Disease Self-Management Program 2012 April 15 (2014). Available from: www.cfda.gov/?s=program&mode=form&tab=step1&id=5469a61f2c5f25cf3984fc3b94051b5f
24. Ory MG, Ahn S, Jiang L, Smith ML, Ritter PL, Whitelaw N, et al. Successes of a national study of the chronic disease self-management program: meeting the triple aim of health care reform. Med Care (2013) 51(11):992–8. doi:10.1097/MLR.0b013e3182a95dd1
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
25. Standford University, Patient Education in the Department of Medicine. Available from: http://patienteducation.stanford.edu/programs/cdsmp.html
26. Ahn S, Basu R, Smith ML, Jiang L, Lorig K, Whitelaw N, et al. The impact of chronic disease self-management programs: healthcare savings through a community-based intervention. BMC Public Health (2013) 13(1):1141. doi:10.1186/1471-2458-13-1141
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
27. Smith ML, Belza B, Altpeter M, Ahn S, Dickerson JB, Ory MG. Disseminating an evidence-based disease self-management program for older Americans: implications for diversifying participant reach through delivery site adoption. In: Maddock J, editor. Public Health: Social and Behavioral Health. Rijeka, Croatia: InTech (2012). p. 385–404.
28. Smith ML, Ory MG, Ahn S, Belza B, Mingo CA, Towne Jr. SD, et al. Reaching diverse participants utilizing a diverse delivery infrastructure: a replication study. Front Public Health Educ Promot (2015) 3:77. doi:10.3389/fpubh.2015.00077
29. Bailey JM, Bieniasz ME, Kmak D, Brenner DE, Ruffin MT. Recruitment and retention of economically underserved women to a cervical cancer prevention trial. Appl Nurs Res (2004) 17(1):55–60. doi:10.1016/j.apnr.2003.12.002
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
30. Warren-Findlow J, Prohaska TR, Freedman D. Challenges and opportunities in recruiting and retaining underrepresented populations into health promotion research. Gerontologist (2003) 43(Spec No 1):37–46. doi:10.1093/geront/43.suppl_1.37
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
31. Chang MW, Brown R, Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low-income overweight and obese mothers. BMC Public Health (2009) 9:424. doi:10.1186/1471-2458-9-424
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
32. Gappoo S, Montgomery ET, Gerdts C, Naidoo S, Chidanyika A, Nkala B, et al. Novel strategies implemented to ensure high participant retention rates in a community based HIV prevention effectiveness trial in South Africa and Zimbabwe. Contemp Clin Trials (2009) 30(5):411–8. doi:10.1016/j.cct.2009.05.002
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
33. Probstfield JL, Frye RL. Strategies for recruitment and retention of participants in clinical trials. JAMA (2011) 306(16):1798–9. doi:10.1001/jama.2011.1544
Keywords: attrition, retention, orientation session, evidence-based programs, chronic disease self-management program
Citation: Jiang L, Smith ML, Chen S, Ahn S, Kulinski KP, Lorig K and Ory MG (2015) The role of Session Zero in successful completion of Chronic Disease Self-Management Program workshops. Front. Public Health 2:205. doi: 10.3389/fpubh.2014.00205
Received: 16 July 2014; Accepted: 07 October 2014;
Published online: 27 April 2015.
Edited by:
Sue Ellen Levkoff, University of South Carolina, USAReviewed by:
Xiaoguang Ma, University of South Carolina, USANilesh Chandrakant Gawde, Tata Institute of Social Sciences, India
Copyright: © 2015 Jiang, Smith, Chen, Ahn, Kulinski, Lorig and Ory. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luohua Jiang, Department of Epidemiology and Biostatistics, Texas A&M Health Science Center, 219 SRPH Administration Building, TAMU 1266, College Station, TX 77843-1266, USA e-mail:bGppYW5nQHNwaC50YW1oc2MuZWR1
 Luohua Jiang
Luohua Jiang Matthew Lee Smith
Matthew Lee Smith Shuai Chen
Shuai Chen SangNam Ahn
SangNam Ahn Kristie P. Kulinski
Kristie P. Kulinski Kate Lorig
Kate Lorig Marcia G. Ory
Marcia G. Ory