
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 19 March 2025
Sec. Anxiety and Stress Disorders
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1558085
This article is part of the Research Topic Bidirectional links between psychological trauma and physical symptoms: pathophysiology, diagnosis, prevention, and treatment View all 4 articles
Background: Exposure to potentially traumatic events (PTE) is associated with a range of negative mental health outcomes, including post-traumatic stress disorder (PTSD) and complex PTSD (cPTSD). Although exposure to PTEs is highly prevalent, and their impact on mental health is pervasive, research is mostly limited to diagnosed populations or specific trauma cohorts in the post-pandemic era.
Methods: We conducted an online survey of 1,000 Seoul residents from October 6-12, 2023, using a stratified sampling method. Participants were asked about their traumatic experiences, mental health outcomes, and experiences with mental health services.
Results: Most participants (98.8%) reported that they had experienced at least one PTE. The average number of PTEs reported was 9.19 (SD=7.908). Ninety participants (9%) were categorized as having probable PTSD (2.8% with PTSD only, and 6.2% with cPTSD). The sum of direct and indirect exposures to PTEs of individuals was associated with mental health outcomes, including PTSD symptom severity. Only 34.4% of patients with probable PTSD reported that they had received appropriate mental health services.
Conclusion: Our results suggest that PTE exposures are highly prevalent, and self-awareness of mental health conditions and utilization of mental health services are low in South Korea. Given the lasting effects of traumatic events and the large number of untreated cases, this study highlights the need for proactive responses to traumatic events and better access to short- and long-term services for traumatized individuals.
Potentially traumatic events (PTE) means various types of stressful events, which range in scope and form from natural disasters or accidents to human-caused disasters or violence. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; 1) suggests an exposure to actual or threatened death, serious injury, or sexual violence in one (or more) as a criterion A for PTSD. The International Classification of Diseases 11th Revision (ICD-11; 2) also suggests exposure to an extremely threatening or horrific event or series of events preceding the PTSD.
Exposure to PTE is associated with a range of negative mental health outcomes, including post-traumatic stress disorder (PTSD) and complex PTSD (cPTSD; 3) (2). Four out of 10 patients have chronic progress, suffering symptoms even after the first episode of PTSD (4). DSM-5 says that the expected lifetime probability of development of PTSD before 75 years old is 8.7%, and 12-month prevalence among adults is 3.5% in America according to DSM-IV criteria (1). Kilpatrick et al. (5) reported 8.3%, 4.7%, and 3.8% of lifetime, past-12-month, and past 6-month PTSD prevalence, respectively according to the DSM-5 criteria among national sample of U.S. adults. Previous research pooled 26 national surveys and estimated the global prevalence of PTSD as 3.9% in the general population and 5.6% in trauma-exposed populations in 2017 (6). Several studies have reported an increased prevalence of PTSD globally as high as 7% (7) and 15% (8) since the pandemic. In addition, PTSD is associated with an increased risk of comorbid major depressive disorder, substance use disorders, alcohol disorders, loneliness, suicide and suicidal ideation (9–14). The cPTSD argued by the ICD-11 working group requires additional features called disturbances in self-organization (DSO), including 1) affective dysregulation 2) negative self-concept and 3) disturbed relationships as well as three core elements of PTSD (re-experiencing; avoidance; and a persistent sense of threat) (2). The previous study reported greater dissociation, anger, difficulties related to moral injury, social isolation, and sleep problems with cPTSD than in PTSD (15).
Currently, several studies including Benjet et al. (16) have reported that exposure to PTEs are common not just among specific populations but also among the community sample (5, 17, 18). However, most previous studies have focused on specific trauma related populations such as combat veterans and refugees or patients with PTSD. Previous studies argued that it is necessary to pay attention to the subthreshold PTSD (19, 20). Research has shown that subthreshold PTSD symptoms were associated with suicidal ideation (20) and functional impairment (21). Fink et al. (19) showed that subthreshold PTSD had a potential risk of PTSD in future in their prospective-longitudinal study of cohort of military personnel.
PTE exposure is also common in South Korea. Chae (22) found that participants aged 20s to 50s experienced an average of 4.8 PTE types using Life Events Checklist for DSM-5 (LEC-5; 23). The lifetime prevalence of PTSD in South Korea has increased slightly from 1.4% in 2016 to 1.5% in 2021, according to the five-yearly Mental Health Status Survey (24). According to recent data, 14,464 people were diagnosed with PTSD in 2022 (25). Previous research in South Korea have reported prevalence of PTSD as 27.4% in victims of nature disaster, 60.91% in Cyber Sexual Assault Investigators, 75% in COVID-19 patients after recovery using Korean version of Impact of Event Scale - Revised (IES-R-K) with cutoff of 25 (26–29). Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) (30) showed 49.7% among community samples aged from 20s to 50s (22). However, most studies have focused on specific trauma-related cohorts or patients with PTSD, which makes generalization and subgroup analysis difficult. Also, to our knowledge, there is a lack of research examining both PTSD and cPTSD prevalence among community samples in South Korea. Although the International Trauma Questionnaire Korean version (ITQ-K) was validated in 2020 in Korean (31), most studies utilized DSM-5-based instruments (e.g., PTSD Checklist for DSM-5 (PCL-5) developed by Blevins et al. (32), translated and validated in Korean by Kim et al. (26)) to estimate the prevalence of PTSD in Korea. Therefore, most studies only reported the prevalence of PTSD and did not include cPTSD. In this study, we used the ITQ to examine the availability and prevalence of cPTSD in the Korean population.
Recently, there have been growing concerns about industrial accidents (33) and social disasters such as Seoul Halloween crowd crush (34). Furthermore, there were increasing reports of abnormal motive crimes also called as ‘mud-ji-ma’ (Don’t ask why in Korean) recently. The sudden stabbings or car rushing toward strangers in everyday public places, followed by many posts on the internet foreshadowing them, threatened not only the victims but also the whole society. It is also suggested that the general population may be more likely to be indirectly exposed to traumatic events through social media and the internet than before (35). Previous studies pointed out that psychological response to social disasters such as indirect trauma must be considered in trauma related study given the impact of indirect exposure to the traumatic events through various pathways (35–37).
Although exposure to PTEs is highly prevalent, and their impact on mental health is pervasive, research is mostly limited to diagnosed populations or specific trauma cohorts. Consequently, little is known about trauma exposure and mental health outcomes in the general population. Furthermore, as far as we are aware, no study has yet examined the prevalence of both PTSD and cPTSD and relationships with other mental disorders in Korea. Examining life experiences of PTE and related mental health outcomes among the general population may extend our understanding of the nature of PTE and PTSD beyond specific types of events and inform trauma interventions in the context of the general population.
The aim of the present study was to examine:
1. PTE exposures in the general population in Seoul, South Korea.
2. The prevalence and symptom severity of PTSD, cPTSD, and comorbidities.
3. Relationships between PTE, PTSD, and other mental health outcomes.
4. The use of mental health services among patients with probable PTSD and cPTSD.
We conducted an online survey from October 6 to 12, 2023. All participants were recruited via panel data, using a stratified sampling method. Sex, age, and residential area were stratified to ensure a representative sample of Seoul residents. All participants were Korean adults who lives in Seoul, South Korea and speaks Korean. In total, 1,000 participants (487 male and 522 female) responded to the survey.
Data was collected through an online panel company, Survey people. A separate online survey link was sent to participants who expressed interest in participating in the study through the company’s homegrown software, V3. All participants signed an informed consent form and were compensated with KRW 5,000 (approximately four dollars) after the survey. All data were anonymized to ensure that they did not contain any identifying information, and only a limited number of members of the research team (1st to 4th authors) were allowed access to the data via encrypted drives.
Since PTSD symptoms and descriptions of index trauma were assessed using self-reported measures, there is a potential risk of overestimating the prevalence of PTSD suggested by previous study (38, 39). At first, 236 participants showed significant PTSD symptom scores in ITQ. However, two of them reported that they had no events implying that their responses for symptom questions were not valid. Therefore, two people were excluded but still a prevalence of 23.4% in the general population not in a specialized cohort was too high, indicating the risk of overestimation. In addition to the two excluded individuals, there were others who reported responses that were difficult to consider traumatic events.
Rubin et al. (38) recommends that when measuring PTSD symptoms and estimating prevalence using self-report questionnaires rather than clinician interviews, at least three raters should rate the “index trauma” that meets DSM Criterion A and report on the initial kappa coefficient and consensus process to ensure that prevalence rates are not inflated. We have agreed to conduct additional ratings to address this issue. We aimed to 1) reduce miscommunication among researchers and international scholars due to differences in definitions from existing literature, and 2) reflect the meaning of trauma as defined in the existing literature. Since Kappa coefficient is usually used when there are two raters, and our team consisted of six raters, we used Cronbach’s alpha instead. We rated the trauma descriptions in the International Trauma Questionnaire (ITQ; 40) of those with significant PTSD symptom scores in ITQ (n=236). Three doctoral students, one master’s degree student, one clinical psychologist, and one trauma-specific clinical psychologist independently rated the index trauma and discussed disagreements. First, the research team discussed how to best define and evaluate the traumatic events before rating them. The definition of traumatic events followed the DSM-5 definition and criteria (specifically criterion A), and the types of events were complemented by the Korean version of the Posttraumatic Diagnostic Scale (PDS; 41, 42). Second, the first author excluded the responses that did not require ratings (None, don’t know, don’t want to tell, don’t want to recall, n=38), and created an anonymized rating sheet for 198 traumatic events. During the scoring process, researchers were blinded to any scores or information other than the traumatic event descriptions. Third, researchers independently rated traumatic events, whether the events were traumatic or not. The number of traumatic events met by each researcher ranged from 78 to 109, with good initial agreement and a Cronbach’s alpha of .924. Overall, 65 cases were rated as non-traumatic, and 59 cases were rated as traumatic. If a majority opinion was obtained (n=92), the final decision was made based on the rating of a trauma-specific clinician (n=85). If a trauma-specific clinician rated the event as traumatic but a majority of the six researchers did not agree, the event needed the agreement of another clinician to be classified as traumatic (n=5). Finally, 90 cases met the requirements of index trauma. Descriptions of the index trauma are not available due to privacy.
Participants were asked to answer about sex (male, female), age, living area, job status, marital status, education level, number of household members, and household income of past year.
The PTEs a person may have experienced were assessed using a self-reported version of the Life Events Checklist for DSM-5 (LEC-5; 23). This study used the Korean version of the LEC-5, translated and validated by Park et al. (43). For each PTE, participants could choose multiple responses from six nominal options: Happened to me; Witnessed it; Learned about it; Part of my job; Not sure; Doesn’t apply. Not sure and Doesn’t apply were recoded as not experienced in the analysis, while the other four selections were recoded as Experienced. Responses were dichotomized (1=Experienced or 0=Not experienced) when counting exposure to trauma or making subgroups according to the exposure. Participants were asked to choose the worst event that affected them and whether they successfully escaped or recovered from the event. Considering the impact of the pandemic on mental health, Death (of others) due to illness or infectious disease was added to the LEC-5 list. Verbal abuse was also included. Although verbal abuse is not considered a traumatic event in the DSM-5 criteria, accumulating evidence supports the need for research on emotional abuse, including verbal abuse, and that verbal forms of abuse often precede physical abuse (44). The participants were allowed to select multiple responses from 19 types of events. This study used the standard total score as a quantitative score of the LEC-5, which is most used in literature and has been shown to be the most reliable (45). Although this study added two more PTE types, when calculating the total of the LEC-5, only 17 original items counted for comparison with previous studies, resulting in a total score range of 0 to 51.
Self-reported PTSD symptoms were assessed with the International Trauma Questionnaire (ITQ; 40). The ITQ is a measure of ICD-11 PTSD and cPTSD. Cronbach’s α was.961. When an ITQ subscale was used as a continuous variable in the analysis, the subscale scores were summed. Based on previous research (46), the subfactors were organized into two factors, PTSD and DSO, and functional impairment was excluded.
The ITQ asks respondents to think of the worst experience (‘Please think of experience that troubles you most and answer the following questions in specific relation to this experience.’). We used Korean version of ITQ (31), which asks respondents to describe this experience in text and asks when it happened in six time points (6month; 6m to 12m; 1-5 years; 5-10 years; 10-20 years; 20+ years). To reduce the burden on respondents, we placed no restrictions on the format of description of the traumatic event; actual responses were reported as single words and as long as several sentences. These descriptions were later reviewed by the authors to determine whether each event qualified as a traumatic event.
Prior to the analysis, Confirmatory factor analysis (CFA) confirmed that the two-factor structure provided a good fit (CFI=.903, TLI=.880).
The Patient Health Questionnaire (PHQ-9), a nine-item questionnaire for assessing major depressive disorder, was developed by Kroenke et al. (47), and its Korean version was translated by Choi et al. (48) and validated by Park et al. (49). The PHQ-9 score was evaluated using a four-point Likert scale ranging from 0 (never) to 3 (almost always) according to the frequency of symptoms experienced in the preceding two weeks, and the sum was calculated. A total score of 10 out of 27 points is the cutoff for depression (48). Based on the total score, depression levels were categorized as 0-4 (no depression), 5-9 (light depression), 10-19 (moderate depression), and 20 or higher (severe depression). Cronbach’s α was.897.
The General Anxiety Disorder-7 (GAD-7), introduced by Spitzer et al. (50), is used to assess general anxiety disorders. The GAD-7 consists of seven items measuring the level of emotional disturbance experienced over the preceding two weeks, answered on a Likert scale ranging from 0 (never) to 3 (almost always). The anxiety level is classified as follows: 0-4 (not anxious), 5-9 (minor anxiety), 10-14 (moderate anxiety), and 15 or higher (severe anxiety) within the general population (51). Cronbach’s α was.929.
The Mental Health Screening Tool for Suicide Risk (MHS: S; 52) was used to evaluate suicide risk. The MHS: S comprises four questions answered on a Likert scale ranging from 0 (never) to 4 (always). Developed and validated using Item Response Theory, the MHS: S assigns specific weights to each response to calculate a cumulative score. Threshold scores for identifying individuals at risk and at high risk were established at total scores of 1 and 3, respectively (52). Cronbach’s α was.901.
The Alcohol Use Disorders Identification Test (AUDIT) is the most frequently used alcohol screening instrument. It was developed by the Saunders et al. (53), and the Korean version was adapted and validated by Lee (54). Comprising 10 questions, the AUDIT-KR includes three questions on alcohol dependence, three questions on harmful alcohol use, and four questions on hazardous alcohol intake. Hazardous alcohol intake is defined as a pattern of alcohol consumption that may lead to a range of physical, psychological, and social consequences, potentially imposing economic burdens on both individuals and society (54). The total score ranges from 0 to 40 points, with each question assigned a score of 0 to 4. A total score of 10 or higher for males and 6 or higher for females (8 or more for the general population) indicates risky alcohol use. Cronbach’s α was.922.
The Loneliness and Social Isolation Scale (LSIS), developed and validated by Hwang et al. (55), is a self-report measure that can objectively assess loneliness and social isolation simultaneously. Understanding social isolation as a complex phenomenon, LSIS encompasses social isolation comprehensively through three sub-factors: social support, social networks, and loneliness. Specifically, the LSIS consists of six items tailored to the Korean social and cultural context, with each item rated on a four-point Likert scale (ranging from 0=never to 3=Always). For each sub-factor, elevated scores reflect greater feelings of loneliness, reduced social support, and diminished social networks. Cronbach’s α was .753.
We designed a questionnaire asking about experiences with mental health services in one’s lifetime and in the past 12 months (e.g., Have you ever sought professional counseling (medical, professional counseling, health center, etc.) or treatment for a mental health problem, such as depressive symptoms, anxiety, sleep problems, or drinking problems throughout your life (including the present))?. Some items were adapted from national mental health surveys conducted by the National Center for Mental Health (57) and the Korea Institute of Health and Social Affairs (56). The questionnaire asked the participants about their use of mental health services, mental health concerns, the types of institutions visited (e.g., psychiatric hospitals, general hospitals, community mental health welfare centers, general welfare centers, health centers, psychological support centers, private psychotherapy centers), and the service received (e.g., medication, personal/group psychotherapy, general counseling, psychoeducation) in lifetime and in the past 12 months.
Data were analyzed using the SPSS Statistics 26. A total of 1,000 responses were analyzed. No data were missing. Factor analysis was conducted using Mplus 8.8. Exploratory Factor Analysis, and Confirmatory Factor Analysis identified the structure of each measurement. T-tests, ANOVA, and post-hoc comparisons using the Scheffe test were conducted using the SPSS Statistics 26.
Detailed demographic information of total sample, sample with probable PTSD and cPTSD is presented in Table 1.
We aimed to identify associations between demographic variables such as sex, age, and residential area and PTE experience and the development of PTSD and group differences. Independent t-tests and one-way ANOVA revealed that there were no significant differences in PTSD symptom severity according to demographic variables.
Of the 1,000 participants, 988 responded that they had experienced at least one of the stressful events in the LEC-5, either directly or indirectly. Among the participants who experienced PTEs (n=988), 42.4% reported that they had successfully escaped or recovered from the events, 12.9% did not, and 44.7% reported that they had recovered from the incident in some ways, but not in others. Among the 988 individuals with PTEs, ANOVA revealed significant differences in depression, anxiety, suicide risk, alcohol abuse, social isolation, PTSD, and DSO severity based on successful escape or recovery from the event (Table 2).
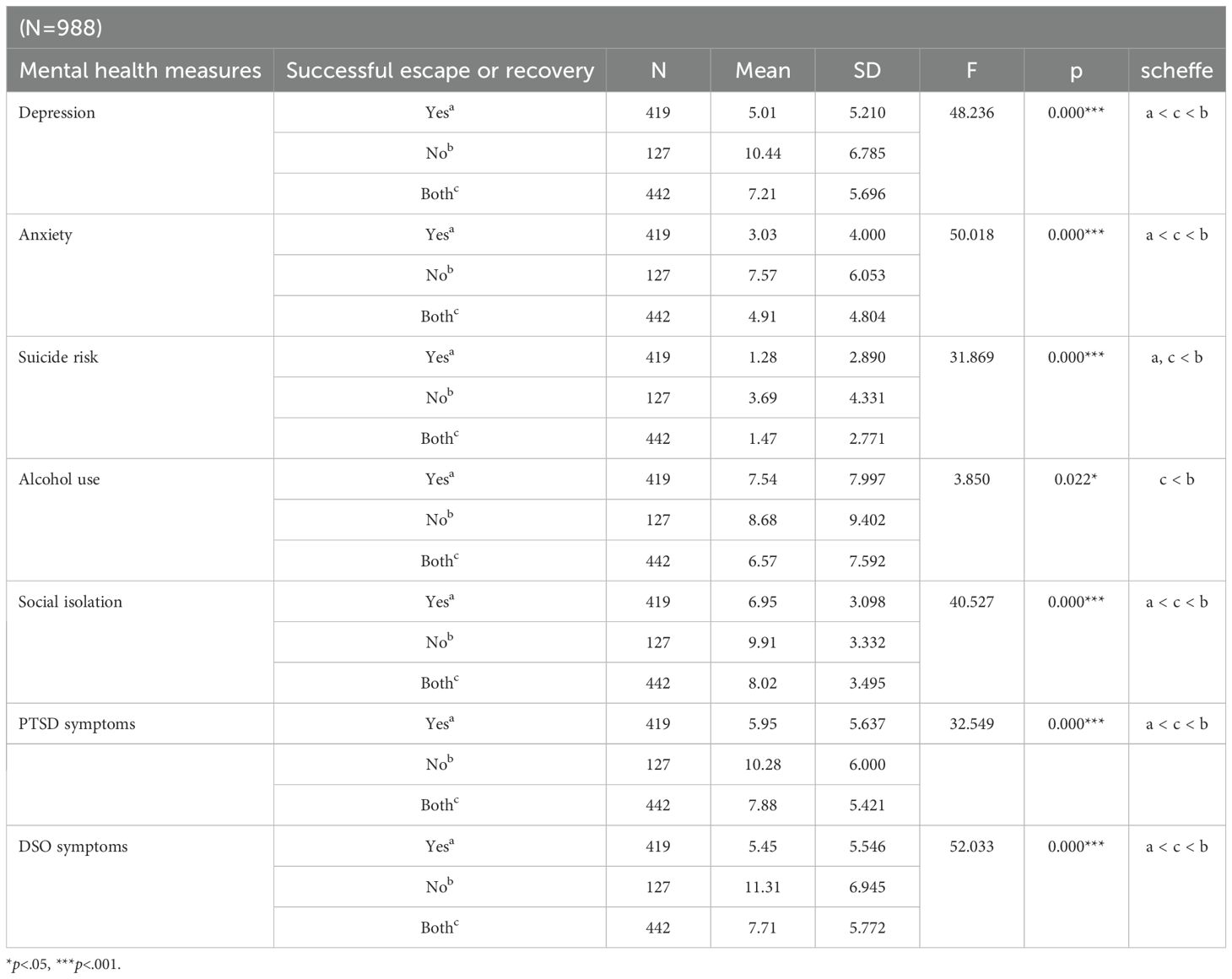
Table 2. One way ANOVA analysis of variance for the differences between successful escape or recovery and mental health measures.
The number of PTE types experienced directly or indirectly ranged from 0 to 57, with a mean of 9.19 (SD=7.908) in total sample and 9.30 in individuals with PTEs (n=988). The number of PTE types was significantly associated with depression, anxiety, and suicide risk. In addition, the number of PTE types differed significantly across the potential PTSD diagnoses (F(2, 997)=10.919, p <.001). The Scheffe test revealed that the cPTSD group reported a significantly higher number of PTE types (mean=13.61) than the PTSD (mean=10.14) and non-PTSD groups (mean=8.86). The PTE types experienced by individuals are listed in Table 3.
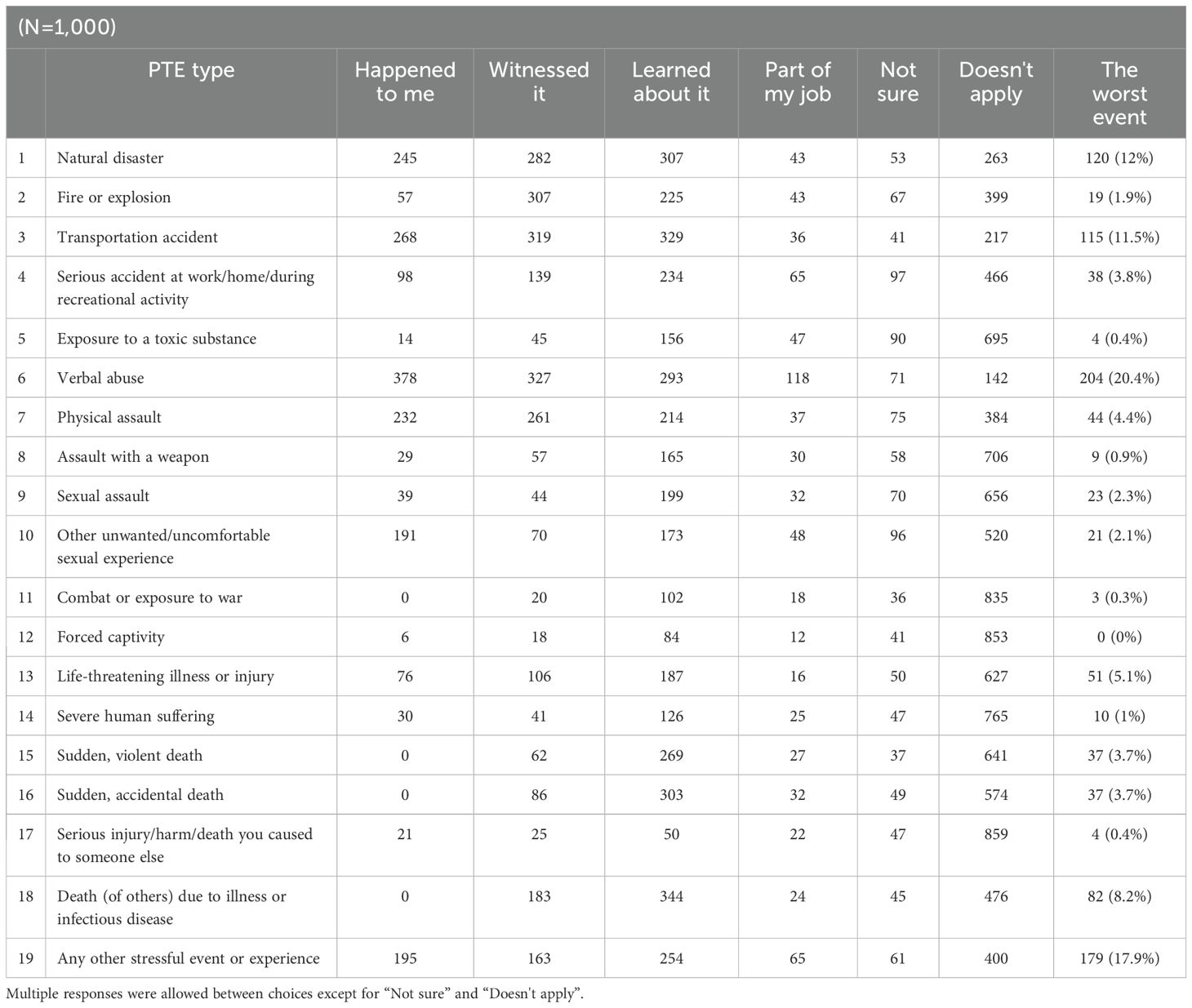
Table 3. Threshold effect analysis of the NHHR on all-cause and cardiovascular mortality in participants with hypertension.
Detailed responses to PTE by sex are presented in Table 4. Male respondents reported significantly more experiences of most PTE types than female respondents. Female respondents were significantly more likely to experience other unwanted/uncomfortable sexual experiences (t(998)=4.792, p <.001). Participants in their 20s, 30s, and 40s reported significantly more experiences of verbal abuse than those in their 60s (F(4, 995)=6.441, p <.001), and those in their 20s and 40s reported more experiences of physical abuse than those in their 60s (F(4, 995)=5.447, p <.001).
Among those with PTEs (n=988), the most common point of time for events that hurt me the most was more than 20 years ago (37.8%, n=373). ANOVA revealed significant differences in PTSD (F(5, 982)=14.101, p <.001), DSO symptom severity (F(5, 982)=5.695, p <.001), suicide risk (F(5, 982)=5.090, p <.001) and alcohol abuse (F(5, 982)=4.242, p=.001) across the time points (Table 5).
Among the probable PTSD cases (n=90), the most common time since the worst event was 20 years or more (n=23), followed by 10-20 years (24.4%), 1-5 years (20%), 5-10 years (12.2%), 6-12 months (8.9%), and less than 6 months (8.9%). There were no significant differences in mental health outcomes across time in this population.
Table 6 presents the correlations among the variables of interest. Pearson’s correlation analysis showed that depression, anxiety, suicide risk, alcohol abuse, and social isolation all had statistically significant positive correlations with the severity of PTSD symptoms and DSO symptoms (p <.01). The LEC-5 sum score showed a significant positive correlation with depression, anxiety, suicide risk, and alcohol abuse (p <.01).
The cut-off scores for depression, anxiety, and suicidality and the detailed prevalence in the probable PTSD and cPTSD groups are shown in Table 7. 26.8%, 15.6%, and 26.9% of participants showed moderate-to-severe depressive symptoms, anxiety symptoms, and suicide risk, respectively. The comorbidity rates for moderate-to-severe depression, anxiety, and suicide risk were 21.4%, 3.6%, and 28.6% for respondents with probable PTSD, and 69.4%, 54.8%, and 72.6% for those with probable cPTSD, respectively.
Participants were asked about their mental health and service experiences throughout their life. A total of 403 (40.3%) participants responded that they had experienced a mental health problem at some point in their lives, but only 182 participants (45.2% of 403) reported that they had ever sought mental health care, such as counseling or treatment. The age of first experiencing a mental health problem was 30.37 years old (SD=13.263), and the age of receiving the first service for the problem was 33.53 years old (SD=12.273). Participants visited the following institutions: psychiatric hospitals (n=130), general hospitals other than mental health departments (internal medicine, pediatrics, etc., n=34), private organizations (psychological counseling centers, clinics, etc., n=34), Seoul psychological support centers (n=21), public mental health service organizations (community mental health welfare centers, national trauma centers, etc., n=16), general public organizations other than mental health services (general welfare centers, health centers, etc., n=15), and others (Religion, n=1).
Among those with probable PTSD (n=90), 56 participants (62.2%) reported that they had experienced some kind of mental health problem, and the remaining 34 participants (37.8%) denied having any mental health problems, although they scored above the cutoff point for self-reported PTSD. Among those who reported having mental health problems (n=56), 31 (55.4%) reported having experienced a mental health consultation, while 25 (44.6%) reported that they had not received services, although they had experienced a problem. Service users visited psychiatric hospitals (n=23), general hospitals other than mental health departments (internal medicine, pediatrics, etc., n=9), private organizations (psychological counseling centers, clinics, etc., n=7), Seoul psychological support centers (n=4), public mental health service organizations (community mental health welfare centers, national trauma centers, etc., n=3), and general public organizations other than mental health services (general welfare centers, health centers, etc., n=3). The mean age at first experiencing a mental health problem was 28.5 years old (SD=13.571), ranging from 5 to 57 years old. The mean age at first receiving services was 31.68 years old (SD=13.622), resulting in an average of 2.35 years delay of treatment. There was no significant difference in treatment delay between participants with and without probable PTSD among those who got treatment.
Our findings have several important clinical implications. To our knowledge, this is the first study to examine the relation between PTEs, the prevalence and symptom severity of PTSD and cPTSD, and their associations with other mental health outcomes among the representative sample in Seoul, South Korea. Most participants (98.8%) experienced at least one PTE category in their life, which is consistent with the findings of previous studies (16, 18, 22). The prevalence of PTSD and cPTSD in Seoul was estimated at 2.8% and 6.2%, respectively.
Both PTSD and DSO symptom severity were significantly associated with depression, anxiety, suicide risk, social isolation, and alcohol abuse. Probable cPTSD group showed significantly higher scores on those variables than PTSD-only and non-PTSD groups. In addition, those with probable cPTSD showed higher comorbidity rates for depression, anxiety, and suicide risk than those with probable PTSD alone. Our findings are in line with results from previous research reporting a stronger association between depression, anxiety, and cPTSD than that between PTSD and those disorders (12). Use of a variety of high-quality measures of PTE and PTSD allowed us to eliminate non-responses by comparing the responses to multiple scales and obtaining more precise information on PTE experiences and prevalence. In addition, adding questions about disease-related deaths considering the impact of the COVID-19 pandemic and verbal abuse to the original questionnaire allowed us to distinguish between events that would otherwise have been categorized as “other types” in the original questionnaire. Specifically, we identified high exposure to verbal abuse (378 participants reported direct exposure).
Participants reported low rates of using services and recognizing the mental health issues. Even among those who did receive treatment, there was an average delay of more than two years between first experiencing a problem and accessing services and their experiences were limited to hospital. Among those with probable PTSD, one-third (n=34) reported no mental health problems or receiving any services, although they showed significant symptoms of PTSD in self-report measures. Moreover, 27.8% of the participants reported that they did not receive mental health services despite reporting mental health symptoms. Even among the probable PTSD group that accessed services (n=31), most of their experience was limited to hospitals. Taken together, our findings suggest that many people do not recognize that they have mental health problems and do not seek treatment. This is not surprising given the low rate of mental health service use reported in previous studies (58, 59). Although evidence-based treatment for PTSD is well documented in the literature, there may be potential barriers to access services, including low accessibility and availability of services and a tendency to be reluctant to talk about and address mental health issues due to the socio-cultural environment in South Korea (58, 59). Reluctance to access mental health services appears to be even more severe in the context of trauma. Given the low rates of recognizing mental health problems and seeking services, mental health policies, especially trauma-related policies, should be proactive, not reactive. Also, this study supports the need for long-term services for traumatized individuals in addition to the initial response and short-term services in that events more than 20 years ago were most frequently reported as the most distressing events, regardless of the potential PTSD diagnosis.
Our results must be interpreted in the context of several limitations. First, the cross-sectional design of this study limits the interpretation of the causal relationships between the variables. Future studies should further examine the causal relationships between the variables using a longitudinal design. Second, as the data is based on self-reported measures, there is a possibility of recall bias or defensive reporting. To minimize the effects of insincere responses and to avoid overestimation of prevalence, inconsistent responses were double-checked and excluded from the analysis (e.g., participants who reported that they had not experienced trauma were excluded when analyzing event-related questions and estimating the prevalence of PTSD). For the index trauma ratings, because most answers were short in length, there was limited understanding of further details about the described events or experiences. For example, whether the death of a loved one is an index trauma or not depends on the context of the event (e.g., old age, murder). The DSM-5 suggests that events such as natural death in the elderly are not considered traumatic (1). Most answers, including death, were short and unclear (e.g., ‘death of loved one’), so unless otherwise noted, these were regarded as natural deaths and considered non-traumatic in this study. However, when contextual information such as suddenness was given, it was categorized as a traumatic event. While examples cannot be provided for privacy reasons, reports of very mundane events, or of expectations of positive luck that were not realized, were categorized as non-traumatic by consensus among the authors to align with the criteria for traumatic events reported in the literature. In addition, in the ITQ-K, responses for time begin with less than six months, making it impossible to determine whether these respondents met the DSM-5 criterion for duration, which is more than one month after the event for diagnosis. Future research may benefit from additional clinician-administered interviews such as the Clinical Administered PTSD Structured interview for DSM-5 (60).
The datasets presented in this article are not readily available because it is the property of the Seoul Metropolitan Government and the research team. Requests to access the datasets should be directed to Gaeun Son, Z2E1MDdAa29yZWEuYWMua3I=.
The studies involving humans were approved by The Institutional Review Board of Korea University [KUIRB-2023-0316-01]. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
GS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. JJ: Investigation, Visualization, Writing – original draft, Writing – review & editing. EH: Investigation, Visualization, Writing – original draft, Writing – review & editing. SP: Investigation, Visualization, Writing – original draft, Writing – review & editing. Y-KC: Supervision, Validation, Writing – original draft, Writing – review & editing. K-HC: Conceptualization, Funding acquisition, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the [Academic research to establish a proactive response plan for PTSD] funded by the Seoul Metropolitan Government. The study was also supported by the National Research Foundation of Korea (NRF-2023S1A5C2A0709598711).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1558085/full#supplementary-material
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association. (2013). doi: 10.1176/appi.books.9780890425596.
2. World Health Organization. International classification of diseases, eleventh revision (ICD-11) (2021). Available online at: https://icd.who.int/browse11 (Accessed January 09, 2025).
3. Karatzias T, Cloitre M, Maercker A, Kazlauskas E, Shevlin M, Hyland P, et al. PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, germany and lithuania. Eur J Psychotraumatol. (2017) 8(sup7):1418103. doi: 10.1080/20008198.2017.1418103
4. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. (1995) 52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012
5. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Traumatic Stress. (2013) 26:537–47. doi: 10.1002/jts.2013.26.issue-5
6. Koenen KC, Ratanatharathorn A, Ng LC, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. psychol Med. (2017) 47:2260–74. doi: 10.1017/s0033291717000708
7. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
8. Zhang L, Pan R, Cai Y, Pan J. The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: A systematic review and single-arm meta-analysis. Psychiatry Invest. (2021) 18:426–33. doi: 10.30773/pi.2020.0458
9. Fox R, Power JM, Coogan AN, Beekman AT, van Tilburg TG, Hyland P. Posttraumatic stress disorder and loneliness are associated over time: A longitudinal study on PTSD symptoms and loneliness, among older adults. Psychiatry Res. (2021) 299:113846. doi: 10.1016/j.psychres.2021.113846
10. Fox V, Dalman C, Dal H, Hollander A, Kirkbride JB, Pitman A. Suicide risk in people with post-traumatic stress disorder: A cohort study of 3.1 million people in Sweden. J Affect Disord. (2021) 279:609–16. doi: 10.1016/j.jad.2020.10.009
11. Hruska B, Delahanty DL. Application of the stressor vulnerability model to understanding posttraumatic stress disorder (PTSD) and alcohol-related problems in an undergraduate population. Psychol Addictive Behav. (2012) 26:734–46. doi: 10.1037/a0027584
12. Karatzias T, Hyland P, Bradley A, Cloitre M, Roberts NP, Bisson JI, et al. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population based sample of adults in the United Kingdom. Depression Anxiety. (2019) 36:887–94. doi: 10.1002/da.2019.36.issue-9
13. Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: A systematic review. Arch Suicide Res. (2010) 14:1–23. doi: 10.1080/13811110903478997
14. Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. (2000) 61:22–32.
15. Murphy D, Karatzias T, Busuttil W, Greenberg N, Shevlin M. ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) in treatment seeking veterans: risk factors and comorbidity. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1289–98. doi: 10.1007/s00127-021-02028-6
16. Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. psychol Med. (2016) 46:327–43. doi: 10.1017/S0033291715001981
17. Hyland P, Vallières F, Cloitre M, Ben-Ezra M, Karatzias T, Olff M, et al. Trauma, PTSD, and complex PTSD in the Republic of Ireland: prevalence, service use, comorbidity, and risk factors. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:649–58. doi: 10.1007/s00127-020-01912-x
18. Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol. (2017) 8:1353383. doi: 10.1080/20008198.2017.1353383
19. Fink DS, Gradus JL, Keyes KM, Calabrese JR, Liberzon I, Tamburrino MB, et al. Subthreshold PTSD and PTSD in a prospective-longitudinal cohort of military personnel: Potential targets for preventive interventions. Depression Anxiety. (2018) 35:1048–55. doi: 10.1002/da.22819
20. Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, Struening EL. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry. (2001) 158:1467–73. doi: 10.1176/appi.ajp.158.9.1467
21. Hellmuth JC, Jaquier V, Swan SC, Sullivan TP. Elucidating posttraumatic stress symptom profiles and their correlates among women experiencing bidirectional intimate partner violence. J Clin Psychol. (2014) 70:1008–21. doi: 10.1002/jclp.22100
22. Chae SM. Trauma among young adults in South Korea. KIHASA. (2022) 417:1–8. Available online at: https://repository.kihasa.re.kr/handle/201002/39148.
23. Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The life events checklist for DSM-5 (LEC-5). National Center for PTSD (2013). Available online at: www.ptsd.va.gov (Accessed January 09, 2025).
24. Ministry of health and welfare. National mental health survey 2021. Sejong, South Korea: Ministry of Health and Welfare. (2021).
25. HIRA. Total number of Post-traumatic stress disorder (PTSD) patients in South Korea in 2022, by age and gender [Graph]. Statista (2023). Available at: https://www.statista.com/statistics/1430278/south-korea-ptsd-patient-number-by-age-and-gender/ (Accessed January 09, 2025).
26. Kim WH, Jung YE, Roh D, Kim D, Chae JH, Park JE. Development of Korean version of PTSD checklist for DSM-5 (K-PCL-5) and the short form (K-PCL-5-S). Psychiatry Invest. (2022) 19:661. doi: 10.30773/pi.2022.0092
27. National Disaster Management Research Institute. How disaster victims’ lives change after a disaster and the development of disaster relief services. Ulsan, South Korea: National Disaster Management Research Institute. (2019).
28. Ji H-a, Choi D. Influence of the risk for post-traumatic stress disorder, social stigma and social support on quality of life of COVID-19 survivors. J Korean Acad Fundamentals Nurs. (2022) 1225:2287–1802. doi: 10.7739/jkafn.2022.29.4.484
29. Sterling M. The impact of event scale (IES). Aust J Physiotherapy. (2008) 54:78. doi: 10.1016/S0004-9514(08)70074-6
30. Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The Primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Internal Med. (2016) 31:1206–11. doi: 10.1007/s11606-016-3703-5
31. Choi H, Lee W, Hyland P. Factor structure and symptom classes of ICD-11 complex posttraumatic stress disorder in a South Korean general population sample with adverse childhood experiences. Child Abuse Negl. (2021) 114:104982. doi: 10.1016/j.chiabu.2021.104982
32. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J traumatic Stress. (2015) 28:489–98. doi: 10.1002/jts.2015.28.issue-6
33. Lee M, Kim. E. Current status and challenges of industrial accident trauma support in korea: A case study of the occupational trauma center in region D. Korean J Couns Psychother. (2023) 35:1517–41. doi: 10.12771/emj.2025.e12
34. Chen H. Reminders everywhere’: Halloween crush haunts survivors one year after Itaewon crowd disaster. New York, NY: CNN (2023). Available online at: https://www.cnn.com (Accessed January 09, 2025).
35. Lee J, Lee SH, Shin C, Yoon HK, Park HE, Cho EB, et al. Exploring the factors associated with indirect trauma caused by a human-made disaster on the general population: A community study five years after the Sewol ferry incident. Int J Disaster Risk Reduction. (2021) 60:102262. doi: 10.1016/j.ijdrr.2021.102262
36. Kim C, Park H. The relation between exposure to the news of the nth room case and world assumptions: the mediating effect of indirect trauma. Korean J Culture Soc Issues. (2021) 27:237–58. doi: 10.20406/kjcs.2021.8.27.3.237
37. Shultz JM, Besser A, Kelly F, Allen A, Schmitz S, Hausmann V, et al. Psychological consequences of indirect exposure to disaster due to the Haiti earthquake. Prehospital Disaster Med. (2012) 27:359–68. doi: 10.1017/s1049023x12001008
38. Rubin M, Foulser AA, Siegel E, Smits J, Powers MB, Angkaw A, et al. Low reliability when determining criterion a for posttraumatic stress disorder from self-report descriptions of traumatic events: The need for transparent methods. psychol Trauma Theory Res Pract Policy. (2024) 16:435–42. doi: 10.1037/tra0001477
39. Van Overmeire R. The methodological problem of identifying Criterion A traumatic events during the COVID-19 era: A commentary on Karatzias et al.(2020). J Traumatic Stress. (2020) 33:864–5. doi: 10.1002/jts.22594
40. Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, et al. The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica. (2018) 138(6):536–46. doi: 10.1111/acps.12956
41. Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychol Assess (1997) 9(4):445. doi: 10.1037/1040-3590.9.4.445
42. Bora N, Kwon H-I, Kwon J-H. Psychometric qualities of the korean version of the posttraumatic diagnosis scale(PDS-K). Korean J Clin Psychol. (2010) 29(1):147–67. doi: 10.15842/kjcp.2010.29.1.009
43. Park JE, Kim WH, Roh DY, Won SD, Kim HK, Kang SH, et al. Workbook for assessment in disaster behavioral health. Seoul, South Korea: Korean Academy of Anxiety and Mood (2016).
44. Karakurt G, Silver KE. Emotional abuse in intimate relationships: The role of gender and age. Violence victims. (2013) 28:804–21. doi: 10.1891/0886-6708.VV-D-12-00041
45. Weis CN, Webb EK, Stevens SK, Larson CL, deRoon-Cassini TA. Scoring the Life Events Checklist: Comparison of three scoring methods. psychol Trauma Theory Res Pract Policy. (2022) 14:714–20. doi: 10.1037/tra0001049
46. Redican E, Nolan E, Hyland P, Cloitre M, McBride O, Karatzias T, et al. A systematic literature review of factor analytic and mixture models of ICD-11 PTSD and CPTSD using the International Trauma Questionnaire. J Anxiety Disord. (2021) 79:102381. doi: 10.1016/j.janxdis.2021.102381
47. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Internal Med (2001) 16(9):606–13.
48. Choi HS, Choi JH, Park KH, Joo KJ, Ga H, Ko HJ, et al. Standardization of the korean version of patient health questionnaire-9 as a screening instrument for major depressive disorder. J Korean Acad Family Med. (2007) 28:114–9.
49. Park SJ, Choi HR, Choi JH, Kim KW, Hong JP. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood. (2010) 6:119–24.
50. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
51. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care (2008) 46(3):266–74.
52. Yoon S, Park K, Choi KH. The ultra brief checklist for suicidality. J Affect Disord. (2020) 276:279–86. doi: 10.1016/j.jad.2020.07.037
53. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction (1993) 88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
54. Lee BO. Development of korean version of alcohol use disorders identification test (AUDIT-k): Its reliability and validity. J Korean Acad Addict Psychiatry (2000) 4:83.
55. Hwang S, Hong J, An J, Kim M, Jeong S, Chang H. Development and validation of loneliness and social isolation scale. J Korean Neuropsychiatr Assoc. (2021) 60:291–7. doi: 10.4306/jknpa.2021.60.4.291
56. Jeon J. Korea Institute of Health and Social Affairs (2019). Available online at: https://repository.kihasa.re.kr/bitstream/201002/34621/1/%EC%97%B0%EA%B5%AC%EB%B3%B4%EA%B3%A0%EC%84%9C%202019-29.pdf.
57. National Center for Mental Health. National mental health literacy and attitudes survey. (Registration no. 11-1352629-000004-10) (2022). Available online at: https://www.ncmh.go.kr/mentalhealth/board/boardView.do;jsessionid=Z8PUxy39nhZMaKtqOcU37bJKihfhY5U2zqOJsmW1pl3zI9QqnlCjCxn0HIwV1VdT.mohwwas1_servlet_engine1?no=9219&fno=106&gubun_no=&menu_cd=04_02_00_03&bn=newsView&bno=&pageIndex=&search_item=&search_content=.
58. Cho SJ, Lee JY, Hong JP, Lee HB, Cho MJ, Hahm BJ. Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. (2009) 44:943–51. doi: 10.1007/s00127-009-0015-7
59. Rim SJ, Hahm B, Seong SJ, Park JE, Chang SM, Kim B, et al. Prevalence of mental disorders and associated factors in Korean adults: National Mental Health Survey of Korea 2021. Psychiatry Invest. (2023) 20:262–72. doi: 10.30773/pi.2022.0307
Keywords: post-traumatic stress disorder (PTSD), complex post-traumatic stress disorder (CPTSD), potentially traumatic event (PTE), prevalence, comorbidity, mental health service use
Citation: Son G, Jang J, Hong E, Park S, Choi Y-K and Choi K-H (2025) The age of trauma: the prevalence and psychological impact of potentially traumatic exposures in South Korea. Front. Psychiatry 16:1558085. doi: 10.3389/fpsyt.2025.1558085
Received: 09 January 2025; Accepted: 14 February 2025;
Published: 19 March 2025.
Edited by:
Saraswati Dhungana, Institute of Medicine, NepalReviewed by:
Jayne Morriss, University of Southampton, United KingdomCopyright © 2025 Son, Jang, Hong, Park, Choi and Choi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kee-Hong Choi, a2Nob2kxQGtvcmVhLmFjLmty
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.