- School of Physical Education, Southwest University, Chongqing, China
Background: Adolescents and young adults (AYAs) aged 10–25 exhibit an increased prevalence of mental health disorders. Resilience has been well established as a positive factor in promoting and protecting mental health. This systematic review and meta-analysis aimed to quantify the correlation between resilience and mental health in AYAs by including relevant observational studies. Additionally, it explored potential moderators such as percentage of female participants, sample regions, and resilience measurements.
Methods: A comprehensive search of the PubMed, Embase, Cochrane Library, Web of Science and Scopus databases was conducted until September 2024. CMA 3.0 software was used to perform meta-analysis, publication bias and sensitivity analysis of the included studies, and the moderating effect was verified by meta-analysis of variance (ANOVA).
Result: Nineteen studies involving a total of 17,746 participants were included, and the summary effect sizes from the random effect model showed that resilience among AYAs had a correlation coefficient of -0.391 with negative indicators of mental health (95% CI: - 0.469, - 0.308, p < 0.001), and a correlation coefficient of 0.499 with positive indicators of mental health (95% CI: 0.400, 0.586, p < 0.001). Additionally, sample regions and resilience measurements significantly moderated the correlation between resilience and positive indicators of mental health.
Conclusion: Resilience in AYAs showed a moderately negative correlation with negative indicators of mental health and a moderately strong positive correlation with positive indicators of mental health. The findings strengthened the basis for future resilience research in AYAs aged 10–25, highlighting the potential of resilience to help mitigate the increasing mental health challenges faced by this population.
1 Introduction
Recent statistics from the World Health Organization showed that the prevalence of diagnosed mental health disorders among adolescents and young adults (AYAs) aged 10-25 ranged between 10% - 20% (1). Mental health disorders refer to health conditions that are characterized by significant changes or disturbances in emotion, thinking, or behavior (2). The 10-25 age group encompasses adolescents aged 10-19 and young adults aged 18-25 (3, 4), where mental health disorders drawn increasing public attention and are now recognized as a critical global public health issue (5, 6). In specific, approximately one in seven adolescents aged 10-19 suffers from mental health disorders, mainly anxiety and depression, which account for 13% of the global burden of disease in this age group (1). Among young adults aged 18-25, the prevalence of major depressive episodes has risen sharply, increasing from 8.8% in 2005 to 15.2% in 2019, and the percentage of people with severe impairment from major depressive episodes nearly doubling from 5.2% to 10.3% during the decade from 2009 to 2019 (7). Without timely intervention, these mental health disorders can result in long-lasting adverse effects across individuals including social isolation (8), unemployment (9), and substance abuse (10), while significantly increasing the incidence of suicidal behaviors among AYAs (11). Alarmingly, suicide has now become the second leading cause of death among individuals aged 15-25 (12). The consistent epidemiological evidence indicates that all major syndromes constituting approximately 75% of mental health disorders begin before the age of 25 (13). Therefore, prevention and intervention mechanisms for mental health disorders in AYAs aged 10-25 are urgently needed to effectively reduce the disease burden.
Building resilience has received considerable attention from researchers due to its crucial role in reducing the risk of mental health disorders and promoting individual mental health (14). The conceptualization and study of resilience initially emerged from research on children at high risk for severe psychopathology (15). Over time, resilience has been defined in various ways, including as a personality trait that enables an individual to cope with adversity and to achieve positive adjustment and development (16, 17), or as a functional or behavioral outcome that overcomes and helps an individual to recover from adversity (18, 19). However, we propose a broader used definition of resilience as the ability and dynamic process of maintaining or regaining mental health despite experiencing adversity (20–22). Notably, many empirical studies have demonstrated its effectiveness in coping with stress and facilitating positive adaptations to protect the mental health of individuals (23–28). Meanwhile, researchers have explored the theoretical mechanisms underlying this positive effect, developing models of the relationship between resilience and mental health that incorporate mediating variables such as positive affect, perceived social support (29), and coping strategies (30). Despite substantial theoretical and empirical evidence supporting the relationship between resilience and mental health (31–33), previous reviews have paid relatively limited attention to AYAs, leaving the precise strength of this association unclear. In fact, individuals aged 10-25 experience an increased biological stress response (34) which makes them a highly susceptible group to various stressors (35). As a result, this age group exhibits a dramatically increased prevalence of mental health disorders (36). Examining the correlation between resilience and mental health specifically within AYAs will be beneficial in informing targeted resilience interventions. In addition, the dual-factor model of mental health (37, 38) emphasizes the need to evaluate mental health comprehensively. This entails considering both the absence of negative psychopathological indicators and the presence of positive psychological indicators such as subjective well-being, life satisfaction (39, 40). However, previous reviews have rarely explored these aspects in an integrated manner. To address this gap, our study attempts to conduct a more comprehensive quantitative review that combines these dimensions, with a particular focus on AYAs.
Potential moderators influencing the relationship between resilience and mental health in AYAs warrant further investigation. Building on previous studies, we focus on examining the moderating effects of gender, sample regions, and resilience measurements. First, regarding gender, researchers have found that as the percentage of female participants increases, the association between resilience and positive indicators of mental health becomes stronger (41). Second, results observed in samples from different regions often vary due to multiple influencing factors, such as sociocultural differences between Western and Eastern societies or disparities in the stages of resilience research (42, 43). These factors may contribute to differences in the strength of the relationship between resilience and mental health indicators. Lastly, the diversity of resilience measurements, with their different measurement properties, may influence the association between resilience and mental health indicators, resulting in variations in the observed outcomes (44).
In summary, this study aims to systematically quantify the correlation between resilience and both positive and negative indicators of mental health in AYAs through a review of the literature, along with an exploration of some potential moderators including percentage of female participants, sample regions, and resilience measurements.
2 Methods
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and was pre-registered in the International Prospective Register of Systematic Reviews (PROSPERO; ID: CRD42024604631).
2.1 Search strategy
We performed a systematic search in the following five electronic databases (PubMed, Embase, Cochrane Library, Web of Science, and Scopus) and used a snowball strategy to find relevant articles from their references and subsequent citations. The search of literature was limited to the period covered from the inception of each database till September 2024. The detailed search strategy is provided in the Supplementary Material, as the PubMed interface.
2.2 Inclusion and exclusion criteria
The retrieved studies were included in the meta-analysis when the following criteria were met: (1) published studies in English; (2) the study types were observational studies, which included cohort studies, case-control studies, cross-sectional studies and longitudinal studies reporting multiple cross-sections; (3) the participants were AYAs aged 10-25 years; (4) measured resilience, negative indicators (including symptoms of psychopathology and negative affect such as anxiety, depression, schizophrenia, bipolar and other reported mental health disorders or problems) or positive indicators (including subjective well-being, life satisfaction, quality of life etc.) of mental health; (5) reported Pearson’s correlation coefficients (r) between resilience and the above indicators of mental health.
The exclusion criteria are as follows: (1) newspaper, conference presentations, and review literature; (2) studies with incomplete or unreported data; (3) non-observational studies and purely descriptive studies.
2.3 Literature screening
Endnote X9 literature management software was used to detect and exclude all the duplications. Then, two authors evaluated the titles and abstracts of the remaining articles to ensure their eligibility for inclusion in the study. No further review was conducted for articles that met the exclusion criteria. After that, the two authors reviewed the full texts of the eligible literature. During this process, any disagreements were discussed to reach a resolution, or addressed by consulting another author.
2.4 Data extraction and quality assessment
After literature screening, the two authors reviewed the full text for data extraction. The following information of each included study was extracted: author, country, mean age, gender, resilience measurements, and mental health measurements of both negative and positive indicators, as well as Pearson’s correlation coefficient between resilience and both indicators of mental health. Separate extractions were performed if several different samples were investigated in the same study.
The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross-Sectional Studies was applied for quality assessment (45). This checklist consists of 8 items, each of which includes four answers (“yes,” “no,” “unclear,” and “not applicable”). Each “yes” answer corresponds to one point and the rest of the answers are assigned no points, with the points summed to give a total score for each study. Converting the total score to percentages, we rated studies scoring 70% and above as high quality, studies scoring 50% to < 70% as moderate quality, and studies scoring less than 50% as low quality (46).
2.5 Data analysis
All statistical analyses of our study were performed using Comprehensive Meta-Analysis version 3.0 (CMA 3.0) software. Pearson’s correlation coefficient was utilized to evaluate the correlation between resilience and both negative and positive indicators of mental health. First, we converted r values to Fisher’s Z by using the formula Fisher’s Z = 0.5 ln [(1 + r)/(1-r)]. The values obtained were then weighted according to the sample size using the formula SEz = (1/(n-3))1/2. Finally, all values were converted to r by the formula Summary r = (e2z – 1)/(e2z + 1) to evaluate the correlation between resilience and mental health. In addition, according to (47), r = 0.1 represented low correlation, r = 0.3 represented moderate correlation, and r = 0.5 and above represented strong correlation. All mean effect sizes were calculated by averaging the correlation coefficients of all independent samples, weighted by their inverse variance. Heterogeneity test was conducted using Cochran’s Q and I2 statistics (48). The fixed effect model was used to summarize the effects when I2 < 50%; otherwise, the random effect model was more appropriate for the analysis of the effect sizes from the existing literature (49). Moreover, a meta-analysis of variance (ANOVA) was used on categorical variables to test whether it was possible to moderate the correlation between resilience and mental health. The moderating variables in this study were identified based on insights from the existing literature, including the percentage of female participants, sample regions, and resilience measurements. The differences between and within groups were assessed by the Q test, and groups with fewer than 3 studies (k < 3) were removed due to concerns regarding under-representation and limited statistical reliability. Funnel plots and Egger’s linear regression (50) were used to evaluate publication bias. Sensitivity analysis was also conducted to test the robustness of the results of this study.
3 Results
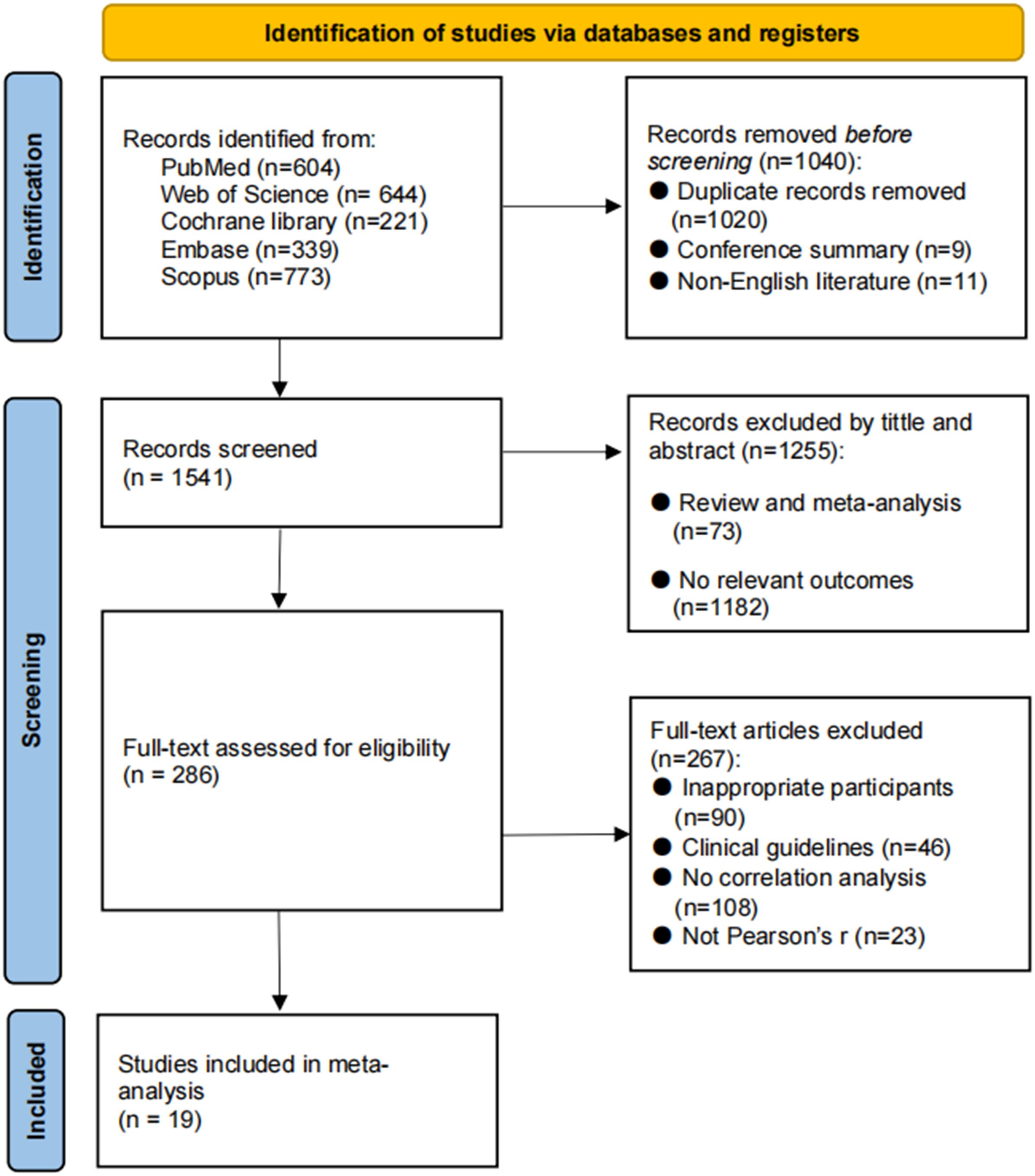
3.1 Literature selection
We retrieved 2581 records from the database in the initial literature search. After removing 1020 duplicates, 11 non-English literature and 9 conference abstracts, 1541 studies were retained. Title and abstract screening excluded 1255 articles that did not match our requirements in terms of sample or topic. The remaining 286 articles were screened in full text, and 267 articles were excluded due to unavailability of data, inappropriate article type, and not reporting Pearson’s correlation coefficient. Finally, a total of 19 studies were included in the current review. Figure 1 shows the flow chart of literature selection process.
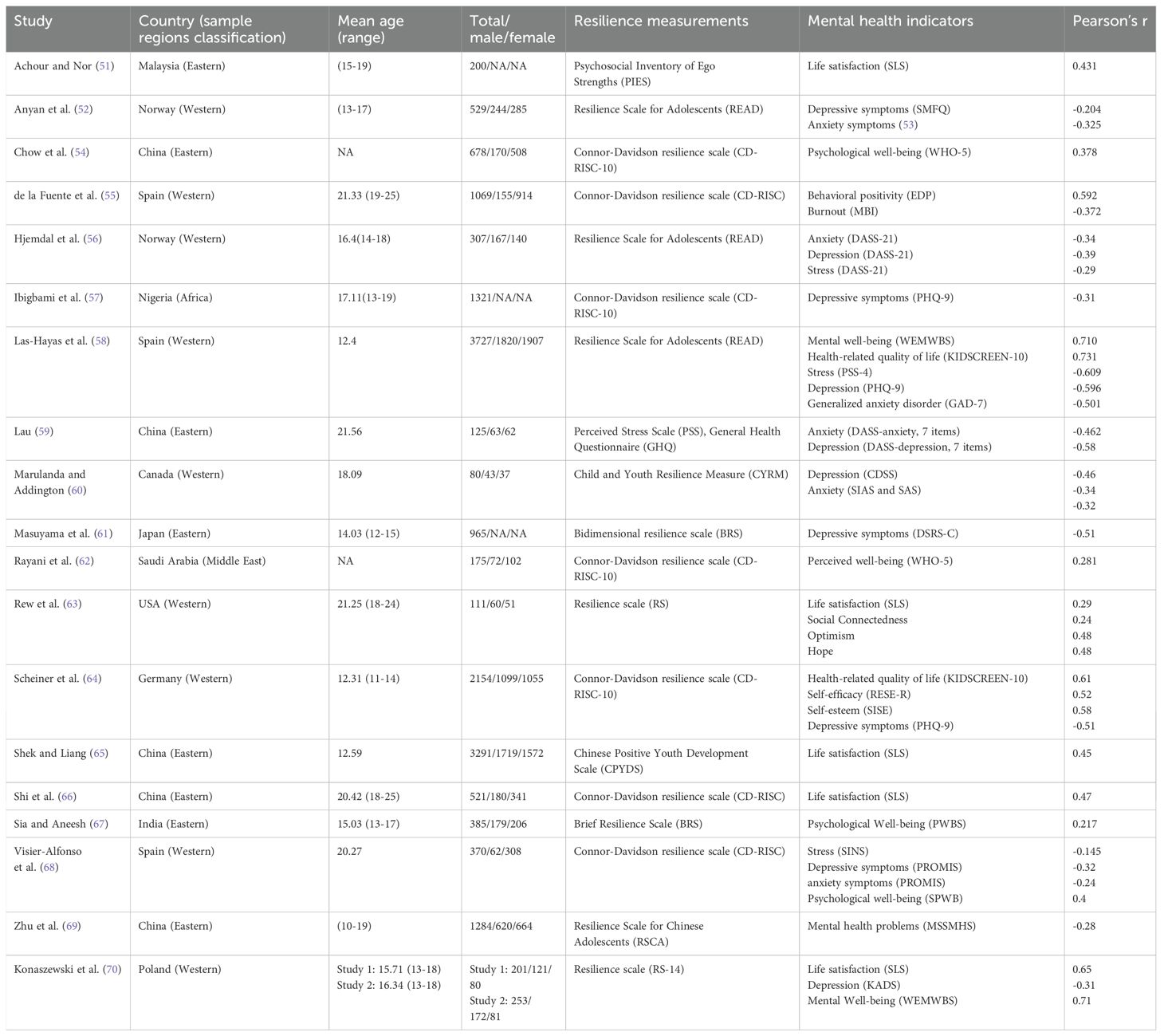
3.2 Study characteristics
The 19 included studies, involving a total of 17746 participants, were conducted between 2011-2024, with more than half of them conducted in the last three years. The detailed characteristics of the included studies are shown in Table 1. Five studies were from China (mainland and HK), three from Spain, two from Norway and Poland, and one each from Malaysia, Nigeria, Canada, Japan, Saudi Arabia, USA, Germany and India. All studies measured both resilience and mental health, and reported Pearson’s correlation coefficient. The CD-RISC was utilized in three studies, while four studies applied the short version (CD-RISC-10). Of the remaining studies, three utilized READ and RS, two used BRS, and PIES, PSS/GHQ, CYRM, CPYDS, RSCA. Out of the 19 included studies, twelve studies measured the negative indicators of mental health, including anxiety, depression, perceived stress, burnout, etc. However, thirteen involved the assessment of various positive indicators of mental health, such as quality of life, life satisfaction, psychological well-being, hope, optimism, self-efficacy.
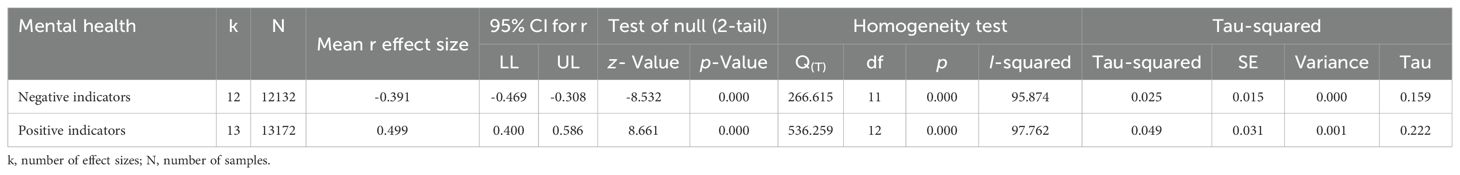
3.3 Effect size and heterogeneity
3.3.1 The summary correlation between resilience and negative indicators of mental health
Data from 12132 AYAs were included in the 12 studies. The results of the heterogeneity test showed a high level of heterogeneity among the included studies (Q = 266.615, p < 0.001, I2 = 95.874%). Therefore, we calculated the mean weighted effect size (r), sample size (k), and 95% confidence intervals using a random effect model (Table 2). The results showed a moderately negative correlation between resilience and negative indicators of mental health (r = - 0.391, 95% CI: - 0.469, - 0.308, p < 0.001; see Figure 2).
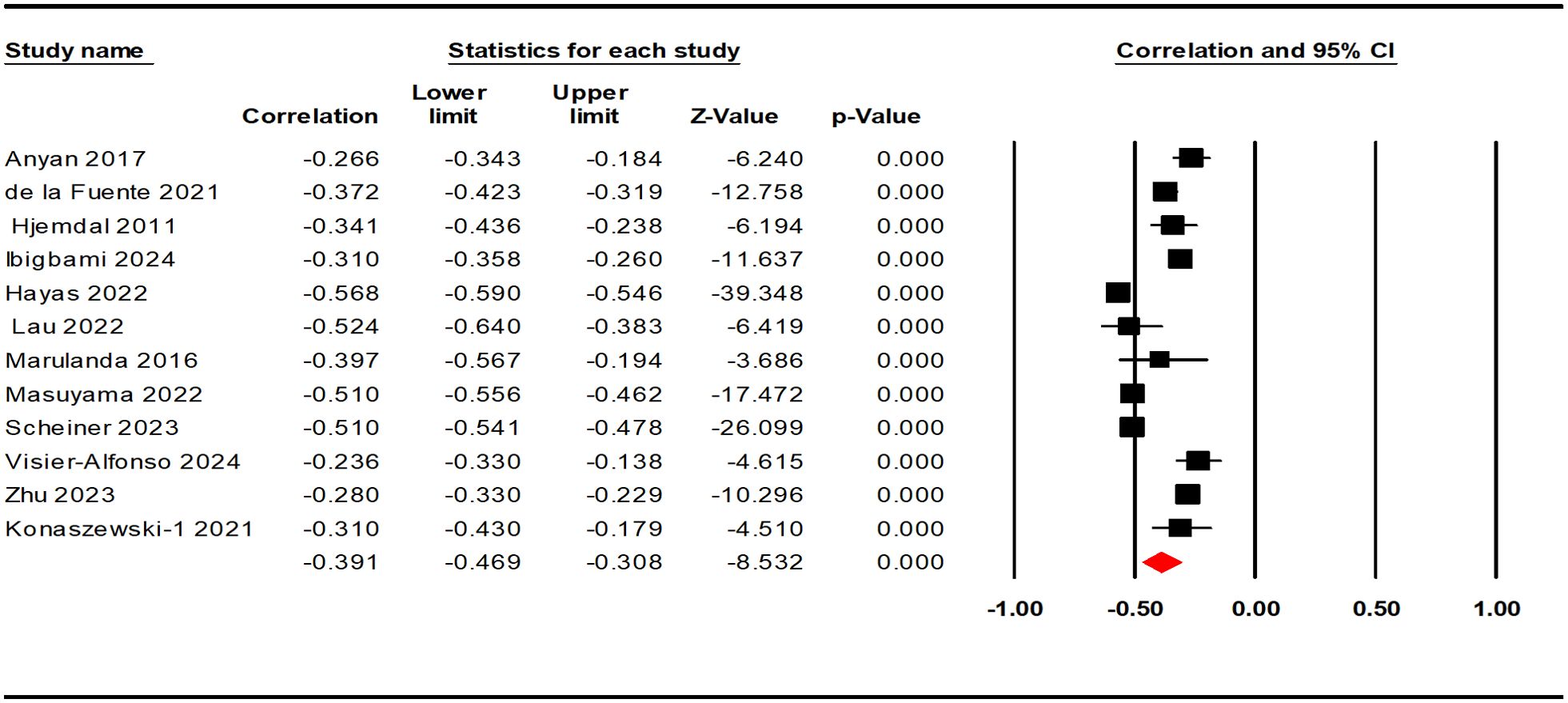
Figure 2. Forest plot of the correlation between resilience and negative indicators of mental health.
3.3.2 The summary correlation between resilience and positive indicators of mental health
The correlations between resilience and positive indicators of mental health were reported in 13 studies, involving 13135 AYAs. The results of the heterogeneity test were similar to the negative indicators, demonstrating high heterogeneity (Q = 536.259; p < 0.001; I2 = 97.762%). The effect size calculated by the random effect model (Table 2) revealed a moderately strong positive correlation between resilience and positive indicators of mental health among the AYAs (r = 0.499, 95% CI: 0.400, 0.586, p < 0.001; see Figure 3).
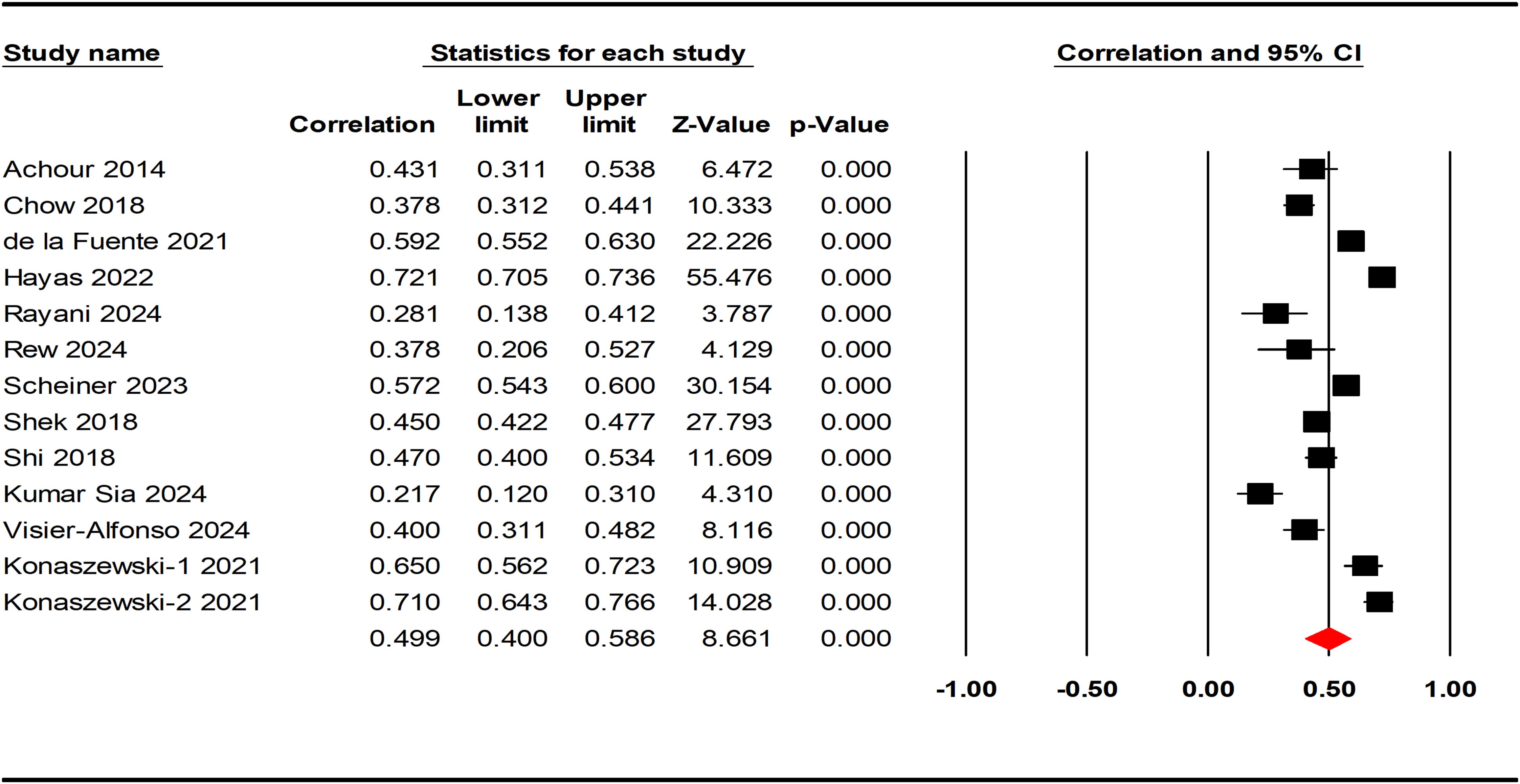
Figure 3. Forest plot of the correlation between resilience and positive indicators of mental health.
3.4 Quality assessment
The quality of included cross-sectional studies was assessed using the JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies, which has been well-validated and considered the most commonly used tool for assessing bias in analytical cross-sectional studies (71). Two authors independently assessed the quality of each study, and any disagreements were resolved through discussions at group meetings. A total of 16 studies received scores above 70%, classifying the majority of the included studies as high quality. Among the remaining three studies, two were categorized as moderate quality, while one was classified as low quality. The detailed results of each included study are shown in the Supplementary Material.
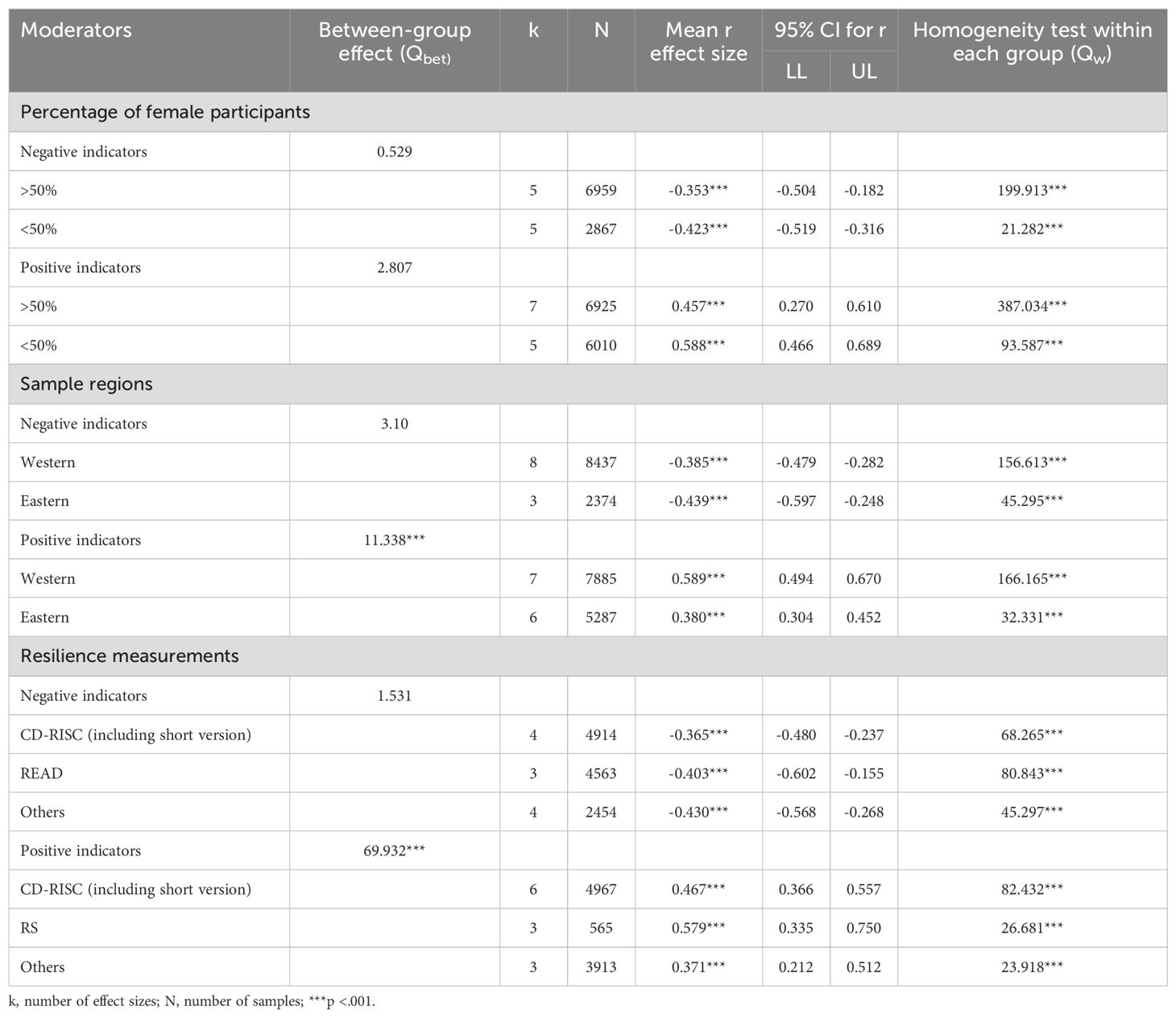
3.5 Moderator analyses
The current study used meta-analysis of variance (ANOVA) to test the moderating effects of three variables below: percentage of female participants, sample regions, and resilience measurements.
Results from the moderator analyses are presented in Tables 3. In terms of the positive indicators of mental health, the sample regions and the resilience measurements significantly moderated the correlation between resilience and mental health (sample regions: QBET = 11.338, p < 0.001, resilience measurements: QBET = 69.932, p < 0.001). More specifically, Studies from Western countries reported the stronger correlation between resilience and mental health (Western: r = 0.589, 95% CI: 0.494, 0.670, p < 0.001, Eastern: r = 0.380, 95% CI: 0.304, 0.452, p < 0.001). For resilience measurements, the RS scale reported stronger correlations than CD-RISC scale and other scales (RS: r = 0.579, 95% CI: 0.335, 0.750, p < 0.001, CD-RISC: r = 0.467, 95% CI: 0.366, 0.557, p < 0.001, Others: r = 0.371, 95% CI: 0.212, 0.512, p < 0.001), while the READ scale group was excluded due to a small sample size of less than 3 studies (k=1). However, percentage of female participants did not have a significant moderating effect on the correlation between resilience and mental health. Regarding the negative indicators of mental health, none of the sample regions, percentage of female participants, or resilience measurements were found to significantly modulate the correlation (p>0.05).
3.6 Publication bias and sensitivity analysis
The present meta-analysis evaluated publication bias using funnel plots and Egger linear regression. The funnel plot provided insufficient evidence of the symmetrical distribution of effect sizes for both negative and positive indicators (Figures 4, 5). Therefore, Egger linear regression was utilized to provide more reliable evidence. The p-values of the results indicate that there were no significant publication biases for both indicators (negative indicators: t = 1.965, p = 0.077; positive indicators: t = 1.545, p = 0.151). The sensitivity analysis was conducted by removing the included samples one by one, and a significant shift in the effect sizes would represent a lack of non-robustness. However, our results indicated that the effect sizes of resilience and both indicators of mental health in AYAs were stable, therefore, the results of this meta-analysis were robust (Figures 6, 7).
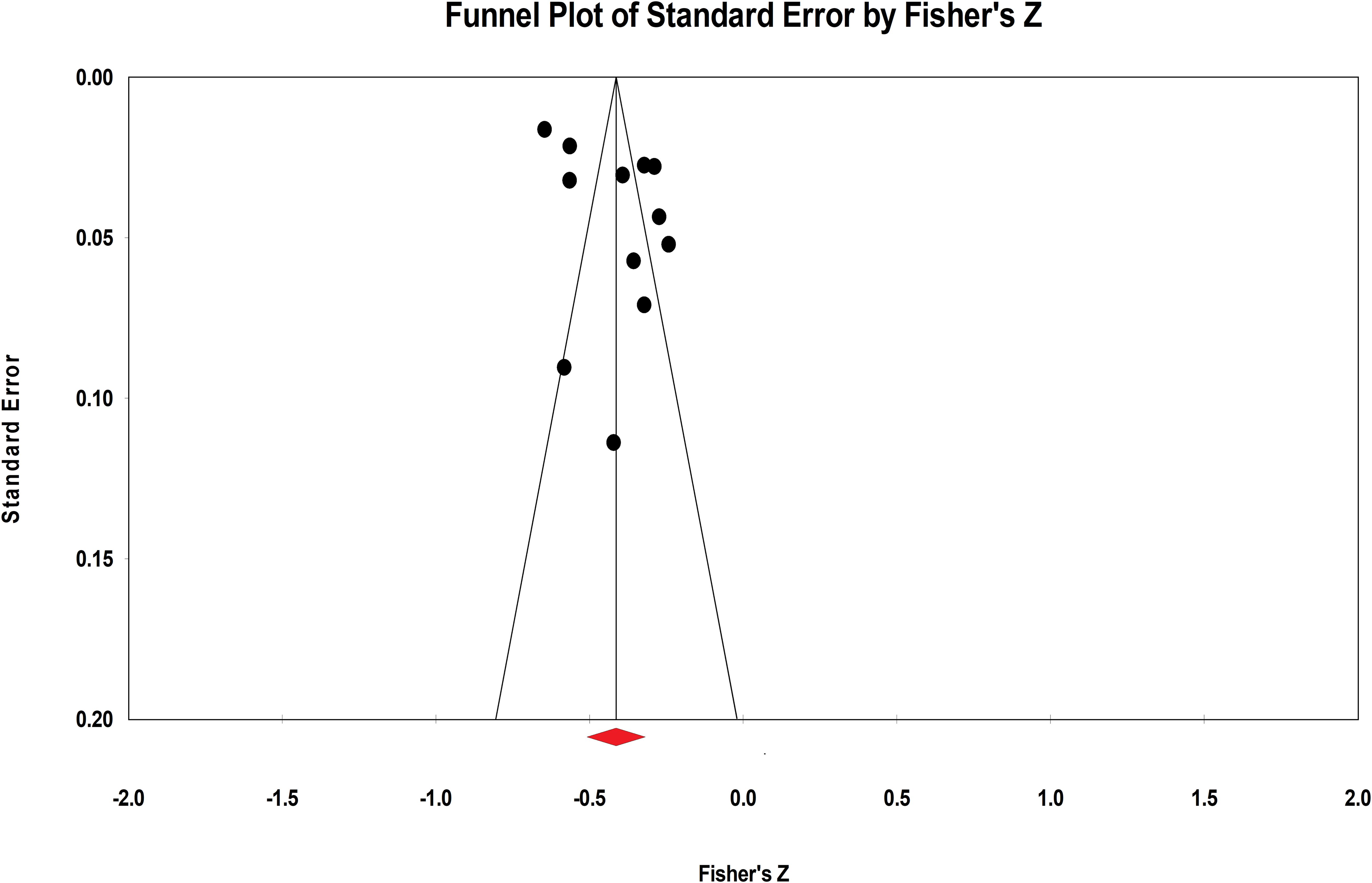
Figure 4. Funnel plot of the correlation between resilience and negative indicators of mental health.
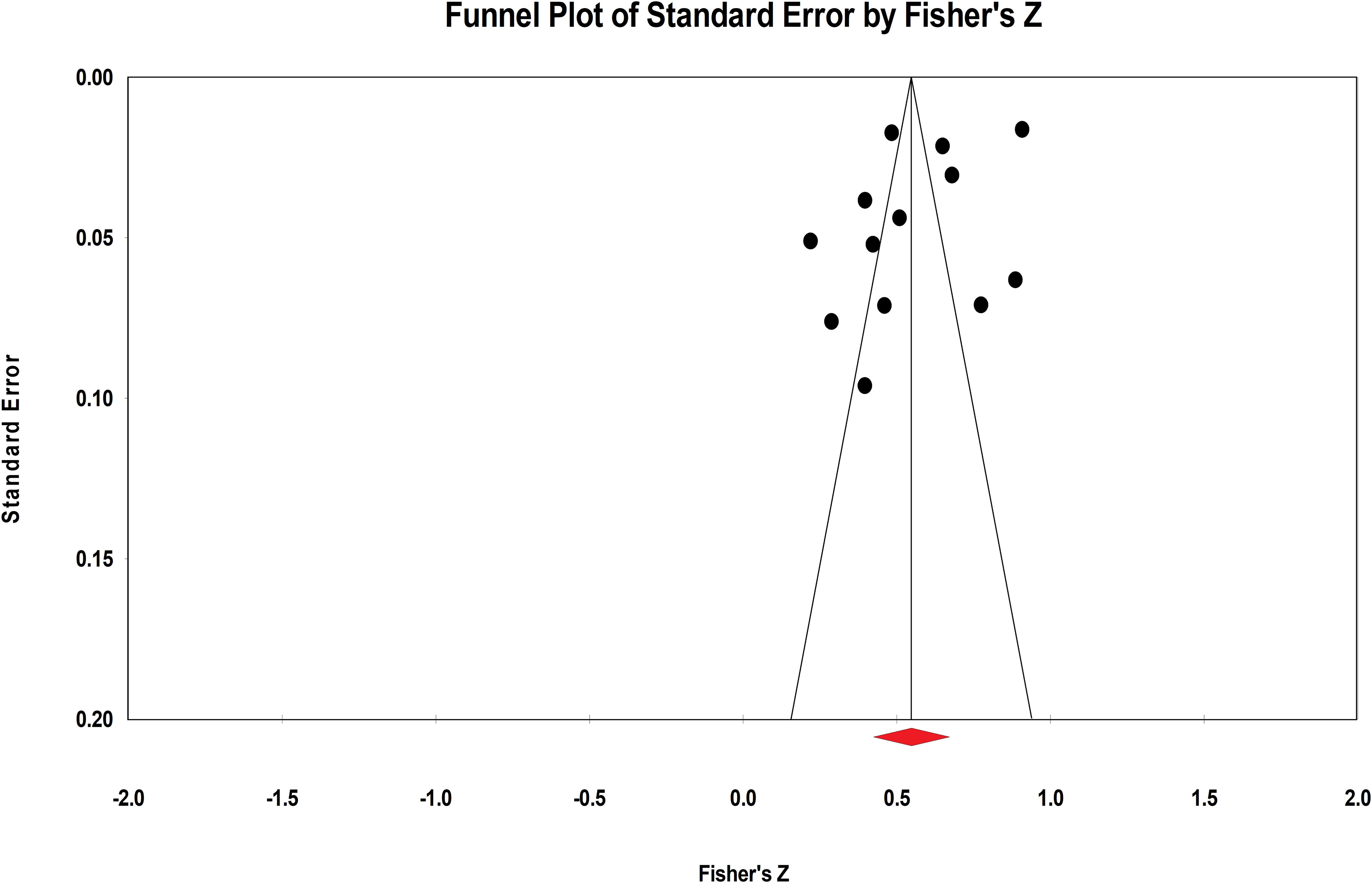
Figure 5. Funnel plot of the correlation between resilience and positive indicators of mental health.
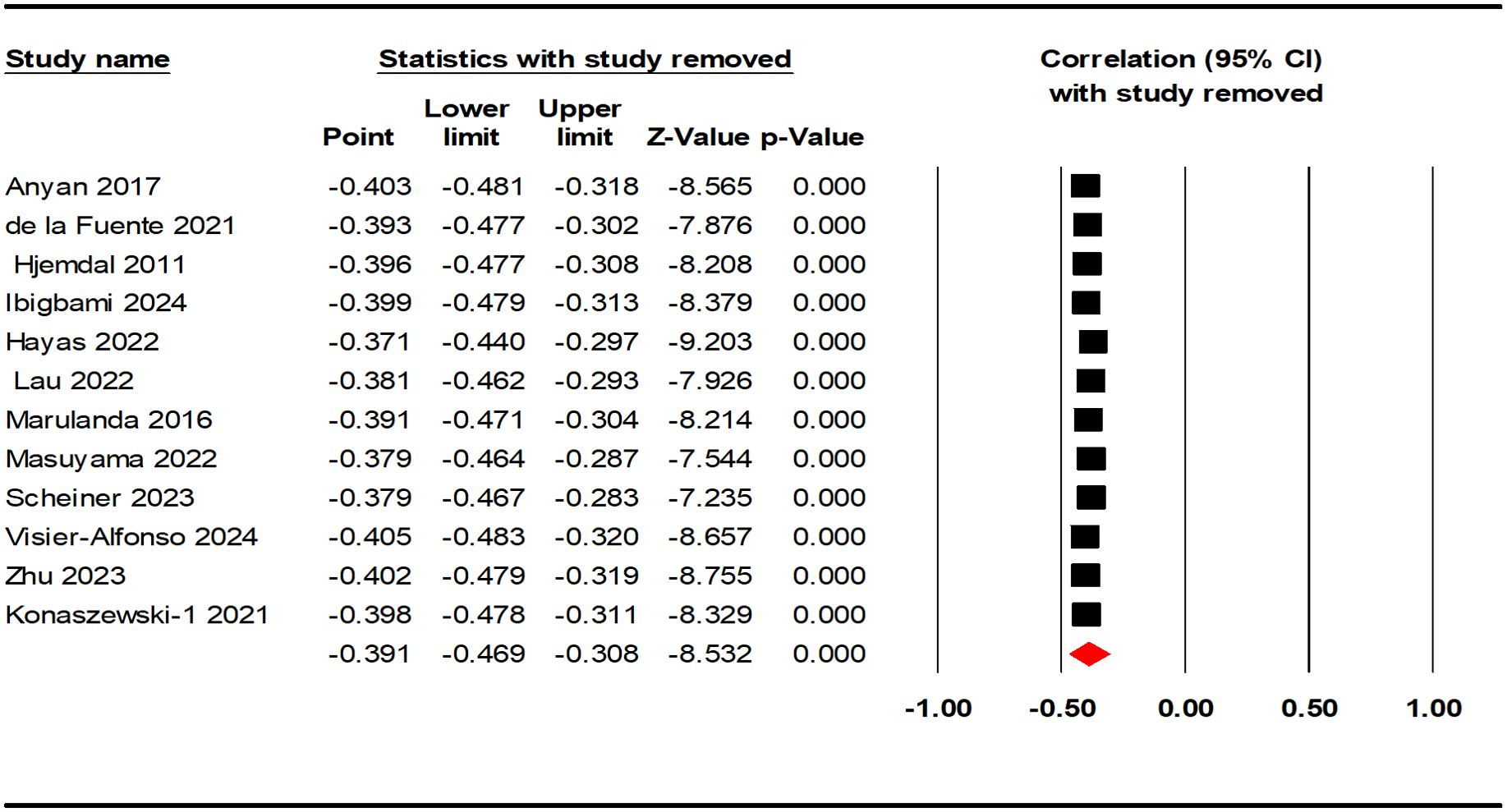
Figure 6. Sensitivity analysis of the correlation between resilience and negative indicators of mental health.
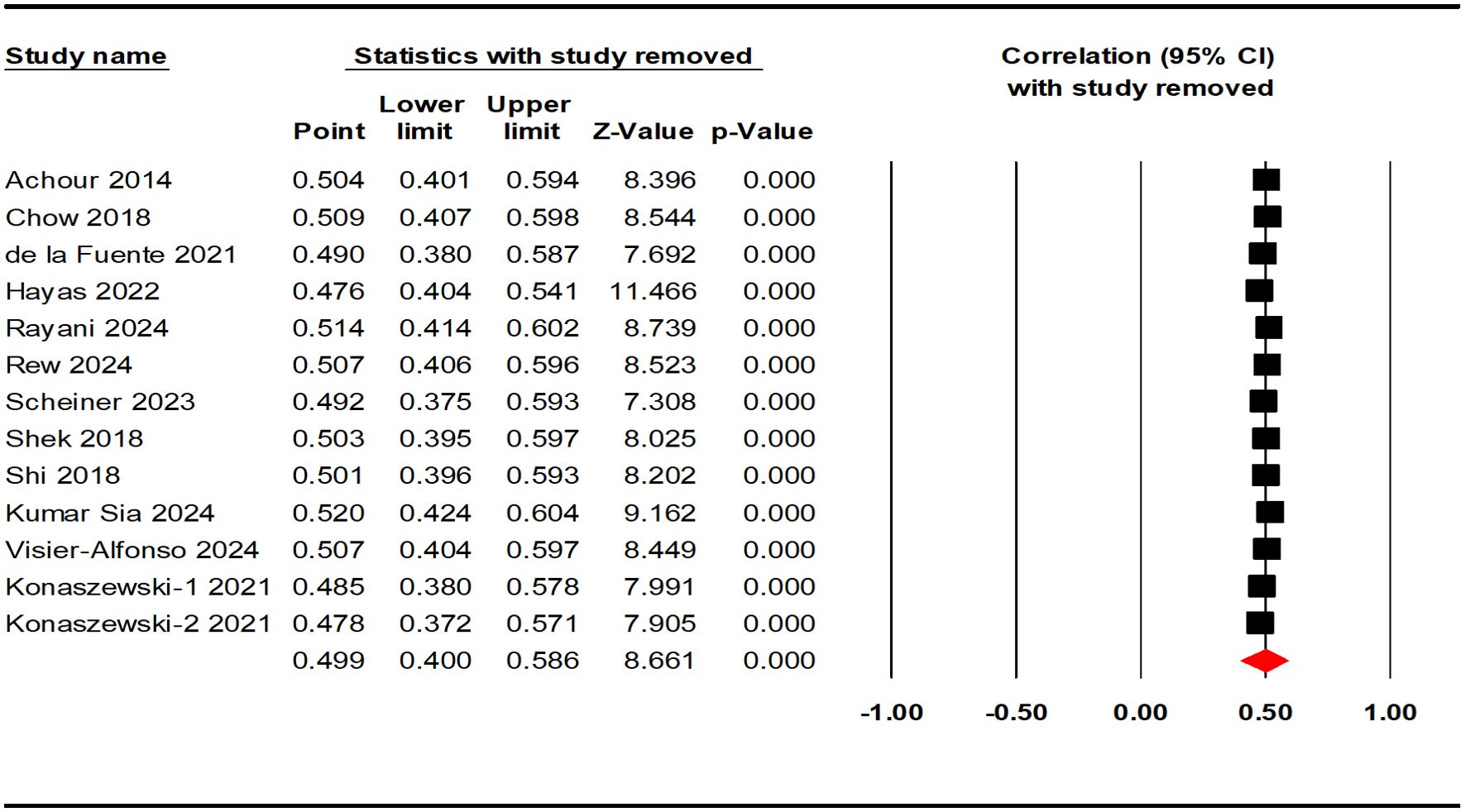
Figure 7. Sensitivity analysis of the correlation between resilience and positive indicators of mental health.
4 Discussion
The current study aimed to systematically summarize the evidence on the correlation between resilience and both negative and positive indicators of mental health in AYAs. A total of 19 studies were included in the meta-analysis, and the results revealed a moderately negative correlation between resilience and negative indicators of mental health (r = - 0.391), and a moderately strong positive correlation with positive indicators of mental health (r = 0.499). Specifically, higher resilience was correlated with reduced levels of perceived stress, anxiety, burnout, and depression, alongside enhanced mental well-being, quality of life, life satisfaction, self-esteem, and self-efficacy among AYAs. These findings are consistent with previous empirical studies covering similar age groups (56, 72–77). Further, in terms of the strength of the correlation, resilience was more strongly correlated with positive indicators of mental health than negative indicators, also supported by the previous evidence (78, 79).
This systematic review provides preliminary evidence on the correlation between resilience and mental health in AYAs. Specifically, this age group encompasses adolescence, from 10 to 19 years old, and emerging adulthood, from 18 to 25 years old, covering a critical developmental stage that spans the transition from education to early social integration. This period is foundational for establishing lifelong health and facilitating personal and professional development (3, 4). Uniquely, this stage is characterized by intensified academic pressure and increased challenges in building and maintaining relationships, which distinguish it from childhood. Meanwhile, the urgency to acquire advanced skills for societal survival exceeds that observed in middle adulthood (80). As a result, this is the period when individuals are most threatened by psychosocial stressors and are vulnerable to mental health disorders (81), which adversely affect academic and occupational achievement, interpersonal relationship formation, self-identity, etc. (36). Over time, untreated mental health disorders during this critical stage may produce long-lasting negative consequences for individuals, including reduced workforce participation, lower incomes, and diminished living standards in later adulthood (82). The more individuals affected, the greater the likelihood of harm at the economic and cultural levels of society.
As highlighted by the World Health Organization, fostering resilience has been an integral part of the strategy for preventing mental health disorders (83), The findings of this study reinforce the significant role of resilience in helping AYAs reduce negative indicators of psychopathology and enhance positive mental health states. These results are supported by relevant empirical studies. In terms of the elimination of negative indicators, resilience has been shown to alleviate symptoms of depression and anxiety in adolescents (84), reduces the after-effects of psychological trauma, and curbs suicidal ideation in young adults (85, 86). Conversely, lower resilience leads to a heightened risk of various mental health disorders (87). In terms of the promotion of positive indicators, resilient adolescent individuals perceive increased life satisfaction (51), possess better emotional regulation to manage negative emotions and prefer positive coping strategies to achieve social adaptation (88). Furthermore, resilience positively affects all dimensions of quality of life (89), while life satisfaction, perceived well-being, and self-efficacy are all negatively affected when resilience is low (90). Although the exact mechanisms that resilience promotes mental health remain complicated (91), resilience theory provides a well-established framework to explain its effects. Resilience facilitates mental health by enabling individuals to counteract the negative consequences of exposure to risk factors. This process involves leveraging environmental, social, and personal protective factors to interrupt the progression from risk exposure to pathological outcomes (33). In specific, through the mobilization of these internal and external protective factors, individuals are able to face up to adverse life events and learn from their struggles to achieve further growth and positive cognitive development (92). As a result, individuals might avoid psychological dysfunction (31), be less likely to suffer from detrimental mental health outcomes (93), and raise the positive indicators such as the perceived well-being (32, 94) to contribute to the promotion of overall mental health (95–97). Additionally, similar positive effects have been explored through theoretical mechanisms. For instance, resilience can promote post-traumatic growth through the mediating effects of internal factors, such as positive emotions, and external factors, such as social support (98). Given the alarming mental health challenges faced by AYAs and the rising demand for effective mental health interventions (99), the results of this study provide a strong referential basis for developing targeted interventions that leverage resilience as a protective and promotive factor for mental health.
This study explored the moderators influencing the correlation between resilience and mental health in AYAs, including percentage of female participants, sample regions, and resilience measurements. First, we found that sample regions moderated the correlation between resilience and positive indicators of mental health, whereas no such moderating effect was observed for negative indicators. Similar results have been found in previous studies, though the specifics vary (100). Our findings revealed that the correlations reported in studies conducted in Western countries were stronger than those from Eastern countries. The perspective of sociocultural differences between Western and Eastern societies may offer a potential explanation for this finding. Current researches and measurements of resilience are predominantly based on cognitive or individual-level characteristics (81), which align more closely with the individualistic cultural context of Western countries (101). In contrast, within the collectivist cultural context of Eastern societies, connections to broader social systems surrounding the individual should also be considered as a key dimension of resilience (102). However, only a limited number of scales in the existing literature have incorporated this aspect. Moreover, this finding may also be attributed to varying levels of awareness of the resilience concept. Greater awareness of resilience tends to foster positive attitudes and adaptive behaviors, which, in turn, strengthen the association between resilience and mental health outcomes (103). Given that the concept of resilience originated in Western contexts and has been studied across disciplines as early as the beginning of the 21st century (20), it is likely more established in Western cultures compared to Eastern ones (101), leading to the present findings of this study. However, in recent years, efforts to localize and adapt the concept of resilience within Eastern cultural frameworks have gained momentum, presenting promising opportunities for advancing cross-cultural resilience research (92, 104, 105).
Second, resilience measurements also moderated the correlations between resilience and positive indicators of mental health in AYAs. Specifically, although the CD-RISC scale was considered the more commonly used instruments for assessing resilience (106), the RS scale yielded higher correlation coefficients in the studies included. One potential explanation is that in terms of applicability to the participant populations, the RS scales (including short versions) are considered to be more appropriate for the adolescent population, as well as possessing cross-age applicability (107). By contrast, the CD-RISC has shown better measurement properties when including general population and clinical samples, making it more applicable in the clinical practice through resilience interventions (16). In addition, the stability of the scales’ factor structure may also serve as a potential explanation for the findings. For instance, the original version of the CD-RISC-25 demonstrated instability in its proposed five-factor structure (16). Many researchers have reported that it is better represented by a three-factor structure (108) or one general factor (109). In contrast, the RS scale has consistently maintained its solid one-factor measure of resilience (81). Concerning the negative indicators of mental health, we did not find a moderating effect of the resilience measurements.
Finally, while prior studies reported that a higher percentage of female participants strengthened the correlation between resilience and mental health (41, 84), this effect was not observed in our analysis when the percentage of female participants was higher (>50%) in either the positive or the negative indicators. This discrepancy may be explained by the limited number of included studies, necessitating cautious interpretation and future research to validate the findings.
5 Limitations and future directions
Although conducted in strict accordance with the relevant standards and procedures, the current meta-analysis has several limitations as follows. First, we used only Pearson’s correlation coefficient to measure effect sizes, which limited the number of studies we included in the meta-analysis and thus might affect the validity and generalization of the results. Future studies should consider incorporating other metrics such as phi-coefficient, point-biserial correlation, and Spearman rank-order correlation coefficient as well. Second, potential moderators were not comprehensive enough as we only considered percentage of female participants, sample regions, and resilience measurements. Future studies should take sufficient account of other variables, such as educational attainment, ethnicity, and adversity factors, all of which may influence the relationship between resilience and mental health in AYAs, particularly adversity factors. Finally, our meta-analysis, based mainly on cross-sectional studies, was not able to provide an explanation for the causal relationship between resilience and mental health among AYAs. Therefore, future research should prioritize the use of longitudinal study designs. For instance, tracking resilience and mental health indicators across multiple time points while addressing confounding factors can provide valuable insights into their potential causal relationships.
6 Conclusions
The current meta-analysis included 19 studies on the correlation between resilience and mental health in AYAs. Our results indicated that resilience showed a moderately negative correlation with negative indicators of mental health and a moderately strong positive correlation with positive indicators of mental health. Additionally, the strength of the correlation between resilience and positive indicators of mental health was moderated by sample regions and resilience measurements. By extending the application of the two-factor model of mental health, this study demonstrated that previous findings on the correlation between resilience and mental health in other age groups are also applicable to AYAs aged 10-25. This provides a more direct and robust basis for future studies of resilience in this population. Therefore, we advocate for the further exploration of targeted resilience-building interventions and strategies in school and workplace settings, which could effectively help to mitigate the increasing mental health challenges faced by AYAs.
Author contributions
SLL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JH: Data curation, Supervision, Validation, Writing – review & editing. JZ: Data curation, Supervision, Validation, Writing – review & editing. ZM: Data curation, Supervision, Validation, Writing – review & editing. ZT: Data curation, Supervision, Writing – review & editing. SL: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Social Science Fund of China (24BTY098).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1536553/full#supplementary-material
References
1. World Health Organization. Adolescent mental health (2020). Available online at: https://www.who.int/newsroom/fact-sheets/detail/adolescent-mental-health (Accessed September 23, 2024).
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5 Vol. 5. Washington, DC: American psychiatric association (2013).
3. Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. (2000) 55:469. doi: 10.1037//0003-066x.55.5.469
4. World Health Organization. Adolescent Health (2020). Available online at: https://www.who.int/zh/health-topics/adolescent-healthtab=tab_1 (Accessed September 23, 2024).
5. Lieberman JA. Shrinks: The untold story of psychiatry. London, United Kingdom: Hachette UK (2015).
6. Daly M. Prevalence of depression among adolescents in the US from 2009 to 2019: analysis of trends by sex, race/ethnicity, and income. J Adolesc Health. (2022) 70:496–9. doi: 10.1016/j.jadohealth.2021.08.026
7. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health (2020). Available online at: https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf (Accessed September 25, 2024).
8. Ma R, Mann F, Wang J, Lloyd-Evans B, Terhune J, Al-Shihabi A, et al. The effectiveness of interventions for reducing subjective and objective social isolation among people with mental health problems: a systematic review. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:839–76. doi: 10.1007/s00127-019-01800-z
9. Brouwers EP. Social stigma is an underestimated contributing factor to unemployment in people with mental illness or mental health issues: position paper and future directions. BMC Psychol. (2020) 8:1–7. doi: 10.1186/s40359-020-00399-0
10. Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the US and Canada—a systematic review and meta-analysis. J Clin Med. (2018) 7:543. doi: 10.3390/jcm7120543
11. Ong MS, Lakoma M, Gees Bhosrekar S, Hickok J, McLean L, Murphy M, et al. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Ment Health. (2021) 26:134–42. doi: 10.1111/camh.12400
12. United Educators. Mental Health Issues on Campus: White Papers (2019). Available online at: https://www.ue.org/risk-management/online-courses/single-courses/fostering-student-mental-health/?gclid=EAIaIQobChMImKHe79Dy6wIVBvlRCh2cKg43EAAYAiAAEgIg6fD_BwE (Accessed September 25, 2024).
13. Uhlhaas PJ, Davey CG, Mehta UM, Shah J, Torous J, Allen NB, et al. Towards a youth mental health paradigm: a perspective and roadmap. Mol Psychiatry. (2023) 28:3171–81. doi: 10.1038/s41380-023-02202-z
14. Riepenhausen A, Wackerhagen C, Reppmann ZC, Deter H-C, Kalisch R, Veer IM, et al. Positive cognitive reappraisal in stress resilience, mental health, and well-being: A comprehensive systematic review. Emotion Rev. (2022) 14:310–31. doi: 10.1177/17540739221114642
15. Garmezy N. The study of competence in children at risk for severe psychopathology. In: Anthony EJ, Koupernik C, editors. The child in his family: Children at psychiatric risk. New York, United States: John Wiley & Sons (1974).
16. Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
17. Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J Pers Soc Psychol. (2006) 91:730. doi: 10.1037/0022-3514.91.4.730
18. Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. (2001) 56:227. doi: 10.1037//0003-066X.56.3.227
19. Harvey J, Delfabbro PH. Psychological resilience in disadvantaged youth: A critical overview. Aust Psychol. (2004) 39:3–13. doi: 10.1080/00050060410001660281
20. Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry. (2011) 56:258–65. doi: 10.1177/070674371105600504
21. Russo SJ, Murrough JW, Han M-H, Charney DS, Nestler EJ. Neurobiology of resilience. Nat Neurosci. (2012) 15:1475–84. doi: 10.1038/nn.3234
22. Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. (2012) 338:79–82. doi: 10.1126/science.1222942
23. Walsh F. Crisis, trauma, and challenge: A relational resilience approach for healing, transformation, and growth. Smith Coll Stud Soc Work. (2003) 74:49–71. doi: 10.1080/00377310309517704
24. Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health. (2008) 56:445–53. doi: 10.3200/JACH.56.44.445-454
25. Rutter M. Annual research review: Resilience–clinical implications. J Child Psychol Psychiatry. (2013) 54:474–87. doi: 10.1111/j.1469-7610.2012.02615.x
26. Zhang C, Ye M, Fu Y, Yang M, Luo F, Yuan J, et al. The psychological impact of the COVID-19 pandemic on teenagers in China. J Adolesc Health. (2020) 67:747–55. doi: 10.1016/j.jadohealth.2020.08.026
27. Lenzo V, Sardella A, Musetti A, Quattropani MC, Franceschini C. Longitudinal associations between resilience and mental health during the COVID-19 pandemic. Clin Neuropsy. (2024) 21:189. doi: 10.36131/cnfioritieditore20240304
28. Xu J, Yang X. The influence of resilience on stress reaction of college students during COVID-19: the mediating role of coping style and positive adaptive response. Curr Psychol. (2024) 43:12120–31. doi: 10.1007/s12144-022-04214-4
29. Yang C, Zhou Y, Xia M. How resilience promotes mental health of patients with DSM-5 substance use disorder? The mediation roles of positive affect, self-esteem, and perceived social support. Front Psychiatry. (2020) 11:588968. doi: 10.3389/fpsyt.2020.588968
30. Muniandy M, Richdale AL, Arnold SR, Trollor JN, Lawson LP. Inter-relationships between trait resilience, coping strategies, and mental health outcomes in autistic adults. Autism Res. (2021) 14:2156–68. doi: 10.1002/aur.2564
31. Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol. (2002) 58:307–21. doi: 10.1002/jclp.10020
32. Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. (2010) 30:479–95. doi: 10.1016/j.cpr.2010.03.003
33. Zimmerman MA, Stoddard SA, Eisman AB, Caldwell CH, Aiyer SM, Miller A. Adolescent resilience: resources and assets for informing prevention. Child Dev Perspect. (2013) 7:215–20. doi: 10.1111/cdep.12042
34. Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, et al. Stress response and the adolescent transition: Performance versus peer rejection stressors. Dev Psychopathol. (2009) 21:47–68. doi: 10.1017/S0954579409000042
35. Kogler L, Müller VI, Chang A, Eickhoff SB, Fox PT, Gur RC, et al. Psychosocial versus physiological stress—Meta-analyses on deactivations and activations of the neural correlates of stress reactions. Neuroimage. (2015) 119:235–51. doi: 10.1016/j.neuroimage.2015.06.059
36. McGorry PD, Mei C, Chanen A, Hodges C, Alvarez-Jimenez M, Killackey E. Designing and scaling up integrated youth mental health care. World Psychiatry. (2022) 21:61–76. doi: 10.1002/wps.20938
37. Jagger C. Mental health indicators in Europe. Rep no ESA/STAT/AC. (2001) 81:7–5. Available at: https://mdgs.un.org/unsd/disability/pdfs/ac.81-7-5.pdf (Accessed September 26, 2024).
38. Fusar-Poli P, de Pablo GS, De Micheli A, Nieman DH, Correll CU, Kessing LV, et al. What is good mental health? A scoping review. Eur Neuropsychopharmacol. (2020) 31:33–46. doi: 10.1016/j.euroneuro.2019.12.105
39. Greenspoon PJ, Saklofske DH. Toward an integration of subjective well-being and psychopathology. Soc Indic Res. (2001) 54:81–108. doi: 10.1023/A:1007219227883
40. Suldo SM, Shaffer EJ. Looking beyond psychopathology: The dual-factor model of mental health in youth. School Psychol Rev. (2008) 37:52–68. doi: 10.1080/02796015.2008.12087908
41. Chuang SP, Wu JYW, Wang CS. Resilience and quality of life in people with mental illness: A systematic review and meta-analysis. Neuropsychiatr Dis Treat. (2023) 19:507–14. doi: 10.2147/NDT.S392332
42. Ungar M. Resilience, trauma, context, and culture. Trauma Viol Abuse. (2013) 14:255–66. doi: 10.1177/1524838013487805
43. Zheng P, Gray MJ, Duan WJ, Ho SM, Xia M, Clapp JD. Cultural variations in resilience capacity and posttraumatic stress: A tri-cultural comparison. Cross-Cultural Res. (2020) 54:273–95. doi: 10.1177/1069397119887669
44. Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. (2011) 9:1–18. doi: 10.1186/1477-7525-9-8
45. Martin J. Critical Appraisal Checklist for Analytical Cross-Sectional Studies Vol. 7. Brisbane, Australia: Joanna Briggs Institute (2017) p. 2019–05. Available at: https://jbi.global/sites/default/files/2020-08/Checklist_for_Analytical_Cross_Sectional_Studies.pdf (Accessed September 27, 2024).
46. Hall NY, Le L, Majmudar I, Mihalopoulos C. Barriers to accessing opioid substitution treatment for opioid use disorder: A systematic review from the client perspective. Drug Alcohol Depend. (2021) 221:108651. doi: 10.1016/j.drugalcdep.2021.108651
47. Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Person Individual Differ. (2016) 102(2016):74–8. doi: 10.1016/j.paid.2016.06.069
48. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
49. Borenstein M. Effect sizes based on means. In: Introduction to meta-analysis. Chichester, West Sussex: John Wiley & Sons Press (2009). p. 21-32. doi: 10.1002/9780470743386.ch4
50. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
51. Achour M, Nor MRM. The effects of social support and resilience on life satisfaction of secondary school students. J Acad Appl Stud. (2014) 4:12–20.
52. Anyan F, Bizumic B, Hjemdal O. Specificity in mediated pathways by anxiety symptoms linking adolescent stress profiles to depressive symptoms: Results of a moderated mediation approach. J Affect Disord. (2018) 228:109–17. doi: 10.1016/j.jad.2017.12.011
53. Doyle N, MacLachlan M, Fraser A, Stilz R, Lismont K, Cox H, et al. Resilience and well-being amongst seafarers: cross-sectional study of crew across 51 ships. Int Arch Occup Environ Health. (2016) 89:199–209. doi: 10.1007/s00420-015-1063-9
54. Chow KM, Tang WKF, Chan WHC, Sit WHJ, Choi KC, Chan S. Resilience and well-being of university nursing students in Hong Kong: a cross-sectional study. BMC Med Educ. (2018) 13:1–8. doi: 10.1186/s12909-018-1119-0
55. De la Fuente J, Santos FH, Garzón-Umerenkova A, Fadda S, Solinas G, Pignata S. Cross-sectional study of resilience, positivity and coping strategies as predictors of engagement-burnout in undergraduate students: implications for prevention and treatment in mental well-being. Front Psychiatry. (2021) 12:596453. doi: 10.3389/fpsyt.2021.596453
56. Hjemdal O, Vogel PA, Solem S, Hagen K, Stiles TC. The relationship between resilience and levels of anxiety, depression, and obsessive–compulsive symptoms in adolescents. Clin Psychol Psychother. (2011) 18:314–21. doi: 10.1002/cpp.719
57. Ibigbami OI, Folayan MO, Oginni OA, Lusher J. Mediating effects of psychological resilience and self-esteem on the association between early childhood adversity and depressive symptoms among adolescents in Nigeria. Adversity Resilience Sci. (2024) 5:257–66. doi: 10.1007/s42844-024-00133-4
58. Las-Hayas C, Mateo-Abad M, Vergara I, Izco-Basurko I, González-Pinto A, Gabrielli S, et al. Relevance of well-being, resilience, and health-related quality of life to mental health profiles of European adolescents: results from a cross-sectional analysis of the school-based multinational UPRIGHT project. Soc Psychiatry Psychiatr Epidemiol. (2022) 57(2):279–91. doi: 10.1007/s00127-021-02156-z
59. Lau WKW. The role of resilience in depression and anxiety symptoms: A three-wave cross-lagged study. Stress Health. (2022) 38(4):804–12. doi: 10.1002/smi.3136
60. Marulanda S, Addington J. Resilience in individuals at clinical high risk for psychosis. Early Intervent Psychiatry. (2016) 10:212–9. doi: 10.1111/eip.2016.10.issue-3
61. Masuyama A, Kubo T, Shinkawa H, Sugawara D. The roles of trait and process resilience in relation of BIS/BAS and depressive symptoms among adolescents. PeerJ. (2022) 10:e13687. doi: 10.7717/peerj.13687
62. Rayani AM, Alodhailah AM, Alreshidi SM. A cross-sectional study of resilience and well-being among nursing students in Saudi Arabia. SAGE Open Med. (2024) 12:20503121241245224. doi: 10.1177/20503121241245224
63. Rew L, Kelley M, Preston A. Psychological capital variables as protective factors in indigenous youth experiencing homelessness. Arch Psychiatr Nurs. (2024) 51:235–40. doi: 10.1016/j.apnu.2024.06.009
64. Scheiner C, Seis C, Kleindienst N, Buerger A. Psychopathology, protective factors, and COVID-19 among adolescents: a structural equation model. Int J Environ Res Public Health. (2023) 20:2493. doi: 10.3390/ijerph20032493
65. Shek DT, Liang LY. Psychosocial factors influencing individual well-being in Chinese adolescents in Hong Kong: A six-year longitudinal study. Appl Res Qual Life. (2018) 13:561–84. doi: 10.1007/s11482-017-9545-4
66. Shi M, Liu L, Sun X, Wang L. Associations between symptoms of attention-deficit/hyperactivity disorder and life satisfaction in medical students: the mediating effect of resilience. BMC Med Educ. (2018) 18:164. doi: 10.1186/s12909-018-1261-8
67. Sia SK, Aneesh A. Single-parent adolescents’ Resilience and psychological well-being: the role of social competence and emotion regulation. J Indian Assoc Child Adolesc Ment Health. (2024) 20:205–11. doi: 10.1177/09731342241239441
68. Visier-Alfonso ME, Sarabia-Cobo C, Cobo-Cuenca AI, Nieto-López M, López-Honrubia R, Bartolomé-Gutiérrez R, et al. Stress, mental health, and protective factors in nursing students: An observational study. Nurse Educ Today. (2024) 139:106258. doi: 10.1016/j.nedt.2024.106258
69. Zhu H, Song J, Zhang R, Wang B, Shen X. Developmental changes in and the relationship between psychological resilience and mental health problems in adolescents relocated for poverty alleviation in the context of COVID-19 epidemic prevention and control. Front Public Health. (2023) 11:1118535. doi: 10.3389/fpubh.2023.1118535
70. Konaszewski K, Niesiobędzka M, Surzykiewicz J. Resilience and mental health among juveniles: role of strategies for coping with stress. Health Qual Life Outcomes. (2021) 19:58. doi: 10.1186/s12955-021-01701-3
71. Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Military Med Res. (2020) 7:1–11. doi: 10.1186/s40779-020-00238-8
72. Dunn LB, Iglewicz A, Moutier C. A conceptual model of medical student well-being: promoting resilience and preventing burnout. Acad Psychiatry. (2008) 32:44–53. doi: 10.1176/appi.ap.32.1.44
73. Ramos-Díaz E, Rodríguez-Fernández A, Axpe I, Ferrara M. Perceived emotional intelligence and life satisfaction among adolescent students: The mediating role of resilience. J Happiness Stud. (2019) 20:2489–506. doi: 10.1007/s10902-018-0058-0
74. Lara-Cabrera ML, Betancort M, Muñoz-Rubilar CA, Rodríguez Novo N, De las Cuevas C. The mediating role of resilience in the relationship between perceived stress and mental health. Int J Environ Res Public Health. (2021) 18:9762. doi: 10.3390/ijerph18189762
75. Mesman E, Vreeker A, Hillegers M. Resilience and mental health in children and adolescents: an update of the recent literature and future directions. Curr Opin Psychiatry. (2021) 34:586–92. doi: 10.1097/YCO.0000000000000741
76. Tang Y, Ma Y, Zhang J, Wang H. The relationship between negative life events and quality of life in adolescents: mediated by resilience and social support. Front Public Health. (2022) 10:980104. doi: 10.3389/fpubh.2022.980104
77. Ioannidou L, Michael K. Mental health and well-being in children: the protective role of resilience, self-esteem, self-efficacy, and parent-child relationship. psychol Thought. (2024) 17:483–507. doi: 10.37708/psyct.v17i2.946
78. Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Pers Individ Dif. (2015) 76:18–27. doi: 10.1016/j.paid.2014.11.039
79. Klainin-Yobas P, Vongsirimas N, Ramirez DQ, Sarmiento J, Fernandez Z. Evaluating the relationships among stress, resilience and psychological well-being among young adults: a structural equation modelling approach. BMC Nurs. (2021) 20:119. doi: 10.1186/s12912-021-00645-9
80. Masten AS, Obradović J, Burt KB. Resilience in Emerging Adulthood: Developmental Perspectives on Continuity and Transformation. In: Arnett JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st century. Washington, DC, United States: American Psychological Association (2006). p. 173–90. doi: 10.1037/11381-007
81. Madewell AN, Ponce-Garcia E. Assessing resilience in emerging adulthood: The resilience scale (RS), Connor–Davidson resilience scale (CD-RISC), and scale of protective factors (SPF). Pers Individ Dif. (2016) 97:249–55. doi: 10.1016/j.paid.2016.03.036
82. Gibb SJ, Fergusson DM, Horwood LJ. Burden of psychiatric disorder in young adulthood and life outcomes at age 30. Br J Psychiatry. (2010) 197:122–7. doi: 10.1192/bjp.bp.109.076570
83. World Health Organization. Mental health (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (Accessed October 5, 2024).
84. Wen L, Yang K, Chen J, He L, Xiu M, Qu M. Associations between resilience and symptoms of depression and anxiety among adolescents: Examining the moderating effects of family environment. J Affect Disord. (2023) 340:703–10. doi: 10.1016/j.jad.2023.08.063
85. Gallagher ML, Miller AB. Suicidal thoughts and behavior in children and adolescents: an ecological model of resilience. Adolesc Res Rev. (2018) 3:123–54. doi: 10.1007/s40894-017-0066-z
86. Srivastava AV, Brown R, Newport DJ, Rousseau JF, Wagner KD, Guzick A, et al. The role of resilience in the development of depression, anxiety, and post-traumatic stress disorder after trauma in children and adolescents. Psychiatry Res. (2024) 334:115772. doi: 10.1016/j.psychres.2024.115772
87. Ağırkaya K, Erdem R. Psikolojik sağlamlık: Sağlık çalışanları açısından bir değerlendirme. Pamukkale Üniversitesi İşletme Araştırmaları Dergisi. (2023) 10:656–78. doi: 10.47097/piar.1254928
88. Wu Y, Yu W, Wu X, Wan H, Wang Y, Lu G. Psychological resilience and positive coping styles among Chinese undergraduate students: a cross-sectional study. BMC Psychol. (2020) 8:79. doi: 10.1186/s40359-020-00444-y
89. Simón-Saiz MJ, Fuentes-Chacón RM, Garrido-Abejar M, Serrano-Parra MD, Larrañaga-Rubio E, Yubero-Jiménez S. Influence of resilience on health-related quality of life in adolescents. Enfermería Clínica (English Edition). (2018) 28:283–91. doi: 10.1016/j.enfcli.2018.06.003
90. Altuntaş S, Genç H. Mutluluğun yordayıcısı olarak psikolojik sağlamlık: Öğretmen örnekleminin incelenmesi. Hacettepe Üniversitesi Eğitim Fakültesi Dergisi. (2020) 35:936–48. doi: 10.16986/HUJE.2018046021
91. Yu X, Zhang J. Resilience: The psychological mechanism for recovery and growth during stress. Adv psychol Sci. (2005) 13:658. Available at: https://journal.psych.ac.cn/adps/EN/Y2005/V13/I05/658 (Accessed October 6, 2024).
92. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Personal: an Int J. (2007) 35:19–30. doi: 10.2224/sbp.2007.35.1.19
93. Mak WW, Ng IS, Wong CC. Resilience: enhancing well-being through the positive cognitive triad. J Couns Psychol. (2011) 58:610. doi: 10.1037/a0025195
94. Burt KB, Paysnick AA. Resilience in the transition to adulthood. Dev Psychopathol. (2012) 24:493–505. doi: 10.1017/S0954579412000119
95. World Health Organization. Promoting mental health: concepts, emerging evidence, practice: a report of the World Health Organization. Geneva: Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne (2005). p. 9791157467679. Available at: https://apps.who.int/iris/bitstream/handle/10665/42940/9241591595.pdf (Accessed October 7, 2024).
96. Yoo C, Kahng SK. Two-dimensional mental health and related predictors among adolescents in Korea. Asian Soc Work Policy Rev. (2019) 13:66–77. doi: 10.1111/aswp.12157
97. Grych J, Taylor E, Banyard V, Hamby S. Applying the dual factor model of mental health to understanding protective factors in adolescence. Am J Orthopsy. (2020) 90:458. doi: 10.1037/ort0000449
98. Kong L, Fang M, Ma T, Li G, Yang F, Meng Q, et al. Positive affect mediates the relationships between resilience, social support and posttraumatic growth of women with infertility. Psycho Health Med. (2018) 23:707–16. doi: 10.1080/13548506.2018.1447679
99. Hsu CJ, Ayres A, Payne L. Evaluating outcomes following adolescent and youth mental health inpatient admissions: A systematic review. Early Interv Psychiatry. (2024) 18(7):481–501. doi: 10.1111/eip.13499
100. Färber F, Rosendahl J. Trait resilience and mental health in older adults: A meta - analytic review. Pers Ment Health. (2020) 14:361–75. doi: 10.1002/pmh.1490
101. Blessin M, Lehmann S, Kunzler AM, van Dick R, Lieb K. Resilience interventions conducted in western and eastern countries—a systematic review. Int J Environ Res Public Health. (2022) 19:6913. doi: 10.3390/ijerph19116913
102. Chai XY, Li XY, Cao J, Lin DH. A short form of the Chinese positive youth development scale: development and validation in a large sample. Stud Psychol Behav. (2020) 18:631–7. Available at: https://psybeh.tjnu.edu.cn/CN/Y2020/V18/I5/631 (Accessed October 6, 2024).
103. Cleary A, Dowling M. Knowledge and attitudes of mental health professionals in Ireland to the concept of recovery in mental health: a questionnaire survey. J Psychiatr Ment Health Nurs. (2009) 16:539–45. doi: 10.1111/j.1365-2850.2009.01411.x
104. Li S, Hao C, Ren J. Cross-cultural adaptation and validation of the Chinese version of the Trauma Resiliency Scale (tRS-18). BMC Psychiatry. (2024) 24:743. doi: 10.1186/s12888-024-06166-4
105. Wang Y, Derakhshan A, Rahimpour H. Developing resilience among Chinese and Iranian EFL teachers: A multi-dimensional cross-cultural study. J Multilingual Multicult Dev. (2024) 45:2111–28. doi: 10.1080/01434632.2022.2042540
106. Gucciardi DF, Jackson B, Coulter TJ, Mallett CJ. The Connor-Davidson Resilience Scale (CD-RISC): Dimensionality and age-related measurement invariance with Australian cricketers. Psychol Sport Exercise. (2011) 12:423–33. doi: 10.1016/j.psychsport.2011.02.005
107. Ahern NR, Kiehl EM, Lou Sole M, Byers J. A review of instruments measuring resilience. Issues Compr Pediatr Nurs. (2006) 29:103–25. doi: 10.1080/01460860600677643
108. Karaırmak Ö. Establishing the psychometric qualities of the Connor–Davidson Resilience Scale (CD-RISC) using exploratory and confirmatory factor analysis in a trauma survivor sample. Psychiatry Res. (2010) 179:350–6. doi: 10.1016/j.psychres.2009.09.012
Keywords: resilience, mental health, adolescents, young adults, meta-analysis, correlation
Citation: Luo S, Hu J, Zhang J, Mei Z, Tang Z and Luo S (2025) The correlation between resilience and mental health of adolescents and young adults: a systematic review and meta-analysis. Front. Psychiatry 16:1536553. doi: 10.3389/fpsyt.2025.1536553
Received: 29 November 2024; Accepted: 15 January 2025;
Published: 10 February 2025.
Edited by:
Yibo Wu, Peking University, ChinaReviewed by:
Avital Laufer, Netanya Academic College, IsraelMagdalena Anna Lazarewicz, Medical University of Warsaw, Poland
Hannah Süss, Psychiatric University Hospital Zurich, Switzerland
Copyright © 2025 Luo, Hu, Zhang, Mei, Tang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi Luo, bHVvc2hpMDYwNEAxMjYuY29t
 Shulai Luo
Shulai Luo Jiangtao Hu
Jiangtao Hu Junshuai Zhang
Junshuai Zhang Zhengyang Mei
Zhengyang Mei Zhongjian Tang
Zhongjian Tang Shi Luo
Shi Luo