
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 10 March 2025
Sec. Anxiety and Stress Disorders
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1479190
 Milutin Vracevic1,2†
Milutin Vracevic1,2† Vedrana Pavlovic3†
Vedrana Pavlovic3† Natasa Todorovic1,2
Natasa Todorovic1,2 Natasa M. Milic3,4
Natasa M. Milic3,4 Bojana Matejic5
Bojana Matejic5 Predrag Brkic6
Predrag Brkic6 Nikola V. Milic3
Nikola V. Milic3 Marko Savic3
Marko Savic3 Srdjan Masic7
Srdjan Masic7 Andrija Pavlovic8
Andrija Pavlovic8 Vladislav Stanisic3
Vladislav Stanisic3 Ana Tasic2
Ana Tasic2 Dragan Spaic7
Dragan Spaic7 Sandra Matovic7*
Sandra Matovic7* Danijela Tiosavljevic8,9‡
Danijela Tiosavljevic8,9‡ Dejana Stanisavljevic3*‡
Dejana Stanisavljevic3*‡Introduction: This study explored the complex relationship between anxiety, depression, compassion fatigue, and satisfaction among long-term care (LTC) workers following the COVID-19 pandemic. In addition, the study assessed psychometric properties of the Professional Quality of Life (ProQOL) scale, to ensure a reliable and valid instrument for identifying compassion fatigue and satisfaction in the Serbian healthcare system.
Methods: A cross-sectional study was conducted across LTC facilities in the Republic of Serbia. A ProQOL was administered to physicians, nurses, and aids, to measure compassion fatigue (including burnout and secondary traumatic stress) and compassion satisfaction. The following standardized instruments were also distributed: Secondary Traumatic Stress Scale (STSS), Depression Anxiety and Stress Scale 21 (DASS-21) and 12-Item Short-Form Health 36 Survey (SF-12).
Results: A total of 300 LTC workers participated, mostly women (86.3%), with an average age of 45.4 ± 10.5 years and a median work experience of 15 years (range: 1 to 42 years). The study reported a significant presence of anxiety and depression symptoms (53.3% and 43.3%, respectively), with LTC workers experiencing moderate levels of compassion fatigue, as indicated by burnout (58.3%) and stress (57.3%) subscales, and moderate or high levels of compassion satisfaction (49.0% and 50.0%, respectively). The study demonstrated that anxiety impacts depression both directly and indirectly (p<0.05). Specifically, burnout and compassion satisfaction mediated the positive effect of anxiety on depression, indicating that increased anxiety led to higher burnout and lower compassion satisfaction, which resulted in greater depression (p<0.05). The three-factor structure of the ProQOL was validated (IFI, TLI, and CFI were above the cut-off of ≥0.95, and the RMSEA was below the suggested value of ≤ 0.06). The Cronbach α of the three subscales was above 0.8, indicating good scale reliability.
Conclusion: This study contributes to the broader literature on LTC workers wellbeing by examining the complex interplay between professional quality of life, anxiety, and depression. The findings should guide decision-makers in developing targeted interventions and policies that promote the psychological resilience and well-being of LTC workers, thereby enhancing both individual and organizational outcomes in the healthcare sector.
The psychological wellbeing of long-term care (LTC) workers is critical to the effective functioning of healthcare systems worldwide (1). During the past two decades this has been a growing concern due to its impact on resident outcomes, healthcare costs, and overall system performance (2–4). This concern has been exacerbated by significant declines in LTC workers mental health, a trend particularly pronounced since the onset of the COVID-19 pandemic (5).
The COVID-19 pandemic presented unprecedented challenges for healthcare systems globally, leading to heightened levels of psychological distress among LTC workers. These challenges included increased work demands, uncertainties regarding resources, social isolation, shifts in healthcare delivery, and heightened exposure to suffering and mortality (5–7). These stressors have had tangible impacts, with an alarming 18% of LTC workers leaving their positions, a departure rate significantly higher than that observed in other professions (8).
Occupational wellness among health care workers is a multifaceted concept that is commonly assessed using various psychometric tools. For this study, the Professional Quality of Life Scale (ProQOL) was selected due to its established relevance, widespread use, and robust psychometric properties (9). The ProQOL assesses two key dimensions: compassion fatigue (CF) and compassion satisfaction (CS). CF, as conceptualized by Figley, refers to a state of exhaustion and dysfunction - biological, psychological, and social - resulting from prolonged exposure to the suffering of others. It can result in a depletion of emotional resources leading to a secondary traumatic stress (STS) response similar to that experienced by trauma survivors themselves (10, 11). In contrast, CS represents positive psychological outcomes derived from helping others, serving as a protective factor against burnout (BO) and STS (10).
While CF has been studied predominantly among nurses, its relevance extends to various professionals where individuals regularly encounter trauma and suffering, such as emergency responders, law enforcement, educators, and social service providers. The prevalence and risk factors associated with CF are still being clarified across these diverse contexts, highlighting the need for continued research in this area (11–18). Moreover, understanding the relationship between psychological factors such as anxiety and depression among LTC workers is crucial. Both anxiety and depression are prevalent among LTC workers (5, 19–21), with studies indicating significant comorbidity and shared underlying mechanisms, as suggested by the tripartite model of anxiety and depression (22). This model suggests that while anxiety and depression share a common component of negative affectivity, they also exhibit distinct features - such as physiological hyperarousal specific to anxiety and diminished positive affectivity specific to depression - that differentiate these conditions (22–24).
Despite the established correlations between anxiety, depression, and quality of life related to occupation (25), there remains a notable gap in research examining how professional quality of life may mediate the relationship between anxiety and depression among LTC workers. Addressing this gap is critical for developing targeted interventions that promote LTC workers well-being and mitigate the risks of mental health disorders within this vulnerable population.
This study intends to fill this gap by investigating the effects of professional quality of life on the relationship between anxiety and depression among Serbian LTC workers. By utilizing structural equation modeling (SEM) techniques, this research aimed to provide a nuanced understanding of how occupational factors, specifically CF and CS, influence the mental health outcomes of LTC workers. In addition, as the validity and reliability of the ProQOL scale have not yet been studied in Serbia, this study also aimed to assess the psychometric properties of the ProQOL, to ensure a reliable and valid instrument for identifying the level of psychological wellbeing of workers in the Serbian LTC system.
A cross-sectional study was conducted among workers in LTC facilities (gerontology centers/retirement homes) during 2024 across the Republic of Serbia. In order to conduct this study, the Faculty of Medicine of the University of Belgrade collaborated with the Red Cross of Serbia and the European Commission and Austrian Development Agency.
According to the Republic Institute for Social Protection, in 2024, there were 40 registered gerontology centers and retirement homes in Serbia, with 71 physicians, 536 nurses, and 865 aids currently employed. The minimum sample size required for performing factor analysis was determined based on the following Tabachnick and Fidell’s (26) requirements: (1) a minimum of 150 respondents for factor analysis, and (2) at least 5 to 7 respondents per each item in the questionnaire. Since ProQOL questionnaire consists of 30 items, the minimum sample size for this study was 210 participants. Eighteen long-term care institutions in Serbia participated in the study: Apatin, Beograd, Bačka Palanka, Blace, Bečej, Jelenac, Kanjiža, Kragujevac, Kruševac, Mataruška Banja, Mladenovac, Novi Kneževac, Novi Pazar, Pančevo, Niš, Surdulica, Prokuplje, and Ruma. The study included physicians, nurses, and aids who were employed by the selected institutions. Exclusion criteria were: discontinuity in employment exceeding one year, such as extended study residencies abroad, prolonged sick leave, or multiple job changes within the past five years; exposure to significant psycho-physical trauma unrelated to the professional setting; and refusal to participate in the research.
The data were collected by self-reported questionnaire consisted of six sections: sociodemographic section, quality of life, professional quality of life, depression, anxiety and stress, secondary traumatic stress and COVID-19. The participants’ cooperation was not affected by the length of the questionnaire. All subjects involved in the study provided informed consent.
Sociodemographic section: Following sociodemographic characteristics were collected: age, sex, marital status, community, educational background (level of education), and occupational data (work experience, occupation).
Professional Quality of Life Scale (ProQOL): CS and CF were measured using the ProQOL, with the latter composed of BO and STS. CS denotes to the gratification derived from performing their responsibilities and help others. This construct comprises 10 items including “I get satisfaction from being able to help people”. Higher ratings indicate greater pleasure and perceptions of one’s effectiveness as a caregiver. The BO construct assesses emotions of hopelessness and difficulty performing one’s job effectively. This construct also has ten items such as “I feel worn out because of my work as a healthcare provider”. The STS construct describes work related secondary exposure to traumatic situations experienced by others. There are ten items composing this construct including “I feel depressed because of the traumatic experiences of the people I help”. The ProQOL instrument measures these three constructs using 30 items rated on a five-point scale (1 – never to 5 – very often). Each item assesses how frequently in the last 30 days a respondent has experienced symptoms. The three constructs each range from 10 to 50. The validity and reliability of the scale is confirmed for various populations, and the scale has been used globally across diverse target populations (27).
Translation and adaptation of ProQOL: The questionnaire was translated into Serbian language and adapted with permission from the copyright owner (ProQOL Office at the Center for Victims of Torture). According to the standard forward and backward translation procedure, the original English version was translated into Serbian (28, 29). Differences observed between the original and back-translated version were resolved through consensus. The Serbian version of ProQOL was previously tested among 20 participants in order to achieve better clarity and understanding. Based on the feedback received from the participants, the final version of ProQOL in the Serbian language was designed and distributed.
Depression Anxiety and Stress Scale 21 (DASS-21): The DASS-21 is a survey tool designed to assess general negative mood symptoms experienced over the past week. It comprises three scales: depression, anxiety, and stress. Participants rate each statement on a 4-point scale ranging from 0 (not at all) to 3 (very much/most of the time). Both the DASS and DASS-21 have shown strong psychometric properties and high internal consistency across different populations. Cronbach α for the Serbian version of DASS-21 was 0.959 (30).
Secondary Traumatic Stress Scale (STSS): The STSS scale includes 17 questions grouped into three subscales: intrusion (5 items), avoidance (7 items), and arousal (5 items). Items are rated on a 5-point Likert scale ranging from 1 to 5 (“never” to “very often”). Total scores range from 17 to 85; a higher score indicates higher levels of STSS. Scores less than 28 indicate little or no STSS; 28 to 37 indicate mild STSS; 38 to 43 indicate moderate STSS; 44 to 48 indicate high STSS; and > 49 indicate severe STSS. Cronbach α for the Serbian version of STSS was 0.955 in total, and for the subcategories were 0.863 for intrusion, 0.888 for avoidance, and 0.891 for arousal (31).
Short Form Health Survey (SF-12): The SF-12 is a self-reported questionnaire assessing a health-related quality of life. It includes the same eight health domains as the SF-36 but with fewer questions. Answers to SF-12 items are expressed on dichotomous (no/yes) scale or on ordinal scale (always to never; excellent to poor). The scoring yields two summary measures: physical health (PCS) and mental health (MCS) (ranging from 0 to 100). Higher PCS and MCS scores indicate better physical and mental health quality of life, respectively. The SF-12 has been shown to be reliable and valid in different populations (32).
COVID-19 Related Questions: Participants were asked to indicate how the COVID-19 outbreak impacted their working conditions and whether they needed psychological help and additional education during the pandemic.
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethical Review Board of the Faculty of Medicine University of Belgrade (reference number: 27/VII-9). Participation was voluntary and anonymous.
Descriptive statistics, including means and confidence intervals for numerical variables, and numbers with percentages for categorical variables were used to summarize the participants’ characteristics. The psychometric properties of the Serbian version of the ProQOL scale were evaluated through an analysis of its factorial structure and internal consistency (reliability). Confirmatory factor analysis (CFA) was conducted to validate the scale’s original three-dimensional structure. Path analysis was chosen for its capability to evaluate both direct and indirect effects of variables through simultaneous modeling of regression relationships. Multiple measures were utilized to assess the model fit, including the χ² test, comparative fit index (CFI), Tucker–Lewis index (TLI), incremental fit index (IFI), and root mean square error of approximation (RMSEA). A χ² test with a p-value greater than 0.05 indicates a good fit, and a value less than twice the degrees of freedom is considered favorable. An RMSEA value below 0.05 indicates good model fit, while CFI, TLI, and IFI values above 0.95 suggest adequate fit. Path estimates are presented as standardized regression coefficients, illustrating the strength of relationships between variables. The bootstrap method (repeated sampling 5000 times) was used to test the mediating effect of ProQOL, and a bias-corrected 95% confidence interval was calculated to test the significance of the mediating effect. Pearson’s correlation coefficient was used to assess concurrent validity with the MCS domain of the SF12, STSS and DASS-21 subscales. The internal consistency of the ProQOL was assessed by using Cronbach’s alpha coefficient (ranges from 0-1, the latter meaning perfect reliability). In all analyses, the significance level was set at 0.05. Statistical analysis was done using Amos 21 (IBM SPSS Inc., Chicago, IL, USA, 2012) and IBM SPSS Statistics 25 software.
A total of 300 LTC workers participated, with an average age 45.4 ± 10.5 years, of which 44.7% (n=134) were nurses, 48.3% (n=145) were aids and 7.0% (n=21) were physicians. Most of the participants were female (86.3%); the majority married or partnered (67.7%). The majority of participants had a second level of education or lower (76.3%), and were living in urban areas (79.7%). The median work experience was 15 years, ranging from several months to 42 years. The participants reported significant anxiety and depression symptoms (53.3% and 43.3%, respectively) (Table 1). Cronbach α for the DASS-21 was 0.955 indicating excellent reliability. The reported average PCS and MCS were 44.9 ± 9.2 and 43.6 ± 11.3, respectively. The Cronbach’s α value (0.902) reflected excellent reliability of SF-12. The mean STSS total scale was 14.21 (95%CI 12.97-15.45). The STSS’s Cronbach α was 0.955 (excellent reliability). Most of participants stated their working conditions were more difficult during the COVID-19, one third needed psychological help (33.7%) and half of the studied population needed additional education during COVID-19. Detailed characteristics of study participants are presented in Table 1.
The three-factor structure of the ProQOL has been validated with maximum likelihood CFA, but the model failed to meet minimum fit criteria. Then, CFA was run on the same sample to test the 26-item (Items 2,4,15 and 29 dropped) three-factor model fit. The 26-item three-factor structure of the ProQOL demonstrated a good fit of the data to the hypothesized model. The chi-square test rejected the three-dimensional model (χ2 = 409.597, P < 0.001), as we expected, due to the large sample size. Values for fit indices IFI (0.96), TLI (0.95) and CFI (0.96) were above the cut-off of ≥ 0.95. The RMSEA value of 0.04 (0.03–0.05) was below the suggested value of 0.06. All standardized factor loadings were statistically significant, and ranged from 0.38 to 0.86 (see Figure 1).
The concurrent validity of the ProQOL was examined by using the MCS of the SF-12 questionnaire, STSS and DASS-21 subscales. CS correlated positively with SF12 and also had moderate negative correlations with STSS and DASS-21 subscales (p<0.001 for all analyses). BO and STS correlated negatively with SF-12 and also had moderate positive correlations with STSS and DASS-21 (p<0.001 for all analyses) indicating adequate validity of the ProQOL instrument (Table 2).
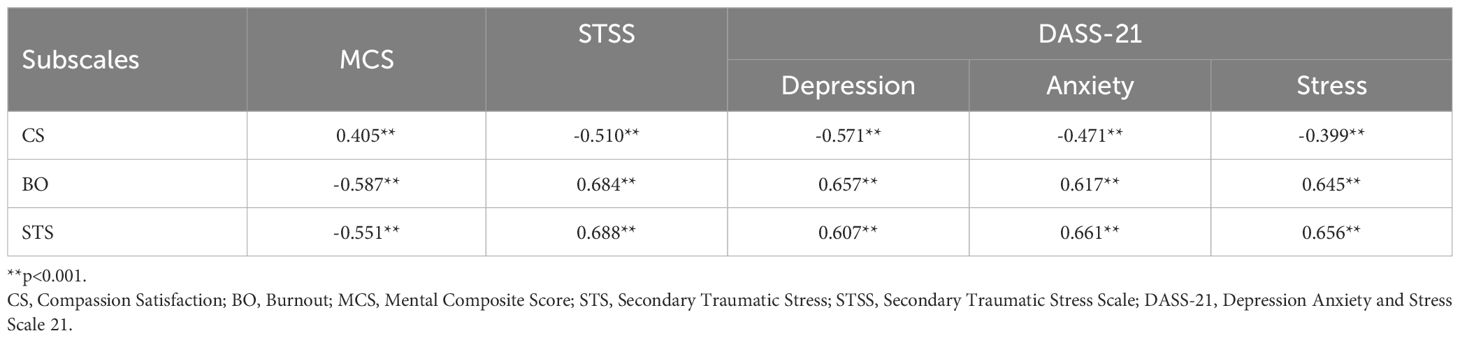
Table 2. Correlations between ProQOL and SF-12 mental health subscale, STSS and DASS-21 depression, anxiety and stress scales.
Analysis of the internal consistency of the Serbian version of the ProQOL showed the Cronbach α of the entire scale of 0.72, indicating good scale reliability. The alpha coefficients of the three subscales were estimated to be 0.88 for CS, 0.82 for BO, and 0.84 for STS. For the test-retest, 20 participants completed the retest, and the ICC ranged from 0.81 to 0.95, indicating good test-retest reliability.
Descriptive statistics of the ProQOL dimensions are shown in Table 3. The average score on the CS scale was 40.28 (SD=6.81), on the BO scale 23.71 (SD=6.89) and on the STS scale 25.07 (SD=7.18). The majority of the sample had a moderate or high level of CS (49.0% and 50.0%, respectively) with moderate levels of CF represented by the BO (58.3%) and STS (57.3%) subscales. It is important to note that very few participants scored low on CS (n=3,1%) and high on STS (n=2, 0.7%), while no participant scored high on BO. Both, the floor and the ceiling effect were below 10% indicating that the scale is well-balanced.
The hypothesized relationships among the variables were tested by path analysis, using a maximum likelihood estimate (Figure 2). Standardized coefficient (B) was used to estimate the effects. The best fit of the path model was achieved with χ2 = 11.113, df=8, CMIN/DF=1.389, p=0.195; TLI=0.991, IFI=0.997, CFI=0.997, and RMSEA=0.036. The constructed path model accounted for 75.1% of the depression. According to this model, anxiety and BO were directly positively related to depression, and CS was directly negatively related to depression. Among variables that directly affected depression, anxiety had the highest effect (B=-0.673), and BO (B=0.145) had the lowest effect. The significant mediating role of CS and BO was also identified in the model. The indirect effect of anxiety on depression through CS was significant. However, although anxiety was associated with lower CS, the mediating effect became positive. In other words, anxiety reduced CS, which in turn resulted in greater depression. The indirect effect of anxiety on depression through BO was both positive and significant, meaning that, in the studied population, greater anxiety was associated with greater BO, which in turn was associated with greater depression. In other words, anxiety increased BO, which in turn resulted in greater depression. Independent of these two mechanisms, there was no evidence that anxiety influenced depression by changing the STS. Age and PCS had significant direct effect on STS, while PCS also had significant indirect effect on depression via BO. The need for psychological help during COVID-19 had significant direct effect on CS, and indirect effect on depression via CS. Direct, indirect, and total effects are shown in Table 4.
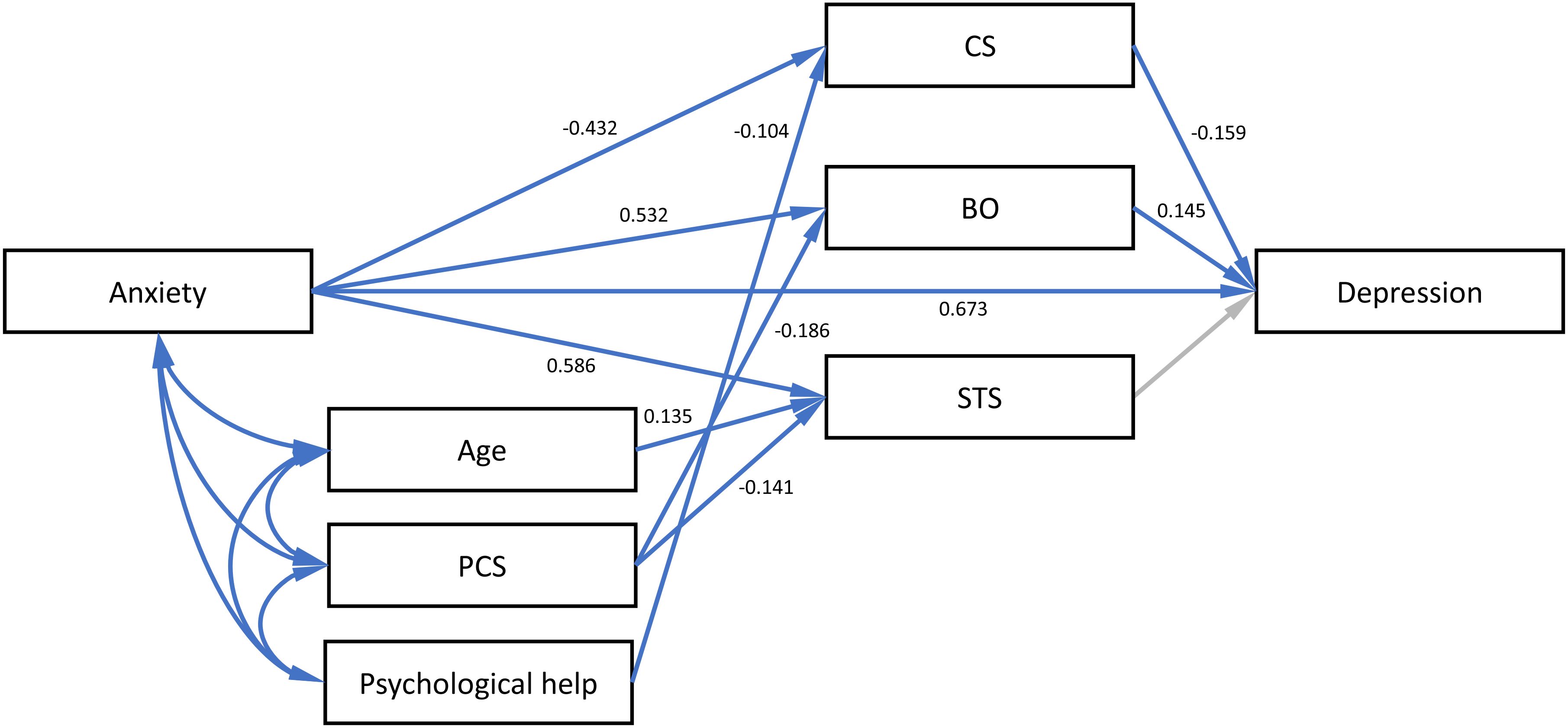
Figure 2. Path model presenting the mediating effects of ProQOL on the relationship between anxiety and depression on a sample of long term care homes staff in Serbia. Arrows colored blue identify significant loadings.
This study explored the complex relationship between anxiety, depression, and professional quality of life among frontline staff at LTC facilities in Serbia following the COVID-19 pandemic. Findings revealed significant levels of anxiety and depression symptoms, with staff experiencing moderate CF and moderate to high CS. The study demonstrated that anxiety impacts depression both directly and indirectly. Specifically, BO and CS mediated the positive effect of anxiety on depression, indicating that increased anxiety led to higher BO and lower CS, which subsequently resulted in greater depression.
The factorial validity of the three-factor model for the 26-item scale was confirmed, although items 2, 4, 15, and 29 were excluded due to low factor loadings. These changes align with previous validation studies (33–38). Keesler, for instance, reported the removal of items 2, 5, 15, and 29 due to similar issues (33). Samson et al. found that four items were dropped from the ProQOL scale due to inadequate internal consistency in data from healthcare professionals (38). Similarly, Galiana et al. identified that items 2, 4, and 29 had low factor loadings (35). To summarize, while the ProQOL components have shown satisfactory validity overall, variations in the psychometric properties of the ProQOL have been observed in different studies and populations (33, 35, 36, 38).
In this study, most respondents reported high CS and fulfillment in their work, with moderate levels of BO and STS, suggesting a generally acceptable professional quality of life. However, further improvement in mental health support for these professionals is needed, which could enhance their job retention and indirectly improve care quality in LTC facilities. Our research also found a positive correlation between CS and MCS, and negative correlations with STSS and DASS-21 subscales. This suggests that higher empathy levels are associated with better mental health and lower levels of depression, anxiety, and stress. Conversely, higher BO and STS correlate with worse mental health outcomes and increased levels of depression, anxiety, and stress, as indicated by the negative correlation with MCS and positive correlation with STSS and DASS-21 subscales.
Compared to studies conducted during the pandemic in Spain (39) and USA (6), our sample showed lower levels of CF. A study from USA found levels of CS similar to our results and reported no high BO among healthcare workers, aligning with our findings (40). Despite this, both our study and others indicate moderate to high levels of CF and BO among healthcare professionals, irrespective of the pandemic’s impact. This underscores the necessity for long-term interventions to prevent these issues. BO requires a multifaceted approach involving communication, teamwork, meditation, and mindfulness (41). To reduce CF, compassion skills programs should be implemented to enhance both CS and overall quality of life, which would improve patient care and safety (42). However, addressing this issue should focus not only on individuals but also on institutional responsibilities (43). The culture within these institutions must evolve, requiring strong commitment from leadership and the support of advocacy champions who can raise awareness about the risks of BO and CF, as well as strategies to mitigate them. Evidence-based services and institutional support are crucial for protecting healthcare professionals, ensuring adequate staffing, promoting psychological care, and strengthening the public health system.
With increasing resource constraints and reliance on part-time caregivers, stress levels and patient care quality are concerns. High BO levels have been reported among caregivers (44) and are unlikely to improve with rising demands. STS from observing traumatic experiences negatively impacts professionals’ health. Lazarus and Folkman’s Transactional Model of stress emphasizes the person–environment transaction and highlights the role of individual appraisal processes in shaping stress responses. Stressors are evaluated through primary appraisal (relevance of stressors) and secondary appraisal (resources to cope), which influence coping strategies. Coping, in turn, affects immediate stress responses and long-term health, well-being, and social functioning (45). Later, Lazarus and colleagues expanded this model into a cognitive–motivational–emotional framework, linking specific appraisal processes to distinct emotions and integrating stress and emotion research within a broader theoretical context (46). Future research should explore whether CS can enhance professionals’ sense of responsibility and control, thus leading to increased trust and hope among patients and residents (35).
Risk factors for CF include an inability to manage stress, high stress levels, low social support, personal trauma history, and emotional suppression or avoidance. Research indicates that nurses with higher empathy levels are at greater risk of CF. Self-care is considered a crucial protective factor, though its definition varies in literature and may include practices such as healthy eating, exercise, and spiritual activities.
The research with LTC home staff found associations between anxiety, work environment characteristics, and depression, consistent with other studies (7, 47, 48). Working conditions significantly affect mental health outcomes, with negative conditions worsening mental health and positive conditions providing protection (49). Using Clark and Watson’s theoretical framework, our study examined ProQOL’s mediating roles and found that BO and CS mediated the relationship between anxiety and depression. The results indicate that anxiety is positively related to depression both directly and indirectly, with reduced CS and increased BO leading to higher depression levels. Consistent with previous research, anxiety did not influence depression through STS (25). Additionally, factors such as age, physical health, and help-seeking behavior were related to depression.
The findings confirm that working conditions and the need for additional support significantly impacted respondents’ mental health. During the COVID-19 crisis, respondents faced longer shifts, inadequate staffing, increased mortality, and isolation from families, contributing to mental health problems. Those who sought professional support generally found it accessible, highlighting the need of integrating support into regular protocols and developing community support services.
CF remains a serious threat to health and social care professionals, potentially reducing their ability to show compassion (50, 51). During the COVID-19 pandemic, frontline workers are at risk of developing CF and psychological distress (52–56). Witnessing suffering and facing personal safety threats can induce anxiety, fear, and emotional distancing (57). Addressing CF and providing support to frontline workers is crucial for maintaining resilience and effective care. Future research should focus on evidence-based practices and conduct a meta-analysis of findings from all studies on the use of the ProQOL in different countries following COVID-19.
Certain limitations impacting the generalizability of the findings should be acknowledged. The study used a cross-sectional design, making establishing causal relationships difficult. The sample came from 18 LTC facilities in Serbia using a convenience sampling strategy, which may introduce bias, as recruited participants may be atypical of the population. Convenience sampling has inherent limitations in terms of representativeness, as it may not encompass the entire population of LTC workers. This sampling strategy was chosen for practical reasons, including availability and the limitations of the data collection process. Multiple psychological, cultural and social factors were not measured, which limits our ability to explain the observed outcomes. To address these limitations, future research is needed to generate a comprehensive understanding of professional quality of life among LTC workers in Serbia.
In conclusion, this study contributes to the broader literature on LTC workers wellbeing by examining the complex interplay between professional quality of life, anxiety, and depression. The findings should guide decision-makers in developing targeted interventions and policies that promote the psychological resilience and well-being of LTC workers, thereby enhancing both individual and organizational outcomes in the healthcare sector.
This study is a pioneering effort in examining LTC facilities in Serbia, offering valuable insights for future research and the enhancement of working conditions. Despite this, challenging job conditions - such as prolonged exposure to suffering and mortality - remain significant contributors to CF and BO. These roles are often characterized by low wages and an increased workload due to workforce migration to Western Europe. To ensure the long-term quality of LTC facilities, it is crucial to improve working conditions and provide accessible psychosocial support within these institutions. Further research is needed to explore the coping strategies of individuals experiencing CS, evaluate the Serbian LTC system’s capacity to adapt working conditions, and develop preventative measures for all staff. However, given that many institutions face training fatigue, any interventions must be practical and manageable within the already demanding workload of LTC workers. Collaborating with LTC staff in designing these interventions could enhance their acceptance and engagement, thereby improving the quality of services provided in LTC facilities and safeguarding employees’ physical and mental wellbeing. Implementing effective interventions will directly and indirectly enhance the quality of working life, supporting the mental and physical health of Serbia’s LTC frontline staff.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethical Review Board of the Faculty of Medicine University of Belgrade (reference number: 27/VII-9). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MV: Conceptualization, Formal analysis, Funding acquisition, Methodology, Resources, Writing – original draft, Writing – review & editing, Data curation, Investigation, Project administration. VP: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing, Software, Visualization. NT: Data curation, Funding acquisition, Project administration, Supervision, Conceptualization, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. NMM: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing, Formal analysis, Software, Visualization. BM: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. PB: Conceptualization, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. NVM: Data curation, Formal analysis, Investigation, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. MS: Data curation, Formal analysis, Software, Visualization, Writing – original draft, Writing – review & editing. SRM: Conceptualization, Supervision, Validation, Writing – original draft, Writing – review & editing, Formal analysis, Funding acquisition, Investigation, Project administration, Resources. AP: Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing. VS: Formal analysis, Funding acquisition, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. AT: Data curation, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. DOS: Formal analysis, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. SVM: Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Validation, Writing – original draft, Writing – review & editing. DT: Conceptualization, Supervision, Validation, Writing – original draft, Writing – review & editing, Methodology. DMS: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Ministry of Science, Technological Development and Innovation of Republic of Serbia (grant No. 200110), and University of East Sarajevo, Faculty of Medicine Foca, RS, BiH (No. 01-3-36).
We are thankful to all staff from long term care facilities who agreed to participate in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1479190/full#supplementary-material
1. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. (2014) 12(6):573–6. doi: 10.1370/afm.1713
2. Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. (1996) 347:724–8. doi: 10.1016/S0140-6736(96)90077-X
3. Shanafelt T, Sloan J, Habermann T. The well-being of physicians. Am J Med. (2003) 114:513–9. doi: 10.1016/S0002-9343(03)00117-7
4. Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. (2015) 90:1600–13. doi: 10.1016/j.mayocp.2015.08.023
5. Varrasi S, Guerrera CS, Platania GA, Castellano S, Pirrone C, Caponnetto P, et al. Professional quality of life and psychopathological symptoms among first-line healthcare workers facing COVID-19 pandemic: an exploratory study in an Italian southern hospital. Heal Psychol Res. (2023) 11:1–8. doi: 10.52965/001c.67961
6. Bailey BC, Cox S, Terris L, Van Oppen D, Howsare J, Berry JH, et al. Rural health care worker wellness during COVID-19: Compassion fatigue, compassion satisfaction & utilization of wellness resources. PloS One. (2023) 18(12):e0295020. doi: 10.1371/journal.pone.0295020
7. La Torre G, Bartleta V, Mattia M, Paludetti F, Faticoni A, Barone LC, et al. Assessment of anxiety, depression, work-related stress, and burnout in health care workers (HCWs) affected by COVID-19: results of a case–control study in Italy. J Cinical Med. (2022) 11(15):4434. doi: 10.3390/jcm11154434
8. Galvin G. Nearly 1 in 5 health care workers have quit their jobs during the pandemic. Morning Consult. (2021). https://morningconsult.com/2021/10/04/health-care-workers-series-part-2-workforce/ (Accessed July 25 2024).
9. Nimmo A, Huggard P. A systematic review of the measurement of compassion fatigue, vicarious trauma, and secondary traumatic stress in physicians. Australas J Disaster Trauma Stud. (2013) 1:37–44.
10. Figley CR. Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel (1995).
11. Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. (2020) 29:2762–4. doi: 10.1111/jocn.v29.15-16
12. Boyle D. Countering compassion fatigue: A requisite nursing agenda. Online J Issues Nurs. (2011) 16(1):2. doi: 10.3912/OJIN.Vol16No01Man02
13. Boyle D. Compassion fatigue: The cost of caring. Nurs (Lond). (2015) 45(7):48–51. doi: 10.1097/01.NURSE.0000461857.48809.a1
14. Figley CR. Compassion fatigue: Psychotherapists’ chronic lack of self-care. J Clin Psychol. (2002) 58:1433–41. doi: 10.1002/jclp.v58:11
15. Mason VM, Leslie G, Clark K, Lyons P, Walke E, Butler C, et al. Compassion fatigue, moral distress, and work engagement in surgical intensive care unit trauma nurses: A pilot study. Dimens Crit Care Nurs. (2014) 33:215–25. doi: 10.1097/DCC.0000000000000056
16. Day JR, Anderson RA. Compassion fatigue: an application of the concept to informal caregivers of family members with dementia. Nurs Res Pract. (2011) 2011:408024. doi: 10.1155/2011/408024
17. Oberg G, Carroll A, Macmahon S. Compassion fatigue and secondary traumatic stress in teachers: How they contribute to burnout and how they are related to trauma-awareness. Front Educ. (2023) 8:1–10. doi: 10.3389/feduc.2023.1128618
18. Adams RE, Figley CR, Boscarino JA. The compassion fatigue scale: its use with social workers following urban disaster. Methods Enzym. (2008) 18:238–50. doi: 10.1177/1049731507310190
19. Hegeney D, Craigie M, Hemsworth D, Osseiran-Moisson R, Francis K, Drury V. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: study 1 results. J Nurs Manag. (2014) 22(4):506–18. doi: 10.1111/jonm.12160
20. Erdur B, Ergin A, Turkcuer I, Al. E. A study of depression and anxiety among doctors working in emergency units in Denizli, Turkey. Emerg Med J. (2006) 23):759–63. doi: 10.1136/emj.2006.035071
21. Chambers R, Campbell I. Anxiety and depression in general practitioners: associations with type of practice, fundholding, gender and other personal characteristics. Fam Pr. (1996) 13):170–3. doi: 10.1093/fampra/13.2.170
22. Clark L, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J Abnorm Psychol. (1991) 100):316–36. doi: 10.1037/0021-843X.100.3.316
23. Anderson E, Hope D. A review of the tripartite model for understanding the link between anxiety and depression in youth. Clin Psychol Rev. (2008) 28):275–87. doi: 10.1016/j.cpr.2007.05.004
24. Dia D, Harrington D, Silverman W. An examination of the tripartite model of anxiety and depression in an outpatient sample of adolescents. J Evid Based Soc Work. (2010) 7):302–12. doi: 10.1080/19371910903178771
25. Xie G, Li W, Mcdermott B. Professional quality of life as potential mediators of the association between anxiety and depression among Chinese health-care clinicians. Int J Psychiatry Med. (2020) 56(2):83–96. doi: 10.1177/0091217420913395
26. Tabachnick B, Fidell L. Using Multivariate Statistics. 6th edition. Boston: Pearson education (2013).
28. Francis Guillemin C. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J Clin Epidemiol. (1993) 46:1414–32. doi: 10.1016/0895-4356(93)90142-n
29. Acquadro C, Conway K, Hareendran A, Aaronson N. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Heal. (2008) 11:509–21. doi: 10.1111/j.1524-4733.2007.00292.x
30. Lovibond SF, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sidney: Psychology Foundation of Australia (1995).
31. Bride B, Robinson M, Yegidis B, Figley C. Development and validation of the secondary traumatic stress scale. Res Soc Work Pr. (2004) 14:27–35. doi: 10.1177/1049731503254106
32. Ware J, Kosinski M, Keller SD. SF-12: How to score the SF-12 physical and mental health summary scales. 2nd ed. Boston MA: The Health Institute, New England Medical Center (1995).
33. Keesler JM, Fukui S. Factor structure of the professional quality of life scale among direct support professionals: factorial validity and scale reliability. J Intellect Disabil Res. (2020) 64(9):681–9. doi: 10.1111/jir.12766
34. Duarte J, Pinto-Gouveia J. Mindfulness, self-compassion and psychological in flexibility mediate the effects of a mindfulness-based intervention in a sample of oncology nurses. J Context Behav Sci. (2017) 6(2):125–33. doi: 10.1016/j.jcbs.2017.03.002
35. Galiana L, Arena F, Amparo O, Noemi S, Benito E. Compassion satisfaction, compassion fatigue, and burnout in Spain and Brazil: proQOL validation and cross-cultural diagnosis. J Pain Symptom Manage. (2017) 53:598–604. doi: 10.1016/j.jpainsymman.2016.09.014
36. Hemsworth D, Baregheh A, Aoun S, Hegney D, Kazanjian A. A critical enquiry into the psychometric properties of the professional quality of life scale (ProQol-5) instrument. Appl Nurs Res. (2017) 39:81–8. doi: 10.1016/j.apnr.2017.09.006
37. Heritage B, Rees CS, Hegney DG. The ProQOL-21: A revised version of the Professional Quality of Life (ProQOL) scale based on Rasch analysis. PloS One. (2018) 13(2):e0193478. doi: 10.1371/journal.pone.0193478
38. Samson T, Iecovich E, Shvartzman P. Psychometric characteristics of the hebrew version of the professional quality-of-life scale. J Pain Symptom Manage. (2016) 52:575–81. doi: 10.1016/j.jpainsymman.2016.03.019
39. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. (2020) (21–22):4321–30. doi: 10.1111/jocn.15469
40. Dwyer M, Alt M, Brooks J, Katz H, Poje A. Burnout and compassion satisfaction: survey findings of healthcare employee wellness during COVID-19 pandemic using ProQOL. Kans J Med. (2021) 14):121–7. doi: 10.17161/kjm.vol1415171
41. Aryankhesal A, Mohammadibakhsh R, Hamidi Y, Alidoost S, Behzadifar M, Sohrabi R, et al. Interventions on reducing burnout in physicians and a nurses: A systematic review. Med J Islam Repub Iran. (2019) 33:77. doi: 10.47176/mjiri.33.77
42. Kim C, Lee Y. Effects of compassion competence on missed nursing care, professional quality of life and quality of life among Korean nurses. J Nurs Manag. (2020) :1–10. doi: 10.1111/jonm.13004
43. Crawford P, Brown B, Kvangarsnes M, Gilbert P. The design of compassionate care. J Clin Nurs. (2014) (23-24):3589–99. doi: 10.1111/jocn.2014.23.issue-23pt24
44. Hooper C, Craig J, Janvrin D, Wetsel M, Reimels E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. YMEN. (2010) 36:420–7. doi: 10.1016/j.jen.2009.11.027
45. Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. Eur J Pers. (1987) 1:141–69. doi: 10.1002/per.2410010304
46. Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Annu Rev Psychol. (1993) 44:1–22. doi: 10.1146/annurev.ps.44.020193.000245
47. Mo Y, Deng L, Zhang L, Lang Q, Liao C, Nannan W, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. (2020) (5):1002–9. doi: 10.1111/jonm.13014
48. Buselli R, Corsi M, Baldanzi S, Chiumiento M, Del Lupo E, Oste VD, et al. Professional quality of life and mental health outcomes among health care workers exposed to sars-cov-2 (Covid-19). Int J Environ Res Public Heal Artic. (2020) 2:1–12. doi: 10.3390/ijerph17176180
49. Nigam JAS, Barker RM, Cunningham TR, Swanson NG, Chosewood LC. Vital signs: health worker–perceived working conditions and symptoms of poor mental health—Quality of worklife survey, United States, 2018 – 2022. Morb Mortal Wkly Rep. (2023) 72:2018–22. doi: 10.15585/mmwr.mm7244e1
50. Balinbin B, Trizia Balatbat K, Balcueva MI, Balicat MG, Balidoy TA, Macindo JR, et al. Occupational determinants of compassion satisfaction and compassion fatigue among Filipino registered nurses. J Clin Nurs. (2020) (5-6):955–63. doi: 10.1111/jocn.v29.5-6
51. Polat H, Turan G, Mehtap T. Determination of the relationship of the spiritual orientation of nurses with compassion fatigue, burnout, and compassion satisfaction. Perspect Psychiatr Care. (2020) 56(4):920–5. doi: 10.1111/ppc.12513
52. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
53. Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID- 19 outbreak. Asian J Psychiatr. (2020) 51:102080. doi: 10.1016/j.ajp.2020.102080
54. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:1–12. doi: 10.1001/jamanetworkopen.2020.3976
55. Bostan S, Akbolat M, Kaya A, Ozata M, Gunes D. Assessments of anxiety levels and working conditions of health employees working in COVİD-19 pandemic hospitals. Electron J Gen Med. (2020) 17(5):em246. doi: 10.29333/ejgm/8228
56. Zhang W, Wang K, Zhao W, Xue Q, Peng M, Min B, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89(4):242–50. doi: 10.1159/000507639
Keywords: compassion fatigue, anxiety, depression, quality of life, long-term care
Citation: Vracevic M, Pavlovic V, Todorovic N, Milic NM, Matejic B, Brkic P, Milic NV, Savic M, Masic S, Pavlovic A, Stanisic V, Tasic A, Spaic D, Matovic S, Tiosavljevic D and Stanisavljevic D (2025) Compassion fatigue and satisfaction among frontline staff in long term care facilities: psychometric properties of the Serbian version of the professional quality of life scale. Front. Psychiatry 16:1479190. doi: 10.3389/fpsyt.2025.1479190
Received: 11 August 2024; Accepted: 17 February 2025;
Published: 10 March 2025.
Edited by:
Mohammad Ali Zakeri, Rafsanjan University of Medical Sciences, IranReviewed by:
Patricia Brownell, Fordham University, United StatesCopyright © 2025 Vracevic, Pavlovic, Todorovic, Milic, Matejic, Brkic, Milic, Savic, Masic, Pavlovic, Stanisic, Tasic, Spaic, Matovic, Tiosavljevic and Stanisavljevic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dejana Stanisavljevic, ZGVqYW5hLnN0YW5pc2F2bGpldmljQG1lZC5iZy5hYy5ycw==; Sandra Matovic, c2FuZHJhLmpva292aWNAaG90bWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.