- 1Department of Psychiatry, College of Health Science and Medicine, Dilla University, Dilla, Ethiopia
- 2Psychiatry Department, Faculty of Medicine, Institute of Health, Jimma University, Jimma, Ethiopia
Background: Refugees encounter a variety of traumatic events throughout their migratory process and in the camp, which increase their risk of developing mental illnesses. Even though depression and anxiety are the most frequent after a stressful life event, there is limited information on Sudanese refugees. Therefore, this study aimed to assess the prevalence and associated factors of depressive and anxiety symptoms at the Bambasi Camp in northwestern Ethiopia.
Method: A cross-sectional study was conducted among 379 participants using a systematic random sampling method. The Hopkins Symptoms Checklist (HSCL-25) was used to assess depressive and anxiety symptoms. The data was collected by the Kobo toolbox mobile application and analyzed using SPSS (version 26). Multiple logistic regressions with the backward elimination method were performed. A p-value of <0.05 with 95% CI was taken as statistically significant.
Result: A total of 379 participants were included, with 96.9% response rate. The prevalence of depressive and anxiety symptoms was 46.2% (95% CI = 41–51.2) and 39.6% (95% CI = 34–41), respectively. A multivariable logistic regression analysis indicated that being a female (AOR = 2.56; 95% CI = 1.50–4.26), duration of stay (≥11 years) in the camp (AOR = 2.32; 95% CI = 1.39–3.86), being jobless (AOR = 2.68; 95% CI = 1.30–5.50), and poor social support (AOR = 3.12; 95% CI = 1.25–7.79) were identified as risk factors of depressive symptoms and also being female (AOR = 3.60; 95% CI = 2.26–5.74) and age above 45 (AOR = 2.48; 95% CI = 1.16–5.30) were identified as risk factors for anxiety symptoms.
Conclusion: The findings highlight the high burden of mental health problems that Sudanese refugees bear. The identified predictors of depressive and anxiety symptoms should alert medical and refugee professionals to identify vulnerable individuals and groups, to link them to appropriate psychological intervention, and also to take action for the identified risk factors.
Introduction
According to the World Health Organization (WHO), depression is the leading cause of disability, with an estimated 264 million people affected globally (1). It is the third most common cause of years lived with disability (YLDs) in the general population (2). Anxiety is an ongoing feeling of worry or apprehension that is inappropriate given the circumstances of one’s life. It can be expressed in different ways, such as uncontrollable worry, intense fear, phobias, and panic attacks (3). In 2017, 260 million people globally were affected by anxiety disorder (4).
The latest figures show that the number of conflict-affected people reached more than 100 million, which is an increase due to recent global events (5). According to the United Nations High Commissioner for Refugees (UNHCR) reports, by the end of 2021, 27.1 million refugees were in refugee camps, 83% were hosted in low- and middle-income countries, and one-fifth of all refugees worldwide are hosted in Africa, predominantly in three countries: Uganda, Sudan, and Ethiopia (6). During the conflict between Sudan and South Sudan in 2013, nearly 400,000 people died, 4 million people were displaced (2 million within Sudan) and another 2.5 million were refugees in neighboring countries like Ethiopia (7).
Nearly all individuals affected by these emergencies will experience psychological distress. An estimated 35 million (42%) of the 82.4 million displaced and stateless people globally experience mental disorders such as depression and anxiety (8). Refugees and internally displaced people had a reported prevalence of post-traumatic stress disorder, depression, and nonspecific anxiety disorders that varied widely from 3% to 88%, 5% to 80%, and 20.3% to 81%, respectively (9). A meta-analysis of studies on long-term mental health with a total of 16,010 war-affected refugees showed that the prevalence of depression was at 2.3–80%, of PTSD at 4.4–86%, and of anxiety disorder at 20.3–88% (10). Recent research found that among 43% of Syrian refugees living in 10 countries, 40% had depression and 26% had anxiety (11). In Africa, the prevalence of depression was 49.9%, 32%, 48.1%, 37.8%, and 45% in southern Sudan, Rwandan refugees in Uganda, and Somali refugees, in Maiayni camp and Dabat town, Ethiopia, respectively (12–15), while the prevalence of anxiety was 49.4% in South Africa (16), 73% in Uganda (17), and 33.6% in Ethiopia (15).
The greater susceptibility of migrants to depression has been connected to both pre-migration events, like exposure to war trauma (18), and post-migration adverse circumstances that refugees frequently encounter in a new country, such as persecution, violence and human right violations (19) and also being separated from family, having trouble with the asylum procedure or even being detained, being unemployed, and having problems assimilating, losing relatives, sexual and physical assault, and lack of food or shelter (20). Moreover, they are underprivileged and vulnerable groups, whose vulnerability is due to the fact that they lack the same legal protections as citizens, making them vulnerable to abuse, hostility from the community, and economic disadvantage, all of which are risk factors for psychological distress (21). Delayed access to mental health care after resettlement increases the risk of depression more than fourfold in traumatized refugees exposed to adverse life experiences compared to the general population (22).
Even though the majority of refugees live in low-income countries, research on refugee mental health is overwhelmingly limited to those who reside in western countries (23). Currently, there is a scarcity of information on the prevalence of depression, anxiety, and their associated factors in the Bambasi refugee’s camp. To address this critical information gap, our study aims to assess the prevalence and its associated factors of depression and anxiety among Sudanese refugees residing in Bambasi Camp, northwest Ethiopia.
This study contributes to the field of existing evidence on mental health issues among refugees, particularly in Ethiopia, and gives insight into the mental health needs of this vulnerable population. It can also inform policymakers and aid organizations about the development of policies and programs that address the mental health needs of refugees and provide the necessary support. Moreover, the study has practical implications for mental health professionals, counselors, social workers, and aid workers working with refugees by identifying those associated factors and providing targeted interventions that address the specific mental health needs.
Materials and methods
Study area and period
A refugee-camp-based cross-sectional study was conducted from August 1 to 30, 2023 in Bambasi Refugee Camp, northwest Ethiopia. It is found in Benishangul Gumuz Regional State, 661 km away from Addis Ababa, which is the capital city of Ethiopia. The camp is located in Womba Kebele, 48.6 km from Assosa town, which is the capital city of the region. The camp was established in 2012 as a temporary home for Sudanese refugees. As of November 2020, UNHCR reports that the camp has 4,085 registered households and hosts 18,296 refugees, of whom 9,149 are female (24). The camp is divided into three zones, namely, zone A, zone B, and zone C. It has one health center jointly funded by the United Nations High Commissioner for Refugees (UNHCR) and the Agency for Refugees and Returnee Affairs (ARRA). It provides several health services, including mental health services. Currently, they mainly depend on monthly aid.
Population
All adults who settled in the Bambasi refugee camp were source of population.
Study population
All randomly selected individuals age 18 years and above were from selected households.
Eligibility criteria
All adults living in the Bambasi refugee camp during the study period were included in this study. Participants who were unable to provide information due to illness during the data collection period were excluded from the study
Sample size determination
A single population proportion formula was used to calculate the sample size. The sample size was determined by taking the assumption that, based on a research conducted among Eritrean refugees in the Tigray region, the proportion of depression was 37.8% (14) and by considering 95% confidence level (zα/2 = 1.96) and 5% marginal error (d = 0.05). Therefore, the sample size was calculated by using the following formula:
q = 1 - p. Thus, (1.96)2 (0.388) (1 - 0.388)/(0.05)2 = 355, and by considering 10% non-response rate, the final sample size was = 391.
Sampling technique
A systematic random sampling method was employed to select 379 individual households from a total of 4,085 households. The camp has three zones; proportional allocation of the sample size to each zone was done. The interval (K) was calculated by dividing the number of households by the sample size allocated to the specific zone and was found to be 10. Then, every k (10) value was used to select a HH from each zone. The first household was selected by a lottery method, and then the next household was selected by adding 10 to the first household. The lottery method was used to select study participants within the household if there were more than one.
Data collection procedure
The questionnaire was first prepared in English, then translated to Arabic (the local language) by fluent language speakers, and again translated back to English by another person to ensure consistency and understandability. Next, three BSc nurses for data collection and one MSc in psychiatry were recruited for supervision. The data collectors and supervisor received training on the data collection tools, procedures, and ethical concerns. The questionnaire was pre-tested before the actual study was conducted. Close supervision was carried out during the data collection period, and the investigators checked the consistency of the completed questionnaire at the end of each day. After that, data collection was performed through a face-to-face interview using a pre-tested structured and standardized questionnaires by Kobo Toolbox mobile application.
Instruments
Depression and anxiety symptoms
The Hopkin Symptom Checklist (HSCL-25) is a symptom inventory that is used to assess symptoms of anxiety and depression. It has 25 items: Part 1 consists of 10 items for anxiety and Part 2 has 15 items for depression. Each question has four response categories on the following scale: “not at all,” “a little,” “quite a bit,” and “extremely,” which are rated 1 to 4, respectively (25). The depression score is the average of 15 depression items, while the anxiety score is the average of 10 anxiety items. The overall score has a strong correlation with severe emotional distress of an unspecified anxiety diagnosis, as demonstrated by numerous refugee groups, and the depression score is comparable with major depression as described by the Diagnostic and Statistical Manual of the American Psychiatric Association, fourth edition (DSM-IV). This study was conducted with the Arabic version of the scale, which had been used and proven to be valid and reliable by previous studies (26). It is also validated in Africa (27) and used in multiple internal displaced and refugee populations in sub-Saharan countries including Ethiopia, Kenya, Uganda, and Sudan (28, 29). For the current study, the Cronbach alpha value was 0.81.
Social support
Oslo Social Support (OSS-3) is a brief assessment of social support and functioning. It consists of three items that ask for the number of close confidants, the attention and concern shown by others, and the ease of getting practical aid from others, covering different aspects of social support. The total scores are calculated by summing up the raw scores for each item. The sum of the raw scores has a range of 3–14. The scores “3–8” indicate poor social support, “9–11” indicate moderate social support, and “12–14” indicate strong social support (30).
Substance use history
Risky substance use-related factors are assessed by using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), which is a brief screening questionnaire developed and validated by the World Health Organization (WHO) (31).
Variables of the study
Dependent variables: depressive and anxiety symptoms (yes/no)
Independent variables: socio-demographic characteristics such as sex, age, marital status, educational status, length of stay in the camp, and occupational status
Behavioral- and social-related factors included risky alcohol, tobacco, khat, other substance use, and social support status.
Clinical-related factors included past psychiatric history, family history of mental illness, and chronic medical illness.
Operational definition
Depressive symptoms: If the participants are scoring a mean score of ≥1.75 out of the potential 4 points on the depression subscale of HSCL-25, they are categorized as experiencing depressive symptoms, and those who scoring <1.75 have no depressive symptoms (26).
Anxiety symptoms: If the participants have a mean score of ≥1.75 on the anxiety subscale of HSCL-25, they have anxiety, and for those with a score <1.75, they have no anxiety symptoms (26).
Level of social support: Participants who scored 3–8 had poor social support, 9–11 had moderate social support, and 12–14 had strong social support (30).
Risky alcohol use: Participants scoring 0–10, 11–26, and ≥27 from the ASSIST questionnaire have low, moderate, and high risk, respectively (31).
Risky substance use (khat, cigarettes, and other substances): Those participants scoring 0–3, 4–26, and ≥27 from the ASSIST questionnaire had low, moderate, and high risk, respectively (31).
Data quality control
A 1-day training was given to the data collectors and supervisor on the objectives, clarity of tools, and overall data collection procedures to standardize the interview procedures and reduce the interviewer bias. The final version of the questionnaire was translated into Arabic and again retranslated into English language by bilingual experts to check for the language consistency of the tool. The questionnaires were pre-tested on 5% (20 refugees) of the sample size to determine the clarity of the tool and the feasibility of the study. At the end of each day during the data collection period, the collected data were checked for consistency and completeness.
Data processing and analysis
The collected data were checked for completeness and consistency, edited and coded by using the Kobo toolbox application, and then exported to SPSS version 26 statistical software for analysis. Descriptive statistics such as frequency and percentage were used to summarize the variables and were presented using charts and tables. Bivariate logistic regression analysis was done separately with outcome variables, and all explanatory variables that have an association with the outcome variables with p <0.25 were selected as candidate variables for multivariable logistic regression analysis. A multivariable logistic regression analysis with backward elimination was carried out. Finally, variables with p <0.05 and 95% confidence interval and odds ratio (OR) are considered as factors associated with the outcome variables (statistically significant). The p-values in the Hosmer and Lemshow tests were 0.69 and 0.64 for anxiety and depression, respectively.
Results
Socio-demographic characteristics of the study participants
Out of 391 selected households in the study, 379 individuals participated, yielding a response rate of 96.9%. Of the 379 participants, more than half (207, 54.6%) were female. Their age ranged from 18 to 74 years; 127 (33.5%) were between 26 and 35 years of age. More than one-third (149, 39.3%), and almost all (367, 96.8%) were married and Muslim by religion, respectively. More than one-third of the participants (143, 37.7%) had no formal education. The average duration of stay in the camp was 11.4 years, ranging from 9 to 12 years. Although the participants had diverse types of occupations before coming to Ethiopia, farmers constituted one-third (32.2%) of the total number of participants (Table 1).
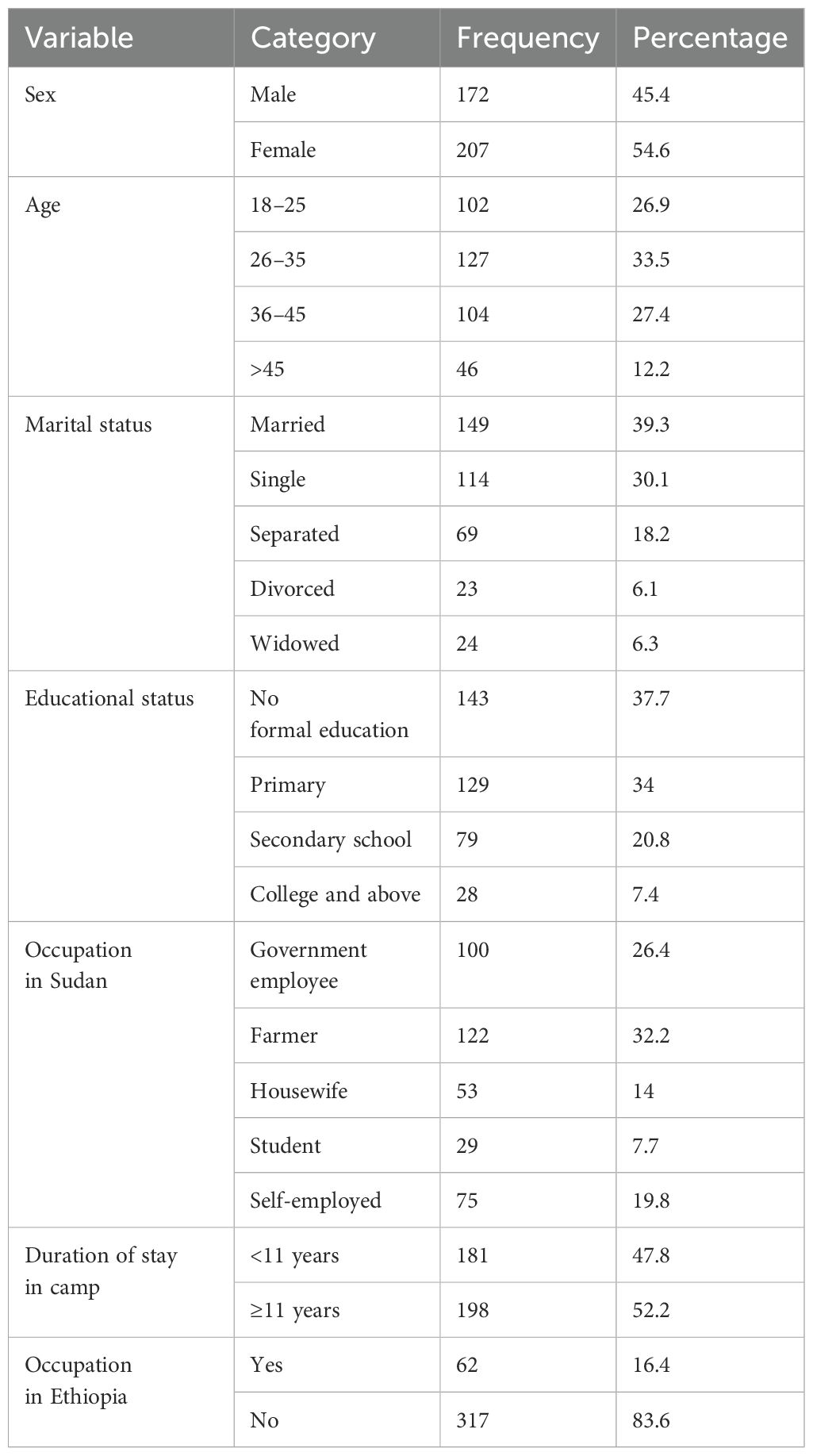
Table 1. Socio-demographic characteristics of participants among Sudanese refugees at Bambasi Camp in northwest Ethiopia, 2023 (n = 379).
Clinical-related factors
Among the participants, 14.2% had chronic medical condition (Table 2).
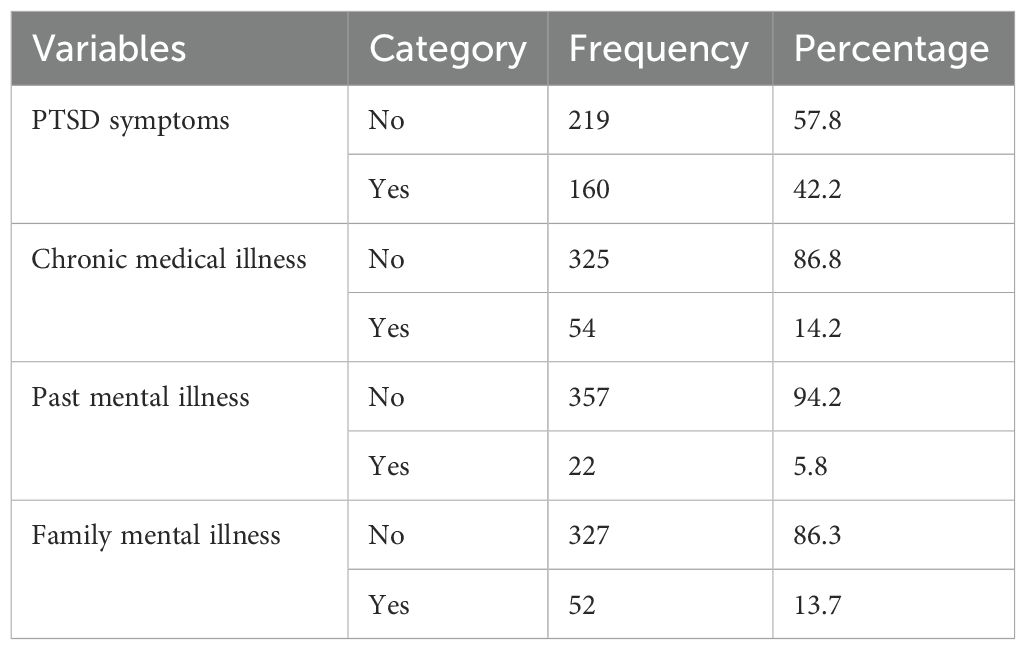
Table 2. Frequency distribution of clinical-related factors among Sudanese refugees at Bambasi Camp in northwest Ethiopia, 2023 (n = 379).
Substance- and psychosocial-related factors
More than half of the participants [206 (54.4%), 168 (44.3%), and 140 (36.9%)] had used khat, alcohol, and cigarette in their lifetime, respectively. Additionally, one out of seven (54, 14.2%) participants had had risky alcohol use behavior. Regarding social support status, nearly half (177, 46.7%) of the participants had poor social support (Table 3).
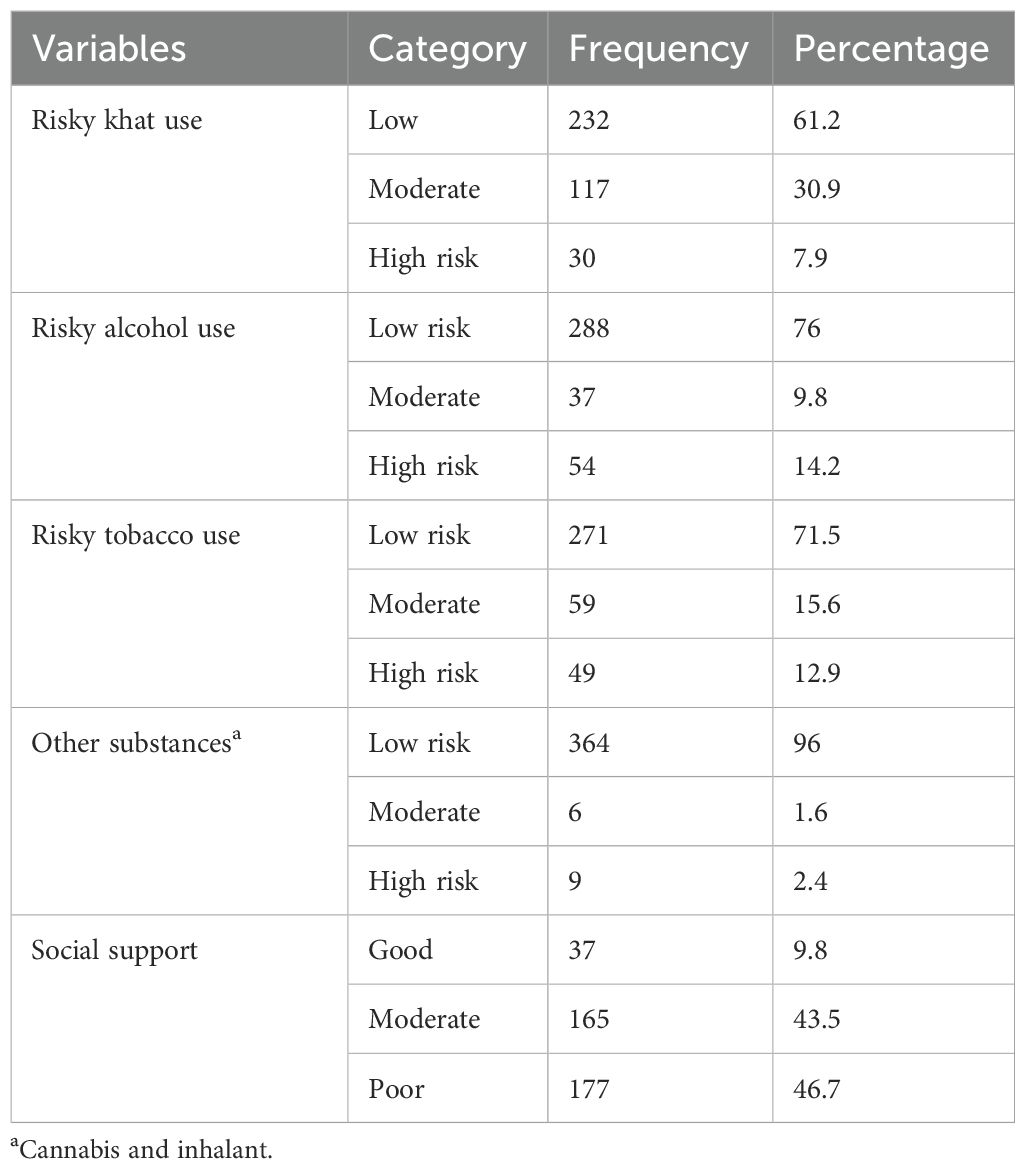
Table 3. Frequency distribution of risky substance use and psychosocial-related factors among Sudanese refugees at Bambasi Camp in northwest Ethiopia, 2023 (n = 379).
Prevalence of depressive and anxiety symptoms
Among the participants, 175 (46.2%, 95% CI = 41–51%) had depression, with more women than men [116 (66.3%) vs. 59 (33.7%)], fulfilling the mean score of ≥1.75 from HSCL-15, and
150 (39.6%, 95% CI = 35–45%) had anxiety, fulfilling the mean score of ≥1.75 from the HSCL-10 anxiety subscale (Figure 1).
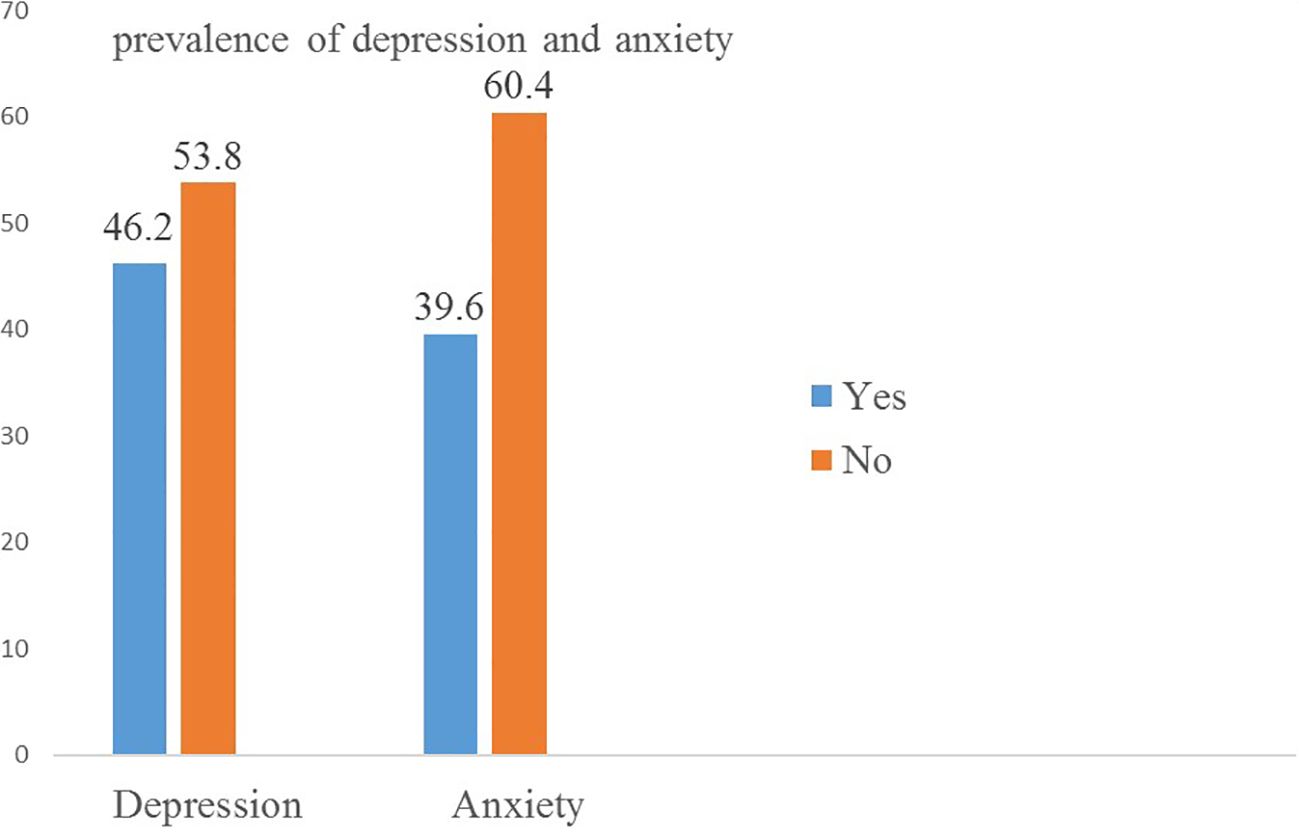
Figure 1. Prevalence of depression and anxiety among Sudanese refugees at Bambasi Camp in northwest Ethiopia, 2023 (n = 379).
Factors associated with depressive symptoms
Among the factors, age, sex, educational status, marital status, job status in Ethiopia, family history of psychiatric illness, presence of chronic medical illness, and social support fulfilled the minimum criteria (p < 0.25) for further multivariable logistic analysis. These variables were then entered into a multivariable logistic regression model (Table 4).
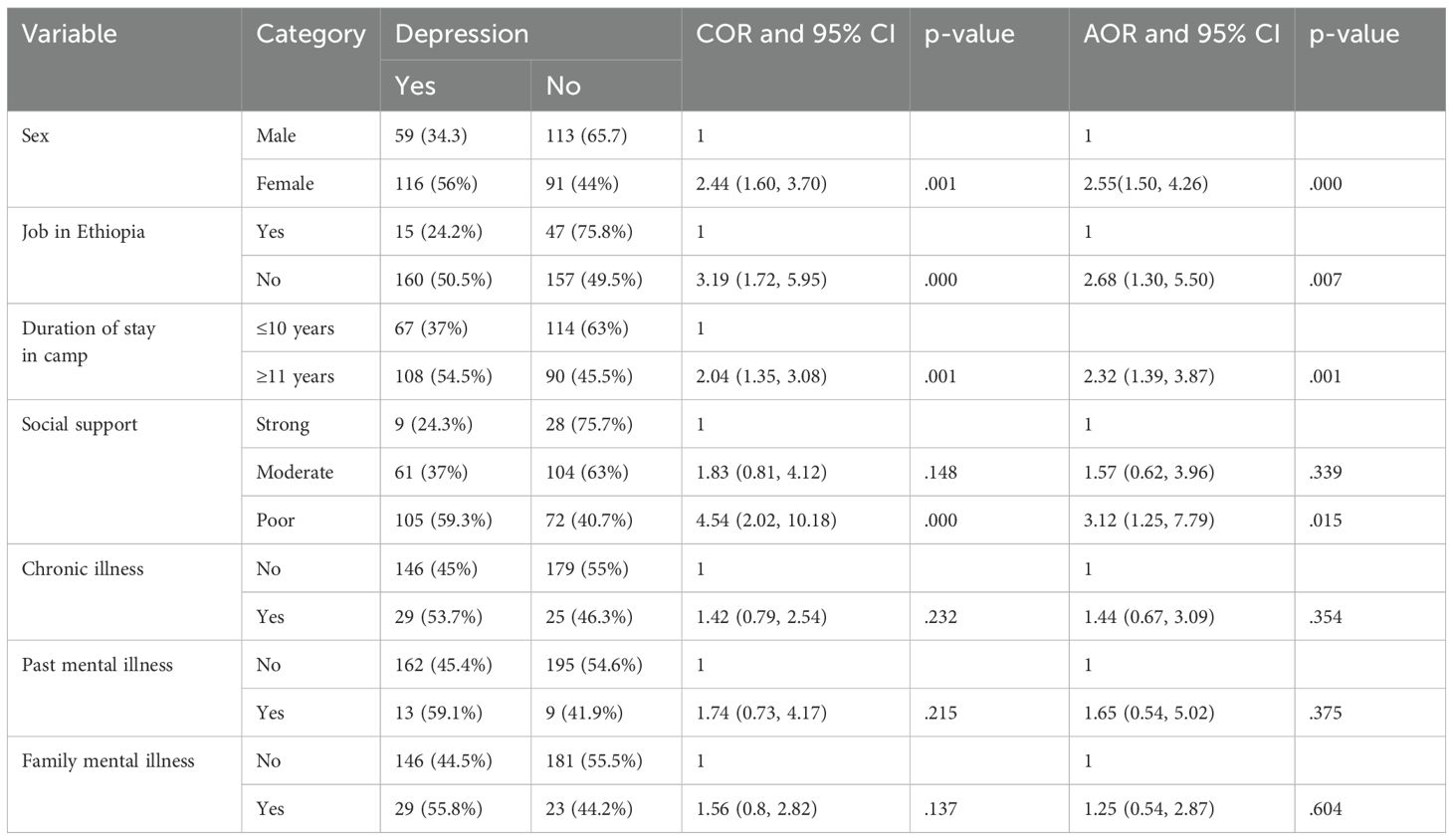
Table 4. Bivariate and multivariable analysis for all candidate factors for depression among Sudanese refugees at Bambasi Camp in northwest Ethiopia (n = 379).
Given this fact, female participants were 2.6 times (AOR = 2.56; 95% CI = 1.50–4.26; P <.001) more likely to experience depressive symptoms than male participants. It was also identified that participants who had a long duration of stay in the refugee camp (≥11 years) were 2.3 times more likely (AOR = 2.32; 95% CI = 1.39–3.86; p = .001) to have increased odds of depressive symptoms than those who had a short duration of stay. Similarly, refugees who have no job had increased odds of depressive symptoms by 2.7 times (AOR = 2.68; 95% CI = 1.30–5.50, p = .007) than those employed. Furthermore, participants with poor social support were three times (AOR = 3.12; 95% CI = 1.25–7.79; p = 0.015) more likely to experience depressive symptoms than those with good social support.
Factors associated with anxiety symptoms
Factors like age, sex, educational status, marital status, family history of psychiatric illness, and social support fulfilled the minimum criteria (p < 0.25) for further multivariable logistic analysis. These variables were then entered into a multivariate logistic regression model (Table 5).
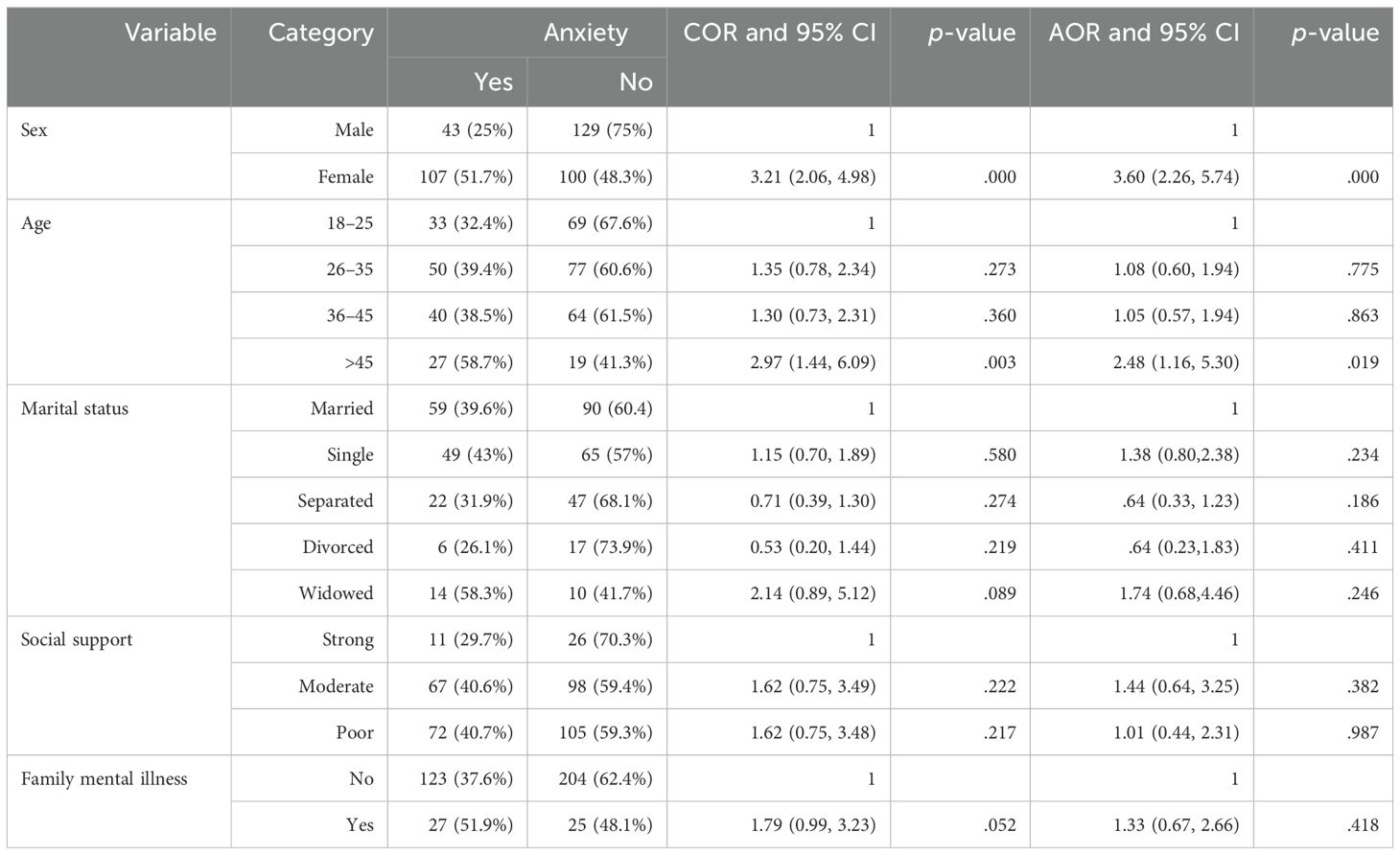
Table 5. Bivariate and multivariable analysis for all candidate factors for anxiety among Sudanese refugees at Bambasi Camp in northwest Ethiopia (n = 379).
The finding from this study shows that female participants are 3.6 times (AOR = 3.60; 95% CI = 2.26–5.74; p <.001) more likely to experience anxiety symptoms compared to male participants. The study also reveals that those participants in the age category above 45 were 2.5 times (AOR = 2.48; 95% CI = 1.16–5.30, p = .019) more likely to show anxiety symptoms compared to the younger age (18– 25) group.
Discussion
The main aim of this study is to assess the prevalence and associated factors of depressive and anxiety symptoms among Sudanese refugees at Bambasi Camp. Our analysis found that the prevalence of depressive and anxiety symptoms in the Bambasi Camp was 46.2% (95% CI: 41–51%) and 39.6% (95% CI: 34.2–41.2), respectively.
The magnitude of depressive symptoms in our finding is in line with previous studies done in Uganda at 46.2% (32), southern Juba at 49.9% (12), Syrian refugees in Greece at 44% (33), Karenina refugees living in the Thai–Burma border at 41.8% (34), and USA at 47.7% (35). However, it was higher in comparison to the previous studies done on Somali and Eritrean refugees in Ethiopia at 38.3% and 37.8%, respectively (14, 36), northern Uganda at 15.2% (37), Somali refugees in Kenya at 40.8% (29), Istanbul at 34.7% (38), Germany at 39.8% (39), and Burmese refugees in Australia at 36% (40). The possible explanation could be the ongoing feeling of insecurity in their home country (Sudan), and the sensitivity of the tool differences may be the reason for the discrepancy—for instance, in a study among Eritrean and Somali refugees’ camps in Ethiopia that used PHQ 9, we used HSCL-25. In addition, refugees in low-income countries have increased odds of depression due to multiple reasons (41). Conversely, the prevalence of depressive symptoms in the current study is lower than in a study conducted among African refugees in South Africa at 54.6% (16), Syrian refugees residing in Iraq at 59.4% (42), Cambodian refugees in the USA at 80% (43), Canada at 51.7% (44), and Bangladesh at 51.6% (45). The possible explanation might be due to the use of different tools in Afghanistan and USA; both used DASS-21 and Composite International Diagnostics Interview, respectively. Furthermore, sampling procedures, study design, cultural differences among refugees, and the use of a large sample size may amplify the prevalence.
The prevalence of anxiety symptoms in our study revealed 39.6% (95% CI: 34.2–41.2), which is in line with research done in Istanbul at 36.1% (38), USA at 40.3% (35), and Karenni refugees in Thai–Burmese at 41% (34). However, the current prevalence study was higher than the study conducted in Germany from Arabic-speaking refugees at 26.8% (46), Syrian refugees in Germany at 13.5% (47), and Australia at 20% (40). The possible explanation for this may be separation anxiety, the type of stress experienced during the post-migration period, and also the added load of resettlement procedures in a new country (48). In addition, the use of a 3-year follow-up study design in Germany, the use of the DASS 21 tool, and a smaller sample size (n = 148) in Australia may be the possible explanations. Conversely, the prevalence of anxiety in the current study is lower than in a study done in Bangladesh at 70% (45), Afghanistan at 72.2% (49), South Africa at 49.4% (16), and Uganda at 73% (17). This variation across these settings could be due to various reasons, such as the use of different tools, cultural differences in illness narratives, sampling techniques, and types of trauma experienced (50).
In our study, being female was associated with depressive symptoms. The finding shows that female participants have 2.6 times more chances of experiencing depressive symptoms than male participants. This finding is consistent with other studies done in Tigray (14), Somalia refugees in Ethiopia (36), Somalia refugees in Kenya (29), Greece (33), Ukrainian refugees in Greece (51), Syrian refugees residing in the Kurdistan region of Iraq (42), and Yazidis refugees in Turkey (52). However, in contrast to this, research done in Uganda shows that female participants are equally affected as men (32), and among Rohingya refugees in Bangladesh, Ethiopian refugees in Toronto, and the conflict-affected population in Somalia, women were less likely to get depression than men (41, 45, 53), respectively. The possible reason for this discrepancy might be that, in the war zone, women faced gender-specific risks as potential victims of rape, sexual abuse, targeted killing, widowhood of deceased soldiers, and pregnancy-related complications due to poor antenatal and postnatal healthcare (54). Additionally, despite the complexity of the sex difference in depression, recent evidence suggests that biological factors, particularly decreases in estrogen during menses, lactation, and menopause, may contribute to the increased prevalence of depression in women (3). On the contrary, testosterone conversion in male patients’ brain via aromatase, presence of androgen receptors in hippocampal neurons, non-recycling nature of testosterone in male patients, and presence of sexually dimorphic brain nuclei in male patients convey special protection for depression among male (55).
Our finding reveals that participants who have no job in the camp are significantly associated with depressive symptoms. Several factors contribute to this association. This study is supported by a study conducted on Eritrean refugees in Tigray (14), Afghanistan post-war (49), Somalia (53), and Rohingya refugees in Bangladesh (45). The possible explanation for these might be that unemployment can lead to feelings of hopelessness, loss of purpose, and reduced self-esteem and can also hinder the refugees’ ability to meet their basic needs and engage in meaningful activities. This leads to social isolation, dependency on aid, and limited opportunity for personal growth and development, which can contribute to feelings of worthlessness and depression (10).
In addition, staying 11 and more years in the refugee camp was a significant predictor of depressive symptoms. This is supported by a study conducted on Eritrean refugees in Tigray (14), Moria refugee camp in Greece (56), and in Canada (57). The possible reason for this might be the limited opportunities for education, employment, and mental health services in the camp, and integration in camp settings can exacerbate feelings of frustration, stagnation, and dependency (56). Over time, the initial support from fellow refugees or external aid organizations may decline, leaving long-term refugees more vulnerable to feelings of loneliness, uncertainty for the future, and disconnection from their homeland and cultural roots (58).
In this study, participants who had poor social support were more likely to increase the odds of getting depressive symptoms than those who had good social support. Our study is in line with the studies done in Tigray, Bangladish, Turkey, and Sudan. The possible reason might be poor social support among refugees, which can contribute to depression through mechanisms such as social isolation, limited access to resources, and recovery from trauma and stress (41).
Being female was another significant predictor for anxiety symptoms. This finding is consistent with studies done in Istanbul (38), Norway (59), and Bangladesh (45). The possible explanation may be that women in refugee camps often have a higher risk of gender-based violence, including sexual assault, domestic violence, and exploitation (60). Moreover, female patients may experience limited access to healthcare services, including mental health support, due to overcrowding and a lack of privacy and confidentiality in seeking healthcare services, which increases the level of stress and anxiety among women (61).
Additionally, our analysis showed that age above 45 was associated with anxiety symptoms, in line with a study conducted in Thailand (62), and Australia (63). The reason might be that refugees over 45 experience unique stressors related to their age, for example, declining physical health, reduced social support networks, acculturation, loss of social roles, and integration into the host society as well as an increased feeling of anxiety and worry about their health (64).
This study is not without limitations. The following are potential limitations: Due to the nature of sensitivity and recall bias, there may be underreporting of traumatic event items. HSCL-25 is a screening tool rather than a diagnostic tool, so the endpoint of depressive and anxiety symptoms might not be certain. Additionally, using self-report data, cross-sectional study design, limited socioeconomic data, and language and cultural barriers.
Conclusion
This study revealed that nearly half and more than one in three of the participants had depressive and anxiety symptoms, respectively. Being female heightened the risk of experiencing depressive and anxiety symptoms. This study recommends routine screening for depression and anxiety in the refugee camp setting. Additionally, community support networks including the host community can be fostered by organizing support groups and peer counseling programs that promote social cohesion and resilience, moreover facilitating conditions for the inclusion with the Ethiopian host society, and involving them in socio-economic participation or sustaining a meaningful resolution to the conflict in Sudan would facilitate the return of refugees back to their homes, support the healing process, and re-build their lives as recommended.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by from Jimma University’s Institutional Review Board (IRB) with Ref No. (JUIH/IRB/561/23). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ES: Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Resources, Validation, Visualization. ET: Conceptualization, Resources, Supervision, Writing – review & editing, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft. GA: Conceptualization, Data curation, Software, Supervision, Writing – review & editing, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to acknowledge Jimma University for giving the chance to conduct this research. Additionally, our genuine gratitude to all study participants, data collectors, and supervisor as well as to ARRA Assosa and Bambasi sub-office administrative staff who were helping for the accomplishment of this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ASSIST, Alcohol, Smoking, and Substance Involvement Screening Test; DASS, Depression Anxiety Stress Scale; HSCL, Hopkins Symptoms Check List; HH, household; HTQ, Harvard Trauma Questionnaire; IOM, International Organization for Migration; IRC, International Rescue Committee; OSSS, Oslo Social Support Scale; PHQ, Patient Health Questionnaire; UNHCR, United Nation Higher Commissioner for Refugee.
References
1. Depressiya — pandemiya XXI veka [Depression - the pandemic of the XXI century]. Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova. (2022) 122(6. Vyp. 2):5–6. doi: 10.17116/jnevro20221220625
2. Tichenor M, Sridhar D. Metric partnerships: global burden of disease estimates within the World Bank, the World Health Organisation and the Institute for Health Metrics and Evaluation. Wellcome Open Res. (2019) 4. doi: 10.12688/wellcomeopenres
3. Sadock BJ, Sadock VA, Ruiz P, Kaplan HI. Kaplan & Sadock's comprehensive textbook of psychiatry (9th ed). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins Philadelphia (2009).
4. Organization, W.H. Monitoring mental health systems and services in the WHO European Region: Mental Health Atlas, 2017. Geneva (2019).
5. UNHCR. Refugee data founder (2022). Available online at: https://www.unhcr.org/refugee-statistics/insights/explainers/100-million-forcibly-displaced.html (accessed May 23, 2022).
6. UNHCR. Global trends Report 2021 (2022). Available online at: https://www.unhcr.org/global-trends (accessed June 14, 2023).
7. MEDICINE, L.S.O.H.T. War in South Sudan estimated to have led to almost 400,000 excess deaths (2018). Available online at: https://www.lshtm.ac.uk/newsevents/news/2019/war-south-Sudan-estimated-have-led-almost-400000-excess-deaths. (accessed September 26, 2018).
8. UNHCR. Observing World Refugee Day With Rising Global Displacement (2021). Available online at: https://www.forbes.com/sites/jackieabramian/2021/06/20/observing-world-refugee-day-with-rising-global-displacement/?sh=6179441355b6 (accessed June 20, 2021).
9. Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Front Psychiatry. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
10. Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights. (2015) 15:29. doi: 10.1186/s12914-015-0064-9
11. Peconga EK, Høgh Thøgersen M. Post-traumatic stress disorder, depression, and anxiety in adult Syrian refugees: What do we know? Scandinavian J Public Health. (2020) 48(7):677–87. doi: 10.1177/1403494819882137
12. Roberts B, Damundu EY, Lomoro O, Sondorp E. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC Psychiatry. (2009) 9(1):7. doi: 10.1186/1471-244X-9-7
13. Onyut LP, Neuner F, Ertl V, Schauer E, Odenwald M, Elbert T. Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugee settlement–an epidemiological study. Conflict Health. (2009) 3:1–16. doi: 10.1186/1752-1505-3-6
14. Berhe SM, Azale T, Fanta T, Demeke W, Minyihun A. Prevalence and predictors of depression among Eritrean refugees in Ethiopia: A cross-sectional survey. Psychol Res Behav Manag. (2021) 14:1971–80. doi: 10.2147/PRBM.S337255
15. Melese M, Simegn W, Esubalew D, Limenh LW, Ayenew W, Chanie GS, et al. Symptoms of posttraumatic stress, anxiety, and depression, along with their associated factors, among Eritrean refugees in Dabat town, northwest Ethiopia, 2023. BMC Psychol. (2024) 12(1):62. doi: 10.1186/s40359-024-01554-7
16. Thela L, Tomita A, Maharaj V, Mhlongo M, Burns JK. Counting the cost of Afrophobia: Post-migration adaptation and mental health challenges of African refugees in South Africa. Transcult Psychiatry. (2017) 54(5-6):715–32. doi: 10.1177/1363461517745472
17. Bapolisi AM, Song SJ, Kesande C, Rukundo GZ, Ashaba S. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. (2020) 20(1):53. doi: 10.1186/s12888-020-2480-1
18. Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Jama. (2009) 302(5):537–49. doi: 10.1001/jama.2009.1132
19. Pejuskovic B, Marković MV. Mental health of refugees, asylum seekers and migrants–an overview of challenges and good practice examples. Psychiatry Today/Psihijatrija Danas. (2020) 52.
20. Mutluer T, Doenyas C, Aslan Genc H. Behavioral implications of the covid-19 process for autism spectrum disorder, and individuals' Comprehension of and reactions to the pandemic conditions. Front Psychiatry. (2020) 11:561882. doi: 10.3389/fpsyt.2020.561882
21. Lott JP. Module three: vulnerable/special participant populations. Developing World Bioethics. (2005) 5:30–54. doi: 10.1111/j.1471-8847.2005.00101.x
22. Song SJ, Subica A, Kaplan C, Tol W, De Jong J. Predicting the mental health and functioning of torture survivors. J Nerv Ment Dis. (2018) 206(1):33–9. doi: 10.1097/NMD.0000000000000678
23. De Jong JT, Komproe IH, Van Ommeren M, El Masri M, Araya M, Khaled N, et al. Lifetime events and posttraumatic stress disorder in 4 postconflict settings. Jama. (2001) 286(5):555–62. doi: 10.1001/jama.286.5.555
24. UNHCR. UNHCR Ethiopia Bambasi Camp Profile (2020). Available online at: https://data.unhcr.org/en/documents/details/83704 (accessed December 15, 2020).
25. Mahfoud Z, Kobeissi L, Peters T, Araya R, Ghantous ZJA. The Arabic validation of the Hopkins symptoms checklist-25 against MINI in a disadvantaged suburb of Beirut, Lebanon. Int J Educ psychol Assess. (2013) 13(1):17–33.
26. Fares S, Dirani J, Darwish H. Arabic validation of the hopkins symptom checklist-25 (HSCL) in a Lebanese sample of adults and older adults. Curr Psychol. (2021) 40:2980–7. doi: 10.1007/s12144-019-00240-x
27. Ashaba S, Kakuhikire B, Vořechovská D, Perkins JM, Cooper-Vince CE, Maling S, et al. Reliability, validity, and factor structure of the Hopkins symptom checklist-25: population-based study of persons living with HIV in rural Uganda. AIDS Behav. (2018) 22(5):1467–74. doi: 10.1007/s10461-017-1843-1
28. Madoro D, Kerebih H, Habtamu Y, M GT, Mokona H, Molla A, et al. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: A cross-sectional study. Neuropsychiatr Dis Treat. (2020) 16:2317–26. doi: 10.2147/NDT.S267307
29. Im H, Swan LE, Warsame AH, Isse MM. Risk and protective factors for comorbidity of PTSD, depression, and anxiety among Somali refugees in Kenya. Int J Soc Psychiatry. (2022) 68(1):134–46. doi: 10.1177/0020764020978685
30. Bøen H. Characteristics of senior centre users–and the impact of a group programme on social support and late-life depression. Norsk epidemiologi. (2012) 22(2). doi: 10.5324/nje.v22i2.1574
31. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. (2002) 97(9):1183–94. doi: 10.1046/j.1360-0443.2002.00185.x
32. Misghinna TK, Nakimuli-Mpungu E, Abbo C, Kinyanda E, Fellowship T, Misghinna TKJ. Major depressive disorder and associated factors among adult refugees attending a refugee center in Kampala, Uganda. Afr J Trauma Stress. (2020) 5(1):1–21.
33. Poole DN, Hedt-Gauthier B, Liao S, Raymond NA, Bärnighausen T. Major depressive disorder prevalence and risk factors among Syrian asylum seekers in Greece. BMC Public Health. (2018) 18(1):908. doi: 10.1186/s12889-018-5822-x
34. Cardozo BL, Talley L, Burton A, Crawford C. Karenni refugees living in Thai–Burmese border camps: traumatic experiences, mental health outcomes, and social functioning. Soc Sci Med. (2004) 58(12):2637–44. doi: 10.1016/j.socscimed.2003.09.024
35. Javanbakht A, Amirsadri A, Abu Suhaiban H, Alsaud MI, Alobaidi Z, Rawi Z, et al. Prevalence of possible mental disorders in Syrian refugees resettling in the United States screened at primary care. J Immigrant Minority Health. (2019) 21(3):664–7. doi: 10.1007/s10903-018-0797-3
36. Feyera F, Mihretie G, Bedaso A, Gedle D, Kumera G. Prevalence of depression and associated factors among Somali refugee at melkadida camp, southeast Ethiopia: a cross-sectional study. BMC Psychiatry. (2015) 15(1):171. doi: 10.1186/s12888-015-0539-1
37. Luo J, Zamar DS, Ogwang MD, Muyinda H, Malamba SS, Katamba A, et al. Cango Lyec (Healing the Elephant): Probable post-traumatic stress disorder (PTSD) and depression in Northern Uganda five years after a violent conflict. J Migr Health. (2022) 6:100125. doi: 10.1016/j.jmh.2022.100125
38. Acarturk C, McGrath M, Roberts B, Ilkkursun Z, Cuijpers P, Sijbrandij M, et al. Prevalence and predictors of common mental disorders among Syrian refugees in Istanbul, Turkey: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. (2021) 56(3):475–84. doi: 10.1007/s00127-020-01941-6
39. Hoell A, Kourmpeli E, Salize HJ, Heinz A, Padberg F, Habel U, et al. Prevalence of depressive symptoms and symptoms of post-traumatic stress disorder among newly arrived refugees and asylum seekers in Germany: systematic review and meta-analysis. BJPsych Open. (2021) 7(3):e93. doi: 10.1192/bjo.2021.54
40. Schweitzer RD, Brough M, Vromans L, Asic-Kobe M. Mental health of newly arrived Burmese refugees in Australia: contributions of pre-migration and post-migration experience. Aust N Z J Psychiatry. (2011) 45(4):299–307. doi: 10.3109/00048674.2010.543412
41. Fenta H, Hyman I, Noh S. Determinants of depression among Ethiopian immigrants and refugees in Toronto. J Nerv Ment Dis. (2004) 192:363–72. doi: 10.1097/01.nmd.0000126729.08179.07
42. Mahmood HN, Ibrahim H, Goessmann K, Ismail AA, Neuner F. Post-traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Confl Health. (2019) 13:51. doi: 10.1186/s13031-019-0238-5
43. Carlson EB, Rosser-Hogan R. Cross-cultural response to trauma: a study of traumatic experiences and posttraumatic symptoms in Cambodian refugees. J Trauma Stress. (1994) 7:43–58. doi: 10.1007/BF02111911
44. Aluh DO, Aigbogun O, Anyachebelu OC. Depression among immigrant Nigerians in Canada. J Immigrant Minority Health. (2023) 25:315–23. doi: 10.1007/s10903-022-01404-x
45. Awang S, Mohamad S, Awaluddin S. Humanitarian disaster: mental health disorders at primary healthcare clinic. Disaster Emergency Med J. (2022) 7:1–10. doi: 10.5603/DEMJ.a2022.0001
46. Georgiadou E, Morawa E, Erim Y. High manifestations of mental distress in Arabic asylum seekers accommodated in collective centers for refugees in Germany. Int J Environ Res Public Health. (2017) 14. doi: 10.3390/ijerph14060612
47. Georgiadou E, Zbidat A, Schmitt GM, Erim Y. Prevalence of mental distress among Syrian refugees with residence permission in Germany: A registry-based study. Front Psychiatry. (2018) 9:393. doi: 10.3389/fpsyt.2018.00393
48. Hameed S, Sadiq A, Din AU. The increased vulnerability of refugee population to mental health disorders. Kans J Med. (2018) 11:1–12.
49. Cardozo BL, Bilukha OO, Crawford CA, Shaikh I, Wolfe MI, Gerber ML, et al. Mental health, social functioning, and disability in postwar Afghanistan. Jama. (2004) 292(5):575–84. doi: 10.1001/jama.292.5.575
50. Ibrahim H, Hassan CQ. Post-traumatic stress disorder symptoms resulting from torture and other traumatic events among Syrian Kurdish refugees in Kurdistan Region, Iraq. Front Psychol. (2017) 8:241. doi: 10.3389/fpsyg.2017.00241
51. Buchcik J, Kovach V, Adedeji A. Mental health outcomes and quality of life of Ukrainian refugees in Germany. Health Qual Life Outcomes. (2023) 21:23. doi: 10.1186/s12955-023-02101-5
52. Tekin A, Karadağ H, Süleymanoğlu M, Tekin M, Kayran Y, Alpak G, et al. Prevalence and gender differences in symptomatology of posttraumatic stress disorder and depression among Iraqi Yazidis displaced into Turkey. Eur J Psychotraumatol. (2016) 7:28556. doi: 10.3402/ejpt.v7.28556
53. Salad AM, Malik S, Ndithia JM, Noor Z, Madeo M, Ibrahim M. Prevalence of mental disorders and psychological trauma among conflict- affected population in Somalia: a cross-sectional study. Front Public Health. (2023) 11:1219992. doi: 10.3389/fpubh.2023.1219992
54. Braun-Lewensohn O, Abu-Kaf S, Al-Said K. Women in refugee camps: which coping resources help them to adapt? Int J Environ Res Public Health. (2019) 16(20):3990. doi: 10.3390/ijerph16203990
55. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
56. van de Wiel W, Castillo-Laborde C, Francisco Urzúa I, Fish M, Scholte WF. Mental health consequences of long-term stays in refugee camps: preliminary evidence from Moria. BMC Public Health. (2021) 21(1):1290. doi: 10.1186/s12889-021-11301-x
57. Ahmad F, Othman N, Hynie M, Bayoumi AM, Oda A, McKenzie K. Depression-level symptoms among Syrian refugees: findings from a Canadian longitudinal study. J Ment Health. (2021) 30(2):246–54. doi: 10.1080/09638237.2020.1765998
58. Siriwardhana C, Ali SS, Roberts B, Stewart R. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Conflict Health. (2014) 8(1):1–14. doi: 10.1186/1752-1505-8-13
59. Nissen A, Cauley P, Saboonchi F, A JA, Solberg Ø. Mental health in adult refugees from Syria resettled in Norway between 2015 and 2017: a nationwide, questionnaire-based, cross-sectional prevalence study. Eur J Psychotraumatol. (2021) 12(1):1994218. doi: 10.1080/20008198.2021.1994218
60. Bacchus L, Bangha M, Cornish-Spencer S, Franchi G, Hess T, Hossain M, et al. Disability, violence, and mental health among Somali refugee women in a humanitarian setting. Global Ment Health. (2020) 7:e30. doi: 10.1017/gmh.2020.23
61. Kaplan V, Düken ME. Mental health states of the refugee women in the 10-year visiting process: an assessment in context of the sociocultural adaptation. Middle East Curr Psychiatry. (2023) 30:72. doi: 10.1186/s43045-023-00345-x
62. Pudpong N, Kosiyaporn H, Phaiyarom M, Kunpeuk W, Sinam P, Julchoo S, et al. Situation of self-reported anxiety and depression among urban refugees and asylum seekers in Thailand, 2019. Int J Environ Res Public Health. (2021) 18(14). doi: 10.3390/ijerph18147269
63. Lumley M, Katsikitis M, Statham D. Depression, anxiety, and acculturative stress among resettled Bhutanese refugees in Australia. J Cross-Cultural Psychol. (2018) 49:1269–82. doi: 10.1177/0022022118786458
Keywords: depression, anxiety, Sudanese refugee, Ethiopia, Bambasi Camp
Citation: Amede ES, Tesfaye E and Ahmed G (2024) Prevalence and associated factors of depression and anxiety among Sudanese refugees at Bambasi Camp in northwest Ethiopia: a cross-sectional study. Front. Psychiatry 15:1505876. doi: 10.3389/fpsyt.2024.1505876
Received: 03 October 2024; Accepted: 13 November 2024;
Published: 19 December 2024.
Edited by:
Alina Wilkowska, Medical University of Gdansk, PolandReviewed by:
Bojana Pejuskovic, University of Belgrade, SerbiaFriyal Alqahtani, Imam Abdulrahman Bin Faisal University, Saudi Arabia
Copyright © 2024 Amede, Tesfaye and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Endris Seid Amede, c2VpZGVuZHJpczMzNEBnbWFpbC5jb20=
 Endris Seid Amede
Endris Seid Amede Elias Tesfaye
Elias Tesfaye Gutema Ahmed2
Gutema Ahmed2