- 1Department of Psychiatry, Sir Run Run Shaw Hospital, School of Medcine, Zhejiang University, Hangzhou, Zhejiang, China
- 2The Second Department of General Psychiatry, The Third Hospital of Quzhou City, Quzhou, Zhejiang, China
- 3Department of Psychiatry, Shaoxing 7th People’s Hospital, Shaoxing, Zhejiang, China
- 4The Affiliated Hospital of Hangzhou Normal University, Hangzhou Normal University, Hangzhou, Zhejiang, China
- 5Department of Gastroenterology, Sir Run Run Shaw Hospital, School of Medcine, Zhejiang University, Hangzhou, Zhejiang, China
Here we report on a case of a 40-year-old female patient who presented with hypomanic episode after hyperthyroidism and major depressive episode after hypothyroidism, which was initially misdiagnosed as bipolar disorder due to another medical condition, and was found to be a co-morbid bipolar disorder of hyperthyroidism after treatment and follow-up. The course of diagnosis and treatment in this case suggests a close temporal relationship does not necessarily mean that there is a causal relationship on a physiologic level. User’s Guide for the SCID-5-CV Structured Clinical Interview for DSM-5 Disorders elaborate that the diagnosis of “……due to another medical condition” is relatively rare, and co-morbidity between psychiatric disorders and somatic diseases is much more common. Therefore, the relationship between somatic diseases and psychiatric disorders requires careful study of symptom correlation and more time for observational follow-up. When in doubt, the examiner’s default assumption should be that the somatic disease is not the cause (i.e., the psychiatric disorder is primary).
Introduction
The integrative concept of psychosomatic disorders (1) is increasingly emphasized in clinical practice. Somatic diseases can lead to psychiatric symptoms, such as adrenal insufficiency causing depressive symptoms (2), and psychiatric disorders can affect physical symptoms, like anxiety disorders exacerbating abdominal pain and diarrhea (3). When somatic disease and psychiatric disorder coexist, especially when the two systems producing the symptoms influence each other, clinicians often use monism to explain all symptoms. However, patients differ, and while we recognize psychosomatic integration, we must also consider the possibility that the relationship between somatic disease and psychiatric disorder is not as strong as assumed.
We report a case of a patient who presented with hypomanic episode after hyperthyroidism and major depressive episode after hypothyroidism, initially misdiagnosed as bipolar disorder due to another medical condition. After treatment and follow-up, it was found to be a co-morbid bipolar disorder with hyperthyroidism.
History of present illness
A 40-year-old female patient presented 10 months ago with heat intolerance, oligomenorrhea, and a weight loss of 1-2 kg over 2 months. Her physical examination report showed hyperthyroidism 8 months ago but did not follow up in time. 7 months ago, she became very happy and energetic, sleeping 2 hours less than usual but still feeling energetic throughout the day. She was more active, went out with friends more often, talked more, and was more confident than usual. She spent more money and often bought unnecessary things. Her family noticed these changes and found her overexcited.
6 months ago, she was reminded by her family to visit the hospital, where she was diagnosed with hyperthyroidism and treated with methimazole tablets 20mg once daily. 4 months ago, her high mood stabilized, and her thyroid function returned to normal.
3 months ago, she developed worrying and overthinking, focusing on the negative, and had difficulty making decisions. She constantly rubbed her hands and thighs together, felt depressed, and wanted to cry. She lost interest in activities she used to enjoy, felt her brain was sluggish, had difficulty concentrating, and experienced memory loss. She has decreased appetite, constipation, fear of cold, easy fatigue. She denied suicidal thoughts.
Upon revisiting the endocrinology department, tests showed hypothyroidism, so the methimazole dose was gradually reduced to 5mg once daily. 1 month ago, her thyroid function was re-examined and found normal, but her mood remained depressive. The endocrinologist referred her to the psychiatry department, and she was hospitalized in our department 2 weeks ago.
Medical history
Apart from hyperthyroidism, the patient denied any other physical illnesses, surgeries, trauma, or substance abuse. Previous annual physicals showed no thyroid function problems.
Personal history
The patient has a Bachelor’s degree and is a college teacher. She was previously outgoing, enjoyed making friends, and was meticulous about hygiene. Since the onset of the COVID-19 pandemic, her cleanliness habits worsened. She frequently washed her hands, more than 10 times a day, and always did so after touching public places. Although her mother thought she was excessively clean, she did not think the symptoms bothered her too much. She is married, has a good relationship with her husband, and has a daughter. However, her husband disliked her cleanliness habits.
Hospitalization treatment
On admission, the patient’s blood tests, blood biochemistry, thyroid function, cranial MRI, anti-syphilis spirochete antibody, HIV antibody, chest CT, and abdominal ultrasound were all negative. Her scores on the Hamilton Rating Scale for Depression (HAMD-17) were 25, Hamilton Anxiety Rating Scale (HAMA) were 18, Pittsburgh Sleep Quality Index (PSQI) were 12, Mood Disorder Questionnaire (MDQ) were 2, and Hypomania Symptom Checklist-32 (HCL-32) were 18.
The diagnosis of major depressive disorder due to another medical condition was considered, and her previous hypomanic symptoms were thought to be due to hyperthyroidism. Escitalopram was gradually increased to 20mg once daily. After two weeks of hospitalization, her depression and anxiety significantly decreased. After her symptoms almost disappeared (5 points for HAMD-17, 4 points for HAMA), she was discharged with normalized thyroid hormone levels.
Follow-up after discharge
After discharge, the patient again exhibited symptoms of high emotion, high energy, and increased activity, scoring 14 on the Young’s Mania Rating Scale (YMRS). Her thyroid function was normal, so the diagnosis was changed to bipolar disorder. Her medication was adjusted to lithium carbonate 0.9 once daily and aripiprazole 10mg once nightly. Her mood stabilized after three weeks. Maintaining the same medications, she was followed up for 5 months with normal thyroid function and stable mood, with HAMD-17 and YMRS scores of 5, 6 (1 month later), 5, 4 (3 months later), and 6, 5 (5 months later), respectively.
Discussion
We believe that this patient’s diagnosis should be bipolar disorder co-morbid with hyperthyroidism rather than bipolar disorder due to hyperthyroidism. The reasons are as follows:
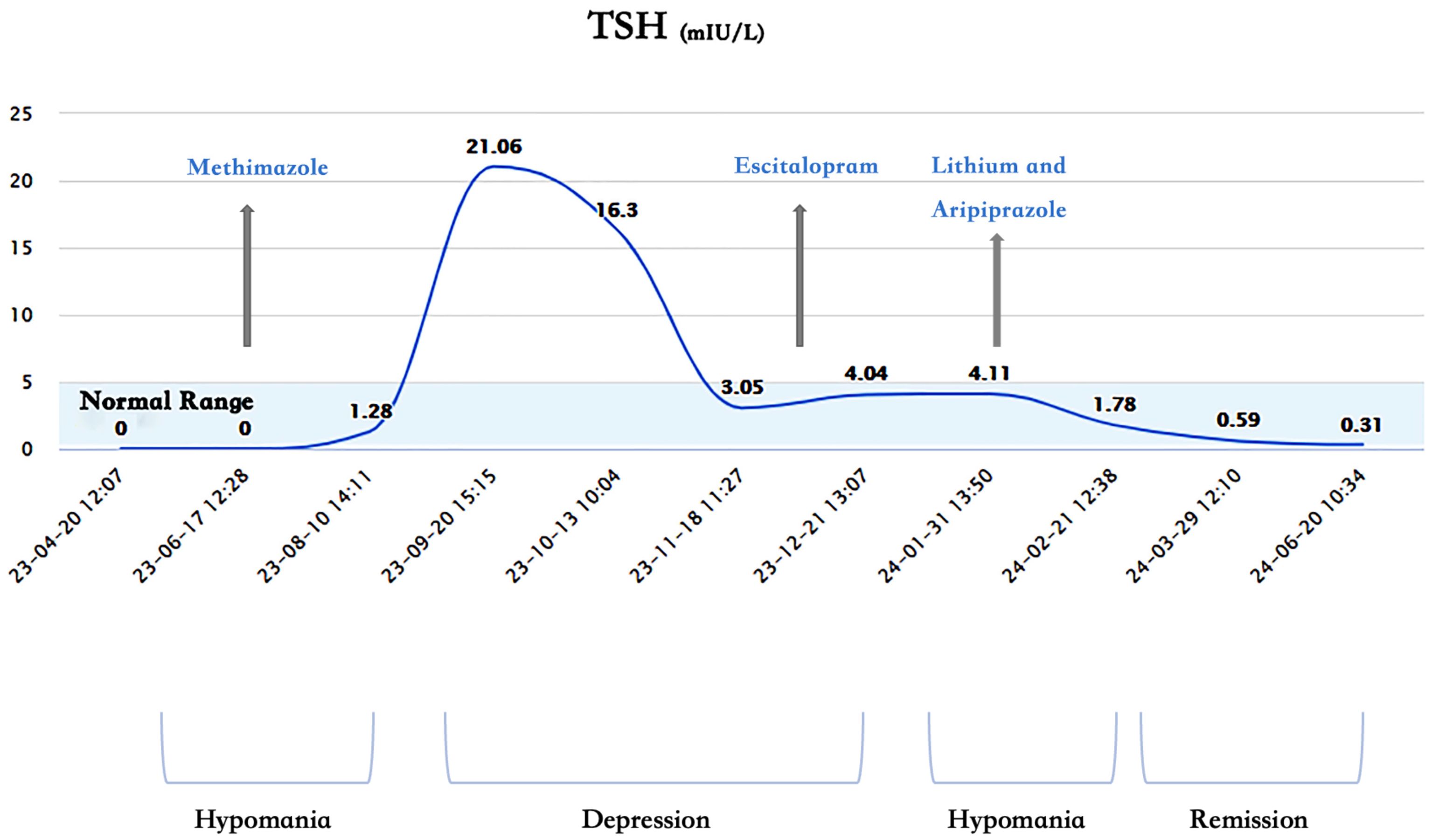
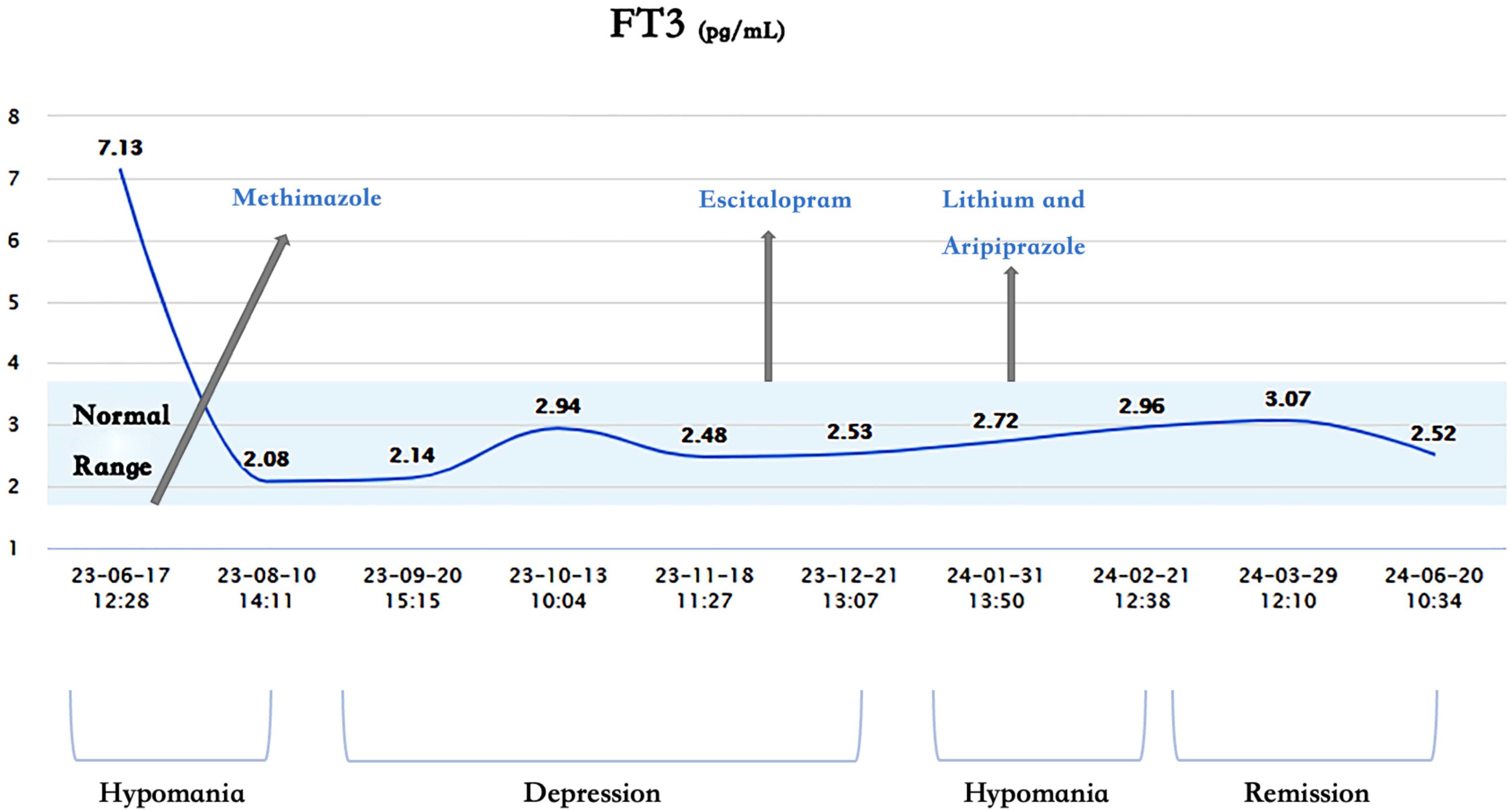
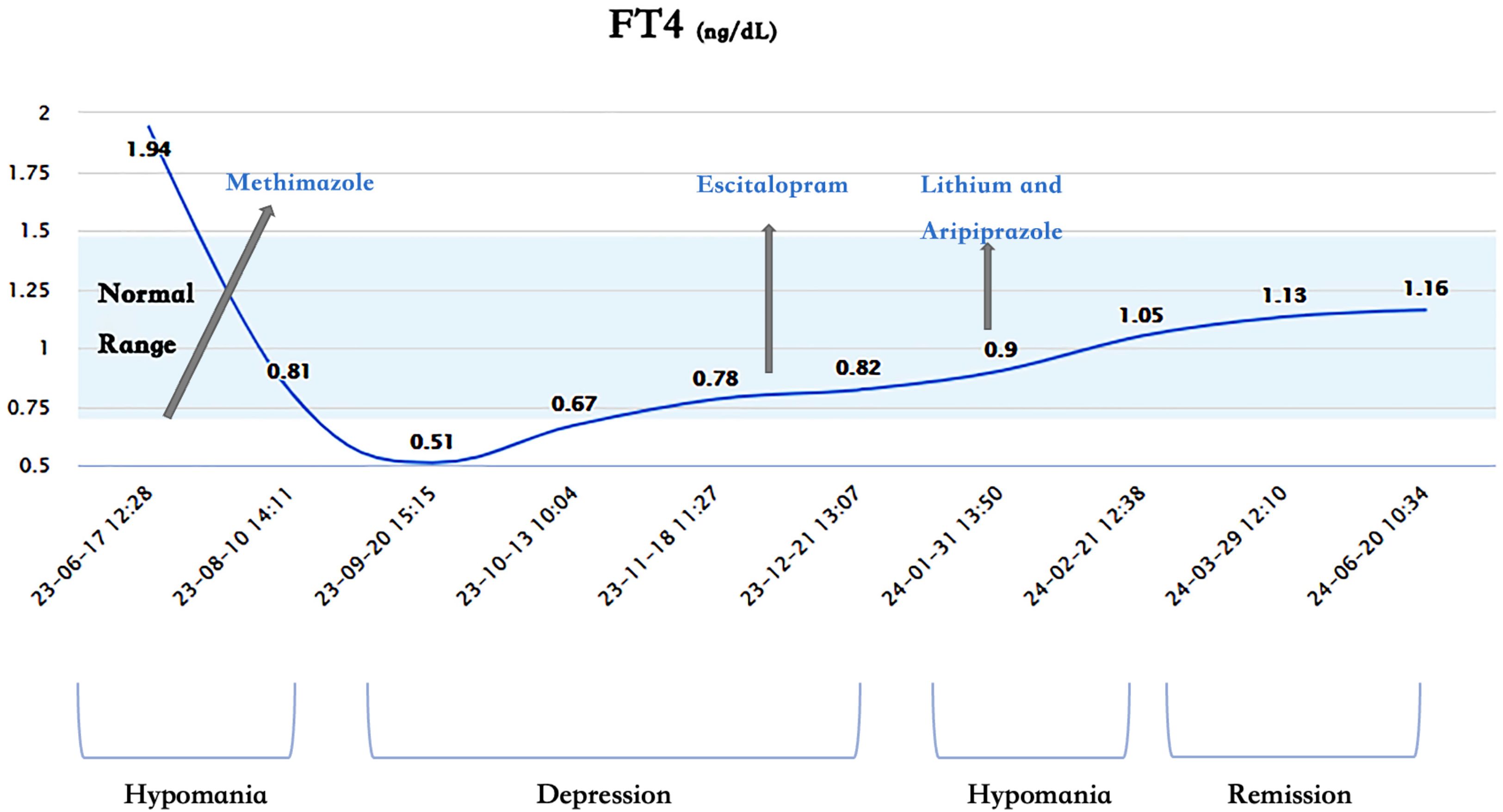
1. Lack of Correlation Between Mood and Thyroid Function: The patient’s mood and thyroid function did not show a significant correlation. Her thyroid hormones were in the normal range from 1 month before hospitalization to 5 months after discharge, during which she experienced three periods: depression, hypomania, and remission (Figures 1–3). Without adjusting methimazole or thyroid hormone medication, her mood was stable during the five-month follow-up after using mood stabilizers, unlike the two episodes of hypomania and one episode of depression in eight months before using mood stabilizers.
2. Hypomania Not Due to Hyperthyroidism: The common emotional and behavioral symptoms seen in patients with hyperthyroidism is anxiety, restlessness, irritability, and emotional lability (4), while mania or hypomania is a multi-symptom syndrome with elevated or irritable mood as the core symptom. According to DSM-5-TR, medical conditions more commonly leading to mania or hypomania include hypercortisolism, multiple sclerosis, stroke, traumatic brain injury, and systemic lupus erythematosus, not hyperthyroidism (5).
3. Depression and Hypothyroidism Not Closely Related:Hypothyroidism, a common side effect of metiomidazole, followed by depressive symptoms. We believe that hypothyroidism may also be a trigger, not a cause. The most important reason is that one month after thyroid function returns to normal, the patient’s mood is still depressive.
4. Existing Obsessive-Compulsive Symptoms Before Hyperthyroidism: The patient had obsessive-compulsive symptoms for several years before the hyperthyroidism diagnosis, and previous annual physicals showed no thyroid function problems. Several clinical features (e.g., mood switches, mood instability, depressive episodes, anxiety, sleep disorders, attention deficits, conduct disorders, and substance use disorders) are associated with a higher risk of developing bipolar spectrum disorder. These symptoms or syndromes may appear years (1.8 to 7.3 years) before an acute manic or hypomanic episode (6). The prevalence of obsessive-compulsive disorder (OCD) in patients with BD is approximately 17%, and OCD is associated with the onset of BD with a hazard ratio of 6.9 (7). OCD may be a key feature in the development of BD.
Although we do not believe it is the cause, hyperthyroidism may have played a role in stimulating the bipolar disorder. A systematic review found that thyroid autoimmunity is an independent risk factor for bipolar disorder (8). Some studies have found a clear association between hyperthyroidism and bipolar disorder (9, 10), while others have suggested that hyperthyroidism may increase the risk of developing bipolar disorder (11, 12), with one study even finding that the correlation between hyperthyroidism and bipolar disorder was the highest of any psychiatric disorder (13). Neurobiological studies have uncovered some mechanisms of thyroid hormone in the brain, providing possible explanations for the interaction between thyroid hormones and emotions (14, 15). However, it is important to note that the above studies were conducted on two disease subjects, rather than two manifestations of a single disease occurrence.
Hypothyroidism was considered to be an etiologic factor for depression, and is also described in DSM-5-TR as a common medical condition leading to depression (5). However, in a systematic review and meta-analysis, the effect size of the association between hypothyroidism and depression was substantially lower than previously hypothesized (16). The psychiatric symptoms of hypothyroidism are most often characterized by slowed mentation, poor concentration, and decreased short-term memory, followed by social withdrawal, psychomotor retardation, depressed mood, and apathy (17).
The age of onset of bipolar disorder is generally low, but the patient in this case did not start until she was 40 years old. One systematic review found that the age of onset of bipolar disorder showed a trinomial distribution: early-onset at an average age of 17.3 years (45% of cases), mid-onset at 26 years (35% of cases) and late-onset at an average age of 41.9 years (20% of cases) (18).
In the context of the biopsychosocial model, the idea of mind-body integration of disease is becoming more emphasized. In this case, the patient developed hypomanic episode after hyperthyroidism and major depressive episode after hypothyroidism, leading to a monistic diagnosis. However, the User’s Guide for the SCID-5-CV Structured Clinical Interview for DSM-5 Disorders states that a close temporal relationship does not necessarily imply a causal relationship on a physiological level. The diagnosis of “…… due to another medical condition” is relatively rare, and co-morbidity between psychiatric disorders and somatic diseases is much more common (19).
From this case and the previous literatures, the relationship between thyroid function and mood was found not to be as strong as previously hypothesized. The relationship between other somatic diseases and psychiatric disorders also requires more researches. When psychiatrists encounter such patients, we need to be more patient to focus on the symptom correlation and more time for observational follow-up. When in doubt, our default assumption should be that the somatic disease is not the cause (i.e., the psychiatric disorder is primary).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by ethics committee of Sir Run Run Shaw hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participant provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JY: Writing – original draft. JX: Writing – original draft. RY: Writing – original draft. RHY: Writing – original draft. YS: Writing – review & editing. ND: Writing – review & editing. WC: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The Science and Technology Program of Hangzhou Municipality (20212013B02, Z20200051) to Yuedi Shen.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. MaClean PD. Psychosomatic disease and the visceral brain; recent developments bearing on the Papez theory of emotion. Psychosom Med. (1949) 11:338–53. doi: 10.1097/00006842-194911000-00003
2. Leigh H, Kramer SI. The psychiatric manifestations of endocrine disease. Adv Intern Med. (1984) 29:413–45.
3. Chang L. The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. Gastroenterology. (2011) 140:761–5. doi: 10.1053/j.gastro.2011.01.032
4. Stern RA, Robinson B, Thorner AR, Arruda JE, Prohaska ML, Prange AJ. A survey study of neuropsychiatric complaints in patients with Graves’ disease. J Neuropsychiatry Clin Neurosci. (1996) 8:181–5. doi: 10.1176/jnp.8.2.181
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5-TR. Washington, DC: American Psychiatric Publishing (2022).
6. Faedda GL, Baldessarini RJ, Marangoni C, Bechdolf A, Berk M, Birmaher B, et al. An International Society of Bipolar Disorders task force report: Precursors and prodromes of bipolar disorder. Bipolar Disord. (2019) 21:720–40. doi: 10.1111/bdi.12831
7. Hofer PD, Wahl K, Meyer AH, Miché M, Beesdo-Baum K, Wong SF, et al. Obsessive–compulsive disorder and the risk of subsequent mental disorders: A community study of adolescents and young adults. Depress Anxiety. (2018) 35:339–45. doi: 10.1002/da.22733
8. Barbuti M, Murru A, Verdolini N, Guiso G, Vieta E, Pacchiarotti I, et al. Thyroid autoimmunity in bipolar disorder: A systematic review. J Affect Disord. (2017) 15:221. doi: 10.1016/j.jad.2017.06.019
9. Thomsen AF, Kessing LV. Increased risk of hyperthyroidism among patients hospitalized with bipolar disorder. Bipolar Disord. (2005) 7:351–7. doi: 10.1111/j.1399-5618.2005.00205.x
10. Krishna VN, Thunga R, Unnikrishnan B, Kanchan T, Bukelo MJ, Mehta RK, et al. Association between bipolar affective disorder and thyroid dysfunction. Asian J Psychiatr. (2013) 6:42–5. doi: 10.1016/j.ajp.2012.08.003
11. Hu LY, Shen CC, Hu YW, Chen MH, Tsai CF, Chiang HL, et al. Hyperthyroidism and risk for bipolar disorders: A nationwide population-based study. PloS One. (2013) 8:e73057. doi: 10.1371/journal.pone.0073057
12. Thomsen AF, Kvist TK, Andersen PK, Kessing LV. Increased risk of affective disorder following hospitalization with hyperthyroidism - A register-based study. Eur J Endocrinol. (2005) 152:535–43. doi: 10.1530/eje.1.01894
13. Zader SJ, Williams E, Buryk MA. Mental health conditions and hyperthyroidism. Pediatrics. (2019) 144:e20182874. doi: 10.1542/peds.2018-2874
14. Hage MP, Azar ST. The link between thyroid function and depression. J Thyroid Res. (2012) 2012:590648. doi: 10.1155/2012/590648
15. Bauer M, Goetz T, Glenn T, Whybrow PC. The thyroid-brain interaction in thyroid disorders and mood disorders. J Neuroendocrinol. (2008) 20:1101–14. doi: 10.1111/j.1365-2826.2008.01774.x
16. Bode H, Ivens B, Bschor T, Schwarzer G, Henssler J, Baethge C. Association of hypothyroidism and clinical depression: A systematic review and meta-analysis. JAMA Psychiatry. (2021) 78:1375–83. doi: 10.1001/jamapsychiatry.2021.250616
17. Osterweil D, Syndulko K, Cohen SN, Pettier-Jennings PD, Hershman JM, Cummings JL, et al. Cognitive function in non-demented older adults with hypothyroidism. J Am Geriatr Soc. (1992) 40:325–35. doi: 10.1111/j.1532-5415.1992.tb02130.x
18. Bolton S, Warner J, Harriss E, Geddes J, Saunders KEA. Bipolar disorder: Trimodal age-at-onset distribution. Bipolar Disord. (2021) 23:341–56. doi: 10.1111/bdi.13016
Keywords: hyperthyroidism, comorbidity, psychosomatic disorders, bipolar disorder, bipolar disorder due to another medical condition
Citation: Yao J, Xu J, Yan R, Ye R, Shen Y, Dai N and Chen W (2024) Is thyroid dysfunction a cause or a trigger of bipolar disorder? a case report. Front. Psychiatry 15:1473536. doi: 10.3389/fpsyt.2024.1473536
Received: 31 July 2024; Accepted: 26 August 2024;
Published: 12 September 2024.
Edited by:
Xiaojun Huang, Central South University, ChinaReviewed by:
Qinghua Luo, First Affiliated Hospital of Chongqing Medical University, ChinaXijia Xu, Nanjing Brain Hospital Affiliated to Nanjing Medical University, China
Copyright © 2024 Yao, Xu, Yan, Ye, Shen, Dai and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ning Dai, bmRhaWNuQHpqdS5lZHUuY24=; Wei Chen, c3JyY3dAemp1LmVkdS5jbg==
 Jiashu Yao1
Jiashu Yao1 Yuedi Shen
Yuedi Shen Ning Dai
Ning Dai Wei Chen
Wei Chen