- 1Ramat-Chen Brüll Mental Health Center, Clalit Health Services Community Division, Tel-Aviv, Israel
- 2Faculty of Medical & Health Sciences, Tel Aviv University, Tel-Aviv, Israel
- 3Baruch Ivcher School of Psychology, Reichman University, Herzliya, Israel
Introduction: Since the onset of the COVID-19 pandemic in 2020, a significant body of research has explored the impact of the virus and its preventative measures on mental health among individuals with OCD. However, to our knowledge, no study has been conducted to test whether the very behaviors considered symptomatic of OCD inadvertently offer a protective shield against COVID-19 infection.
Methods: This retrospective cohort study utilized the electronic health record database of Israel’s largest healthcare provider, Clalit Health Services (CHS), to compare patients with and without recorded OCD diagnoses in terms of the number of COVID-19 tests taken, hospitalizations, vaccination rates, and infection rates during and after different pandemic waves.
Results: The OCD group had a slightly higher rate of positive COVID-19 tests compared to the control group (p<0.001), but only since the easing of restrictions after the end of the fifth wave. The OCD group was also more likely to receive a third dose of the COVID-19 vaccine (p<0.001).
Discussion: Our findings suggest that OCD may not confer protection against COVID-19 and may even be associated with slightly higher infection rates, particularly in the post-restrictions period.
1 Introduction
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition affecting 1–3% of individuals, characterized by obsessions—unwanted, recurring thoughts—and compulsions—repetitive behaviors performed to alleviate distress. Symptoms often persist and can worsen over time, leading to significant impairment and reduced quality of life. The etiology of OCD is multifactorial, involving genetic, neurobiological, and environmental factors (1, 2).
In patients with OCD, the relentless dread of contamination is the most commonly observed symptom (3, 4). Contamination fear is the fear of direct or indirect contact with a person or item perceived as dirty or harmful (5). This form of OCD is marked by enduring and overarching concerns about contamination, a characteristic widely recognized as a defining, distinctive, and predominant facet of the disorder (6). Individuals with these obsessions often engage in compensatory behaviors such as excessive washing, cleaning, and checking to eliminate the perceived threat of contamination and protect themselves from various feared outcomes, such as illness. This aspect of OCD can dominate a person’s life, leading to significant distress and impairment. Moreover, the fear of contamination can lead to a preoccupation with not only personal cleanliness but also with the cleanliness of one’s surroundings, prompting avoidance of anything considered contaminant (1).
From an evolutionary standpoint, some OCD characteristics, especially those related to cleanliness and avoiding germs, might have offered survival benefits in the past. Behaviors aimed at reducing exposure to pathogens could have been beneficial in ancestral environments where infectious diseases were a major cause of mortality. This perspective suggests that certain OCD traits may be an exaggeration of evolutionarily adaptive behaviors evolved to avoid harm, with the emergence of a fully-fledged disorder in a minority of the population representing a pathological extreme of these otherwise advantageous traits (7, 8).
In early 2020, Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2, emerged as a global pandemic. It has posed unprecedented challenges to public health, economies, and social structures worldwide. The virus primarily spreads through respiratory droplets, necessitating public health measures such as social distancing, mask-wearing, and enhanced hygiene practices (9).
The COVID-19 pandemic has brought unique considerations for individuals with OCD, especially those with contamination fears. However, studies have shown that OCD symptoms did not universally exacerbate during the COVID-19 pandemic as previously feared (10–12). This period has also sparked renewed interest in the idea that certain obsessive-compulsive behaviors may offer an evolutionary advantage in reducing infectious disease transmission. The emergence of COVID-19 provided a critical moment to explore this concept further (13).
While there is an increasing amount of research on how COVID-19 and its prevention strategies have affected the mental health and symptoms of those with OCD (14), there remains a notable gap in understanding how having OCD affects the likelihood of contracting COVID-19, which this study intends to address.
Existing literature has established that specific comorbidities commonly associated with OCD, such as Attention-Deficit Hyperactivity Disorder (ADHD) and Schizophrenia (15–18), may affect one’s chances of contracting COVID-19. However, to our knowledge, no study has specifically examined the direct impact of OCD diagnosis on COVID-19 infection rates.
Using the database of Clalit Health Services (CHS), the largest healthcare provider in Israel, this study examines whether OCD may provide any protective benefits against COVID-19 and explores the complex interactions between OCD and susceptibility to the virus.
2 Materials and methods
The study was approved by the institutional review boards (Study designation 0143-22-COM). It was conducted in accordance with the International Conference on Harmonisation guidelines and ethical principles of the Declaration of Helsinki.
2.1 Study design and procedure
This retrospective cohort study was conducted using CHS’s electronic health record database. CHS is an Israeli payer-provider integrated health care system serving over 4.5 million members, constituting 54% of the Israeli population. The database includes patient demographic and clinical characteristics, hospital discharge and outpatient clinic diagnoses, laboratory test results, medical treatments, and medication dispensation information. Data was accessed and extracted from the CHS database using the Clalit Research Data secure anonymized data-sharing platform powered by MDClone (https://www.mdclone.com).
The dataset was used to investigate the differences in COVID-19 infection rates between patients with and without a recorded diagnosis of OCD.
To delineate the progression of the COVID-19 pandemic, distinct waves were defined based on COVID-19 wave data collected and published by the Israeli Ministry of Health (19). The first COVID-19 wave spanned from March 1st to May 31st, 2020, followed by the second wave from June 1st to October 30th, 2020. The third wave was from November 1st, 2020, to April 30th, 2021, the fourth from May 1st to October 30th, 2021, and the fifth wave extended from November 1st, 2021, to April 30th, 2022. Mask restrictions were lifted on all low-risk settings in Israel on April 23rd 2022 (20).
2.2 Inclusion criteria
Patients were eligible if they were born on or before February 1st, 2016, ensuring they were at least four years old at the onset of the pandemic. Additionally, they needed to have been insured by CHS on or before February 1st, 2020. The coverage by CHS needed to extend up to February 1st, 2023, or until the patient’s demise, whichever occurred first. These criteria ensured a consistent and comprehensive patient data analysis over the pandemic’s specified duration.
2.3 Measures
Demographic information, including gender and socioeconomic status (SES) categorized as Low, Medium, or High, was obtained from CHS’s computerized database. Age was computed based on the year of birth, establishing the age of participants as of the year 2020.
OCD diagnosis: Patients were classified as having an OCD diagnosis based on the presence of any diagnosis under the ICD-10 code F42.
Comorbid psychopathology: This study assessed comorbid psychopathology by identifying psychiatric conditions through historical ICD-10 diagnoses, including: Post-traumatic stress disorder (PTSD) as F43.1; Attention-deficit hyperactivity disorder (ADHD) as F90; Schizophrenia as F20; Schizoaffective disorder as F25; and Bipolar disorder as F31, excluding cases with schizoaffective disorder or schizophrenia diagnoses. Anxiety was categorized under F40.0, F40.2, F41.0, F41.1, and F41.9, while Depression was identified through F32 and F33, omitting cases with bipolar, schizoaffective, or schizophrenia disorders. Panic and agoraphobia were specified with codes F41.0 and F40.01, respectively.
Severe psychopathology was defined as a historical diagnosis of either Schizophrenia or schizoaffective disorders, and Any psychopathology was determined by the presence of any psychiatric diagnosis.
2.4 Statistical analysis
Initially, we compared the entire sample, which included the control group, with the OCD group in relation to sociodemographic characteristics and the existence of any psychiatric disorders. Categorical variables were assessed using the χ2 test, while continuous variables were examined utilizing an independent-samples t-test.
After a preliminary review, we matched individuals with OCD to controls, ensuring a balanced comparison across sociodemographic and comorbid psychopathology variables. Matching was conducted on age, gender, socioeconomic status, severe psychopathology, any psychopathology, ADHD diagnosis, and bipolar disorder diagnosis. Leveraging the control group’s large size relative to the OCD group we attained a precise 1:1 match for all variables, resulting in identical distributions between the OCD and control groups. When multiple controls fit an OCD case, we randomly selected one to pair with each OCD individual.
To compare the OCD and control groups across COVID-19 outcomes, we performed logistic regression analyses for binary outcomes (e.g., positive COVID-19 test, wave-specific positivity, hospitalization, and vaccination) and linear regression analyses for continuous outcomes (e.g., number of COVID tests). For each binary outcome, two logistic regression models were fitted. The first model was unadjusted, predicting the outcome from the group (OCD vs. control). The second model adjusted for psychiatric comorbidities that differed between the groups, specifically PTSD, schizoaffective disorder, panic disorder, anxiety, and depression. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for each model. For the continuous outcomes, linear regression models were used to estimate unadjusted and adjusted differences in means (β coefficients) between the OCD and control groups, with 95% CIs reported. Additionally, chi-square tests were used to compare the proportions between the OCD and control groups for each binary outcome, with the corresponding p-values reported.
We conducted a Kaplan-Meier survival analysis to evaluate the time to the first positive COVID-19 test for individuals with OCD compared to the control group. Additionally, we performed Cox proportional hazards regression models to analyze the effect of OCD on the time to first positive COVID-19 test, using hazard ratios (HRs) to assess the risk. Both unadjusted and adjusted models were fitted. The adjusted model controlled for psychiatric comorbidities, including PTSD, schizoaffective disorder, panic disorder, anxiety, and depression.
The subsequent analysis compared matched OCD individuals and controls, examining COVID-19 infection rates, testing frequency, hospital stays, and vaccination rates. A linear regression predicted the time to the first positive result for those testing positive, considering the same variables. Additionally, a Cox proportional hazards regression analyzed OCD’s impact on infection timing, using hazard ratios to assess risk.
All statistical analyses were conducted using R version 4.2.3.
3 Results
3.1 Descriptive statistics and baseline group comparison
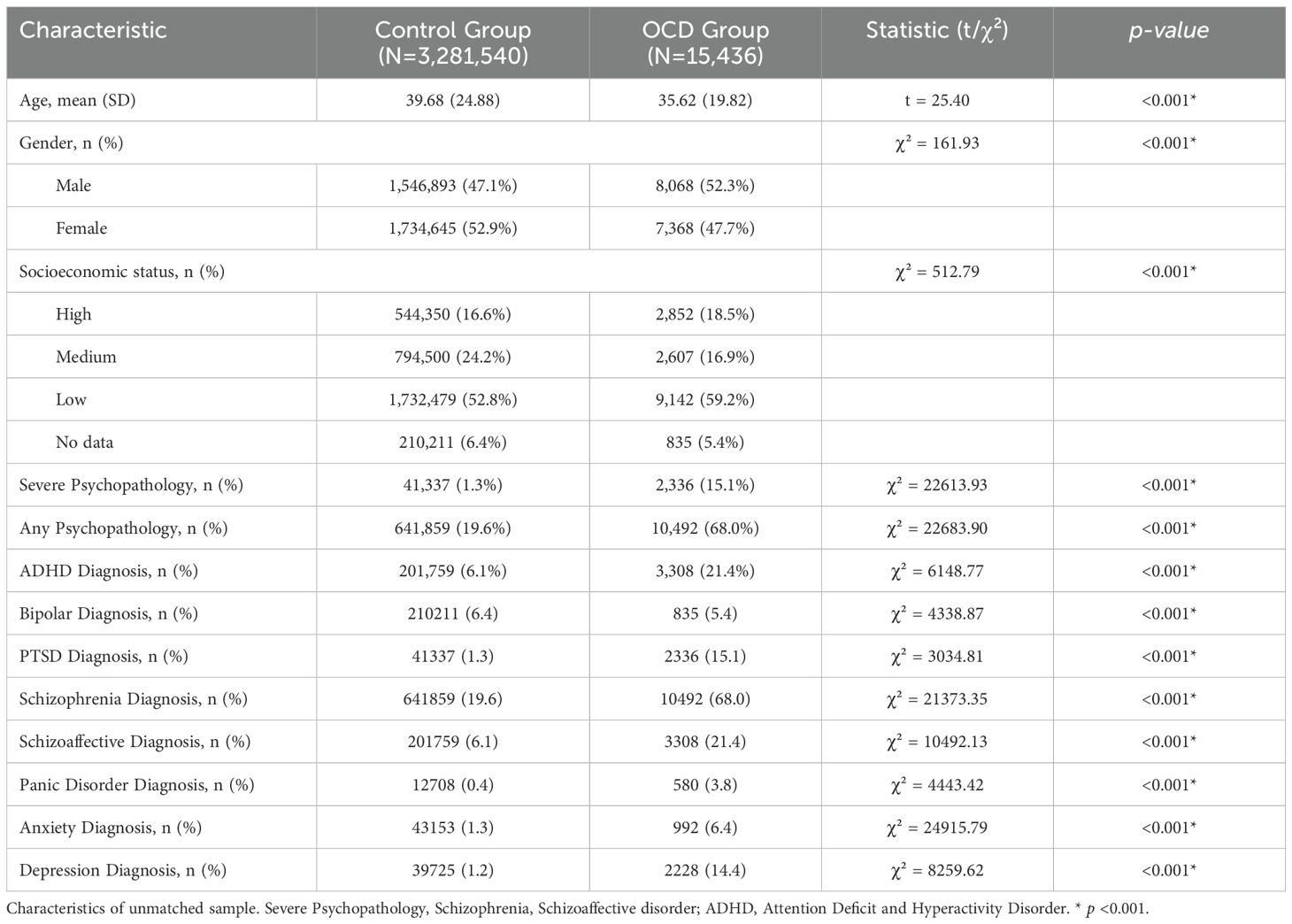
The sample included N=3,281,540 members in the control group and N=15,436 in the OCD group. Table 1 shows baseline differences: the OCD group was younger (mean age 35.62 vs. 39.68; p<0.001) and had more males (52.3% vs. 47.1%; p<0.001). Socioeconomic status varied, with OCD participants represented more in the highest and lowest brackets (18.5% vs. 16.6% and 59.2% vs. 52.8%; p<0.001). Severe psychiatric comorbidities were more common in the OCD group, with 15.1% showing severe psychopathology versus 1.3% in controls and 68.0% having any psychopathology compared to 19.6%. ADHD prevalence was also higher in the OCD group (21.4% vs. 6.1%).
3.2 Baseline characteristics of matched cohort
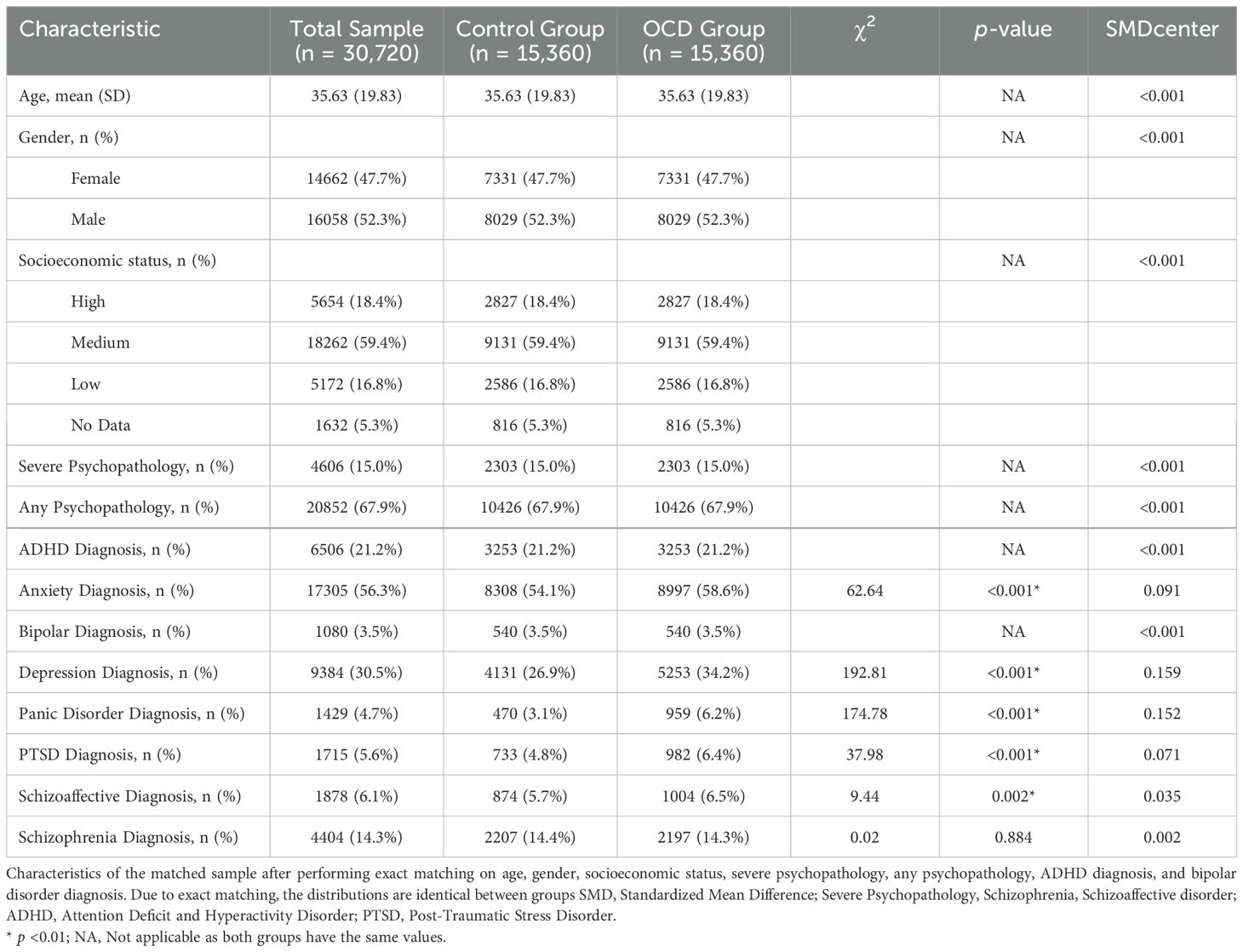
After performing exact matching on age, gender, SES, severe psychopathology, any psychopathology, ADHD diagnosis, and bipolar disorder diagnosis, the matched cohort consisted of 15,360 individuals in each group (OCD and control). The characteristics of the matched cohort are shown in Table 2.
The distribution of the matched variables was identical between the OCD and control groups, with all standardized mean differences (SMDs) less than 0.001, reflecting perfectly matched samples.
Regarding the remaining psychiatric comorbidities, some differences were observed. PTSD was more prevalent in the OCD group (6.4%) compared to controls (4.8%), although the standardized mean difference (SMD = 0.071) indicated minimal imbalance. Similarly, schizoaffective disorder was slightly more common in the OCD group (6.5% vs. 5.7%, SMD = 0.035). Panic disorder and anxiety disorder were also more prevalent in the OCD group (6.2% vs. 3.1% for panic, SMD = 0.152; 58.6% vs. 54.1% for anxiety, SMD = 0.091), though these differences remained small. Depression diagnosis was higher in the OCD group (34.2% vs. 26.9%, SMD = 0.159). Overall, the exact matching process resulted in a highly balanced cohort, with SMD values below 0.2 for all variables, indicating that any differences between the groups were minimal and within acceptable thresholds for cohort studies.
3.3 Comparison of COVID-19 outcomes: OCD and control groups
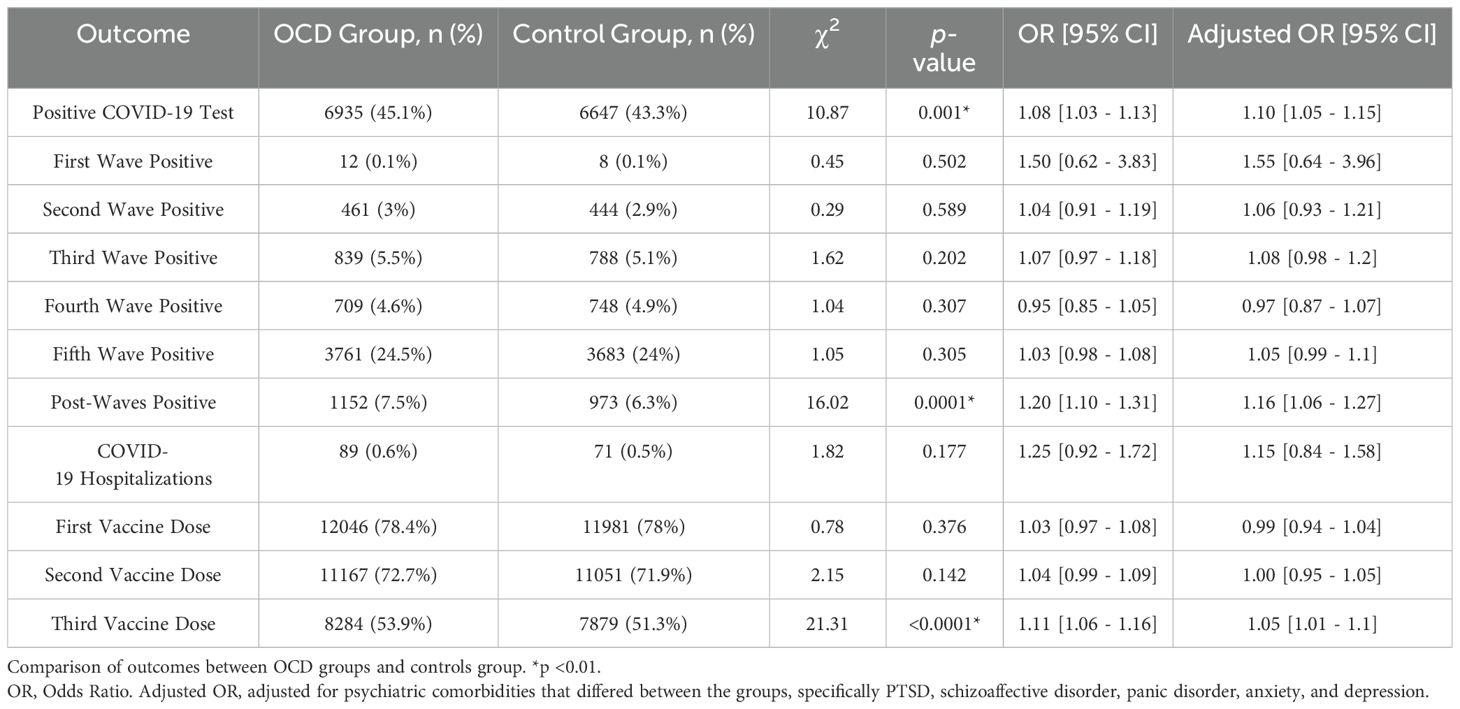
The results of the logistic regression analyses are presented in Table 3. Overall, the OCD group showed a slightly higher likelihood of testing positive for COVID-19 (45.1%) compared to the control group (43.3%), with the difference reaching statistical significance in both unadjusted (OR = 1.08 [1.03 - 1.13]) and adjusted models (OR = 1.10 [1.05 - 1.15]). Across the individual COVID-19 waves (first to fifth), there were no significant differences between the OCD and control groups in terms of positivity rates, as shown in the table. However, after the fifth wave, the OCD group had a significantly higher likelihood of testing positive (7.5%) compared to the control group (6.3%), with statistically significant results in both the unadjusted (OR = 1.20 [1.10 - 1.31]) and adjusted models (OR = 1.16 [1.06 - 1.27]) (see Figure 1). In terms of COVID-19 hospitalization, 0.6% of the OCD group and 0.5% of the control group were hospitalized, with no significant difference observed. For vaccination, there were no significant differences for the first or second doses between the two groups. However, the OCD group was more likely to receive the third vaccine dose (53.9% vs. 51.3%), with statistically significant differences in both the unadjusted (OR = 1.11 [1.06 - 1.16]) and adjusted models (OR = 1.05 [1.01 - 1.10]).
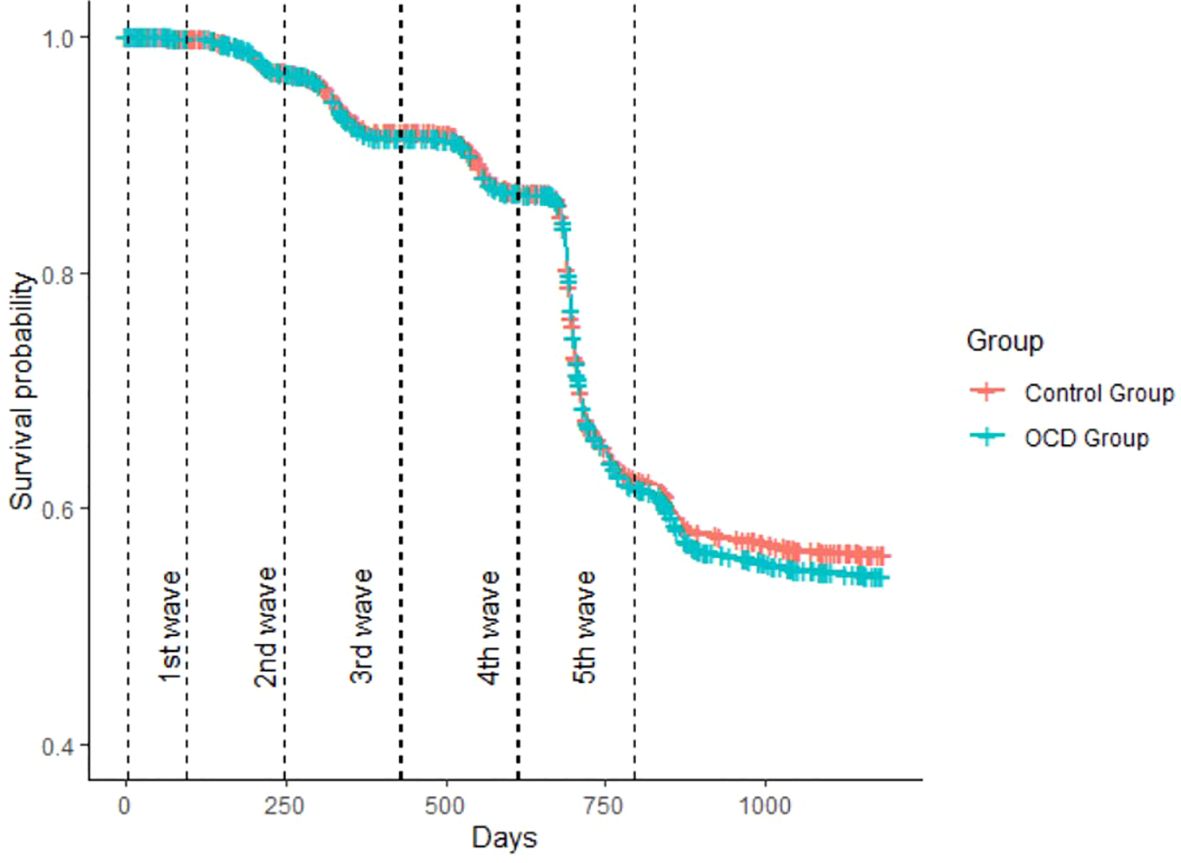
Figure 1. Kaplan-Meier Survival Analysis of Infection Timelines in OCD Patients vs. Matched Control Group. Kaplan–Meier plot showing days until the first positive COVID-19 test. Differences became significant in the time period after the fifth wave.
3.4 Prediction of days to infection
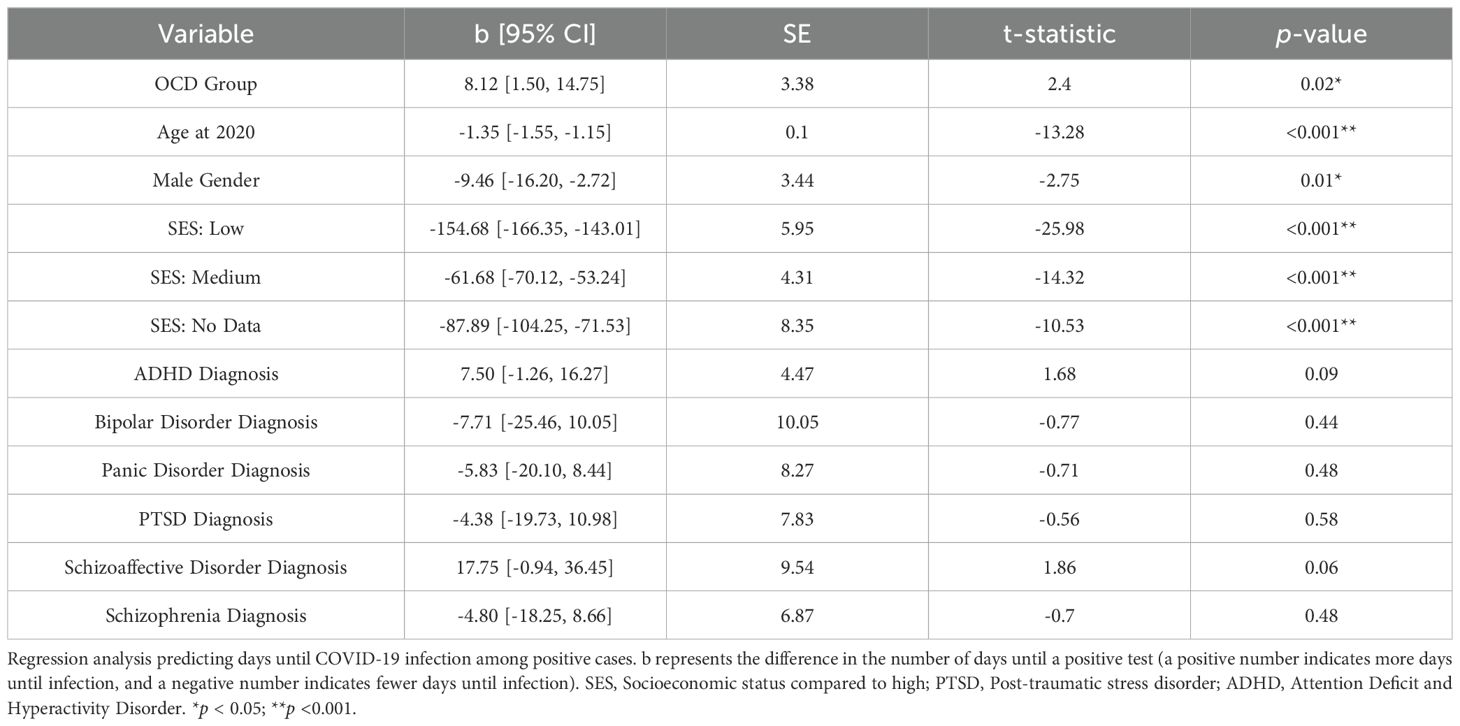
Among those who tested positive for COVID-19, a regression analysis predicted the number of days until infection. This analysis, which included the group and various covariates, is detailed in Table 4. Being in the OCD group was significantly linked with a longer time until infection, averaging an additional 8.12 days compared to the control group, even when considering other covariates (b=8.12, SE=3.38, p=0.02).
4 Discussion
In the shadow of the COVID-19 pandemic, a global health crisis that has upended lives and reshaped societal norms, our study explored the intricate interplay between OCD and susceptibility to the virus. OCD, a condition that exists at the crossroads of mental health and behavioral reactions to perceived threats, becomes particularly pertinent in this scenario. Of particular importance is the OCD subtype marked by contamination fears, a symptom pattern that naturally aligns with the heightened hygiene protocols practices that have become crucial in combating COVID-19 (9, 21). While many studies examined how the COVID-19 pandemic influenced patients with OCD (11–13), to our knowledge, none examined whether OCD behaviors influenced the likelihood of contracting COVID-19.
For this research, we utilized the comprehensive database of Clalit Health Services, Israel’s largest healthcare provider. The study was driven by the hypothesis that OCD, especially its contamination-centric manifestations, may confer a protective effect against the novel coronavirus. This hypothesis is rooted in the evolutionary perspective, which posits that certain OCD obsessions and compulsions could be exaggerated forms of once-advantageous behaviors from the unprecedented focus on cleanliness and infection control that has marked the global response to the pandemic (8, 21). The results of our study challenge the hypothesis by suggesting that OCD does not offer protection against COVID-19. This surprising outcome questions the preconceived notions of both patients and researchers regarding the protective role of OCD behaviors against infectious diseases.
After extracting our sample of patients, we initiated our study with a meticulous matching process. This was necessary because the pre-matched group of individuals with OCD was notably younger, predominantly male, and was more frequently represented at both the lower and higher ends of the socioeconomic spectrum. There was also a marginally higher occurrence of comorbidities within this group, necessitating a careful adjustment to ensure a robust and unbiased comparison in our subsequent analysis.
We observed that the frequency of COVID-19 testing was similar between the matched control group and the OCD group. Despite this similarity, the OCD group had a marginally higher rate of positive COVID-19 tests. This difference only became significant after the fifth and final wave. This finding is particularly striking given that the OCD group was more likely to receive the vaccine booster (third dose) compared to the control group. The additional vaccination suggests that individuals with OCD may engage in behavior that is more cautious when it comes to vaccination, though this did not translate into lower infection rates.
Several factors might contribute to this unexpected pattern, contradicting our initial hypothesis. First, the variable of reporting behavior warrants consideration. Patients with OCD were possibly more likely to remain concerned about COVID-19 infection and continued to adhere to regular COVID-19 testing protocols even after the relaxation of pandemic-related restrictions. In contrast, the general population might have perceived a diminished necessity for testing in the presence of symptoms, leading to reduced reporting to healthcare providers. Unfortunately, our study was unable to ascertain whether the testing frequency for the OCD group differed before and after the end of the fifth wave, rendering this aspect inconclusive. Second, the behavior of OCD patients regarding safety measures may have impacted these results. Those with more rigorous adherence to safety protocols may have neglected other preventive behaviors, such as social distancing, due to mental fatigue, particularly post-vaccination (22). A detailed analysis of the time from vaccination to potential infection could have potentially supported this explanation. Third, the prolonged stress induced by the pandemic could have negatively affected patients’ immune responses, compromising their ability to combat infections effectively (23). Lastly, the increased comorbidity of ADHD in the OCD group, known as a risk factor for contracting COVID-19, may have contributed to the overall pattern (15, 18).
According to our data, individuals with OCD or anxiety diagnoses who were infected with COVID-19 experienced infection a few days later compared to those in the control group. On average, they were able to delay infection by 8 ± 3.4 to 10 ± 3.5 days. This represents a minimal difference over the timespan of a few years. This small delay may reflect a higher initial adherence to diligent preventive measures. However, over time, such behaviors may have become less effective, due to either behavioral fatigue or the unavoidable nature of certain transmission sources, such as close contact with household members (e.g., children) (24).
4.1 Limitations
Several limitations of our study warrant attention and are crucial for interpreting our findings.
First, the nature of our large-scale data analysis raises concerns about data quality and completeness, especially with the common issue of missing or inaccurately recorded information in medical and psychiatric databases. This can be especially problematic in the context of OCD, where diagnostic criteria and reporting standards may vary significantly across different healthcare settings. Additionally, some individuals may either remain undiagnosed or choose to seek private healthcare treatment to avoid their conditions from being recorded in public healthcare records. Notably, the prevalence of OCD observed in our study was 0.4%, which is significantly lower than the 2-8 times higher estimates commonly cited in the literature, suggesting underdiagnosis. However, this underreporting implies that the differences we observed between OCD patients and the general population might actually be understated, as the inclusion of undiagnosed OCD individuals in the non-OCD group could dilute the observed differences between groups. Conversely, our analysis did not distinguish between OCD subtypes, such as those with contamination fears, versus other forms not related to cleanliness, nor could we assess the severity of the disorder. This lack of specificity means that some individuals classified within the OCD group might not exhibit significant behavioral differences from the general population. As these issues potentially weaken our conclusion and strengthen our initial hypothesis, further individual-level studies are necessary to refine these insights.
Second, while the numbers and results of COVID-19 tests taken publicly are nationally transmitted and considered accurate, they do not include the frequency of at-home COVID-19 tests. The reported rate of positive tests also depends on individuals reporting their infections to community clinics, which may not always happen.
Third, the COVID-19 pandemic was characterized by extensive guidance from the Ministry of Health on minimizing the risk of infection, which the general population mostly adopted. This widespread adherence may have lessened the relative advantage of any natural protective behaviors associated with OCD, which might have been more beneficial before such guidance was available and government restrictions were implemented. This context is essential for understanding the potential impact of OCD behaviors on the risk of COVID-19 infection.
Finally, the positive test figures we derived indicate whether an individual was infected at any point; they do not reflect the frequency of infections per person. It is important to note that some individuals contracted the virus multiple times within the period under review, suggesting that a disparity in reinfection rates between the OCD and non-OCD populations might still be present.
4.2 Conclusion
Our findings contradict the hypothesis that a diagnosis of OCD provides protection against COVID-19. On the contrary, we observed a higher incidence of COVID-19 diagnoses among individuals with OCD. This outcome, coupled with several limitations and potential confounders, highlights a critical consideration: the most common hygiene behaviors associated with contamination-focused OCD, such as hand-washing, are primarily effective against diseases spread through direct contact, feco-oral routes or via contaminated surfaces, rather than respiratory illnesses like COVID-19. Therefore, while OCD-related hygiene practices may still offer some defense against various disease outbreaks, particularly those spread through non-respiratory means and were apparently ineffective in the COVID-19 pandemic. This finding is important for dispelling the misconception that intensified OCD-related hygiene practices could provide immunity against diseases like COVID-19. Understanding this can help correct false beliefs among OCD patients, thereby aiding in the provision of more accurate psychoeducation and enhancing the effectiveness of cognitive-behavioral therapy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Institutional Review Board of Clalit Health Services. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
CA: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. DS: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. PT: Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
In the writing of this manuscript, the authors used OpenAI’s GPT-4o to enhance readability and clarity. The authors have reviewed the content and take full responsibility for the content of the publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive–compulsive disorder. Nat Rev Dis Prim. (2019) 5:1–21. doi: 10.1038/s41572-019-0102-3
2. Bhikram T, Abi-Jaoude E, Sandor P. OCD: Obsessive-compulsive … disgust? The role of disgust in obsessive-compulsive disorder. J Psychiatry Neurosci. (2017) 42:300–6. doi: 10.1503/jpn.160079
3. Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA. DSM-IV field trial: obsessive-compulsive disorder. Am J Psychiatry. (1995) 152:90–6. doi: 10.1176/ajp.152.1.90
4. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:53–63. doi: 10.1038/mp.2008.94
5. Poli A, Melli G, Radomsky AS. Different disgust domains specifically relate to mental and contact contamination fear in obsessive-compulsive disorder: evidence from a path analytic model in an italian clinical sample. Behav Ther. (2019) 50:380–94. doi: 10.1016/j.beth.2018.07.006
6. Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF. Meta-analysis of the symptom structure of obsessive-compulsive disorder. Am J Psychiatry. (2008) 165:1532–42. doi: 10.1176/appi.ajp.2008.08020320
7. Brune M. The Evolutionary Psychology of Obsessive-Compulsive Disorder: the role of cognitive metarepresentation. Perspect Biol Med. (2006) 49:317–29. doi: 10.1353/pbm.2006.0037
8. Feygin DL, Swain JE, Leckman JF. The normalcy of neurosis: Evolutionary origins of obsessive-compulsive disorder and related behaviors. Prog Neuropsychopharmacol Biol Psychiatry. (2006) 30:854–64. doi: 10.1016/j.pnpbp.2006.01.009
9. World Health Organization. Coronavirus disease (COVID-19): How is it transmitted? (2021). WHO website. Available online at: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (Accessed November 12, 2023).
10. Jelinek L, Voderholzer U, Moritz S, Carsten HP, Riesel A, Miegel F. When a nightmare comes true: Change in obsessive-compulsive disorder over the first months of the COVID-19 pandemic. J Anxiety Disord. (2021) 84:102493. doi: 10.1016/j.janxdis.2021.102493
11. D’Urso G, Magliacano A, Dell’Osso B, Lamberti H, Luciani A, Mariniello TS, et al. Effects of strict COVID-19 lockdown on patients with obsessive-compulsive disorder compared to a clinical and a nonclinical sample. Eur Psychiatry. (2023) 66:e45. doi: 10.1192/j.eurpsy.2023.2416
12. Carmi L, Ben-Arush O, Fostick L, Cohen H, Zohar J. Obsessive compulsive disorder during coronavirus disease 2019 (COVID-19): 2- and 6-month follow-ups in a clinical trial. Int J Neuropsychopharmacol. (2021) 24:703–9. doi: 10.1093/ijnp/pyab024
13. Fontenelle LF, Miguel EC. The impact of coronavirus (COVID-19) in the diagnosis and treatment of obsessive-compulsive disorder. Depress Anxiety. (2020) 37:510–1. doi: 10.1002/da.23037
14. Maye CE, Wojcik KD, Candelari AE, Goodman WK, Storch EA. Obsessive compulsive disorder during the COVID-19 pandemic: A brief review of course, psychological assessment and treatment considerations. J Obsessive Compuls Relat Disord. (2022) 33:100722. doi: 10.1016/j.jocrd.2022.100722
15. Merzon E, Manor I, Rotem A, Schneider T, Vinker S, Golan Cohen A, et al. ADHD as a risk factor for infection with covid-19. J Atten Disord. (2021) 25:1783–90. doi: 10.1177/1087054720943271
16. Karaoulanis SE, Christodoulou NG. Do patients with schizophrenia have higher infection and mortality rates due to COVID-19? A systematic review. Psychiatriki. (2021) 32:219–23. doi: 10.22365/jpsych.2021.027
17. Tzur Bitan D, Krieger I, Kridin K, Komantscher D, Scheinman Y, Weinstein O, et al. COVID-19 prevalence and mortality among schizophrenia patients: A large-scale retrospective cohort study. Schizophr Bull. (2021) 47:1211–7. doi: 10.1093/schbul/sbab012
18. Cohen HA, Gerstein M, Yaniv N, Richenberg Y, Jacobson E, Marton S, et al. Attention-deficit/hyperactivity disorder as a risk factor for COVID-19 infection. J Atten Disord. (2022) 26:985–90. doi: 10.1177/10870547211044217
19. Ministry of Health of Israel. Data world - COVID-19 (2024). Minist Heal Isr Website. Available online at: https://datadashboard.health.gov.il/portal/dashboard/corona (Accessed October 27, 2024).
20. Ministry of Foreign Affairs. Joint statement from PM naftali bennett and health minister nitzan horowitz (2022). gov.il. Available online at: https://www.gov.il/en/departments/general/joint-statement-from-pm-bennett-and-health-minister-horowitz-20-apr-2022 (Accessed October 27, 2024).
21. Rajkumar RP. Contamination and infection: What the coronavirus pandemic could reveal about the evolutionary origins of obsessive-compulsive disorder. Psychiatry Res. (2020) 289:113062. doi: 10.1016/j.psychres.2020.113062
22. World Health Organization. Pandemic fatigue – reinvigorating the public to prevent COVID-19: policy framework for supporting pandemic prevention and management. Copenhagen, Denmark: Regional Office for Europe (2020). Available at: https://iris.who.int/handle/10665/335820.
23. Schneiderman N, Ironson G, Siegel SD. Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol. (2005) 1:607–28. doi: 10.1146/annurev.clinpsy.1.102803.144141
Keywords: obsessive-compulsive disorder (OCD), COVID-19, infection rates, vaccination rates, psychoeducation
Citation: Avni C, Sinai D and Toren P (2024) Between compulsions and contagions: examining the protective role of OCD against COVID-19 in a large cohort study. Front. Psychiatry 15:1464353. doi: 10.3389/fpsyt.2024.1464353
Received: 13 July 2024; Accepted: 28 October 2024;
Published: 25 November 2024.
Edited by:
Pedro Morgado, University of Minho, PortugalReviewed by:
Doron Gothelf, Sheba Medical Center, IsraelMarc Peraire, Consorcio Hospitalario Provincial de Castellón, Spain
Anand Prakash, Xavier University School of Medicine, Netherlands
Copyright © 2024 Avni, Sinai and Toren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chen Avni, Y2hlbi5hdm5pQGNsYWxpdC5vcmcuaWw=
 Chen Avni
Chen Avni Dana Sinai1,3
Dana Sinai1,3 Paz Toren
Paz Toren