- 1Department of Public Health, Health Commission of Rongchang District, Chongqing, China
- 2Center for Mental Health of Rongchang District, Chongqing, China
- 3Department of Public Health, The People’s Hospital of Rongchang District, Chongqing, China
- 4First Clinical College, Mudanjiang Medical College, Mudanjiang, Heilongjiang, China
- 5Department of Hospital Information, The People’s Hospital of Rongchang District, Chongqing, China
Background: Although the negative impact of smoking and health-related quality of life (HRQoL) on depression has been confirmed in various studies, There has been little exploration of how HRQoL mediates the relationship between smoking and depression. The purpose of the current study was to examine the relationship between smoking and depression in the Chinese current smokers with nicotine dependence and the mediating role of HRQoL.
Methods: A cross-sectional study named “Psychology and Behavior Investigation of Chinese Residents” was conducted from July 10 to September 15, 2021 in China. Nicotine dependence, HRQoL and depression were measured by Fagerstrom Test for Nicotine Dependence (FTND), the European Five Dimensional Five Level Health scale (EQ-5D-5L) and the 9-item Patient Health Questionnaire (PHQ-9) respectively. Information on age, gender, place of residence, household registration, education level, marital status, employment status, average family monthly income, drinking frequency, living status, BMI, multiple chronic conditions were also collected. Pearson’s correlation test and logistic regression analysis were conducted to explore the association between nicotine dependence, HRQoL and depression and a mediation analysis was applied to explore the mediating effect of the HRQoL on this relationship.
Results: A total of 1,381 current smokers were included in the study. The participants showed a moderate level of nicotine dependence with a mean of 1.36(SD=1.50), a relatively high level of HRQoL scores (Mean=0.94, SD=0.13), and a depression score with a mean of 6.48(SD=6.09). Approximately 22.74% (314/1,381) of the participants were considered to indicate depression. In the univariable regression model, it was found that nicotine dependence was positively associated with depression (OR:1.094, 95%CI: 1.008-1.187), while HRQoL was negatively associated with depression (OR:0.011, 95%CI: 0.004-0.033). In the multivariable regression model, HRQoL was still notably associated with depression (OR:0.008, 95%CI: 0.002-0.027), however, the positive association was not observed between nicotine dependence and depression. The Pearson’s correlation test demonstrated that nicotine dependence was negatively correlated with HRQoL(rs= -0.147, P<0.001) and HRQoL was negatively correlated with depression(rs= -0.275, P<0.001). In contrast, nicotine dependence was positively correlated with depression(rs= 0.136, P<0.001). Mediation analysis found that HRQoL moderated the relationship between nicotine dependence and depression with a mediating effect of 26.49%.
Conclusions: The findings support that nicotine dependence is positively associated with depression and HRQoL is negatively associated with depression in current smokers. HRQoL mediated the relationship between nicotine dependence and depression. The well-established imperative interventions aimed at promoting smoking cessation and improving quality of life may benefit for alleviation of depression in current smokers.
Introduction
Depression is the most common mental disorder, with a lifetime prevalence rate of about 11-15% (1). Previous studies have demonstrated that age (2), gender and living alone (3), chronic diseases (2), cigarette smoking (4), impaired essential ability of daily living (5) were associated with depression. However, in some areas of China, the stigma of depression prevents patients from receiving diagnosis or treatment (6).
Previous literature suggests a bidirectional relationship between smoking and depression. Some studies have demonstrated that smoking was associated with a higher risk of depression compared with never smoker (7–10), while individuals with depressive symptoms are more likely to engage in smoking behavior (11). This bidirectional and complex relationship forces us to ponder whether nicotine dependence is more linked to depression than smoking behavior. Tobacco/nicotine dependence is classified as a mental and behavioral disorder (12). It is estimated that there are 54 million people aged 40 years and older with severe tobacco dependence in China (13). A Egyptian study found a high correlation between nicotine dependence and depression (14) and studies have emphasized that smoking/nicotine dependence is not only correlated with depression but also leads to respiratory symptoms (15), fatigue, frailty and cognitive decline, ultimately worsening an individual’s health-related quality of life (HRQoL) (16).
The relationship between depression and HRQoL has been observed in older population (17, 18) and individuals with diabetes (19), malnutrition (18), systemic lupus erythematosus (20), adult epilepsy (21). However, individuals with medical conditions, such as friedreich ataxia (22), were found to have their health-related quality of life impacted by the development of depressive symptoms. Similarly, patients with Wilson’s disease (23) exhibited a higher risk of depression. Therefore, evidence in seeking for the association between HRQoL and depression is essential in general population.
Further research under these mechanisms provides new insights into how the independent variable affects the dependent variable. In the current study, we hypothesized that HRQoL mediates the association between nicotine dependence and depression for the following reasons. First, The association between smoking and depression remains controversial because some studies found no link between smoking and depression (24). Second, a previous study found that non-smokers and former smokers have higher HRQoL scores than the current smokers (25). In addition, nicotine dependence was found to be negatively associated with lower HRQoL scores (26), and a poor HRQoL score was negatively associated with depression (27). Few studies have elaborated on HRQoL mediating the relationship between smoking and depression in low and middle income countries, especially in China, which is the world’s largest producer and consumer of tobacco, accounting for one-third of the worlds smoking population (28). Accordingly, it is of great significance to clarify whether HRQoL serves as a mediating role influencing the relationship between nicotine dependence and depression.
Existing studies have revealed the association between nicotine dependence, health-related quality of life, and depression in general populations, while scant attention has been given to the interactions among them in the specific population. It is essential to determine the relationship between nicotine dependence and depression with a large sample size and whether HRQoL may explain this association. Therefore, the aim of current study was to elucidate twofold (1): to explore the relationship between nicotine dependence, HRQoL and depression based on data from community-dwelling smoking adults in China; and (2) to explore whether HRQoL mediates the relationship between nicotine dependence and depression.
Methods
Study design and participants
All data were obtained from the “Psychology and Behavior Investigation of Chinese Residents (RBICR) 2021” in China, which was a large-sample, multi-center, replicated cross-sectional study co-sponsored by Peking University. From July 10 to Sep 15, 2021, a multistage random sampling method was conducted in the current study. Firstly, 31 provincial capitals cities including 5 autonomous regions and 4 municipalitie (including Beijng, Tianjin, Shanghai and Chongqing) were directly included. Secondly, 2-6 prefecture-level cities were selected by using a random number table and at last, a total of 120 cities (excluding Hong Kong, Macao, and Taiwan) were included. In order to achieve a representative population distribution, participants of each city were selected using quota sampling (quota attributes such as gender, age, and urban-rural distribution). Consequently, the population distribution of the obtained samples (per 100 people) basically matching the demographic characteristics of the results of the “Seventh National Census in 2021”. This study had been approved by the Medical Ethics Committee of Health Commission of Rongchang District, Chongqing (No. Rcwjw2024018). More details about the study design can be found in the published literature (2, 29–31).
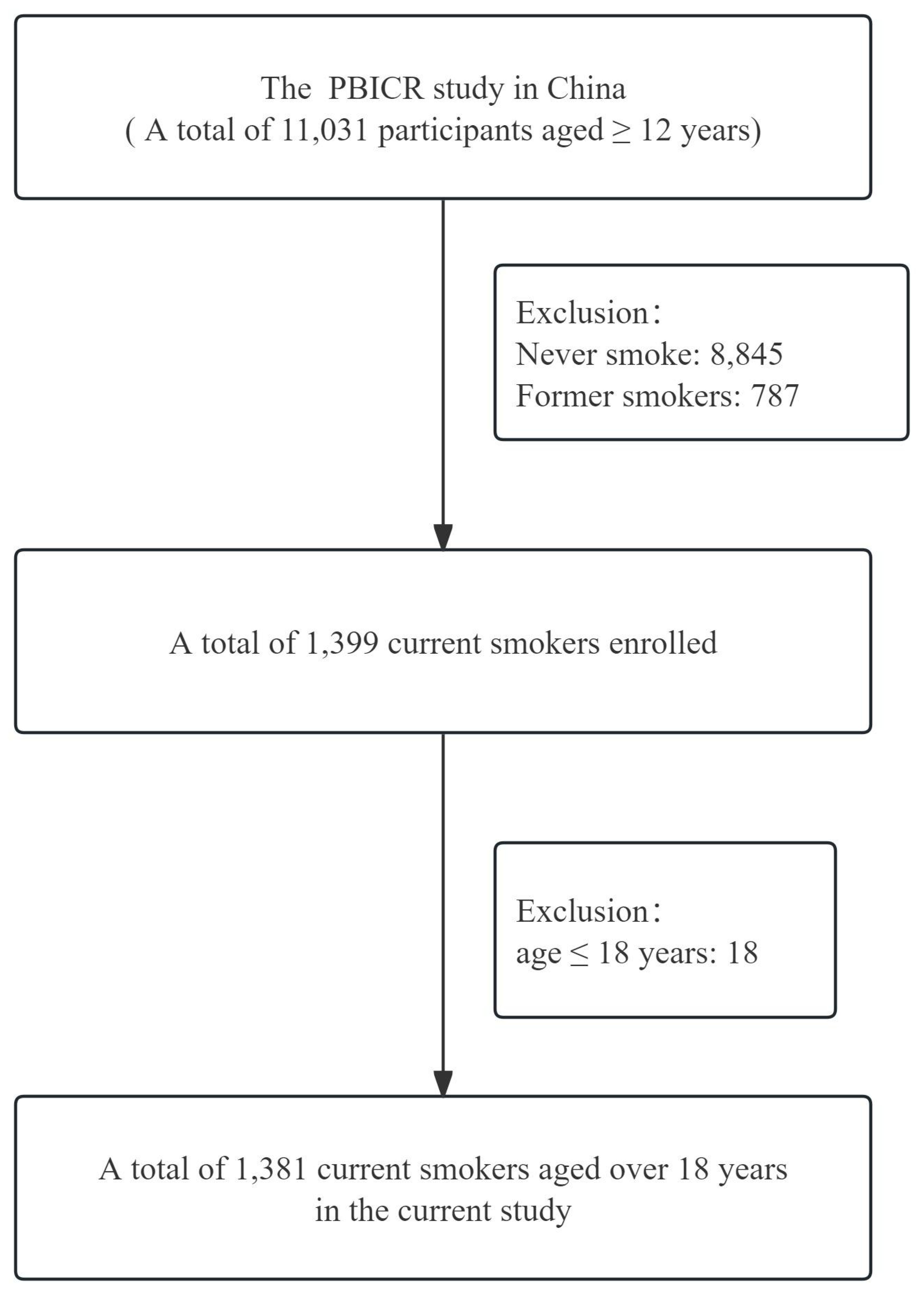
In the current study, only 1,381 cases were included in the analysis, the inclusion and exclusion criteria of the study participants were as follows.
Inclusion criteria: (1) age >18 years; (2) current smokers; (3) participants who voluntarily participate in the current study and complete the informed consent form; (4) participants who complete the questionnaire by themselves or with the help of the investigator;(5) participants who can understand the meaning of each item in the questionnaire.
Exclusion criteria: (1) participants with limited mobility, delirium or mental abnormality; (2) participants who were in other similar research projects; (3) participants unwilling to cooperate with the instructions of the study group. As shown in Figure 1, the selection process for study participants was conducted.
Data collection
With the assistance “Questionnaire Star (https://www.wjx.cn/)”, which was widely used for online questionnaire survey of data collection procedure in China, the survey was conducted from July 10th to Sep 15th, 2021. Investigators or investigation team (less than 10 people) were recruited from local universities. The survey personnel were well trained in sampling methods, research tools and quality control of the study. Prior to the start of the formal survey, a simulated survey was organized to guarantee the quality of investigations; surveyors were considered qualified and competent to participate in the study only if they complied with trained survey procedures (90%). The investigators administered the questionnaire to the participants one by one and face to face. Before the data collection process, participants were asked to click on a link to indicate their informed consent and confirm they understood the survey’s purpose. Participants were assigned a questionnaire number to ensure the uniqueness of the electronic questionnaire. If the participants were capable of thinking but unable to complete the questionnaire on his/her own, the investigator filled out the questionnaire based on the questions he/she answered. A total of 11,709 questionnaires were distributed, and 11,031 valid questionnaires were returned, resulting in 94.2% response rate.
Measures
Nicotine dependence
Two items in the Fagerstrom Test for Nicotine Dependence (FTND) were used to elevate the current smoker’s nicotine dependence level. The first item assessed “How soon after waking up in the morning the participant smoked their first cigarette?” with response options of “>60 min” or “31-60 min” or “6-30 min” or “≤5 min”. The second item asked “How many cigarettes the participant smoked each day?” with response options of “≤10 cigarettes/day” or “11-20 cigarettes/day” or “21-30 cigarettes/day” or “≥31 cigarettes/day”. The scale has good reliability and validity (32, 33). Each response was scored from 0 to 3 depending on the degree of severity (0 =>60 min, 1 = 31-60 min, 2 = 6-30 min, 3=≤5 min;0=≤10 cigarettes/day, 1 = 11-20 cigarettes/day, 2 = 21-30 cigarettes/day, 3=≥31 cigarettes/day). The total score of the two items was 6 points. A higher scores indicates greater nicotine dependence of participants, and a score of ≥4 indicated that severe nicotine dependence might exist (34) and score of 0-1 was defined as light nicotine dependence and score of 2-3 was defined as moderate nicotine dependence.
Health-related quality of life
HRQoL was measured with the European Five-Dimensional Five-level Health Scale (EQ-5D-5L) instruments (35), which allows for better differentiation of respondents’ health status and objectify the subjective experience (36). It is commonly used for estimating HRQoL. HRQoL refers to a multi-dimensional indicator for estimating physical state, mental function, social competence, and overall personal condition (37), which could reflect the impact of diseases, physical or mental impairment on an individual’s overall quality of health. The EQ-5D-5L instrument consists of 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension consists of 5 levels: no difficulty, slight difficulty, moderate difficulty, severe difficulty, and unable to complete/extreme difficulty. The five response levels (1, 2, 3, 4, 5) correspond to each dimension in the given order. Firstly, a five level health scale was obtained (like:11111, means no difficulty in mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), the EQ-5D-5L can represent a total of 3,125 (55) different health states (38). Secondly, a single EQ-5D-5L value was obtained from a utility value integral system developed by Luo (39), which ranges from -0.391 to 1. 0 indicates death and 1 indicates the “perfect health” of HRQoL of an individual (40). EQ-5D-5L value less than 0 represents a health state considered worse than death (37, 41). Chinese scholars have validated the Chinese version of the EQ-5D-5L, which has demonstrated good reliability and validity. The matching process of obtaining EQ-5D-5L value can be found in the additional file (Supplementary Tables 1, 2)
Depression
The 9-item Patient Health Questionnaire (PHQ-9) was used to measure the depressive symptomatology in the study participants. For example, participants were asked the question, “How often do you feel bored with everything or not want to do anything at all” and the respondent selects 1 answer out of 4 alternative items, including “Never (scored as 0), A couple days (scored as 1), more than half the days (scored as 2), close to every day (scored as 3)”, each item is scored from 0 to 3 as a response mechanism to measure the depressive symptomatology in the past two weeks. The total score ranges from 0 to 27, with higher scores indicating greater symptoms of depression (17). The cut off score over or equal to 10 is considered to indicate depression in accordance with previous study (2). The Chinese version of PHQ-9 has been well-validated in China (2, 41, 42) and has demonstrated good internal consistency. Additionally, due to its high sensitivity, simplicity, and ease of operation of PHQ-9 itself, most participants can complete the questionnaire within 5 min even without any assistance.
Covariates
Associated factors contributing to depression included in the current study were identified through a literature review about the RBICR study in China (2, 43, 44). Age was grouped into “19-30 years”, “31-40 years”, “41-50 years”, “51-59 years”, “≥60 years “; place of residence was grouped into “urban” and “rural”; household registration was grouped into “non-agriculture” and “agriculture”; education level was grouped into “primary school or below”, “junior middle school”, “high school”, “2/3 year college degree”, “undergraduate” and “postgraduate/doctor”; marital status was grouped into “unmarried”, “married”, “divorced” and “widowed”; employment status was grouped into “students”, “on a job”, “retired” and “else”; average family monthly income was grouped into “≤3000 yuan”, “3001-6000 yuan”, “6001-9000 yuan” and “≥9001yuan”; drinking frequency was grouped into “never”, “less than 1 d/month”, “1-3 d/month”, “1-2 d/week”, “3-4 d/week”, “4-5 d/week” and “everyday”. BMI was calculated by the formulas BMI= Weight(/Kg)/Height(/m)2 and grouped into “<24Kg/m2”, “24-27.99Kg/m2” and “≥28Kg/m2” (45). A total of 16 kind of diseases were investigated (30), including hypertension, stroke, coronary heart disease, dyslipidemia, Diabetes mellitus, malignant neoplasm, asthma, chronic obstructive pulmonary disease, chronic kidney disease, chronic enteritis, chronic gastritis, viral hepatitis, fatty liver disease, Alzheimer’s disease, Parkinson’s disease, mood disorders and the total number of chronic diseases were renamed multiple chronic conditions, which were grouped into “0”, “1”, “2”, and “≥3”.
Statistical analyses
SPSS 25.0 (SPSS, Chicago, IL, USA) was conducted for the data analysis. Numerical variables were expressed as mean ± standard deviation and the difference between two groups was conducted by independent sample t-test. Categorical variables were expressed as frequencies and percentage and frequency distributions were evaluated by chi-square (χ2) test between two groups. The associated factors (including age, gender, place of residence, household register, education level, marital status, employment status, average family monthly income, nicotine dependence, drinking frequency, living alone, BMI, multiple chronic conditions, HRQoL) contributing to depression were evaluated using logistic regression analysis, OR (odds ratio) and 95%CI (confidence interval) were calculated to demonstrate the association. Pearson’s correlation test was conducted to examine the correlation among nicotine dependence, HRQoL and depression. The reliability and validity of the measurements for HRQoL and depression were assessed using Cronbach’s α. Based on the previous studies, nicotine dependence was demonstrated to have a direct effect on HRQoL (path a), and HRQoL was demonstrated to have a direct effect on depression (path b). Thus, nicotine dependence can indirectly affect depression by the mediating effects of HRQoL, which is presented as path c’. The detailed framework of mediation analysis is presented in Figure 2. The mediating effect of HRQoL on the relationship between nicotine dependence and depression was assessed using Macro PROCESS 3.1 in SPSS. A bias-corrected bootstrap confidence interval was generated with model 4 after adjusting for confounding factors (using a bootstrap sample of 5,000). Considering the bidirectional relationship between smoking and depression, we also analyzed depression leading to nicotine dependence with HRQoL mediating the relationship, see Supplementary Table 3. It is considered statistically significant when the p-value falls below 0.05.
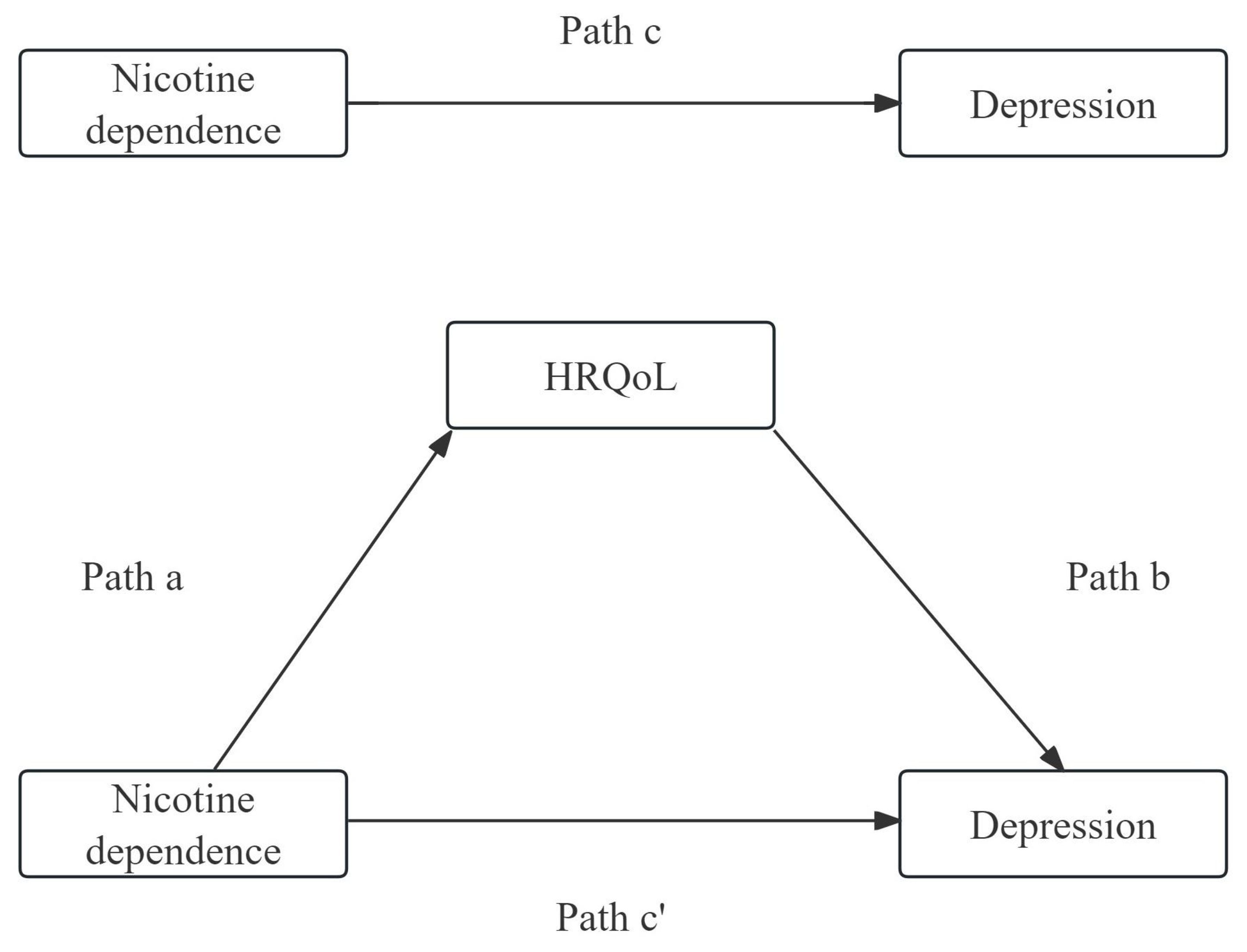
Figure 2. The detailed framework of mediation analysis of HRQoL on the relationship between nicotine dependence and depression.
Results
Demographic characteristics of the participants
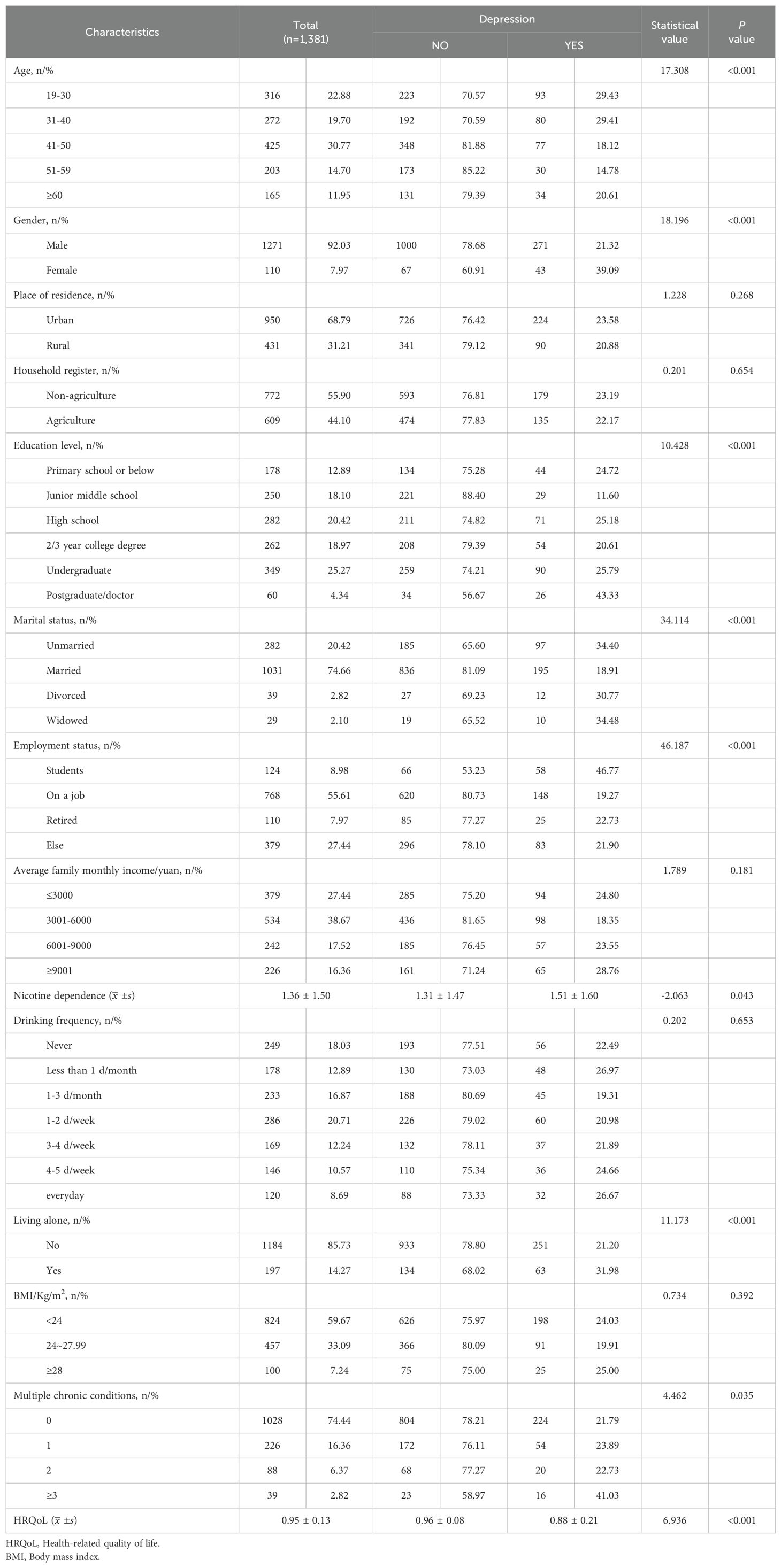
The demographic characteristics of the participants are summarized in Table 1. A total of 1,381 current smokers were included in the current study. Among these participants, approximately 11.95% were over 60 years old, 92.03% of the participants were males. 68.79% of the participants were resided in urban areas. 55.90% of the participants had a non-agricultural household registration, In terms of education, 25.27% of the participants had an undergraduate level of education. 74.66% of the participants were married. 55.61% of the participants were on a job. 38.67% of the participants had an average income of ¥3001-6000 yuan. Additionally, 18.03% of the participants reported never drank alcohol. 14.27% of the participants were living alone. 33.09% of the participants were in the status of overweight (24~27.99Kg/m2) and 7.24% of the participants were in the status of obesity (≥28Kg/m2). 74.44% of the participants did not suffer from chronic diseases.
The association between different characteristics and depression using χ2/t test
The association between basic characteristics and depression is presented in Table 1. The total prevalence of depression was 22.74% (314/1,381). The prevalence of depression was found to be statistically significant in different age, gender, education level, marital status, employment status, nicotine dependence scores, whether living alone, multiple chronic conditions and HRQoL scores.
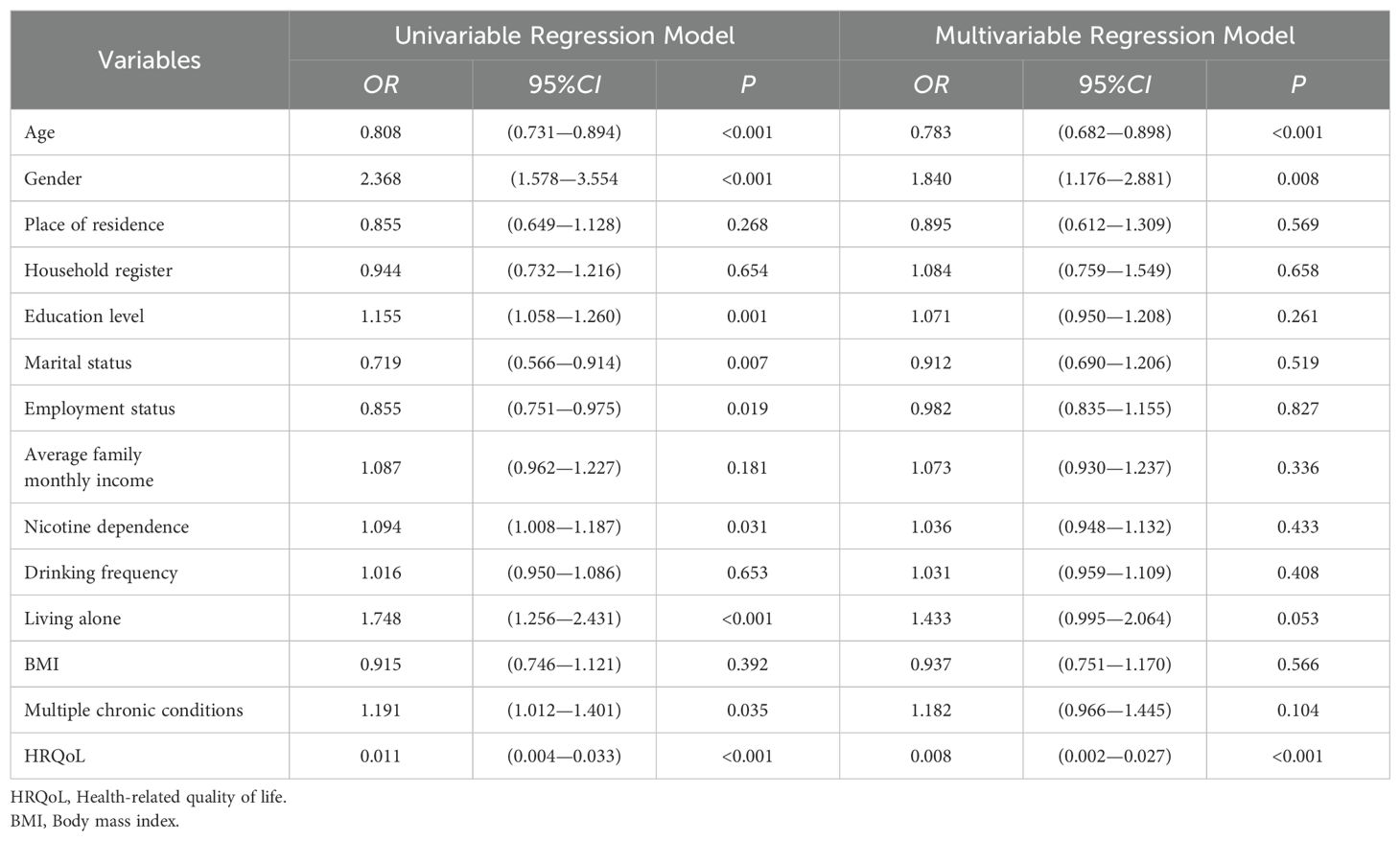
The association between different characteristics and depression using logit model
Subsequently, the Logit model was conducted to analyze the association between different characteristics and depression, the results are presented in Table 2. In the univariable regression model, nicotine dependence was positively associated with depression(OR:1.094, 95%CI: 1.008—1.187), while HRQoL was negatively associated with depression(OR:0.011, 95%CI: 0.004—0.033). In the multivariable regression model, HRQoL remained notably associated with depression(OR:0.008, 95%CI: 0.002—0.027). However, the positive association between nicotine dependence and depression was not observed.
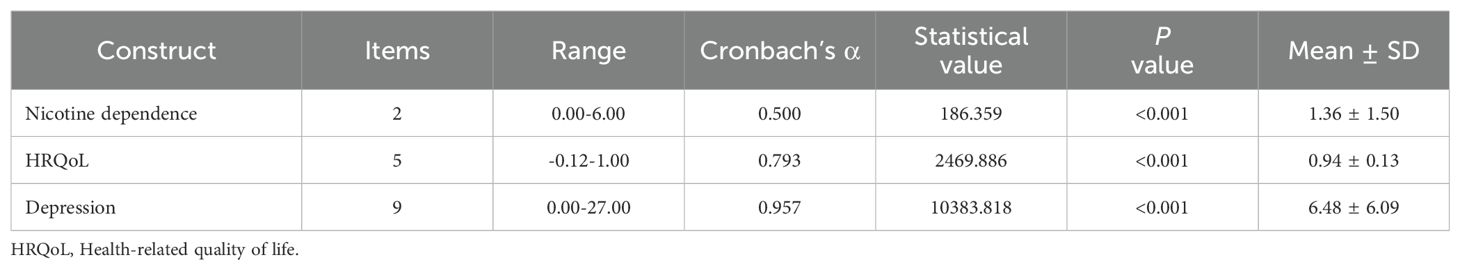
Descriptive results of nicotine dependence, HRQoL, and depression scores
The descriptive results of nicotine dependence, HRQoL, and depression scores are presented in Table 3. The 1,381 participants showed a moderate level of nicotine dependence with a mean of 1.36(SD=1.50, range: 0-6). Approximately 9.49% (131/1,381) of the participants were classified as having heavy nicotine dependence. The participants had a relatively high level of HRQoL scores, with a mean score of 0.94 (SD=0.13, Range:-0.12-1.00). Approximately 64.73% (894/1,381) of the participants were reported being in “perfect health”. The participants’ depression score ranged from 0 to 27, with a mean of 6.48(SD=6.09). Approximately 22.74% (314/1,381) of the participants’ scores were ≥ 10, which was considered to indicate depression.
The correlation among nicotine dependence, HRQoL, and depression scores using Pearson’s correlation test
The correlation among nicotine dependence, HRQoL, and depression scores using Pearson’s correlation test is presented in Table 4. Nicotine dependence was negatively correlated with HRQoL (rs= -0.147, P<0.001), indicating that higher nicotine dependence was associated with lower HRQoL. HRQoL was negatively correlated with depression (rs= -0.275, P<0.001), indicating that lower HRQoL was associated with higher levels of depression. In contrast, nicotine dependence was positively correlated with depression (rs= 0.136, P<0.001), suggesting that higher nicotine dependence was associated with higher levels of depression.
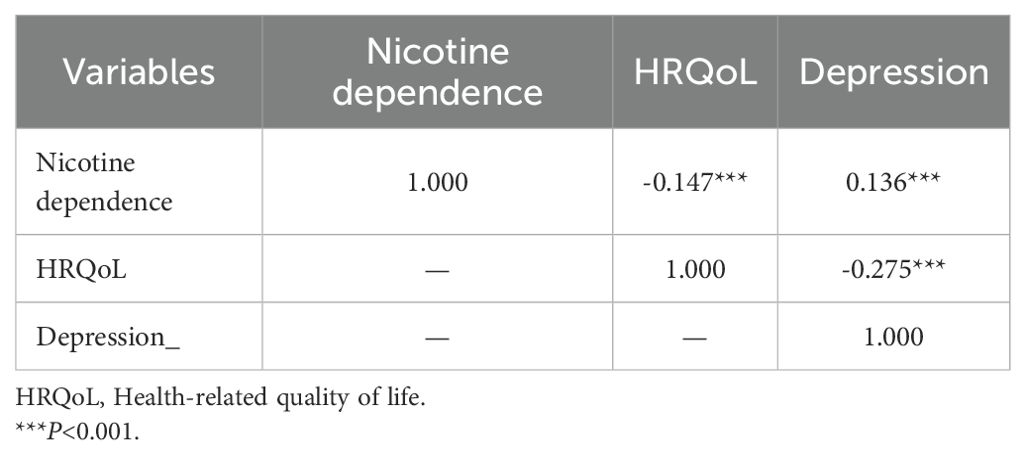
Table 4. The correlation among nicotine dependence, HRQoL, and depression scores using Pearson’s correlation test.
Mediation analysis of HRQoL on the relationship between nicotine dependence and depression
The total effect, direct effect, indirect effect, and the different pathways among nicotine dependence, HRQoL and depression are presented in Table 5. Nicotine dependence was negatively correlated with HRQoL while positively correlated with depression. There was a negative correlation between HRQoL and depression and a mediating effect between nicotine dependence and depression mediated by HRQoL, with the proportion of the mediating effect being 26.49%. The mediated effect analysis is shown in Figure 3.
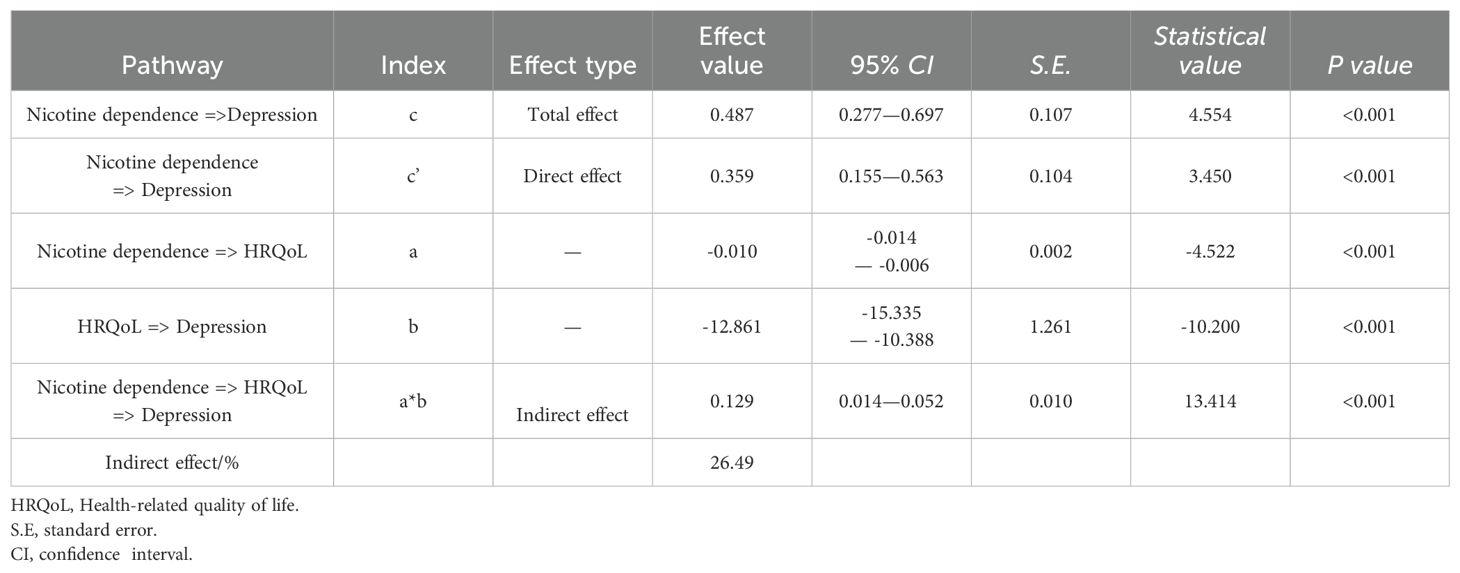
Table 5. The total effect, direct effect, indirect effect and the different pathways among nicotine dependence, HRQoL and depression.
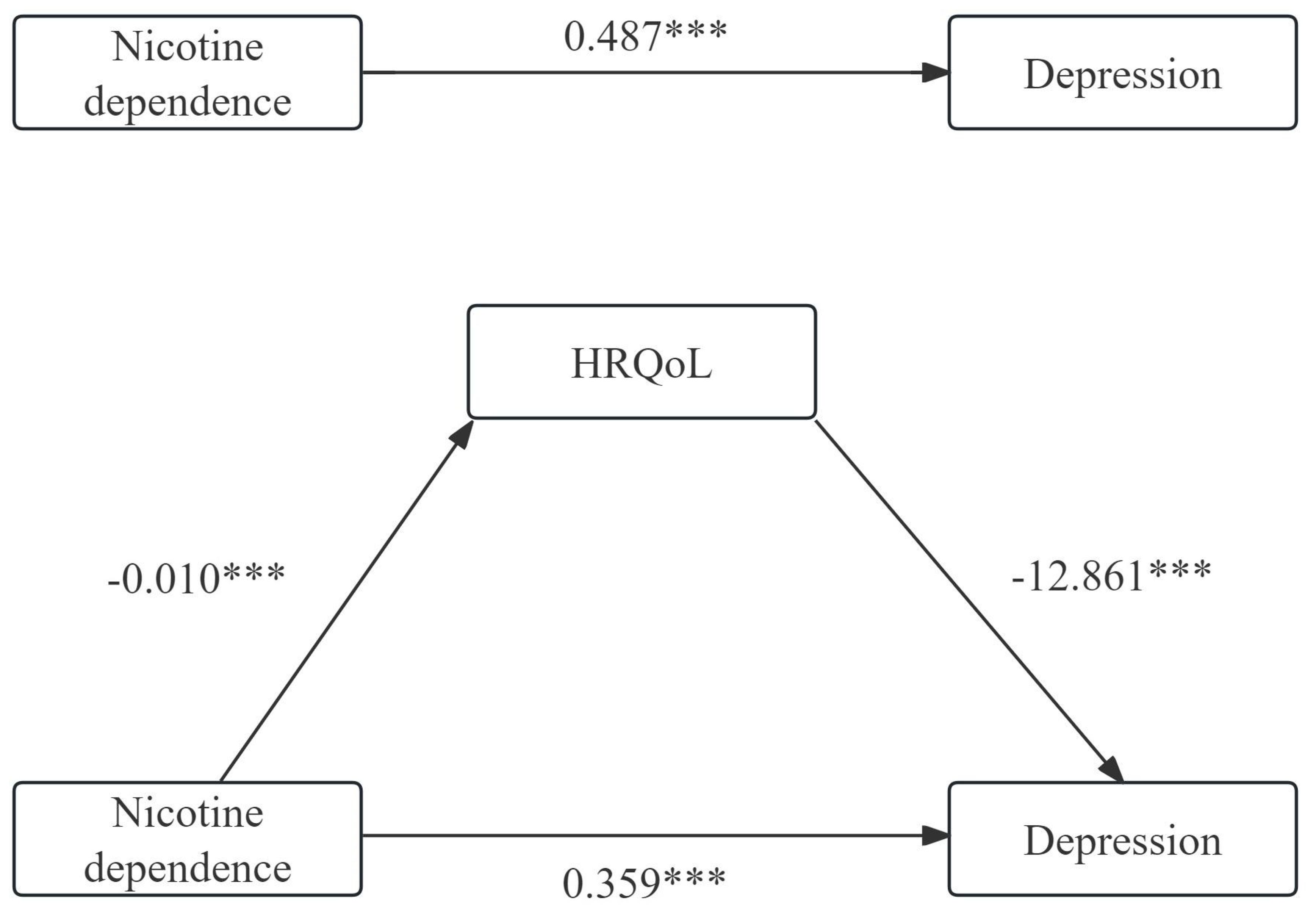
Figure 3. The mediating analysis of HRQoL on the relationship between nicotine dependence and depression. ***P<0.001.
Discussion
To our knowledge, this is the first study focusing on HRQoL involved in the relationship between nicotine dependence and depression in the general Chinese current smokers. We found that HRQoL mediated 26.49% of the association between nicotine dependence and depression in current smokers.
In the analysis, we observed that smokers with depression had higher scores of nicotine dependence and there was a positive association between nicotine dependence and depression (rs=0.136, P<0.001). Despite those findings, there was no significant association between nicotine dependence and depression (OR=1.036, 95%CI:0.948 to 1.132) in multivariable regression model. There are several reasons that could help explain this discrepancy. First, in the current study, only 9.49% of smokers in our study exhibited heavy nicotine dependence. This relatively low prevalence of heavy nicotine dependence in our sample may have limited the statistical power to detect a significant association. Second, the nicotine dependence level between participants with and without depression were relatively close, with most participants scoring below 2. This narrow range of nicotine dependence scores and lower Cronbach’s α used to evaluate the nicotine dependence level may have weakened the impact of nicotine dependence on depression, making the significant association cannot be clearly concluded from multivariable regression analysis.
Published manuscripts have suggested that smoking may be associated with an increased risk of developing depression (7, 8). A systematic review of 148 studies on the association of cigarette smoking with depression and anxiety found that smoking at baseline is associated with an increased risk of depression in later life (46). During a 6.7 years follow-up, a Korean longitudinal study found a dose dependent relationship between smoking and the risk of depression (8). It was found that 21.0% of smokers were identified as suffering from possible anxiety or depression (47). Nicotine may enhance the intensity and duration of positive emotions and self-perceived energy (48), and may also reduce depressive symptoms by aiding in mood regulation (49).
There is a complicated and reciprocal relationship between smoking and depression. In 1998, Escobedo et al. found that depressive symptom or depression predicted the initiation of smoking (50). The prevalence of smoking is higher in depressed patients than in non-depressed patients, but the success rate of smoking cessation is lower than in non-depressed patients (51). Smoking behavior can predict the risk of depression, and depression also can predict the onset of smoking behavior. Additionally, there was an interaction effect between depressive symptoms and total daily cigarettes consumption in heavy smokers (1). According to study of Wootton et al., smoking was a risk factor for depression and Pasco (10) et al. reported that tobacco smoking doubled the risk of developing major depression in females followed up for 10 years (52).
Nicotine dependence has been found to increase the risk of depression. Nicotine dependent smokers exhibit more severe symptoms of depression and/or anxiety compared to smokers without nicotine dependence, former smokers, and never smokers (53). Sung et al. demonstrated that smoking amount was associated with the risk of depressive symptoms (8). Prolonged smoking can lead to nicotine dependence, which is associated with several common neurobiological mechanisms underlying depression (54). Previous studies have found that depressed mood was positively correlated with tobacco dependence, the higher of tobacco dependence, the more severe of depressive mood (55, 56). Smoking can provide temporary relief from depression by stimulating the nervous system (57). While prolonged smoking can lead to nicotine dependence, which increases susceptibility to develop depression (49).
The mechanisms behind nicotine dependence affected depression are likely to be complex, involving biogenetic, psychological factors. As a result of nicotine activating the nicotinic acetylcholine receptors (nACHRs), increases the release of neurotransmitters, such as dopamine, 5-hydroxytryptophan, and γ-aminobutyric acid, this leads to a sense of excitement and pleasure, reducing anxiety and tension (12, 51). Nicotine dependence was mediated by dopaminergic reward pathways and dopamine dysfunction could drive depression (58). For another angle, smokers rely on smoking to cope with negative emotions. On the other hand, when they quit, they may experience withdrawal symptoms, including negative emotions, which can lead to a relapse in smoking. To alleviate these negative emotions, individuals who have quit smoking may resume smoking behavior. Therefore, addressing negative emotions in smokers is more conducive to successful smoking cessation.
Previous studies have demonstrated that smoking was negatively correlated with lower HRQoL (59–61). In the current study, nicotine dependence was negatively associated with poor HRQoL. Smokers with light nicotine dependence had a higher score of HRQoL than those with moderate and heavy nicotine dependence smokers. This may be that nicotine dependent smokers experience barriers to mental health, which affect their subjective assessment of HRQoL. Thus, the current study highlights the differences among smokers with varying levels of nicotine dependence and calls for exploration of the association between nicotine dependence and HRQoL. This is important for raising social awareness about the health concerns of smokers and improving HRQoL among those smokers with nicotine dependence.
The present study conducted a bootstrap mediation analysis to partially verify the hypothesis that HRQoL affected as an indirect factor in the correlation between nicotine dependence and HRQoL. The results demonstrated that HRQoL mediated 26.49% of the association between nicotine dependence and depression in current smokers, indicating that HRQoL played a mediating role. However, longitudinal studies are required to confirm this mediating relationship.
Our study provides deeper and additional insight into the association between smoking and depression from a mediation perspective mediated by HRQoL. From a practice perspective, we recommend that professionals, such as public health agencies, policymakers, and community members, pay more attention to smokers with nicotine dependence in order to inform the smokers of the effects of smoking on depression mediated by HRQoL. When starting treatment for depression in smokers, attention should be considered to increase the smoker’s physical state, mental function, social competence, and overall personal condition. The current study has the following limitations. First, the causal relationship between nicotine dependence, HRQoL and depression could not be determined with a cross-sectional study. Second, nicotine dependence, HRQoL and depression were measured by self-reported measures from the study participants, which might be underestimated or overestimated by recall or social expectation bias. Third, we only considered depression; other negative emotions, including, anxiety, anger, panic and etc. were not included in the current study. Future research should consider these negative emotions. Fourth, the measure of PHQ-9 in depression and EQ-5D-5L in HRQoL are partly overlapped in depressive symptoms. Whether this overlap will affect the conclusions is unknown, so we recommend that future researchers should realize this overlap between HRQoL and depression measure. Finally, the relationship among nicotine dependence, HRQoL and depression are complicated and reciprocal, and we have only explored their relationship from the perspective of mediation analysis in 1,381 participants. Considering that China’s huge nicotine dependence population, which is also a limitation for the results to extrapolate, cohort studies with large samples are needed to support our conclusions.
Conclusions
The current study demonstrates that nicotine dependence is negatively correlated with HRQoL while positively correlated with depression and HRQoL is negatively associated with depression in current smokers. HRQoL mediated the relationship between nicotine dependence and depression. Based on the results of our study, these findings can help develop interventions to improve quality of life in current smokers to alleviate depression.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The current study had been approved by the Medical Ethics Committee of Health Commission of Rongchang District, Chongqing (No. Rcwjw2024018) and study of the RBICR2021 had been approved by the Ethics Committee of Jinan University, China (JNUKY-2021-018). The study was conducted in accordance with the Declaration of Helsinki of the World Medical Association. All the participants signed written informed consent before participating in the study.
Author contributions
HX: Writing – review & editing, Writing – original draft, Validation, Software, Resources, Formal analysis, Data curation. FM: Writing – review & editing, Writing – original draft, Validation, Data curation. DT: Writing – review & editing, Resources, Formal analysis, Data curation. DL: Writing – review & editing, Software, Investigation, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We appreciate all the staff involved in the “Psychology and Behavior Investigation of Chinese Residents (RBICR) 2021” study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1455918/full#supplementary-material
References
1. Han JW, Lee H. The longitudinal relationships between depression and smoking in hardcore smokers using autoregressive cross-lagged modeling. J Korean Acad Nurs. (2019) . 49:69–79. doi: 10.4040/jkan.2019.49.1.69
2. Kong X, Wu Y, Wang X, Sun Y, Chen K, Li Q, et al. Analysis of the prevalence and influencing factors of anxiety and depression in the Chinese population: A cross-sectional survey. Heliyon. (2023) . 9:e15889. doi: 10.1016/j.heliyon.2023.e15889
3. Lin H, Jin M, Liu Q, Du Y, Fu J, Sun C, et al. Gender-specific prevalence and influencing factors of depression in elderly in rural China: A cross-sectional study. J Affect Disord. (2021) . 288:99–106. doi: 10.1016/j.jad.2021.03.078
4. Tomita A, Manuel JI. Evidence on the association between cigarette smoking and incident depression from the South African national income dynamics study 2008-2015: mental health implications for a resource-limited setting. Nicotine Tob Res. (2020) . 22:118–23. doi: 10.1093/ntr/nty163
5. Wang D, Qi SG, Wang BH, Hu QT, Wang ZK, Wang Z. Depression status and its influencing factors among the elderly aged 60 years and above in three provinces of China. Zhonghua Liu Xing Bing Xue Za Zhi. (2022) . 43:1925–31. doi: 10.3760/cma.j.cn112338-20220418-00313
6. Jiang CH, Zhu F, Qin TT. Relationships between chronic diseases and depression among middle-aged and elderly people in China: A prospective study from CHARLS. Curr Med Sci. (2020) . 40:858–70. doi: 10.1007/s11596-020-2270-5
7. Wu Z, Yue Q, Zhao Z, Wen J, Tang L, Zhong Z, et al. A cross-sectional study of smoking and depression among US adults: NHANES (2005-2018). Front Public Health. (2023) . 11:1081706. doi: 10.3389/fpubh.2023.1081706
8. Park SK, Oh CM, Kim E, Ryoo JH, Jung JY. The longitudinal analysis for the association between smoking and the risk of depressive symptoms. BMC Psychiatry. (2024) . 24:364. doi: 10.1186/s12888-024-05828-7
9. Du X, Wu R, Kang L, Zhao L, Li C. Tobacco smoking and depressive symptoms in Chinese middle-aged and older adults: Handling missing values in panel data with multiple imputation. Front Public Health. (2022) . 10:913636. doi: 10.3389/fpubh.2022.913636
10. Wootton RE, Richmond RC, Stuijfzand BG, Lawn RB, Sallis HM, Taylor GMJ, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychol Med. (2020) . 50:2435–43. doi: 10.1017/s0033291719002678
11. Melin EO, Wanby P, Neumark T, Holmberg S, Neumark AN, Johansson K, et al. Depression was associated with younger age, female sex, obesity, smoking, and physical inactivity, in 1027 patients with newly diagnosed type 2 diabetes: a Swedish multicentre cross-sectional study. BMC Endocr Disord. (2022) . 22:273. doi: 10.1186/s12902-022-01184-3
12. Cui MJ, GQ FEI, Sun QN, Qian YN, Meng QY, Gu JC, et al. Construction of a risk predictive nomogram model for nocotine dependence among medical students. Chin Prev Med. (2021) . 22:125–30. doi: 10.16506/j.1009-6639.2021.02.009
13. Cong S, Wang N, Fan J, Wang BH, An J, Bao HL, et al. Tobacco dependence status and influencing factors among smokers aged 40 or older in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2021) . 42:807–13. doi: 10.3760/cma.j.cn112338-20210204-00092
14. El-Sherbiny NA, Elsary AY. Smoking and nicotine dependence in relation to depression, anxiety, and stress in Egyptian adults: A cross-sectional study. J Family Community Med. (2022) . 29:8–16. doi: 10.4103/jfcm.jfcm_290_21
15. Ho CSH, Tan ELY, Ho RCM, Chiu MYL. Relationship of anxiety and depression with respiratory symptoms: comparison between depressed and non-depressed smokers in Singapore. Int J Environ Res Public Health. (2019) 16:163. doi: 10.3390/ijerph16010163
16. Cui Y, Forget EL, Torabi M, Oguzoglu U, Ohinmaa A, Zhu Y. Health-related quality of life and economic burden to smoking behaviour among Canadians. Can J Public Health. (2019) . 110:533–41. doi: 10.17269/s41997-019-00244-x
17. Han K, Yang S, Jia W, Wang S, Song Y, Cao W, et al. Health-related quality of life and its correlation with depression among chinese centenarians. Front Public Health. (2020) . 8:580757. doi: 10.3389/fpubh.2020.580757
18. Ghimire S, Baral BK, Pokhrel BR, Pokhrel A, Acharya A, Amatya D, et al. Depression, malnutrition, and health-related quality of life among Nepali older patients. BMC Geriatr. (2018) . 18:191. doi: 10.1186/s12877-018-0881-5
19. Selenius JS, Wasenius NS, Kautiainen H, Salonen M, von Bonsdorff M, Eriksson JG. Impaired glucose regulation, depressive symptoms, and health-related quality of life. BMJ Open Diabetes Res Care. (2020) 8:e001568. doi: 10.1136/bmjdrc-2020-001568
20. Chalhoub NE, Luggen ME. Depression, pain, and health-related quality of life in patients with systemic lupus erythematosus. Int J Rheumatol. (2022) . 2022:6290736. doi: 10.1155/2022/6290736
21. Song H, Zhao Y, Hu C, Zhao C, Wang X, Xiao Z. Relationships among anxiety, depression, and health-related quality of life in adult epilepsy: A network analysis. Epilepsy Behav. (2024) . 154:109748. doi: 10.1016/j.yebeh.2024.109748
22. Pérez-Flores J, Hernández-Torres A, Montón F, Nieto A. Health-related quality of life and depressive symptoms in Friedreich ataxia. Qual Life Res. (2020) . 29:413–20. doi: 10.1007/s11136-019-02311-9
23. Schaefer M, Gotthardt DN, Ganion N, Wohnsland S, Seessle J, Stremmel W, et al. Wilson disease: Health-related quality of life and risk for depression. Clin Res Hepatol Gastroenterol. (2016) . 40:349–56. doi: 10.1016/j.clinre.2015.09.007
24. Johnsen MB, Winsvold BS, Børte S, Vie G, Pedersen LM, Storheim K, et al. The causal role of smoking on the risk of headache. A Mendelian randomization analysis in the HUNT study. Eur J Neurol. (2018) . 25:1148–e102. doi: 10.1111/ene.13675
25. Kahraman T, Ozdogar AT, Abasiyanik Z, Ozakbas S. Associations between smoking and walking, fatigue, depression, and health-related quality of life in persons with multiple sclerosis. Acta Neurol Belg. (2021) . 121:1199–206. doi: 10.1007/s13760-020-01341-2
26. Dhawan P, Goel S, Ghosh A. Quality of life of tobacco users- A correlation with duration of use and nicotine dependence. Indian J Tuberc. (2021) 68s:S60–s64. doi: 10.1016/j.ijtb.2021.08.025
27. Dos Santos AP, Lazzari TK, Silva DR. Health-related quality of life, depression and anxiety in hospitalized patients with tuberculosis. Tuberc Respir Dis (Seoul). (2017) . 80:69–76. doi: 10.4046/trd.2017.80.1.69
28. Liu Z, Li YH, Cui ZY, Li L, Nie XQ, Yu CD, et al. Prevalence of tobacco dependence and associated factors in China: Findings from nationwide China Health Literacy Survey during 2018-19. Lancet Reg Health West Pac. (2022) . 24:100464. doi: 10.1016/j.lanwpc.2022.100464
29. Gong F, Lei Z, Min H, Yu Y, Huang Z, Liu J, et al. Can smartphone use affect chronic disease self-management among Chinese middle-aged and older adults? A moderated mediation model. Front Psychol. (2022) . 13:1019335. doi: 10.3389/fpsyg.2022.1019335
30. Chen J, Tian Y, Yin M, Lin W, Tuersun Y, Li L, et al. Relationship between self-efficacy and adherence to self-management and medication among patients with chronic diseases in China: A multicentre cross-sectional study. J Psychosom Res. (2023) . 164:111105. doi: 10.1016/j.jpsychores.2022.111105
31. Wang D, Sun X, He F, Liu C, Wu Y. The mediating effect of family health on the relationship between health literacy and mental health: A national cross-sectional survey in China. Int J Soc Psychiatry. (2023) . 69:1490–500. doi: 10.1177/00207640231166628
32. Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. (1989) . 84:791–9. doi: 10.1111/j.1360-0443.1989.tb03059.x
33. Etter JF. A comparison of the content, construct and predictive validity of the cigarette dependence scale and the Fagerström test for nicotine dependence. Drug Alcohol Depend. (2005) . 77:259–68. doi: 10.1016/j.drugalcdep.2004.08.015
34. Min HW, Wu YB, Sun XY. Relation of family health and depression to nicotine dependence in adult smokers. Chin J Dis Control Prev. (2023) . 27:294–99. doi: 10.16462/j.cnki.zhjbkz.2023.03.008
35. Gandhi M, Ang M, Teo K, Wong CW, Wei YC, Tan RL, et al. EQ-5D-5L is more responsive than EQ-5D-3L to treatment benefit of cataract surgery. Patient. (2019). 12:383–92. doi: 10.1007/s40271-018-00354-7
36. Lolas F. Quality of life: objectifying the subjective experience. Alpha Psychiatry. (2023) . 24:67. doi: 10.5152/alphapsychiatry.2023.280223
37. Zou S, Feng G, Li D, Ge P, Wang S, Liu T, et al. Lifestyles and health-related quality of life in Chinese people: a national family study. BMC Public Health. (2022). 22:2208. doi: 10.1186/s12889-022-14680-x
38. Chen HM, Hua L, Wang J, Chen Y, Chen Y, Jin YL, et al. Investigation on the health-related quality of life in residents in Anhui Province based on EQ-5D-5L. J Wannan Med colleage. (2023). 42:489–93. doi: doi: 10.3969/j.issn.1002.0217.2023.05.021
39. Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L value set for China. Value Health. (2017). 20:662–69. doi: 10.1016/j.jval.2016.11.016
40. Carlton J, Peasgood T, Khan S, Barber R, Bostock J, Keetharuth AD. An emerging framework for fully incorporating public involvement (PI) into patient-reported outcome measures (PROMs). J Patient Rep Outcomes. (2020). 4:4. doi: 10.1186/s41687-019-0172-8
41. Nan H, Ni MY, Lee PH, Tam WW, Lam TH, Leung GM, et al. Psychometric evaluation of the Chinese version of the Subjective Happiness Scale: evidence from the Hong Kong FAMILY Cohort. Int J Behav Med. (2014). 21:646–52. doi: 10.1007/s12529-014-9389-3
42. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014). 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
43. Dong XX, Li DL, Miao YF, Zhang T, Wu Y, Pan CW. Prevalence of depressive symptoms and associated factors during the COVID-19 pandemic: A national-based study. J Affect Disord. (2023). 333:1–9. doi: 10.1016/j.jad.2023.04.034
44. Miao YF, Dong XX, Li DL, Zhang T, Wu Y, Pan CW. Chronic conditions and depressive symptoms in middle-aged and older Chinese adults: Roles of perceived social support and area of residence. J Affect Disord. (2023). 340:290–98. doi: 10.1016/j.jad.2023.08.045
45. Xiong HL, Liu DQ, Tang DY, Ma FX. Exposure to Chinese famine and the risk of hyperuricemia in later life: a population-based cross-sectional study. Front Nutr. (2024). 11:1266817. doi: 10.3389/fnut.2024.1266817
46. Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine Tob Res. (2017). 19:3–13. doi: 10.1093/ntr/ntw140
47. Petroulia I, Kyriakos CN, Papadakis S, Tzavara C, Filippidis FT, Girvalaki C, et al. Patterns of tobacco use, quit attempts, readiness to quit and self-efficacy among smokers with anxiety or depression: Findings among six countries of the EUREST-PLUS ITC Europe Surveys. Tob Induc Dis. (2018). 16:A9. doi: 10.18332/tid/98965
48. Cook JW, Baker TB, Beckham JC, McFall M. Smoking-induced affect modulation in nonwithdrawn smokers with posttraumatic stress disorder, depression, and in those with no psychiatric disorder. J Abnorm Psychol. (2017). 126:184–98. doi: 10.1037/abn0000247
49. Piirtola M, Kaprio J, Baker TB, Piasecki TM, Piper ME, Korhonen T. The associations of smoking dependence motives with depression among daily smokers. Addiction. (2021). 116:2162–74. doi: 10.1111/add.15390
50. Escobedo LG, Reddy M, Giovino GA. The relationship between depressive symptoms and cigarette smoking in US adolescents. Addiction. (1998). 93:433–40. doi: 10.1046/j.1360-0443.1998.93343311.x
51. Feng YH, Xu WZ. Advances in research on the relationship between depression and smoking. Chin Prev Med. (2022). 23:298–302. doi: 10.16506/j.1009-6639.2022.04.011
52. Pasco JA, Williams LJ, Jacka FN, Ng F, Henry MJ, Nicholson GC, et al. Tobacco smoking as a risk factor for major depressive disorder: population-based study. Br J Psychiatry. (2008). 193:322–6. doi: 10.1192/bjp.bp.107.046706
53. Jamal M, van der Does W, Penninx BW. Effect of variation in BDNF Val(66)Met polymorphism, smoking, and nicotine dependence on symptom severity of depressive and anxiety disorders. Drug Alcohol Depend. (2015). 148:150–7. doi: 10.1016/j.drugalcdep.2014.12.032
54. Markou A, Kosten TR, Koob GF. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis. Neuropsychopharmacology. (1998). 18:135–74. doi: 10.1016/s0893-133x(97)00113-9
55. Leventhal AM, Piper ME, Japuntich SJ, Baker TB, Cook JW. Anhedonia, depressed mood, and smoking cessation outcome. J Consult Clin Psychol. (2014). 82:122–9. doi: 10.1037/a0035046
56. Mickens L, Greenberg J, Ameringer KJ, Brightman M, Sun P, Leventhal AM. Associations between depressive symptom dimensions and smoking dependence motives. Eval Health Prof. (2011). 34:81–102. doi: 10.1177/0163278710383562
57. Secades-Villa R, Weidberg S, González-Roz A, Reed DD, Fernández-Hermida JR. Cigarette demand among smokers with elevated depressive symptoms: an experimental comparison with low depressive symptoms. Psychopharmacol (Berl). (2018). 235:719–28. doi: 10.1007/s00213-017-4788-1
58. Malhi GS, Berk M. Does dopamine dysfunction drive depression? Acta Psychiatr Scand Suppl. (2007) 115:116–24. doi: 10.1111/j.1600-0447.2007.00969.x
59. Milic M, Gazibara T, Pekmezovic T, Kisic Tepavcevic D, Maric G, Popovic A, et al. Tobacco smoking and health-related quality of life among university students: Mediating effect of depression. PLoS One. (2020). 15:e0227042. doi: 10.1371/journal.pone.0227042
60. Geng Y, Gu J, Zhu X, Yang M, Shi D, Shang J, et al. Negative emotions and quality of life among adolescents: A moderated mediation model. Int J Clin Health Psychol. (2020). 20:118–25. doi: 10.1016/j.ijchp.2020.02.001
Keywords: nicotine dependence, health-related quality of life, depression, mediator, current smokers
Citation: Xiong H, Ma F, Tang D and Liu D (2024) Correlations among nicotine dependence, health-related quality of life, and depression in current smokers: a cross-sectional study with a mediation model. Front. Psychiatry 15:1455918. doi: 10.3389/fpsyt.2024.1455918
Received: 27 June 2024; Accepted: 07 August 2024;
Published: 27 August 2024.
Edited by:
Yibo Wu, Peking University, ChinaCopyright © 2024 Xiong, Ma, Tang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengxun Ma, d29haXNlc0AxMjYuY29t
 Huali Xiong
Huali Xiong Fengxun Ma
Fengxun Ma Dayi Tang4
Dayi Tang4 Daiqiang Liu
Daiqiang Liu