
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 30 October 2024
Sec. Public Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1454087
 Amanuel Dukato1
Amanuel Dukato1 Abera Beyamo1
Abera Beyamo1 Aklilu Habte Hailegebireal1
Aklilu Habte Hailegebireal1 Wegayehu Zeneb Teklehaimanot2
Wegayehu Zeneb Teklehaimanot2 Abatwoy Ayfokru2
Abatwoy Ayfokru2 Metages Alemnew3
Metages Alemnew3 Daniel Birhanu Abate3
Daniel Birhanu Abate3 Worku Abemie2
Worku Abemie2 Bethlehem Taye Mengistu2
Bethlehem Taye Mengistu2 Yihenew Ayehu Dessie4
Yihenew Ayehu Dessie4 Leweyehu Alemaw Mengstie2
Leweyehu Alemaw Mengstie2 Bekahegn Girma2*
Bekahegn Girma2*Background: Depression is a significant public health concern in both developed and developing countries. The burden of depression is particularly high among patients with chronic illnesses in developing countries, creating a dual challenge for both patients and the community. However, depression goes undiagnosed in 50%-75% of patients with chronic conditions such as diabetes mellitus. Additionally, there is limited information about the prevalence of depression among diabetic patients in Ethiopia. Therefore, this study aimed to assess the prevalence and associated factors of depression among type 2 diabetic patients in Ethiopia.
Method: An institution-based cross-sectional study was conducted on 376 randomly selected type 2 diabetic patients. Data were collected through face-to-face interviews and from patients’ follow-up records. The data were entered into EpiData version 4.6 and analyzed using STATA 14. Bivariable and multivariate logistic regression analyses were employed to identify associated factors. Variables with a p-value of less than 0.25 in the bivariable analysis were selected for multivariate logistic regression. Model fitness was assessed using Hosmer-Lemeshow’s test, and associations were reported using adjusted odds ratios with 95% confidence intervals
Results: In this study, the prevalence of depression among type 2 diabetic patients was found to be 69.72% (95% CI: 64.75, 74.27). Three factors were significantly associated with depression in these patients: the duration of diabetes mellitus since diagnosis [AOR: 1.17; 95% CI (1.02, 1.34)], glycaemic control [AOR: 1.8; 95% CI (1.09, 3.01)] and cigarette smoking [AOR: 2.18; 95% CI (1.07, 4.46)].
Conclusion: The prevalence of depression among type 2 diabetic patients was high. The Federal Ministry of Health, stakeholders, and the Ethiopian Diabetes Association should collaborate to reduce this burden. Mental health assessment and treatment should be integrated into chronic care follow-up services. Additionally, healthcare providers should closely monitor and counsel patients who smoke and those with poor glycemic control.
Depression is a prevalent mental condition characterized by persistent sadness, anhedonia, fatigue, changes in appetite, disinterest in daily activities, feelings of guilt, low self-esteem, sleep disturbances, exhaustion, and suicidal thoughts (1). It significantly impacts individuals and the country due to its disruption of daily life (2, 3). If left untreated, depression can worsen and persist; however, treatments are often very effective in alleviating symptoms (4).
Diabetes is a chronic condition where the body either does not produce sufficient insulin, produces no insulin at all, or cannot effectively use the insulin it does produce. Type 2 diabetes mellitus (T2DM) typically develops in adulthood (5, 6). The global prevalence of diabetes among individuals aged 20 to 79 is 9.3%, with 79.4% of cases occurring in low- and middle-income countries (7, 8). Recent studies indicate that 28% of T2DM patients globally, 24% in Europe, 29% in Australia, 32% in Asia, and 27% in Africa experience concurrent depression (9, 10). In Ethiopia, the prevalence of depression among T2DM patients ranges from 13% to 40.4%, reflecting variations in study duration, settings, and assessment tools (11).
Depression and diabetes mellitus (DM) have a bidirectional relationship, with early-life depression increasing the risk of developing diabetes, and diabetes subsequently raising the likelihood of depression later in life (12). Individuals with DM are at a heightened risk for depression (13). The mechanism of their interaction is expressed like depression can be stimulated by hyperglycaemia and dyslipidaemia because they worsen inflammation and lower serotonin levels in the brain. Disrupted insulin signaling in T2DM can decrease glycaemic control, and depression can affect insulin signing. Prolonged stress in individuals with depression further exacerbate type 2 diabetes by increasing cortisol levels, which in turn causes insulin resistance and accelerates the development of T2DM (14–16).
The intricate relationship between mental health and illness treatment is highlighted by recent developments in our understanding of the psychological problems related to diabetes mellitus (17, 18). Diabetes care now includes psychological issues such as melancholy, anxiety, and diabetes distress as essential components (19–21). According to research, the constant demands of self-care, particularly worries about complications, cause significant mental discomfort for people with diabetes (18, 22). The Diabetes Distress Scale is one of the instruments used in modern clinical practice to provide prompt and focused mental health interventions (14–16, 23, 24). Furthermore, patients who get psychological assistance are better able to control their anxiety of hypoglycemia (15, 25).
Technological advancements have made diabetic psychological concerns management even more advanced. Research demonstrates that these digital methods of delivering cognitive-behavioral therapy, mindfulness-based therapies, and acceptance and commitment therapy are beneficial in reducing diabetes-related suffering and enhancing mental health (26–29).
The coexistence of diabetes and depression can lead to poor treatment adherence, poor glycaemic control, higher complication rates, reduced quality of life, increased healthcare utilization and costs, greater disability, loss of productivity, and an elevated risk of death (30–33). It also heightens the risk of both micro vascular and macro vascular complications (8, 34). Moreover, it has work related risks like sickness absence, unemployment and reduced income (35).
Preceding studies identified age, smoking habit, being women, poor social support, number of comorbidities, higher level of cholesterol, physical disability and body mass index as risk factors for depression among diabetic adults (36–38).
In the developed world, numerous studies have been conducted to assess the prevalence and determinants of depression among diabetic patients. However, fewer studies have been carried out in Africa, including Ethiopia. Therefore, this study aimed to assess the prevalence and associated factors of depression among patients with T2DM in Ethiopia.
The study was conducted from June 30 to July 30, 2022, in comprehensive specialized hospitals located in Southern Ethiopia. These hospitals include Wachamo University Comprehensive Specialized Hospital (WUCSH), Wolaita Sodo University Comprehensive Specialized Hospital, and Worabe Comprehensive Specialized Hospital. Our study took place at WUCSH, situated in Hosanna Town, Hadiya Zone, Southern Ethiopia, approximately 232 kilometres from Addis Ababa, the capital city of Ethiopia.
WUCSH provides general and specialized healthcare services, along with teaching and research activities. It offers comprehensive diabetes-related services, with the diabetic clinic being one of the hospital’s oldest clinics, providing care and follow-ups for patients with all types of diabetes.
An institutional based cross-sectional study.
All adult patients with T2DM who have follow-up in comprehensive specialized hospitals found in southern Ethiopia.
All adult patients diagnosed with type 2 Diabetes Mellitus receiving follow-up care at the selected hospital (WUCSH).
All adult patients (>18 years old) diagnosed with type 2 Diabetes Mellitus who were receiving care at WUCSH and provided consent were included. However, patients who were currently taking antidepressant medication for their depressive symptoms, those who were severely ill during the data collection period, and newly diagnosed type 2 diabetes mellitus patients at the time of data collection were excluded.
The sample size was determined using the single population proportion formula, based on the following assumptions: a prevalence (p) of depression among adult patients with Diabetes Mellitus (37%), as reported in a previous study conducted in Ethiopia (39), a confidence level (Zα/2) of 95%, and a margin of error of 5%.
After adding 5% non-response rate, the minimum required sample size was 376.
Before data collection, the total number of diabetic patients who had visited the hospital since 2021 was obtained from patient records. The average number of diabetic patients visiting the hospital over a one-month period was then calculated to be 1071. Participants for interviews were selected using systematic random sampling. The sampling interval (k) was determined by dividing the expected number of diabetic patients having a follow-up visit at the time of data collection by the calculated sample size (k = 3). Starting from a random number between one and three, eligible individuals were interviewed at every third interval based on the order of their clinical evaluation.
Depression: if patients Patient Health Questionnaire (PHQ) score was 5 or higher (38).
Poor glycaemic control: having an average fasting blood sugar (FBS) level greater than 130 mg/dl over a three-month period (40).
Regular physical activity: defined as engaging in exercise for at least 30 minutes or walking for 3 or more days per week (40).
Current cigarette smokers: individuals who had smoked cigarettes within the 30 days preceding the data collection (35).
A semi-structured questionnaire was utilized to collect data through face-to-face interviews and record reviews. The questionnaire was originally designed in English and translated into Amharic, then back-translated into English to ensure consistency.
A pre-test was conducted on 5% of the sample size to assess language clarity, appropriateness of data collection tools, time estimation, and necessary adjustments based on the feedback. Data collectors and supervisors underwent comprehensive training on the data collection tool and process. Subsequently, investigators and supervisors meticulously reviewed all collected data for completeness and consistency. Random samples of questionnaires were checked for inconsistencies, coding errors, completeness, clarity, and any missing values before data entry.
The PHQ tool is 9-item depression screening and diagnostic questionnaire. Each question requires participants to rate the frequency of depressive symptoms experienced during the two weeks prior to evaluation. These items include: 1) loss of interest, 2) depressed mood, 3) insomnia or hypersomnia, 4) fatigue or loss of energy, 5) appetite disturbances, 6) guilt or worthlessness, 7) diminished ability to think or concentrate, 8) psychomotor agitation or retardation, and 9) suicidal thoughts. Scores for each item range from 0 (“not at all”) to 3 “nearly every day” with a total score ranging from 0 to 27 (41).
The PHQ tool was previously validated in a study conducted in East Africa, which reported a Cronbach’s alpha of 0.85. Furthermore, its reliability was found to be 0.92 (42). Additionally, the Amharic version of the PHQ was specifically validated in a study conducted in Ethiopia, where the kappa agreement and interclass correlation coefficient were 0.80 and 0.92, respectively (43). Even though the Amharic version had already been validated in earlier studies, in this study the Cronbach’s alpha was also 0.79.
The data were entered using EpiData version 4.6.0.2 and exported to STATA version 14 for analysis. Descriptive statistics such as frequencies, means, and standard deviations were computed to characterize the variables.
Logistic regression analysis was conducted to identify factors associated with depression. Variables with a p-value less than 0.25 in the bivariable analysis were included in the multivariable logistic regression model. The Hosmer-Lemeshow’s test was performed to assess the goodness of fit of the model. In the multivariable logistic regression model, adjusted odds ratios with 95% confidence intervals were calculated to determine the strength and direction of associations.
In the current study, a total of 360 respondents were participated with a response rate of 95.7%.
The respondents had a mean age of 47.2 years, with a standard deviation of ±15.7. Of the participants, 210 (58.3%) were male and identified as Protestant. Approximately seventy-two percent of the respondents were married, and 161 (44.7%) had completed a diploma or higher education. Lastly, 102 (28.3%) of the respondents were self-employed (Table 1).
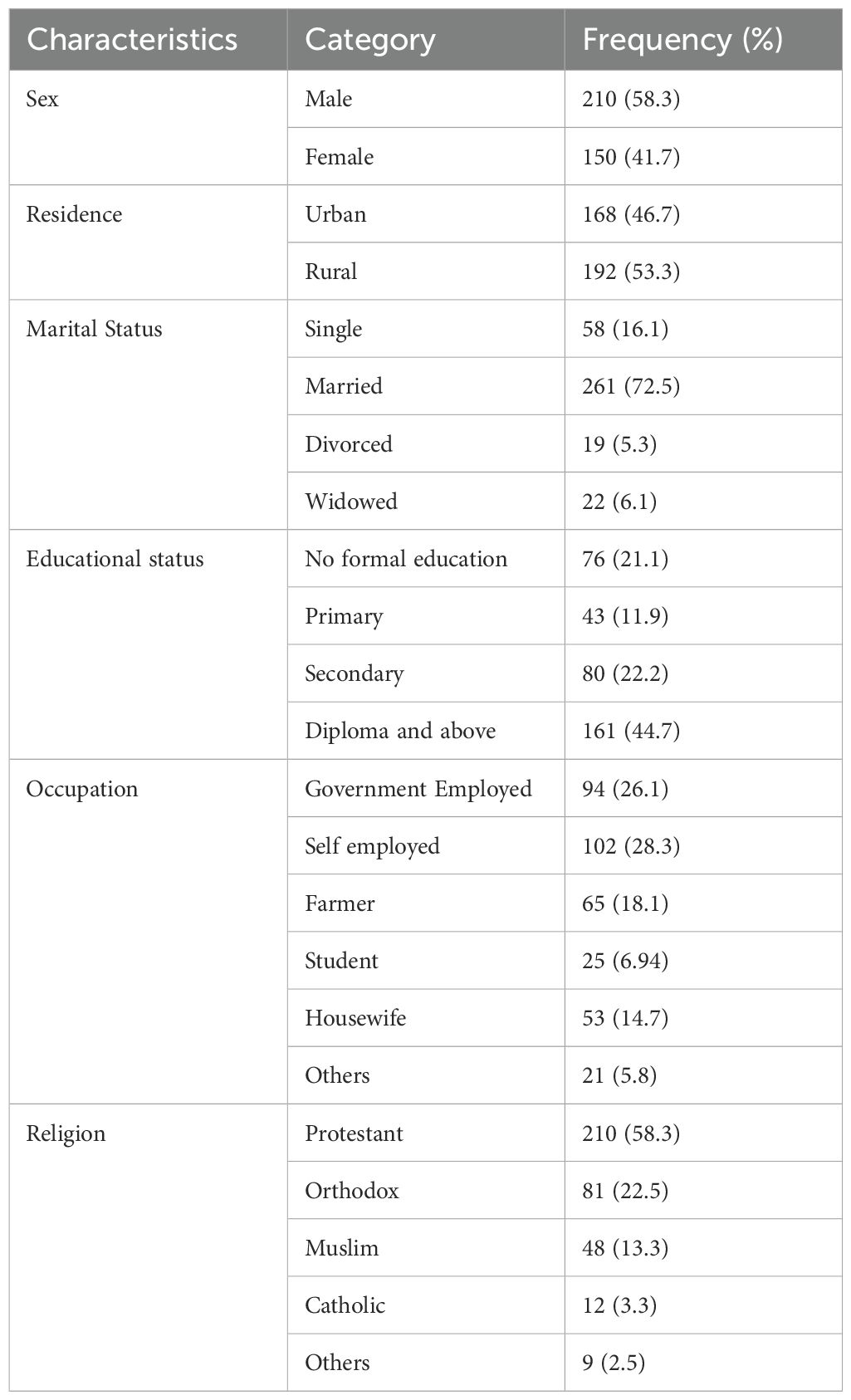
Table 1. Socio-demographic characteristics of type 2 diabetic patients included in this study, 2024 (n = 360).
Two hundred three (56.4%) of the participants were receiving non-insulin treatment, and one hundred (27.8%) of them were also diagnosed with hypertension. The mean fasting blood sugar (FBS) level among respondents was 197.1 mg/dl (± SD: 85.0), and the average duration of diabetes mellitus (DM) was 3.1 years (± SD: 2.1). One hundred eighty-eight (52.2%) of the respondents achieved good glycaemic control, and the majority (83.1%) did not have a family history of DM (Table 2).
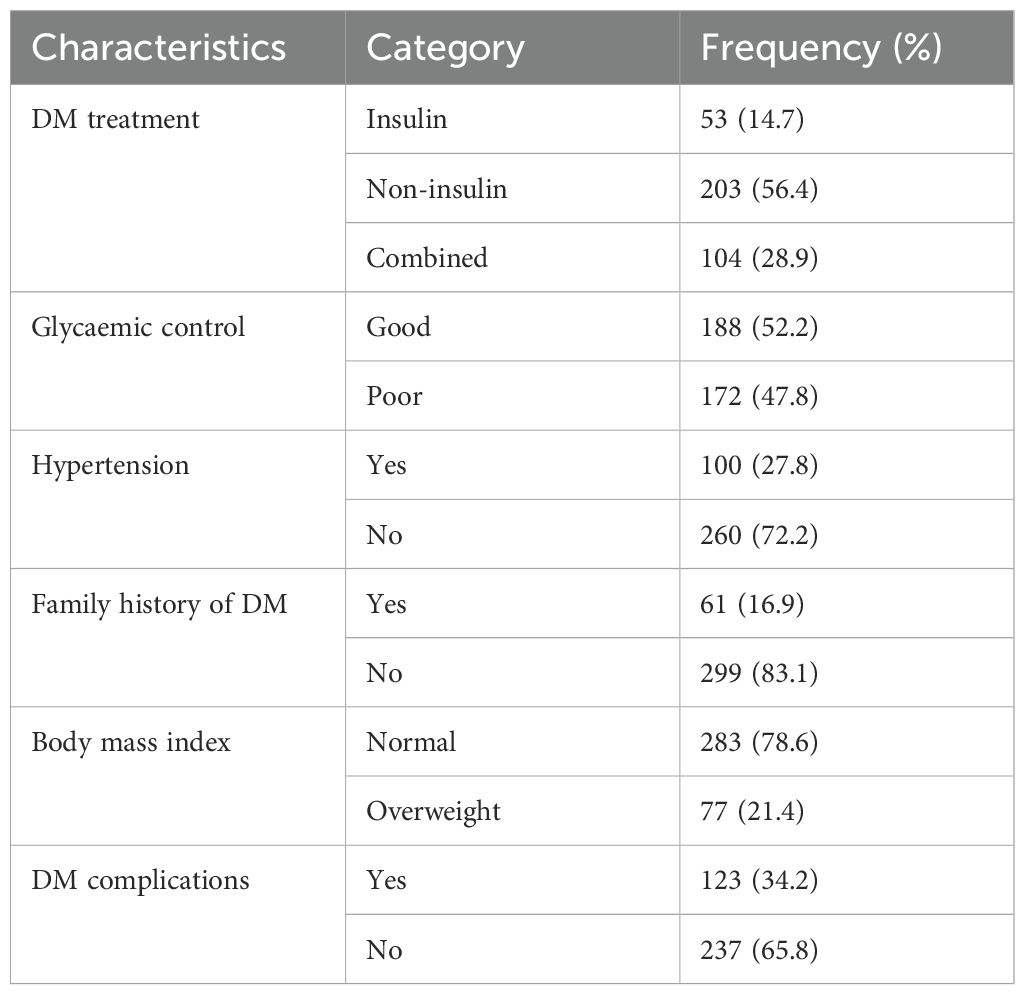
Table 2. Clinical characteristics of type 2 diabetic patients included in this study, 2024 (n = 360).
Three hundred thirty-three (92.5%) of the participants did not engage in regular exercise. Forty-seven (13.1%) of them reported being smokers. Finally, approximately one-fifth (20.3%) of our respondents experienced sexual dysfunction (Table 3).
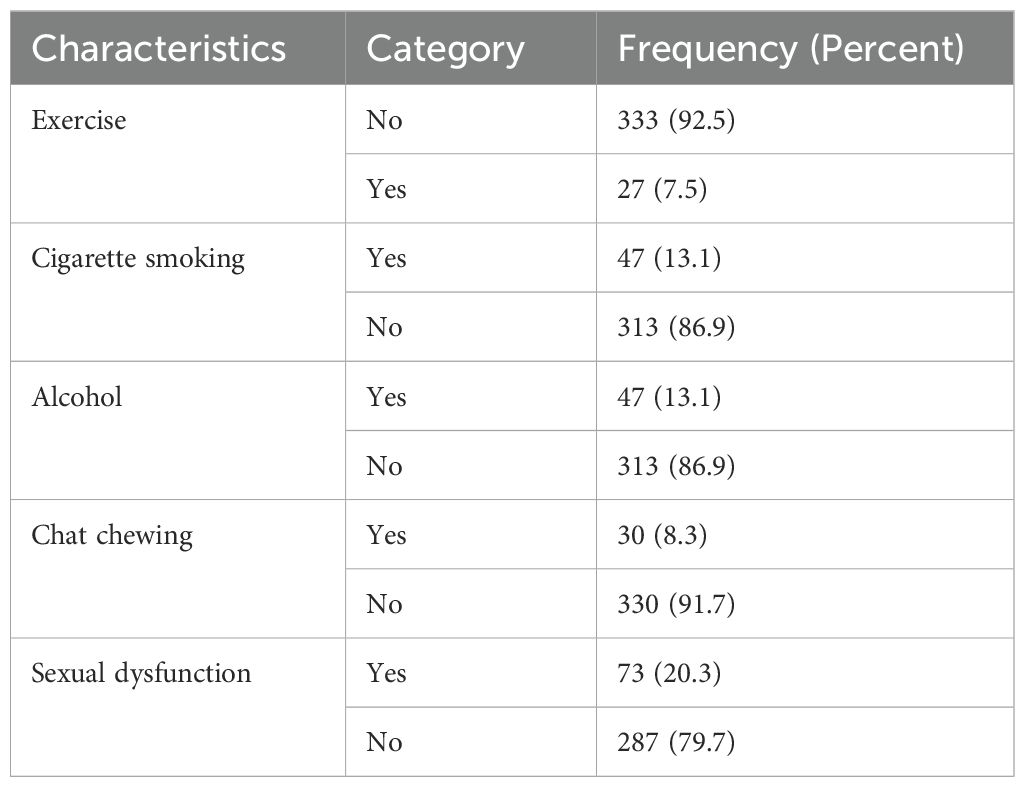
Table 3. Behavioral related characteristics among type 2 diabetic patients included in this study, 2024 (n = 360).
The prevalence of depression among diabetic patients was 69.72% (95% CI: 64.75, 74.27).
Gender, marital status, duration of diabetes mellitus since diagnosis, hypertension, family history of diabetes mellitus, adherence to exercise, body mass index, diabetes mellitus complications, alcohol consumption, glycaemic control, chat chewing, and cigarette smoking status were considered as candidate variables for multivariable logistic regression analysis. However, in the multivariable logistic regression analysis, only three variables duration of diabetes, glycaemic control, and cigarette smoking showed a significant association with depression among type 2 diabetic patients (Table 4).
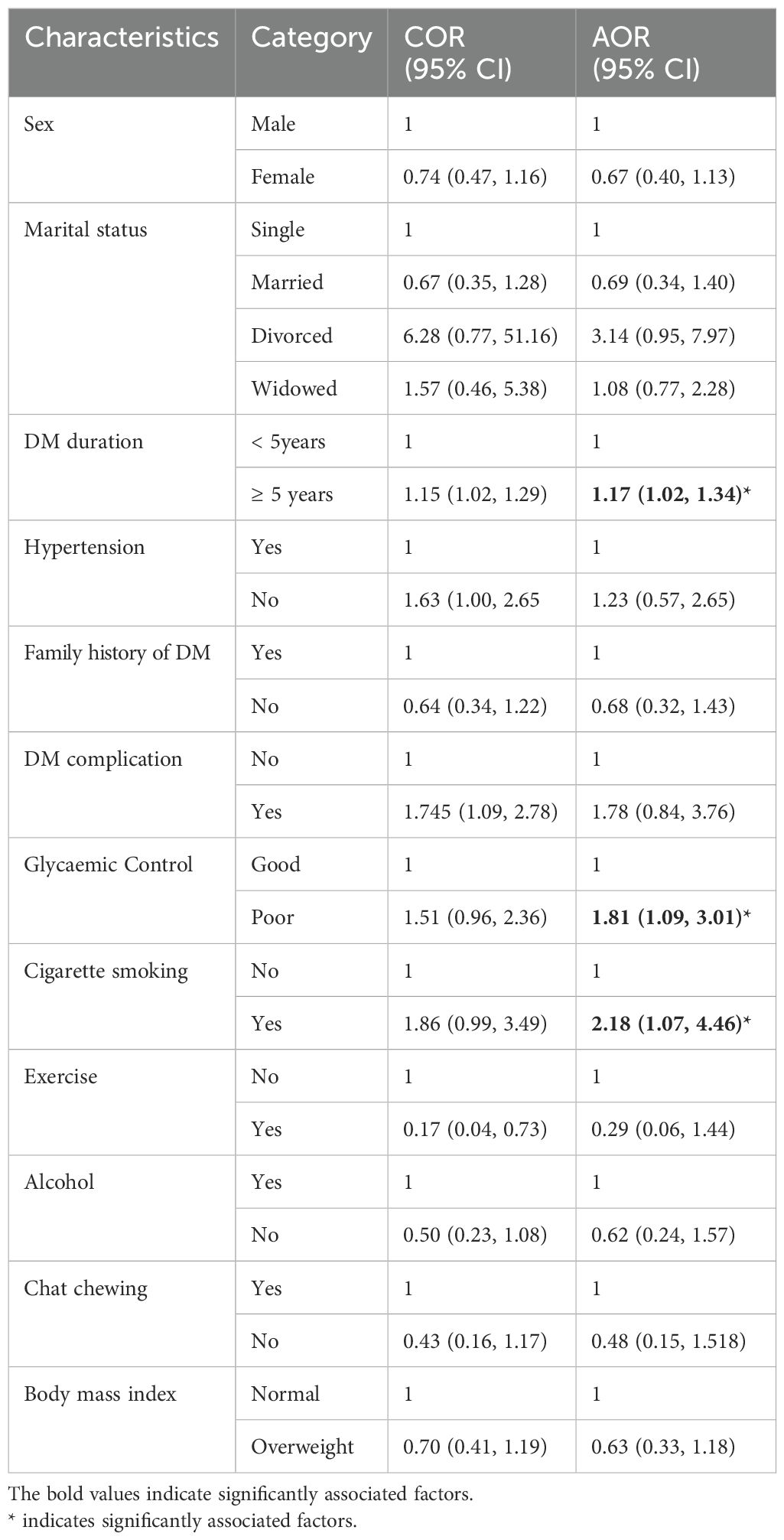
Table 4. Bivariable and Multivariable analysis to identify factors associated with depression among people with T2DM in Ethiopia, 2024 (n= 360).
Therefore, this study supports the association between clinical and psychosocial factors with depression among diabetic patients. However, not support the hypothesis that declares the connection between socioeconomic factors and depression among diabetic patients.
In this study, Type 2 diabetic patients with poor glycaemic control had 1.8 times higher risk of depression compared to those with better control [AOR: 1.8; 95% CI (1.09, 3.01)]. Patients with a longer duration since diabetes diagnosis had increased odds of depression [AOR: 1.17; 95% CI (1.02, 1.34)]. Lastly, diabetic patients who smoked cigarettes were at 2.1 times higher risk of depression compared to non-smokers [AOR: 2.18; 95% CI (1.07, 4.46)].
The current study aimed to determine the prevalence of depression and its contributing factors among patients with T2DM diabetes mellitus in Ethiopia. The prevalence of depression was 69.72% (95% CI: 64.75, 74.27).
This finding was in line with studies conducted in Egypt (44) and Iran (45). This might be due to similarity in diagnostic tool and study design. However, the prevalence was higher than studies conducted in Sudan (46), India (47), Vietnam (48), Saudi Arabia (49) and Ethiopia (38, 39, 50–52). This variation may be attributed to differences in sample size, study settings, and assessment tools. Additionally, it could be influenced by changes in environmental, cultural, and social contexts, as well as disparities in healthcare service availability and quality. Lastly, the prevalence reported in our study was low as compared to study conducted in Tanzania (13). This might be due to difference in health care seeking behavior and availability of psychiatric services for patients with chronic diseases.
Diabetic patients who had poor glycaemic control had more likely to manifest depression. This finding was supported by studies conducted in Ghana (53), Iran (54), China (55) and Peru (56). This could be attributed to poor glycaemic control, which increases levels of brain neurotransmitters linked to depression and alters connections between brain regions that regulate emotions (57). Additionally, it may be related to the fact that lower HbA1C levels are associated with a reduced risk of diabetic complications (58).
The duration of diabetes mellitus since diagnosis was also found to be positively associated with depression. This finding is consistent with studies conducted in Ethiopia (39). This could be because a longer duration of diabetes mellitus is associated with an increased risk of developing diabetes-related complications and comorbidities, which may explain the higher likelihood of depression with longer illness duration.
Finally, diabetic patients who smoke cigarettes were found to have a higher risk of depression. This finding is consistent with a study conducted in Tanzania (13). This may be because smoking can alter neurocircuitry, increasing sensitivity to environmental stressors and thereby raising the risk of developing depression.
This study had several limitations. Firstly, due to its cross-sectional design, establishing the temporal relationship between dependent and independent variables was challenging. Secondly, important factors such as intimate partner violence, food security, and social support were not assessed.
In the current study, the prevalence of depression among diabetic patients was found to be higher compared to other studies. Additionally, three factors duration of the disease, poor glycaemic control, and cigarette smoking were identified as independent risk factors for depression among patients with type 2 diabetes mellitus.
To fill this gap, the Federal Ministry of Health, stakeholders, and the Ethiopian Diabetic Association should collaborate and design new strategies like integrating the mental health assessment and treatment service into chronic follow-up clinics. Moreover, in future innovative technologies like mHealth and telemedicine as well as cognitive behavioral therapy should be considered and implemented to decrease the burden of depression.
Furthermore, mindfulness-based interventions, and acceptance and commitment therapy should be delivered through digital technologies to increase awareness and self-care practice skills. Healthcare providers should also prioritize and provide counseling to patients who smoke and those with poor glycaemic control. Lastly, future researchers should conduct longitudinal studies to gain a deeper understanding of this issue.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by IRB of Wachemo University, Ethiopia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WT: Writing – original draft, Writing – review & editing. AA: Writing – original draft, Writing – review & editing. MA: Writing – original draft, Writing – review & editing. DB: Writing – original draft, Writing – review & editing. WA: Writing – original draft, Writing – review & editing. BM: Writing – review & editing, Writing – original draft. YA: Writing – original draft, Writing – review & editing. LM: Writing – original draft, Writing – review & editing. BG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. We acknowledge funding from Wachemo University, Ethiopia (grant number 1675/15).
We greatly acknowledge Wachemo University, participants, data collectors and supervisors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, Adjusted odds ratio; CI, Confidence interval; COR, Crude odds ratio; DM, Diabetic Mellitus; T2DM, Type 2 Diabetic Mellitus; WUCSH, Wachemo University comprehensive specialized hospital.
1. Parveen T, Hameed F, Kahn J. The impact of maternal obesity on neonatal Apgar score and neonatal intensive care unit admissions in a tertiary care hospital. Pak J Surj. (2018) 34:161–5.
2. Fino P, Di Taranto G, Pierro A, Kacjulite J, Codolini L, Onesti MG, et al. Depression risk among patients with chronic wounds. Eur Rev Med Pharmacol Sci. (2019) 23:4310–2. doi: 10.26355/eurrev_201905_17936
3. Wachholz PA, Masuda PY, Nascimento DC, Taira CM, Cleto NG. Quality of life profile and correlated factors in chronic leg ulcer patients in the mid-west of São Paulo State, Brazil. Anais Brasileiros Dermatol. (2014) 89:73–81. doi: 10.1590/abd1806-4841.20142156
4. Cleveland Clinic, Depression: Types, Symptoms, Couses and Treatments (2021). Available online at: https://my.clevelandclinic.org/health/diseases/9290-depression (accessed March 29, 2024).
5. Bollinger ST, Butcher MK, Condon JE, Cypress M, C-ANP CD, Faulkner P, et al. 2017 National standards for diabetes self-management education and support. Diabetes Care. (2017) 40:1409–19. doi: 10.2337/dci17-0025
6. Rodgers GP. Message from Griffin P. Rodgers, MD, MACP, director, NIDDK, on the institute’s obesity research. Obesity. (2007) 15:1631. doi: 10.1038/oby.2007.193
7. International Diabetes Federation, IDF Diabetes Atlas, 10th Edition. (2021). Available online at: https://diabetesatlas.org/atlas/tenth-edition/https://diabetesatlas.org/atlas/tenth-edition/ (accessed April 27, 2024).
8. Tesfaye B, Alebel A, Gebrie A, Zegeye A, Leshargie CT, Ferede A, et al. Diabetes mellitus and its association with hypertension in Ethiopia: A systematic review and meta-analysis. Diabetes Res Clin Pract. (2019) 156:107838. doi: 10.1016/j.diabres.2019.107838
9. Khaledi M, Haghighatdoost F, Feizi A. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. (2019) 56:631–50. doi: 10.1007/s00592-019-01295-9
10. Sartorius N. Depression and diabetes. Dialogues Clin Neurosci. (2018) 20:47–52. doi: 10.31887/DCNS.2018.20.1/nsartorius
11. Dejenie Habtewold T, Radie YT, Sharew NT. Prevalence of depression among type 2 diabetic outpatients in black lion general specialized hospital, Addis Ababa, Ethiopia. Depression Res Treat. (2015) 2015. doi: 10.1155/2015/184902
12. Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. (2011) 13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton
13. Khan ZD, Lutale J, Moledina SM. Prevalence of depression and associated factors among diabetic patients in an outpatient diabetes clinic. Psychiatry Journal. (2019) 2019:2083196. doi: 10.1155/2019/2083196
14. Khawagi WY, Al-kuraishy HM, Hussein NR, Al-Gareeb AI, Atef E, Elhussieny O, et al. Depression and type 2 diabetes: A causal relationship and mechanistic pathway. Diabetes Obes Metab. (2024) 26:3031–44. doi: 10.1111/dom.15630
15. Puşcaşu A, Bolocan A, Păduraru DN, Salmen T, Bica C, Andronic O. The implications of chronic psychological stress in the development of diabetes mellitus type 2. Mediterr J Clin Psychol. (2022) 10. doi: 10.13129/2282-1619/mjcp-3455
16. Basiri R, Seidu B, Rudich M. Exploring the interrelationships between diabetes, nutrition, anxiety, and depression: implications for treatment and prevention strategies. Nutrients. (2023) 15:4226. doi: 10.3390/nu15194226
17. Martino G, Caputo A, Vicario CM, Catalano A, Schwarz P, Quattropani MC. The relationship between alexithymia and type 2 diabetes: A systematic review. Front Psychol. (2020) 11:2026. doi: 10.3389/fpsyg.2020.02026
18. Perrin N, Davies MJ, Robertson N, Snoek FJ, Khunti K. The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: a systematic review and meta-analysis. Diabetic Med. (2017) 34:1508–20. doi: 10.1111/dme.2017.34.issue-11
19. Martino G, Catalano A, Bellone F, Russo GT, Vicario CM, Lasco A, et al. As time goes by: anxiety negatively affects the perceived quality of life in patients with type 2 diabetes of long duration. Front Psychol. (2019) 10:1779. doi: 10.3389/fpsyg.2019.01779
20. Moroianu LA, Motofei IG, Curis C, Barbu R-E, Toma A. The impact of anxiety and depression on the pediatric patients with diabetes. Mediterr J Clin Psychol. (2020) 8. doi: 10.6092/2282-1619/mjcp-2435
21. Sagar R, Talwar S, Desai G, Chaturvedi SK. Relationship between alexithymia and depression: A narrative review. Indian J Psychiatry. (2021) 63:127–33. doi: 10.4103/psychiatry.IndianJPsychiatry_738_19
22. Ademoyegun AB, Afolabi OE, Aghedo IA, Adelowokan OI, Mbada CE, Awotidebe TO. The mediating role of sedentary behaviour in the relationship between social support and depression among individuals with diabetes. Mediterr J Clin Psychol. (2022) 10. doi: 10.13129/2282-1619/mjcp-3420
23. Fisher L, Polonsky WH, Hessler D. Addressing diabetes distress in clinical care: a practical guide. Diabetic Med. (2019) 36:803–12. doi: 10.1111/dme.2019.36.issue-7
24. Martino G, Bellone F, Langher V, Caputo A, Catalano A, Quattropani MC, et al. Alexithymia and psychological distress affect perceived quality of life in patients with type 2 diabetes mellitus. Mediterr J Clin Psychol. (2019) 7:1–15. doi: 10.6092/2282-1619/2019.7.2328
25. Caputo A, Vicario CM, Cazzato V, Martino G. psychological factors as determinants of medical conditions, volume II. Switzerland: Frontiers Media SA (2022). p. 865235.
26. Kumar DS, Prakash B, Chandra BS, Kadkol PS, Arun V, Thomas JJ, et al. Technological innovations to improve health outcome in type 2 diabetes mellitus: A randomized controlled study. Clin Epidemiol Global Health. (2021) 9:53–6. doi: 10.1016/j.cegh.2020.06.011
27. Akturk HK, Garg S. Technological advances shaping diabetes care. Curr Opin Endocrinol Diabetes Obes. (2019) 26:84–9. doi: 10.1097/MED.0000000000000467
28. Jenkinson E, Knoop I, Hudson JL, Moss‐Morris R, Hackett RA. The effectiveness of cognitive behavioural therapy and third-wave cognitive behavioural interventions on diabetes-related distress: A systematic review and meta-analysis. Diabetes Med. (2022) 39:e14948. doi: 10.1111/dme.v39.11
29. Ngan HY, Chong YY, Chien WT. Effects of mindfulness-and acceptance-based interventions on diabetes distress and glycaemic level in people with type 2 diabetes: Systematic review and meta-analysis. Diabetic Med. (2021) 38:e14525. doi: 10.1111/dme.14525
30. Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. (2010) 87:302–12. doi: 10.1016/j.diabres.2010.01.024
31. Niraula K, Kohrt BA, Flora MS, Thapa N, Mumu SJ, Pathak R, et al. Prevalence of depression and associated risk factors among persons with type-2 diabetes mellitus without a prior psychiatric history: a cross-sectional study in clinical settings in urban Nepal. BMC Psychiatry. (2013) 13:1–12. doi: 10.1186/1471-244X-13-309
32. de Groot M, Anderson Ryan BA, Freedland Kenneth E, Clouse Ray E, Lustman Patrick J. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. (2001) 63:619–30. doi: 10.1097/00006842-200107000-00015
33. Acee AM, Fahs MC. Can treating depression improve diabetic management? Nurse Pract. (2012) 37:46–52. doi: 10.1097/01.NPR.0000408509.34689.72
34. Trief PM. Depression in elderly diabetes patients. Diabetes Spectr. (2007) 20:71–5. doi: 10.2337/diaspect.20.2.71
35. de Wit M, Trief PM, Huber JW, Willaing I. State of the art: understanding and integration of the social context in diabetes care. Diabetic Med. (2020) 37:473–82. doi: 10.1111/dme.14226
36. Dejene S, Negash A, Tesfay K, Jobset A, Abera M. Depression and diabetes in jimma university specialized hospital, Southwest Ethiopia. J Psychiatry. (2014) 17:2. doi: 10.4172/Psychiatry.1000126
37. Engidaw NA, Wubetu AD, Basha EA. Prevalence of depression and its associated factors among patients with diabetes mellitus at Tirunesh-Beijing general hospital, Addis Ababa, Ethiopia. BMC Public Health. (2020) 20:266. doi: 10.1186/s12889-020-8360-2
38. Tegegne KD, Gebeyehu NA, Kassaw MW. Depression and determinants among diabetes mellitus patients in Ethiopia, a systematic review and meta-analysis. BMC Psychiatry. (2023) 23:209. doi: 10.1186/s12888-023-04655-6
39. Asefa A, Zewudie A, Henok A, Mamo Y, Nigussie T. Depression and its associated factors among diabetes mellitus patients attending selected hospitals in southwest Ethiopia: A cross-sectional study. Psychiatry J. (2020) 2020:6486030. doi: 10.1155/2020/6486030
40. Birhanu AM, Alemu FM, Ashenafie TD, Balcha SA, Dachew BA. Depression in diabetic patients attending University of Gondar Hospital Diabetic Clinic, Northwest Ethiopia. Diabetes Metab Syndr Obes. (2016) 9:155–62. doi: 10.2147/DMSO.S97623
41. Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Jama. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
42. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210:653–61. doi: 10.1016/j.psychres.2013.07.015
43. Gelaye B, Wilson I, Berhane HY, Deyessa N, Bahretibeb Y, Wondimagegn D, et al. Diagnostic validity of the Patient Health Questionnaire-2 (PHQ-2) among Ethiopian adults. Compr Psychiatry. (2016) 70:216–21. doi: 10.1016/j.comppsych.2016.07.011
44. Ismail MFS, Fares MM, Abd-Alrhman AG. Prevalence of depression and predictors of glycemic control among type 2 diabetes mellitus patients at family medicine clinic, Suez Canal University Hospital Egypt. Middle East J Family Med. (2019) 7. doi: 10.5742/MEWFM.2019.93611
45. Mendenhall E, Norris SA, Shidhaye R, Prabhakaran D. Depression and type 2 diabetes in low-and middle-income countries: a systematic review. Diabetes Res Clin Pract. (2014) 103:276–85. doi: 10.1016/j.diabres.2014.01.001
46. Abdelaziz MO, Alzain MA, Abdalkhaleg MA. Prevalence and risk factors of depression among adult Type 2 diabetic patients at Al-Jemaih Diabetic Center, Dongola, Northern State, Sudan, 2019. Sudan J Med Sci. (2020) 15:408–17. doi: 10.18502/sjms.v15i4.8163
47. Kant R, Yadav P, Barnwal S, Dhiman V, Abraham B, Gawande K. Prevalence and predictors of depression in type 2 diabetes mellitus. J Educ Health Promot. (2021) 10:352. doi: 10.4103/jehp.jehp_1507_20
48. Tran NMH, Nguyen QN, Vo TH, Le TT, Ngo NH. Depression among patients with type 2 diabetes mellitus: prevalence and associated factors in Hue City, Vietnam. Diabetes Metab Syndrome Obesity: Targets Ther. (2021) p:505–13. doi: 10.2147/DMSO.S289988
49. Mukrim AE, Alshammari NM, Alshammari WM, Alshammari MS, Alshammari YN, Alshammari AS, et al. Prevalence of depression, anxiety, and stress among diabetes mellitus patients in Arar, Northern Saudi Arabia. Age. (2019) 62:22–3. doi: 10.24911/IJMDC.51-1542576396
50. Teshome HM, Ayalew GD, Shiferaw FW, Leshargie CT, Boneya DJ. The prevalence of depression among diabetic patients in Ethiopia: A systematic review and meta-analysis, 2018. Depress Res Treat. (2018) 2018:6135460. doi: 10.1155/2018/6135460
51. Jarso MH, Likasa DD. Prevalence and associated factors of depression among diabetic outpatients in Ethiopia. Prim Care Companion CNS Disord. (2020) 22. doi: 10.4088/PCC.19m02479
52. Mossie TB, Berhe GH, Kahsay GH, Tareke M. Prevalence of Depression and Associated Factors among Diabetic Patients at Mekelle City, North Ethiopia. Indian J Psychol Med. (2017) 39:52–8. doi: 10.4103/0253-7176.198947
53. Akpalu J, Yorke E, Ainuson-Quampah J. Depression and glycaemic control among type 2 diabetes patients: a cross-sectional study in a tertiary healthcare facility in Ghana. BMC Psychiatry. (2018) 18:1–7. doi: 10.1186/s12888-018-1933-2
54. Azami G, Soh Lam K, Sazlina S-G, Salmiah M, Khosravi A, Aazami S, et al. The effect of depression on poor glycemic control in adults with type 2 diabetes: The mediating roles of self-efficacy and self-management behaviors. Dubai Diabetes Endocrinol J. (2019) 25:80–9. doi: 10.1159/000502126
55. Sun N, Lou P, Shang Y, Zhang P, Wang J, Chang G, et al. Prevalence and determinants of depressive and anxiety symptoms in adults with type 2 diabetes in China: a cross-sectional study. BMJ Open. (2016) 6:e012540. doi: 10.1136/bmjopen-2016-012540
56. Crispín-Trebejo B, Robles-Cuadros MC, Bernabé-Ortiz A. Association between depression and glycemic control among type 2 diabetes patients in L ima, P eru. Asia-Pacific Psychiatry. (2015) 7:419–26. doi: 10.1111/appy.12190
57. Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm–2018 executive summary. Endocrine Pract. (2018) 24:91–121. doi: 10.4158/CS-2017-0153
Keywords: depression, type 2 diabetic mellitus, factors, Ethiopia, psychopathology
Citation: Dukato A, Beyamo A, Habte Hailegebireal A, Teklehaimanot WZ, Ayfokru A, Alemnew M, Birhanu Abate D, Abemie W, Mengistu BT, Ayehu Dessie Y, Mengstie LA and Girma B (2024) Depression and associated factors among patients with type 2 diabetic mellitus in Ethiopia: a cross sectional study. Front. Psychiatry 15:1454087. doi: 10.3389/fpsyt.2024.1454087
Received: 24 June 2024; Accepted: 02 October 2024;
Published: 30 October 2024.
Edited by:
Samantha Ramkisson, KZN Department of Health, South AfricaReviewed by:
Komal Chawla Verma, Chitkara University, IndiaCopyright © 2024 Dukato, Beyamo, Habte Hailegebireal, Teklehaimanot, Ayfokru, Alemnew, Birhanu Abate, Abemie, Mengistu, Ayehu Dessie, Mengstie and Girma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bekahegn Girma, QmVrYWhlZ25nQGR1LmVkdS5ldA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.