- 1Institute for Development, Research, Advocacy, and Applied Care (IDRAAC), Beirut, Lebanon
- 2Department of Psychiatry and Clinical Psychology, Saint George University of Beirut, Beirut, Lebanon
- 3Department of Psychiatry and Clinical Psychology, St George Hospital University Medical Center, Beirut, Lebanon
- 4Research Department, Ipsos SAL, Beirut, Lebanon
Objective: This study examines the national prevalence of mental health disorders and their associated factors in Lebanon, specifically in the aftermath of the 2020 events, including the catastrophic events of Beirut blast and the concurrent financial meltdown amid the global pandemic.
Methods: Conducted between July and September 2022, the study interviewed a nationally representative sample of 1,000 Lebanese via telephone, using the Computer Assisted Telephone Interview (CATI) system. Gender-specific bivariate and multivariate models were generated for probable posttraumatic stress disorder (PTSD), depression, and anxiety.
Results: High rates of mental health disorders emerged — 47.8% screened positive for probable depression, 45.3% for probable anxiety, and 43.5% met the probable diagnosis for PTSD. Multivariate gender-specific analyses revealed no significant associations with governorate, employment status, or marital status, while the financial composite score consistently influenced all disorders.
Conclusion: Lebanon faces a severe mental health crisis, evidenced by elevated rates of probable depression, anxiety, and PTSD. The universal impact of multiple traumas transcends typical determinants, emphasizing the need for nuanced interventions and targeted policy considerations.
1 Introduction
In recent years, Lebanon, now a lower-income Middle Eastern country, has experienced its worst combination of crises in history. In 2020, the Lebanese were concomitantly hit by a dual internal trauma: the financial meltdown and the Beirut Port Blast. The Beirut Port Blast was the largest non-nuclear blast recorded in modern history and resulted in many fatalities and thousands of destroyed dwellings and displaced families (1). Moreover, in 2020 the value of the Lebanese currency started deteriorating and by 2022 it lost more than 98 percent of its pre-crisis value with an average inflation of 171.2%—one of the highest rates globally (2). Both these traumas happened concurrently during the COVID-19 pandemic.
These multifaceted challenges have not only inflicted immense losses on the material front, but they have also given rise to a pressing concern—mental health disorders. When countries experience major adversities, including economic crises and disasters, mental health disorders become more pronounced and impede any recovery on the individual and societal levels (3–5). In the aftermath of disasters, whether natural or man-made, the rates of mental health disorders increase both within and outside the immediate vicinity of the trauma (5). In 2014, China experienced a series of Ammonium Nitrate explosions, which led to injuries and significant loss of life (6). Among the 2,395 participants directly exposed to the explosion, nearly 17% displayed symptoms of moderate to severe PTSD (7). In the United States, after the September 11 terrorist attack, a nationally representative cross-sectional study surveyed 2,273 adults found that PTSD affected individuals both directly impacted by the attack and those residing outside of New York. The prevalence of PTSD was 11.2% in New York, 2.7% in Washington, 3.6% in major metropolitan areas, and 4.0% in the rest of the country—one to two months after the attacks (8). The far-reaching effect of trauma was further underscored in a longitudinal study that revealed an incidence of 17% of probable PTSD among individuals residing outside New York two months after the attacks (9).
In parallel to the Beirut Port Blast, Lebanon was witnessing a financial collapse. The literature is rich with evidence of how such events can exacerbate mental health disorders. For example, following the recession of 2008 in Hong Kong, there was a rise in major depressive episodes (MDEs) that reached 20.1% among individuals with significant investment losses (10). Similarly in 2009, the economic recession in Greece resulted in a twofold increase in MDEs of the nationally studied population (11). Meanwhile, in Venezuela, a country grappling with a severe economic crisis, individuals with poor and extremely poor socioeconomic status were respectively 2.0 and 2.8 times more likely to exhibit anxiety symptoms, and 2.5 and 4.4 times more likely to display depressive symptoms compared to those with higher socioeconomic status (12). These findings offer significant insights into the mental health situation in Lebanon, shedding light on the potential challenges the country has faced, particularly in the aftermath of the banking crisis, which experts have likened to a Ponzi scheme (13, 14).
Concurrent with these events, as of August 21, 2022, COVID-19 has had a profound global impact, registering 593 million confirmed cases and 6.4 million reported deaths worldwide (15). Beyond the physical health toll, the literature consistently underscores the pandemic’s profound impact on global mental health, manifesting in heightened rates of anxiety and depression. For instance, PHQ-9 depression rates surged from 8.5% pre-pandemic to 27.8% post-pandemic in the United States (16). This trend was evident also in many other areas such as Peru, where depression scores quintupled from 6.4% in 2018 to 35% in 2020 (17). Other national studies echo these findings, with anxiety rates reaching up to 27.8% in Mexico by 2020 (18).
Given the unique situation in Lebanon, many have suspected that the mental health of the Lebanese to be severely affected (19). Unfortunately, to date, we do not have nationally representative studies that have explored this complex landscape. The only studies at our disposal are either collected their data through convenient samples from social media (20, 21), or investigated mental health outcomes within small, restricted subpopulation groups such as university students (22) or hemodialysis patients (23). None of the studies we are aware of evaluated the mental health of the Lebanese population on a national level. The latest nationwide study of this kind was conducted in 2006 in the context of the World Mental Health survey project (24) well before the calamities converged in the country. The 2006 surveys were face-to-face interviews utilizing the Composite International Diagnostic Interviews (CIDI), a well-known established fully structured diagnostic interview to assess disorders and treatment. They have contributed in shaping the mental health strategy of the country and served as benchmarks for many other studies in the region as evidenced by their application in Iraq, Qatar, and Saudi Arabia (25–27).
To bridge this gap in the literature, the current paper aims to describe the prevalence of mental health disorders, including probable depression, anxiety, and PTSD, in Lebanon and their associated correlates. Data was collected through telephone interviews using a nationally representative sample in the aftermath of the double assault of the Beirut Port Blast, the economic collapse during the prevailing COVID-19 pandemic. Although telephone interviewing as a research method is often met with skepticism, several studies have demonstrated its high reliability and effectiveness. When compared to traditional face-to-face interviews, telephone interviews have shown significant agreement in assessing various psychiatric disorders and mental health conditions (28–31). For instance, research has revealed excellent agreement for anxiety disorders, very good agreement for major depressive disorder, and alcohol/substance use disorders, and no significant differences in outcomes when using identical questionnaires for both telephone and face-to-face interviews (28, 32, 33).
2 Materials and methods
2.1 Sample
This study is a collaboration between IDRAAC, the research section of Saint George University Medical Center (SGUMC) and the global market research and consulting firm, Ipsos SAL. It aims to estimate the prevalence of mental health disorders and their associated factors within a nationally representative sample of Lebanese adults (18+) in the aftermath of the multiple co-occurring stressors in Lebanon including the Beirut Blast and Lebanese financial meltdown during the global pandemic. To achieve a nationally representative sample of the Lebanese population, we used the most recent Central Administration of Statistics report published by the Ministry of Public Health of Lebanon in 2019 which was completed in 1932 (34), to reach proportional representation of the gender and governorate within our sample. We utilized Ipsos’ proprietary database and employed the Computer Assisted Telephone Interview (CATI) system for the random selection of our representative sample. Accordingly, a total of 1,000 final participants were included in our study. Informed verbal consent was obtained before conducting interviews. These procedures were approved by the Institutional Review Board (IRB) committee of the Saint George Hospital University Medical Center, Faculty of Medicine, Lebanon. Grammar correction and language refinement for this manuscript were conducted using OpenAI's GPT-3.5, a generative AI technology accessed in January 2024 via the ChatGPT platform. The tool was employed solely to enhance the manuscript's clarity and readability.
2.2 Interviews
Interviews were held over the phone between July and September of 2022 by Ipsos’ team which come from a reputable outfit with a very long and well-established history of conducting phone interviews. To maintain meticulous record-keeping, all calls were systematically recorded, documenting interview outcomes, whether completed or not, responses or lack thereof, postponements, and other relevant metrics. Our study successfully interviewed a final sample of 1,000 participants, allowing for a margin of error of 5%. The average interview duration was approximately 15 minutes. Of the attempts made, 2,257 individuals did not respond to the call, 291 requested a callback, 611 encountered busy phone lines, 24 had their phones switched off, 168 declined to participate, and 6 exceeded the quota in case of no answer, three attempts were made before refraining from calling the number again. Additionally, 38 individuals did not complete the interviews, and 95 expressed a preference for a later appointment. Notably, 495 phone numbers were disconnected.
2.3 Enumerator training & quality control
Prior to data collection, enumerators and supervisors underwent rigorous training by Ipsos with regular feedback from IDRAAC. The program covered key aspects such as understanding study objectives, proficiency in administering components like the screener and questionnaire, familiarity with data collection protocols, adherence to ethical guidelines, strategies for respondent engagement, and effective handling of survey materials and equipment. To ensure data integrity, an internal quality control system which involved a systematic review of interview recordings to evaluate the quality and adherence to established protocols. Furthermore, to achieve external quality control, two researchers from IDRAAC reviewed a random subset of recordings using metrics that evaluated consistency (i.e., whether the interviewer read each question as it is), clarity (i.e., whether the interviewer repeated the question upon demand), and completeness (i.e., whether the interviewer read the introduction fully). The comprehensive revision confirmed the accuracy of the recordings and upheld the data integrity standards of our study.
2.4 Measurement
Our study builds upon the Ipsos international study that delved into public health concerns in 34 countries (35). While their investigation primarily addressed attitudes towards various government services, our team introduced additional questions encompassing demographic variables (age, gender, marital status, place of residence, and employment status) alongside an exploration of the impact of Lebanon’s economic situation on respondents. Moreover, we also included scales to evaluate the prevalence of probable PTSD secondary to the Beirut Port Blast, anxiety, and depression. The selection of questions underwent a meticulous process led by our research team. Below is a breakdown of the scales and scores added to the survey.
2.4.1 PCL-5 (PTSD checklist for DSM-5)
To determine probable PTSD prevalence following the Beirut port explosion, we used the PTSD Checklist for DSM-5 (PCL-5), 20-item self-report questionnaire rating symptoms from 0 (not at all) to 4 (extremely) as per DSM-5 criteria (36). Symptoms rated moderately (2) or higher were endorsed. A DSM-5 proxy diagnosis requires meeting specific criteria: 1 item from Intrusion (B), 1 from Persistent Avoidance (C), 2 from Negative Alterations in Cognitions and Mood (D), and 2 from Arousal and Reactivity (E).
2.4.2 GAD-7 (generalized anxiety disorder questionnaire)
To determine probable anxiety prevalence, we used the General Anxiety Disorder (GAD) questionnaire consisting of 7 items to evaluate recent symptoms. Each question received a rating from 0 (not at all) to 3 (nearly every day). Participants’ scores on the 7 questions were summed, resulting in a total score ranging from 0 to 21. Based on this continuous score, participants were categorized into two groups: those without anxiety (total score < 8) and those screening positive for anxiety (total score ≥ 8). This cutoff, as determined by Plummer et al. (37), has an 84% specificity and 83% sensitivity.
2.4.3 PHQ-9 (patient health questionnaire for depression)
To determine the prevalence of probable depression, we used the PHQ-9, a 9-item tool that explores respondents’ experiences over the preceding two weeks. Each question is assigned a score from 0 to 3, where 0 signifies “not at all” and 3 denotes “nearly every day.” After summing the 9 items of PHQ-9, a total score ranging from 0 to 27 is obtained for each participant. A cut-off score of 10 was used for PHQ-9, which yields a specificity of 0.89 and a sensitivity of 0.85 (38).
2.4.4 Composite financial score
To assess economic conditions, a composite score was derived from six variables, including income rank, monthly surplus, financial security, financial strain during gift-giving occasions, basic lifestyle changes, and leisure lifestyle changes. Variable codes were recoded to generate a composite score, with values ranging from 0 (favorable economic situation) to 17 (unfavorable economic situation). The variable codes were changed (recoded values are present in the Supplementary Materials S1).
2.5 Statistical analysis
The analyses conducted for this study were gender-specific, ensuring a nuanced exploration of outcomes. Frequencies and percentages were calculated for categorical variables, while means and standard deviations were computed for continuous variables. The bivariate level analysis involved Chi-squared tests for categorical variables and t-tests for continuous variables.
Following the initial analyses, multivariate analyses were conducted for each outcome variable, namely probable PTSD, depression, and anxiety, within the context of gender specificity. Variables showing significance at the bivariate level were included in the respective models. Additionally, 95% confidence intervals were calculated for these multivariate analyses, providing a range of plausible values for the observed effects. The analyses were performed using STATA version 13.
3 Results
3.1 Sample characteristics
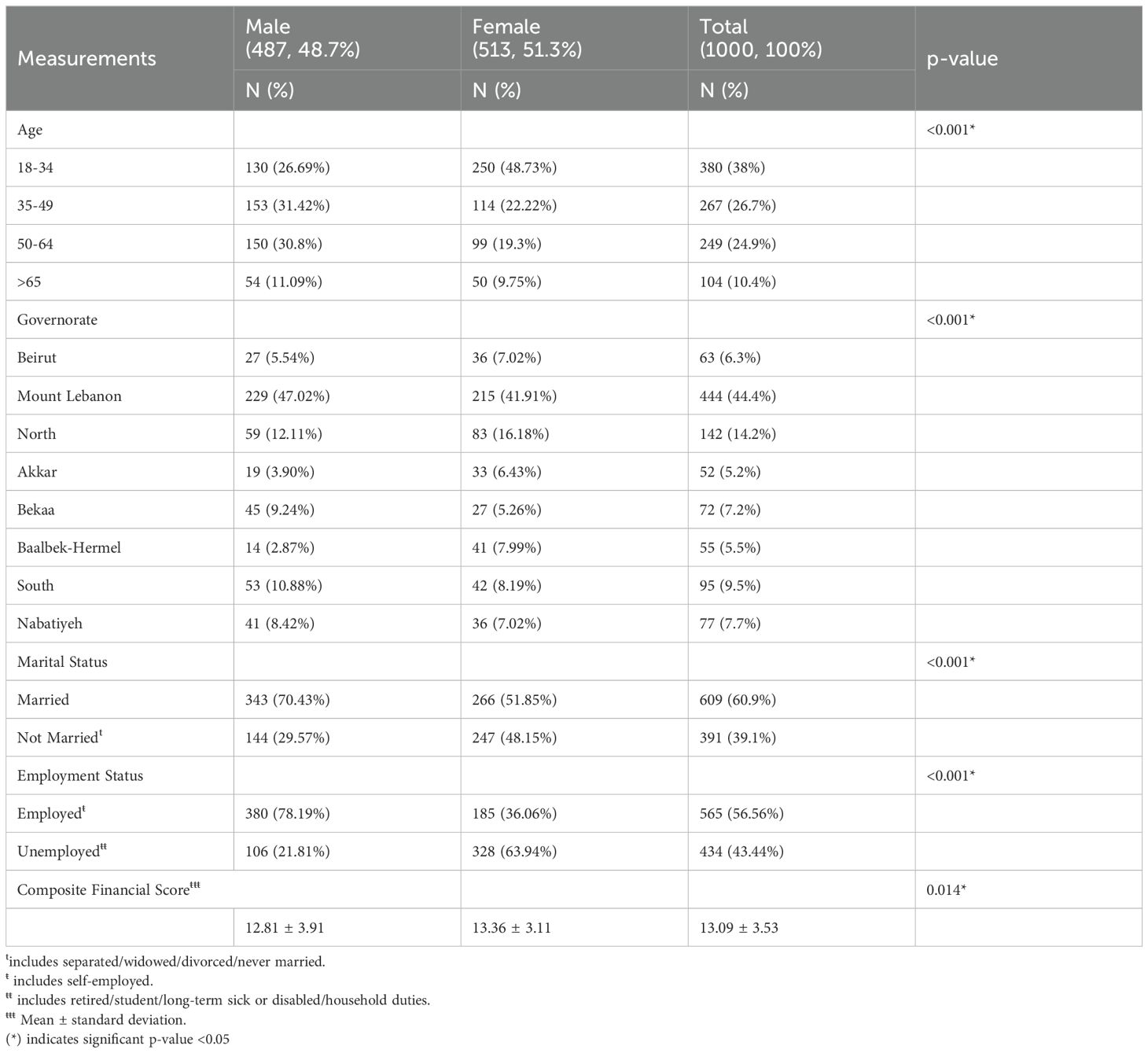
Table 1 provides a comprehensive overview of the socio-demographic characteristics of our study sample. Females constituted approximately half of the participants (51.3%), with a predominant presence in the 18 to 34-year age range (48.7%). The majority of individuals were married (Overall: 60.9%, Males: 70.3%, Females: 51.85%). Employment patterns varied between genders, with a higher percentage of employed men (78.19%) compared to employed women (36.06%). Geographically, Mount Lebanon had the highest representation at 44.4%, followed by the North (14.2%), the South (9.5%), Beirut (6.3%), and other regions. The total sample exhibited a mean composite financial score of 13.09 ± 3.53, with females scoring slightly higher (13.36 ± 3.11). For a detailed breakdown of the gender distribution of the sociodemographic features in our sample, please refer to Table 1.
It is important to point out that our study’s data closely mirrors the latest Lebanese population census published by the Central Administration of Statistics (34), which assures a representative snapshot of the country’s demographic at the level of governorate and gender separately. This alignment validates the broad applicability of our findings to the general Lebanese population.
3.2 Prevalence and comorbidities
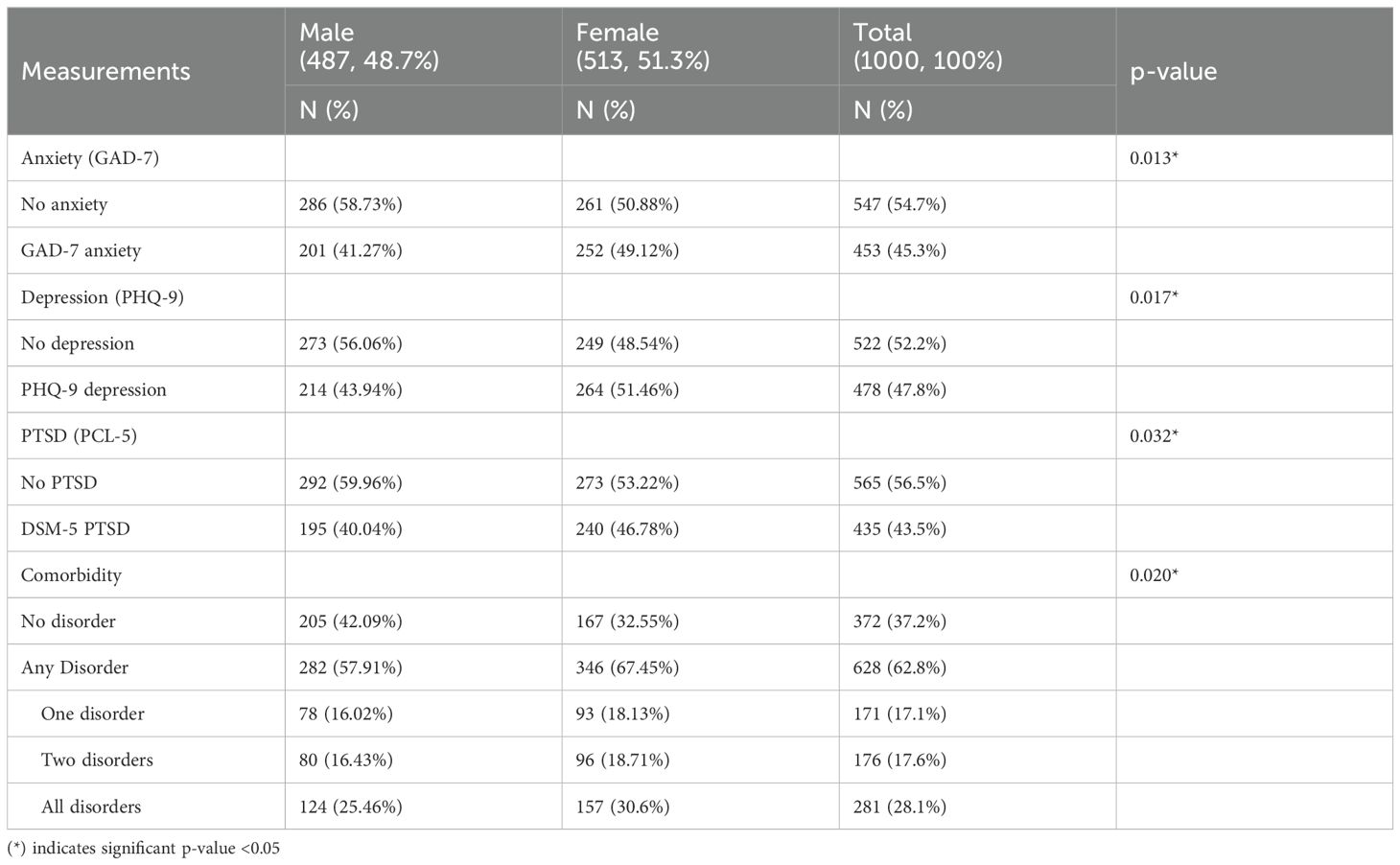
Mental health disorders were prevalent among the study participants, as detailed in Table 2. Notably, 45.3% exceeded the threshold on the GAD-7 probable anxiety scale, showing gender disparities (49.12% of females and 41.27% of males; p-value=0.013). Similarly, 47.8% scored above 10 on the PHQ-9 depression scale, with variations between genders (51.46% of females and 43.94% of males; p-value=0.017). Furthermore, 43.5% met the probable diagnosis criteria for probable PTSD, with gender-specific prevalence (46.78% of females and 40.04% of males; p-value=0.032). These mental health disorders exhibited significant gender differences.
Table 2 also illustrates the intricate interplay of these disorders within the general sample. A substantial 62.8% of participants screened positive for at least one disorder. Notably, 28.10% screened positive for all three disorders, while 17.1% and 17.6% screened positive for one or two disorders alone, respectively.
For a detailed breakdown of comorbidities by gender, refer to Table 2.
3.3 Correlates at multivariate level
In the multivariate analysis (Table 3), we explored the factors associated with probable anxiety, depression, and PTSD across the genders, and our analysis yielded distinct patterns. Variables such as governorate, employment status, and marital status did not exhibit any significant associations with any of the mental health disorders.
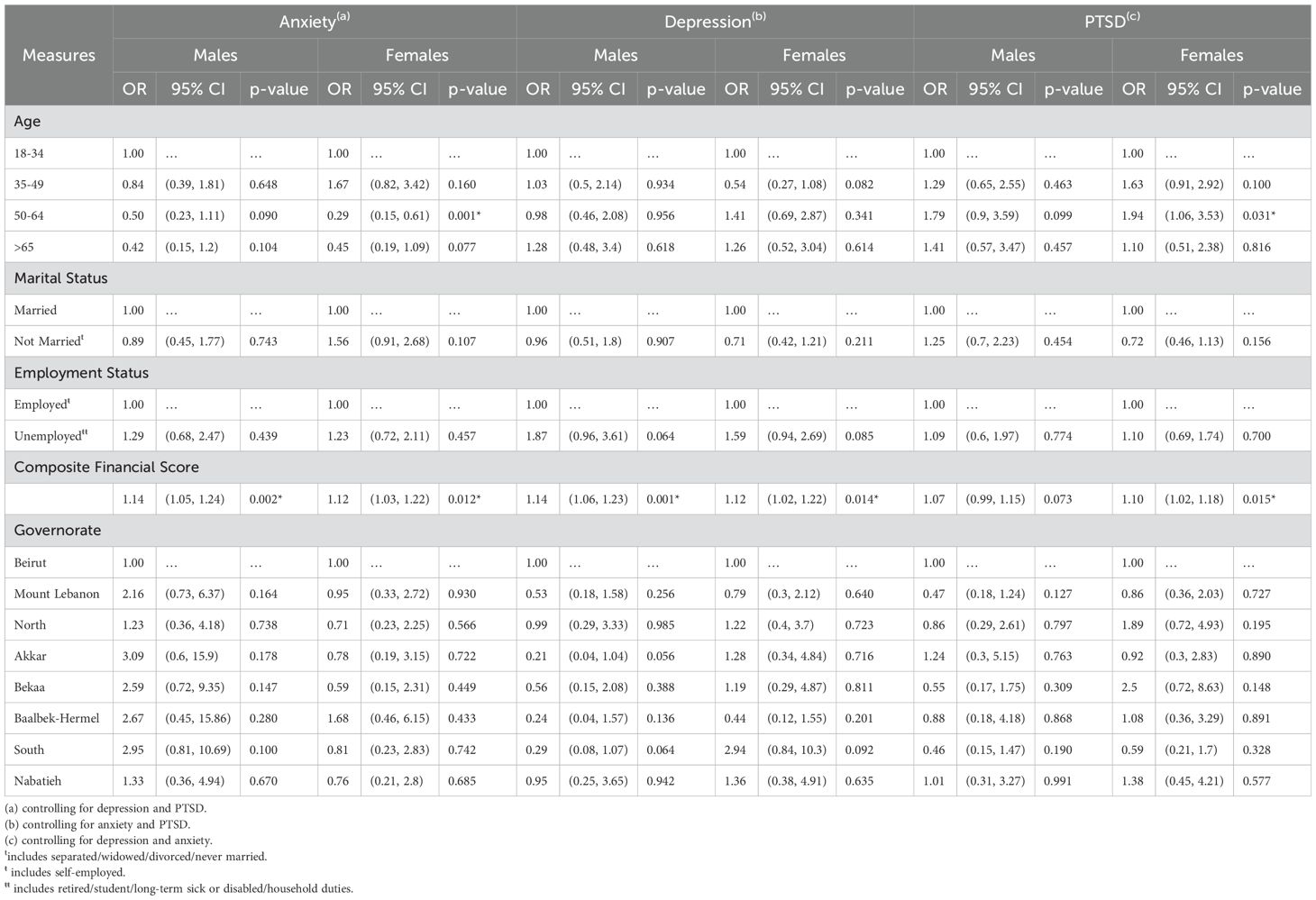
Table 3. Multivariate analyses of anxiety, depression, and posttraumatic stress disorder within the sample population.
Age, on the other hand, showed a distinct association with probable anxiety and PTSD in females aged 50-64 compared to ages 18-34 (OR: 0.29, p-value=0.001; OR= 1.94, p-value=0.031 respectively) while remaining non-significant with other outcomes.
The financial composite score emerged as a consistent factor significantly associated with all three mental health disorders across genders, except for males with probable PTSD: probable anxiety (Males: OR= 1.14, p-value=0.002, Females: 1.12, p-value=0.012), probable depression (Males: OR= 1.14, p-value=0.001, Females: OR= 1.12, p-value=0.014), and probable PTSD (Males: OR= 1.08, p-value=0.073, Females: 1.10, p-value=0.015).
These nuanced findings suggest that, within the specific context of our study, geographic location, employment, marital status, and age may not hold substantial effect over the likelihood of experiencing mental health disorders.
3.4 Perceptions and outcomes
In the supplementary material, we present the results of the associations between participants’ perceptions and probable anxiety, depression, and PTSD while controlling for various relevant variables as shown in Supplementary Table S2. Nearly half the participants in the sample rate the quality of healthcare in the country as poor and very poor, and 54.8% believe that the quality of healthcare will get worse in the upcoming years. Most participants (65.1%) think about their mental wellbeing fairly and very often, and 28.5% think that mental health is more important than physical health.
For probable anxiety, perceiving physical health as more important than mental health at the level of the country was associated with a heightened risk (OR=1.59, p-value=0.032) when compared to perceiving the two as equally important.
For probable PTSD, none of the examined perceptions exhibited a significant association. Probable depression, on the other hand, demonstrated robust associations with various perceptions. Participants anticipating that the quality of healthcare will stay the same (OR=2.15, p-value=0.01) or get worse (OR=1.64, p-value=0.03) in the upcoming years, as opposed to improving, exhibited significant associations with probable depression. Similarly, those who reported thinking about mental well-being fairly often (OR=1.98, p-value=0.04) or very often (OR=1.98, p-value=0.03), in comparison to never thinking about it, were at an increased risk of probable depression. Conversely, believing that physical health is treated as more important than mental health at the level of the country was a protective factor for probable depression (OR=0.61, p-value=0.02) when compared to perceiving mental and physical health as equally important.
4 Discussion
This nationwide telephone interview study aimed to investigate the prevalence, comorbidity, and associated factors of mental health disorders particularly of probable anxiety, depression, and PTSD within a nationally representative sample from Lebanon. Conducted in the aftermath of cataclysmic events, most importantly, the Beirut Port Blast of 2020, a severe financial meltdown in Lebanon, and the COVID-19 pandemic, this study uncovers substantial rates of mental health disorders, indicating a considerable burden on the country’s mental health.
Our study revealed heightened rates of probable depression (47%), anxiety (45%), and PTSD (43%) within the general population. These figures are not surprising given the shocks experienced since 2020. Population shocks, including economic recessions, can increase the rates of mental health disorder (4). Our study’s results align with this evidence, revealing a significant association between deteriorating financial standing and depressive and anxiety disorders. This pattern is observable globally, including in regions such as Greece, Hong Kong, and others, where economic recessions correlated with elevated rates of anxiety and depressive disorders (10, 11, 39).
Moreover, recent reports from the Global Burden of Disease revealed that the estimates of depressive and anxiety disorders have increased in their global incidence (by an average of 27.6% and 25.6% respectively) as a result of COVID-19 pandemic and its ensuing social and economic repercussions (40). Peru serves as a good example, experiencing a fivefold increase in depression rates by 2020 compared to those reported in 2018 (17). This rise in global rates provides further context for the heightened prevalence rates of probable depression and anxiety observed in our sample.
However, when it comes to the high rates of probable PTSD in our sample, the story shifts. The rates observed in our sample do not compare to global estimates of PTSD—which often range between 0.5% and 14.5% across the general population who have suffered from trauma (41). Moreso, our rates do not compare to the rates of probable PTSD in exposed populations of China (17%) following similar Ammonium Nitrate explosions (7).
Our rates do compare to the reported rates across displaced populations of Ethiopians (40.8%), Sudanese (46%), Syrians (32%), and Iraqis (64%) — nations that have weathered multiple episodes of turmoil and unrest (42–44). This suggests a unique impact, potentially stemming from cumulative adversities experienced by the Lebanese population.
Historically, Lebanon’s lifetime prevalence of any mental disorder, as indicated by the LEBANON study (45), stood at 25.8%, falling within the World Mental Health (WMH) surveys’ normal range (12.0% to 47.4%, IQR: 18.1-36.1%) involving 85,052 respondents (46). Today, after the multiple cataclysmic events that have hit Lebanon, we observe an elevated rate of 62.8% for any disorder, surpassing our previous rates, further showcasing the shift in Lebanon’s mental health landscape.
Conventional determinants such as marital status, age, or governorate do not provide a clear explanation for our outcomes. The far-reaching impact of multiple traumas in Lebanon appear to affect individuals universally, irrespective of these typical determinants. A parallel can be drawn with a recent study by Atwoli conducted in South Africa, where conventional sociodemographic factors failed to explain trauma-related rates (47). Similarly, a study on Hurricane Katrina survivors in the US demonstrated that typical socio-economic and demographic associations with PTSD were not observed, highlighting the complex and pervasive nature of trauma’s impact (48).
This study is subject to several limitations, the foremost being the use of telephone interviews instead of traditional in-person household surveys due to financial constraints. It is noteworthy that this methodological choice is not unique to our study but is a pragmatic approach seen in various national studies around the world, validating its reliability in the literature (11, 49, 50). Additionally due to logistical challenges, we were unable to include detailed exposure questions and comprehensive inquiries into participants’ previous mental health history or treatment-seeking patterns. Particularly, we did not ask participants about their substance use which often increases during time of crises.
In conclusion, this study represents Lebanon’s first national study to be conducted on mental health disorders since the WMH in 2006 (24). Our findings revealed elevated rates of mental health disorders in Lebanon, namely probable depression, anxiety, and PTSD till present. There has been a shift since 2006, where low treatment-seeking rates were observed (45). Today, our Lebanese sample shows a substantial 65% recognizing mental health disorders as primary concerns – in contrast to the American Psychiatric Association’s report of only 25% prioritizing mental health in the U.S. by 2024 (51). This growing openness to seeking help for mental health issues underscores the importance of government action to provide comprehensive support at a national level. Furthermore, this study contributes valuable insights into mental health dynamics in Low- and Middle-Income Countries, filling a crucial gap in the existing literature.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://doi.org/10.6084/m9.figshare.25974934.v1.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) committee of the Saint George Hospital University Medical Center, Faculty of Medicine, Lebanon. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because Data was collected through telephone interviews. Consent was obtained verbally.
Author contributions
EGK: Conceptualization, Data curation, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. ME-J: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. RO: Data curation, Investigation, Writing – review & editing. ST: Conceptualization, Data curation, Methodology, Writing – review & editing. GM: Data curation, Project administration, Validation, Writing – review & editing. JB: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge the use of OpenAI's GPT-3.5 for grammar correction and language editing during the preparation of this manuscript in January 2024.
Conflict of interest
Authors ST and GM were employed by Ipsos SAL.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1444245/full#supplementary-material
References
1. Wikipedia. 2020 Beirut Explosion. Wikipedia (2023). Available at: https://en.wikipedia.org/wiki/2020_Beirut_explosion (Accessed January 30, 2024).
2. World Bank. Lebanon: Normalization of Crisis Is No Road to Stabilization 2023. Available online at: https://www.worldbank.org/en/news/press-release/2023/05/16/Lebanon-normalization-of-crisis-is-no-road-to-stabilization (Accessed August 14, 2023).
3. Carpiniello B. The mental health costs of armed conflicts-A review of systematic reviews conducted on refugees, asylum-seekers and people living in war zones. Int J Environ Res Public Health. (2023) 20. doi: 10.3390/ijerph20042840
4. Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. (2016) 16:115. doi: 10.1186/s12889-016-2720-y
5. Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. (2005) 27:78–91. doi: 10.1093/epirev/mxi003
6. Yu M, Lv Q, Ding H, Zeng X, Cao J, Liu J, et al. Evaluation of blast injury patients from the 2015 Tianjin explosions in China. Burns. (2016) 42:1133–40. doi: 10.1016/j.burns.2016.03.004
7. Wei C, Han J, Zhang Y, Hannak W, Liu Z. The characteristics of emotional response of post-traumatic stress disorder and post-traumatic growth among chinese adults exposed to an explosion incident. Front Public Health. (2017) 5. doi: 10.3389/fpubh.2017.00003
8. Schlenger WE, Caddell JM, Ebert L, Jordan BK, Rourke KM, Wilson D, et al. Psychological reactions to terrorist attacks: findings from the National Study of Americans' Reactions to September 11. JAMA. (2002) 288:581–8. doi: 10.1001/jama.288.5.581
9. Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA. (2002) 288:1235–44. doi: 10.1001/jama.288.10.1235
10. Lee S, Guo WJ, Tsang A, Mak AD, Wu J, Ng KL, et al. Evidence for the 2008 economic crisis exacerbating depression in Hong Kong. J Affect Disord. (2010) 126:125–33. doi: 10.1016/j.jad.2010.03.007
11. Madianos M, Economou M, Alexiou T, Stefanis C. Depression and economic hardship across Greece in 2008 and 2009: two cross-sectional surveys nationwide. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:943–52. doi: 10.1007/s00127-010-0265-4
12. González-Rivas J, Iglesias-Fortes R, De Oliveira-Gomes D, Infante-García M, Durán M, Ugel E, et al. High prevalence of anxiety symptoms in Venezuelan adults during the beginning of the Venezuelan crisis. Data from a National Representative Sample. The EVESCAM Study. Res Square. (2022). doi: 10.21203/rs.3.rs-2365599/v1
13. Heller S. The Ponzi Scheme That Broke Lebanon 2022. Available online at: https://www.foreignaffairs.com/articles/Lebanon/2022-04-18/ponzi-scheme-broke-Lebanon:~:text=The%20crisis%2C%20which%20is%20among%20the%20worst%20to,corrupt%20and%20wasteful%20spending%20of%20successive%20Lebanese%20governments (Accessed August 14, 2023).
14. World Bank. Lebanon Public Finance Review: Ponzi Finance (2022). Available online at: http://hdl.handle.net/10986/37824 (Accessed August 14, 2023).
15. World Health Organization. COVID-19 Dashboard 2023. Available online at: https://data.who.int/dashboards/covid19/cases?n=c (Accessed August 14, 2023).
16. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. (2020) 3:e2019686–e. doi: 10.1001/jamanetworkopen.2020.19686
17. Antiporta DA, Cutipé YL, Mendoza M, Celentano DD, Stuart EA, Bruni A. Depressive symptoms among Peruvian adult residents amidst a National Lockdown during the COVID-19 pandemic. BMC Psychiatry. (2021) 21:111. doi: 10.1186/s12888-021-03107-3
18. Galindo-Vazquez O, Ramirez-Orozco M, Costas-Muniz R, Mendoza-Contreras LA, Calderillo-Ruiz G, Meneses-Garcia A. Symptoms of anxiety, depression and self-care behaviors during the COVID-19 pandemic in the general population. Gac Med Mex. (2020) 156:298–305. doi: 10.24875/gmm.20000266
19. Farran N. Mental health in Lebanon: Tomorrow's silent epidemic. Ment Health Prev. (2021) 24:200218. doi: 10.1016/j.mhp.2021.200218
20. Chabbouh A, Fahd G. Beirut blast: post-traumatic stress disorder, depression, & Post-traumatic growth after 6 months. (2022). doi: 10.31237/osf.io/rdwap
21. Maalouf FT, Haidar R, Mansour F, Elbejjani M, Khoury JE, Khoury B, et al. Anxiety, depression and PTSD in children and adolescents following the Beirut port explosion. J Affect Disord. (2022) 302:58–65. doi: 10.1016/j.jad.2022.01.086
22. Mhanna M, El Zouki CJ, Chahine A, Obeid S, Hallit S. Dissociative experiences among Lebanese university students: Association with mental health issues, the economic crisis, the COVID-19 pandemic, and the Beirut port explosion. PloS One. (2022) 17:e0277883. doi: 10.1371/journal.pone.0277883
23. Khoury R, Ghantous Z, Ibrahim R, Ghossoub E, Madaghjian P, Karam E, et al. Anxiety, depression and post-traumatic stress disorder in patients on hemodialysis in the setting of the pandemic, inflation, and the Beirut blast: a cross-sectional study. BMC Psychiatry. (2023) 23:284. doi: 10.1186/s12888-023-04798-6
24. Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S, et al. Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet. (2006) 367:1000–6. doi: 10.1016/S0140-6736(06)68427-4
25. Al-Hamzawi AO, Rosellini AJ, Lindberg M, Petukhova M, Kessler RC, Bruffaerts R. The role of common mental and physical disorders in days out of role in the Iraqi general population: results from the WHO World Mental Health Surveys. J Psychiatr Res. (2014) 53:23–9. doi: 10.1016/j.jpsychires.2014.02.006
26. Khaled SM, Wilkins SS, Woodruff P. Lifetime prevalence and potential determinants of psychotic experiences in the general population of Qatar. Psychol Med. (2020) 50:1110–20. doi: 10.1017/S0033291719000977
27. Altwaijri YA, Al-Habeeb A, Al-Subaie AS, Bilal L, Al-Desouki M, Shahab MK, et al. Twelve-month prevalence and severity of mental disorders in the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1831. doi: 10.1002/mpr.v29.3
28. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatr Pract. (2004) 10:307–13. doi: 10.1097/00131746-200409000-00004
29. Ryan TA, Bailey A, Fearon P, King J. Factorial invariance of the patient health questionnaire and generalized anxiety disorder questionnaire. Br J Clin Psychol. (2013) 52:438–. doi: 10.1111/bjc.2013.52.issue-4
30. Fine TH, Contractor AA, Tamburrino M, Elhai JD, Prescott MR, Cohen GH, et al. Validation of the telephone-administered PHQ-9 against the in-person administered SCID-I major depression module. J Affect Disord. (2013) 150:1001–7. doi: 10.1016/j.jad.2013.05.029
31. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
32. Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. (1997) 154:1593–8. doi: 10.1176/ajp.154.11.1593
33. Evans M, Kessler D, Lewis G, Peters TJ, Sharp D. Assessing mental health in primary care research using standardized scales: can it be carried out over the telephone? Psychol Med. (2004) 34:157–62. doi: 10.1017/S0033291703008055
34. Central Administration of Statistics. Demographic and Social Statistics - Population 2023. Available online at: http://www.cas.gov.lb/index.php/demographic-and-social-en/population-en (Accessed August 14, 2023).
35. Ipsos. Three in five globally say their healthcare system is overstretched 2022. Available online at: https://www.ipsos.com/en/three-five-globally-say-their-healthcare-system-overstretched (Accessed August 14, 2023).
36. Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol Assess. (2018) 30:383–95. doi: 10.1037/pas0000486
37. Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. (2016) 39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005
38. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
39. Aretz B. The short- and long-term effects of the Great Recession on late-life depression in Europe: The role of area deprivation. Soc Sci Med. (2022) 294:114697. doi: 10.1016/j.socscimed.2021.114697
40. Covid- Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/s0140-6736(21)02143-7
41. Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708
42. Teshome A, Chekol Abebe E, Mengstie M, Abdu Seid M, Yitbarek G, Molla Y, et al. Post-traumatic stress disorder and associated factors among adult war survivors in Northwest Ethiopia: Community-based, cross-sectional study. Front. Psychiatry (2023) 14:1083138. doi: 10.3389/fpsyt.2023.1083138
43. Karunakara UK, Neuner F, Schauer M, Singh K, Hill K, Elbert T, et al. Traumatic events and symptoms of post-traumatic stress disorder amongst Sudanese nationals, refugees and Ugandans in the West Nile. Afr Health Sci. (2004) 4:83–93.
44. Ibrahim H, Catani C, Ismail AA, Neuner F. Dimensional structure and cultural invariance of DSM V post-traumatic stress disorder among Iraqi and Syrian displaced people. Front Psychol. (2019) 10:1505. doi: 10.3389/fpsyg.2019.01505
45. Karam EG, Mneimneh ZN, Dimassi H, Fayyad JA, Karam AN, Nasser SC, et al. Lifetime prevalence of mental disorders in Lebanon: first onset, treatment, and exposure to war. PloS Med. (2008) 5:e61. doi: 10.1371/journal.pmed.0050061
46. Kessler RC, Angermeyer M, Anthony JC, DEG R, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. (2007) 6:168–76.
47. Atwoli L, Stein DJ, Williams DR, McLaughlin KA, Petukhova M, Kessler RC, et al. Trauma and posttraumatic stress disorder in South Africa: analysis from the South African Stress and Health Study. BMC Psychiatry. (2013) 13:182. doi: 10.1186/1471-244X-13-182
48. Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. (2007) 64:1427–34. doi: 10.1001/archpsyc.64.12.1427
49. Economou M, Angelopoulos E, Peppou LE, Souliotis K, Tzavara C, Kontoangelos K, et al. Enduring financial crisis in Greece: prevalence and correlates of major depression and suicidality. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1015–24. doi: 10.1007/s00127-016-1238-z
50. Isometsa E, Aro S, Aro H. Depression in Finland: a computer assisted telephone interview study. Acta Psychiatr Scand. (1997) 96:122–8. doi: 10.1111/j.1600-0447.1997.tb09916.x
51. American Psychiatric Association. Making a Mental Health New Year’s Resolution? One in Three Americans Are 2023. Available online at: https://www.psychiatry.org/News-room/News-Releases/Making-a-Mental-Health-New-Year%92s-Resolution-One-i (Accessed December 20, 2023).
Keywords: prevalence, PTSD, depression, anxiety, national study
Citation: Karam EG, El-Jamal M, Osman R, Toukan S, Mouawad GI and Al Barathie J (2025) The aftermath of multiple trauma on a nation: unraveling Lebanon’s unique mental health struggle. Front. Psychiatry 15:1444245. doi: 10.3389/fpsyt.2024.1444245
Received: 05 June 2024; Accepted: 16 December 2024;
Published: 14 January 2025.
Edited by:
Mauro Giovanni Carta, University of Cagliari, ItalyReviewed by:
Massimo Tusconi, University of Cagliari, ItalyFarid Talih, American University of Beirut, Lebanon
Copyright © 2025 Karam, El-Jamal, Osman, Toukan, Mouawad and Al Barathie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elie G. Karam, ZWdrYXJhbUBpZHJhYWMub3Jn
 Elie G. Karam
Elie G. Karam Mariam El-Jamal
Mariam El-Jamal Rayane Osman
Rayane Osman Sana Toukan
Sana Toukan Ghiwa Ishac Mouawad
Ghiwa Ishac Mouawad Josleen Al Barathie1
Josleen Al Barathie1