- 1Department of Pulmonary Diseases, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Division of Pulmonary, Critical Care, Allergy, and Sleep, Department of Medicine, University of California, San Francisco, San Francisco, CA, United States
Objective: The mental health issues of individuals with coronavirus disease 2019 (COVID-19) are currently widespread. Traditional Chinese exercise (Daoyin) plays an important role in relieving patients’ psychological problems. This study aims to assess the efficacy of Daoyin in mitigating mental health issues among individuals diagnosed with COVID-19.
Methods: PubMed, the Cochrane library, Embase, CNKI, Wanfang, VIP database, and SinoMed were searched from their inception to October 2023. Two researchers independently selected the eligible studies. The analysis and presentation of the findings were conducted using Review Manager 5.2 software. The data were analyzed using mean difference (MD), inverse variance, and 95% confidence intervals (CIs).
Results: A total of 12 studies (N = 1291) were included in this study. The results showed that Daoyin can significantly reduce the scores of the Self-Rating Anxiety Scale (SAS: MD = −13.03, 95% CI −19.56 to −6.49, P<.49,yca Self-Rating Depression Scale (SDS: MD = −11.13, 95% CI −14.56 to −7.71, P<.71,sion Pittsburgh Sleep Quality Index (PSQI: MD = −2.00, 95% CI −5.43 to 1.43, P = 0.25), Hamilton Anxiety Scale (HAMA: MD = −2.42, 95% CI −5.25 to 0.41, P = 0.09), and Hamilton Depression Scale (HAMD: MD = −11.17, 95% CI −25.5 to 3.15, P = 0.13).
Conclusion: In COVID-19 patients, Daoyin can alleviate feelings of anxiety and depression, as well as improve sleep quality. The use of Daoyin has no adverse effects and side effects and can reduce the cost of medication. Therefore, Daoyin can be widely promoted. Further research is warranted to analyze the effect of Daoyin on mental health.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/#recordDetails, identifier CRD42023391845.
1 Introduction
COVID-19 has caused global crises in social, economic, and health sectors. Simultaneously, to a considerable degree, it has caused adverse impacts on individuals’ psychological well-being. During the COVID-19 treatment and rehabilitation periods, the mental health status of patients needs to be closely watched. Many COVID-19 patients have anxiety, depression, and sleep disorders, which have a serious impact on their physical and mental health (1–3). The COVID-19 treatment process has been significantly influenced by Traditional Chinese Medicine (TCM). To better help COVID-19 patients recover their physical and mental health, a variety of TCM Daoyin has been used in clinical adjuvant treatment. Daoyin is a form of health maintenance that involves a combination of breathing and limb movements. This practice was known to significantly improve the physical and mental well-being of individuals. Commonly used Daoyin techniques include Baduanjin, Yijinjing, Wuqinxi, and Tai Chi. In recent years, research on Daoyin has mostly focused on mental health problems, such as anxiety, depression, fatigue, and stress (4–6).
Multiple guidelines (7–10) have indicated that the use of TCM Daoyin has significantly contributed to the improvement in psychological recovery among individuals affected by COVID-19. Numerous studies have documented the use of Baduanjin in addressing anxiety, depression, insomnia, lung function recovery, immune system improvement, and physical endurance associated with COVID-19. Through the combination of exercise and breathing, it can effectively relieve anxiety and depression and improve sleep quality and body immunity. At the same time, TCM Daoyin can also promote the flow of energy inside the body, improve the circulation of Qi and blood, relieve fatigue and pressure, and improve the body’s self-healing ability. In summary, TCM Daoyin plays a crucial role in the management of individuals with COVID-19, effectively improving mental and physical recovery. The objective of our research is to thoroughly examine the adjuvant therapeutic impact of Daoyin in individuals suffering from COVID-19. Additionally, we aim to investigate the efficacy and practicality of Daoyin in clinical practice, and furnish more advanced clinical proof for the application of Daoyin.
2 Methods
The study protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42023391845). The study followed the referred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist (11) and Cochrane Handbook (12) guidelines for conducting systematic reviews and meta-analyses.
2.1 Data source and search strategy
We conducted a comprehensive search of several databases, including PubMed, the Cochrane library, Embase, CNKI, Wanfang, VIP database, and SinoMed from their establishment until February 2024. MeSH words and free words or phrases and their abbreviations were used as a search strategy and modified to fit the style of each Chinese and English database. The search terms consisted of two parts (1): COVID-19 (MeSH); 2019-nCoV Infection; SARS-CoV-2 Infection; 2019 Novel Coronavirus Disease; COVID-19 Virus Infection; Coronavirus Disease 2019; (2) Daoyin (MeSH); Traditional Chinese Exercise; Qigong; Gongfa; Baduanjin; BDJ; Yijinjing; YJJ; Wuqinxi; WQX; Tai Ji Quan; TJQ; Taichi; Liuzijue; pulmonary rehabilitation. Additionally, we manually searched for studies from alternative sources that satisfied the inclusion and exclusion criteria but were not included in the aforementioned databases. Two researchers (N.F. Duan and F. Chen) independently selected the appropriate studies. All databases were searched in any language.
2.2 Inclusion and exclusion criteria
2.2.1 Participants
This study exclusively involved individuals diagnosed with COVID-19.
2.2.2 Interventions
Included in the studies were comparisons between Daoyin plus usual care and usual care, regardless of whether blinding was implemented. The Daoyin methods include but are not limited to Baduanjin, Yijinjing, Wuqinxi, Tai Ji Quan, Liuzijue, pulmonary rehabilitation, etc. The defined exclusion criteria consisted of (1) excluding case reports, case series, reviews, editorials, and animal studies; (2) excluding scale results that are not presented as scores; (3) excluding results that do not meet the statistical data format requirements; (4) excluding duplicate publications that report the same results.
2.2.3 Controls
The control interventions solely consisted of usual care. Usual care primarily involves pharmacotherapy, encompassing TCM and antiviral medications, among other interventions (13).
2.2.4 Outcomes
We assessed the main measures of outcomes, which encompassed (1) scores from the Self-Rating Anxiety Scale (SAS) and (2) scores from the Self-Rating Depression Scale (SDS). The secondary outcome measures we evaluated included: (1) Pittsburgh Sleep Quality Index scores (PSQI scores); (2) Hamilton Anxiety Scale scores (HAMA scores); and (3) Hamilton Depression Scale scores (HAMD scores).
2.2.5 Study design
Only Randomized Controlled Trials (RCTs) was considered for inclusion. These studies focused on examining the effectiveness and safety of Daoyin in treating COVID-19 patients with psychological symptoms.
2.3 Data collection, extraction, and evaluation
2.3.1 Study selection
Two researchers (N.F. Duan and F. Chen) individually reviewed the titles and abstracts of the studies that were obtained, assessing them based on predetermined criteria and documenting their judgments accordingly. If a disagreement occurred, it was discussed with another author (W. Zhang).
2.3.2 Data extraction
Two independent researchers (N.F. Duan and F. Chen) examined all the research papers and collected pertinent information based on pre-established criteria. The primary information obtained from the research encompassed the names of the authors, year of publication, geographical location of publication, study design type, method of randomization, case count, age range, method of blinding, criteria for inclusion and exclusion, diagnostic criteria, criteria for evaluating efficacy, methods of intervention, measures of outcome, and duration of treatment. If missing data were found, we contacted the original corresponding author via email to obtain sufficient information. Only one study was included when multiple studies reported the identical trial. If any missing data were discovered, the authors in charge of the correspondence were reached out to via email to provide the necessary information.
2.3.3 Evaluation of the risk of bias
The assessment of bias was conducted based on the following criteria: (1) random sequence generation (selection bias); (2) allocation concealment (selection bias); (3) blinding of participants and personnel (performance bias); (4) blinding of outcome assessment (detection bias); (5) incomplete outcome data (attrition bias); (6) selective outcome reporting (reporting bias); and (7) other biases. Every possible factor that could introduce bias was assessed and categorized as either high, low, or uncertain. High risk is indicated by the color red, unclear risk is indicated by the color yellow, and low risk is indicated by the color green. Data were extracted and bias risk was evaluated by two researchers (N.F. Duan and F. Chen) individually, using the criteria table from the Cochrane Handbook of 2019. If a disagreement occurred, it was discussed with another author (W. Zhang).
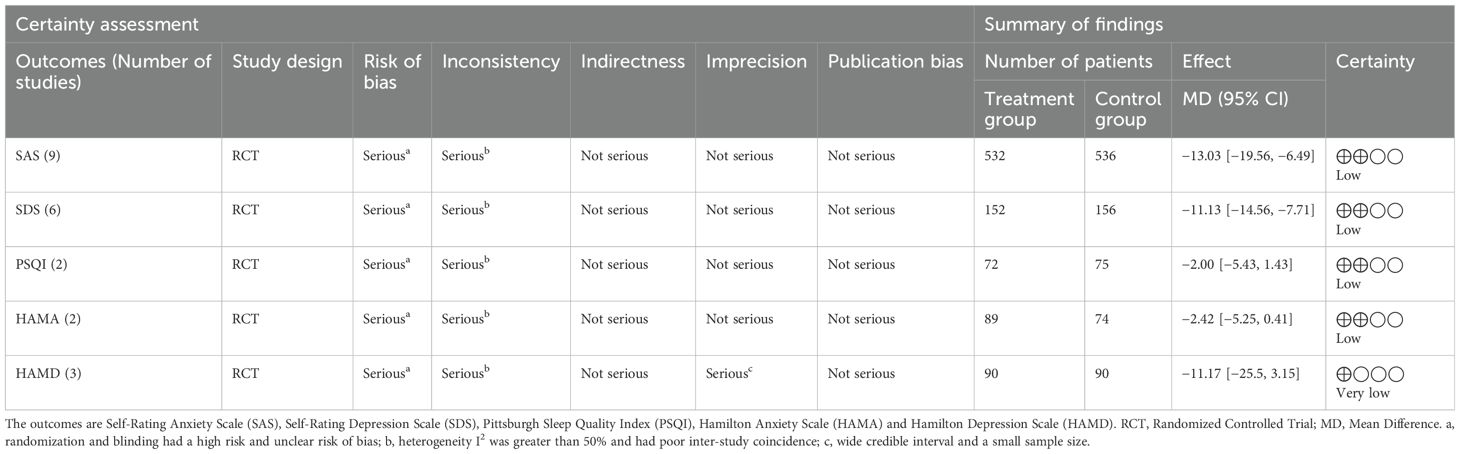
2.4 GRADE evaluation
To evaluate the quality of the evidence, the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system was employed (14, 15). The initial score for the quality of evidence for the RCT was 4 and then downgraded according to the five factors of risk of bias, inconsistency, indirectness, imprecision, and publication bias. The evidence was categorized into four levels of certainty: ‘high’, ‘moderate’, ‘low’, and ‘very low’. Two researchers (Y.L.Li and L.Q.Zhou) conducted the GRADE evaluation on their own and any differences were resolved by a third researcher (G.H.Xu).
2.5 Data synthesis and statistical analysis
The analysis and presentation of the findings were conducted using Review Manager 5.2 software. Continuous variables were determined using mean difference (MD), inverse variance, and 95% confidence intervals (CIs). The range of I2 values was between 0% and 100%, and they were classified as follows: I2 ollows which may not be significant; 30% < I2 0% < i indicating moderate heterogeneity; 50% < I2 0% < g suggesting substantial heterogeneity; and 75% < I2 5% < %, indicating considerable heterogeneity (16). The estimates were combined using a fixed-effect model. Subgroup and sensitivity analyses were used to identify potential sources of heterogeneity. Statistically significant differences were deemed at P-values below 0.05. Subgroup analysis was performed on each Daoyin method. Forest plots are used to present the findings. Publication bias was analyzed using funnel plot and Egger’s analysis.
3 Results
3.1 Literature selection
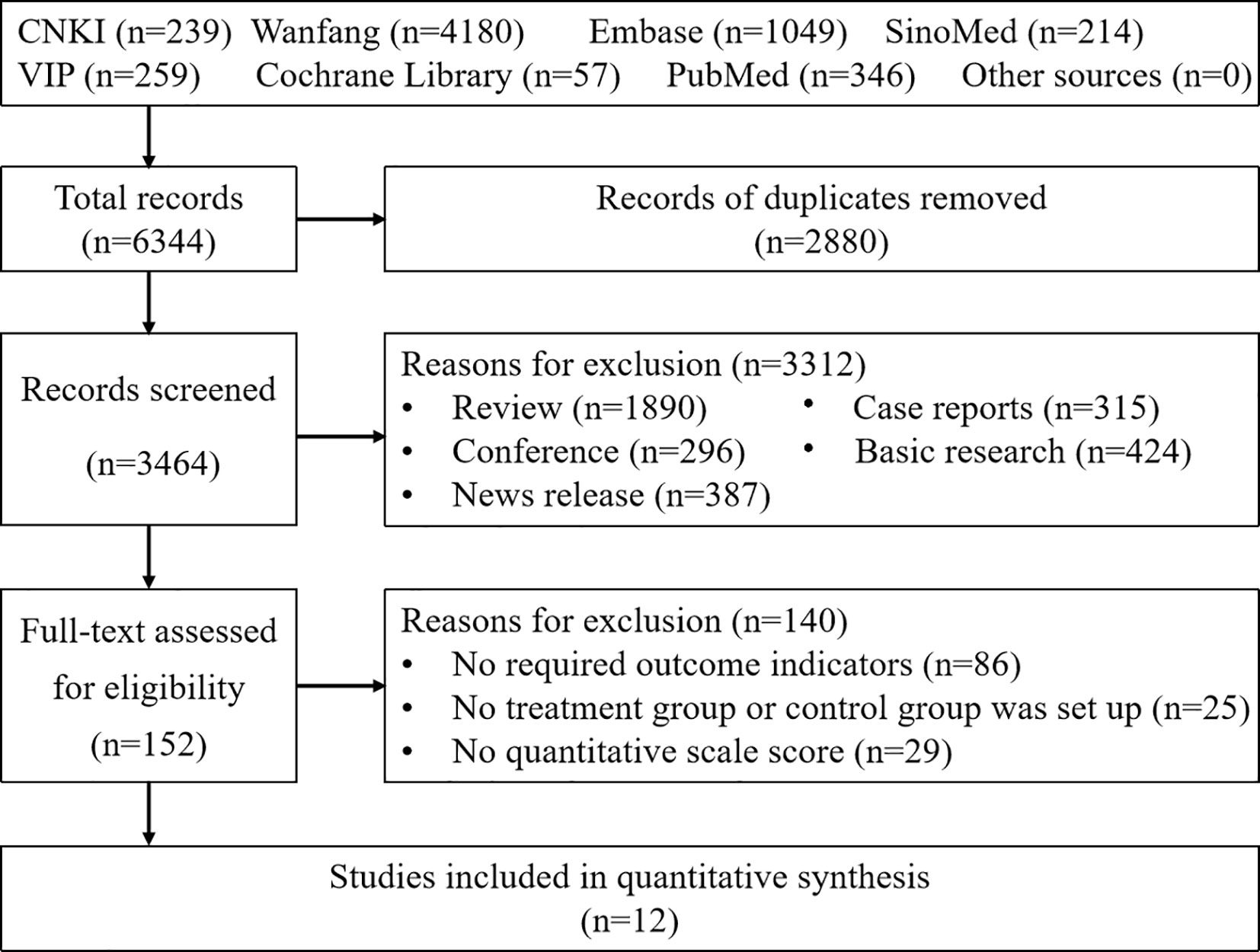
A total of 6,344 articles were retrieved by searching CNKI (239), Wanfang (4180), VIP (259), SinoMed (214), PubMed (346), Embase (1049) and the Cochrane library (57). A total of 2,880 articles were excluded by duplicate checking. After reading the abstract and full text, 3,312 and 140 articles were excluded, respectively. Ultimately, 12 RCTs involving 1,291 cases were included (17–28). The screening process is presented in Figure 1.
3.2 Characteristics of the included studies
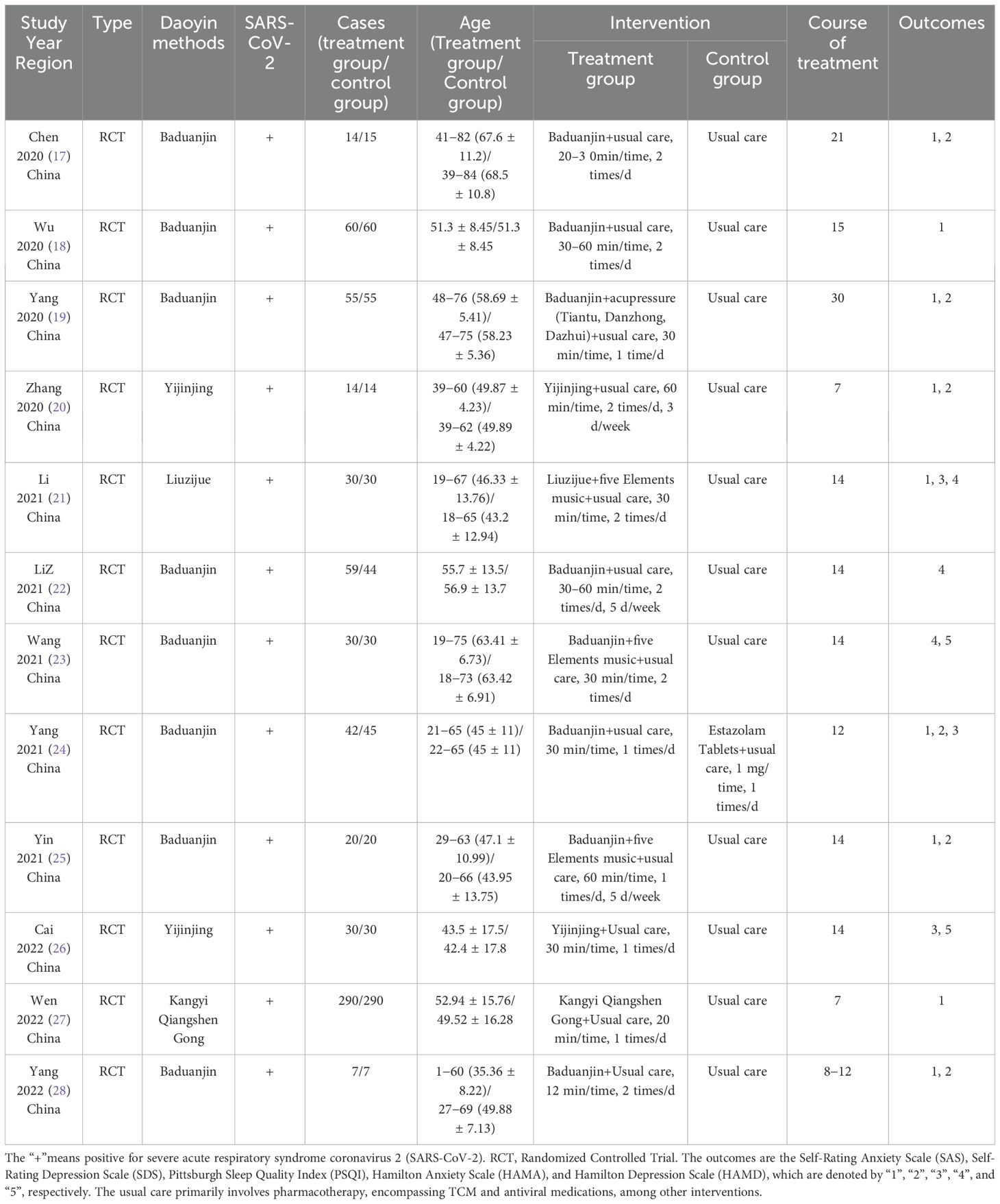
There were 651 and 640 cases in the treatment and control groups, respectively. All the studies were published in China, including four Daoyin methods: Baduanjin, Yijinjing, Liuzijue, and Kangyi Qiangshen Gong. Publication years were between 2020 and 2022. The studies exhibited consistent baseline characteristics. Two researchers independently performed data extraction on the included studies. Table 1 provides a comprehensive overview of the specific attributes of the research.
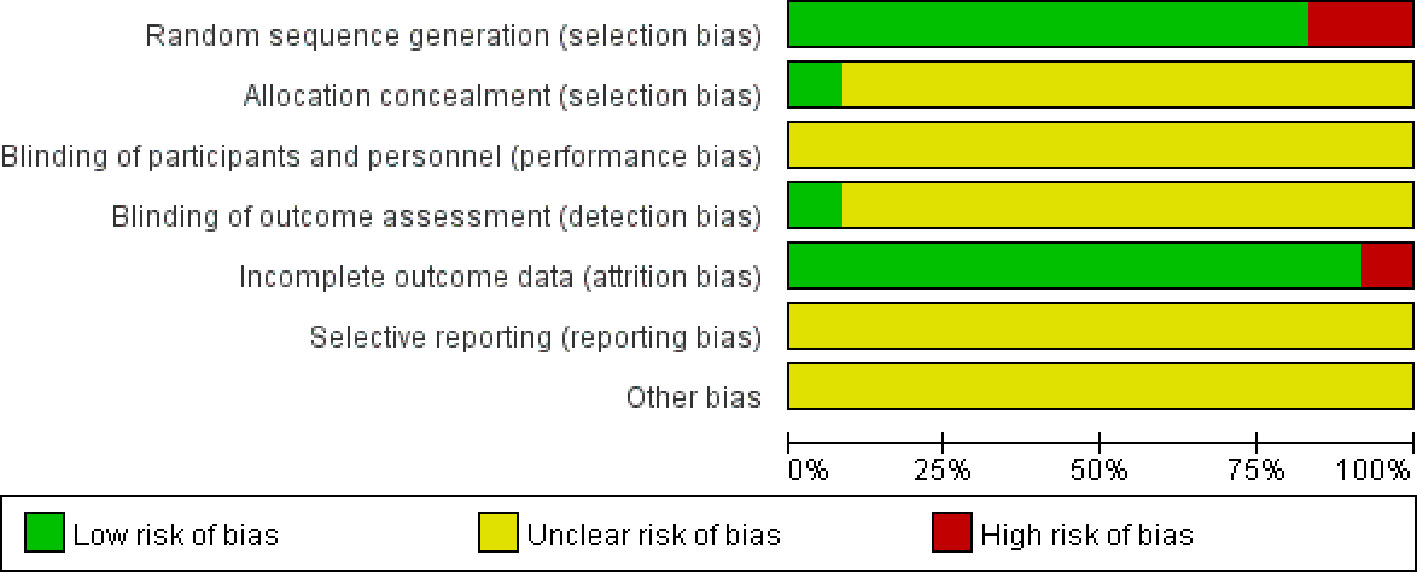
3.3 Risk of bias assessment
The risk bias assessment details for the 12 studies included are depicted in Figures 2 and 3. In the context of random sequence generation, 10 studies employed the randomization method and were assessed as having a low risk of bias, nine of which (17–21, 23, 25–27) used the random number table method and one (24) obtained a random number through a central randomization system. Of the remaining 2 studies, one study did not mention the randomization method (22) and the other (28) was grouped by patient age and gender, which was rated as high risk. In the section pertaining to allocation concealment, one study (24) provided a detailed description of the allocation concealment method, resulting in a low risk rating. A separate study (22) implemented blinding during outcome assessment and was deemed to have a low risk of bias. In the data integrity section, one study (18) reported case shedding without reason and was rated as high risk. For selective reporting and other bias sections, all studies did not mention this section and were rated as unclear risk.
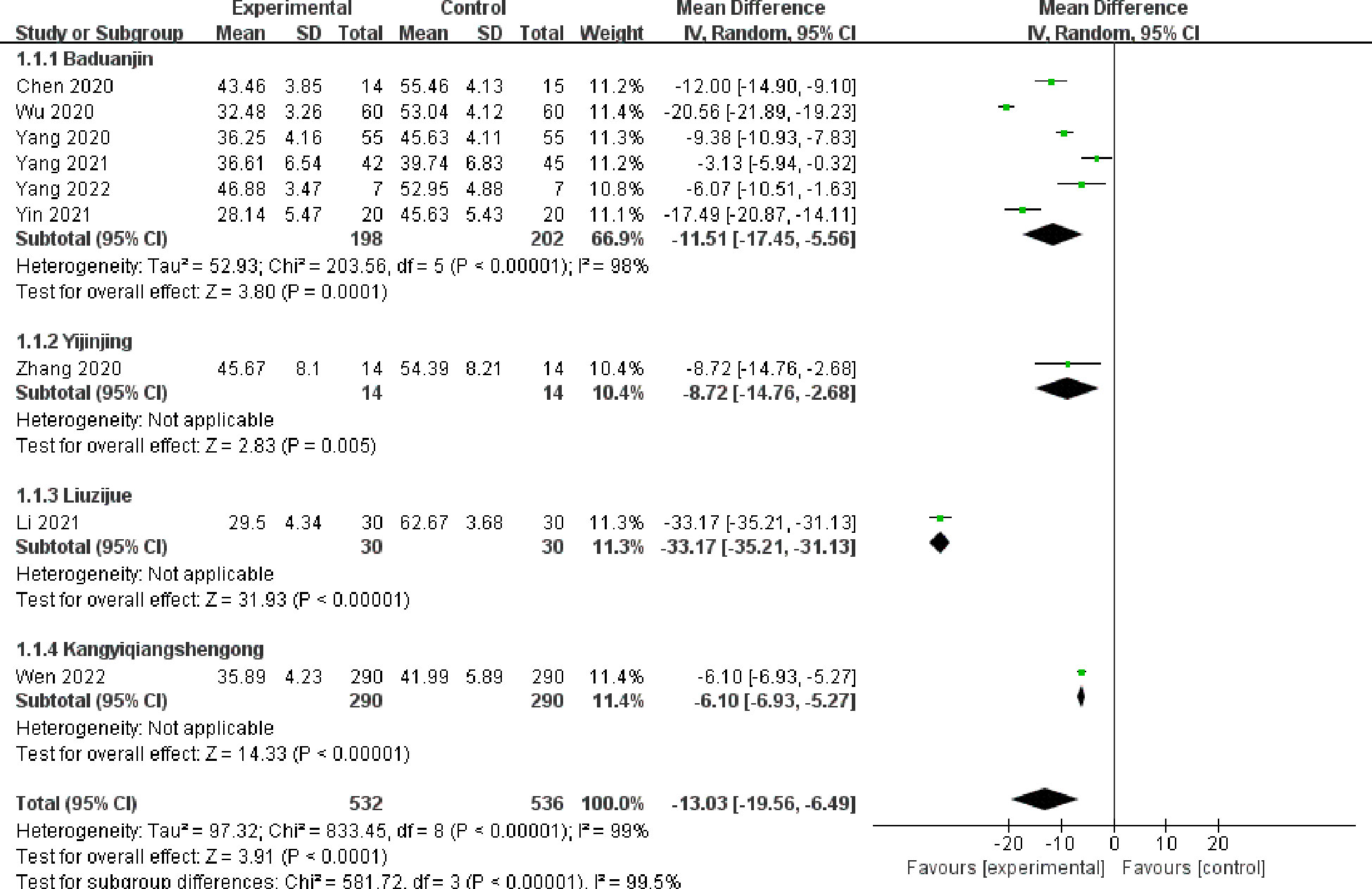
3.4 Primary outcome: SAS
Nine studies (17–21, 24, 25, 27, 28) comprising 1,068 patients evaluated the differences in SAS scores between the Daoyin treatment (532 patients) group and control (536 patients) group (Figure 4). Nine studies including four Daoyin methods: Baduanjin, Yijinjing, Liuzijue, and Kangyi Qiangshen Gong. Among them, six studies used the Baduanjin method. The findings indicated that the integrated Daoyin intervention led to a statistically significant decrease in the SAS score (MD = −13.03, 95% CI: −19.56 to −6.49, P <0.0001). The findings of the heterogeneity test indicated a significantly high level of statistical heterogeneity among the studies (I2 = 99%, P <0.00001), leading to the use of the random effects model for data analysis.
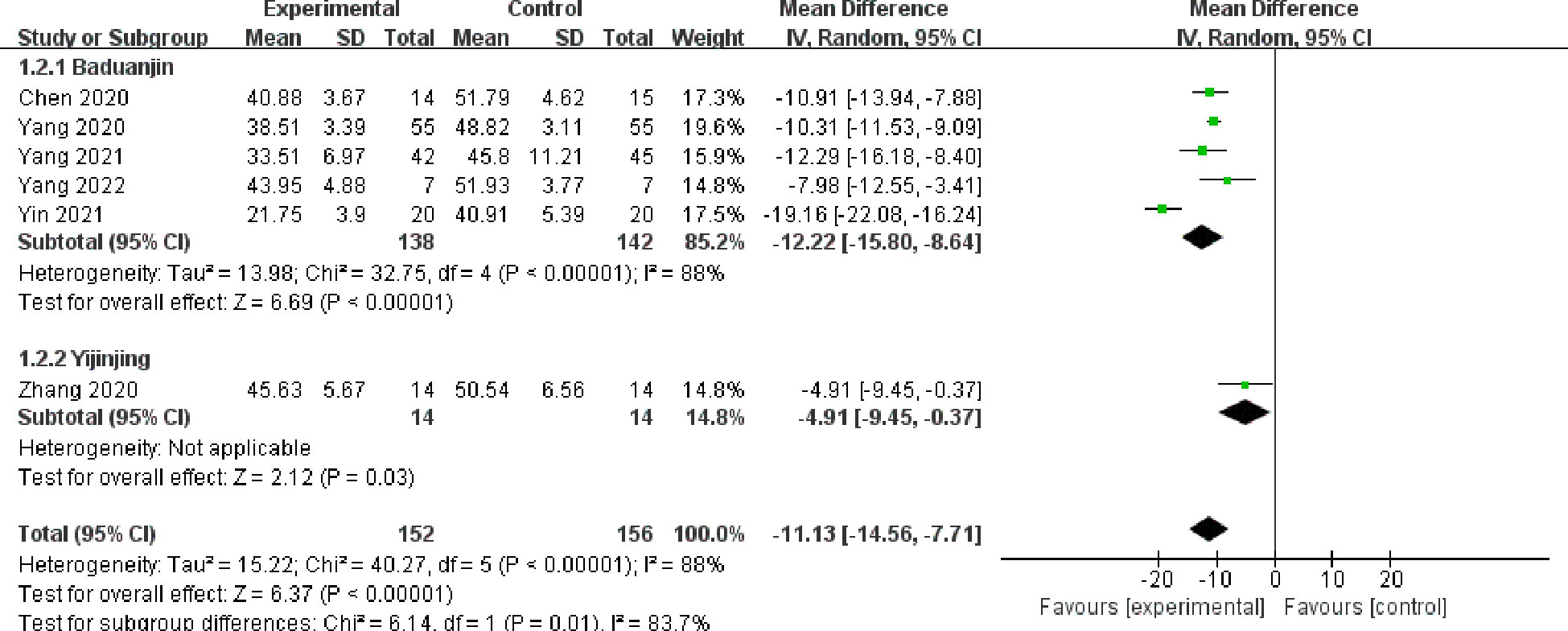
3.5 Primary outcome: SDS
Six studies (17, 19, 20, 24, 25, 28) involving 308 cases reported the changes in SDS scores (Figure 5). There were 152 patients and 156 patients in the treatment and control groups, respectively. Six studies included two Daoyin methods: Baduanjin and Yijinjing. Among them, five studies used the Baduanjin method. According to the findings, the group receiving Daoyin treatment exhibited a significant decrease in SDS scores compared with the control group (MD = −11.13, 95% CI: −14.56 to −7.71, P <0.00001). There was a significant level of heterogeneity (I2 = 88%, P < 0.00001). The data were analyzed using a random effects model.
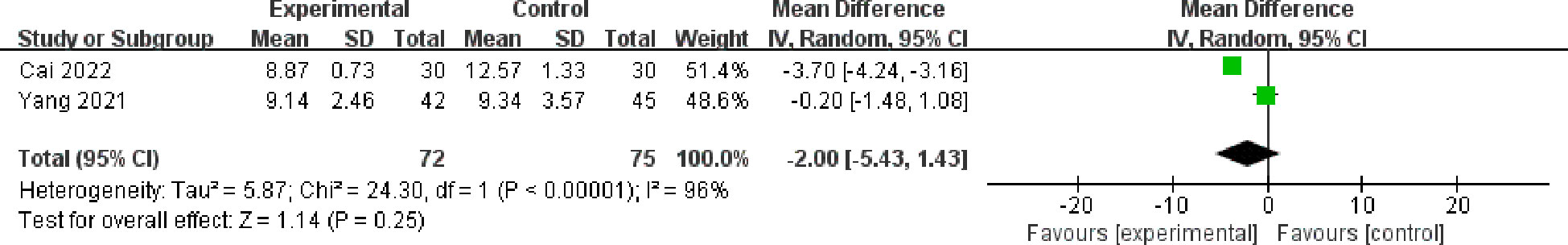
3.6 Secondary outcome: PSQI
Changes in the PSQI scores were assessed in two studies (24, 26) including 147 patients (Figure 6). There were 72 patients and 75 patients in the treatment and control groups, respectively. The results showed that the combined Daoyin intervention could reduce the PSQI scores (MD = −2.00, 95% CI: -−5.43 to 1.43, P = 0.25). Although the results were not statistically significant, there was a trend toward lower PSQI scores. The degree of heterogeneity was found to be substantial (I2 = 96%, P < 0.00001), leading to the use of the random effects model for data analysis.
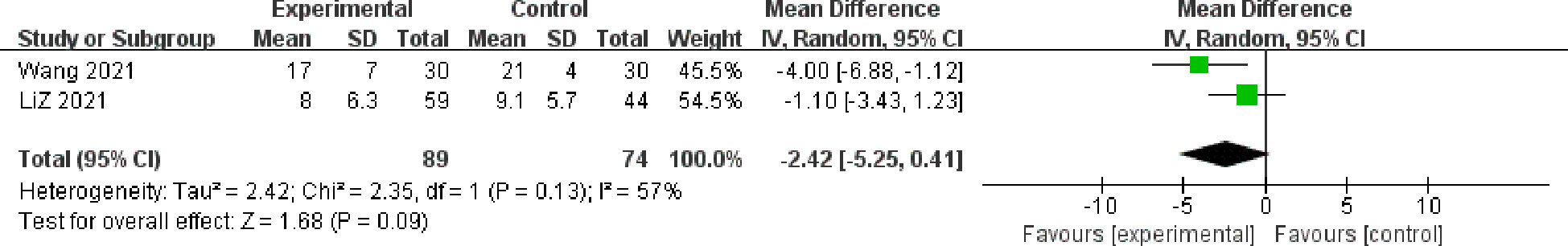
3.7 Secondary outcome: HAMA
Two studies (22, 23) involving 163 cases reported the changes in HAMA scores (Figure 7). There were 89 patients and 74 patients in the treatment and control groups, respectively. The findings indicated that the Daoyin treatment group exhibited a statistically significant reduction in HAMA scores compared with the control group (MD = −2.42, 95%CI: −5.25 to 0.41, P = 0.09). Although the results were not statistically significant, there was a trend toward lower HAMA scores. High heterogeneity was present (I2 = 57%, P = 0.13); therefore, a random effects model was used for data analysis.
3.8 Secondary outcome: HAMD
Changes in the HAMD scores were assessed in three studies (21, 23, 26) including 180 patients (Figure 8). There were 90 patients each in the treatment and control groups. The results showed that the combined Daoyin intervention could reduce the HAMD scores (MD = −11.17, 95%CI: −25.5 to 3.15, P = 0.13). Although the results were not statistically significant, there was a trend toward lower HAMD scores. There was a significant high level of heterogeneity (I2 = 99%, P < 0.00001). The data were analyzed using the random effects model.
3.9 Safety analysis: adverse effects
All studies had no adverse effects during the whole research process.
3.10 Subgroup analysis
Subgroup analysis was performed using different Daoyin methods as classification. For the SAS scores, 6 (17–19, 24, 25, 28) out of 9 studies used Baduanjin. The subgroup analysis results indicated significant heterogeneity among the studies (I2 = 98%, P <0.00001). The remaining 3 studies (20, 21, 27) used the Daoyin methods of Yijinjing, Liuzijue, and Kangyi Qiangshen Gong. Heterogenetic analysis could not be performed due to a single study. There were no subgroup heterogeneous data in these three studies. In term of SDS scores, 5 (17, 19, 24, 25, 28) of 6 studies used the Baduanjin Daoyin method, and heterogeneity was still high (I2 = 88%, P <0.00001).
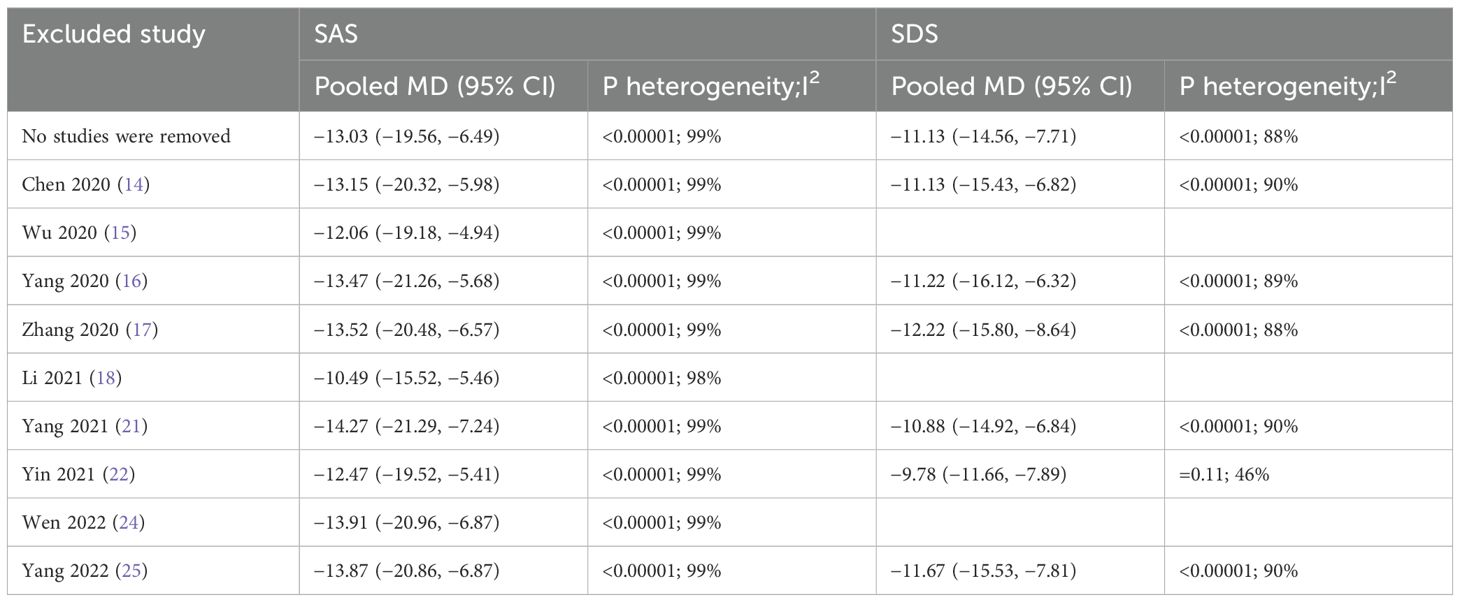
3.11 Sensitivity analysis
Sensitivity analysis was conducted to assess potential sources of heterogeneity through systematic removal of individual studies to observe changes in the data. For the SAS scores, the heterogeneity data remained 99% or 98% after removing the studies individually. There was no significant change observed in the heterogeneity results. For the SDS scores, most heterogeneity data were approximately 90%. When only one study was removed, the heterogeneity data decreased to 46% (details are shown in Table 2).
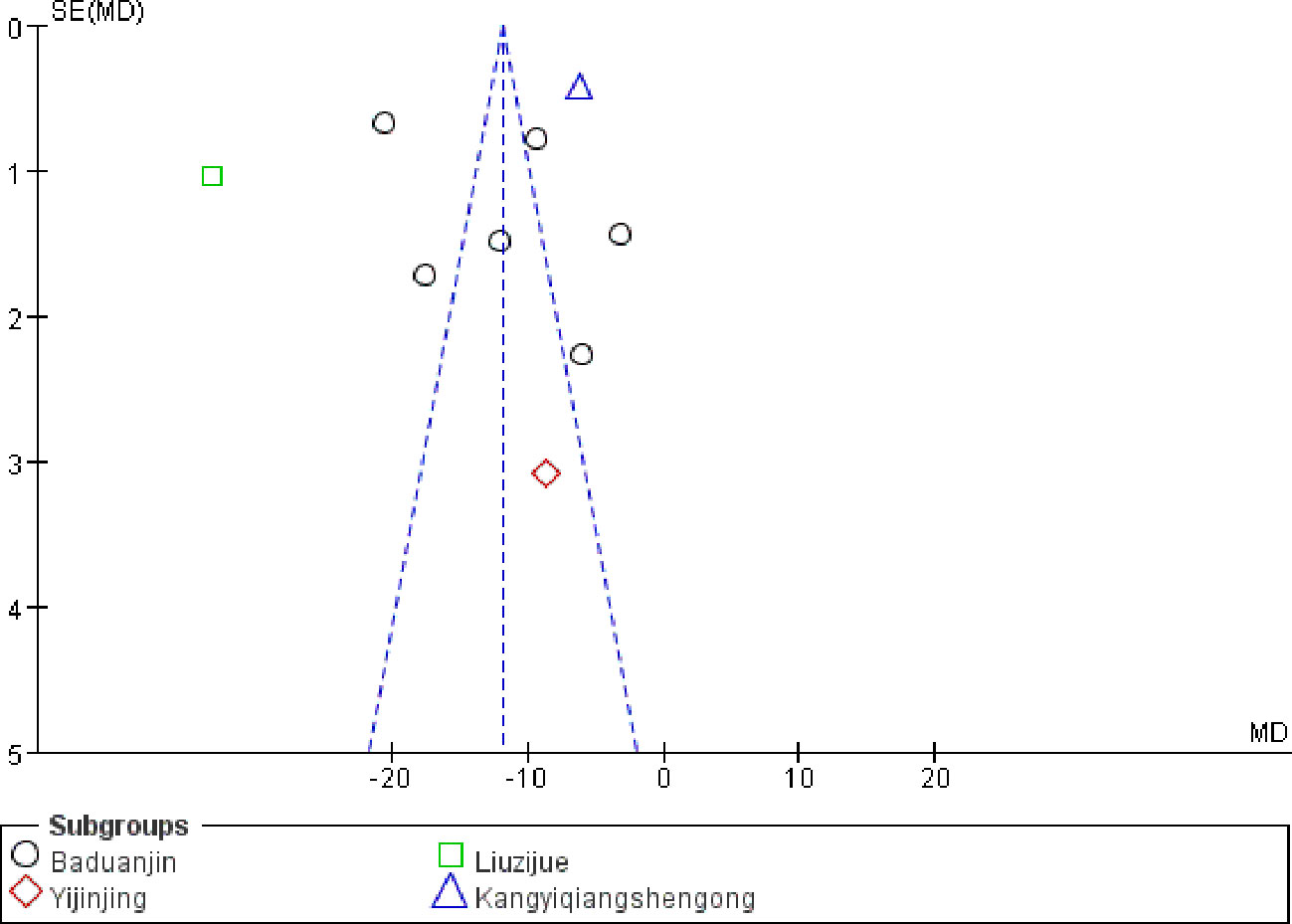
3.12 Evaluation of publication bias
The SAS scores data were used to draw the funnel plot (Figure 9). A total of nine studies (17–21, 24, 25, 27, 28) were included. The symmetrical nature of the figure implies the absence of any discernible publication bias. An Egger’s analysis was further performed (P = 0.086 > 0.05), indicating the absence of significant publication bias.
3.13 Certainty of evidence assessed by the GRADE system
The certainty of evidence was assessed using the GRADE system, with the overall quality deemed to be of low and very low levels (Table 3). The reasons for the potential downgrading of the study’s quality related to the high risk of bias associated with the randomization and blinding methods. For inconsistency, the downgrading was due to all I2 values being greater than 50%, and the forest plot shows a poor overlap. For indirectness, the study population, intervention methods and outcome indicators have good clinical applicability; therefore, it is not downgraded. The reasons for the downgrade were attributed to imprecision, as evidenced by the small sample size and wide range of confidence intervals in the outcome of the HAMD. The remaining outcomes were not downgraded. For publication bias, there was no publication bias such as corporate funding; therefore, it was not downgraded.
4 Discussion
In the present meta-analysis, 12 RCTs involving 1,291 cases were included involving four Daoyin methods: Baduanjin, Yijinjing, Liuzijue, and Kangyi Qiangshen Gong. The results showed a significant reduction in SAS and SDS scores. Although the PSQI, HAMA, and HAMD scores did not demonstrate statistical significance, they did exhibit a significant decreasing trend. The aforementioned findings suggest that Daoyin has a significant impact on the regulation of the mental health and sleep of individuals affected by COVID-19. However, the heterogeneity of the included studies was relatively high. As different Daoyin methods have their own characteristics, this may lead to higher clinical heterogeneity. Therefore, we performed subgroup analysis using different Daoyin methods as groups. The results showed that the subgroup analysis did not significantly reduce the heterogeneity, which may be due to the uneven distribution of the number of cases and the large difference in the improvement of outcome indicators. Following that, sensitivity analysis was conducted and revealed no substantial alteration in the heterogeneity findings, suggesting that the incorporated studies remained relatively stable. We used two methods, funnel plotting and Egger’s analysis, to verify that there was no publication bias in this study. The certainty of evidence was evaluated using the GRADE system, and the overall quality was determined to be low and very low. By integrating these data, the study demonstrated that combined Daoyin treatment can significantly improve anxiety, depression, and sleep status in COVID-19 patients. As a result of the disparate levels of evidence present in the studies that were incorporated, a higher level of evidence is still needed to verify this result.
COVID-19 represents a significant public health crisis characterized by its extensive scope and profound implications. It has a great psychological impact on the patients and can easily cause negative emotions, such as panic and anxiety. Therefore, it is of great significance to explore targeted psychological crisis intervention programs to relieve negative emotions, reduce psychological stress, and maintain a stable attitude. Studies have shown that the literature on the behavioral and psychosocial aspects of the COVID-19 pandemic has been dominated by topics about stress or distress (29). A significant proportion of individuals who had recuperated from acute COVID-19 infection experienced persistent symptoms that significantly impacted their daily functioning and quality of life. These individuals are known as long COVID-19 patients. Even after recovering from the infection, individuals may experience lingering atypical chronic symptoms, such as profound tiredness, breathing difficulty, joint discomfort, cognitive impairment, uneasiness, and sadness for several months, indicating that the fundamental disease pathology continues to exist (30). According to a meta-analysis (31) of 151 studies with 1,285,407 individuals from 32 different nations, a minimum of 50.1% of individuals who recovered from COVID-19 experienced long-term effects within a year following the infection. The most frequent abnormalities were pulmonary CT (56.9%) and lung function tests (45.6%), followed by fatigue (28.7%), depression (18.3%), and post-traumatic stress disorder (17.9%). Based on another meta-analysis (32), fatigue (27.4%) was found to be the most prevalent consequence within 2 years of contracting COVID-19, closely followed by sleep problems (25.1%). The main focus now is to offer suitable measures for prevention and intervention management to reduce the long-term consequences and improve the overall well-being of individuals who have recovered from COVID-19. Our study used the SAS and SDS as the main study indicators. These two scales are used to assess how well individuals feel in terms of anxiety and depression and help people better understand their mental health status. Our study findings indicated that the inclusion of Daoyin therapy can effectively reduce the levels of anxiety and depression experienced by patients. Within the current social background, it can provide a variety of options for the treatment of psychological problems.
A total of 4 Daoyin methods were included in our study, including Baduanjin, Yijinjing, Liuzijue, and Kangyi Qiangshen Gong. The shared characteristic among these Daoyin methods is the integration of respiratory and limb movements, with the goal of preventing and treating illnesses by altering body posture, regulating breathing, and modifying psychological states. Baduanjin comprises eight graceful movements that are relatively uncomplicated and easily mastered, making it a widely accepted instructional method. This exercise routine seamlessly blends soft and firm elements, incorporating both dynamic and static components. Practitioners are encouraged to synchronize their breathing, physical movements, and mental focus to achieve a state of relaxation during physical and psychological workouts (33). One study (34) showed that Baduanjin, as an auxiliary rehabilitation method, can improve psychological and physiological parameters in different age groups and different clinical populations, and effectively improve cognitive function. According to an RCT (35), Baduanjin can decrease depression in individuals without any health issues and increase oxygenated hemoglobin levels in the left prefrontal cortex of the brain. The results suggest that Baduanjin is a beneficial workout for improving executive function and potentially regulating brain activity in individuals who are in good health. One study (36) explored the mechanism of Baduanjin and showed that it alleviates diabetes and depression by regulating the expression of mRNA, lncRNA, and circRNA. KEGG and GO enrichment analysis showed that the pathway mainly focused on immune function and inflammatory response, including the IL-17 signaling pathway and TNF signaling pathway. No further analysis was carried out in the study. Although the mechanism was not fully explored, it provides guidance for the further development of Baduanjin. The aforementioned research indicates that Baduanjin plays a crucial role in the regulation of mental well-being for individuals who are both in good health and those who are unwell. Yijinjing, an ancient Chinese medical practice, encompasses 12 movements and is regarded as a form of complementary and alternative medicine used for maintaining health, providing medical care, and treating diseases. Yijinjing employs a variety of pulling and stretching exercises to promote relaxation of the body’s muscles and joints, ultimately aiming to improve blood circulation, alleviate pain, and reduce fatigue (37). The practice of Yijinjing has been shown to have a positive impact on sleep disorders, fatigue, and overall quality of life in individuals with chronic fatigue syndrome. Additionally, it has been found to be more effective than behavioral cognitive education in reducing pain and increasing vitality (38). The essence of Liuzijue lies in the regulation of exhalation and inspiration through the production of six distinct sounds. The pronunciation of Xu, He, Hu, Si, Chui, and Xi, six words of different mouth, lip, teeth, and tongue force, affect different viscera meridians qi and blood operations (39). Liuzijue is a promising rehabilitation exercise program for discharged COVID-19 patients. Four weeks after the intervention, the patient’s lung function was improved, dyspnea was relieved, and exercise capacity was improved. It can also significantly relieve the state of depression and anxiety (40). Kangyi Qiangshen Gong is a combination of various traditional Daoyin methods, such as Taijiquan, Baduanjin, Yijinjing, and Liuzijue (41). The researchers selected targeted movements from various Daoyin methods and optimized them for patients with clinical symptoms such as dyspnea, chest tightness, fatigue, and cough. Kangyi Qiangshen Gong can improve lung function and immunity and is widely used in the rehabilitation and adjuvant treatment of lung-related diseases (42).
The above studies expressed the significant improvement effect of Daoyin on COVID-19, respiratory diseases, and psychological diseases, and contributed more options for clinical treatment. In comparison with pharmaceutical interventions, Daoyin exercises can decrease healthcare expenditures and alleviate the physical and financial strain on individuals, which deserves wider promotion.
5 Conclusion
To summarize, the existing evidence indicates that Daoyin has a notable impact on alleviating anxiety, depression, and sleep disturbances in individuals suffering from COVID-19. Nevertheless, as a result of the inadequate standard of the studies incorporated in this examination and the findings indicating substantial heterogeneity, there is a need to increase the level of evidence. In the future, it is necessary to conduct additional validation of high-quality well-designed multi-center RCTs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
ND: Writing – review & editing, Writing – original draft, Visualization, Project administration, Conceptualization. FC: Writing – review & editing, Writing – original draft, Visualization, Project administration, Conceptualization. YL: Writing – review & editing, Writing – original draft, Resources, Data curation. LZ: Writing – review & editing, Writing – original draft, Resources, Data curation. XZ: Writing – review & editing, Writing – original draft, Methodology, Formal analysis. GX: Writing – review & editing, Writing – original draft, Investigation, Funding acquisition, Formal analysis. WZ: Writing – review & editing, Writing – original draft, Validation, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by “Clinical research and evaluation of TCM diagnosis and treatment of sudden acute infectious diseases (grant numbers ZXS004R4-2)”, “Based on the “Lung and Intestine are Exteriorly-interiorly Related” theory to study the mechanism of Tanreqing capsule by protecting lung epithelial cells in the treatment of respiratory virus-induced lung injury (grant numbers 22ZR1460100)”, “Shanghai Key Laboratory of Internal Medicine of Traditional Chinese Medicine (grant numbers 20DZ2272200)” and “Zhang Wei Medical Technology Doctor Site Construction-Respiratory therapy Technology Direction (grant numbers A1-N23-204-0405)”.
Acknowledgments
We sincerely thank the Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine for its assistance. Thanks to everyone in the research group for their help.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1422229/full#supplementary-material
Abbreviations
COVID-19, Coronavirus disease 2019; SAS, Self-Rating Anxiety Scale scores; SDS, Self-Rating Depression Scale scores; PSQI, Pittsburgh Sleep Quality Index scores; HAMA, Hamilton Anxiety Scale scores; HAMD, Hamilton Depression Scale scores; TCM, Traditional Chinese Medicine; RCTs, Randomized Controlled Trials; GRADE, Grading of Recommendations, Assessment, Development and Evaluation; MD, mean difference; 95%CI, 95% confidence interval
References
1. Ma C, Yan XK. Research progress in psychological stress response and prevention and control strategies of COVID-19. J Jilin Univ Med Ed. (2020) 46:649–54. doi: 10.13481/j.1671-587x.20200336
2. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. (2021) 397:220–32. doi: 10.1016/S0140-6736(20)32656-8
3. Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun. (2022) 101:93–135. doi: 10.1016/j.bbi.2021.12.020
4. Qiu DR, Lin XL, Zhao JY, Chen XY. Meta-analysis of Baduanjin on the improvement of depressive symptoms. J New Chin Med. (2019) 51:51–4. doi: 10.13457/j.cnki.jncm.2019.06.015
5. Zhang JY, Li Z, Xiao T. A Meta-analysis of the effects of traditional Chinese medicine health exercises on anxiety and depression symptoms in college students. Mod Prev Med. (2021) 48:4324–30.
6. Ye JY. The research frontier and hot spot of the influence of Chinese traditional health practice on mental health. SHNU. (2022), 001582. doi: 10.27312/d.cnki.gshsu.2022.001582
7. Badakhsh M, Dastras M, Sarchahi Z, Doostkami M, Mir A, Bouya S. Complementary and alternative medicine therapies and COVID-19: a systematic review. Rev Environ Health. (2021) 36:443–50. doi: 10.1515/reveh-2021-0012
8. Han J, Xu X, Zhou J, Yao F, Lv LJ, Zhao Y. Effects of TCM guidance physical exercise on prevention and treatment of novel coronavirus pneumonia. Chin J Info Tradit Chin Med. (2020) 27:20–2. doi: 10.3969/j.issn.1005-5304.202002122
9. CACM CARM. Guidelines for Integrated Chinese and Western Medicine Rehabilitation during COVID-19 Recovery (first edition). Tianjin J Tradit Chin Med. (2020) 37:484–9. doi: 10.11656/j.issn.1672-1519.2020.05.02
10. Zhang BL, Chen BG, Zhang ZL, Mao JY, Luo MC, Sun ZT, et al. Rehabilitation Program of Integrated Traditional Chinese and Western Medicine for COVID-19 recovery period in Tianjin (Trial). Tianjin J Tradit Chin Med. (2022) 39:275–7. doi: 10.11656/j.issn.1672-1519.2022.03.02. WSJK.TJ.GOV.
11. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
12. Cochrane Handbook. Assessing risk of bias in a randomized trial. Cochrane Handb Syst Rev. (2019) Interventions 2:205–28. doi: 10.1002/9781119536604.ch8
13. NHC of the PRC, NATCM. Traditional Chinese medicine treatment in COVID-19 diagnosis and treatment protocol (Trial version 9th). China Med. (2022) 17:481–7. doi: 10.3760/j.issn.1673-4777.2022.04.001
14. Schünemann H, Bro zek J, Guyatt G, Oxman A. Introduction to GRADE handbook(2013). Available online at: https://gdt.gradepro.org/app/handbook/handbook.html (Accessed 15 December 2023).
15. Liu JP. GRADE Methods in traditional medicine. Integr Med Res. (2022) 11:100836. doi: 10.1016/j.imr.2022.100836
16. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.0. 1 The Cochrane Collaboration(2011). Available online at: http://wwwcochranehandbookorg.2011.
17. Chen XY, Chen YP, Pan XJ. Effect of bed Baduanjin on mental health of COVID-19 patients. Chin J Conv Med. (2020) 29:1137–9. doi: 10.13517/j.cnki.ccm.2020.11.006
18. Wu HY, Pan L, Li L, Huang Y, Liu YY, Chen JH. The effect of the Baduanjin training on the anxiety of patients with COVID-19 in the cabin hospital. Special Health. (2020) 34:120–1.
19. Yang X, Luo Y, Zhou CM, Li J, Zheng XM. Study on the application of Baduanjin combined acupressure to relieve anxiety and depression in COVID-19 patients. Worl Late Med Info. (2020) 20:97–8. doi: 10.3969/j.issn.1671-3141.2020.71.040
20. Zhang YH, Rao JF. The effects of Yijinjing on the psychological status of COVID-19 patients. Prac Clin Med. (2020) 21:81–3. doi: 10.13764/j.cnki.lcsy.2020.08.027
21. Li L, Ni J, Jiao J, Li DY, Xia Y, Chen OY, et al. Clinical nursing observation of five elements music combined with six words formula on improving negative emotion of patients with novel coronavirus pneumonia. J Tradit Chin Med Univ Hunan. (2021) 41:765–9. doi: 10.3969/j.issn.1674-070X.2021.05.021
22. Li ZL. Clinical study on the rehabilitation treatment of integrated Chinese and Western medicine for COVID-19. HBTCM. (2021). doi: 10.27134/d.cnki.ghbzc.2021.000141
23. Wang XF, Wang SJ, Feng X, Kong DH, Tian WY, Xu XN, et al. Influence of Baduanjin combined with five element music on negative emotion, the quality of life and sleep in patients suffering COVID-19. West J Tradit Chin Med. (2021) 34:9–12. doi: 10.12174/j.issn.1004-6852.2021.09.04
24. Yang C, Ma Y, Mei JH, Gong X, Wang M, Liu K. Observation of therapeutic effect on coronavirus disease 2019 with insomnia in treatment with baduanjin and auricular point sticking therapy. Zhongguo Zhen Jiu. (2021) 41:243–6. doi: 10.13703/j.0255-2930.20200327-0002
25. Yin LS, Wang YX, Li Y, Xiong EP, Chen YK, Wang J. Clinical study on relieving negative emotions in patients with COVID-19 treated with music therapy of five elements combined with Baduanjin. Prog Mode Biomed. (2021) 21:2739–43. doi: 10.13241/j.cnki.pmb.2021.14.030
26. Cai GF, Guo SH, Zhuang Z, Liu K, Wang XZ, Jia KP, et al. Effect of the classics of tendon changing on sleep and depression in patients with sleep disorder after novel coronavirus infection. Sichuan Sports Sci. (2022) 41:44–8. doi: 10.13932/j.cnki.sctykx.2022.05.10
27. Wen ZL, Wang JW, Hao WW, Wang XZ, Fang M. Influence of Kangyi Qiangshen Gong intervention on nucleic acid negative conversion rate and anxiety in patients with mild and asymptomatic infection of COVID-19 Omicron variant. Shanghai J Tradit Chin Med. (2022) 56:1–3. doi: 10.16305/j.1007-1334.2022.2206119
28. Yang L. The effect of Baduanjin combined psychological intervention in the recovery period of COVID-19 patients. Health Care Today. (2022) 22:321–3. doi: 10.3969/j.issn.1671-0223(s).2022.03.001
29. Freedland KE, Dew MA, Sarwer DB, Burg MM, Hart TA, Ewing SWF, et al. Health psychology in the time of COVID-19. Health Psychol. (2020) 39:1021–5. doi: 10.1037/hea0001049
30. Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM. Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front Immunol. (2021) 12:686029. doi: 10.3389/fimmu.2021.686029
31. Zeng N, Zhao YM, Yan W, Li C, Lu QD, Liu L, et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol Psychiatry. (2023) 28:423–33. doi: 10.1038/s41380-022-01614-7
32. Rahmati M, Udeh R, Yon DK, Lee SW, Dolja-Gore X, McEVoy M, et al. A systematic review and meta-analysis of long-term sequelae of COVID-19 2-year after SARS-CoV-2 infection: A call to action for neurological, physical, and psychological sciences. J Med Virol. (2023) 95:e28852. doi: 10.1002/jmv.28852
33. Qin H, Zhang GC, Liu HH, Su LM, Qin YH. Progress in clinical application research of Baduanjin. J Guangxi Univ Chin Med. (2020) 23:83–6. doi: 10.3969/j.issn.2095-4441.2020.03.027
34. Zou L, Pan Z, Yeung A, Talwar S, Wang C, Liu Y, et al. A review study on the beneficial effects of Baduanjin. J Altern Complement Med. (2018) 24:324–35. doi: 10.1089/acm.2017.0241
35. Chen T, Yue GH, Tian Y, Jiang C. Baduanjin mind-body intervention improves the executive control function. Front Psychol. (2017) 7:2015. doi: 10.3389/fpsyg.2016.02015
36. An T, He ZC, Zhang XQ, Li J, Chen AL, Tan F, et al. Baduanjin exerts anti-diabetic and anti-depression effects by regulating the expression of mRNA, lncRNA, and circRNA. Chin Med. (2019) 14:3. doi: 10.1186/s13020-019-0225-1
37. Kong YM, Yan JT, Shi ZJ. Clinical research progress in health Qigong Yijinjing. Chin J Info Trad Chin Med. (2019) 26:133–6. doi: 10.3969/j.issn.1005-5304.2019.02.031
38. Xie F, Dong W, Guan C, Yao F. Effects of Yijinjing Qigongin alleviating fatigue, sleep quality, and health status on patients with chronic fatigue syndrome: A randomized, controlled, and parallel group clinical study. Complement Med Res. (2023) 30:204–12. doi: 10.1159/000528827
39. Li WL, Fan TG. A review on the clinical application of Liuzi Jue. Clin J Chin Med. (2021) 13:127–30. doi: 10.3969/j.issn.1674-7860.2021.35.040
40. Tang Y, Jiang J, Shen P, Li M, You H, Liu C, et al. Liuzijue is a promising exercise option for rehabilitating discharged COVID-19 patients. Med (Baltimore). (2021) 100:e24564. doi: 10.1097/MD.0000000000024564
41. Fang L, Zhu QG, Cheng W, Zhan C, Fang XM, Guo CY, et al. Retrospective analysis on 308 cases of COVID-19 and clinical application protocol of Kangyi Qiangshen Gong exercise prescription. Shanghai J Tradit Chin Med. (2020) 54:40–5. doi: 10.16305/j.1007-1334.2020.05.095
Keywords: COVID-19, Daoyin, traditional Chinese medicine, SAS, SDS, meta-analysis
Citation: Duan N, Chen F, Li Y, Zhou L, Zhang X, Xu G and Zhang W (2024) How traditional Chinese exercise (Daoyin) can help COVID-19 patients relieve psychological symptoms: a systematic review and meta-analysis. Front. Psychiatry 15:1422229. doi: 10.3389/fpsyt.2024.1422229
Received: 24 April 2024; Accepted: 18 July 2024;
Published: 13 August 2024.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Xiaodan Wu, Fudan University, ChinaWenchao Gu, Shanghai Pudong New Area People’s Hospital, China
Copyright © 2024 Duan, Chen, Li, Zhou, Zhang, Xu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Zhang, zhangw1190a@sina.com
†These authors have contributed equally to this work
 Naifan Duan
Naifan Duan Feng Chen1†
Feng Chen1† Xing Zhang
Xing Zhang Wei Zhang
Wei Zhang