- 1Section of Psychiatry, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy
- 2Section of Clinical Psychology, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy
Background: The COVID-19 pandemic has prompted significant changes in healthcare, particularly affecting psychiatric and psychological Consultation-Liaison (CL) services in general hospital settings.
Aim: To assess the effects of COVID-19-related restrictions on utilization of psychiatric and psychological CL services in Northeast Italy during 2020, and to compare it to the use of services in the previous year (2019).
Methods: The study collected data on psychiatric and psychological consultations in 2019 and 2020 from a hospital database. It categorizes consultations by type of patient (inpatient or outpatient) and referral source (hospital wards, general practitioners, other specialists). Pandemic-related restrictions were classified as “lockdown,” “intermediate restrictions,” and “no or reduced restrictions” based on the Covid Stringency Index (CSI). Poisson regression models were employed to analyze the data.
Results: The findings reveal a significant 28% increase in the number of psychiatric and psychological consultations in 2020. Consultations for outpatients increased by 51%, while those for inpatients decreased by 11%. However, the lockdown and intermediate restriction phases were deemed responsible of a decrease of 42.9% and 19.5% in consultations respectively.
Discussion: This study highlights the persistent psychological burden during the COVID-19 pandemic, alongside reduced CL services due to lockdown measures. Integrating telemedicine into these types of services becomes imperative for meeting patient needs during restrictions. These findings can inform policies and practices to improve effective mental health care delivery during and beyond pandemics. Future research should explore the impact of pandemic-related restrictions on mental healthcare across settings and clinical factors affecting service accessibility.
1 Introduction
Psychiatric and psychological Consultation-Liaison (CL) services are specialized in providing psychiatric and psychological care in collaboration with various healthcare practitioners, typically within general hospital settings (1–3). These professionals play an active role in addressing psychiatric symptoms, including atypical clinical presentations, diagnosing complex cases (4, 5), dealing with stress management and other areas of maladaptive health reactions and behaviors and helping patients in enhancing their coping strategies (6).
The COVID-19 pandemic has required significant changes in the daily activity of psychiatric and psychological CL services to maintain a high standard of clinical care (7–9). Specifically, clinical challenges for psychiatric and psychological services in community settings included mitigating the psychological effects of the pandemic on patients, responding to the immediate needs of individuals with severe mental illnesses, recognizing and treating neuropsychiatric symptoms associated with COVID-19, and providing support to healthcare professionals (5, 10–13). For patients hospitalized with COVID-19 infection, researchers indeed observed symptoms of anxiety, stress, depression, increased suicidal behavior, alcohol consumption, and psychotic symptoms (5, 14–16).
In addition to the above challenges, an essential aspect of CL psychiatry and psychology involves managing neuropsychiatric manifestations and identifying symptoms not typically associated with psychiatric disorders, both during the acute and post-acute pandemic phase. In the acute phase, COVID-19 patients appear to be at risk of a range of neuropsychiatric symptoms and disorders, including delirium, encephalopathy, impaired consciousness, depressed mood, anxiety, and insomnia (17–19), with fatigue, cognitive deficits, depression, and post-traumatic symptoms in the post-acute phase (17, 20–23). Overall, such clinical manifestations deeply impact on survivors’ physical and mental quality of life (20).
Following the first documented cases on February 21, 2020, Italy experienced significant impacts from the COVID-19 pandemic, ranking second only to China in terms of affected countries (24). Consequently, on March 9, the government implemented stringent measures to restrict population movement and prevent gatherings. This was followed by a national quarantine declaration on March 11, which mandated the closure of all non-essential businesses and restricted movement except for essential reasons such as work activities and health issues, aimed at reducing the spread of the coronavirus. Subsequently, on April 26, the Italian government announced the conclusion of the lockdown, leading to a gradual resumption of economic activities starting from May 4 (24). However, due to an increase of COVID-19 cases in October 2020, more stringent restrictions were imposed, culminating in the establishment of a regional-based system on November 3, which implemented varying levels of measures based on the pandemic’s trend in different country’s areas (25).
Despite this challenging context, the Italian literature highlights a substantial decrease in both the total number of psychiatric emergency consultations and psychiatric admission rates during the lockdown period (26, 27). However, there is a lack of evidence regarding the organizational changes in psychiatric and psychological CL services in Italy and especially their long-term consequences on patients’ mental health during the COVID-19 pandemic (28, 29).
The present study aims to assess the effects of lockdown and intermediate restrictions on the clinical activities of a psychiatric and psychological CL service in a General Hospital in Northeast Italy according to the characteristics of referrals and through a comparison of similar time-periods in 2019 and 2020.
2 Materials and methods
This is a retrospective study conducted on all psychiatric and/or psychological consultations of adult patients (>18 years of age, inpatient and/or outpatient) in the years 2019 and 2020. This project complied with the principles of the Declaration of Helsinki with respect to medical research involving human subjects. Approval for the study was obtained from the local Ethics Committee (Prog. 3327CESC).
2.1 Setting
This study was conducted at the Verona University Hospital Trust, situated in the northeast of Italy. The Verona University Hospital is the second largest hospital trust in Italy in 230 terms of the number of beds (1617 beds in 2019) and the fifth largest in terms of admissions (44,593 planned and urgent admissions, and 12,214 day-hospital admissions in 2019). Outpatient contacts were about 3.7 millions in 2019. The Verona Trust treats patients coming from all over Italy (17% come from outside the Veneto Region). The trust is formed by two hospitals, located in two different parts of the city, both having psychiatric and psychological services. The consultations considered in this paper were carried out by the “Psychosomatic and Psychological Medicine Unit” and the “Clinical Psychology Unit” of one of the two hospitals, the G.B. Rossi Hospital, which has a capacity of about 500 beds for inpatients and dedicated clinics for day-hospital and day surgery care (delivering about one-third of all admissions and outpatient contacts produced by the trust).
The two Units receive requests for consultation through an online platform from all G.B. Rossi Hospital services, including inpatients, day-patients and outpatients undergoing treatment for organic diseases. They are available from Monday to Friday. Consultations for inpatients are usually conducted within 48 hours after receiving the request, while consultations for day-patients and outpatients are scheduled within few weeks (mainly 2 weeks). Along with in-person or telephone consultations with the requesting medical and/or psychological staff, written reports and diagnoses are provided. The clinical team is composed of psychiatrists, residents in psychiatry, psychologists, psychologists in training and psychotherapists.
For urgent requests from the Emergency Room or other hospital wards, a pool of psychiatrists from another unit (Psychiatry Unit) is available on-call. Furthermore, the “Psychosomatic and Psychological Medicine Unit” and the “Clinical Psychology Unit” serve as a center for the diagnosis and treatment of psychosomatic disorders with several dedicated ambulatories (i.e.: for patients with multiple sclerosis, mastocytosis, functional neurological disorders, hematological diseases, etc.). Additionally, they provide as psychological and psychiatric support to health care professionals. Patients seeking consultation can be also referred by their general practitioners (GPs) or other specialists outside the Verona hospital.
2.2 Data source
All data on patients and contacts were obtained from the Hospital Clinical Database (HCD): this database collects all medical records, including planned consultation requests from both surgical and medical wards units. These requests come from the hospital, and also from GPs and other specialists outside the hospital. The database includes comprehensive information regarding the patient clinical history, and number and characteristics of consultations.
During the pandemic, some hospital wards have been completely dedicated to COVID-19 patients, the requests from these wards were classified as “COVID-19-related” consultations.
Information about restrictions and lockdown adopted in Italy by the Government has been obtained using the Covid Stringency Index (CSI). The CSI (25) is a composite measure that assesses the strictness of various COVID-19 response indicators, by considering factors such as school closures, workplace closures, and travel bans. The index has a score ranging from 0 to 100, with higher values indicating more stringent measures implemented in response to the pandemic. We applied the CSI related to Italy.
2.3 Data analysis
2.3.1 Comparison between year 2019 and year 2020
We calculated the total number of contacts in the two-year period 2019-2020. The analyses have been conducted considering the type of patients (inpatient and outpatient), in combination with sociodemographic variables, and then with type of referral (hospital wards and external referrals). In this latter case, consultations, both for outpatient and for inpatients, were categorized into three main groups: (1) Outpatients from General Hospital (divided into psychiatric or psychological consultations), (2) Inpatients from General Hospital (divided into surgical or medical wards), (3) Outpatients referred to the CL service by GPs and other specialists outside the hospital (divided again into psychiatric or psychological consultations). Patients who are admitted to the hospital frequently have interaction with both psychiatrists and psychologists during their stay, for this reason and in order to minimize the number of analyses carried out, inpatient consultations were solely categorized based on referral wards. Sociodemographic variables were citizenship (Italian vs. Other); age categories (18-24, 25-44, 45-64, and 65+), and gender (male or female).
To test the equality of the number of contacts between 2019 and 2020 for each variable and globally, the conditional exact binomial test on the equality of proportions has been used. This test, proposed by Przyborowski and Wilenski (30), is suitable for analyzing Poisson variables.pt?>
2.3.2 Identification of the impact of restrictive measures on the number of clinical contacts
Our dataset was composed of the weeks of 2019 and 2020, and the CSI has been adopted as the primary variable of interest to measure the extent of pandemic-related restrictions. The CSI, measured daily for Italy, served to categorize the weeks of 2020 (and 2019 for comparative analysis) into three distinct periods: “no or reduced restrictions,” (average CSI below 0.7) “intermediate restrictions,” (average CSI between 0.7 and 0.8) and “lockdown” (average CSI above 0.8).
To address the discrete nature of the outcome variable, which is the number of contacts per working day, a Poisson regression model has been employed. Robust standard errors were incorporated to account for overdispersion.
Given the variability in the number of working days among weeks due to public holidays and the extended last week of each year, the variable representing the number of working days per week was included. This adjustment allows to normalize contact numbers by considering variations in working days.
Considering that COVID-19 restrictions encompassed travel limitations, an indicator variable has been introduced to accommodate weeks that featured public holidays during which inter-regional travel was either prohibited or discouraged. This control variable ensures that potential reductions in contacts during holiday weeks are appropriately considered.
In summary, this methodology allows us to examine the impact of restriction levels on contacts number, while considering the discrete nature of the outcome and accounting for factors such as the number of working days and travel restrictions.
The study employed a “difference-in-differences” approach, as outlined by Higgins et al. (31). Specifically, this approach involved comparing the difference in the number of contacts between the years 2019 and 2020 during weeks characterized by lockdown and intermediate restrictions with the corresponding difference in weeks presenting no or reduced restrictions. This comparison allowed us to interpret the effects of the pandemic-related restrictions. To implement this approach, three indicators have been incorporated into the regression analysis: one related to the year 2020 and two related to specific periods within that year (one for weeks with intermediate restrictions and another for weeks with lockdown measures).
Our parameters of interest were the two interactions between the year indicator and those related to the level of restrictions in 2020. We conducted both a comprehensive regression analysis considering all contacts and separate regressions for each type of contact, by distinguishing between outpatient and admission contacts.
Furthermore, to assess whether variations in the effects of restrictions across different service types were statistically significant, a global test has been performed using a Poisson regression model. This model incorporated an exposure variable representing the number of working days in each week, allowing to account for potential differences in contact patterns arising from variations in working days.
3 Results
In the year 2020, a 28% increase in the number of psychiatric and psychological consultations was observed when compared to 2019 (Table 1). In particular, consultations requested for outpatients increased by 51%, and those requested for inpatients decreased by 11%. With respect to sociodemographic variables, all categories showed a similar trend towards an increase of the overall number of contacts and outpatient contacts, while overall inpatient contacts decreased, with the exception of young (18-24 years old), elderly (> 65 years old), and female.
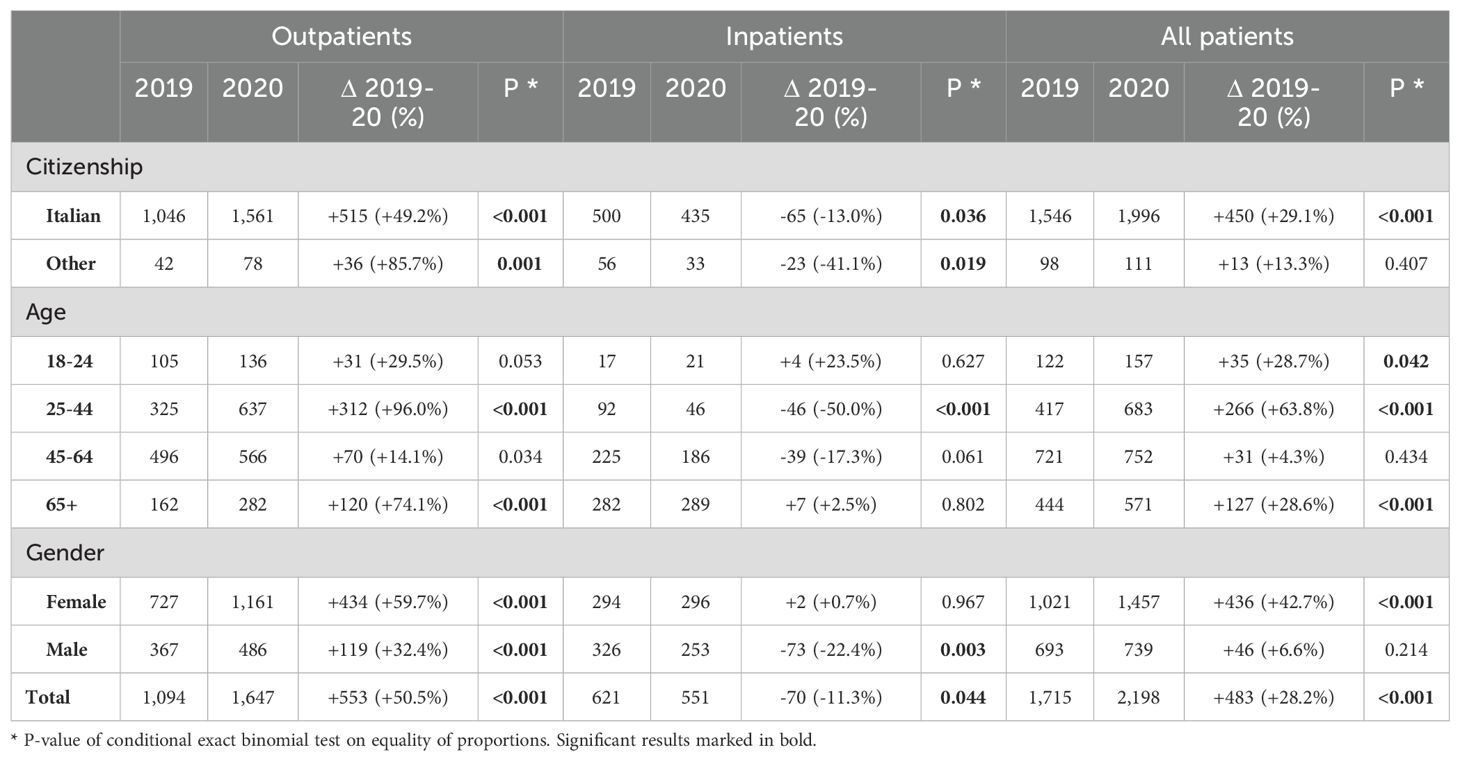
Table 1. Number of consultations requested during years 2019 and 2020 by patients’ sociodemographic characteristics.
In terms of type of consultations (Table 2), the comparison between 2019 and 2020 showed an increase in psychological consultations for outpatients, both requested by GPs or other specialists outside the hospital (+60.4%), and by specialists working in hospital wards (+50.6%). Also, the number of both types of psychiatric consultations increased in 2020, respectively of 35.7% and 38.7%. The number of consultations for inpatients decreased in 2020 by about 11%, such decrease being statistically significant both globally and for requests from surgical wards (-33.5%).
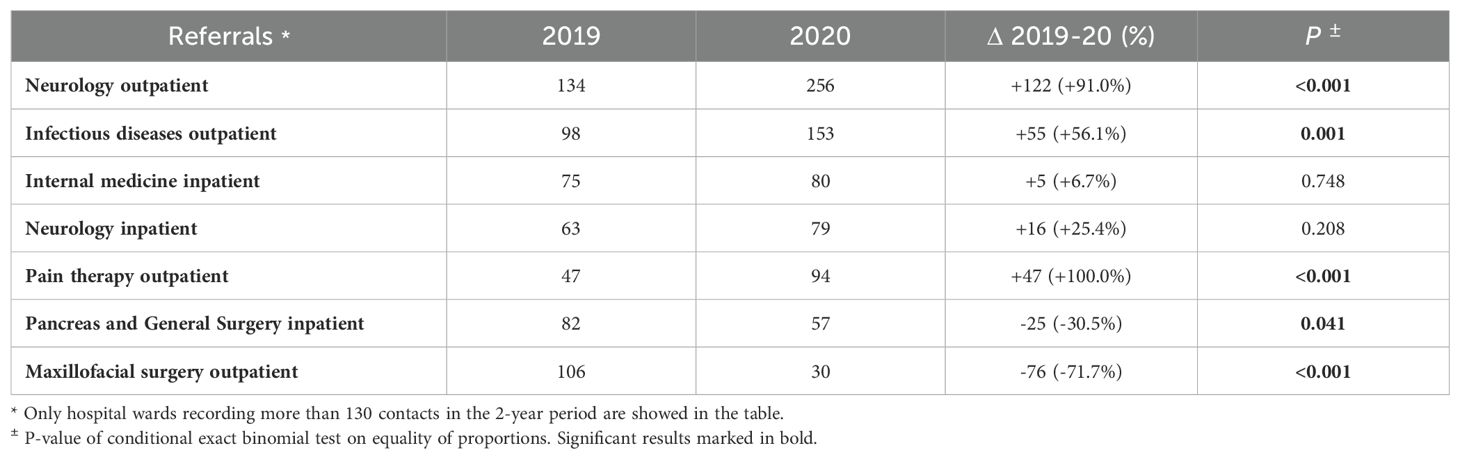
In units that request more psychiatric and psychological consultations (Table 3) (more than 130 in the two years), the increase was significant for outpatients in care at the neurology unit (+91.0%), infectious diseases unit (+56.1%), and pain therapy unit (+100.0%). Significant decreases were observed in requests from Pancreas and General Surgery for inpatients (-30.5%), and from Maxillofacial surgery for outpatients (-71.7%).
Poisson regression analyses (Table 4) revealed statistically significant effects of lockdown measures and intermediate restrictions in reducing the number of consultations. The lockdown was associated with a reduction of 39.5% (p-value<0.001), while intermediate restrictions led to a 21.5% decline (p-value 0.017). These percentages increased to 41.8% (p-value<0.001) and 27.3% (p-value 0.001), respectively, when excluding COVID-19-related consultations from the analysis.
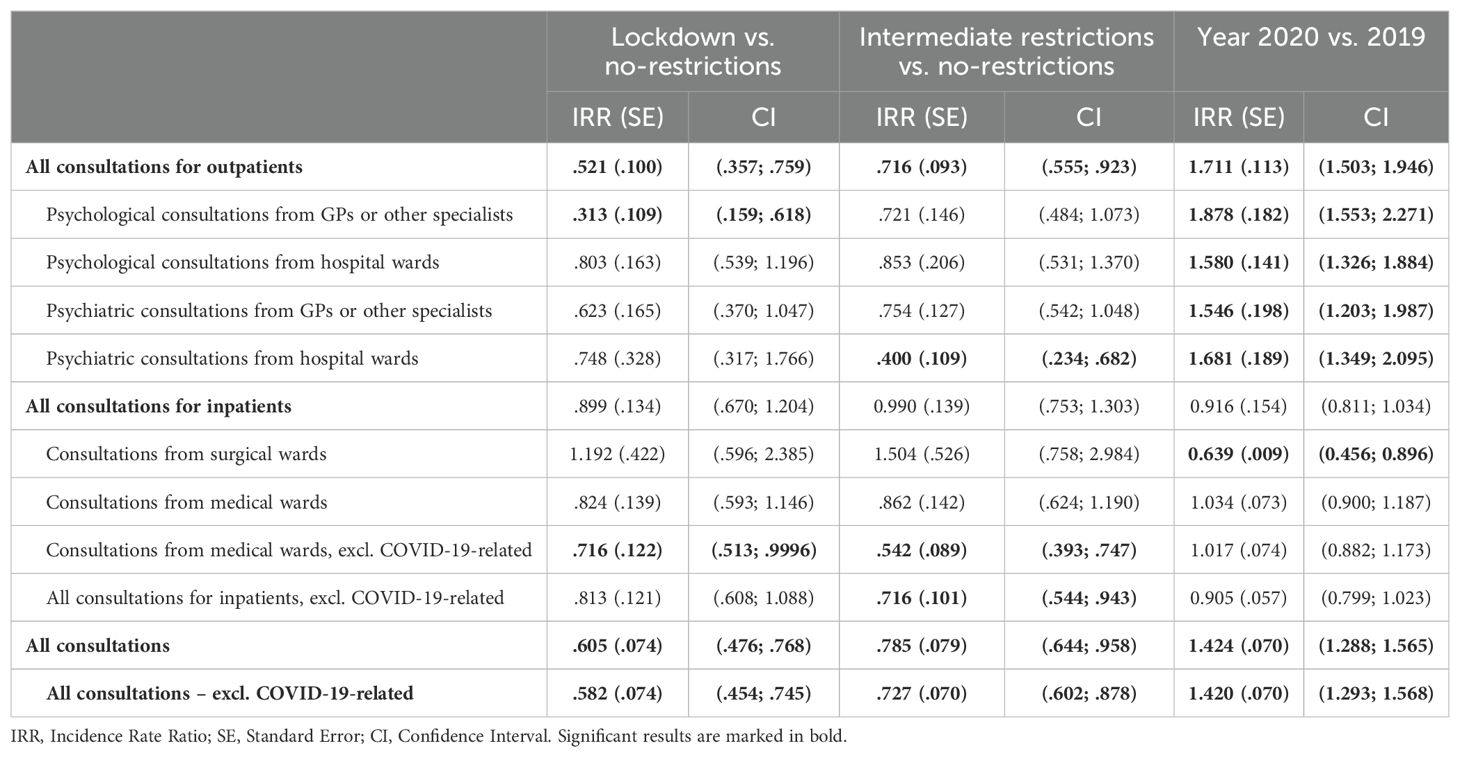
Table 4. Poisson regression model on number of consultations per working-day during lockdown and restrictions.
The impact of these measures varied significantly (with a p-value of 0.020 when considering all consultations and a p-value of 0.026 when excluding those related to COVID-19) depending on the types of consultations. An instance of this can be seen in psychiatric consultations requested by GPs or other specialists, which exhibited a similar effect of the lockdown as of observed in overall consultations. However, this effect did not achieve statistical significance at the conventional threshold of 5% (p-value 0.074). The impact of restrictions and lockdown on psychological and psychiatric consultations for outpatient requested by hospital units, and on those for inpatients in medical wards was estimated to be comparatively lower, without statistical significance. There was a substantial reduction (68.7%; p-value 0.001) of psychological consultations requested by GPs or other specialists outside the hospital ascribed to the lockdown.
Regarding the impact of intermediate restrictions on psychological and psychiatric consultations requested by GPs or other specialists, psychological outpatient consultations requested by hospital units and inpatient consultations requested by medical 530 wards, results showed estimates comparable to those derived from the overall data, but no statistical signi!cance was found due to the smaller sample sizes. We estimated a 60% reduction (p-value 0.001) of psychiatric outpatient consultations within hospital units following the implementation of intermediate restrictions on contact.
For the number of consultations requested by surgical wards, the parameters displayed an opposite trend, indicating a positive estimated effect of both lockdown and restrictions. However, in both cases statistical significance was not reached.
When contacts were categorized into “all outpatient” vs “all inpatients” types, results were statistically significant for the former category only. In particular, both the lockdown (p-value 0.001, estimated reduction: 47.9%) and intermediate restrictions (p-value 0.010, estimated reduction: 28.4%) had a lowering effect on the number of outpatient consultations.
Furthermore, when COVID-19 related consultations were excluded from the analysis, we found a reduction of 28.4% due to the lockdown (p-value 0.0497), and of 45.8% due to intermediate restrictions (p-value<0.001) on medical ward contacts. We also found a decrease in the total number of inpatients consultations due to both COVID-19 containment measures. This reduction was specifically evident during intermediate restrictions (28.4%, p-value 0.017).
The number of contacts in 2020 would have been increased of 42.4% (p-value<0.001) compared to 2019, in case no restrictions were introduced. This is linked to outpatient consultations only (that would have shown, a 71.1% increase, p-value<0.001), while we estimate a reduction in consultations from surgical wards would have been observed (-36.1%; p-value 0.009).
4 Discussion
This is an observational retrospective study focused on the impact of the COVID-19 pandemic on CL psychiatric and psychological services conducted in a General Hospital in the Northeast Italy. The data clearly shows a significant increase in the number of requests for psychiatric and psychological consultations in 2020, concurrently with the COVID-19 pandemic, compared to the previous year.
This increase in demand is consistent with recent global reports on the mental health impact of the COVID-19 pandemic, which reported an increased request and need of mental health care (32–35). Despite the greater demand for psychiatric and psychological CL services, the lockdown was estimated to reduce consultations by 42.9%, with a smaller drop of 19.5% during the intermediate restriction phase.
This finding could potentially be explained by patients’ hesitance to access the hospital due to their pandemic-related fear (36). Despite the increased level of psychological distress experienced by the general population (37), distressed individuals might have tried to avoid or limit in-person meetings with healthcare providers (36). On the other hand, clinicians may have tried to manage hospital admissions cautiously, possibly to preserve hospital beds for potential increases in COVID-19 cases (2). This attitude could explain the decrease in CL psychiatry and psychology appointments. At this regard, in the Verona hospital during the pandemic phase, several wards were repurposed to admit COVID-19 patients. To minimize the infection spread, psychiatric and psychological consultations were often conducted via telephone or video calls. The Hospital Clinical Database was updated accordingly, to support the registration of teleconsultations. In light of the clinical demand observed during the pandemic, the implementation of telemedicine options - in particular in the field of psychiatric and psychological consultations – may be effective to meet the clinical needs of patients. Telemedicine has the potential to provide prompt treatment and preventive measures for patients, while also alleviating the strain on healthcare professionals (38).
Considering that, despite the significant effect of lockdown and restrictions in reducing the number of consultation requests, there was an increase in consultations in 2020, it is plausible that there was a rebound in demand once the number of COVID-19 cases decreased, and restrictions were reduced, to recover the previously lost consultations. Our results support this hypothesis, suggesting a potential increased demand for CL psychiatry and psychological services as the pandemic situation improved.
4.1 Limitations and strengths
Findings of the present study should be interpreted cautiously, as several methodological limitations are acknowledged. Firstly, our study faces a potential risk of information bias due to data collection conducted by various mental health professionals. This diversity in data collection methods has revealed gaps in sociodemographic data, which could potentially influence the study’s outcomes. Secondly, the registration of tele-consultation was implemented in the dataset only at the end of 2020. This delayed inclusion prevented us from separately analyzing the teleconsultation variable, which could have provided valuable insights for data interpretation. The inclusion of this information could have significantly contributed to our comprehension of the impact of tele-consultations on the observed trends. Thirdly, our dataset lacked critical information about reason for referral, individual clinical pathways and follow-ups. The absence of this data may potentially impact the comprehensive understanding of the factors affecting patients’ choices regarding seeking psychiatric or psychological consultations during and after the pandemic.
Lastly, our study was conducted within a single hospital, and it is essential to acknowledge the absence of certain departments, such as gynecology/obstetrics and pediatrics. Consequently, we must exercise caution when attempting to generalize the data across all specialties or other healthcare facilities or different regions in Italy. It is important to recognize that the Province of Verona experienced one of the most significant health impacts of the pandemic in Europe in terms of infections number (35, 39). Therefore, the unique circumstances of this heavily affected area may have influenced the observed trends, potentially limiting the applicability of our findings to other contexts.
In summary, the study compared the number of consultations in the years 2019 and 2020, and employed a robust “difference-in-differences” methodology. It explored multiple indicators and an appropriate regression model to reasonably estimate the effect of different level of pandemic-related restrictions on the number of consultations requests in 2020.
4.2 Implications
In terms of implications for further research, there is a need to expand the exploration to additional clinical and organizational factors that may influence the accessibility of psychiatric and psychological CL services. For example, evaluating specific individual factors such as socioeconomic status (40), diagnosis-related groups for each patient, service variables associated with healthcare system provisions and utilization, staff resources, or more general factors like the level of urbanization in relation to the use of CL services (41). A deeper understanding of these elements can offer valuable insights on the barriers and facilitators that impact the access to mental health support during periods of pandemic.
5 Conclusions
Our study identified an overall increase in the number of psychiatric and psychological consultations during 2020, despite a decreasing effect due to lockdown and intermediate restriction. To date, there are no observational studies investigating the long-term effects of the COVID-19 pandemic on psychiatric and psychological CL services. Further research and initiatives, that expand clinical and organizational factors impacting the accessibility of psychiatric and psychological CL services, are crucial for optimizing mental health care delivery during and beyond the pandemic (38). Implications from this study hold the potential to inform and shape policy and practice both at national and international level.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Comitato Etico per la Sperimentazione Clinica - Azienda Ospedaliera Universitaria Integrata di Verona (protocol number: 3327CESC). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EP: Writing – review & editing, Writing – original draft, Visualization, Methodology, Investigation, Conceptualization. AM: Writing – review & editing, Writing – original draft, Data curation, Conceptualization. FT: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Data curation, Conceptualization. LR: Writing – review & editing, Writing – original draft, Visualization, Validation, Data curation, Conceptualization. DS: Writing – review & editing, Writing – original draft, Visualization, Data curation, Conceptualization. MB: Writing – review & editing, Writing – original draft, Visualization, Data curation, Conceptualization. MP: Writing – review & editing, Writing – original draft, Data curation. GO: Writing – review & editing, Writing – original draft, Data curation. VD: Writing – original draft, Data curation, Writing – review & editing. CP: Writing – review & editing, Writing – original draft, Data curation. MR: Writing – review & editing, Writing – original draft, Data curation. LD: Writing – review & editing, Writing – original draft, Project administration, Data curation. FA: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Financial support was received from the University of Verona for open access publication of this article.
Acknowledgments
The authors thank the University of Verona for financially funding this open access publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gautam S, Gautam M, Jain A, Yadav K. Overview of practice of consultation-liaison psychiatry. Indian J Psychiatry. (2022) 64:201. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_1019_21
2. Lele K, Cartoon J, Griffiths A. Increased referrals to an Australian Consultation Liaison Psychiatry service during the COVID-19 pandemic. Australas Psychiatry. (2021) 29:340–3. doi: 10.1177/1039856221992937
3. Stein B, Müller MM, Meyer LK, Söllner W, the CL Guidelines Working Group. Psychiatric and psychosomatic consultation-liaison services in general hospitals: A systematic review and meta-analysis of effects on symptoms of depression and anxiety. Psychother Psychosom. (2020) 89:6–16. doi: 10.1159/000503177
4. Dua D, Grover S. Profile of patients seen in consultation-liaison psychiatry in India: A systematic review. Indian J Psychol Med. (2020) 42:503–12. doi: 10.1177/0253717620964970
5. Horn M, Granon B, Vaiva G, Fovet T, Amad A. Role and importance of consultation-liaison psychiatry during the Covid-19 epidemic. J Psychosom Res. (2020) 137:110214. doi: 10.1016/j.jpsychores.2020.110214
6. Wise TN. Consultation-liaison research: the use of differing perspectives. Psychotherapy and psychosomatics (1995) 63(1):9–21. doi: 10.1159/000288932
7. Barry H, Doherty AM, Clancy M, Moore S, MacHale S. Lockdown logistics in consultation–liaison psychiatry. Ir J Psychol Med. (2022) 39:414–22. doi: 10.1017/ipm.2020.104
8. Beran C, Sowa NA. Adaptation of an academic inpatient consultation-liaison psychiatry service during the SARS-coV-2 pandemic: effects on clinical practice and trainee supervision. J Acad Consult-Liaison Psychiatry. (2021) 62:186–92. doi: 10.1016/j.psym.2020.11.002
9. Flavel MJ, Holmes A, Ellen S, Khanna R. Evaluation of consultation liaison psychiatry in Australian public hospitals (AU-CLS-1). Australas Psychiatry. (2023) 31:95–8. doi: 10.1177/10398562221143930
10. Iqbal Y, Alabdulla M, Kumar R, Latoo J, Albrahim S, Wadoo O, et al. Characteristics of 100 consecutive patients with COVID-19 referred to consultation-liaison psychiatry services in Qatar: A comparison of patients with delirium versus other psychiatric diagnoses. Qatar Med J. (2022) 3. doi: 10.5339/qmj.2022.28
11. Kurotschka PK, Serafini A, Demontis M, Serafini A, Mereu A, Moro MF, et al. General practitioners’ Experiences during the first phase of the COVID-19 pandemic in Italy: A critical incident technique study. Front Public Health. (2021) 3:623904. doi: 10.3389/fpubh.2021.623904
12. Moro MF, Calamandrei G, Poli R, Di Mattei V, Perra A, Kurotschka PK, et al. The impact of the COVID-19 pandemic on the mental health of healthcare workers in Italy: analyzing the role of individual and workplace-level factors in the reopening phase after lockdown. Front Psychiatry. (2022) 2:867080. doi: 10.3389/fpsyt.2022.867080
13. Prina E, Tedeschi F, Salazzari D, Botte T, Ballarin M, Rabbi L, et al. Effect of COVID-19 pandemic on utilisation of community-based mental health care in North-East of Italy: A psychiatric case register study. Epidemiol Psychiatr Sci. (2023) 32:e17. doi: 10.1017/S2045796023000100
14. Piumatti G, Amati R, Richard A, Baysson H, Purgato M, Guessous I, et al. Associations between depression and self-reported COVID-19 symptoms among adults: results from two population-based seroprevalence studies in Switzerland. Int J Environ Res Public Health. (2022) 19:16696. doi: 10.3390/ijerph192416696
15. Schaefert R, Stein B, Meinlschmidt G, Roemmel N, Blanch J, Boye B, et al. COVID-19-related consultation-liaison (CL) mental health services in general hospitals: A perspective from Europe and beyond. J Psychosom Res. (2023) 167:111183. doi: 10.1016/j.jpsychores.2023.111183
16. Witteveen AB, Young SY, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F, et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: An umbrella review of the evidence. Kola L, editor. PloS Med. (2023) 20:e1004206. doi: 10.1371/journal.pmed.1004206
17. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. doi: 10.1016/S2215-0366(20)30203-0
18. Ferrando SJ, Lynch S, Ferrando N, Dornbush R, Shahar S, Klepacz L. Anxiety and posttraumatic stress in post-acute sequelae of COVID-19: prevalence, characteristics, comorbidity, and clinical correlates. Front Psychiatry. (2023) 14:1160852. doi: 10.3389/fpsyt.2023.1160852
19. Zhang H, Xie F, Yang B, Zhao F, Wang C, Chen X. Psychological experience of COVID-19 patients: A systematic review and qualitative meta-synthesis. Am J Infect Control. (2022) 50:809–19. doi: 10.1016/j.ajic.2022.01.023
20. Gentilotti E, Górska A, Tami A, Gusinow R, Mirandola M, Rodríguez Baño J, et al. Clinical phenotypes and quality of life to define post-COVID-19 syndrome: a cluster analysis of the multinational, prospective ORCHESTRA cohort. eClinicalMedicine. (2023) 62:102107. doi: 10.1016/j.eclinm.2023.102107
21. Craparo G, La Rosa VL, Marino G, Vezzoli M, Cinà GS, Colombi M, et al. Risk of post-traumatic stress symptoms in hospitalized and non-hospitalized COVID-19 recovered patients. A cross-sectional study. Psychiatry Res. (2022) 308:114353. doi: 10.1016/j.psychres.2021.114353
22. Spada MS, Biffi AM, Belotti L, Cremaschi L, Palumbo C, Locatelli C, et al. Psychological impact of COVID-19 after hospital discharge: A follow-up study on Italian recovered patients. J Affect Disord. (2022) 317:84–90. doi: 10.1016/j.jad.2022.08.086
23. Taha P, Tahir A, Ahmed F, Radha R, Taha A, Slewa-Younan S. Depression and generalized anxiety as long-term mental health consequences of COVID-19 in Iraqi Kurdistan. Int J Environ Res Public Health. (2023) 20:6319. doi: 10.3390/ijerph20136319
24. Governo Italiano. Covid-19 (2020). Available online at: https://www.governo.it/it/coronavirus. (accessed January, 4 2024)
25. Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. (2021) 5:529–38. doi: 10.1038/s41562-021-01079-8
26. Capuzzi E, Di Brita C, Caldiroli A, Colmegna F, Nava R, Buoli M, et al. Psychiatric emergency care during Coronavirus 2019 (COVID 19) pandemic lockdown: results from a Department of Mental Health and Addiction of northern Italy. Psychiatry Res. (2020) 293:113463. doi: 10.1016/j.psychres.2020.113463
27. Clerici M, Durbano F, Spinogatti F, Vita A, De Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. (2020) 37:283–90. doi: 10.1017/ipm.2020.29
28. Meloni S, de Girolamo G, Rossi R. COVID-19 e servizi di salute mentale in Europa. Epidemiol Prev. (2020) 44:383–93. doi: 10.19191/EP20.5-6.S2.142
29. Carpiniello B, Vita A. Impact of COVID-19 on the italian mental health system: A narrative review. Schizophr Bull Open. (2022) 3:sgac038. doi: 10.1093/schizbullopen/sgac038
30. Przyborowski J, Wilenski H. Homogeneity of results in testing samples from poisson series: with an application to testing clover seed for dodder. Biometrika. (1940) 31:313. doi: 10.1093/biomet/31.3-4.313
31. Higgins JP, Ramsay C, Reeves BC, Deeks JJ, Shea B, Valentine JC, et al. Issues relating to study design and risk of bias when including non-randomized studies in systematic reviews on the effects of interventions. Res Synth Methods. (2013) 4:12–25. doi: 10.1002/jrsm.1056
32. de Girolamo G, Cerveri G, Clerici M, Monzani E, Spinogatti F, Starace F, et al. Mental health in the coronavirus disease 2019 emergency—The italian response. JAMA Psychiatry. (2020) 77:974. doi: 10.1001/jamapsychiatry.2020.1276
33. Donisi V, Gajofatto A, Mazzi MA, Gobbin F, Busch IM, Ghellere A, et al. Insights for fostering resilience in young adults with multiple sclerosis in the aftermath of the COVID-19 emergency: an italian survey. Front Psychiatry. (2021) 11:588275. doi: 10.3389/fpsyt.2020.588275
34. Fiorillo A, Sampogna G, Giallonardo V, Del Vecchio V, Luciano M, Albert U, et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur Psychiatry. (2020) 63:e87. doi: 10.1192/j.eurpsy.2020.89
35. Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. (2021) 11:e045127. doi: 10.1136/bmjopen-2020-045127
36. Naqvi H. Mental health in the aftermath of COVID-19: A new normal. J Pak Med Assoc. (2020) 0):1. doi: 10.5455/JPMA.30
37. Marzo R. R., Ismail Z., Htay M. N. N., Bahari R., Ismail R., Villanueva E. Q., et al. Psychological distress during pandemic Covid-19 among adult general population: Result across 13 countries. Clin Epidemiol Glob Health. (2021) 10:100708. doi: 10.1016/j.cegh.2021.100708
38. Prajapati NK, Parikh NC, Shah ND, Darji VM, Jariwala HB, Miroliya MT. Evaluation of psychiatric morbidity in COVID-19-positive inpatients referred to consultation liaison psychiatry in a tertiary care hospital. Indian J Psychol Med. (2021) 43:330–5. doi: 10.1177/02537176211022146
39. Goumenou M, Sarigiannis D, Tsatsakis A, Anesti O, Docea A, Petrakis D, et al. COVID−19 in Northern Italy: An integrative overview of factors possibly influencing the sharp increase of the outbreak (Review). Mol Med Rep. (2020). 22:20–32. doi: 10.3892/mmr.2020.11079
40. Donisi V, Tedeschi F, Percudani M, Fiorillo A, Confalonieri L, De Rosa C, et al. Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Res. (2013) 209:691–8. doi: 10.1016/j.psychres.2013.02.031
Keywords: consultation-liaison, psychiatry, psychology, COVID-19 pandemic, mental health services, general hospitals
Citation: Prina E, Marquis A, Tedeschi F, Rabbi L, Salazzari D, Ballarin M, Purgato M, Ostuzzi G, Donisi V, Perlini C, Rimondini M, Del Piccolo L and Amaddeo F (2024) Effects of COVID-19 pandemic on psychiatric and psychological consultation-liaison contacts in a general hospital in North-East of Italy: a retrospective study. Front. Psychiatry 15:1414248. doi: 10.3389/fpsyt.2024.1414248
Received: 08 April 2024; Accepted: 14 October 2024;
Published: 06 November 2024.
Edited by:
Gloria-Beatrice Wintermann, Technische Universität Dresden, GermanyReviewed by:
Stefano Barlati, University of Brescia, ItalyDamir Huremović, Zucker Hillside Hospital, United States
Copyright © 2024 Prina, Marquis, Tedeschi, Rabbi, Salazzari, Ballarin, Purgato, Ostuzzi, Donisi, Perlini, Rimondini, Del Piccolo and Amaddeo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eleonora Prina, ZWxlb25vcmEucHJpbmFAdW5pdnIuaXQ=
 Eleonora Prina
Eleonora Prina Alice Marquis1
Alice Marquis1 Federico Tedeschi
Federico Tedeschi Marianna Purgato
Marianna Purgato Giovanni Ostuzzi
Giovanni Ostuzzi Valeria Donisi
Valeria Donisi Cinzia Perlini
Cinzia Perlini Michela Rimondini
Michela Rimondini Lidia Del Piccolo
Lidia Del Piccolo