- 1Department of Psychiatry, School of Medicine, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
- 2Department of Psychiatry, School of Medicine, College of Health Science, Bahir Dar University, Bahir Dar, Ethiopia
Background: Post-traumatic stress disorder (PTSD) is one of the most common mental health problems that military personnel encounter. It could be lifelong and affect every aspect of military personnel, including their mental and physical health, family and social interactions, and their work. However, in Ethiopia, the magnitude and its associated factors have not been well investigated.
Objective: This study aimed to determine the prevalence of PTSD and its associated factors among military personnel, who were admitted at the Northwest Command Level Three Military Hospital, Bahir Dar, Northwest, Ethiopia, 2022.
Methods: An institution-based cross-sectional study was conducted from 21 June to 21 July 2022, at the Northwest Command Level Three Military Hospital. A computer-generated simple random sampling technique was used to select a total of 627 participants. The 17-item Military Version Checklist was utilized to measure PTSD. The Patient Health Questionnaire, Brief Resilience Coping, and Critical War Zone Experience scale were utilized to measure depression, resilience, and combat exposure, respectively. Descriptive, bivariate, and multivariate binary logistic regressions with odds ratios and a 95% confidence interval were used. The level of significance of the association was determined at a p-value < 0.05.
Results: A total of 612 respondents participated, with a response rate of 97.6%. The prevalence of PTSD in this study was 21.9% (95% CI: 18.6, 25.2). In multivariable regression, female sex [adjusted odds ratio (AOR) = 2.3, 95% CI; 1.3, 3.87], combat personnel (AOR = 2.75, 95% CI; 1.44, 6.36), handling dead bodies (AOR = 2.5, 95% CI,1.24, 5.02), having 4–5 deployments (AOR = 2.94, 95% CI, 1.63, 5.32), having ≥6 deployments (AOR = 3.4, 95% CI, 1.95, 6.17), low resilience coping (AOR = 2.02, 95% CI; 1.16, 3.53), poor social support (AOR = 2.46, 95% CI, 1.39, 4.35), very high combat exposures (AOR = 4.8, 95% CI, 2.03, 11.93), and depression (AOR = 2.8, 95% CI, 1.68, 4.67) were significantly associated with PTSD.
Conclusion: PTSD is markedly prevalent among the Ethiopian military population, with key risk factors identified as being female, poor social support, low resilience coping skills, handling dead bodies, multiple deployments (four or more), high combat experiences, and depression. Healthcare professionals must prioritize the early diagnosis and intervention of PTSD in vulnerable groups of military personnel.
Introduction
Post-traumatic stress disorder (PTSD) is a syndrome that arises from exposure to actual or potential death, sexual assault, and military combat (1). PTSD has a significant impact on public health, with approximately 8 million individuals developing PTSD each year (2), contributing to 0.4% of years lived with disability (3), and approximately 3 million disability-adjusted life years are associated with PTSD in low- to middle-income countries (LMICs) (4).
PTSD is a common mental disorder, with slightly higher rates among military personnel (13%) compared to the general population (6%) (5). This might be because military personnel experience more combat trauma and paramilitary trauma than civilians (6). Hence, exposure to trauma is a prerequisite for PTSD (7, 8). Additionally, military personnel experience various stressful situations, including repeated exposure to death and injuries, exhaustion and deprivation, and separation from family and friends (9–11). Furthermore, approximately 44%–72% of veterans experience high levels of stress after returning to civilian life (12) and they are at high risk of violence and aggressive traumatic-related disorders (13). Together, these conditions contribute to military personnel being more prone to PTSD.
Approximately 50% of those who have been in the military have suffered mental health problems, including PTSD (14). Similarly, studies revealed that one in five (22%) of the Australian defense force population had experienced a mental disorder in the previous 12 months (15).
PTSD is one of the signature injuries; an estimated 13%–20% of more than 2.6 million troops deployed in Iraq and Afghanistan suffer from PTSD (16). PTSD is the most frequent mental illness among military people, with a lifetime prevalence rate of 22% (17). Notably, it affects 16.8% of Australian veterans (18), 7.6% of Canadian armed forces members (19), 29% of China’s veterans (20), and 25.8% of individuals serving in the South African defense force (6). Furthermore, the prevalence ranges from 6% to 31% among combat veterans in the United States (21).
PTSD in the military causes increased suicidal behavior (22), mounting substance use behaviors (23), difficulties in the mental health of spouses (24), reduced quality of life, impaired work performance, and a decline in the quality of family life (25). PTSD is frequently associated with other mental illnesses; 83.3% of PTSD patients had a co-occurring mental illness (26). Since then, active military personnel with comorbid psychological conditions had more severe symptomatology, lower rates of recovery, higher attrition from service, and higher rates of attempted and completed suicide (27).
Despite the significant burden of PTSD among the military population, over 80% of armed forces members with mental illness did not receive medication or counseling (28). Consequently, untreated mental health conditions can lead to a decline in operational readiness, an elevated likelihood of premature separation from the military, and mortality due to suicide (29). Especially in Ethiopia, like many LMICs, primary care clinics are staffed by providers with limited training in mental health, and high staff turnover (30). This might be contributing to Ethiopia’s mounting burden of providing mental health services to military personnel.
The study in Ethiopia is limited; in a previous study, the prevalence of PTSD among Ethiopian military personnel was approximately 16% (31). Additionally, some factors such as time spent in forwarding, coping, and resilience, which were significantly associated in most others studies, were added in this study. Thus, this study aimed to determine the prevalence of PTSD and its associated factors among military personnel in a military treatment center at the Northwest Command Level Three Military Hospital in Bahir Dar.
Materials and methods
Study area and study period
The study was conducted from 21 June to 21 July 2022, at the Northwest Command Level Three Military Hospital, located in Bahir Dar city, in the Amhara region, approximately 565 km northwest of Addis Ababa, the capital city of Ethiopia. Since the rise of the conflict in northern Ethiopia between the Tigray People’s Liberation Front party and the Ethiopian National Defense Forces (32), the attacked and injured soldiers have been receiving treatment at the Northwest Command Level Three Military Hospital, which is the Ethiopian Defense Force North West Command’s residential area near Bahir Dar.
Since various hospitals provide treatments for injured troops, including the Northwest Command Level Three Military Hospital, the hospital serves as the base hospital for casualties. It renders dental, psychiatric, medical, and surgical services to outpatients and medical and surgical services to inpatients. Two Bachelor of Science (BSc) psychiatry professionals provide outpatient psychiatric services.
Study design and population
An institution-based cross-sectional study design was conducted. All admitted military personnel at the Northwest Command Level Three Military Hospital are the source population, whereas all admitted military personnel who were randomly selected during the data collection period were the study population.
Inclusion and exclusion criteria
All admitted military personnel during the data collection period who were capable of responding to the questionnaire were included in the study, whereas individuals who were seriously ill (failure to respond due to severe pain and unable to communicate) were excluded.
Sample size determination
The sample size was determined by using a single population proportion formula based on the estimated prevalence rate of PTSD of 16% taken from the previous research conducted in Ethiopia (31), with a 95% confidence level and 3% margin of error to increase the sample size, while applying the formula and the final sample size of 627 with a 10% non-response rate.
Sampling procedure
In this study, a simple random sampling technique was applied. To establish a sampling frame, we executed bed number labeling. To begin, a list of military personnel from all wards was compiled to create a single sampling frame. After selecting the military personnel and their bed numbers, assigned and labeled by four data collectors 2 days before the data collection period, a single sample frame was established. Finally, a computer-generated simple random number was used to pick study participants.
Data collection procedures
The questionnaire was initially written in English and translated into the local Amharic language by language experts. The questionnaire was then translated back into English by an independent person to verify the consistency and comprehensibility of the tool. A pre-test was also conducted on 5% (32) of participants at the Feleg hiwot compressive specialized hospital (which rendered service to military personnel during the conflict) to ensure the clarity of the questionnaires. Four BSc generic nurse data collectors and two BSc psychiatry nurse supervisors were recruited. Before data collection, the data collectors provided a comprehensive explanation of the study’s objectives to every participant. Subsequently, the participants were requested to indicate their willingness and provide written consent. Finally, the participants filled out the questionnaires provided to them. Data quality was ensured by training the data collectors 3 days before data collection and continuous monitoring of the daily evaluation of each completed questionnaire by the principal investigator, who holds a Master of Sciences degree in mental health.
Data collection tools
The military version of the PTSD questionnaire (PCL-M) was used. The PTSD Checklist-Military Version is a self-report rating scale that assesses the severity of PTSD symptoms in the military. Participants respond with a five-point Likert scale ranging from 1 (not at all) to 5 (extremely) (1 = not at all, 2 = a little bit, 3 = moderately, 4 = quite a bit, and 5 = extremely). This score is calculated by summing all of the scale item responses together. The overall score can vary from 17 to 85, with higher levels indicating more seriousness. Ratings are based on current DSM criteria, based on how much a veteran has been affected by a specific traumatic military-related event, with a sensitivity of 0.82, a specificity of 0.83, and an internal consistency of 0.97 (33). The local language-translated version of PCL-M has demonstrated good reliability in this study, exhibiting a Cronbach’s alpha coefficient of 0.93. The PCL-M has been employed in prior research conducted in Ethiopia, demonstrating commendable reliability in assessing PTSD among military personnel receiving hospital care (31). Furthermore, it has been utilized in numerous studies conducted on military populations (34, 35).
The Patient Health Questionnaire (PHQ-9), a nine-item self-report questionnaire, was employed to assess depression, with a four-point ordinal scale used for scoring purposes. Individuals with a PHQ-9 score equal to or exceeding 10 were screened for depression, with scores ranging from 5 to 27. Validation studies conducted in adult populations in Ethiopia indicated a sensitivity of 86% and a specificity of 67% for the PHQ-9 (36). PHQ-9 has good measure of depression among the military population.
Combat exposure was measured on the Critical War Zone Experience scale. The combat exposure scale consisted of seven items assessing experiences. Participants were asked to indicate how often they experienced each combat stressor using a five-point Likert scale from 0 (“never”) to 4 (“10+ times”) and to respond based on the frequency of their experiences, such as “seeing ill or injured women or children who you were unable to help,” “being directly responsible for the death of an enemy combatant,” and “having a buddy shot or hit who was near you.” It was validated for PTSD in veterans’ clinics. The scale has a high alpha coefficient of 0.73 (37). The overall combat exposure score was created by summing across all scale items. The level of combat exposure was classified into four groups (low, medium, high, and very high) in accordance with a similar study done previously (38).
The patient’s life threat was measured using the perceived stress scale, which has possible scores ranging from 0 to 40 on a five-point Likert scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often). This tool was validated in Ethiopian university students, and its Cronbach’s alpha value of internal consistency was 0.80 (39).
The Brief Resilience Coping Scale measures a five-point scale response ranging from 1 (does not describe me at all) to 5 (very well describes me). Total sum scores range from 4 to 20. Scores of 4–13 indicate low resilient coping, 14–16 indicate medium resilient coping, and 17–20 indicate high resilient coping, which have adequate internal consistency (r = 0.76) and test–retest reliability (r = 0.71) (40). The Oslo-3 scale, which ranges from 3 to 8, was used to assess social support. The total score ranged from 3 to 14 on the OSS-3 questionnaire; sub-domain scores of “3–8,” “9–11,” and “12–14” indicate poor social support, intermediate social support, and strong social support, respectively (41).
Types of combat exposures were assessed as yes or no and were adapted from the Army Mental Health Advisory Team combat exposure scale and different literature (38). The patients’ background information was assessed using a questionnaire that included sociodemographic and military-related demographic data. Child abuse (physical, sexual, and neglect) was assessed with yes or no questions. The respondents’ yes/no responses were analyzed to evaluate their history of substance use and clinical factors, which will be operationalized based on different literary works.
Data processing and analysis
After ensuring the completeness of the data, it was entered into Epi Data version 4.46 and then exported to Statistical Package for Social Science version 25.0. Dependent and independent variables in the study were described using descriptive statistics such as mean, standard deviation, frequency, and percentage. The results were visually presented through graphs and tables.
To identify PTSD and related factors, bivariate and multivariate binary logistic regression analyses were used. Variables that are significant in bivariate analysis (with a p-value 0.25) were considered for multivariable logistic regression analysis. The adjusted odds ratio (AOR) at the 95% confidence interval was used to evaluate the strength of the association. A p-value of 0.05 in multivariate logistic regression was deemed statistically significant. The goodness of the model fit was evaluated using the Hosmer and Lemeshow test, yielding a value of 0.93.
Results
A total of 627 participants with a response rate of 97.6% participated in this study. The mean age of the respondents was 30 years, with a standard deviation of ±6.4 years. Among the participants, 278 individuals (36.6%) were aged 30 years and older, with 466 (76.1%) being men and 261 (42.6%) identifying as orthodox followers. As regards educational status, 228 participants (37.3%) were in grades 9–12.
Regarding military characteristics, most respondents were non-commissioned officers [507 (82.6%)], mean age at first deployment was 25 years with a standard deviation of ±3.1, and the majority of the respondents [526 (85.9%)] had more than one deployment (Table 1).
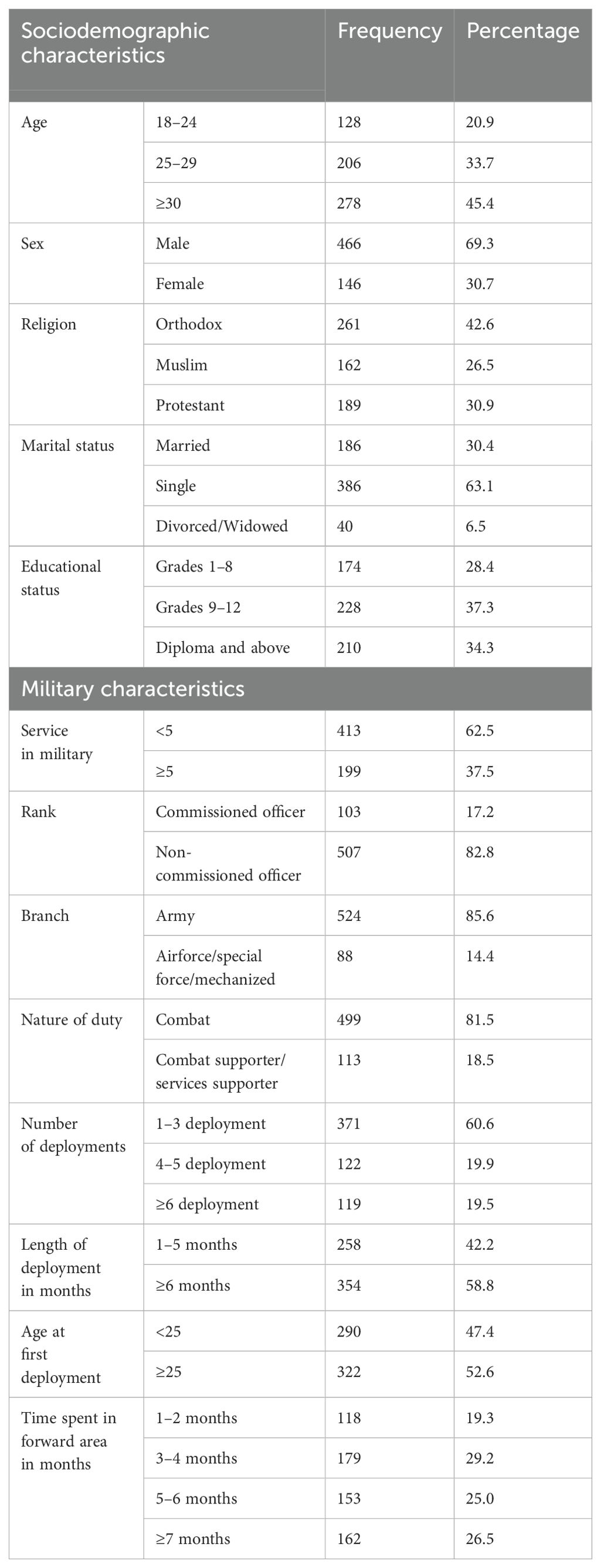
Table 1. Sociodemographic and military characteristics of military personnel, Northwest Command Level Three Military Hospital, Ethiopia, 2022 (n = 612).
Substance-related factors
Out of the 612 participants, 234 individuals (38.1%) reported ever use of alcohol, while approximately 10.2% of the respondents indicated current alcohol consumption (Figure 1).
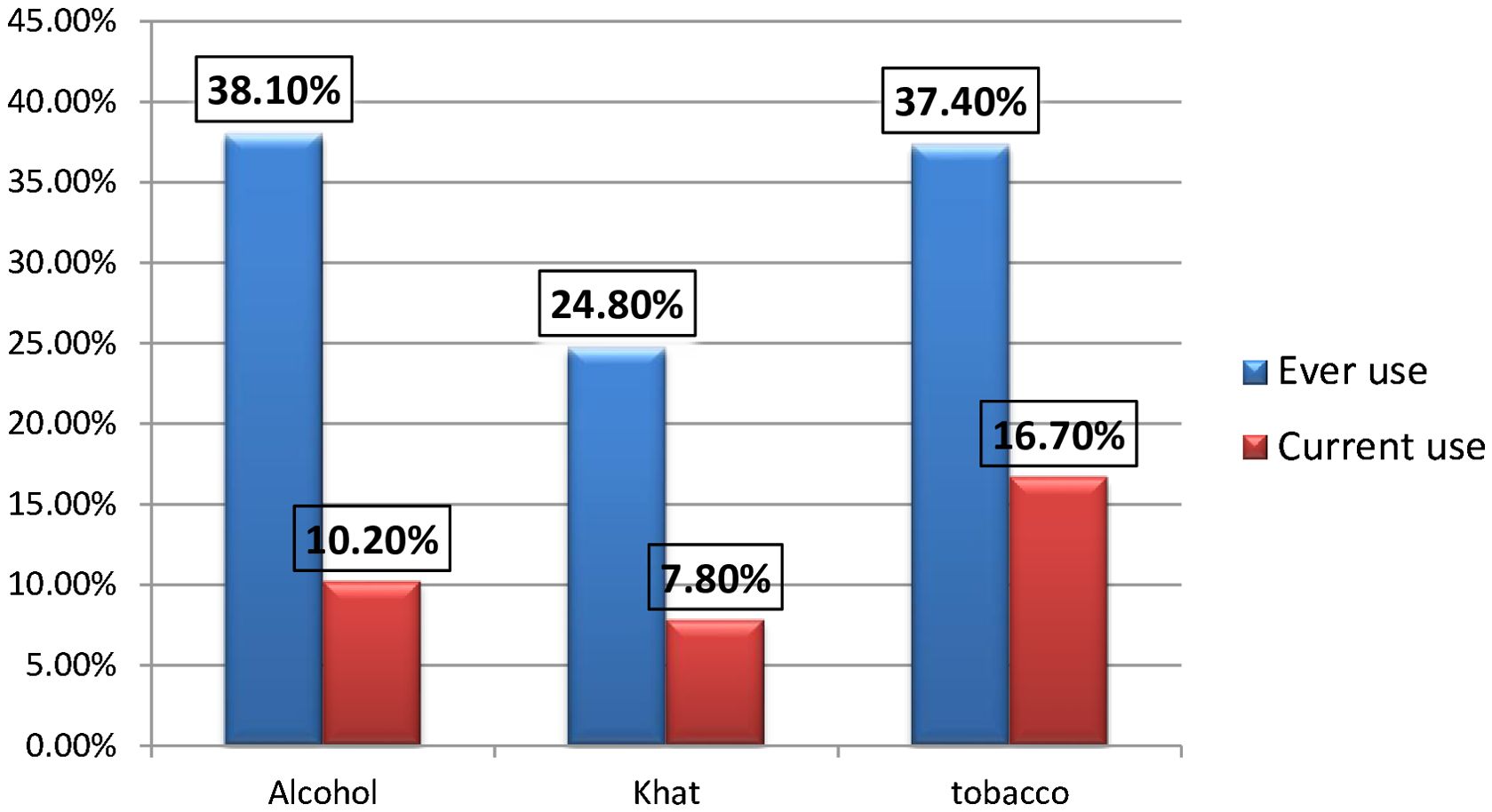
Figure 1. Showing the distribution of substance-related factors of the respondents among military personnel Northwest command level three military hospital, Ethiopia 2022 (n=612).
Clinical factors of the respondents
Approximately 40 participants (6.5%) reported a family history of mental illness, while 62 participants (10.1%) had a known history of chronic medical illness. Overall, 172 (28.1%) of all participants were found to have depression (Table 2).
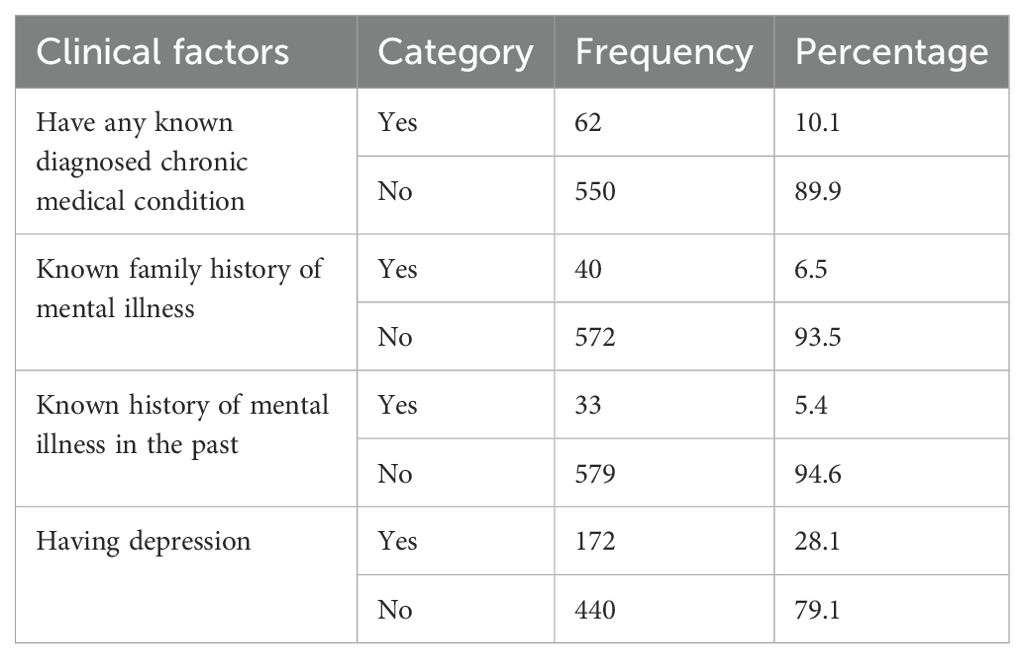
Table 2. Clinical factors of the respondents (military personnel, Northwest Command Level Three Military Hospital, Ethiopia, 2022; n = 612).
Combat trauma exposure factors
The majority of the respondents, 466 (76.1%) and 497 (81.2%), have experience handling dead bodies and have faced being shot or receiving small arms fire, respectively. Regarding combat exposure, 175 (28.6%) of the participants had high combat exposure (Table 3).
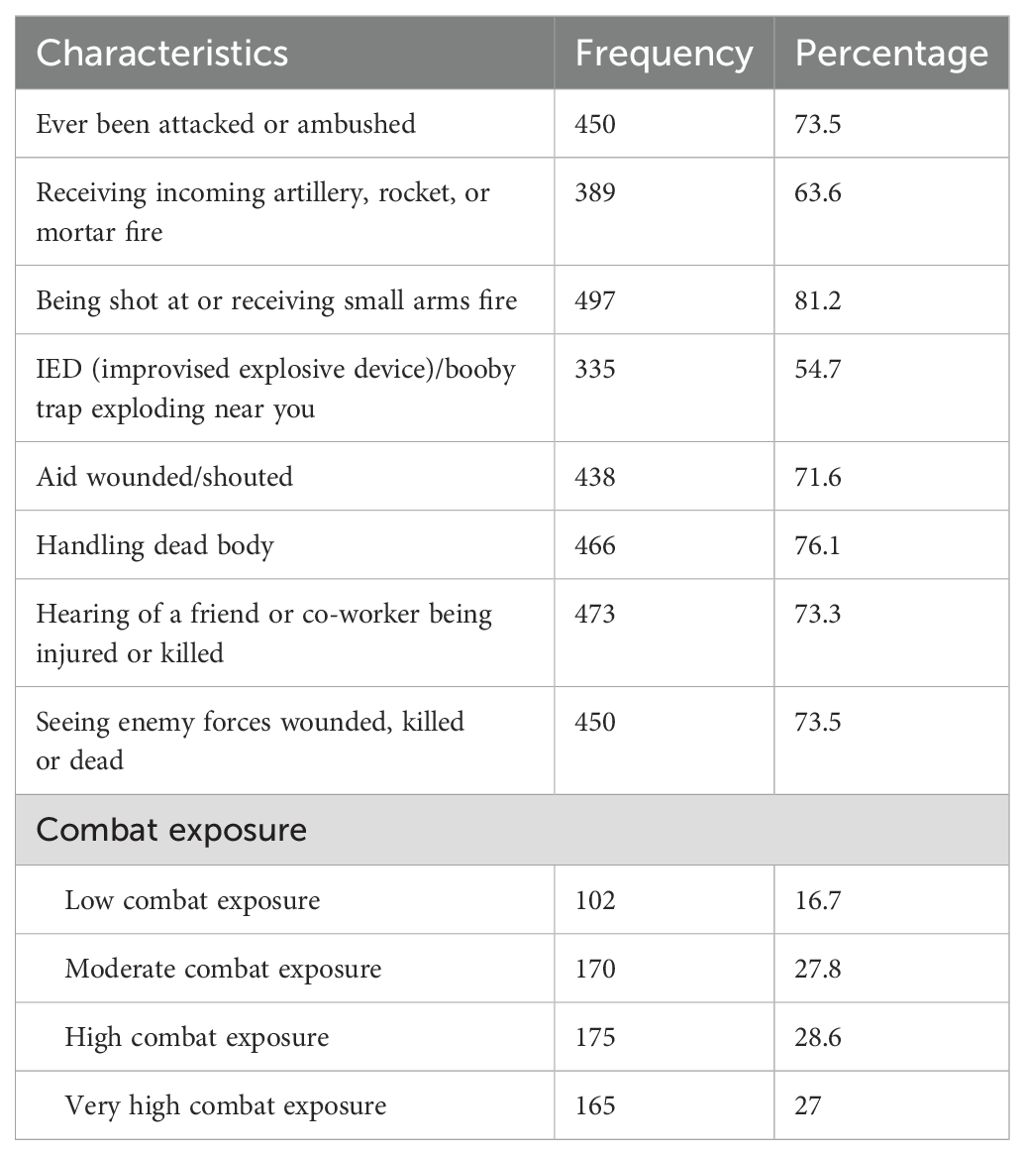
Table 3. Distribution of combat trauma exposure factors of the respondents (military personnel, Northwest Command Level Three Military Hospital, Ethiopia, 2022; n = 612).
Psychosocial factors
Out of the 612 participants, almost half, 285 (45.9%), reported having strong social support. Additionally, one-quarter of the participants, 155 (25.3%), reported a high perceived life threat, while 94 individuals (15.4%) disclosed experiencing childhood physical abuse and neglect in the past (Table 4).
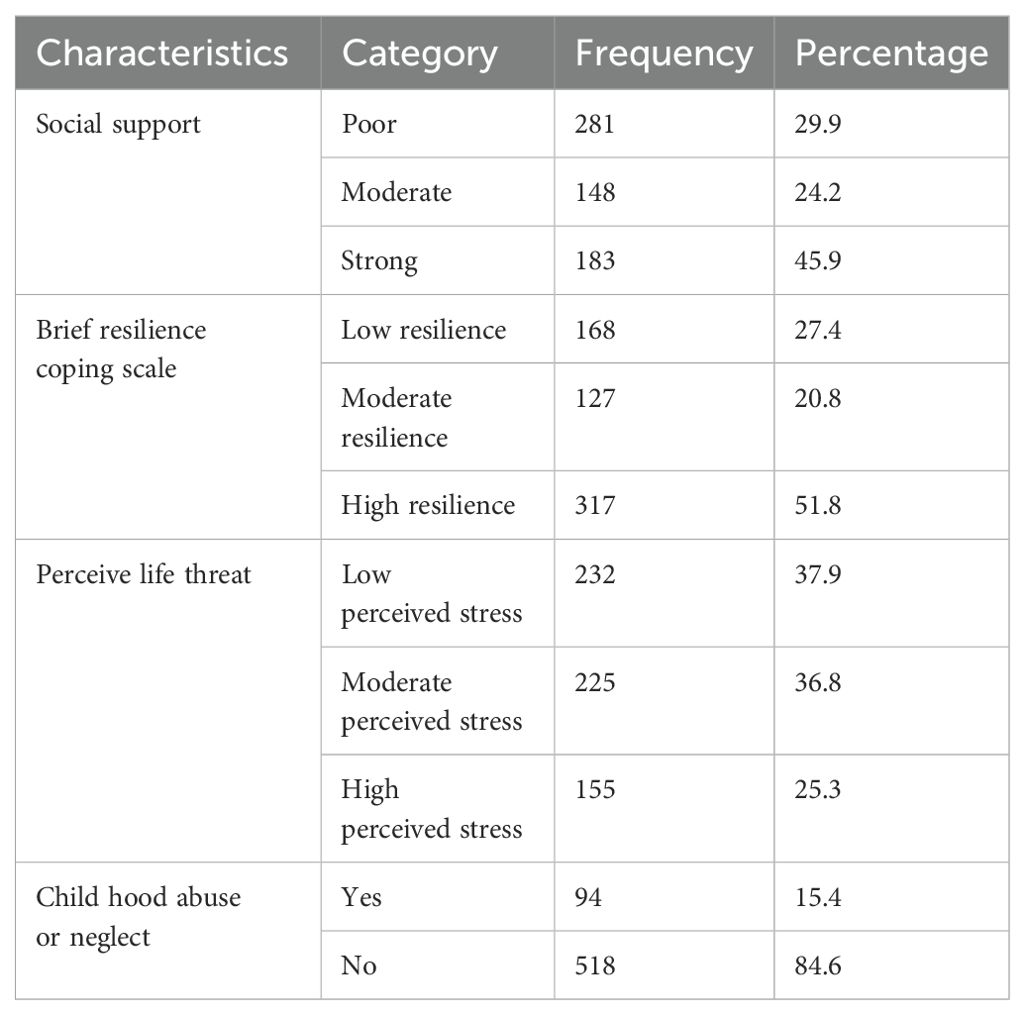
Table 4. Distribution of psychosocial factors of the respondents (military personnel, Northwest Command Level Three Military Hospital, Ethiopia, 2022; n = 612).
Prevalence of PTSD
The prevalence of PTSD in this population was 21.9% (95% CI: 18.6, 25.2).
Factors associated with post-traumatic stress disorder
To determine the association of independent variables with PTSD, bivariate and multivariate binary logistic regression analyses were carried out.
On the bivariate analysis of PTSD to each explanatory variable: female sex, number of deployments, nature of duty in the military, single, history of mental illness, family history of mental illness, experiencing childhood physical trauma and neglect, depression, combat exposures, brief resilience scale, handling dead bodies, aiding wounded, being attacked or ambushed, receiving in coming artillery, being shot at or receiving incoming small arms fire, and seeing enemy forces wounded, killed, or dead were found to be significant at a p-value less than 0.25.
These factors were entered into multivariable binary logistic regression for further analysis. In multivariate analysis, female sex, a larger number of deployments, combat participants, poor social support, low resilience copers, handling dead bodies, very high combat exposures, and depression were significantly associated with PTSD at a p-value less than 0.05.
Being female was 2.3 times more likely to develop PTSD as compared with those male respondents (AOR = 2.3, 95% CI; 1.3, 3.87). The odds of developing PTSD was three times higher among respondents who participated as combat personnel as compared with those respondents who participated as combat supporters and combat service supporters (AOR = 2.75, 95% CI: 1.44, 6.36). Handling dead bodies increased the odds of PTSD by 2.5 times (AOR = 2.5, 95% CI, 1.24, 5.02), whereas the odds of PTSD were 2.94 times higher with 4–5 deployments (AOR = 2.94, 95% CI: 1.63, 5.32) and 3.4 times higher with ≥6 deployments (AOR = 3.4, 95% CI, 1.95, 6.17) as compared to 1–3 deployments (Table 5).
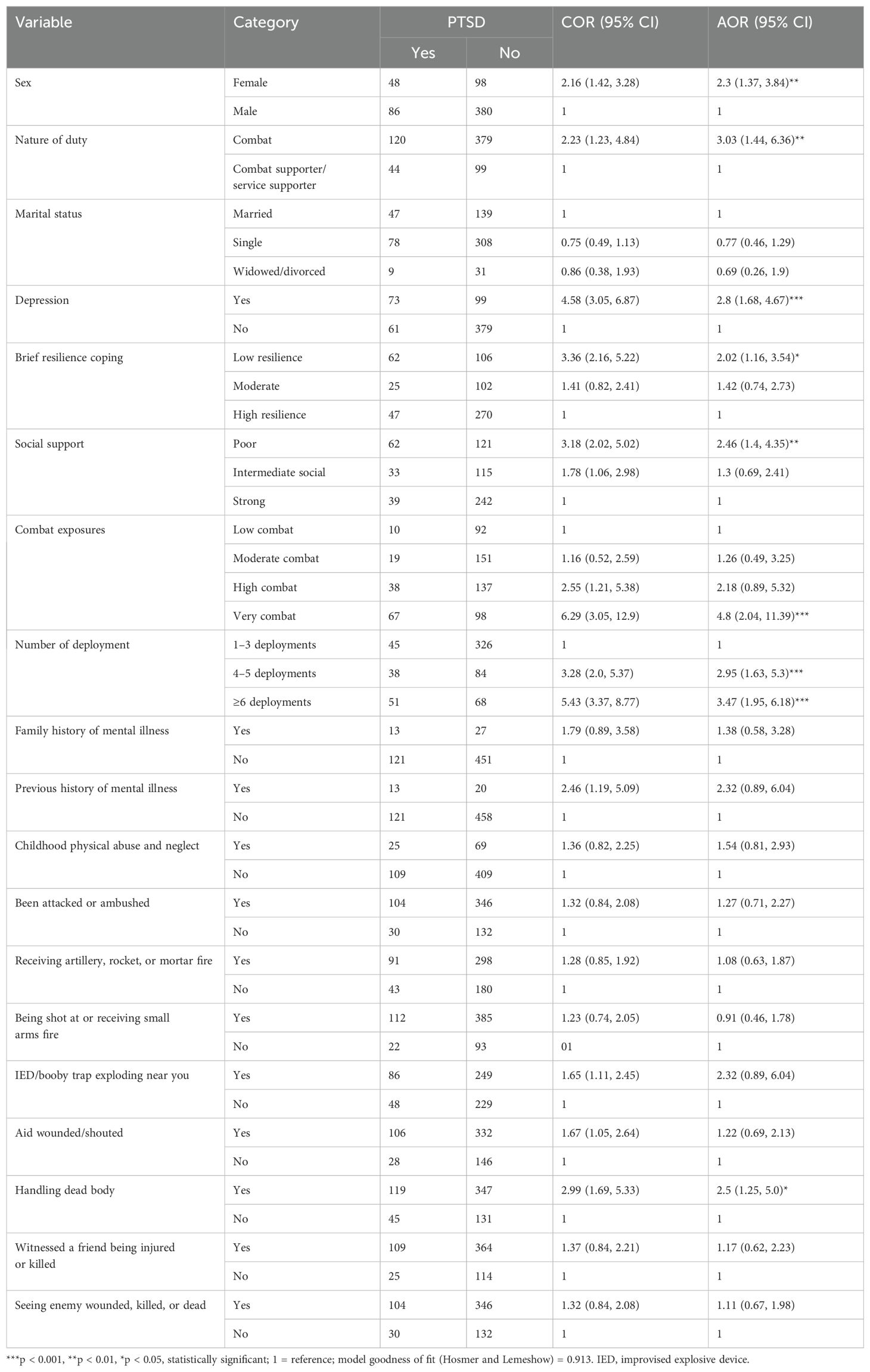
Table 5. Bivariable and multivariable independent factors of PTSD among respondents (military personnel, Northwest Command Level Three Military Hospital, Ethiopia, 2022; n = 612).
Respondents with low resilience were twice as likely to develop PTSD as those with high resilience (AOR = 2.0, 95% CI: 1.16, 3.53), and those with low social support had 2.46 times higher odds of PTSD compared to individuals with strong social support (AOR = 2.46, 95% CI: 1.39, 4.35). Additionally, the likelihood of developing PTSD was 4.8 times greater for respondents who experienced very high combat exposure relative to those with low exposure (AOR = 4.81, 95% CI: 2.03, 11.93). The odds of developing PTSD were 2.80 times higher among those respondents who had depression than those who had no depression (AOR = 2.8, 95% CI: 1.68, 4.67).
Discussion
The military community at large, as well as those who have experienced combat battle in the war, may be adversely affected by PTSD. The prevalence of PTSD in this study was 21.9% (95% CI: 18.6, 25.2). This finding was in line with the studies conducted among US military personnel (25.1%) (42), Nepal’s army combatants (21.9%) (35), UK combat-injured military personnel (18.5%) (43), US soldiers exposed to combat (19%) (44), and admitted veterans in Nigeria (22%) (45).
On the other hand, the outcome of this study indicated a PTSD prevalence of 21.9%, which was lower than those of earlier studies on South African military veterans (33%) (46)., military veterans in China’s Xinjiang region (29%) (20), soldiers with amputation of a limb or spinal injury in Sri Lanka (41.7%) (47), New Zealand military personnel (30%) (34), US military service members (47%) (48), and US War Veterans Health Care clinic patients (37.8%) (49).
The possible reason for the high prevalence among Sri Lankan military personnel is that the study focuses on those who have suffered spinal injuries and amputations; as a result, individuals who have undergone amputations have higher rates of anxiety and depression (50), which are associated with PTSD. Furthermore, the severity of the trauma predicts the onset of PTSD (51). Likewise, there is increased prevalence in the study done in Western countries, the US (48, 49), and New Zealand (34). It might be that Ethiopia has intimate family structures and a stronger extended family system than Western nations. According to the study, strong support networks (family and community) can enhance resilience and help to mitigate the psychological effects of severe battlefield injuries, including PTSD (52, 53).
Furthermore, the research carried out in South Africa employed a non-probability sampling method that utilized convenience and snowball sampling techniques. Similarly, it could be a sample size difference, an instrument difference (lower PCL-C cutoff of <30 in the New Zealand military), a lower cutoff point that increases the magnitude of PTSD, and possible sociocultural differences that contribute to the difference.
This study had a PTSD prevalence of 21.9%, which is higher than the 15.5% reported in an earlier study at an Ethiopian military hospital (31). The difference might be that the current study was undertaken during the conflict, and those who have deployment-related injuries and combat exposure could be a possible factor, because combat exposure and minor wounds and injuries increase the prevalence of PTSD (54, 55). Additionally, the lifetime prevalence of PTSD is two to three times higher in the injured than in the uninjured (42).
The result of this study is also higher than studies done on hospitalized US soldiers with combat injuries (4.2%) (55), Australian veteran peacekeepers (16.8%) (18), Canadian armed forces (7.6%) (19), war veterans in Kosovo (11.2%) (56), UK armed forces personnel (3.5%) (57), and Nepali army personnel and veterans (9%) (58). The low PTSD prevalence rates in the research done in Kosovo (56) and Canadian armed forces (59) could be due to the fact that the research involved non-admitted and non-injured military personnel, which would contribute to a lower chance of reporting PTSD (60). The delay in starting the study and the occurrence of trauma 15 years after the insurgency in Nepal’s military army (58) and 8 years after the war in Kosovo might contribute to the difference (56). Evidence showed that after 1 year of the occurrence of trauma, the prevalence of PTSD decreased by 50% (61). Additionally, the difference might also be due to a difference in the instruments (Harvard Trauma Questionnaire-40 HTQ, WHO’s Composite International Diagnostic Interview).
As regards the independent predictors of PTSD among admitted military personnel, female sex, low social support, a greater number of deployments, depression, low brief resilience, very high combat exposure, and handling dead bodies are significantly associated with PTSD.
In this study, being female was significantly associated with PTSD. This finding was supported in previous studies (62–65). The possible reason might be that women have experienced more sexual and gender harassment than men. This is evidenced by the data indicating that half of military women face some type of gender harassment each year (66), and have experienced military sexual trauma each year (67), suggesting that gender harassment and military sexual trauma are negatively associated with mental health outcomes, including PTSD (68).
Respondents who participated as combat personnel were 3.0 times more likely to develop PTSD than respondents who participated as combat supporters and combat service supporters. The possible reason could be that combat personnel could have been more susceptible to enemy attack, deployment, and combat exposure (23). Data revealed a threefold increase in PTSD symptoms or diagnoses among deployed military personnel who reported combat exposures than among deployed military personnel who did not report combat exposures (68). This result is in line with previous studies (69, 70).
Participants who had a higher cumulative length of deployment (i.e., ≥4 deployments) were more likely to develop PTSD as compared with respondents with a lower cumulative length of deployment. This was supported by previous studies (69, 71). This is implicated by multiple deployments, which are thought to be an underlying factor in the high prevalence of substance use disorders (72). Thus, substance abuse prevents the body from naturally resolving trauma-related discomfort, increases physiologic arousal, and exacerbates PTSD symptoms (73).
Likewise, military personnel who had poor social support were 2.46 times more likely to develop PTSD as compared with those who had strong social support. This was also affirmed by previous studies (31, 69, 74–76). Findings consistently demonstrate that people who receive greater social support are better able to handle crises. In contrast, those with less social support could find it more challenging to heal from trauma (77).
The odds of developing PTSD were two times higher among respondents who had low resilience than among those who had high resilience. This was supported by a previous study (76). It is evidenced by a high level of resilience, which is a protective factor against unfavorable consequences, such as PTSD. People with high levels of resilience are less likely to experience PTSD symptoms after a traumatic event (52). In addition, low emotional resilience and stress response have been linked to deficits in the catechol-O-methyltransferase Val158 Met polymorphism, i.e., an enzyme that metabolizes important nucleotides for PTSD, which is shown to affect the risk of developing PTSD (78).
Military personnel who had very high combat exposures were 4.8 times more likely to develop PTSD as compared with those who had experienced low combat exposures. This was also affirmed by previous studies (23, 48, 55, 69, 79). Moreover, the odds of developing PTSD were 2.5 times higher among respondents who had experienced handling dead bodies than those who had not. Other studies also found that military members who have encountered high combat situations are at an increased risk of developing PTSD (31). Military personnel who had depression were 2.8 times more likely to develop PTSD than respondents who had no depression. This finding was supported by the results of previous studies (48, 56).
Overall, the military population is characterized by a notable prevalence of PTSD, which exerts a paramount influence on society, families, and individuals. The substantial impact of depression and other co-occurring conditions should not be overlooked and requires due consideration. Especially for individuals who have actively participated in combat and/or multiple deployments and have endured injuries and hospitalization during military activities, there exists a pressing need for comprehensive and easily accessible therapy and monitoring to effectively address their PTSD.
Limitations
The cross-sectional nature of the study design might not show temporal relationships between PTSD and its predictors. There may be recall bias in some tools especially for the duration of deployment and number of deployments. Moreover, important factors such as sleep pattern that cause PTSD have been missed, which could predict PTSD.
Conclusion
According to this study, the prevalence of PTSD in Ethiopia is significant among hospitalized military personnel. One in five admitted military personnel had screened positive for PTSD. Additionally, it was also found that female sex, low social support, a greater number of deployments, depression, low brief resilience, very high combat exposure, and handling dead bodies are significantly associated with PTSD. Moreover, the abovementioned military experiences and sociodemographic and clinical factor profiles need to be considered during the design and implementation of psychosocial interventions for military personnel. A longitudinal study is recommended to gain a better understanding of the causal relationship between PTSD and its associated risk factors.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
Ethical clearance was obtained from the institutional ethical review Board of Bahir Dar University College of Medicine and Health Sciences with protocol number 497/2022 and a permission letter was obtained from the Amhara Public Health Institute. Finally, permission was obtained from North West Command of the Ethiopian Defense Force administrative office of level three military hospital. All study participants were asked about their willingness to participate and provided informed signed consent.
Author contributions
AT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. GL: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. BM: Conceptualization, Methodology, Software, Writing – original draft, Writing – review & editing. MT: Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. MB: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We express our gratitude to the Bahir Dar University College of Medicine and Health Sciences for their invaluable support and assistance. Additionally, we extend our acknowledgment to the administrative office staff of the Northwest Command Level Three Military Hospital, the dedicated data collectors, supervisors, and the study participants for their valuable time and unwavering effort.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; CIDI, Composite International Diagnostic Interview; DALYs, disability-adjusted life years; LMICs, low- and middle-income countries; IED, improvised explosive device; IES-R, Impact of Event Scale-Revised; OR, odds ratio; OSSS, Oslo Social Support scale; PTSD, post-traumatic stress disorder; PCL-M, post-traumatic stress disorder military version; PHQ9, Patient Health Questionnaire; SPSS, Statistical Packages for Social Sciences; WHO, World Health Organization; YLDs, years lived with disability.
References
1. Association AP. DSM 5 Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Publishing (2013). p. 947.
2. Koenen K, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the world mental health surveys. psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708
3. Ayuso-Mateos JL. Global Burden of post-traumatic stress disorder in the year 2000: version 1 estimates. Geneva, World Health Organ (2002).
4. Hoppen TH, et al. Global burden of post-traumatic stress disorder and major depression in countries affected by war between 1989 and 2019: a systematic review and meta-analysis. BMJ Global Health. (2021) 6:e006303. doi: 10.1136/bmjgh-2021-006303
5. Kok BC, et al. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling prevalence differences between studies. J nervous Ment Dis. (2012) 200:444–50. doi: 10.1097/NMD.0b013e3182532312
6. Seedat S, Roux C.l., Stein DJ. Prevalence and characteristics of trauma and post-traumatic stress symptoms in operational members of the South African National Defence Force. Military Med. (2003) 168:71–5. doi: 10.1093/milmed/168.1.71
7. Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. psychol Med. (2016) 46:327–43. doi: 10.1017/S0033291715001981
8. Compean E, Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Prog Neuropsychopharmacol Biol Psychiatry. (2019) 88:265–75. doi: 10.1016/j.pnpbp.2018.08.001
9. Hruby A, Lieberman HR, Smith TJ. Symptoms of depression, anxiety, and post-traumatic stress disorder and their relationship to health-related behaviors in over 12,000 US military personnel: Bi-directional associations. J Affect Disord. (2021) 283:84–93. doi: 10.1016/j.jad.2021.01.029
10. Brooks SK, Greenberg N. Non-deployment factors affecting psychological wellbeing in military personnel: literature review. J Ment Health. (2018) 27:80–90. doi: 10.1080/09638237.2016.1276536
11. Inoue C, et al. Veteran and military mental health issues. In: StatPearls. StatPearls Publishing LLC, Treasure Island (FL (2022).
12. Mobbs MC, Bonanno GA. Beyond war and PTSD: The crucial role of transition stress in the lives of military veterans. Clin Psychol Rev. (2018) 59:137–44. doi: 10.1016/j.cpr.2017.11.007
13. Hecker T, et al. Treating traumatized offenders and veterans by means of narrative exposure therapy. Front Psychiatry. (2015) 6:80. doi: 10.3389/fpsyt.2015.00080
14. Asare-Doku W, Donnir GM, Ae-Ngibise KA, Peprah J, Awuviry-Newton K, Acquah F, et al. Psychiatric disorders among the military in West Africa: A systematic narrative review. Behav Sci. (2021) 11:138. doi: 10.3390/bs11100138
15. Van Hooff M, McFarlane AC, Davies CE, Searle AK, Fairweather-Schmidt AK, Verhagen A, et al. The Australian defence force mental health prevalence and wellbeing study: design and methods. Eur J Psychotraumatol. (2014) 5:23950. doi: 10.3402/ejpt.v5.23950
16. Committee on the assessment of ongoing effects in the treatment of posttraumatic stress, D. and M. Institute of. In: Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. National Academies Press (US, Washington (DC.
17. Sareen J, Bolton S-L, Mota N, Afifi TO, Enns MW, Taillieu T, et al. Lifetime Prevalence and Comorbidity of Mental Disorders in the Two-wave 2002-2018 Canadian Armed Forces Members and Veterans Mental Health Follow-up Survey (CAFVMHS): Prévalence et Comorbidité de Durée de vie Des Troubles Mentaux Dans l’Enquête de Suivi Sur la Santé Mentale Auprès des Membres des Forces Armées Canadiennes et Des ex-Militaires (ESSMFACM) en Deux Cycles de 2002 à 2018. Can J Psychiatry. (2021) 66:951–60. doi: 10.1177/07067437211000636
18. Forbes D, O'Donnell M, Brand RM, Korn S, Creamer M, McFarlane AC, et al. The long-term mental health impact of peacekeeping: prevalence and predictors of psychiatric disorder. BJPsych Open. (2016) 2:32–7. doi: 10.1192/bjpo.bp.115.001321
19. Nazarov A, et al. Greater prevalence of post-traumatic stress disorder and depression in deployed Canadian Armed Forces personnel at risk for moral injury. Acta Psychiatrica Scandinavica. (2018) 137:342–54. doi: 10.1111/acps.12866
20. Liu B, Li R, Lu D, Zhao J, Guan S, Tang J, et al. Risk factors associated with post-traumatic stress disorder among Uyghur and Han veterans in Xinjiang region of China. Int J Clin Exp Med. (2016) 9:22232–40.
21. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. (2010) 44:4–19. doi: 10.3109/00048670903393597
22. Arenson MB, Whooley MA, Neylan TC, Maguen S, Metzler TJ, Cohen BE, et al. Posttraumatic stress disorder, depression, and suicidal ideation in veterans: Results from the mind your heart study. Psychiatry Res. (2018) 265:224–30. doi: 10.1016/j.psychres.2018.04.046
23. Abel J, Anongo FS, Dami BE, Ogbole AJ, Abel A, Dagona ZK, et al. Combat exposure and peritraumatic factors predicting PTSD among military personnel fighting insurgency in Nigeria. J Anxiety Depression. (2018) 1:108. doi: 10.46527/2582-3264.108
24. Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran’s family and possible interventions. Aggression violent Behav. (2004) 9:477–501. doi: 10.1016/S1359-1789(03)00045-4
25. Vogt D, Smith BN, Fox AB, Amoroso T, Taverna E, Schnurr PP, et al. Consequences of PTSD for the work and family quality of life of female and male US Afghanistan and Iraq War veterans. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:341–52. doi: 10.1007/s00127-016-1321-5
26. Walter KH, et al. Prevalence of posttraumatic stress disorder and psychological comorbidities among U.S. Active duty service members, 2006-2013. J Trauma Stress. (2018) 31:837–44. doi: 10.1002/jts.22337
27. Walter KH, et al. Prevalence of posttraumatic stress disorder and psychological comorbidities among US active duty service members, 2006–2013. J Traumatic Stress. (2018) 31:837–44. doi: 10.1002/jts.22337
28. Thériault FL, Gardner W, Momoli F, Garber BG, Kingsbury M, Clayborne Z, et al. Mental health service use in depressed military personnel: a systematic review. Military Med. (2020) 185:e1255–62. doi: 10.1093/milmed/usaa015
29. Thyloth M, Singh H, Subramanian V. Increasing burden of mental illnesses across the globe: current status. Indian J Soc Psychiatry. (2016) 32:254. doi: 10.4103/0971-9962.193208
30. Ng LC, et al. Posttraumatic stress disorder intervention for people with severe mental illness in a low-income country primary care setting: a randomized feasibility trial protocol. Pilot Feasibility Stud. (2021) 7:149. doi: 10.1186/s40814-021-00883-3
31. Amare TA, Mohamedhagos H, Awoke T. Prevalence and factors associated with post-traumatic stress disorder among military personnel admitted to Armed Forces Referral and Teaching Hospital, Addis Ababa, Ethiopia: Cross-sectional study. East Afr J Health Sci. (2019) 1:116–27.
32. Plaut M. The International community struggles to address the Ethiopian conflict. London, RUSI Newsbrief RUSI (2021).
33. Weathers FW, et al. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In: annual convention of the international society for traumatic stress studies. San Antonio, TX (1993).
34. Richardson A, Gurung G, Samaranayaka A, Gardner D, deGraaf B, Wyeth EH, et al. Risk and protective factors for post-traumatic stress among New Zealand military personnel: A cross sectional study. PloS One. (2020) 15:e0231460. doi: 10.1371/journal.pone.0231460
35. Rawal N, et al. Factors associated with post traumatic stress disorder and depression among Nepalese combatants during armed insurgency. J Psychiatrists’ Assoc Nepal. (2017) 6:24–8. doi: 10.3126/jpan.v6i1.21768
36. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210:653–61. doi: 10.1016/j.psychres.2013.07.015
37. Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gullive SB, et al. The Critical Warzone Experiences (CWE) Scale: Initial psychometric properties and association with PTSD, anxiety, and depression. Psychiatry Res. (2014) 220:1118–24. doi: 10.1016/j.psychres.2014.08.053
38. Booth-Kewley S, Larson GE, Highfill-McRoy RM, Garland CF, Gaskin TA, et al. Correlates of posttraumatic stress disorder symptoms in Marines back from war. J Traumatic Stress. (2010) 23:69–77. doi: 10.1002/jts.20485
39. Manzar MD, Salahuddin M, Peter S, Alghadir A, Anwer S, Bahammam AS, et al. Psychometric properties of the perceived stress scale in Ethiopian university students. BMC Public Health. (2019) 19:1–8. doi: 10.1186/s12889-018-6310-z
40. Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. (2004) 11:94–101. doi: 10.1177/1073191103258144
41. Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC geriatrics. (2012) 12:1–12. doi: 10.1186/1471-2318-12-27
42. MacGregor AJ, et al. Deployment-related injury and posttraumatic stress disorder in US military personnel. Injury. (2013) 44:1458–64. doi: 10.1016/j.injury.2012.10.009
43. Forbes HJ, Jones N, Woodhead C, Greenberg N, Harrison K, White S, et al. What are the effects of having an illness or injury whilst deployed on post deployment mental health? A population based record linkage study of UK Army personnel who have served in Iraq or Afghanistan. BMC Psychiatry. (2012) 12:1–11. doi: 10.1186/1471-244X-12-178
44. Hoge CW, et al. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. Lancet Psychiatry. (2014) 1:269–77. doi: 10.1016/S2215-0366(14)70235-4
45. Okulate G, Jones O. Post-traumatic stress disorder, survivor guilt and substance use-a study of hospitalised Nigerian army veterans. South Afr Med J. (2006) 96:144–6.
46. Connell M, et al. Post traumatic stress disorder and resilience in veterans who served in the South African border war: original. Afr J Psychiatry. (2013) 16:430–6. doi: 10.4314/ajpsy.v16i6.55
47. Abeyasinghe NL, et al. The prevalence of symptoms of Post-Traumatic Stress Disorder among soldiers with amputation of a limb or spinal injury: A report from a rehabilitation centre in Sri Lanka. Psychology Health Med. (2012) 17:376–81. doi: 10.1080/13548506.2011.608805
48. Armenta RF, et al. Factors associated with persistent posttraumatic stress disorder among US military service members and veterans. BMC Psychiatry. (2018) 18:1–11. doi: 10.1186/s12888-018-1590-5
49. Jakupcak M, et al. Posttraumatic stress and its relationship to physical health functioning in a sample of Iraq and Afghanistan War veterans seeking postdeployment VA health care. J nervous Ment Dis. (2008) 196:425–8. doi: 10.1097/NMD.0b013e31817108ed
50. Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disability Rehabil. (2004) 26:837–50. doi: 10.1080/09638280410001708869
52. Thompson NJ, et al. Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord. (2018) 225:153–9. doi: 10.1016/j.jad.2017.08.049
53. Kopinak JK. Mental health in developing countries: challenges and opportunities in introducing western mental health system in Uganda. Int J MCH AIDS. (2015) 3:22.
54. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Jama. (2007) 298:2141–8. doi: 10.1001/jama.298.18.2141
55. Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE. Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry. (2006) 163:1777–83. doi: 10.1176/ajp.2006.163.10.1777
56. Shahini M, Shala M. Post-traumatic stress disorder in Kosovo veterans. SAGE Open. (2016) 6:2158244016633737. doi: 10.1177/2158244016633737
57. Goodwin L, et al. Prevalence of delayed-onset posttraumatic stress disorder in military personnel: is there evidence for this disorder? Results of a prospective UK cohort study. J nervous Ment Dis. (2012) 200:429–37. doi: 10.1097/NMD.0b013e31825322fe
58. Rawal NM, et al. Prevalence of Post-Traumatic Stress Disorder and its Associated Factors among Nepali Army Service Members and Veterans: 15 Years Post Insurgency. Nepal Med Coll J. (2021) 23:281–9. doi: 10.3126/nmcj.v23i4.42208
59. Zamorski MA, Bennett RE, Rusu C, Weeks M, Boulos D, Garber BG, et al. Prevalence of past-year mental disorders in the Canadian armed forces, 2002-2013. Can J Psychiatry. (2016) 61:26s–35s. doi: 10.1177/0706743716628854
60. Dyball D, Bennett AN, Schofield S, Cullinan P, Boos CJ, Bull AMJ, et al. Mental health outcomes of male UK military personnel deployed to Afghanistan and the role of combat injury: analysis of baseline data from the ADVANCE cohort study. Lancet Psychiatry. (2022) 9:547–54. doi: 10.1016/S2215-0366(22)00112-2
61. Sadock BJ. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. Philadelphia: Lippincott Williams & Wilkins (2007).
62. Dobie DJ, et al. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Internal Med. (2004) 164:394–400. doi: 10.1001/archinte.164.4.394
63. Brunet A, et al. Trauma exposure and posttraumatic stress disorder in the Canadian military. Can J Psychiatry. (2015) 60:488–96. doi: 10.1177/070674371506001104
64. Lehavot K, et al. Post-traumatic stress disorder by gender and veteran status. Am J Prev Med. (2018) 54:e1–9. doi: 10.1016/j.amepre.2017.09.008
65. Smith TC, et al. PTSD prevalence, associated exposures, and functional health outcomes in a large, population-based military cohort. Public Health Rep. (2009) 124:90–102. doi: 10.1177/003335490912400112
66. Lipari RN, et al. 2006 Gender Relations of Active-Duty Members. Arlington, Defense Manpower Data Center Arlington VA (2008).
67. Yaeger D, et al. DSM-IV diagnosed posttraumatic stress disorder in women veterans with and without military sexual trauma. J Gen Internal Med. (2006) 21:S65–9. doi: 10.1111/j.1525-1497.2006.00377.x
68. O’Brien BS, Sher L. 15 Military sexual trauma as a determinant in the development of mental and physical illness in male and female veterans. Adolesc Psychiatry. (2013) p:185.
69. Xue C, et al. A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. PloS One. (2015) 10:e0120270. doi: 10.1371/journal.pone.0120270
70. Mayo JA, et al. Role of occupation on new-onset post-traumatic stress disorder and depression among deployed military personnel. Military Med. (2013) 178:945–50. doi: 10.7205/MILMED-D-12-00527
71. Bleier J, et al. Risk of adverse health outcomes associated with frequency and duration of deployment with the Australian Defence Force. Military Med. (2011) 176:139–46. doi: 10.7205/MILMED-D-10-00241
72. Yu J, et al. Substance use, military experience, and posttraumatic stress disorder among veterans in community-based residential treatment. Military Behav Health. (2019) 7:279–85. doi: 10.1080/21635781.2018.1530623
73. Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. (2001) 158:1184–90. doi: 10.1176/appi.ajp.158.8.1184
74. Cameron KL, Sturdivant RX, Baker SP. Trends in the incidence of physician-diagnosed posttraumatic stress disorder among active-duty US military personnel between 1999 and 2008. Military Med Res. (2019) 6:1–13. doi: 10.1186/s40779-019-0198-5
75. Iversen AC, Fear NT, Ehlers A, Hacker Hughes J, Hull L, Earnshaw M, et al. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. psychol Med. (2008) 38:511–22. doi: 10.1017/S0033291708002778
76. Pietrzak RH, et al. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depression Anxiety. (2009) 26:745–51. doi: 10.1002/da.v26:8
77. Liu C, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS, et al. Association between social support and post-traumatic stress disorder symptoms among Chinese patients with ovarian cancer: A multiple mediation model. PloS One. (2017) 12:e0177055. doi: 10.1371/journal.pone.0177055
78. Wu G, et al. Understanding resilience. Front Behav Neurosci. (2013) 7:10. doi: 10.3389/fnbeh.2013.00010
Keywords: depression, Ethiopia, military personnel, PTSD, prevalence
Citation: Tedla A, Asnakew S, Legas G, Munie BM, Tareke M and Beka M (2024) Post-traumatic stress disorder among military personnel admitted at the Northwest Command Level Three Military Hospital, Bahir Dar, Ethiopia, 2022: an institution-based cross-sectional study. Front. Psychiatry 15:1410630. doi: 10.3389/fpsyt.2024.1410630
Received: 01 April 2024; Accepted: 05 August 2024;
Published: 18 September 2024.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Xiaoying Feng, American Institutes for Research, United StatesAtefeh Zandifar, Alborz University of Medical Sciences, Iran
Helen Niemeyer, Free University of Berlin, Germany
Zelalem Birhan, Wollo University, Ethiopia
Copyright © 2024 Tedla, Asnakew, Legas, Munie, Tareke and Beka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Assasahegn Tedla, QXNzYXNhaGVnbnRlZGxhMjFAZ21haWwuY29t
 Assasahegn Tedla
Assasahegn Tedla Sintayehu Asnakew
Sintayehu Asnakew Getasew Legas
Getasew Legas Birhanu Mengist Munie
Birhanu Mengist Munie Minale Tareke
Minale Tareke Micheal Beka
Micheal Beka