
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 28 May 2024
Sec. Sleep Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1407741
 Haoxiong Sun1*
Haoxiong Sun1* Sijia Li2
Sijia Li2Introduction: Sleeping disorders is a high prevalent disorder, and although previous research has suggested a link between smoking and sleep disorders, there is a lack of large-scale, nationally representative studies examining this association across multiple sleep outcomes and exploring dose-response relationships.
Methods: This study used data from 30,269 participants from the NHANES database (2007–2020). Weighted logistic regression models were used to assess the associations between smoking status (non-smoker, light smoker, moderate smoker, and heavy smoker) and various sleep outcomes, including insufficient sleep duration, reported sleep problems, snoring, snorting, or stopping breathing during sleep, and daytime sleepiness. Dose-response relationships were explored using restricted cubic splines.
Results: Compared to non-smokers, heavy smokers had significantly higher odds of experiencing insufficient sleep duration with OR 1.732 (95% CI 1.528–1.963, P <0.001), reported sleep problems with OR 1.990 (95% CI 1.766–2.243, P <0.001), occasional or frequent snoring with OR 1.908 (95% CI 1.164–3.128, P = 0.03), and occasional or frequent snorting or stopping breathing during sleep with OR 1.863 (95% CI 1.183–2.936, P = 0.022), while results for sometimes, often or almost always being overly sleepy during the day with OR 1.257 (95% CI 0.872–1.810, P = 0.115) are not significant. A trend of positive correlation was observed between smoking and all sleep disorder outcomes (P for trend < 0.05). Dose-response analyses revealed that the odds of these sleep outcomes increased with higher smoking levels.
Conclusion: Smoking is significantly associated with various sleep disorders, and a dose-response relationship exists between smoking levels and the odds of experiencing these sleep problems. These findings underscore the importance of addressing smoking as a modifiable risk factor for poor sleep health and suggest that reducing smoking, even if complete cessation is not achieved, may have positive effects on sleep outcomes.
Sleep is an important physiological process that plays a crucial role in maintaining physical and mental well-being (1, 2). Poor sleep quality has been associated with various adverse health outcomes, including cardiovascular diseases (3), metabolic disorders such as diabetes (4), and cognitive impairments (5). Sleep disorders are prevalent in the general population, with an estimated 83.6 million adults in the United States experiencing some form of sleep or wakefulness disorder (6). In recent years, there has been growing interest in identifying modifiable risk factors for poor sleep quality (7).
Smoking is a global health issue associated with numerous chronic diseases and premature deaths (8). Although the diverse harmful effects of smoking on respiratory and cardiovascular health are well recognized (9), the relationship between smoking and sleep quality remains understudied. Although some studies have identified pathological and epidemiological links between smoking and sleep disorders, like previous research has suggested that smoking may disrupt sleep architecture and lead to sleep disturbances (10–12), there is a lack of large-scale, nationally representative studies examining this association across multiple sleep outcomes and exploring dose-response relationships. Understanding the relationship between smoking and sleep quality is crucial for developing targeted interventions and public health strategies to improve sleep health and overall well-being.
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative survey conducted in the United States that collects comprehensive data on various health-related factors, including smoking habits and sleep parameters (13). By leveraging NHANES data from 2007–2020 March, we can explore potential associations between smoking and multiple sleep outcomes (14). In this study, we aim to investigate the association between smoking and poor sleep quality or sleeping disorders by using data from multiple NHANES survey cycles. We will also explore dose-response relationships between smoking and sleep outcomes while adjusting for important covariates. We hypothesize that smokers have a higher prevalence of poor sleep quality and various sleep disorders compared to non-smokers.
This cross-sectional study used data from the National Health and Nutrition Examination Survey (NHANES), a nationally representative survey conducted by the Centers for Disease Control and Prevention (CDC) in the United States. NHANES employs a complex, multistage probability sampling design to assess the health and nutritional status of the civilian, non-institutionalized U.S. population (15).
Data from six consecutive NHANES cycles (2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017- 2020 March) were combined for this study, yielding a total sample size of 66,148 participants. Among these, 30,269 subjects had complete data on smoking status (including non-smokers) and were included in the analysis. Subjects who did not provide information on their smoking status (n = 35,879) were excluded.
The study population varied depending on the sleep outcome of interest. For the analysis of sleep duration, 22,745 subjects with valid sleep duration data were included. The analysis of sleep problems included 22,796 subjects with available data. For the analyses of snoring, snorting or stop breathing during sleep, and overly sleepy, 10,905, 10,487, and 10,099 subjects were included, respectively, based on the availability of relevant data (Figure 1). Basic characteristics of included and excluded participants, including age, BMI, gender and race distribution were compared (Supplementary Table S1).
All participants provided written informed consent, and the NHANES study protocol was approved by the National Center for Health Statistics Research Ethics Review Board (15).
Smoking status was determined using the NHANES questionnaire item “SMQ020 - Smoked at least 100 cigarettes in life”. Participants who reported having smoked less than 100 cigarettes in their lifetime were classified as “non-smokers”. Among those who had smoked at least 100 cigarettes, we define the previous smoker by determining subjects whose answer for item “SMQ040 - Do you now smoke cigarettes?” is “3, Not at all”. For participants currently smoking, the intensity of smoking was assessed using the questionnaire item “SMD650 - Avg # cigarettes/day during past 30 days”.
Based on the responses to SMD650, smokers were further categorized into three groups: light smokers, who reported smoking more than 0 but fewer than 5 cigarettes per day, moderate smokers, who reported smoking more than 5 but fewer than 10 cigarettes per day and heavy smokers, who reported smoking 10 or more cigarettes per day.
For the dose-response analysis, the continuous variable derived from “SMD650 - Avg # cigarettes/day during past 30 days” was used to represent the average number of cigarettes smoked per day. This approach allowed for a more granular examination of the relationship between smoking quantity and sleep outcomes.
This study examined several sleep-related outcomes, including sleep duration sufficiency, diagnosed sleep problems, the frequency of snoring or snorting and stop breathing during sleep, and feeling overly sleepy during the day.
Sleep duration was assessed using two different questionnaire items across the NHANES cycles. In the 2007–2014 cycles, sleep duration was measured using the item “SLD010H - How much sleep do you get (hours)?”. For the 2015–2020 cycles, sleep duration was assessed using the item “SLD012 - Sleep hours”. Based on previous research, sleep duration was dichotomized into sufficient (>7 hours per night) and insufficient (≤7 hours per night) sleep (6, 14). Diagnosed sleep problems were determined using the questionnaire item “SLQ050 - Ever told doctor had trouble sleeping?”. Participants who reported being told by a doctor that they had trouble sleeping were considered to have a diagnosed sleep problem.
Snoring frequency was assessed using the questionnaire item “SLQ030 - How often do you snore?”. Responses were categorized as ‘never’, ‘rarely’ (1–2 nights per week), ‘occasionally’ (3–4 nights per week), and ‘frequently’ (5 or more nights per week).
The frequency of snorting or stop breathing during sleep was measured using the questionnaire item “SLQ040 - How often do you snort or stop breathing?”. Responses were categorized as ‘never’, ‘rarely’ (1–2 nights per week), ‘occasionally’ (3–4 nights per week), and ‘frequently’ (5 or more nights per week).
The frequency of feeling overly sleepy during the day was defined by “SLQ120 - How often feel overly sleepy during day?”, and Responses were categorized as ‘never’, ‘rarely’ (1 time a month), ‘sometimes’ (2–4 times a month), ‘frequently’ (5–15 times a month), and ‘almost always’ (more than 15 times a month).
In the dose-response analysis, we treated the ordinal categorical variables (snoring, snorting or stop breathing, and feeling overly sleepy) as binary variables. We defined ‘never’ and ‘rarely’ as 0, and ‘occasionally’ or more frequent categories as 1. The purpose of this approach was to investigate the relationship between smoking and the presence of occasional or more severe sleep problems, which we believe has more practical significance.
Covariables were chosen based on previous research (13, 14). Demographic characteristics were extracted from the demographic questionnaire, including age, gender, race/ethnicity, marital status, family poverty income ratio, and education level. These variables were categorized as follows: Race/ethnicity: Non-Hispanic White, Non-Hispanic Black, Mexican American, Other Hispanic, and Other Race - Including Multi-Racial. Marital status: Married/living with partner, Widowed/divorced/separated, and Never married. Family poverty income ratio: Low income (<1), Middle income (1–3), and High income (≥3). Education level: Below high school, High school/GED, and College or above. Body mass index (BMI) was extracted from “BMXBMI - Body Mass Index (kg/m**2)”. BMI was treated as a continuous variable in the analysis. The exercise load is determined based on whether people have done 75–150 minutes of high-intensity exercise or 150–300 minutes of moderate-intensity exercise per week based on the physical activity guidelines for American (16). Subjects were categorized into lack of exercise (below the standard), adequate exercise (meeting the standard), or highly active exercise (exceeding the standard). Dietary energy intake was also considered. The recommended energy intake for males is 2000–3000 kcal per day, while for females, it is 1600–2400 kcal per day (17). Based on these recommendations, subjects were divided into three categories: low energy intake, adequate energy intake, or excessive energy intake. Medication status, including the presence of asthma, diabetes, heart failure, emphysema, and chronic bronchitis, was also considered as a covariate.
According to the NHANES protocol, all the data were integrated into a single dataset, and data analysis took into account the masked variance and applied the suggested weighting methodology. Sample weights from the Mobile Examination Center (MEC) interviews were used to address non-response, non-coverage, and unequal probabilities of selection (18).
Participants were divided into two groups based on sleep sufficiency or reported sleep problems, or divided into groups based on the frequency of snoring, snorting, or stopping breathing during sleep, or being overly sleepy during the day. To explore the differences between these groups, weighted descriptive analyses were performed. For continuous variables such as age and BMI, weighted percentages were computed. For categorical variables such as gender, race, education level, and smoking status, weighted percentages were computed, and the weighted chi-square test was used to assess group differences. Data are expressed as mean ± SE. Odds ratios (ORs) and 95% confidence intervals (CIs) for the association between sleep disorders and smoking status were calculated using weighted logistic regression models. Both unadjusted and multivariate adjusted models were used in this research: the crude model was adjusted for no covariates; Model 1 was adjusted for age, sex, and race/ethnicity; Model 2 was further adjusted for body mass index, education level, marital status, poverty level, exercise level, dietary energy intake level, and medication status.
To determine the association of smoking with sleep disorders, we performed the Cochran-Armitage trend test and used logistic regression models to test whether sleep disorder outcomes exhibited a positive trend across smoking levels, while adjusting for potential confounders.
The non-linear relationship between the amount of smoking and binary sleep outcomes was evaluated using restricted cubic splines. A dose-response curve was plotted to visualize the relationship, with the odds ratios and 95% CIs predicted for different smoking amounts using the Predict function.
All statistical analyses were performed using R software version 4.3.2 (http://www.R-project.org, The R Foundation). A p-value of < 0.05 was statistically significant.
Table 1 presents the weighted baseline characteristics of all participants, participants who have insufficient sleep duration, and participants who have sufficient sleep duration. Among the analyzed sample subjects, age, BMI, gender, race, education level, poverty level, marital status, exercise load, dietary energy intake, asthma, diabetes, emphysema, chronic bronchitis, and smoking status were associated with significant differences in sleep sufficiency.
Table 2 presents the weighted baseline characteristics of all participants, participants who reported sleep problems, and participants who never reported sleep problems. Among the analyzed sample subjects, age, BMI, gender, race, education level, poverty level, marital status, exercise load, dietary energy intake, asthma, diabetes, heart failure, emphysema, chronic bronchitis, and smoking status were significantly associated with whether participants reported sleep problems.
Table 3 presents the weighted baseline characteristics of participants who never snore, rarely snore, occasionally snore, and frequently snore. Among the analyzed sample subjects, age, BMI, gender, race, education level, poverty level, marital status, asthma, diabetes, heart failure, chronic bronchitis and smoking status were significantly associated with the distribution of snoring frequency.
Table 4 presents the weighted baseline characteristics of participants who never, rarely, occasionally, and frequently experience snorting or stopping breathing during sleep. Among the analyzed sample subjects, age, BMI, gender, education level, poverty level, marital status, asthma, diabetes, heart failure, emphysema, chronic bronchitis, and smoking status were significantly associated with the distribution of snorting or stopping breathing frequency.
Table 5 presents the weighted baseline characteristics of participants who never, rarely, sometimes, often, and almost always feel overly sleepy during the day. Among the analyzed sample subjects, age, BMI, gender, race, education level, poverty level, dietary energy intake, asthma, diabetes, heart failure, emphysema, chronic bronchitis and smoking status were significantly associated with the distribution of feeling overly sleepy frequency.
Table 6 presents the weighted associations between smoking status and various sleep disorders outcomes, including insufficient sleep duration, reported sleep problems, snoring, snorting or stopping breathing during sleep, and feeling overly sleepy, after adjusting for confounders. Crude models and models adjusted for age, gender, and race are provided in the Supplementary Data (Supplementary Tables S2–6).
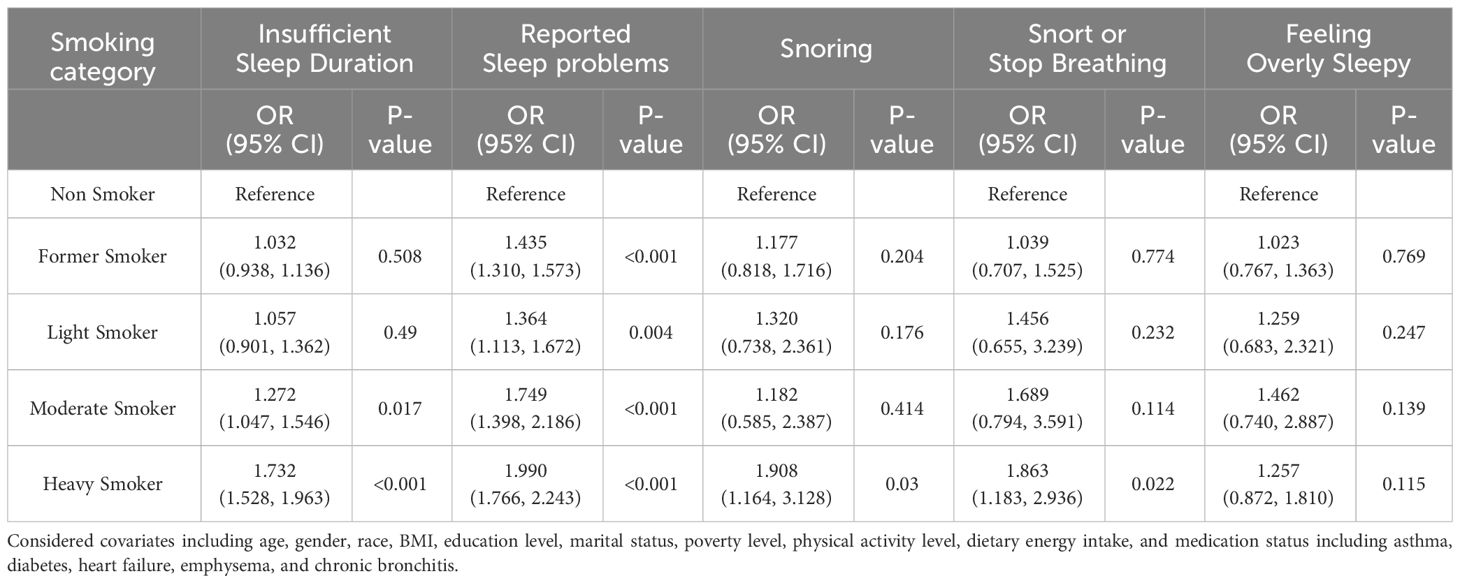
Table 6 Adjusted associations between smoking levels and insufficient sleep duration, reported sleep problems, snoring, snorting or stop breathing, and feeling overly sleepy during the day.
Compared to non-smokers, former smokers had significantly higher odds of reporting sleep problems (OR: 1.435, 95% CI: 1.310–1.573, P<0.001). Light smokers exhibited significantly higher odds of reporting sleep problems (OR: 1.364, 95% CI: 1.113–1.672, P=0.004) compared to non-smokers. Moderate smokers had significantly higher odds of insufficient sleep duration (OR: 1.272, 95% CI: 1.047–1.546, P=0.017) and reported sleep problems (OR: 1.749, 95% CI: 1.398–2.186, P<0.001) compared to non-smokers. Heavy smokers consistently demonstrated significant associations across multiple sleep outcomes. They had higher odds of insufficient sleep duration (OR: 1.732, 95% CI: 1.528–1.963, P<0.001), reported sleep problems (OR: 1.990, 95% CI: 1.766–2.243, P<0.001), snoring (OR: 1.908, 95% CI: 1.164–3.128, P=0.03), and snorting or stopping breathing during sleep (OR: 1.863, 95% CI: 1.183–2.936, P=0.022) compared to non-smokers. However, no significant association was found for feeling overly sleepy.
Table 7 presents the associations between smoking trend and various sleep-related outcomes. Compared to non-smokers, smokers had a higher odds of reporting insufficient sleep duration (OR: 1.112, 95% CI: 1.088–1.136, P<0.001). Similarly, smokers were more likely to report sleep problems (OR: 1.187, 95% CI: 1.159–1.215, P<0.001) and snoring (OR: 1.154, 95% CI: 1.114–1.195, P<0.001) than non-smokers. The odds of experiencing snorting or stopping breathing during sleep were also higher among smokers (OR: 1.172, 95% CI: 1.116–1.231, P<0.001). Additionally, smokers had a higher likelihood of feeling overly sleepy during the day compared to non-smokers (OR: 1.079, 95% CI: 1.043–1.116, P<0.001).
Figure 2 presents dose-response curves showing an increase in the adjusted odds ratios for various sleep outcomes, including insufficient sleep, reported sleep problems, snoring, snorting or stopping breathing, and feeling overly sleepy during the day, as the amount of smoking rises. The dose-response curves reveal that when the daily smoking amount is less than approximate 30 cigarettes, the risk of these sleep problems increases with the rise in smoking quantity, suggesting a dose-dependent adverse effect of smoking on sleep. However, when the daily smoking amount exceeds approximate 30 cigarettes, the curves exhibit a flattening or declining trend, accompanied by widening confidence intervals. This might be attributed to the relatively smaller sample size within the high smoking quantity range, leading to increased uncertainty in the estimates. The expanding confidence intervals suggest greater variability in the odds ratio estimates at higher smoking levels, but the overall patterns remain consistent.

Figure 2 Dose-response relationship between smoking amount and (A) sleep insufficiency, (B) reported sleep problems, (C) snoring at a high frequency, (D) snorting or stopping breathing at a high frequency, and (E) feeling overly sleepy during the day at a high frequency. The results were obtained using restricted cubic splines. The red lines indicate the estimated odds ratios, and the blue regions indicate the 95% confidence intervals.
Several previous research have investigated the relationship between sleep disorder and smoking, and smoking have been shown to lead to several sleep disorder outcomes, including insomnia, sleep disturbances and poor sleep quality (11, 12, 19–21). This large, nationally representative cross-sectional study found significant associations between smoking and a variety of sleep outcomes, including insufficient sleep duration, sleep problems, snoring, snorting or stopping breathing during sleep, and feeling overly sleepy during the day. Dose-response analyses revealed that a higher frequency of smoking was associated with a greater probability of poor sleep outcomes, which is consistent with previous findings. However, compared to previous research, our study provides more conclusive evidence due to the large sample size. We also considered more sleep outcomes, which provides a more complete picture of the impact of smoking on sleep health. We also conducted dose-response analyses to quantify the relationship between smoking amount and the probability of poor sleep outcomes. These findings underscore the importance of addressing smoking as a modifiable risk factor for sleep disorders, which can have significant implications for public health.
Several potential mechanisms may underlie the link between smoking and sleep disturbances. Nicotine, the main stimulant in cigarettes, can increase arousal, leading to withdrawal symptoms during the nighttime (22, 23). Previous research has found that smoking has various negative impacts on the central nervous system, exacerbating neurodegenerative diseases, insomnia, and cerebrovascular diseases (24). Smoking also affects circadian rhythms, especially since smokers typically have lower melatonin levels, this effect may further disrupt their sleep-wake cycle (25). Nicotine also interferes with acetylcholine pathway, which further disrupt the sleep-wake cycles (26). Smoking also activates inflammatory pathways in the body, leading to a chronic state of systemic inflammation associated with sleep disorders (27, 28). Furthermore, smoking has been associated with various mental health problems such as anxiety and depression, which are two major risk factors for sleep disorders (29). Chronic diseases caused by smoking, such as chronic obstructive pulmonary disease (COPD) and cardiovascular disease, may also affect sleep quality through multiple mechanisms (30, 31). Lastly, the act of smoking itself may affect sleep hygiene and sleep habits, as many smokers smoke before bedtime or upon awakening during the night, which can delay sleep onset or disrupt sleep (32).
The dose-response relationship indicates that while complete cessation of smoking is the ideal goal, reducing the amount of smoking can still positively affect sleep quality and reduce the risk of sleep disorders for those who are unable to quit entirely. Previous studies have suggested that cessation rather than reduction of smoking can improve health outcomes such as cardiovascular status (33, 34). However, our research suggests that, at least for sleep disorders, reducing the amount of smoking may also improve the consequences, providing a rationale for developing more flexible and realistic public health strategies. These findings can inform the development of targeted interventions and smoking cessation programs that emphasize the benefits of reducing smoking, even if complete abstinence is not achievable. Such strategies may include gradual reduction approaches and nicotine replacement therapies to help smokers improve their sleep quality while working towards the ultimate goal of quitting (35, 36).
Our study has several strengths, including the use of a nationally representative sample, examination of multiple sleep outcomes, and exploration of dose-response relationships. Our findings have important implications for public health and clinical practice, and addressing smoking could be a key strategy for improving sleep health in populations. However, this research also has some limitations. One of the limitations of this study is its cross-sectional design, which precludes the establishment of causal relationships between smoking and sleep outcomes. Additionally, the use of self-reported smoking status may introduce potential biases, such as recall bias or social desirability bias, leading to underreporting or overreporting of smoking, which could affect the accuracy of the results (37, 38). Finally, although we adjusted for several important confounders, the possibility of residual confounding by unmeasured factors cannot be entirely ruled out. Another limitation is that the sample volume of subjects who have a high daily cigarette consumption is low, leading to an unexplored relationship between smoking and sleep outcomes in the dose-response curves when the smoking level is high. In the future, research could focus on subjects with high smoking levels to explore the underlying relationship further.
In conclusion, this study found significant associations and a dose-response relationship between smoking and various sleep problems. These findings underscore the importance of addressing smoking to improve sleep health and reduce the risk of related health problems. As part of sleep disorder management, healthcare providers should routinely assess smoking status and provide support for quitting or reducing smoking. Public health campaigns should also include information about the negative impact of smoking on sleep and the potential benefits of smoking reduction.
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
The studies involving humans were approved by National Center for Health Statistics (NCHS) Ethics Review Board (ERB). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
HS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SL: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1407741/full#supplementary-material
1. Worley SL. The extraordinary importance of sleep: the detrimental effects of inadequate sleep on health and public safety drive an explosion of sleep research. P T. (2018) 43:758–63.
2. Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. (2023) 77:59–69. doi: 10.1016/j.pcad.2023.02.005
3. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. (2011) 32:1484–92. doi: 10.1093/eurheartj/ehr007
4. Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann New York Acad Sci. (2008) 1129:287–304. doi: 10.1196/annals.1417.033
5. Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. (2014) 13:1017–28. doi: 10.1016/S1474–4422(14)70172–3
6. Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). (2018) 7. doi: 10.3390/healthcare7010001
7. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/j.sleep.2016.08.006
8. West R. Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol Health. (2017) 32:1018–36. doi: 10.1080/08870446.2017.1325890
9. Parmar MP, Kaur M, Bhavanam S, Mulaka GSR, Ishfaq L, Vempati R, et al. A systematic review of the effects of smoking on the cardiovascular system and general health. Cureus. (2023) 15:e38073. doi: 10.7759/cureus.38073
10. Zhang L, Samet J, Caffo B, Punjabi NM. Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol. (2006) 164:529–37. doi: 10.1093/aje/kwj231
11. McNamara JP, Wang J, Holiday DB, Warren JY, Paradoa M, Balkhi AM, et al. Sleep disturbances associated with cigarette smoking. Psychol Health Med. (2014) 19:410–9. doi: 10.1080/13548506.2013.832782
12. Dugas EN, Sylvestre MP, O'Loughlin EK, Brunet J, Kakinami L, Constantin E, et al. Nicotine dependence and sleep quality in young adults. Addict Behav. (2017) 65:154–60. doi: 10.1016/j.addbeh.2016.10.020
13. Wu Z, Yue Q, Zhao Z, Wen J, Tang L, Zhong Z, et al. A cross-sectional study of smoking and depression among US adults: NHANES, (2005–2018). Front Public Health. (2023) 11:1081706. doi: 10.3389/fpubh.2023.1081706
14. You Y, Wei M, Chen Y, Fu Y, Ablitip A, Liu J, et al. The association between recreational physical activity and depression in the short sleep population: a cross-sectional study. Front Neurosci. (2023) 17:1016619. doi: 10.3389/fnins.2023.1016619
15. CDC. National Health and Nutrition Examination Survey (2024). Available at: https://www.cdc.gov/nchs/nhanes/index.htm.
16. Services, U. S. D. o. H. a. H. Physical Activity Guidelines for Americans. 2nd edition. Washington, DC: U.S. Department of Health and Human Services (2018). Available at: https://health.gov/paguidelines/second-edition/.
17. Agriculture, U. S. D. o. H. a. H. S. a. U. S. D. o. 2015–2020 Dietary Guidelines for Americans. Washington, D.C: U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015). Available at: https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines/previous-dietary-guidelines/2015.
18. You Y, Chen Y, Wang X, Wei M, Zhang Q, Cao Q. Accelerometer-measured physical activity patterns are associated with phenotypic age: Isotemporal substitution effects. Heliyon. (2023) 9:e19158. doi: 10.1016/j.heliyon.2023.e19158
19. Cohrs S, Rodenbeck A, Riemann D, Szagun B, Jaehne A, Brinkmeyer J, et al. Impaired sleep quality and sleep duration in smokers-results from the German Multicenter Study on Nicotine Dependence. Addict Biol. (2014) 19:486–96. doi: 10.1111/j.1369-1600.2012.00487.x
20. Liao Y, Xie L, Chen X, Kelly BC, Qi C, Pan C, et al. Sleep quality in cigarette smokers and nonsmokers: findings from the general population in central China. BMC Public Health. (2019) 19:808. doi: 10.1186/s12889–019-6929–4
21. Jang YS, Nerobkova N, Hurh K, Park E-C, Shin J. Association between smoking and obstructive sleep apnea based on the STOP-Bang index. Sci Rep. (2023) 13:9085. doi: 10.1038/s41598–023-34956–5
22. Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine Tob Res. (2007) 9:315–27. doi: 10.1080/14622200701188919
23. Jaehne A, Unbehaun T, Feige B, Cohrs S, Rodenbeck A, Schutz AL, et al. Sleep changes in smokers before, during and 3 months after nicotine withdrawal. Addict Biol. (2015) 20:747–55. doi: 10.1111/adb.12151
24. Hajdusianek W, Zorawik A, Waliszewska-Prosol M, Poreba R, Gac P. Tobacco and nervous system development and function-new findings 2015–2020. Brain Sci. (2021) 11. doi: 10.3390/brainsci11060797
25. Ursing C, von Bahr C, Brismar K, Rojdmark S. Influence of cigarette smoking on melatonin levels in man. Eur J Clin Pharmacol. (2005) 61:197–201. doi: 10.1007/s00228–005-0908–7
26. Salin-Pascual RJ, Moro-Lopez ML, Gonzalez-Sanchez H, Blanco-Centurion C. Changes in sleep after acute and repeated administration of nicotine in the rat. Psychopharmacol (Berl). (1999) 145:133–8. doi: 10.1007/s002130051041
27. Lee J, Taneja V, Vassallo R. Cigarette smoking and inflammation: cellular and molecular mechanisms. J Dent Res. (2012) 91:142–9. doi: 10.1177/0022034511421200
28. Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE. Sleep inconsistency and markers of inflammation. Front Neurol. (2020) 11:1042. doi: 10.3389/fneur.2020.01042
29. Fluharty M, Taylor AE, Grabski M, Munafo MR. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine Tob Res. (2017) 19:3–13. doi: 10.1093/ntr/ntw140
30. Badran M, Yassin BA, Fox N, Laher I, Ayas N. Epidemiology of sleep disturbances and cardiovascular consequences. Can J Cardiol. (2015) 31:873–9. doi: 10.1016/j.cjca.2015.03.011
31. Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med. (2015) 11:259–70. doi: 10.5664/jcsm.4540
32. Peters EN, Fucito LM, Novosad C, Toll BA, O'Malley SS. Effect of night smoking, sleep disturbance, and their co-occurrence on smoking outcomes. Psychol Addict Behav. (2011) 25:312–9. doi: 10.1037/a0023128
33. Godtfredsen NS, Holst C, Prescott E, Vestbo J, Osler M. Smoking reduction, smoking cessation, and mortality: a 16-year follow-up of 19,732 men and women from The Copenhagen Centre for Prospective Population Studies. Am J Epidemiol. (2002) 156:994–1001. doi: 10.1093/aje/kwf150
34. Jeong SM, Jeon KH, Shin DW, Han K, Kim D, Park SH, et al. Smoking cessation, but not reduction, reduces cardiovascular disease incidence. Eur Heart J. (2021) 42:4141–53. doi: 10.1093/eurheartj/ehab578
35. Cheung YT, Lam TH, Leung DY, Abdullah AS, Chan SS. Nicotine replacement therapy to aid gradual cessation in smokers with no intention to quit: Association between reduction quantity and later abstinence. Prev Med Rep. (2015) 2:196–201. doi: 10.1016/j.pmedr.2015.02.014
36. Klemperer EM, Hughes JR, Naud S. Reduction in cigarettes per day prospectively predicts making a quit attempt: A fine-grained secondary analysis of a natural history study. Nicotine Tob Res. (2019) 21:648–54. doi: 10.1093/ntr/nty056
37. Raphael K. Recall bias: a proposal for assessment and control. Int J Epidemiol. (1987) 16:167–70. doi: 10.1093/ije/16.2.167
Keywords: sleep disorder, smoking, nicotine, snoring, sleep insufficiency
Citation: Sun H and Li S (2024) Exploring the relationship between smoking and poor sleep quality: a cross-sectional study using NHANES. Front. Psychiatry 15:1407741. doi: 10.3389/fpsyt.2024.1407741
Received: 28 March 2024; Accepted: 09 May 2024;
Published: 28 May 2024.
Edited by:
Ingo Fietze, Charité University Medicine Berlin, GermanyReviewed by:
Marta Waliszewska-Prosół, Wroclaw Medical University, PolandCopyright © 2024 Sun and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haoxiong Sun, c3VuaGFveGlvbmczMTBAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.