
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 04 June 2024
Sec. Public Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1402122
This article is part of the Research Topic The Role of Stress in Pathologies View all 4 articles
 Hamid Sharif-Nia1,2
Hamid Sharif-Nia1,2 Erika Sivarajan Froelicher3
Erika Sivarajan Froelicher3 Esmail Hoseinzadeh4
Esmail Hoseinzadeh4 Omolhoda Kaveh5
Omolhoda Kaveh5 Reza Fatehi6
Reza Fatehi6 Poorya Nowrozi6*
Poorya Nowrozi6*Introduction: The 10-item Perceived Stress Scale (PSS-10) is commonly used to measure stress levels in postoperative patients, as research shows that high levels of stress can affect postoperative outcomes. By using the PSS-10, healthcare providers can understand patients’ psychological well-being before and after surgery, helping improve recovery and overall health. This study focuses on assessing the reliability and validity of the 10-item Persian version of the PSS (PSS-10-P) in postoperative patients.
Methods: In a methodological study conducted between October to December 2023, a sample of 400 patients who had undergone surgery in 17 Shahrivar Hospital, Amol, Iran were selected using a convenience sampling method. The PSS-10 scale utilized in the study was translated, and its psychometric properties were evaluated through assessments of construct validity, including exploratory (n = 200) and confirmatory (n = 200) factor analysis, convergent validity, and discriminant validity. Furthermore, the study examined the internal consistency of the scale to ensure its reliability.
Results: The mean age of the participants was 44.38 (SD= 13.49) years. The results of exploratory factor analysis with Promax rotation extracted two factors accounting for 83.82% of the variance comprising 10 items. After necessary modifications during CFA, the final model was approved. As for reliability, the Cronbach’s alpha, CR, and MaxR for all constructs were greater than 0.7, demonstrating good internal consistency and construct reliability.
Conclusion: According to these results, the Persian version of PSS-10 has a valid structure and acceptable reliability. This scale can be used by health professionals in many ways.
Surgery is one of the situations that can cause stress and anxiety in patients (1). Surgery is a deliberate change in the anatomical structures of the body for the purpose of creating comfort, alleviating or eliminating pathological processes, and repairing traumatic injuries (2). Surgery is a stressful experience for patients and their families due to the physical and psychological stress it causes. The fear of the unknown, loss of control, and potential risk of harm all contribute to this anxiety-inducing situation (3, 4). Several studies demonstrated that physical stress, psychological stress, stress due to hospitalization, self-care stress, and spiritual stress are the main sources of stress experienced by patients who are candidates for various surgery that result in enhancing the risk of complications, morbidity, and mortality (5–11). A situation is stressful when it is perceived by a person as threatening and uncontrollable and that person does not have the necessary resources to face the situation (12). Previous studies indicate that the statistics for anxiety and stress in patients undergoing surgery are significant (13–16); therefore, assessment and appropriate interventions are needed (17–20). The skills that an individual develops throughout their life, particularly cognitive and emotional skills that are acquired when individuals are facing stressful situations, play a crucial role in their ability to manage stress (21).
There are a variety of tools available for assessing stress levels. One commonly used scale is the Perceived Stress Scale (PSS), which measures an individual’s perceived level of stress. The original version of the PSS was developed by Cohen et al. in 1983 and consisted of 14 items (22). PSS10- item and PSS 4- item are shorter forms of the PSS scale. Psychometric properties of the above scale have been done in different countries among the numerous participants including Italian precarious workers (23), Czech general adult population (24), Chinese cardiac patients who smoke (25), patients with Multiple Sclerosis in the USA (26), German adults (27), Arabic Version among women Emeriti students (28), Brazilian pregnant women (29), Chinese adults during the COVID-19 Pandemic (30), Ecuadorian university students (31), Korean patients with chronic diseases (32), and in different languages such as the Swedish (33) and France versions (34).
The 10-item version has been used in most of the studies, and on the other hand, the results of numerous studies also showed that the psychometric properties of PSS-10 are higher than they are in the PSS-14 and PSS-4 (23–26, 35); for this reason, we chose to assess the validity and reliability of the 10-item version in our study. Only one study in Iran assessed the factorial validity of the 14-item version of this scale in cancer patients (36), but psychometric properties have not been thoroughly investigated and the reliability was not reported. Also, two studies conducted in Iran were among different samples (chronic headache and asthmatic patients) (37, 38). Therefore, the purpose of this study was to examine the psychometric properties of Persian versions of the PSS-10 (PSS-10-P) in postoperative patients.
This methodological cross-sectional study was carried out between October to December 2023. Patients from 17 Shahrivar Hospital, Amol, Iran, were recruited for this study.
The inclusion criteria for participants in the study were: being at least 18 years old, being able to communicate in Farsi and being literate, volunteering to participate, and being hospitalized in hospital wards after surgery. Exclusion criteria included cognitive disorders, presence of mental illness, reduced level of consciousness, heart diseases such as uncontrolled unstable angina and uncontrolled severe arrhythmia, limited activity due to severe physical diseases or cerebrovascular diseases, pregnancy, cancer and malignancies, other neurological diseases or rheumatoid arthritis, drug addiction, and drug dependencies, and not having a mental illness such as schizophrenia or anxiety disorder.
In their 1999 study, MacCallum and et al. recommended a minimum sample size of 200 cases for psychometric studies (39). To ensure the construct validity, it was necessary to invite 400 individuals to participate (two different samples for construct validity). The participants were approached in the hospital wards following their surgeries. After receiving a thorough explanation of the study’s objectives, they were invited to voluntarily participate and complete the 10-item Perceived Stress Scale (PSS-10) questionnaire.
The 10-item PSS developed by Cohen deals with perceived stress and includes two associated areas. The scale questions include positive and negative aspects of stress. Response options are scored on a 5-point Likert scale (0-4) with the following scores: 4: never, 3: rarely, 2: sometimes, 1: often, 0: always. It should be noted that items 4, 5, 7, and 8 were positively calculated. A total score of 13 represents a normal stress level, but scores of 20 or higher represent high stress levels that require therapeutic intervention (35).
The scale was translated from English to Persian by the established translation protocols (40). Two skilled translators proficient in both English and Persian independently translated the PSS-10 into Persian. An expert panel, consisting of the authors of this article (EF, and RF), and two professional translators, carefully reviewed and combined the two translations to produce a Persian version of the PSS-10. Following this, a Persian-English translator was hired to translate the PSS-10-P back into English. The panel of experts then reviewed and approved this PSS-10-P final version. Then the panel of experts compiled and compared the results of the back-translation with the original scale to detect any differences and similarities between the original scale and the back-translated version. All items are translated into Persian and back-translated into English without any required modifications.
Skewness ( ± 3) and kurtosis ( ± 7) were used to individually investigate the univariate distribution of data. Also, the multivariate normality distribution was assessed by the Mardia coefficient of multivariate kurtosis (<8). Mahalanobis d-squared (p < 0.001) was used to determine whether there were any multivariate outliers (41). The missing data were assessed using multiple imputations, and the average participant response was used to replace the missing data (42).
To assess the construct validity, the original dataset consisting of 400 cases was randomly split into two datasets, each containing 200 cases. The first dataset was subjected to Maximum Likelihood Exploratory Factor Analysis (MLEFA) with Promax rotation and Kaiser normalization, along with exploratory graph analysis methods to identify the underlying factor structure. The Kaiser-Meyer-Olkin (KMO) measure exceeding 0.8 and the significance of Bartlett’s test of sphericity (p < 0.01) were considered to confirm the suitability and relevance of the data for conducting factor analysis. Parallel analysis was utilized to determine the number of factors (43). The Eigenvalues of more than 1, communalities of more than 0.2, and factor loadings of more than 0.5 were also used for the factor extraction (44). Eigenvalues (λ) are calculated as the sum of squared factor loadings (SSL) across all items (k) for each factor. This value indicates the proportion of variance in each item that can be accounted for by the analysis. To determine the percentage of total variance explained by a factor, the Eigenvalue is divided by the total number of items (43). The MLEFA was performed using SPSS version 27.
In the next step, the factor structures obtained from MLEFA were analyzed and confirmed by conducting Confirmatory Factor Analysis (CFA) based on the second random dataset (n = 200) using AMOS version 27. The following model fit indices were used to assess the model fit: Comparative Fit Index (CFI), Normed Fit Index (NFI), Goodness of Fit Index (GFI), Relative Fit Index (RFI), and Incremental Fit Index (IFI) was > 0.9; that of Root Mean Square Error of Approximation (RMSEA) was < 0.08; and for Minimum Discrepancy Function divided by degrees of freedom (CMIN/DF) < 3 was considered good (45).
Also, convergent and discriminant validity were evaluated. For convergent validity, composite reliability (CR) should be greater than 0.7, and Average Variance Extracted (AVE) should be greater than 0.5 for each construct. Fornell and Larcker (46) stated that for psychological constructs, if AVE is less than 0.5, but CR is more than 0.7, the convergent validity can be considered acceptable.
For discriminant validity, this study used the heterotrait-monotrait ratio (HTMT) of the correlations criterion, where the HTMT ratio between all constructs should be less than 0.85 to achieve discriminant validity. Discriminant validity is a measure of how distinct a concept is from others in a framework. It is important for construct validity. The HTMT ratio is used to evaluate discriminant validity, calculated by comparing correlations between constructs. A value of 1 indicates perfect discriminant validity, while a value close to 1 suggests a problem. A high HTMT ratio indicates a lack of discriminant validity (47).
The Cronbach’s alpha, McDonald’s omega, average inter-item correlation coefficient (AIC), Composite Reliability (CR), and Maximal Reliability (MaxR) were calculated to estimate the internal consistency and construct reliability. If the α, Ω, CR, and MaxR were greater than 0.7 and AIC values of 0.2 to 0.4 were interpreted as acceptable internal consistency (48).
Descriptive statistics were employed to calculate the mean score of the PSS-10. Additionally, an independent samples t-test was conducted to evaluate differences between the groups of men and women for the scale.
The mean age of the participants was 44.38 (SD= 13.49) years. Among the 400 participants, 152 (46.1%) were women and 178 (53.9%) were men. The demographic characteristics of the participants are listed in Table 1.
The results of MLEFA with Promax with Kaiser Normalization rotation using the first random dataset (n = 200) extracted two factors accounting for 83.82% of the variance comprising 10 items. The none of items were removed from the original version. Moreover, the results of the KMO (0.919) and Bartlett’s test of sphericity (p < 0.001, Chi-square= 6734.747, df = 45) showed the sampling was adequate and appropriate for conducting the factor analysis. The detailed results of the MLEFA are shown in Table 2.
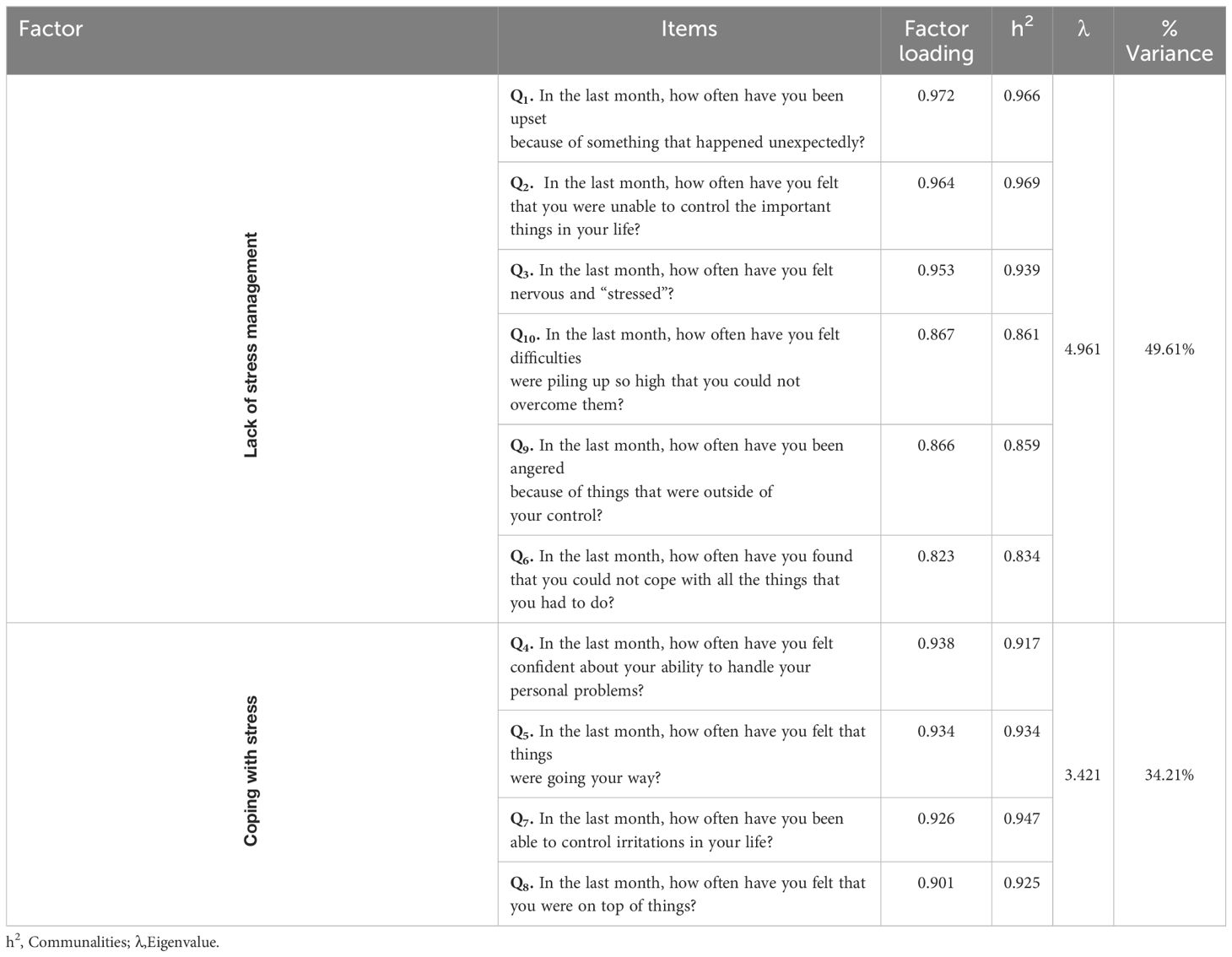
Table 2 The result of MLEFA on the two factors Persian version of the Perceived Stress Scale (n = 200).
The CFA was conducted to confirm and validate the factor structure obtained from MLEFA using the second random dataset (n = 200). The results showed that the data fit the model well as evidenced by (χ2(132) =218.505, p < 0.001, χ2/df = 1.655, CFI = 0.978, IFI = 0.978, TLI = 0.969, SRMR = 0.067, RMSEA (90% C.I.) = 0.040 [0.043, 0.059]). The Figure 1 shows the results of the CFA final model.
The results showed that AVE for factors “lack of stress management and coping with stress” were greater than 0.5, indicating good convergent validity. As for discriminant validity, the results of the HTMT ratio were lower than 0.85, demonstrating good discriminant validity for all constructs. So results showed that the correlation between factor one and two (0.785). Cronbach’s alpha, McDonald’s omega, CR, and MaxR for all factors were greater than 0.7, and AIC was more than 0.2, demonstrating good internal consistency and construct reliability (Table 3).
In the overall population, the mean score for PSS-10 was 20.14 (SD = 13.40, 95% CI: 18.69, 21.59) which 193 (48.25%) patients showed a high level of stress (perceived stress score greater than 20). Furthermore, there were no significant differences (p = 0.575) in PSS-10 scores between men (20.58, SD = 12.78) and women (19.69, SD = 14.12).
Perceived stress is commonly defined as the perception of stressful events encountered within a defined timeframe. Given the significant impact of stress on health (49), the primary objective of the current investigation was to assess the psychometric properties of the PSS-10 in Iranian surgical patients. The results of this research revealed that the PSS-10 exhibited acceptable factor structure, validity, and reliability.
The study found that the Persian version of the 10-item Perceived Stress Scale (PSS-10-P) had 10 items divided into two categories: lack of stress management and coping with stress. These two factors explained 83.82% of the variance in stress levels among Iranian surgical patients. In line with the objective of maximizing variance in factor analysis, reported variances of 56.23% (50) and in two other studies reported variances of 56.8% (49) and 61.9% (51).
The first factor of the PSS-10-P was designated as “Lack of stress management”. The term “stress management” is commonly utilized and appears to possess a well-defined definition (52). Inadequate stress management is when someone doesn’t have good strategies to deal with stress, which can harm their physical, mental, and emotional health. Symptoms can include headaches, fatigue, and more. If not managed, it can lead to distress and feeling overwhelmed. Effective stress management involves skills like problem-solving, time management, and relaxation techniques to navigate stress and maintain well-being (53). Interventions aimed at stress management encompass a range of techniques that offer opportunities for personal development (54). The focus on stress management is crucial to safeguard individuals’ physical and emotional well-being, as well as their capacity to function effectively in their daily lives. It is imperative to recognize stress and implement strategies to manage it effectively to mitigate the adverse repercussions it may engender (55). Lack of stress management means not having the right tools to deal with stress, which can have negative impacts on mental and physical health. It can lead to anxiety, depression, physical pain, and overall reduced quality of life. Without proper stress management, individuals may struggle with stressful situations and face long-term consequences on their health and functioning (56). Clinical studies have demonstrated that patients who exhibit a predefined adaptive stress response during surgery tend to experience superior recovery outcomes compared to those who do not (57). The items associated with the first factor underscore the importance for healthcare professionals to identify instances of inadequate stress management in patients. By imparting stress management techniques to patients, healthcare providers can help prevent the detrimental impacts of stress on surgical patients and can facilitate their swift recovery.
The second factor of (PSS-10-P) was denoted as “Coping with stress”. Coping, as defined, refers to the mental strategies and behavioral responses employed to manage stressful situations, whether they originate internally or externally. This term specifically pertains to purposeful, conscious decisions made with the aim of alleviating or enduring stress (58). Also Managing stress involves actively and intentionally addressing challenges that can trigger negative emotions. This includes utilizing strategies such as meditation, counseling, and engaging in hobbies to effectively manage and decrease stress levels. Coping with stress does not entail completely avoiding stress, but rather learning to handle it healthily to enhance overall well-being and resilience (56). The experience of preoperative stress induced by anesthesia and surgery prompts patients to employ coping mechanisms in an endeavor to regain a sense of emotional control. When coping is supported by specific techniques or external assistance, its efficacy may be enhanced (59). Consequently, nurses can play a pivotal role in alleviating the stress experienced by surgical patients by identifying their existing strengths in stress management and augmenting these capabilities through the application of stress coping strategies.
The CFA revealed that the data did not align well with the model, a finding consistent with previous studies (49, 60). Based on the analysis of construct validity and reliability, there is insufficient evidence to justify the utilization of two distinct sub-scales within the current population. The study’s outcomes also indicate that the items on this scale exhibit robust divergent and convergent validity. Divergent validity signifies complete segregation between constructs, while convergent validity is evident when elements of a construct are closely semantically related and account for variance (61).
Furthermore, the internal consistency coefficients of the scale dimensions demonstrate that the items within each factor exhibit substantial internal correlations, aiding in the clarification and measurement of a broader concept. Essentially, the components of each dimension effectively represent and assess a specific concept. Given the existing cross-cultural gap in health outcomes research (50), utilizing the PSS-10-P in the Persian culture with appropriate cultural variables can facilitate the identification of perceived stress among surgical patients and inform necessary interventions to mitigate it.
Validating the Persian Version PSS-10-P for postoperative patients is essential for nurses to accurately assess stress levels and customize care plans accordingly. This validation process enables nurses to deliver personalized interventions, address specific stressors, and enhance emotional resilience to facilitate smoother recoveries. By integrating the PSS-10-P into clinical practice, nurses can offer comprehensive care that acknowledges the influence of psychological factors on postoperative recuperation, ultimately fostering patient-centered care and enhancing outcomes for Persian-speaking populations.
Two limitations of the current study may introduce bias and subjectivity into the results. Therefore, there is a need for more robust clinical trials with longer-term follow-up to validate the findings and enhance their clinical significance.
It can provide valid data for understanding the prevalence of this problem and investigating the impact of different interventions to reduce it. It is recommended that in future studies, other psychometric properties such as the responsiveness, sensitivity, and reliability (stability) of this scale, be investigated in diverse populations of both patients and healthy individuals who speak Farsi.
The EFA results revealed the extraction of two factors, with ten items., which collectively account for 83.82% of the total variance in perceived stress among Iranian surgical patients. The findings affirm the appropriateness of employing the Persian iteration of the PSS-10-P as a dependable and valid instrument for assessing perceived stress in postoperative patients Healthcare professionals can effectively employ the PSS-10-P to educate patients on stress reduction strategies, thereby facilitating quicker post-surgical recovery and minimizing the likelihood of complications.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The Ethics Committee of Mazandaran University of Medical Sciences (Sari, Iran) gave its approval to this study (Ethics code: IR.MAZUMS.REC.1402.599). The participants were given a thorough explanation of the study’s goals and methods, as well as assurances that their participation was entirely voluntary. The researcher gave the scale to the patient to complete by themselves. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HS: Formal analysis, Supervision, Writing – original draft, Writing – review & editing. ES: Writing – review & editing. EH: Writing – original draft, Writing – review & editing. OK: Writing – original draft, Writing – review & editing. RF: Writing – original draft, Writing – review & editing. PN: Data curation, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors wish to extend their sincere gratitude to the participants who generously contributed to this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Iryanidar I, Irwan AM. Stress and coping mechanisms in patients undergoing CABG: An integrative review. Clin Epidemiol Global Health. (2023) 23:101388. doi: 10.1016/j.cegh.2023.101388
2. Cho YJ, Choi GJ, Ahn EJ, Kang H. Pharmacologic interventions for postoperative nausea and vomiting after thyroidectomy: A systematic review and network meta-analysis. PLoS One. (2021) 16:e0243865. doi: 10.1371/journal.pone.0243865
3. Zare Marzouni H, Karimi M, Narimi Z, Ghasemi A, Janaki M. Effects of education on reduction of stress and anxiety of orthopedic surgery. Navid No. (2016) 19:62–8. doi: 10.22038/NNJ.2016.8741
4. Akutay S, Ceyhan Ö. The relationship between fear of surgery and affecting factors in surgical patients. Perioperative Med. (2023) 12:22. doi: 10.1186/s13741-023-00316-0
5. Gelogahi ZK, Aghebati N, Mazloum SR, Mohajer S. Effectiveness of nurse's intentional presence as a holistic modality on depression, anxiety, and stress of cardiac surgery patients. Holistic Nurs practice. (2018) 32:296–306. doi: 10.1097/HNP.0000000000000294
6. Protogerou C, Fleeman N, Dwan K, Richardson M, Dundar Y, Hagger MS. Moderators of the effect of psychological interventions on depression and anxiety in cardiac surgery patients: A systematic review and meta-analysis. Behav Res Ther. (2015) 73:151–64. doi: 10.1016/j.brat.2015.08.004
7. AbuRuz ME, Al-Dweik G, Al-Akash HY. Checking the moderating effect of perceived control on the relationship between anxiety and postoperative hospital length of stay among coronary artery bypass graft patients. Int J Gen Med. (2019) 12:79–85. doi: 10.2147/IJGM
8. McCann WD, Hou XY, Stolic S, Ireland MJ. Predictors of psychological distress among post-operative cardiac patients: A narrative review. Healthcare (2023) 11(20):2721. doi: 10.3390/healthcare11202721
9. Weinerman J, Vazquez A, Schurhoff N, Shatz C, Goldenberg B, Constantinescu D, et al. The impacts of anxiety and depression on outcomes in orthopaedic trauma surgery: a narrative review. Ann Med Surg. (2023) 85:5523–7. doi: 10.1097/MS9.0000000000001307
10. Karabulut N, Gürçayır D, Abi Ö, Kızıloğlu Ağgül B, Söylemez N. Does surgery cause anxiety, stress and fear in geriatric patients? Psychogeriatrics. (2023) 23:808–14. doi: 10.1111/psyg.13000
11. Ni K, Zhu J, Ma Z. Preoperative anxiety and postoperative adverse events: a narrative overview. Anesthesiology Perioperative Science. (2023) 1:23. doi: 10.1007/s44254-023-00019-1
12. Nielsen NR, Kristensen TS, Schnohr P, Grønbæk M. Perceived stress and cause-specific mortality among men and women: results from a prospective cohort study. Am J Epidemiol. (2008) 168:481–91. doi: 10.1093/aje/kwn157
13. Tunç E, Keskin SG. Determining the levels of perceived stress and anxiety in patients undergoing coronary angiography in accordance with their status of being informed about the procedure. J Radiol Nursing. (2020) 39:331–5. doi: 10.1016/j.jradnu.2020.06.009
14. Harms J, Kunzmann B, Bredereke J, Harms L, Jungbluth T, Zimmermann T. Anxiety in patients with gastrointestinal cancer undergoing primary surgery. J Cancer Res Clin Oncol. (2023) 149:8191–200. doi: 10.1007/s00432-023-04759-2
15. Shawahna R, Jaber M, Maqboul I, Hijaz H, Tebi M, Ahmed NA-S, et al. Prevalence of preoperative anxiety among hospitalized patients in a developing country: a study of associated factors. Perioperative Med. (2023) 12:47. doi: 10.1186/s13741-023-00336-w
16. Mars DG, Coffey D, Miller RS, Taylor S, Rufini A. Perceived stress level of the postoperative coronary artery bypass graft patients in the intensive care unit. J Nurs Educ Pract. (2022) 12:14–21. doi: 10.5430/jnep.v12n7p14
17. Kassahun WT, Mehdorn M, Wagner TC, Babel J, Danker H, Gockel I. The effect of preoperative patient-reported anxiety on morbidity and mortality outcomes in patients undergoing major general surgery. Sci Rep. (2022) 12:6312. doi: 10.1038/s41598-022-10302-z
18. Moldes-Moro R, de Dios-Duarte MJ. Colorectal cancer surgery: influence of psychosocial factors. Cancers. (2023) 15:4140. doi: 10.3390/cancers15164140
19. Bahcelı P, Ulker G. The relationship between perceived stress and coping styles in women following breast cancer surgery: A cross-sectional descriptive study. Prog Health Sci. (2023) 13:43–50. doi: 10.5604/01.3001.0054.2475
20. Senthil G, Selvaganesh S, Nessapan T, Veeraragavan VP, Eswaramoorthy R. Comparison of pre and post-operative stresses among Indian patients undergoing intra-oral grafting procedures. Bioinformation. (2023) 19:484. doi: 10.6026/bioinformation
21. Jamali S, Sabokdast S, Sharif Nia H, Goudarzian AH, Beik S, Allen K-A. The effect of life skills training on mental health of Iranian middle school students: A preliminary study. Iranian J Psychiatry. (2016) 11:269.
22. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
23. Mondo M, Sechi C, Cabras C. Psychometric evaluation of three versions of the Italian Perceived Stress Scale. Curr Psychol. (2021) 40:1884–92. doi: 10.1007/s12144-019-0132-8
24. Figalová N, Charvát M. The perceived stress scale: Reliability and validity study in the Czech Republic. Československá psychologie. (2021) 65:46–59. doi: 10.51561/cspsych.65.1.46
25. Leung DY, Lam T-h, Chan SS. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. (2010) 10:1–7. doi: 10.1186/1471-2458-10-513
26. Wu SM, Amtmann D. Psychometric evaluation of the perceived stress scale in multiple sclerosis. Int Scholarly Res Notices. (2013) 2013:1–9. doi: 10.1155/2013/608356
27. Reis D, Lehr D, Heber E, Ebert DD. The German version of the Perceived Stress Scale (PSS-10): evaluation of dimensionality, validity, and measurement invariance with exploratory and confirmatory bifactor modeling. Assessment. (2019) 26:1246–59. doi: 10.1177/1073191117715731
28. Ali AM, Hendawy AO, Ahmad O, Al Sabbah H, Smail L, Kunugi H. The Arabic version of the Cohen perceived stress scale: factorial validity and measurement invariance. Brain Sci. (2021) 11:419. doi: 10.3390/brainsci11040419
29. Yokokura AVCP, Silva A, Fernandes J, Del-Ben CM, Figueiredo F, Barbieri MA, et al. Perceived Stress Scale: confirmatory factor analysis of the PSS14 and PSS10 versions in two samples of pregnant women from the BRISA cohort. Cadernos saude publica. (2017) 33:1–13. doi: 10.1590/0102-311x00184615
30. She Z, Li D, Zhang W, Zhou N, Xi J, Ju K. Three versions of the perceived stress scale: psychometric evaluation in a nationally representative sample of Chinese adults during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:8312. doi: 10.3390/ijerph18168312
31. Ruisoto P, López-Guerra VM, Paladines MB, Vaca SL, Cacho R. Psychometric properties of the three versions of the Perceived Stress Scale in Ecuador. Physiol Behavior. (2020) 224:113045. doi: 10.1016/j.physbeh.2020.113045
32. Lee EH, Chung BY, Suh CH, Jung JY. K orean versions of the P erceived S tress S cale (PSS-14, 10 and 4): psychometric evaluation in patients with chronic disease. Scandinavian J caring Sci. (2015) 29:183–92. doi: 10.1111/scs.12131
33. Nordin M, Nordin S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scandinavian J Psychol. (2013) 54:502–7. doi: 10.1111/sjop.12071
34. Lesage F-X, Berjot S, Deschamps F. Psychometric properties of the French versions of the Perceived Stress Scale. Int J Occup Med Environ Health. (2012) 25:178–84. doi: 10.2478/s13382-012-0024-8
35. Cohen S. Perceived stress in a probability sample of the United States. Thousand Oaks, California, USA: Sage (1988).
36. Safaei M, Shokri O. Assessing stress in cancer patients: Factorial validity of the perceived stress scale in Iran. Iran: Iranian Nursing Scientific Association (2014).
37. Khalili R, Ebadi A, Tavallai A, Habibi M. Validity and reliability of the Cohen 10-item Perceived Stress Scale in patients with chronic headache: Persian version. Asian J Psychiatry. (2017) 26:136–40. doi: 10.1016/j.ajp.2017.01.010
38. Maroufizadeh S, Zareiyan A, Sigari N. Psychometric properties of the 14, 10 and 4-item “Perceived Stress Scale” among asthmatic patients in Iran. Payesh (Health Monitor). (2014) 13:457–65.
39. MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. psychol Methods. (1999) 4:84–99. doi: 10.1037//1082-989X.4.1.84
40. Gudmundsson E. Guidelines for translating and adapting psychological instruments. Nordic Psychol. (2009) 61:29–45. doi: 10.1027/1901-2276.61.2.29
41. Sharif Nia H, Kaur H, Fomani FK, Rahmatpour P, Kaveh O, Pahlevan Sharif S, et al. Psychometric properties of the impact of events scale-revised (IES-R) among general Iranian population during the COVID-19 pandemic. Front Psychiatry. (2021) 12:692498. doi: 10.3389/fpsyt.2021.692498
42. Patrician PA. Multiple imputation for missing data. Res Nurs Health. (2002) 25:76–84. doi: 10.1002/nur.10015
43. Sharif-Nia H, She L, Osborne J, Gorgulu O, Fomani FK, Goudarzian AH. Statistical concerns, invalid construct validity, and future recommendations. Nurs Pract Today. (2024) 11:16–21. doi: 10.18502/npt.v11i1.14938
44. Sharif Nia H, She L, Fomani FK, Kaur H, Sánchez-Teruel D, Froelicher ES, et al. Psychometric evaluation of the Persian version of religious orientation scale in Iranian patients with cancer. J Religion Health. (2021) 60:3658–74. doi: 10.1007/s10943-021-01384-6
45. Hosseini L, Sharif Nia H, Ashghali Farahani M. Development and psychometric evaluation of family caregivers’ hardiness scale: a sequential-exploratory mixed-method study. Front Psychol. (2022) 13:807049. doi: 10.3389/fpsyg.2022.807049
46. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Marketing Res. (1981) 18:39–50. doi: 10.1177/002224378101800104
47. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Marketing Science. (2015) 43:115–35. doi: 10.1007/s11747-014-0403-8
49. Reis RS, Hino A, Añez C. Perceived stress scale. J Health Psychol. (2010) 15:107–14. doi: 10.1177/1359105309346343
50. Örücü MÇ, Demir A. Psychometric evaluation of perceived stress scale for Turkish university students. Stress Health: J Int Soc Invest Stress. (2009) 25:103–9. doi: 10.1002/smi.1218
51. Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Counseling. (2006) 9:135–47. doi: 10.1002/j.2161-1882.2006.tb00100.x
52. Ong L, Linden W, Young S. Stress management: what is it? J psychosomatic Res. (2004) 56:133–7. doi: 10.1016/S0022-3999(03)00128-4
53. Sharif Nia H, She L, Kaur H, Boyle C, Khoshnavay Fomani F, Hoseinzadeh E, et al. A predictive study between anxiety and fear of COVID-19 with psychological behavior response: the mediation role of perceived stress. Front Psychiatry. (2022) 13:851212. doi: 10.3389/fpsyt.2022.851212
54. Dewe P, O’Driscoll M. Stress management interventions: what do managers actually do? Personnel Rev. (2002) 31:143–65. doi: 10.1108/00483480210416847
55. Boyacı K, Şensoy F, Beydağ KD, Kıyak M. Stress and stress management in health institutions. Procedia-Social Behav Sci. (2014) 152:470–5. doi: 10.1016/j.sbspro.2014.09.233
56. Orzechowska A, Zajączkowska M, Talarowska M, Gałecki P. Depression and ways of coping with stress: a preliminary study. Med Sci Monit. (2013) 19:1050–6. doi: 10.12659/MSM.889778
57. Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. (2019) 125:1417–31. doi: 10.1002/cncr.31943
58. Algorani EB, Gupta V. Coping mechanisms. In: StatPearls. Florida, USA: StatPearls Publishing (2023).
59. Aust H, Rüsch D, Schuster M, Sturm T, Brehm F, Nestoriuc Y. Coping strategies in anxious surgical patients. BMC Health Serv Res. (2016) 16:1–10. doi: 10.1186/s12913-016-1492-5
60. Golden-Kreutz DM, Browne MW, Frierson GM, Andersen BL. Assessing stress in cancer patients: A second-order factor analysis model for the Perceived Stress Scale. Assessment. (2004) 11:216–23. doi: 10.1177/1073191104267398
Keywords: perceived stress, validity, reliability, psychometrics, Iran
Citation: Sharif-Nia H, Froelicher ES, Hoseinzadeh E, Kaveh O, Fatehi R and Nowrozi P (2024) Assessing the validity and reliability of the 10-item Persian version of the perceived stress scale in post-surgery patients. Front. Psychiatry 15:1402122. doi: 10.3389/fpsyt.2024.1402122
Received: 16 March 2024; Accepted: 17 May 2024;
Published: 04 June 2024.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
João Carlos Alchieri, Federal University of Rio Grande do Norte, BrazilCopyright © 2024 Sharif-Nia, Froelicher, Hoseinzadeh, Kaveh, Fatehi and Nowrozi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Poorya Nowrozi, bnBvb3J5YTkxQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.