- 1The Third People’s Hospital of Ganzhou, Ganzhou, China
- 2Department of Psychiatry and Psychology, College of Basic Medical Sciences, Tianjin Medical University, Tianjin, China
- 3Chinese Academy of Sciences (CAS) Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, China
- 4Department of Psychology, University of Chinese Academy of Sciences, Beijing, China
Introduction: Several studies have reported that Internet addiction (IA) is more prevalent in the psychiatric disorder population. However, the prevalence of IA and its relationship with clinical variables among Chinese adolescents with schizophrenia is unclear. This study sought to investigate the prevalence of IA and its clinical correlates in Chinese adolescents with schizophrenia, which has not yet been reported.
Methods: Seven hundred and six inpatient adolescents with schizophrenia were recruited. All patients underwent Young’s Internet Addiction Test (IAT) to measure Internet addiction, as well as the Positive and Negative Syndrome Scale (PANSS) for psychopathology.
Results: Our results showed that 186 patients had a total IAT score of 50 or more, bringing the prevalence of IA to 26.3%. Girls (21.7%, 92/424) were less likely to have combined IA than boys (33.3%, 94/282). Compared to those patients without IA, patients with IA had better socioeconomic status, higher probability of living in the city, higher levels of depressive symptoms, excited symptoms, and lower levels of concrete symptoms and PANSS total scores (all p<0.05). Further binary logistic regression analysis indicated that good socioeconomic status, living in the city and PANSS total scores were significantly associated with IA. In addition, correlation analysis showed significant correlations between IA total score and the following parameters: good socioeconomic status, living in the city, negative subscore, concrete subscore, depression subscore, excited subscore and PANSS total score (Bonferroni corrected all p <0.05).
Conclusion: The results of this study indicate that the prevalence of IA in Chinese adolescents with schizophrenia is higher than that in the general population. Several demographic and clinical variables are risk factors for IA in adolescents with schizophrenia.
1 Introduction
Nowadays, the Internet has become an integral part of daily life, bringing great convenience to people in communicating with others, obtaining relaxing entertainment available, and searching for information. The use of the Internet is becoming more and more common in daily life, especially amongst the youth population. However, the Internet has also had negative impacts on individual, which has been described as Internet addiction (IA) or problematic Internet use (1, 2). According to Kandell (3), it is well established that IA is defined as a psychological dependence on the Internet characterized by an increasing investment of resources in Internet-related activities, unpleasant feelings when offline, increasing tolerance for the effects of being online, and denial of problematic behaviors. Although IA has not been diagnosed as a clinical disorder, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, has included Internet Gaming Disorder as an emerging problem for further research (4). There is growing evidence of an association between IA and a range of negative outcomes in adolescents, such as interpersonal problems (5), insomnia (6), suicidal ideation (7, 8), smoking problem behaviors (9), and mental health (10–12). IA is a prominent public health problem among adolescents that has attracted worldwide attention (13). A meta-analysis of data from 31 nationwide studies in seven regions of the world found an overall prevalence of IA of 6% (14). Specifically, the prevalence rates of IA in China range from 6% to 17.4% (15–17).
Several studies have reported that IA is more prevalent among people with psychiatric disorder (18, 19). For example, the prevalence of IA and use of portable games among adolescents with autism spectrum disorder is substantially higher than in the general population (10, 20). Dieris-Hirche, Bottel (21) reported that depressed patients exhibited a high prevalence of co-occurrence of maladaptive Internet use and IA, suggesting that the co-occurrence of depression and IA should be noted and considered in psychiatric service. In addition, Ko, Yen (22) also determined that adolescents with problematic alcohol use were more likely to have IA. However, only a few studies have investigated the prevalence of IA in patients with schizophrenia. One recent study by Lee, Chung (23) examined the contribution of stress and coping strategies to problematic internet use in Korean adults with schizophrenia spectrum disorders. They reported that patients with schizophrenia spectrum disorders showed a high prevalence of problematic Internet use at 22.0%. However, it is noteworthy that no studies have reported the prevalence of IA among adolescents with schizophrenia.
To our knowledge, there are no studies on schizophrenia with Internet addiction in the Chinese Han population, especially in the adolescent population. Therefore, the main objectives of this were to 1) investigate the prevalence of IA among Chinese adolescents with schizophrenia, 2) compare the prevalence in this study sample with previous surveys conducted in the general adolescent population in China, and 3) determine the demographic and clinical characteristics of IA among Chinese adolescents with schizophrenia. We hypothesized that the prevalence of IA in Chinese adolescents with schizophrenia would be much higher than in the general adolescent population and that some clinical variables would be risk factors for IA.
2 Methods
2.1 Setting and subjects
The study was conducted at the Third People’s Hospital of Ganzhou city from June, 2018 to October, 2021. This hospital is a public psychiatric hospital owned by Ganzhou city, with a total population of approximately 9 million. We approached all inpatients using a cross-sectional naturalistic design.
We recruited 706 patients who met the following criteria: 1) 13-18 years old and Han Chinese; 2) diagnosed with schizophrenia or schizoaffective disorder by two psychiatrists using the Chinese version of Structured Clinical Interview for DSM-IV (SCID); and 3) no other psychiatric diagnoses.
Participants were excluded when the following criteria were met: 1) having severe physical disorders; 2) having drug and alcohol abuse/dependence except for nicotine; 3) being unable to provide written formal informed consent.
The study was approved by the Institutional Review Board (IRB) of the Third People’s Hospital of Ganzhou, and written informed consent was obtained from all patients or their legal guardians after receiving a full explanations regarding the study procedures.
The sample size was determined using the formula n = Z2p(1-p)/d2. n = sample size; Z= 95% confidence interval, equal to 1.96; p = expected prevalence, equal to 0.22 based on a study of adult schizophrenia (23); d = 0.05 (5%), marginal error. The final sample size included in this study (n = 706) was significantly larger than the required sample size (n = 264), which indicates that our sample size had adequate power.
2.2 Data collection and measurements
A detailed questionnaire was completed collecting general information, socio-demographic characteristics, and medical and psychological conditions. Also, the researchers collected available records and collateral data sources (from family and/or treating clinician). The following data were collected for each patients: sex, age, education, family structure, socioeconomic status, place of residence, age of onset, age at first hospitalization, number of hospitalizations, and duration of illness. Gender- and age-specific body mass index (BMI) cutoff points recommended by the Working Group for Obesity in China (WGOC) were used to define overweight and obesity (24).
Patients’ psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS) (25) by four psychiatrists who were blind to the clinical status of patients. To ensure consistency and reliability of the measurement throughout the study, these four psychiatrists, who had at least 5 years of clinical experience, simultaneously attended a training course in the use of the PANSS before the study began. After training, their inter-rater correlation coefficients for the PANSS total score were maintained at 0.83. In addition, the five-factor model of the PANSS proposed by Wallwork, Fortgang (26) was used to assess the psychopathology of patients. The five factors include a positive factor (items P1, P3, P5, G9), a negative factor (items N1, N2, N3, N4, N6, G7), a concrete/disorganized factor (items P2, N5, G11), an excited factor (items P4, P7, G8, G14) and a depressed factor (items G2,G3 and G6).
IA was assessed by a Chinese version of the Internet addiction test (IAT) (27, 28), which consisted of 20 items rated on a five-point Likert scale, covering the extent to which their Internet use affects their daily life, social life, productivity, sleeping pattern, and feelings. The total score ranges from 20 to 100, with higher score indicating more serious problems caused by internet use. IA was assessed by summing the IAT scores with a cut-off point of ≥ 50 being classified as IA (29).
2.3 Data analysis
In the present study, the Kolmogorov-Smirnov one-sample test was used to measure the normal distribution of continuous data. Since all continuous data conformed to a normal distribution, comparisons of demographic and clinical variables between the IA and non-IA groups were performed using independent samples t-tests for continuous variables and chi-square tests for categorical variables. Prevalence of IA was described as a percentage and analyzed using chi-square tests. Bonferroni correction was used to adjust for multiple testing. A binary logistic regression model was used to determine which factors had a significant effect on IA. In addition, odds ratios (OR) for categorical variables were calculated by X2 tests and adjusted ORs were calculated by binary logistic methods after controlling for confounders.
All statistical analyses were performed in SPSS (version 21.0; SPSS Inc., Chicago, Illinois, USA). All p-values were 2-tailed, and the significance level was set at 0.05.
3 Results
3.1 Demographic and clinical characteristics of Chinese adolescents with schizophrenia
A total of 706 inpatients, including 282 boys and 424 girls, were included in our study. The mean age of the patients was 15.41 [standard deviation (SD) =1.45], ranging from 13 to 18 years. The mean duration of education was 8.48 years (SD =1.38) with a range of 6 to 12 years. The mean age of onset was 13.84 years (SD =2.14), with a range of 6 to 18 years. The mean duration of illness was 20.81 months (SD =23.12), with a range of 1 to 240 months. The average of age of hospitalization at onset was 14.45 years (SD =1.69), ranging from 9 to 18 years. The mean number of hospitalizations was 3.10 (SD =2.19) with a range of 1 to 17.
The mean PANSS scores were: positive, 14.82 ± 6.83; negative, 23.93 ± 8.40; concrete, 5.06 ± 1.65; depressive, 8.94 ± 4.20; excited, 13.39 ± 7.62 and total score, 98.06 ± 15.88.
3.2 Prevalence, demographic and clinical variables in IA versus non-IA participants
The prevalence of IA was 26.3% (186/706). Girls (21.69%, 92 of 424) were less likely than boys (33.33%, 94 of 282) to have a comorbid IA (X2 = 11.82, df=1, p=0.001). After controlling for age and education, IA rates for boys were 1.80 times higher than for girls (B=0.59, Wald statistic=11.674, p <0.001, OR=1.804, 95%CI=1.286-2.531).
As shown in Table 1, the clinical and sociodemographic characteristics of IA and non-IA adolescents with schizophrenia were compared. IA patients were more likely to be boys (p=0.001), have better socioeconomic status (p=0.000), live in urban areas (p=0.000), higher levels of depressive symptoms (p=0.000), and excited symptoms (p=0.000), but lower levels of concrete symptoms (p=0.043) and PANSS total score (p=0.000).
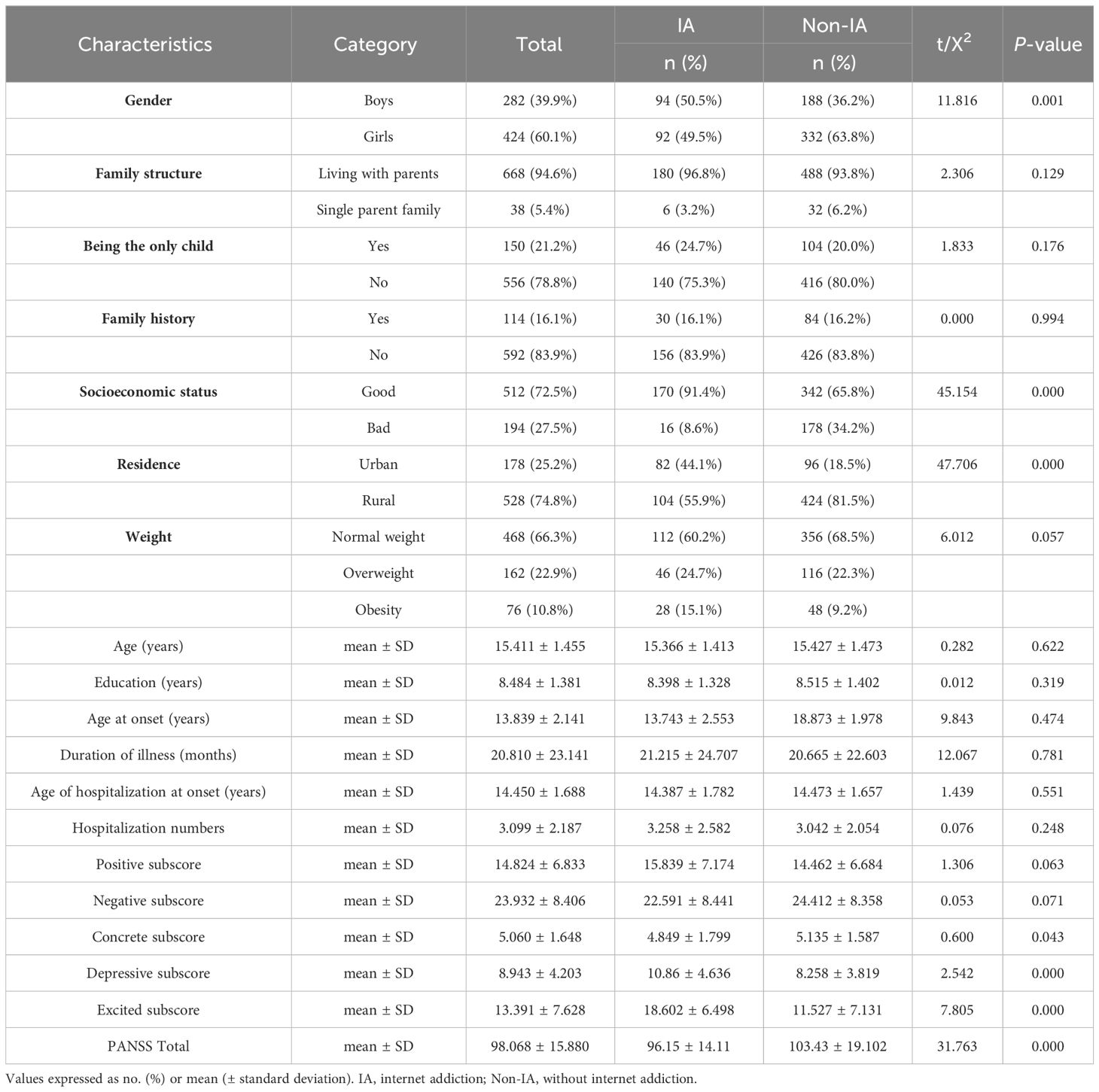
Table 1 Demographic and clinical characteristics between the IA and non-IA in adolescents with schizophrenia (n = 706).
3.3 Correlation of IA with demographic and clinical characteristics
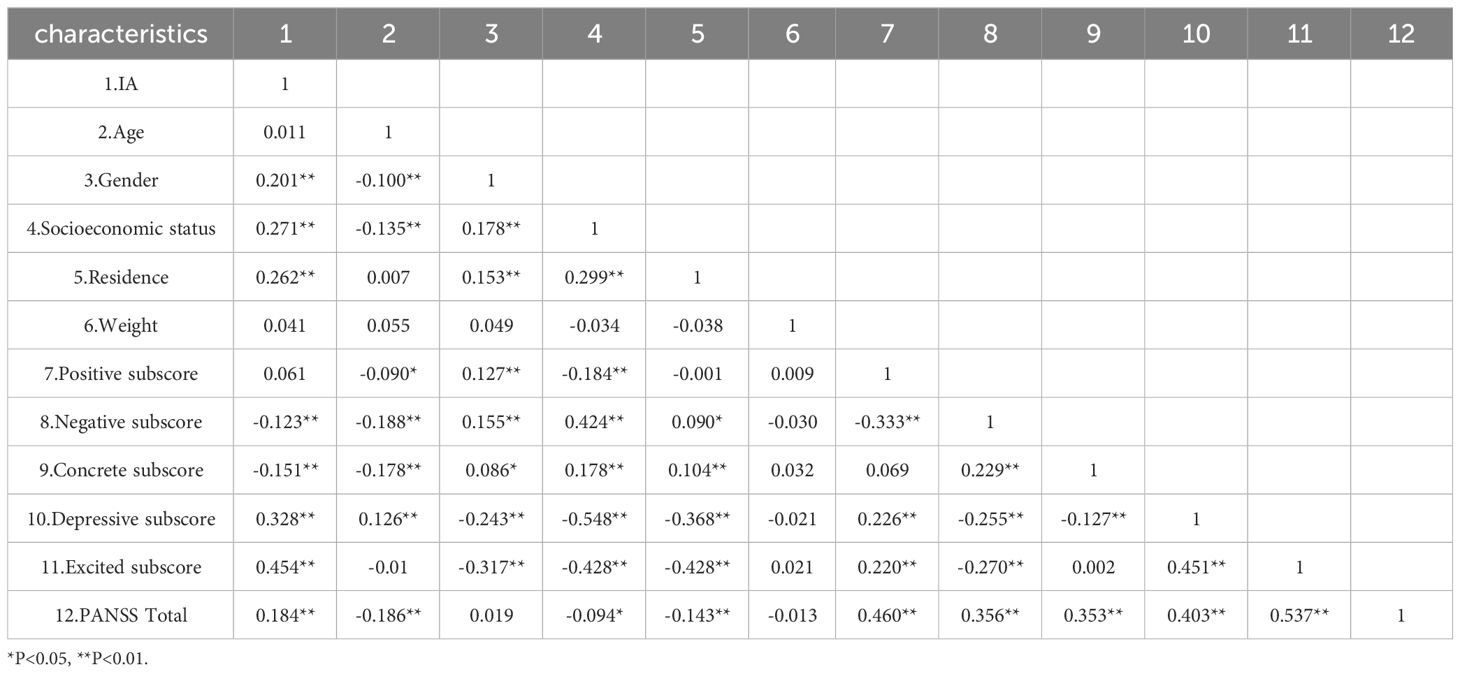
The mean total IA score for all patients was 41.90 ± 18.93. Pearson correlation analysis showed that IA total score was associated with gender (r=0.201, p<0.01), socioeconomic status (r=0.271, p<0.01), place of residence (r=0.262, p<0.01), negative score (r=-0.123, p<0.01), concrete score (r=-0.151, p<0.01), depression score (r=0.328, p<0.01), excited score (r=0.454, p<0.01), and total PANSS score (r=0.184, p<0.01). All these associations remained significant after Bonferroni correction (all p<0.05). Table 2 shows the correlations between IA and demographic data or clinical characteristics.
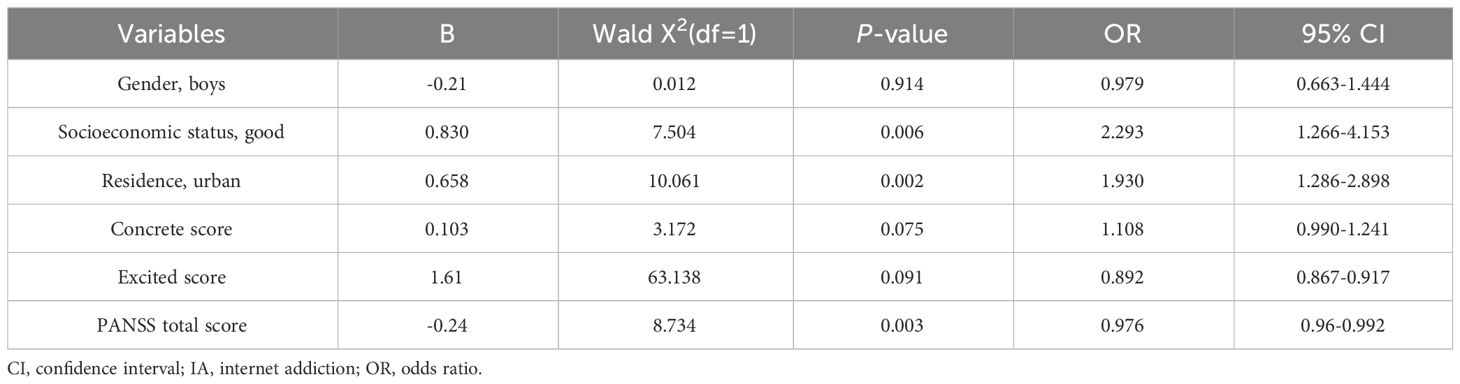
We then focused on risk factors for IA in adolescents with schizophrenia. Variables with significant differences in univariate analysis were included in logistic regression analysis (Backward: Wald). As shown in Table 3, the risk factors for IA were as follows: socioeconomic status(good) (B=0.83, P<0.01, OR=2.293), place of residence(urban) (B=0.658, P<0.01, OR=1.93), and PANSS total score (B=-0.24, P<0.01, OR=0.976).
4 Discussion
To our best knowledge, this was the first study to examine the prevalence and clinical correlates of IA among inpatients with schizophrenia in a Chinese adolescent population. We found that 26.3% of adolescents with schizophrenia met the criteria for IA and that significant clinical correlates of IA in this population were having good socioeconomic status, living in an urban area, and having a low PANSS total score.
Based on the IAT, Lam, Peng (30) found that 10.8% of adolescents aged 13-18 year in China were moderately to severely addicted to the Internet. Cao and Su (31) reported that 18.2% of junior high school students in China were classified as IA based on the same test. Notably, the prevalence of IA among adolescents with schizophrenia in our study was 26.3%, indicating a relatively high prevalence of IA compared to the prevalence in the general adolescent population in China. Schizophrenia is a well-known risk factor for addictive disorders (32). Brunette, Mueser (33) showed that more than half of the patients with first-episode psychosis had a substance use disorders. Also, Desai and Potenza (34) found that individuals with schizophrenia/schizoaffective disorder may be at particularly high risk for problem and pathological gambling. Taken together, these findings suggest that higher prevalence of IA may occur in patients with schizophrenia, especially in adolescents with schizophrenia. One possible explanation is that dopamine dysregulation has been implicated in both schizophrenia and addiction disorders (35, 36). Adolescents with schizophrenia may exhibit dysregulated dopamine transmission, leading to a heightened sensitivity to rewarding stimuli, including those encountered online. This hyperdopaminergic state could contribute to the reinforcing effects of internet use, promoting addictive behaviors.
Another possible explanation for the high prevalence of IA in adolescents with schizophrenia is the perceived stigma of the patients. Perceived and experienced stigma as well as self-stigma are phenomena involving a high proportion of patients with schizophrenia spectrum disorders (37). A previous study by Li, Guo (38) reported that stigma is associated with social withdrawal in patients with schizophrenia, which leads them to lose their jobs or drop out of school. Due to anonymity, people with schizophrenia who experience stigma avoid face-to-face contact whenever possible, preferring to use the Internet to exchange information (39, 40). In this way, it is relatively easy to become addicted to the Internet in the absence of control.
We also found a significant gender difference in the prevalence of comorbid IA among adolescents with schizophrenia, showing a higher prevalence among males than females (33.3% vs. 21.7%). Numerous studies have shown gender differences in the prevalence of IA among the general adolescent population in China (41, 42). According to Chen, Kang (41), this may be due to the fact that males are more involved in online activities such as gaming, pornography, and gambling, which may lead to pathological Internet use. Consistent with the results for the general adolescent population, our results also suggest that the prevalence of IA is higher among males than females. The gender differences in IA found in this study may be due to the fact that females with schizophrenia have less social cognitive impairment than males (43).
Another finding of our present study was that good socioeconomic status and living in an urban area were independently associated with IA. Our study showed that Internet use among adolescents with schizophrenia was influenced by environmental factors. Good socioeconomic status and living in an urban area gave patients more access to the Internet. Previous findings reported that more Internet use was associated with higher economic income (44, 45) and living in urban areas (46).
Consistent with previous studies (2, 47), we also found that IA was associated with patients psychopathology. In our current study, those patients with lower PANSS levels were significantly associated with an increased risk of IA. One reason for this may be that well-conditioned patients can successfully use the Internet. Higher PANSS scores mean that patients are in worse condition, such attention deficit or delusional interpretations, as well as motivational deficits, which lead to rejection of Internet use (48).
Several limitations of this study should be noted. First, the sample was drawn from a general hospital in Ganzhou, mainland China. Therefore, the results are not necessarily representative of the entire mainland China, let alone other Asian countries. Second, regarding our sample of study subjects, the participants in this study were recruited from an acute inpatient psychiatry unit. Therefore, the results of the study cannot be generalized to outpatients or community patients. Third, our investigation was a cross-sectional design, which precludes proof of causality. Fourth, we did not collect data on all the variables that could be related to IA, such as the purpose of Internet use and medical conditions, including medications. Fifth, previous studies have shown that, there is a positive relationship between internet addiction and obesity (49, 50). However, due to the sample size of the subjects, the correlation between internet addiction and obesity in this study did not reach a significant level, which requires further research in the future.
In summary, our results show the prevalence of comorbid IA among Chinese adolescents with schizophrenia was 26.3%, suggesting that IA is common in this population. Furthermore, patients with IA have good socioeconomic status, live in urban areas, and have low PANSS score. The present study may suggest that IA in adolescents with schizophrenia is influenced by environmental and psychopathology factors. Therefore, clinicians working with adolescents with schizophrenia should consider IA and related factors and intervene with IA.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Institutional Review Board (IRB) of the Third People’s Hospital of Ganzhou. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
YZ: Investigation, Writing – original draft. YL: Methodology, Writing – review & editing. AH: Data curation, Investigation, Writing – original draft. X-YZ: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We acknowledge all study participants and all mental health professional in selected clinic for their support and help.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kuss DJ, Van Rooij AJ, Shorter GW, Griffiths MD, van de Mheen D. Internet addiction in adolescents: Prevalence and risk factors. Comput Hum Behav. (2013) 29:1987–96. doi: 10.1016/j.chb.2013.04.002
2. Lee J-Y, Kim SY, Bae KY, Kim JM, Shin IS, Yoon JS, et al. Prevalence and risk factors for problematic Internet use among rural adolescents in Korea. Asiaa.centsh Psychiatry. (2018) 14:e12310. doi: 10.1111/appy.12310
3. Kandell JJ. Internet addiction on campus: the vulnerability of college students. Cyberpsychol Behav. (1998) 1:11–7. doi: 10.1089/cpb.1998.1.11
4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Pub, Washington, DC (2013).
5. Seo M, Kang HS, Yom Y-H. Internet addiction and interpersonal problems in Korean adolescents. Comput Inf Nurs. (2009) 27:226–33. doi: 10.1097/NCN.0b013e3181a91b3f
6. Choi K, Son H, Park M, Han J, Kim K, Lee B, et al. Internet overuse and excessive daytime sleepiness in adolescents. Psychiatry Clin Neurosci. (2010) 63:455–62. doi: 10.1111/j.1440-1819.2009.01925.x
7. Liu H-C, Liu SI, Tjung JJ, Sun FJ, Huang HC, Fang CK. Self-harm and its association with internet addiction and internet exposure to suicidal thought in adolescents. J Formosan Med Assoc. (2016) 116:153–60. doi: 10.1016/j.jfma.2016.03.010
8. Sami H, Danielle L, Lihi D, Elena S. The effect of sleep disturbances and internet addiction on suicidal ideation among adolescents in the presence of depressive symptoms. Psychiatry Res. (2018) 267:327–32. doi: 10.1016/j.psychres.2018.03.067
9. Mei S, Gao T, Li J, Zhang Y, Chai J, Wang L, et al. Internet addiction in college students and its relationship with cigarette smoking and alcohol use in Northeast China. Asiaa.asthip Psychiatry. (2017) 9:e12281. doi: 10.1111/appy.12281
10. Kawabe K, Horiuchi F, Miyama T, Jogamoto T, Aibara K, Ishii E, et al. Internet addiction and attention-deficit/hyperactivity disorder symptoms in adolescents with autism spectrum disorder. Res Dev Disabil. (2019) 89:22–8. doi: 10.1016/j.ridd.2019.03.002
11. Taylor S, Pattara-Angkoon S, Sirirat S, Woods D. The theoretical underpinnings of Internet addiction and its association with psychopathology in adolescence. Int J Adolesc Med Health. (2017) 31.20170046. doi: 10.1515/ijamh-2017-0046
12. Yadav P, Banwari G, Parmar C, Maniar R. Internet addiction and its correlates among high school students: a preliminary study from Ahmedabad, India. Asian J Psychiatr. (2013) 6:500–5. doi: 10.1016/j.ajp.2013.06.004
13. Kim BS, Chang SM, Park JE, Seong SJ, Won SH, Cho MJ. Prevalence, correlates, psychiatric comorbidities, and suicidality in a community population with problematic Internet use. Psychiatry Res. (2016) 244:249–56. doi: 10.1016/j.psychres.2016.07.009
14. Cheng C, Li AY-L. Internet addiction prevalence and quality of (real) life: a meta-analysis of 31 nations across seven world regions. Cyberpsychol Behavior Soc Network. (2014) 17:755–60. doi: 10.1089/cyber.2014.0317
15. Lai C-M, Mak KK, Watanabe H, Ang RP, Pang JS, Ho RC. Psychometric properties of the internet addiction test in Chinese adolescents. J Pediatr Psychol. (2013) 38:794–807. doi: 10.1093/jpepsy/jst022
16. Lin M-P, Wu JYW, You J, Hu WH, Yen CF. Prevalence of internet addiction and its risk and protective factors in a representative sample of senior high school students in Taiwan. J Adolescence. (2018) 62:38–46. doi: 10.1016/j.adolescence.2017.11.004
17. Wu X, Chen X, Han J, Meng H, Luo J, Nydegger L, et al. Prevalence and factors of addictive internet use among adolescents in Wuhan, China: interactions of parental relationship with age and hyperactivity-impulsivity. PloS One. (2013) 8:e61782. doi: 10.1371/journal.pone.0061782
18. Ho RC, Zhang MW, Tsang TY, Toh AH, Pan F, Lu Y, et al. The association between internet addiction and psychiatric co-morbidity: a meta-analysis. BMC Psychiatry. (2014) 14:183. doi: 10.1186/1471-244X-14-183
19. Ko C-H, Yen JY, Yen CF, Chen CS, Chen CC. The association between Internet addiction and psychiatric disorder: A review of the literature. Eur Psychiatry. (2012) 27:1–8. doi: 10.1016/j.eurpsy.2010.04.011
20. So R, Makino K, Fujiwara M, Hirota T, Ohcho K, Ikeda S, et al. The prevalence of internet addiction among a Japanese adolescent psychiatric clinic sample with autism spectrum disorder and/or attention-deficit hyperactivity disorder: A cross-sectional study. J Autism Dev Disord. (2017) 47:1–8. doi: 10.1007/s10803-017-3148-7
21. Dieris-Hirche J, Bottel L, Bielefeld M, Steinbüchel T, Kehyayan A, Dieris B, et al. Media use and Internet addiction in adult depression: A case-control study. Comput Hum Behav. (2017) 68:96–103. doi: 10.1016/j.chb.2016.11.016
22. Ko C-H, Yen JY, Yen CF, Chen CS, Weng CC, Chen CC. The association between Internet addiction and problematic alcohol use in adolescents: the problem behavior model. CyberPsychol Behav. (2008) 11:571–6. doi: 10.1089/cpb.2007.0199
23. Lee J-Y, Chung YC, Song JH, Lee YH, Kim JM, Shin IS, et al. Contribution of stress and coping strategies to problematic Internet use in patients with schizophrenia spectrum disorders. Compr Psychiatry. (2018) 87:89–94. doi: 10.1016/j.comppsych.2018.09.007
24. Zhang J, Wang H, Wang Z, Du W, Su C, Zhang J, et al. Prevalence and stabilizing trends in overweight and obesity among children and adolescents in China, 2011-2015. BMC Public Health. (2018) 18:571. doi: 10.1186/s12889-018-5483-9
25. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1986) 13:261–76. doi: 10.1093/schbul/13.2.261
26. Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr Res. (2012) 137:246–50. doi: 10.1016/j.schres.2012.01.031
27. Ni X, Yan H, Chen S, Liu Z. Factors influencing internet addiction in a sample of freshmen university students in China. Cyberpsychol Behav. (2009) 12:327–30. doi: 10.1089/cpb.2008.0321
28. Young KS. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol Behav. (1998) 1. doi: 10.1089/cpb.1998.1.237
29. Khazaal Y, Billieux J, Thorens G, Khan R, Louati Y, Scarlatti E, et al. French validation of the internet addiction test. Cyberpsychol Behav. (2008) 11:703–6. doi: 10.1089/cpb.2007.0249
30. Lam LT, Peng ZW, Mai JC, Jing J. Factors associated with Internet addiction among adolescents. Cyberpsychol Behav. (2009) 12:551–5. doi: 10.1089/cpb.2009.0036
31. Cao F, Su L. Internet addiction among Chinese adolescents: prevalence and psychological features. Child Care Health Dev. (2010) 33:275–81. doi: 10.1016/j.schres.2017.06.039
32. Green AI, Khokhar JY. Addiction and schizophrenia: A translational perspective. Schizophr Res. (2017) 194:1–3. doi: 10.1016/j.schres.2017.10.008
33. Brunette MF, Mueser KT, Babbin S, Meyer-Kalos P, Rosenheck R, Correll CU, et al. Demographic and clinical correlates of substance use disorders in first episode psychosis. Schizophr Res. (2017) 194:4–12. doi: 10.1016/j.schres.2017.06.039
34. Desai RA, Potenza MN. A cross-sectional study of problem and pathological gambling in patients with schizophrenia/schizoaffective disorder. J Clin Psychiatry. (2009) 70:1250–7. doi: 10.4088/JCP.08m04359
35. Khokhar JY, Dwiel LL, Henricks AM, Doucette WT, Green AI. The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr Res. (2018) 194:78–85. doi: 10.1016/j.schres.2017.04.016
36. Lowe DJE, Sasiadek JD, Coles AS, George TP. Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci. (2018) 269:107–20. doi: 10.1007/s00406-018-0970-7
37. Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. (2013) 12:155–64. doi: 10.1002/wps.20040
38. Li J, Guo YB, Huang YG, Liu JW, Chen W, Zhang XY, et al. Stigma and discrimination experienced by people with schizophrenia living in the community in Guangzhou, China. Psychiatry Res. (2017) 255:225–31. doi: 10.1016/j.psychres.2017.05.040
39. Schrank B, Sibitz I, Unger A, Amering M. How patients with schizophrenia use the internet: qualitative study. J Med Internet Res. (2010) 12:e70. doi: 10.2196/jmir.1550
40. Sunil S, Sharma MK, Amudhan S. Schizophrenia and internet use: Perils and potentials. Asian J Psychiatr. (2021) 58:102586. doi: 10.1016/j.ajp.2021.102586
41. Chen Y, Kang Y, Gong W, He L, Jin Y, Zhu X, et al. Investigation on Internet addiction disorder in adolescents in Anhui, People’s Republic of China. Neuropsychiatr Dis Treat. (2016) 12:2233–6. doi: 10.2147/NDT.S110156
42. Xin M, Xing J, Pengfei W, Houru L, Mengcheng W, Hong Z. Online activities, prevalence of Internet addiction and risk factors related to family and school among adolescents in China. Addictive Behav Rep. (2018) 7:14–8. doi: 10.1016/j.abrep.2017.10.003
43. Caqueo-Urízar A, Fond G, Urzúa A, Boyer L. Gender differences in schizophrenia: A multicentric study from three Latin-America countries. Psychiatry Res. (2018) 266:65–71. doi: 10.1016/j.psychres.2018.05.032
44. Jo HS, Hwang M-S, Lee HJ. Market segmentation of health information use on the Internet in Korea. Int J Med Inf. (2010) 79:707–15. doi: 10.1016/j.ijmedinf.2010.07.006
45. Klinar I, Balažin A, Bašić M, Plantaš I, Biškupić K. Increased demand for E-mail health consultation service: analysis of a Web survey. Coll Antropol. (2010) 34:481–5.
46. Maijala R, Anttila M, Koivunen M, Pitkänen A, Kuosmanen L, Välimäki M. Internet delivered question and answer column for patients with schizophrenia. Med Inf. (2015) 40:267–78. doi: 10.3109/17538157.2014.924946
47. Liberatore KA, Rosario K, Martí LNCD, Martínez KG. Prevalence of internet addiction in latino adolescents with psychiatric diagnosis. Cyberpsychol Behav Soc Network. (2011) 14:399–402. doi: 10.1089/cyber.2010.0252
48. Välimäki M, Kuosmanen L, Hätönen H, Koivunen M, Pitkänen A, Athanasopoulou C, et al. Connectivity to computers and the Internet among patients with schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr Dis Treat. (2017) 13:1201–9. doi: 10.2147/NDT.S130818
49. Azizi M, Abbasi B, Aghaei H. Relationship between Internet addiction and body mass index and the predictive role of emotion dysregulation. Front Psychol. (2024) 14:1305828. doi: 10.3389/fpsyg.2023.1305828
Keywords: adolescents, Chinese, internet addiction, schizophrenia, prevalence
Citation: Zhong Y, Li Y, Hu A and Zhang X-Y (2024) Prevalence, demographics and clinical characteristics of Internet addiction among Chinese adolescents with schizophrenia. Front. Psychiatry 15:1398479. doi: 10.3389/fpsyt.2024.1398479
Received: 10 March 2024; Accepted: 15 April 2024;
Published: 03 May 2024.
Edited by:
Soumitra Das, NorthWestern Mental Health, AustraliaReviewed by:
Kaushik Nag, Tripura Medical College & Dr. B.R. Ambedkar Memorial Teaching Hospital, IndiaEvan Johnson, Western Health, Australia
Copyright © 2024 Zhong, Li, Hu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiang-Yang Zhang, emhhbmd4eUBwc3ljaC5hYy5jbg==
 Yunhui Zhong
Yunhui Zhong Yibo Li2
Yibo Li2 Xiang-Yang Zhang
Xiang-Yang Zhang