- 1Department of Acupuncture and Moxibustion, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 2College of Acupuncture and Massage, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 3School of Basic Medical Sciences, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, Shandong, China
- 4Department of Acupuncture-Moxibustion and Tuina, Qilu Hospital of Shandong University, Jinan, Shandong, China
Objective: This study aimed to assess the clinical effectiveness and safety of electroacupuncture (EA) for the treatment of postpartum depression (PPD).
Methods: We systematically retrieved relevant randomized controlled trials (RCTs) from electronic databases, including PubMed, Cochrane Library, China National Knowledge Infrastructure, EMBASE, China Science and Technology Journal Database, Chinese Biological Medical Database, and the Wanfang database from their inception to November 2023. The outcomes measured were the Hamilton Depression Rating Scale (HAMD) scores, Edinburgh Postnatal Depression Scale (EPDS) scores, adverse events (AEs), and the total response rate. The study aimed to estimate heterogeneity, publication bias, mean difference (MD), and risk ratios (RR) with 95% confidence intervals (CIs).
Results: This study included 12 RCTs with a total of 1364 participants (571 in the treatment group and 793 in the control group) for analysis. The results of the meta-analysis indicated that EA did not significantly reduce HAMD (MD = 1.49, 95% CI = [−0.30, 3.27], P = 0.1, I2 = 0%) and EPDS (MD = 1.12, 95% CI = [−1.62, 3.85], P = 0.42, I2 = 32%) scores compared to sham EA among patients with PPD, resulting in low heterogeneity. In terms of the total response rate, the EA group exhibited superior results compared to the placebo group (RR = 1.77, 95% CI = [1.15, 2.74], P = 0.01, I2 = 0%) and the sham EA group (RR = 1.2, 95% CI = [1.02, 4.4], P = 0.02, I2 = 0%), with statistical significance and low heterogeneity. The incidence of AEs was lower, also with low heterogeneity (RR = 0.9, 95% CI = [0.57, 1.43], P = 0.66, I2 = 12%).
Conclusion: The current evidence indicates that the effectiveness and safety of EA in the treatment of PPD warrant affirmation. However, EA does not demonstrate superiority over sham EA in reducing HAMD and EPDS scores in patients with PPD. Due to the limited quantity and quality of curent research, the above conclusion should be further validated through high-quality studies to confirm the efectiveness of EA in PPD management.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=318917, identifier CRD42023318917.
1 Introduction
Postpartum depression (PPD) is a significant mental health issue that has detrimental effects on both mothers and their infants. It is characterized by evident depressive symptoms during the postpartum period, mainly manifesting as feelings of depression, lethargy, and an increased tendency to cry (1). According to a recent meta-analysis encompassing 565 studies from 80 different countries or regions, the global incidence rate of PPD was estimated to be approximately 17.22% (2). Between 10% and 20% of women are at risk of experiencing PPD within the first year after childbirth (3). In addition to the physical discomfort and functional limitations experienced by women after giving birth, PPD exerts a negative impact on the offspring of the affected mothers. Studies have shown that PPD can restrict a woman’s capacity to effectively perform her maternal duties, leading to suboptimal care for her infant (4–6).
Currently, the primary approach for treating PPD involves drug therapy, specifically the use of medications such as fluoxetine and sertraline (7, 8). Despite the minimal effects of these drugs on breastfeeding, concerns persist among breastfeeding mothers. Studies have associated the use of these medications with irritability and sleep disturbances, particularly in premature or low-birth-weight infants (9, 10). In addition, abruptly discontinuing these medications is detrimental to the well-being of the mother and the newborn, leading to numerous adverse effects. An alternative approach to the treatment of PPD involves nonpharmacological methods. Cognitive behavioral therapy (CBT) has been recommended as an evidence-based psychotherapy by clinical practice guidelines for the majority of individuals with PPD (11). Although CBT offers a promising approach, it is essential to take into account the challenges associated with compliance with it (12).
Electroacupuncture (EA) therapy is a form of acupuncture used in complementary and alternative medicine. Its fundamental principle involves the application of electrical current at specific acupoints to regulate the physiological function of the human body, with the aim of treating diseases. Compared to manual acupuncture, EA offers improved control over stimulation parameters, as well as greater repeatability and objectivity (13). There is emerging evidence indicating the therapeutic potential of EA in addressing psychological disorders such as anxiety and depression (14–17). EA has also been used in PPD treatment, showing specific therapeutic benefits. Nevertheless, there is currently a dearth of meta-analyses and systematic reviews on the effectiveness of EA for PPD. The objective of this study is to evaluate the evidence of EA for PPD through a meta-analysis of randomized controlled trials (RCTs).
2 Materials and methods
The Cochrane Handbook for Systematic Reviews of Interventions was used to conduct this meta-analysis, and the Preferred Reporting Items for Systematic Reviews and meta-analyses guidelines were used to describe the results (Supplementary Table S1). The meta-analysis protocol (CRD42023318917) was found in the PROSPERO database.
2.1 Search strategy
To retrieve pertinent articles published up to November 2023, two independent researchers conducted searches on electronic databases, including PubMed, Cochrane Library, China Science and Technology Journal Database (VIP), China National Knowledge Infrastructure (CNKI), Chinese Biological Medical Database (CBM, SinoMed), Wanfang database, and EMBASE. The search included the terms “electroacupuncture” and “Postpartum Depression”. Supplementary Table S2 presents a comprehensive list of the search techniques utilized in this study.
2.2 Inclusion criteria
The studies had to meet specific criteria in order to be eligible for inclusion in this review. The population consisted of individuals diagnosed with PPD, based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM) (18), the Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD) (19), as well as the Hamilton Depression Scale (HAMD), Edinburgh Postpartum Depression Scale (EPDS), and clinical manifestations. Interventions in the study groups included EA alone, EA combined with traditional Chinese medicine (TCM), and EA combined with antidepressants. There were no restrictions on the selection of acupuncture points, specific manipulation techniques, treatment duration, or frequency.
The control group employed treatment methods excluding EA intervention, such as sham EA; blank control; TCM; psychological intervention; and antidepressants such as paroxetine, sertraline, mirtazapine, and venlafaxine. Primary outcome indicators comprised the HAMD scores, EPDS scores, and the total response rate, whereas secondary outcomes involved adverse events (AEs). The study design was based on RCTs that provide comprehensive baseline data and comparative efficacy assessments, encompassing reports containing comprehensive information.
2.3 Data extraction
Two independent researchers (X.F. and X.B.G.) individually examined and calculated all the data. In cases of disagreement, the two investigators engaged in discussions to resolve their differences. If a consensus could not be reached, they consulted another investigator (X.Y.W.), and decisions were made based on a majority vote. All the involved researchers demonstrated proficiency in the administration of EA for the treatment of PPD.
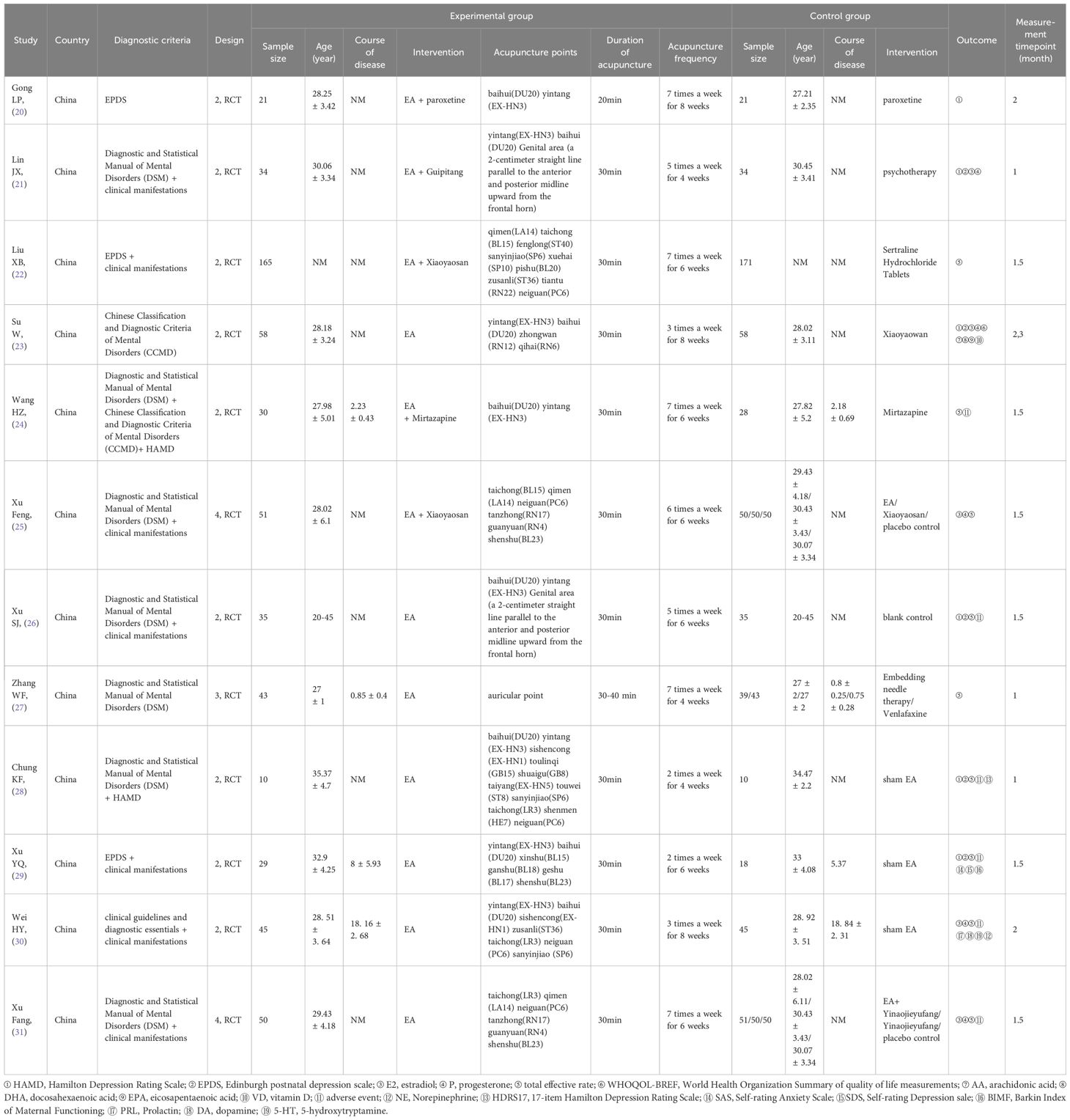
The data presented in this study were obtained from individual clinical trials, including details such as the number of participants in the EA and control groups, demographic details (age), geographical location, study methodology, duration, interventions (such as type of acupuncture, duration, treatment frequency, and acupoint selection), and outcomes (Table 1). If the chosen reports lacked complete data, the authors were contacted via email. Studies that did not yield a response were excluded from our analysis. The third investigator was tasked with resolving any inconsistencies in the data.
2.4 Quality assessment
The quality of the retrieved studies was assessed independently by the two investigators, using revised Cochrane risk-of-bias tool for randomized trials (RoB 2) (32). The RoB 2 tool encompasses six aspects for assessing the risk of bias, which are randomization process, deviations from intended interventions, mising outcome data, measurement of the outcome, selection of the reported result, overall Bias. Each criterion was analyzed and categorized based on the level of risk of bias as low, some concerns, or high.
2.5 Statistical analysis
Data were analyzed using Review Manager (version 5.3) and Stata (version 17.0). Continuous data were processed using the inverse variance method to determine the mean difference (MD) and 95% confidence interval (CI). Using the Mantel–Haenszel method, the total response rate and AEs were incorporated to calculate the risk ratio (RR) and a 95% CI (33). The I2 statistic was employed to assess the heterogeneity among the studies. The studies were classified based on the level of heterogeneity, with low, moderate, or high levels corresponding to I2 values of 25–50%, 50–75%, or >75%, respectively (34). The fixed-effects model was used for meta-analysis if there was no statistical heterogeneity among the findings, while the random-effects model was used when there was statistical heterogeneity. A p-value of less than 0.05 indicated statistical significance. Significant heterogeneity was addressed through sensitivity analysis, subgroup analysis, or solely description.
3 Results
3.1 Overview of literature search
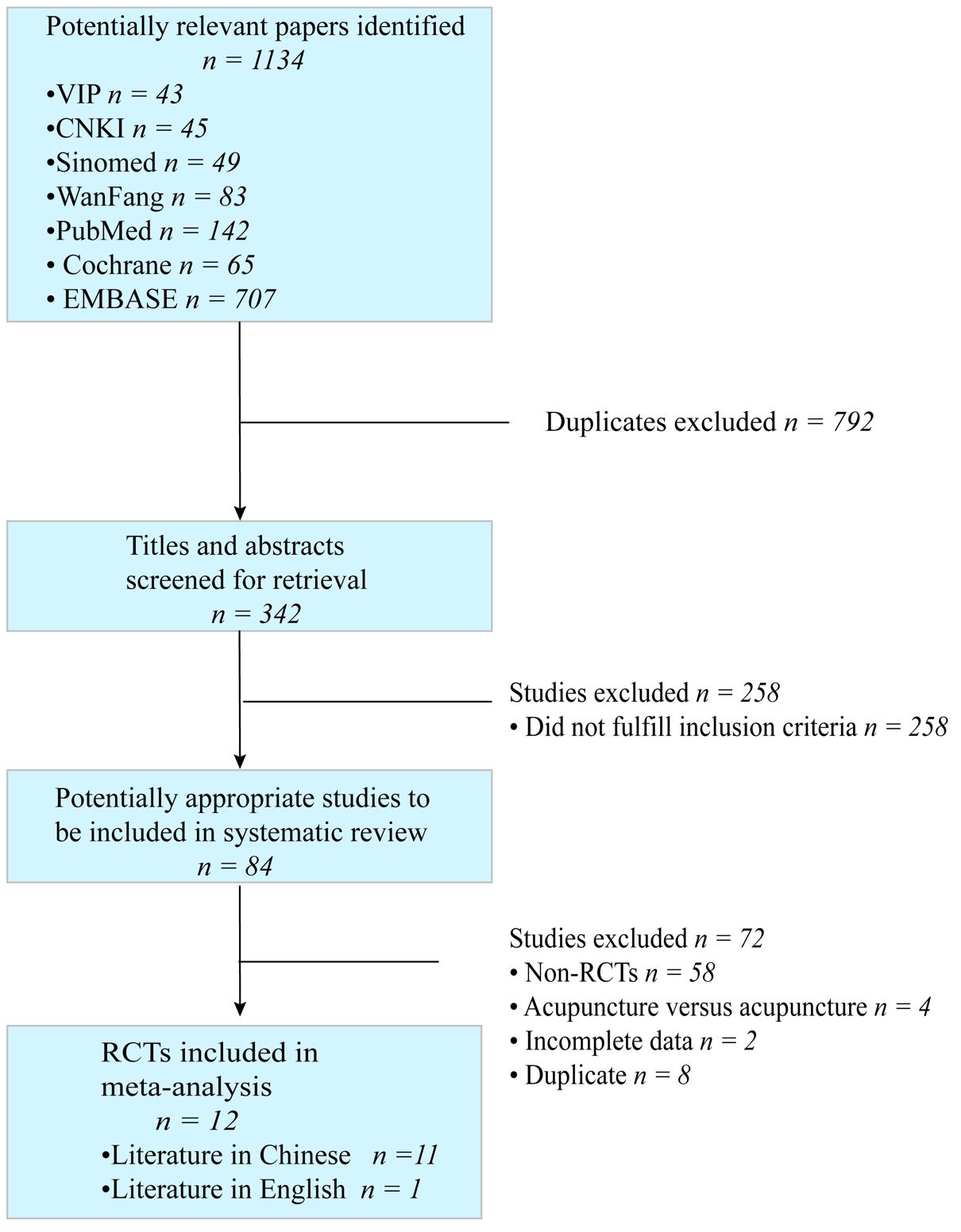
Initially, 1134 studies were retrieved for evaluation and screened according to their title and abstract content. Ultimately, 84 studies were chosen for further analysis. This study included 12 RCTs that investigated the use of EA for the treatment of PPD. Of these, 11 articles were in Chinese and 1 was in English. Figure 1 illustrates the search and selection process.
3.2 Study characteristics
3.2.1 Patients
A total of 571 patients from 12 studies (three of which were divided into two groups) were administered EA, while 793 patients in the control group received sham EA, TCM, antidepressants, no treatment (blank control group), or psychotherapy. Chinese researchers completed the entire work. It is worth watching that there is a lack of standardized diagnostic criteria for PPD. Among the studies included in our analysis, the CCMD was referenced in one study (24), while DSM was cited in eight studies (21, 23–28, 31). EPDS was utilized in four studies (20, 22, 23, 29), and the HAMD was employed in two studies (24, 28). Clinical manifestations were collectively considered in seven studies (21, 22, 25, 26, 29–31), and clinical guidelines and diagnostic essentials, specifically the International Classification of Diseases, 10th edition, were utilized in one study (30). The experimental group comprised a sample size ranging from 10 to 165 patients, while the control group included 10 to 171 patients. Except for one study (27) that did not specify the age of the patients, the participants in the research ranged in age from 20 to 45. Shown in Table 1.
3.2.2 EA interventions
In terms of specific interventions, seven studies (23, 26–31) involved the use of EA alone, two studies (20, 24) involved a combined use of EA and antidepressants, and three studies (21, 22, 25) involved a combined use of EA and TCM. With regard to the selection of acupoints, the names of points were provided in all studies except one (27). The top four acupoints in terms of frequency of use were Baihui (GV20), Yintang (EX-HN3), Taichong (LR3), and Neiguan (PC6). The duration of treatment ranged from four to eight weeks.
3.2.3 Control interventions
In the control group, four studies (20, 22, 24, 27) involved treatment with antidepressants, including paroxetine, sertraline hydrochloride tablets, venlafaxine, and mirtazapine. Furthermore, three cases involved sham EA (28–30), three cases used TCM (23, 25, 31), two cases used placebo control (25, 31), one study used a blank control (26), and one study involved psychotherapy (21).
3.2.4 Outcome measures
Six studies utilized the HAMD (20, 21, 23, 26, 28, 29) scores to assess the alterations in PPD. The EPDS scale was utilized in five studies (21, 23, 26, 28, 29) to evaluate the condition of patients with PPD. Five studies (21, 23, 25, 30, 31) documented alterations in the levels of estradiol and progesterone in the bloodstream of patients with PPD. In addition, the study incorporated outcome indicators such as the score variations of the World Health Organization Summary of Quality of Life measurements, the Self-rating Anxiety Scale, and the Self-rating Depression Scale among patients with PPD. Furthermore, it examined alterations in the levels of dopamine, prolactin, arachidonic acid, vitamin D, docosahexaenoic acid, serotonin, eicosapentaenoic acid, and norepinephrine in the blood of patients with PPD. A total of nine studies (22, 24–31) evaluated the efficacy of the treatment (three of which were divided into two groups) (25, 27, 31). AEs were documented in six studies (24, 26, 28–31).
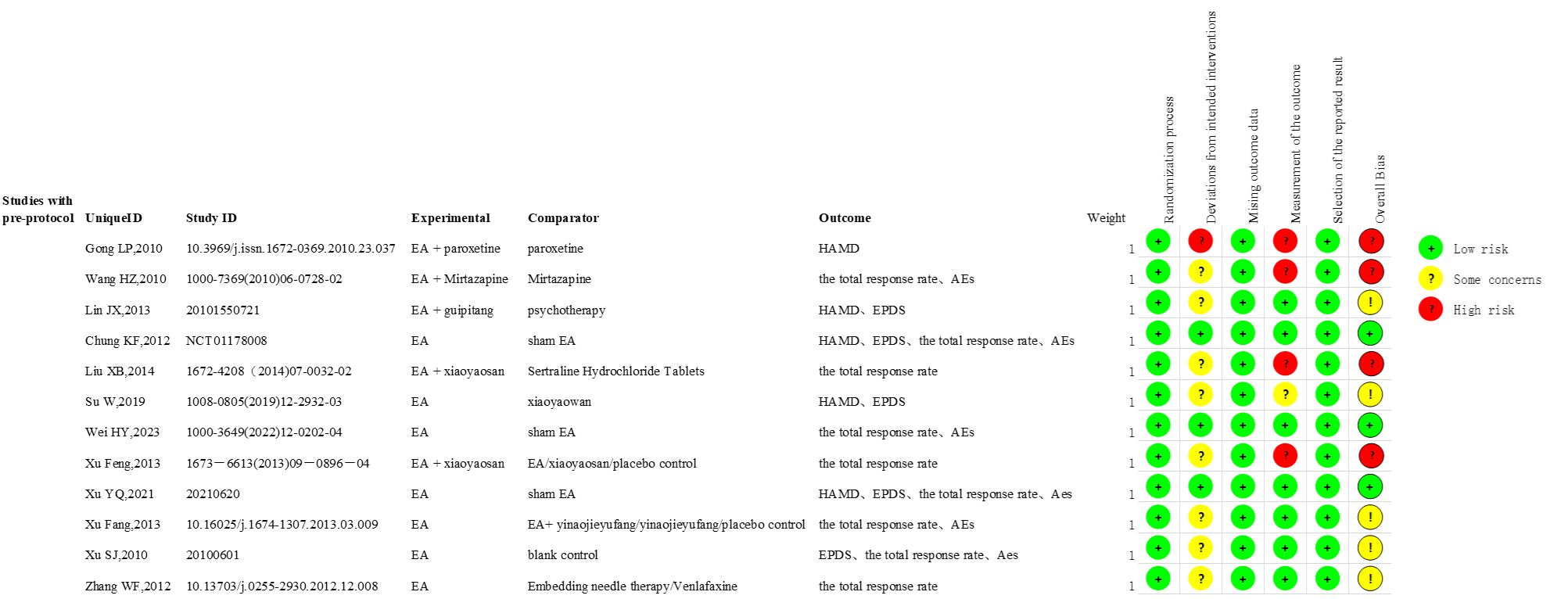
3.3 Risk assessment results
The Cochrane Handbook for Systematic Reviews of Interventions was utilized to access the risk of bias (32). Randomization was demonstrated in the 12 studies included. Eight studies utilized random number tables (21, 23, 25, 26, 28–31), while two studies employed the order of visits (24, 27). The details of the randomization process were not reported in two studies (20, 22). Three studies (21, 26, 29) documented the use of sealed envelopes for concealing the distribution of materials. Two studies (24, 27) achieved concealment through sequential numbering. Other studies did not document the methods for concealing the allocation. Baseline differences between all study intervention groups suggest no problems with the randomization process.
Blinding participants and practitioners is challenging in studies involving acupuncture interventions due to their specific study design characteristics. Nonetheless, three studies (28–30) attempted participant blinding to minimize performance bias. Five studies (21, 28–31) documented the use of blind evaluators, while the majority of other studies did not provide specific details on blinding procedures. All included RCTs maintained data integrity, and no selective reporting of results was identified. Figure 2, Supplementary Figure S1 illustrates the quality assessment findings documented in this study.
3.4 Meta-analysis findings
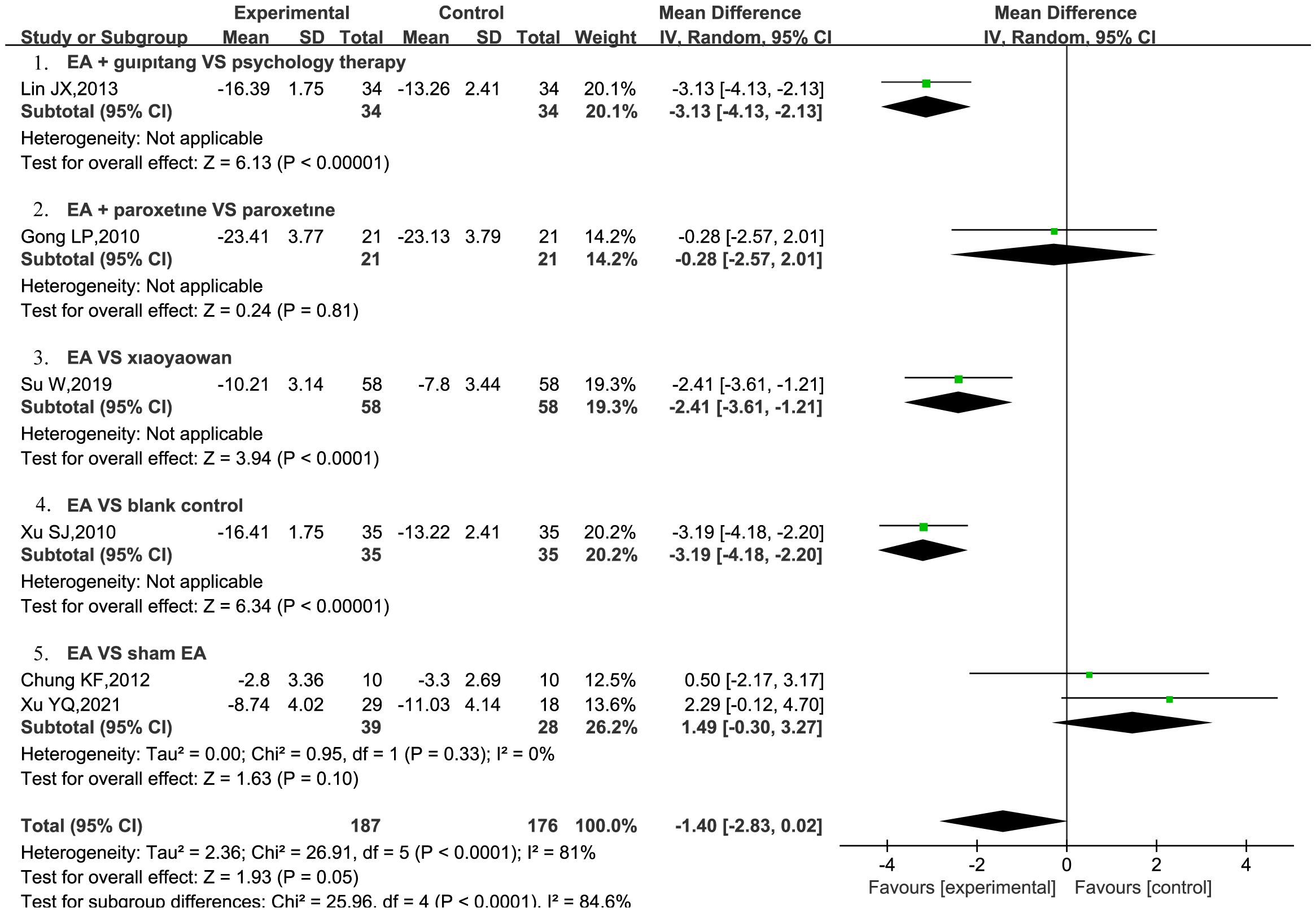
3.4.1 HAMD
A total of six RCTs (20, 21, 23, 26, 28, 29) were included to assess the impact of EA on HAMD scores in patients with PPD. Furthermore, two RCTs (28, 29) provided a comparison between EA and sham EA. The results of the meta-analysis showed that EA was not more effective than sham EA in reducing HAMD scores, showing low heterogeneity (MD = 1.49, 95% CI = [−0.30, 3.27], I2 = 0%). However, these results were not statistically significant (P = 0.1). However, a solitary study indicated that EA demonstrated greater efficacy compared to a blank control (MD = −3.19, 95%CI = [−4.18, −2.2], P < 0.00001) (26), and was also found to be more effective than Xiaoyaowan in reducing HAMD scores (MD = −2.41, 95%CI = [−3.61, −1.21], P < 0.0001) (23). Additionally, EA combined with Guipitang was found to be more effective than psychotherapy alone in reducing HAMD scores (MD = −3.13, 95% CI = [−4.13, −2.13], P<0.0001) (21) (Figure 3).
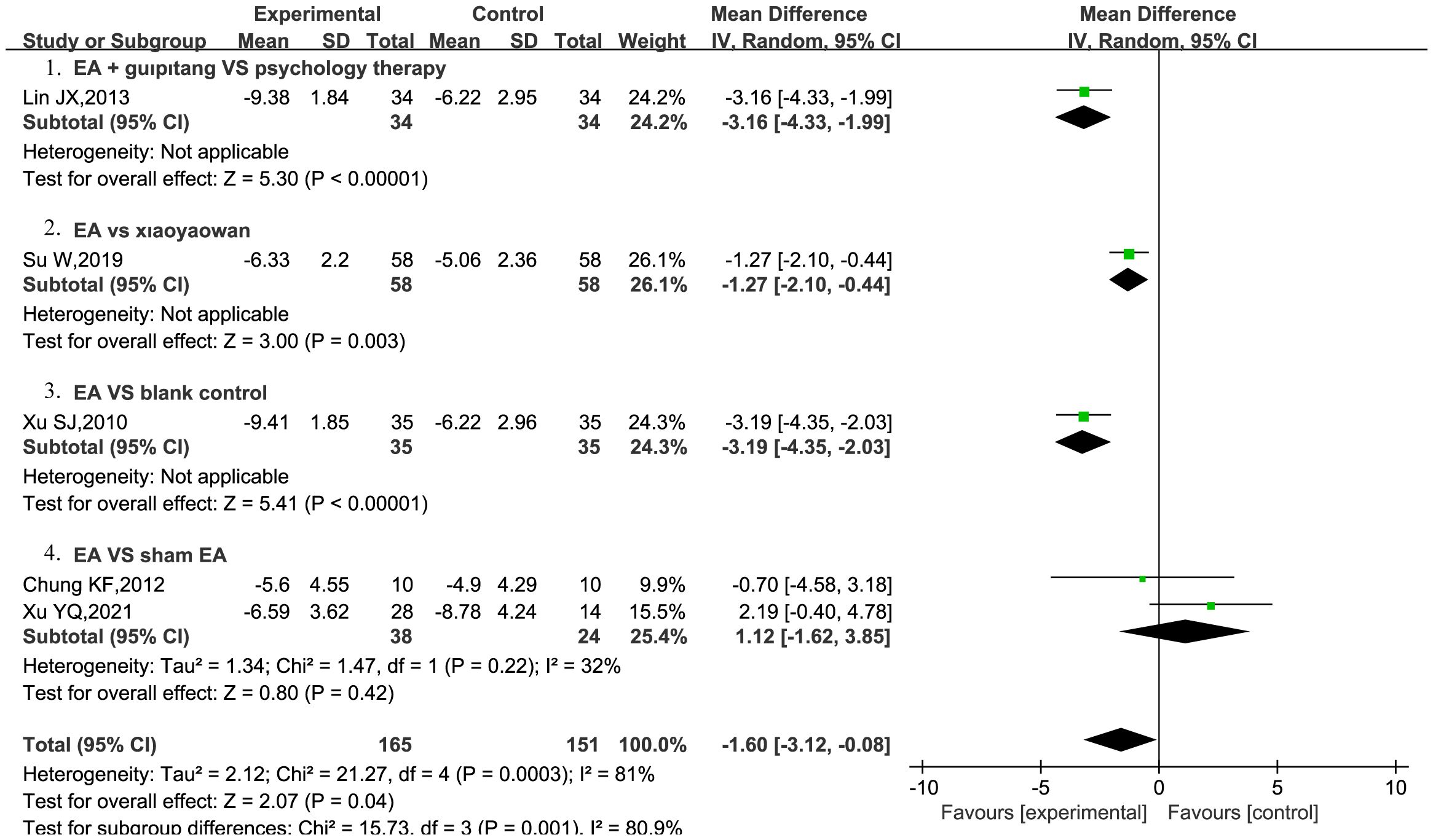
3.4.2 EPDS
Five RCTs (21, 23, 26, 28, 29) were included to assess the effect of EA on EPDS scores in patients with PPD. Among these, two RCTs (28, 29) compared EA with sham EA. The results indicated that EA did not demonstrate superiority over sham EA in reducing EPDS scores, showing low heterogeneity (MD = 1.12, 95% CI = [−1.62, 3.85], I2 = 32%), and the results were not statistically significant (P = 0.42). Only one study reported that EA outperformed the blank control in lowering EPDS scores (MD = −3.19, 95%CI = [−4.35, −2.03], P < 0.00001) (26). Moreover, EA was better than Xiaoyaowan in reducing EPDS scores (MD = −1.27, 95%CI = [−2.10, −0.44], P = 0.003) (23). Moreover, EA combined with Guipitang was found to be more effective than psychotherapy in reducing EPDS scores (MD = −3.16, 95% CI = [−4.33, −1.99], P<0.0001) (21) (Figure 4).
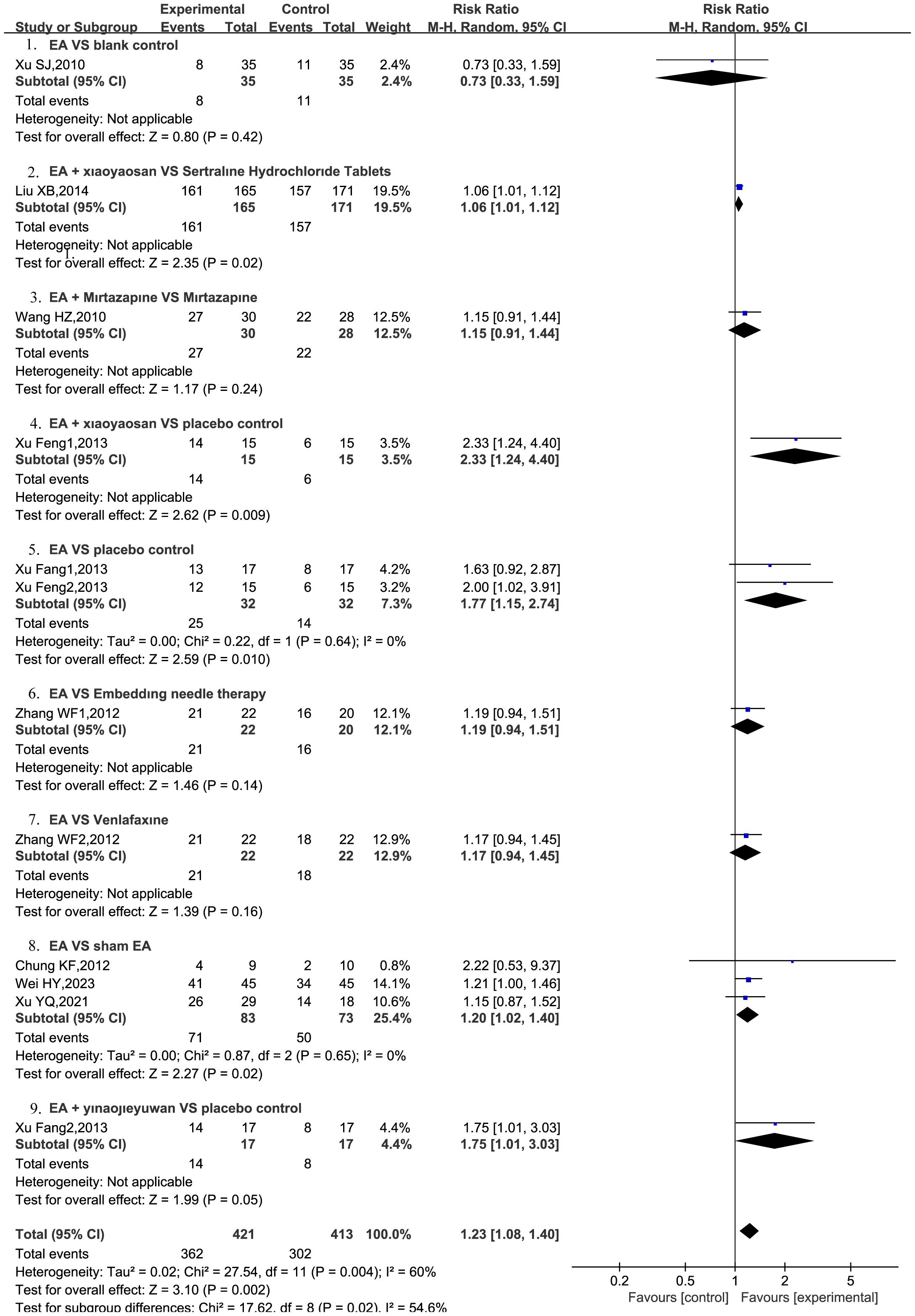
3.4.3 Total response rate
A total of nine RCTs (22, 24–31) were included, and the total response rate was reported, with three RCTs (25, 27, 31) divided into two groups. The meta-analysis revealed total response rate of the EA intervention was significantly higher compared to other therapies, with statistically significant results (RR = 1.23, 95%CI = [1.08, 1.40], P = 0.002) and moderate heterogeneity (I2 = 60%). Subsequent sensitivity analysis revealed that after excluding the study by Liu (22), the heterogeneity across the remaining studies decreased (I2 = 22%), indicating a robust model.
The comparison between EA and placebo control was reported in two RCTs (25, 31), whereas the comparison between EA and sham EA was reported in three RCTs (28–30). Furthermore, only one RCT each reported on EA + Xiaoyaosan vs. sertraline hydrochloride tablets (22), EA + mirtazapine vs. mirtazapine alone (24), EA + Xiaoyaosan vs. placebo control (25), EA vs. embedding needle therapy (27), EA vs. venlafaxine (27), EA + Yinaojieyufang vs. placebo control (31), and EA vs. blank control (26). The meta-analysis indicated that EA combined with Xiaoyaosan demonstrated superiority over sertraline hydrochloride tablets (RR = 1.06, 95%CI = [1.01, 1.12], P = 0.02) (22), Additionally, EA combined with Xiaoyaosan was found to be more effective than placebo control (RR = 2.33, 95% CI = [1.24, 4.40], P = 0.009) (25). EA + Yinaojieyufang was also found to be significantly more effective than placebo control (RR = 1.75, 95% CI = [1.01, 3.30], P = 0.05) (31). EA was found to be significantly more effective than placebo control (RR = 1.77, 95% CI = [1.15, 2.74], P = 0.01, I2 = 0%) (25, 31) as well as sham EA (RR = 1.2, 95% CI = [1.02, 1.40], P = 0.02, I2 = 0%) (28–30), with the results indicating statistical significance and low heterogeneity, as shown in Figure 5.
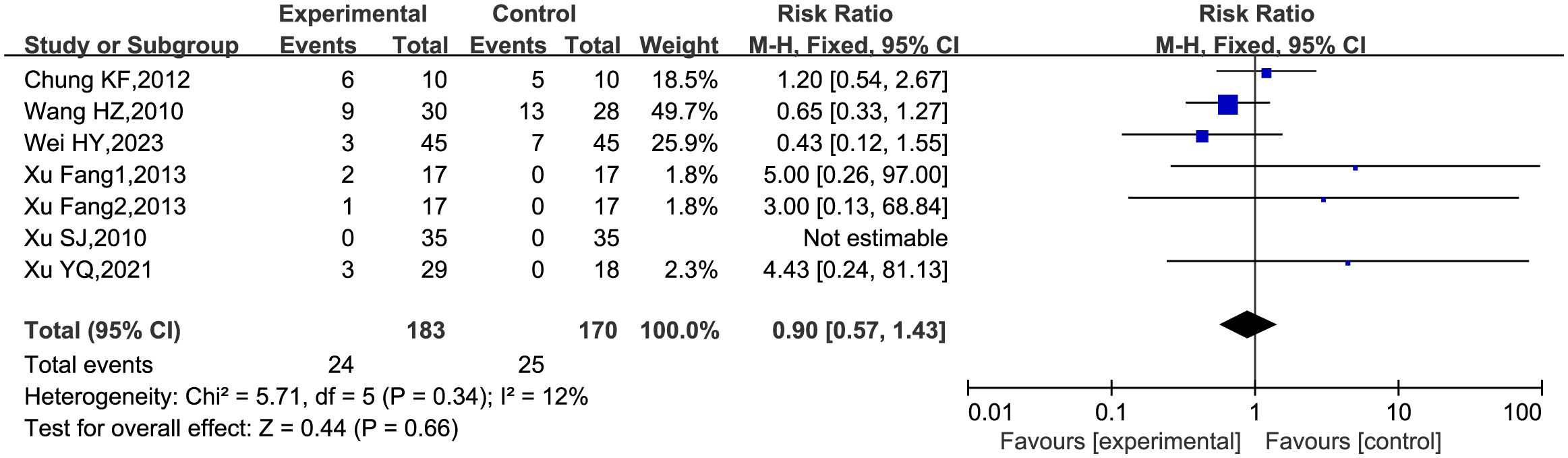
3.4.4 Adverse events
Six RCTs (24, 26, 28–31) included in the analysis reported AEs, with one RCT being divided into two groups (31). The meta-analysis indicated a low incidence of AEs associated with EA (RR = 0.9, 95%CI = [0.57, 1.43], P = 0.66, I2 = 12%), with low heterogeneity among the studies. The primary adverse reactions associated with EA were pain and bruising at the site of needle insertion, as shown in Figure 6.
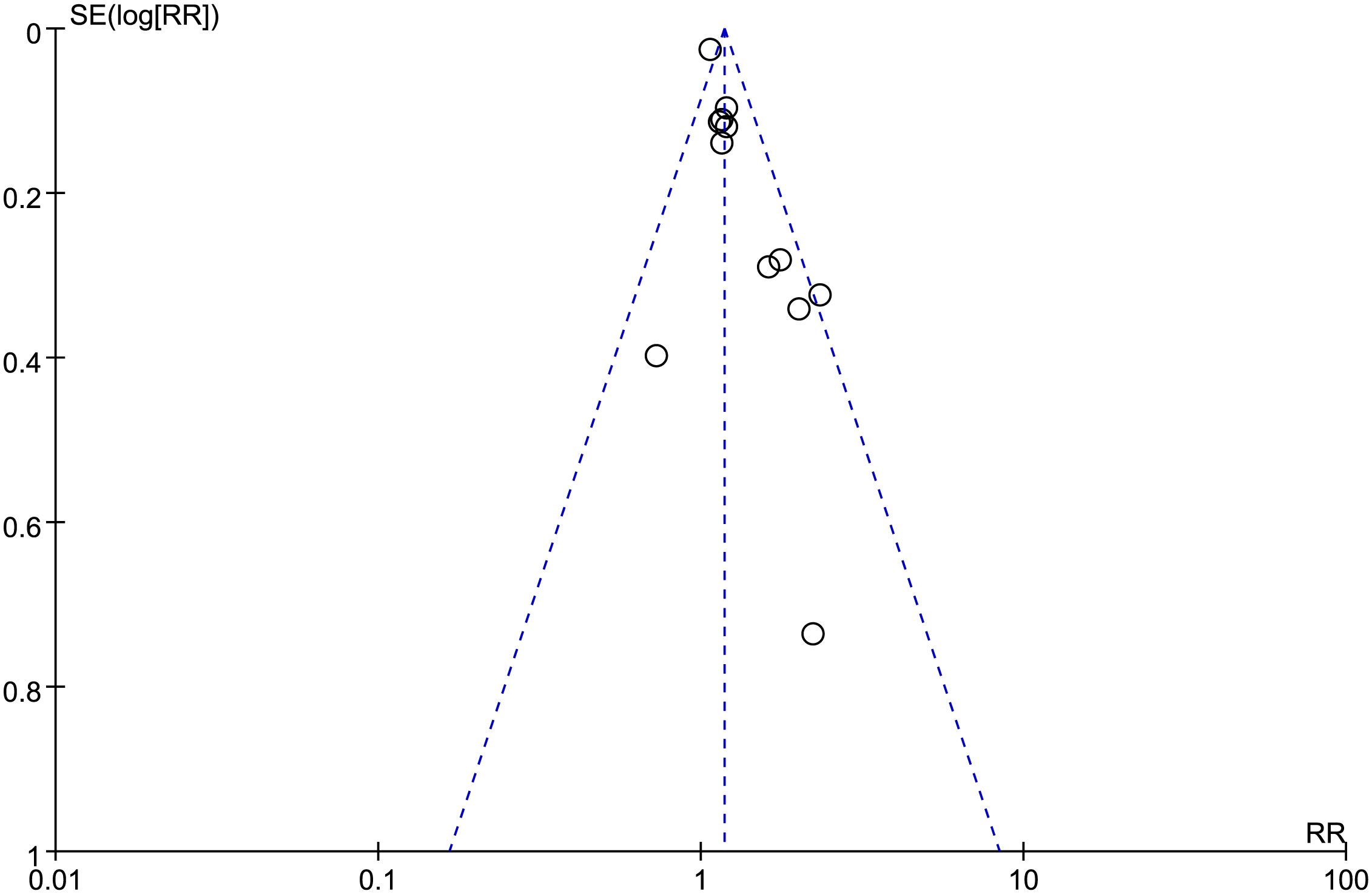
3.5 Detection of publication bias
In this study, the researchers assessed publication bias by examining indicators that involved more than 10 studies. The Egger test, applied to the included literature assessing the total response rate of EA for PPD, suggested publication bias (P = 0.0011, < 0.05). Simultaneously, the funnel plot analysis also showed asymmetry, which also indicated the existence of publication bias in this study, as shown in Figure 7.
4 Discussion
Acupuncture plays a significant role in complementary and alternative medicine (35), and has been utilized for millennia to treat illnesses and restore the body’s equilibrium through the stimulation of acupoints (36). EA enhances the effect of acupuncture through electrical stimulation, has made significant advancements in treating depression. Research indicates that EA may achieve its therapeutic effects on depression by modulating brain network regulation (37). One study has demonstratedhat EA could potentially modulate depression by up-regulating theexpression of basic fibroblast growth factor, thereby influencing astrocyte proliferation (38). The mechanism of EA treatment for PPD may involve regulating hormone secretion in the hypothalamic-pituitary-gonadal axis and plasma estradiol levels (39). The mechanism of action may also involve improving the distribution of intestinal flora in PPD patients (40, 41).
Previous meta-analyses (42, 43) have shown the potential benefits of acupuncture, including manual acupuncture, moxibustion and other techniques for PPD (44–46), but did not specifically discuss the efficacy and safety of EA in PPD treatment. Therefore, this meta-analysis aims to further explore the efficacy and safety of EA in treating PPD.
The results of this study indicate that the EA group showed significantly higher overall response rates in comparison to both the placebo group and the sham EA group. These results suggest that EA may possess superior clinical efficacy to a certain degree. However, there was no discernible advantage of EA over sham EA in reducing HAMD and EPDS scores among patients with PPD. While the evidence remains inconclusive, EA has exhibited promise in the treatment of PPD. For instance, in comparison to the blank control group (26) and TCM Xiaoyaowan (23), EA showed better efficacy in reducing HAMD and EPDS scores. Another independent study (21) highlighted the advantages of integrating EA with TCM Guipitang, compared to psychotherapy, in decreasing HAMD and EPDS scores in PPD patients. Although the findings of our meta-analysis suggest that EA did not lead to a significant reduction in depression scores, it did show a higher overall response rate compared to both placebo and sham EA groups. Furthermore, our investigation demonstrated a minimal occurrence of AEs linked to EA; hence, EA remains a safe and effective treatment for postpartum depression.
Nevertheless, it is crucial to acknowledge a few limitations in this meta-analysis. Firstly, it is important to note that certain study results exhibited high heterogeneity and are subject to publication bias. Additionally, the competitive nature of academic research may result in the unavoidable exclusion of negative research results. Another limitation is that all studies were carried out in a single country, namely China. Furthermore, the limited number of included studies and their relatively small sample sizes further affected the accuracy of our meta-analysis. Ultimately, the majority of studies failed to provide details on allocation concealment and blinding techniques. This lack of rigorous methodological transparency can introduce bias into the study results and weaken the validity of the conclusions. Addressing these methodological shortcomings in future research is essential to improve the quality and reliability of RCTs in this field.
In summary, the existing evidence indicates that EA shows promise in effectively and safely treating PPD. The above conclusions should be validated through additional high-quality studies, given the limitations pertaining to the quantity and quality of the studies included in this meta-analysis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
XF: Writing – original draft, Writing – review & editing. XW: Writing – review & editing, Conceptualization. WZ: Data curation, Software, Writing – review & editing. JH: Funding acquisition, Writing – review & editing. XG: Writing – review & editing, Formal analysis, Visualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Taishan Scholar Project of Shandong Province (No. tsqn202312376). Natural Science Foundation of Shandong Province (No.2015ZRB14325).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1393531/full#supplementary-material
References
1. Zeng M, Gong A, Wu Z. Paroxetine combined with traditional chinese medicine prescriptions in the treatment of postpartum depression: A systematic review of randomized controlled trials. Front Neuroendocrinol. (2022) 67:101019. doi: 10.1016/j.yfrne.2022.101019
2. Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. (2021) 11:543. doi: 10.1038/s41398-021-01663-6
3. Sriraman NK, Melvin K, Meltzer-Brody S. ABM clinical protocol #18: use of antidepressants in breastfeeding mothers. Breastfeed Med. (2015) 10:290–9. doi: 10.1089/bfm.2015.29002
4. Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. (2010) 33:1–6. doi: 10.1016/j.infbeh.2009.10.005
5. Hoffman C, Dunn DM, Njoroge WFM. Impact of postpartum mental illness upon infant development. Curr Psychiatry Rep. (2017) 19:100. doi: 10.1007/s11920-017-0857-8
6. Wu Q. The degree of fluctuations in maternal depressive symptoms in early childhood is associated with children’s depression risk: initial evidence and replication between two independent samples. Res Child Adolesc Psychopathol. (2023) 52(5):727–41. doi: 10.1007/s10802-023-01159-5
7. Hantsoo L, Ward-O’Brien D, Czarkowski KA, Gueorguieva R, Price LH, Epperson CN. A randomized, placebo-controlled, double-blind trial of sertraline for postpartum depression. Psychopharmacol (Berl). (2014) 231:939–48. doi: 10.1007/s00213-013-3316-1
8. Milgrom J, Gemmill AW, Ericksen J, Burrows G, Buist A, Reece J. Treatment of postnatal depression with cognitive behavioural therapy, sertraline and combination therapy: a randomised controlled trial. Aust N Z J Psychiatry. (2015) 49:236–45. doi: 10.1177/0004867414565474
9. Wisner KL, Perel JM, Peindl KS, Hanusa BH, Piontek CM, Findling RL. Prevention of postpartum depression: a pilot randomized clinical trial. Am J Psychiatry. (2004) 161:1290–2. doi: 10.1176/appi.ajp.161.7.1290
10. Cuomo A, Maina G, Neal SM, De Montis G, Rosso G, Scheggi S, et al. Using sertraline in postpartum and breastfeeding: balancing risks and benefits. Expert Opin Drug Saf. (2018) 17:719–25. doi: 10.1080/14740338.2018.1491546
11. Li X, Laplante DP, Paquin V, Lafortune S, Elgbeili G, King S. Effectiveness of cognitive behavioral therapy for perinatal maternal depression, anxiety and stress: A systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev. (2022) 92:102129. doi: 10.1016/j.cpr.2022.102129
12. Carson AJ, McWhirter L. Cognitive behavioral therapy: principles, science, and patient selection in neurology. Semin Neurol. (2022) 42:114–22. doi: 10.1055/s-0042-1750851
14. Chen B, Wang CC, Lee KH, Xia JC, Luo Z. Efficacy and safety of acupuncture for depression: A systematic review and meta-analysis. Res Nurs Health. (2023) 46:48–67. doi: 10.1002/nur.22284
15. Amorim D, Brito I, Caseiro A, Figueiredo JP, Pinto A, Macedo I, et al. Electroacupuncture and acupuncture in the treatment of anxiety - A double blinded randomized parallel clinical trial. Complement Ther Clin Pract. (2022) 46:101541. doi: 10.1016/j.ctcp.2022.101541
16. Lottering B, Lin YW. TRPV1 responses in the cerebellum lobules VI, VII, VIII using electroacupuncture treatment for chronic pain and depression comorbidity in a murine model. Int J Mol Sci. (2021) 22(9):5028. doi: 10.3390/ijms22095028
17. Lin SS, Zhou B, Chen BJ, Jiang RT, Li B, Illes P, et al. Electroacupuncture prevents astrocyte atrophy to alleviate depression. Cell Death Dis. (2023) 14:343. doi: 10.1038/s41419-023-05839-4
18. Battle DE. Diagnostic and statistical manual of mental disorders (DSM). Codas. (2013) 25:191–2. doi: 10.1590/s2317-17822013000200017
19. Zhang MY, Yang DS, Jin H, Wu WY, He YL. National field trial of the Chinese classification and diagnostic criteria of mental disorders: comprehensibility, acceptability and applicability. Chin Med J (Engl). (1994) 107:124–8.
20. Gong LP. Synergistic effect of electroacupuncture on postpartum depression. Med J Chin People’s Health. (2010) 22:3045. Available at: https://kns.cnki.net/kcms2/article/abstract?v=XEQRgWHfXDGofLRd_Vit-giwbvlPkMS-luPSpeh6Skso8J5kFxreE_wtoligdkfTtkHvTv4L9mRzXYiQ4-_2-IODyMPZP3UvH20hF8XhQG3GeXIWB4KWDolgrPKCGqg-Qgj1WwR6venbmxDRieiocA==&uniplatform=NZKPT&language=CHS.
21. Lin JX. Heart and spleen deficiency type with acupuncture and chinese herbal medicine plus psychology therapy. Guangzhou, China: Guangzhou University of TCM. (2013).
22. Liu XB. Modified Xiaoyao Powder combined with electroacupuncture in the treatment of 165 cases of postpartum depression. J Community Med. (2014) 12:32–3. Available at: https://kns.cnki.net/kcms2/article/abstract?v=XEQRgWHfXDH6rlkUCI0q9HwQ1MKYdauPI5OF8HeDJav01c69ZiyUGZ0nxhMdZbAveWhqfuFxmwyuTeI4QcqIknlPwLxS1gMfL85TLiaFQsF3x0yfd_J11Zz6SOlcbwAdQqNrU5schlxy6xODa2WYVA==&uniplatform=NZKPT&language=CHS.
23. Su W, Liu SC, Hai Y, Mei WJ, Shi Y. Analysis of the therapeutic effect of acupuncture with the method of “Regulating Conception Vessel and Unblocking Governor Vessel” on patients with mild to moderate postpartum depression. Lishizhen Medcine Materia Med Res. (2019) 30:2932–4. Available at: https://kns.cnki.net/kcms2/article/abstract?v=XEQRgWHfXDGDzaY1CMq0OCPCm2-_eufhM606fCe-HAydVe7A2VVmfe61dcVLUgpU5IffjSL_KakcviKYqcPewx0-oMoXwxSRVCBdiLUoquZyyNkCiFy_ehO0kkWTvMqkV-BIXQIv5BP8AExVpynv2Ioj_2scMyTQ&uniplatform=NZKPT&language=CHS.
24. Wang HZ, Cheng SZ, Wang HR. 30 cases of postpartum depression treated by electroacupuncture combined with mirtazapine. Shaanxi J Traditional Chin Med. (2010) 31:728–9. Available at: https://kns.cnki.net/kcms2/article/abstract?v=XEQRgWHfXDGNdkp-39s7QLqNAkkydEB8ooXy6M21r5bHErtBBAKxuAh58CGm5cCBb5m6jhJn27etceiva8G63G7BCcfxdxvA6V9hRRxd7rg5hRWFApkKSlQiebS2btvsR0lKFYom1ad_ZBBpE2iXzQ==&uniplatform=NZKPT&language=CHS.
25. Xu F. Clinical research of postpartum depression treated with xiaoyaosan, acupuncture and moxibustion. World J Integrated Traditional Western Med. (2013) 8:896–9. doi: 10.13935/j.cnki.sjzx.2013.09.022
26. Xu SJ. Clinical observation on acupuncture in treating postpartum depression. Guangzhou, China: Guangzhou University of TCM (2010).
27. Zhang WF, Sun M, Lu DM, Yuan XH, Yu YR, Li SJ. 43 cases of postpartum depression treated by electroacupuncture at auricular points. Chin J Acupuncture Moxibustion. (2012) 32:1075–6. doi: 10.13703/j.0255-2930.2012.12.008
28. Chung KF, Yeung WF, Zhang ZJ, Yung KP, Man SC, Lee CP, et al. Randomized non-invasive sham-controlled pilot trial of electroacupuncture for postpartum depression. J Affect Disord. (2012) 142:115–21. doi: 10.1016/j.jad.2012.04.008
29. Xu YQ. Clinical efficacy evaluation study of Electro-acupuncture Combined with Psychotherapy on Mild and Moderate Postpartum Depression. Beijing, China: China Academy of Chinese Medical Sciences (2021). doi: 10.27658/d.cnki.gzzyy.2021.000115
30. Wei HY, Wang J, Qiu XL, Wang SA. Clinical effect of applying electro-acupuncture combined with CBT in the treatment of mild to moderate postpartum depression and its influence on serum sex hormones. J Sichuan Traditional Chin Med. (2022) 40:202–5. Available at: https://kns.cnki.net/kcms2/article/abstract?v=jkwd3qsBIELooUHbTRJFgQOj0itqn1K_4H3SaB-3OsC8N6DaZb75aab1jJU8wAtbZtnXk7e-cKqG7WmQ9EIqks9b24q21nKEKQ3P2XYvtebgKa03tMg-ojqJ3L-fWHKnGWpCJkHjy5M=&uniplatform=NZKPT&language=CHS.
31. Xu F, Tang QS, Li XL. Replenishing kidney and regulating qi therapy for postpartum depression: a randomized controlled trial. Beijing J Traditional Chin Med. (2013) 32:200–3. doi: 10.16025/j.1674-1307.2013.03.009
32. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. (2019) 366:l4898. doi: 10.1136/bmj.l4898
33. Chen B, Benedetti A. Quantifying heterogeneity in individual participant data meta-analysis with binary outcomes. Syst Rev. (2017) 6:243. doi: 10.1186/s13643-017-0630-4
34. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
35. Zhang A, Li J, He T, Xie H, Mou X, Yeung TC, et al. Efficacy and safety of acupuncture in treating low back and pelvic girdle pain during pregnancy: A systematic review and meta-analysis of randomized controlled trials. Acupuncture Herbal Med. (2024), 9900. doi: 10.1097/HM9.0000000000000093
36. Wu Q, Liu S, Zhang R, Tang Q, Dong L, Li S, et al. ACU&MOX-DATA: a platform for fusion analysis and visual display acupuncture multi-omics heterogeneous data. Acupuncture Herbal Med. (2023) 3:59–62. doi: 10.1097/HM9.0000000000000051
37. Han X, Gao Y, Yin X, Zhang Z, Lao L, Chen Q, et al. The mechanism of electroacupuncture for depression on basic research: a systematic review. Chin Med. (2021) 16:10. doi: 10.1186/s13020-020-00421-y
38. Yao Z, Zhang Z, Zhang J, Cai X, Zhong Z, Huang Y, et al. Electroacupuncture alleviated the depression-like behavior by regulating FGF2 and astrocytes in the hippocampus of rats with chronic unpredictable mild stress. Brain Res Bull. (2021) 169:43–50. doi: 10.1016/j.brainresbull.2021.01.005
39. Liu SC, Pei Y, Tang C, Gao YT, Hai Y. Theoretical analysis on treatment of postpartum depression by acupuncture. Chin Arch Traditional Chin Med. (2019) 37:2621–4. doi: 10.13193/j.issn.1673-7717.2019.11.013
40. Liu JY, Liu XQ, Sun RH, Jin SF. Explore the therapeutic effect of acupuncture on postpartum depression and its influence on intestinal flora based on brain-gut axis theory. Jilin Med J. (2022) 43:2524–7. Available at: https://kns.cnki.net/kcms2/article/abstract?v=jkwd3qsBIEJ81neNQJwrJ68URB6pDeyg4V8HF2hSmhVF1Tohyn-0gRSgp0EqYVcVJktlE_1fZlBNIx4387V56_0aX3WjgfgDH0sDWKVsp4o5FF0qs6BMVgqW4ce_BrKfI9K4u1KZGVs=&uniplatform=NZKPT&language=CHS.
41. Liu L, Wang H, Chen X, Zhang Y, Zhang H, Xie P. Gut microbiota and its metabolites in depression: from pathogenesis to treatment. EBioMedicine. (2023) 90:104527. doi: 10.1016/j.ebiom.2023.104527
42. Tong P, Dong LP, Yang Y, Shi YH, Sun T, Bo P. Traditional Chinese acupuncture and postpartum depression: A systematic review and meta-analysis. J Chin Med Assoc. (2019) 82:719–26. doi: 10.1097/JCMA.0000000000000140
43. Fan B, Zhao Y, Chai J, Bing B, Wang W. Effectiveness of acupuncture in postpartum depression: A protocol for an overview of systematic reviews. Med (Baltimore). (2022) 101:e28678. doi: 10.1097/MD.0000000000028678
44. Hu X, Fan Q, Ma L, Jin R, Gong R, Zhao X, et al. Reliability of evidence to guide decision-making in the use of acupuncture for postpartum depression. Front Public Health. (2022) 10:942595. doi: 10.3389/fpubh.2022.942595
45. Li S, Zhong W, Peng W, Jiang G. Effectiveness of acupuncture in postpartum depression: a systematic review and meta-analysis. Acupunct Med. (2018) 36:295–301. doi: 10.1136/acupmed-2017-011530
Keywords: postpartum depression, electroacupuncture, HAMD, EPDS, meta-analysis
Citation: Fang X, Wang X, Zheng W, Han J and Ge X (2024) Efficacy and safety of electroacupuncture in patients with postpartum depression: a meta-analysis. Front. Psychiatry 15:1393531. doi: 10.3389/fpsyt.2024.1393531
Received: 29 February 2024; Accepted: 24 June 2024;
Published: 11 July 2024.
Edited by:
Stefano Turi, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Ahmad Neyazi, Afghanistan Center for Epidemiological Studies, AfghanistanAtefeh Zandifar, Alborz University of Medical Sciences, Iran
Anyang Rao, Diabetes Research ETS Foundation, Italy
Xiaoying Zhao, Tianjin University of Traditional Chinese Medicine, China
Copyright © 2024 Fang, Wang, Zheng, Han and Ge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaobin Ge, MTg1NjAwODAxNTZAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Xue Fang
Xue Fang Xiaoyan Wang
Xiaoyan Wang Wenjun Zheng
Wenjun Zheng Jing Han
Jing Han Xiaobin Ge
Xiaobin Ge