- 1Department of Clinical Child and Adolescent Psychology, Philipps University Marburg, Marburg, Germany
- 2German Center for Mental Health, Philipps University Marburg, Marburg, Germany
Introduction: Mental disorders are often stigmatized in society. The stigma of mental illness affects people with a mental illness themselves as well as their family members—a phenomenon called stigma by association (SBA). Children of parents with a mental illness (COPMI) are a particular vulnerable group for SBA. In our systematic review, experienced SBA, anticipated SBA, affiliate SBA, and structural discrimination were identified as relevant stigma dimensions for children of parents with a mental illness. To assess SBA in adolescents who grow up with a parent with a mental illness, the COPMI-SQ was developed.
Methods: N = 930 adolescents completed the study. Of those, N = 380 adolescents (sample 1; 72.6% female, mean age 17.12 (SD = 2.01) years) reported growing up with at least one parent with a mental illness. Using confirmatory (CFA) and exploratory factor analyses (EFA) as well as standard item and reliability analyses, we analyzed and revised the COPMI-SQ in the first sample. To validate the factorial structure of the revised COPMI-SQ, CFA was also conducted in the independent sample of the other N = 550 adolescents (sample 2; 80.0% female, mean age 16.36 (SD = 1.98) years) who reported not growing up with a parent with a mental illness. To test four measurement invariance, a multiple-group CFA was conducted in the combined sample of adolescents who reported growing up with and without a parent with a mental illness (sample 1 and sample 2).
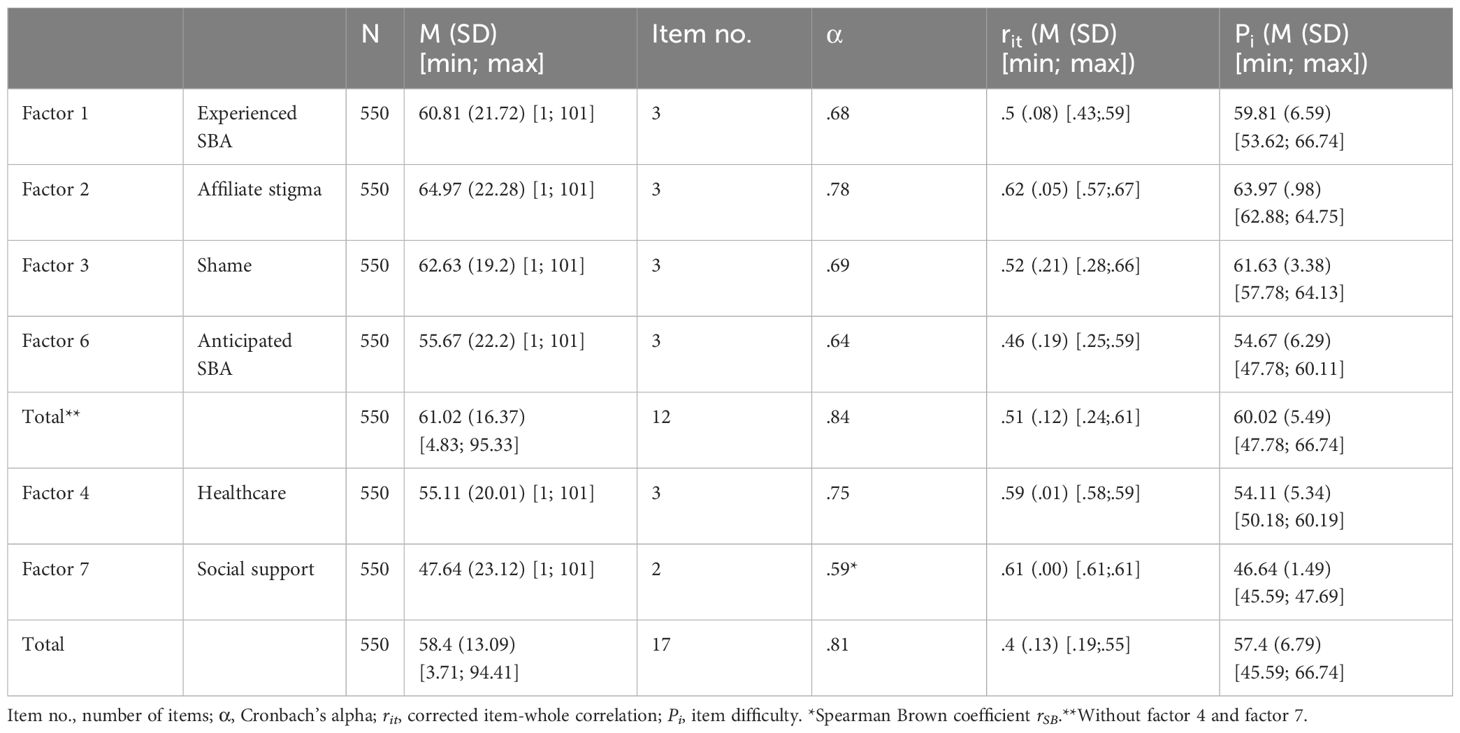
Results: CFA in sample 1 resulted in an inadequate model fit for the theoretically assumed four-factor structure (CFI = .687; RMSEA = .064 (90% CI = .062–.066); SRMR = .092; AIC = 229 155.63). Following EFA and item and reliability analyses in sample 1, the COPMI-SQ was reduced to four scales (“Experienced SBA,” “Affiliate SBA,” “Shame,” and “Anticipated SBA”) and two additional screening scales (“Healthcare” and “Social support”). To facilitate questionnaire use, only the three best items were retained in each scale, reducing the total item number to 12 plus five additional screener items. CFA in sample 2 also resulted in an inadequate model fit for the theoretically assumed four factor structure (CFI = .667; RMSEA = .065 (90% CI = .063–.066); SRMR = .101; AIC = 335 651.99). In comparison, the final version of the COPMI-SQ-r showed the best model fit (CFI = .945; RMSEA = .062 (90% CI = .052–.072); SRMR = .049; AIC = 60 008.05). In the multiple-group CFA (sample 1 and sample 2), metric invariance was established (χ2 (208) = 481.58, p < .001; CFI = .939; RMSEA = .053 (90% CI = .047-.059); SRMR = .056). In sample 2, internal consistency was found to be good for the total scale (α = .84) and almost acceptable to almost good for the subscales (α = .64 to.78).
Discussion: The revised version of the COPMI-SQ (COPMI-SQ-r) is a reliable and economic questionnaire to assess SBA in adolescents who grow up with a parent with a mental illness. The COPMI-SQ-r can be used to help develop and evaluate anti-stigma and general interventions for affected adolescents.
1 Introduction
Since mental disorders are still frequently stigmatized in society, the World Health Organization (WHO) calls in its “Comprehensive Mental Health Action Plan 2013–2030” for targeted actions to lower the stigmatization of people with mental disorders (1). The term stigma (Greek for stab, burn, or wound mark) goes back to the ancient Greeks, who cut or burned marks into the skin of criminals or slaves to identify them as corrupt or immoral people to be avoided (2). Today, stigmatization is understood as a process in which individuals are assigned to a group based on a characteristic or trait that is consensually categorized by society as deviating from the norm and therefore devaluated (3, 4). Stigmata are not inherent in the individuals themselves but are social constructs and depend on historically shaped cultural norms (4). The process of stigmatization consists of cognitive (stereotypes), emotional (prejudices), and behavioral (discrimination) components (5, 6). Stereotypes are simplified and generalized knowledge structures about social groups. The approval of the existing stereotype in association with negative emotions creates a prejudice, which, in turn, can result in a behavioral reaction in the form of discrimination (5, 6). Taken together, stereotypes and prejudices in the society are also referred to as public stigma (7). Negative stereotypes of people with mental disorders include stereotypical assumptions of character weakness, incompetence, dangerousness, or unpredictability (6, 8). The stigmatization of people with mental disorders is associated with serious and far-reaching consequences for those affected. Some authors argue that the consequences of stigma are actually worse than those of the mental disorder itself (9). Experiences of discrimination due to a mental disorder can lead to less help seeking (10), social isolation, hopelessness, and suicidal thoughts from internalizing the stigma (11). For those affected by stigmatization, three mechanisms are known to be most relevant (5): experienced stigma, anticipated stigma, and internalized stigma. Whereas experienced stigma refers to personally experienced stereotypes, prejudices, and discriminations in past or present, anticipated stigma represents the expectation of stigmatization in the future. Last but not least, internalized stigma, which is also called self-stigma (12), is defined as the internalization of stereotypes and prejudices to the self.
Regarding various discredited groups affected by stigmatization (e.g., people with AIDS, physical or mental illness), there is evidence that both the trait-bearing individuals themselves experience and expect stigmatization as well as people associated with them (13–16). This form of stigmatization, first referred to as courtesy stigma (2), is nowadays called stigma by association (SBA) (17). SBA depends on the entitativity, that is, the degree to which the trait-bearing individual and other associated people are perceived as a social unit. Since the highest degree of entitativity is attributed to families (17, 18), family members carry a higher risk of experiencing SBA. When SBA exists within families, it is also called family stigma (19). In terms of the stigmatization of people with mental disorders, this means that the whole family system experiences stigmatization due to the mental illness of one family member. Embarrassment, shame, guilt, and fear of contamination are reportedly frequent consequences of family stigma concerning mental illness (20–22).
Worldwide, every fourth child and adolescent grows up with at least one parent with a mental illness (23, 24). Children and adolescents who grow up with a parent with a mental illness are a particularly vulnerable group to develop a mental disorder themselves (25–28). A recent large meta-analysis reported a lifetime risk of 55% among those children and adolescents to develop any mental disorder (27), whereby subclinical symptoms occur more often and earlier in life (29). Due to their close and dependent relationship to their parents, these children and adolescents are also considered to be particularly affected by SBA (21, 30) and stigmatization has been identified as a potential social mechanism in the transgenerational transmission of mental disorders (TTMD) (29).
Thus, to reduce the stigma of mental illness in general and SBA in children of parents with a mental illness specifically, we need to develop general anti-stigma campaigns and targeted interventions to reduce SBA in children and adolescents who grow up with a parent with a mental illness (1, 31). To make this possible, a better understanding of the specific stigma experiences of affected children and adolescents is necessary, as are valid questionnaires to assess this information. Analogous to the mechanisms concerning the stigmatization of people with mental disorders in general (5), our recent systematic mixed studies review identified experienced stigma, anticipated stigma, affiliate stigma, and structural discrimination as important stigma dimensions for children and adolescents who grow up with a parent with a mental illness (32). Affiliate stigma (33) can be understood as the SBA version of the aforementioned internalized stigma or self-stigma (5, 12, 32, 33). Structural discrimination refers to the societal and policy structures perpetuating stigmatization (34). Since—to our knowledge—no adequate scale measuring SBA in adolescents who grow up with a parent with a mental illness exists, we developed the Children of Parents With a Mental Illness-Stigma Questionnaire (COPMI-SQ) (30) based on the identified stigma dimensions that are specifically relevant for children and adolescents who grow up with a parent with a mental illness (32). In our first pilot study (N = 32), we observed the COPMI-SQ’s promising psychometric properties, but as our sample was too small, analysis of the factor structure of the COPMI-SQ was not possible.
Therefore, the present study aims to report on the factor structure of the COPMI-SQ and its validation in a larger sample. A valid instrument to measure SBA in adolescents who grow up with a parent with a mental illness will enable us to better understand their stigma experiences and can be used to help develop and evaluate anti-stigma and general interventions for affected adolescents.
2 Methods
2.1 Ethics
This study was approved by the Ethics Committee of the Department of Psychology at Philipps University Marburg. Prior to study participation, adolescents were given information about the study and gave their informed consent. If they were under the age of 18, information was also given to their legal guardians, and their informed consent was also obtained. Data were collected anonymously. As long as the questionnaire was not submitted to the online platform, participants could withdraw from answering the questionnaire at any time and without giving any reason. In case of distress due to study participation, participants could contact clinically trained study personnel at any time. None of the participants took advantage of this offer.
2.2 Participants
Eligible participants were all German-speaking adolescents between 12 and 21 years of age who reported growing up with at least one parent with a mental illness. No further inclusion or exclusion criteria were applied. Since recruiting children of parents with a mental illness has proven to be difficult (35, 36), adolescents who reported not growing up with a parent with a mental illness could also participate in this study and a parallel version of the COPMI-SQ that only differed on item stem was presented to them.
2.3 Procedure
Participants were recruited Germany-wide through an ongoing research project concerning children of parents with a mental illness (23, 37), university mailing lists, and social media advertising on Instagram and also by directly contacting (social) services for children and adolescents who grow up with a parent with a mental illness. Data were collected between January and March 2023 using the online platform SoSci Survey (38) (www.soscisurvey.de). The survey was programmed so that all items had to be answered as it was otherwise automatically terminated. At the beginning of the survey, participants completed sociodemographic questions (age, sex, socioeconomic status) as well as questions regarding their parents’ and their own mental health. Socioeconomic status was assessed using the four item Family Affluence Scale and accordingly rated as low, medium, or high (39). At the end of the survey, participants were offered to take part in a prize draw as compensation for study participation.
2.4 COPMI-SQ
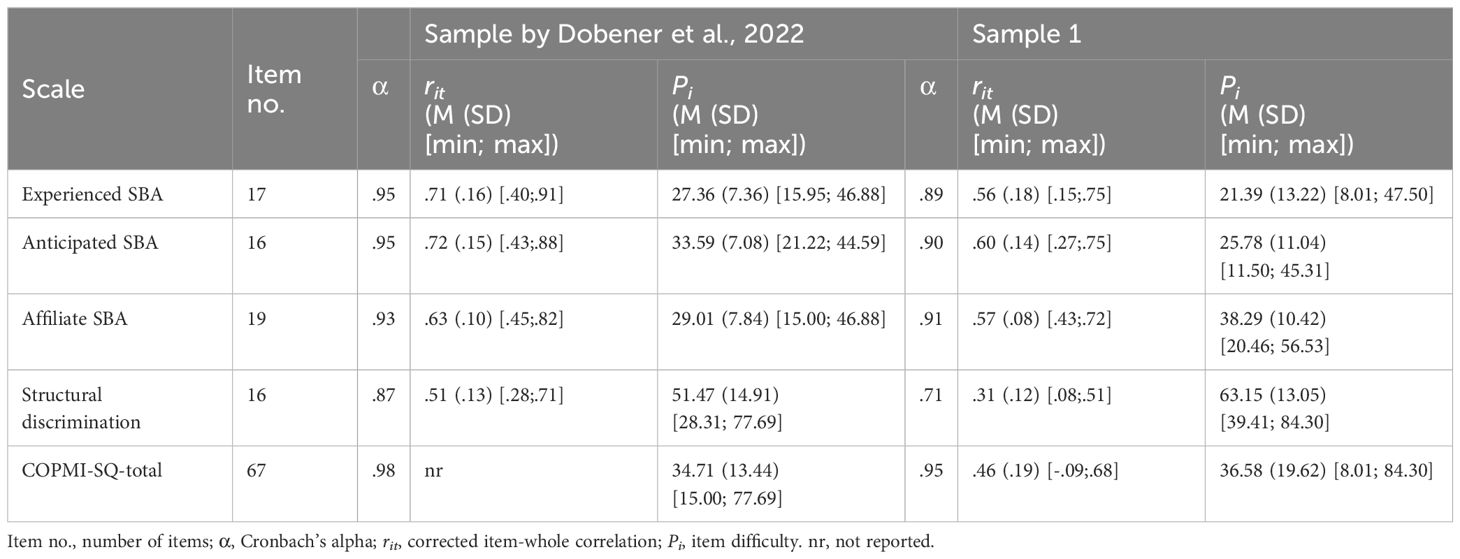
Based on a systematic review (32), the COPMI-SQ (30) was created as an instrument to assess the stigma experiences of adolescents who grow up with a parent with a mental illness in daily life. According to theory, the items were expected to load on the four different scales “Experienced SBA,” “Anticipated SBA,” “Affiliate SBA,” and “Structural Discrimination”. In a first pilot study with N = 32, the item number of the COPMI-SQ was reduced from initially 109 to 67. Items are rated from 1 (“does not apply at all”) to 101 (“fully applies”) on a 100-point visual Likert scale. Cronbach’s alpha for the subscales was good to excellent (α = .87 to.95), and excellent for the total scale (α = .98). Item difficulties ranged between Pi = 15.00 and Pi = 77.69. Corrected item-whole correlations for the subscales ranged between rit = .28 and rit = .91. For the total scale, no corrected item-whole correlations were reported. Further information is found in Table 1.
For adolescents who reported not growing up with a parent with a mental illness, a parallel version of the COPMI-SQ was created. All item stems were adapted without changing the meaning of the items: e.g., “Because my mother/my father has a mental illness, others make fun of my mother/my mother.” was reformulated to “Because the parent of a child has a mental illness, others make fun of the parent”.
2.5 Statistical analysis
Statistical analyses were conducted with RStudio (40) using the packages “psych” (41), “nFactors” (42), and “lavaan” (43). For all analyses, p-values ≤.05 were set as thresholds for statistical significance.
Since rules of thumb for confirmatory factor analyses (CFA) propose a ratio of number of items to number of participants (N) of 1 to 5 (44), a sample size of at least N = 335 was calculated in advance (67 items to 335 participants).
Initially, a CFA with robust maximum likelihood estimations was conducted in sample 1 to test the theoretically derived four-factor structure of the COPMI-SQ. Goodness of fit was assessed using the chi-square test statistics, the χ2/df ratio, the root mean square error of approximation (RMSEA), the standardized root mean squared residual (SRMR), the comparative fit index (CFI), and the Akaike information criterion (AIC) (45, 46). According to conventions, non-significant chi-square test statistics, RMSEA <.08, SRMR <.08, and CFI ≥.90 are regarded as good model fit (45). Concerning AIC, the model with the lowest value is regarded as the best model fit, as it is the most parsimonious one (46). This also applies to the χ2/df ratio, although values between 2 and 3 are also considered a good fit here (47).
Since an inadequate model fit was found for the theoretically derived four-factor structure, subsequent exploratory factor analyses (EFA) were conducted in sample 1 to further investigate the factor structure of the COPMI-SQ. Using Bartlett’s test (48) and Kaiser–Meyer–Olkin (KMO) criterion (49, 50), the suitability of the data for EFA was tested. EFA was conducted using maximum-likelihood factor analysis with promax rotation. Factor extraction was based on Velicer’s MAP test and Horn’s parallel analysis as well as content considerations (51). Step by step, all items with factor loadings <.3 or with factor cross loadings ≤.2 were removed and EFA repeated until a clear factorial structure was found. At all steps, Bartlett’s test and Kaiser–Meyer–Olkin criterion were used to test the suitability of the data for EFA, and factor extraction was based on MAP test, parallel analysis, and content considerations.
Subsequently, item analyses were performed in sample 1 based on item difficulties, item discriminatory power (corrected item-whole correlations), and Cronbach’s alpha if the item is deleted. Furthermore, Cronbach’s alpha was calculated as reliability coefficient of the scales and subscales. If scales consisted of fewer than three items, the Spearman–Brown coefficient rSB was used as reliability coefficient. Item and scale analyses were always first conducted for the subscales, then for the total scale. Cronbach’s alpha of ≥.7 was deemed acceptable, ≥.8 good, and ≥.9 excellent (52). The distribution of item difficulties was aimed to be 20 ≤ Pi ≤ 80 (53). Corrected item-whole correlations of.3 ≤ rit ≤.5 were regarded as acceptable and.5 < rit <.07 as good discriminatory power (53). All items with item difficulties Pi < 20 or Pi > 80 and with corrected item-whole correlations rit <.3 were removed.
Results of the EFA were subjected to CFA in sample 2 to confirm the derived factor structure. Furthermore, a multiple-group CFA was conducted in the combined sample of adolescents who reported growing up with and without a parent with a mental illness (sample 1 and sample 2) to test for measurement invariance. Finally, item analyses as described above were also performed in sample 2 for the derived factor structure.
3 Results
3.1 Participants
Our survey was accessed 6,649 times. Among the participants, 2,512 gave informed consent, 2,312 met the inclusion criteria (language, age), and 930 completed the survey. Of these, 380 also reported growing up with at least one parent with a mental illness and were included in sample 1. The remaining 550 adolescents who reported that their parents have no a mental illness were included in sample 2.
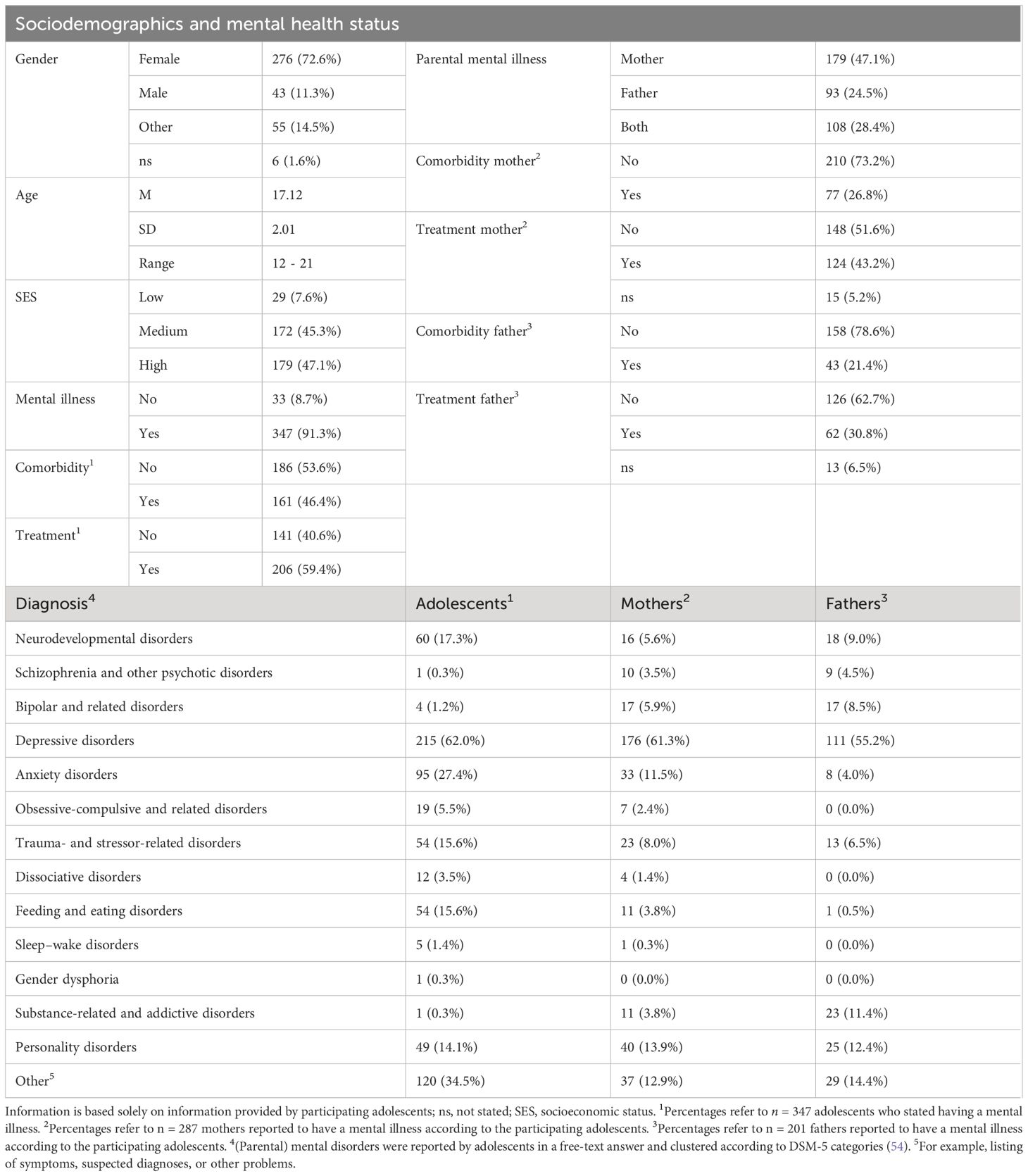
In sample 1, participating adolescents were mostly female (72.6%) and on average 17.12 years old (SD = 2.01). Almost all adolescents reported a medium (45.3%) to high (47.1%) socioeconomic status. 91.3% of the participating adolescents indicated having a mental illness themselves. Of those, almost half (46.4%) reported having more than one relevant diagnosis and 59.4% stated that they were undergoing treatment for their mental illness. Adolescents’ mental disorders were mostly classified as depressive disorders (62.0%), other symptoms (34.5%), and anxiety disorders (27.4%). Concerning the parental mental illness, almost half (47.1%) of the participating adolescents reported that only their mother and 24.5% that only their father was affected. 28.4% of the adolescents reported that both their parents were affected. Most common parental disorders were depressive disorders (61.3% for mothers, 55.2% for fathers), personality disorders (13.9% for mothers, 12.4% for fathers), and other symptoms (12.9% for mothers, 14.4% for fathers). More than one relevant diagnosis was reported for 26.8% of the mothers and for 21.4% of the fathers reported to have a mental illness. Furthermore, participating adolescents indicated that 43.2% of the mothers and 30.8% of the fathers reported to have a mental illness were being treated for their mental illness. More detailed sample characteristics for sample 1 are provided in Table 2.
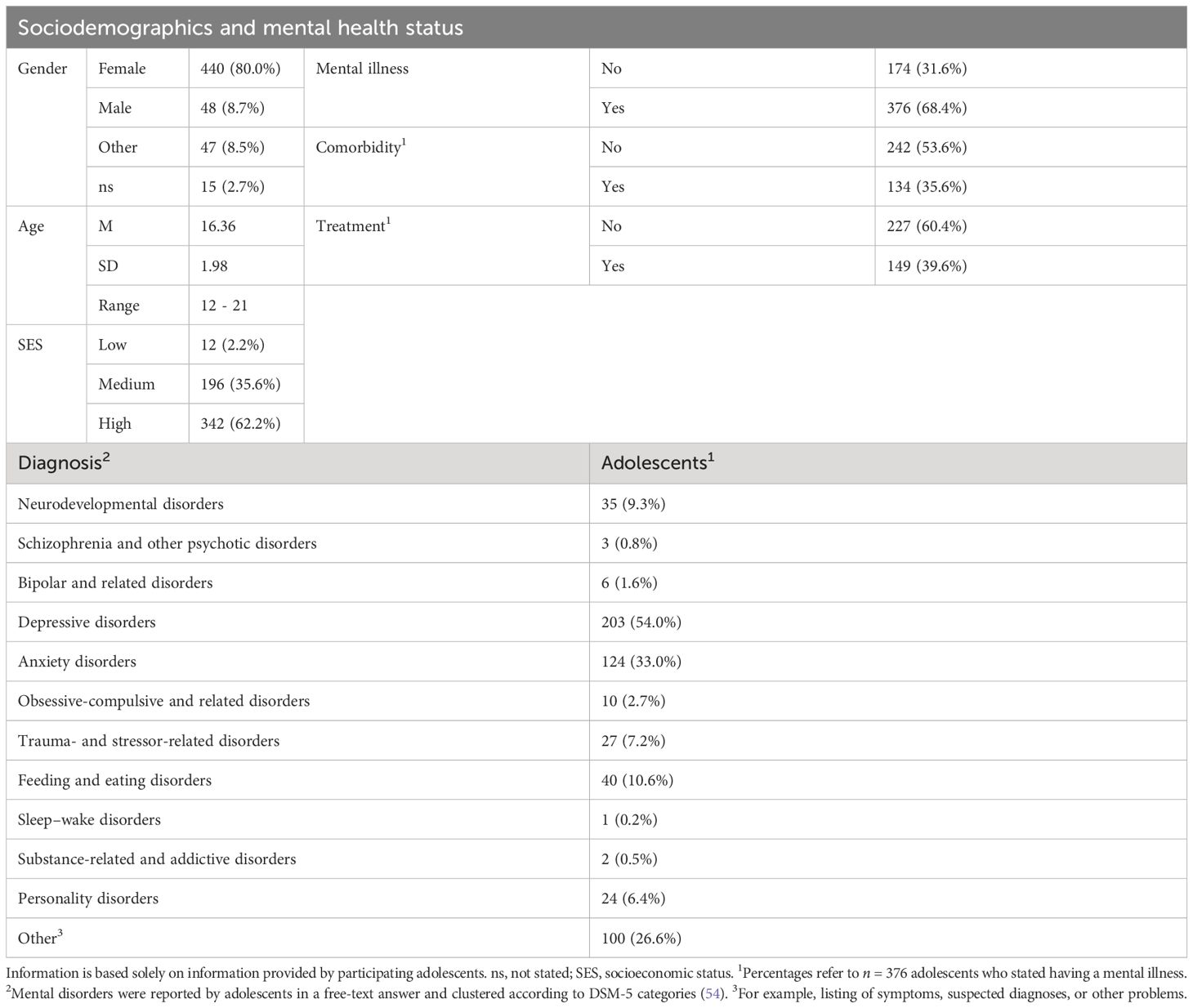
In sample 2, participating adolescents were mostly female (80.0%) and on average 16.36 years old (SD = 1.98). Almost all adolescents reported a medium (35.6%) to high (62.2%) socioeconomic status. 68.4% of the participating adolescents indicated having a mental illness themselves. Of those, 35.6% reported having more than one relevant diagnosis and 39.6% stated that they were undergoing treatment for the mental illness. Adolescents’ mental disorders were mostly classified as depressive disorders (54.0%), anxiety disorders (33.0%), and other symptoms (26.6%). More detailed sample characteristics for sample 2 are provided in Table 3.
3.2 Initial scale and item analyses (sample 1)
Initially, item and scale analyses were conducted for the theoretically derived four-factor structure in sample 1. Cronbach’s alpha was good to excellent (α >.89) for all subscales as well as the total scale (α = .95), except for the subscale “Structural Discrimination” (acceptable with α = .71). Item difficulties ranged between Pi = 8.01 and Pi = 84.30. Corrected item-whole correlations for the subscales ranged between rit = .08 and rit = .75, and for the total scale between rit = -.09 and rit = .68. Further information can be found in Table 1.
3.3 Confirmatory factor analysis of the original COPMI-SQ scales (sample 1)
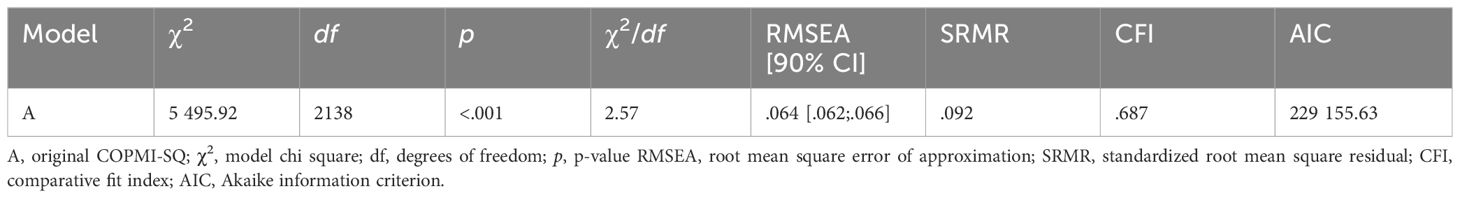
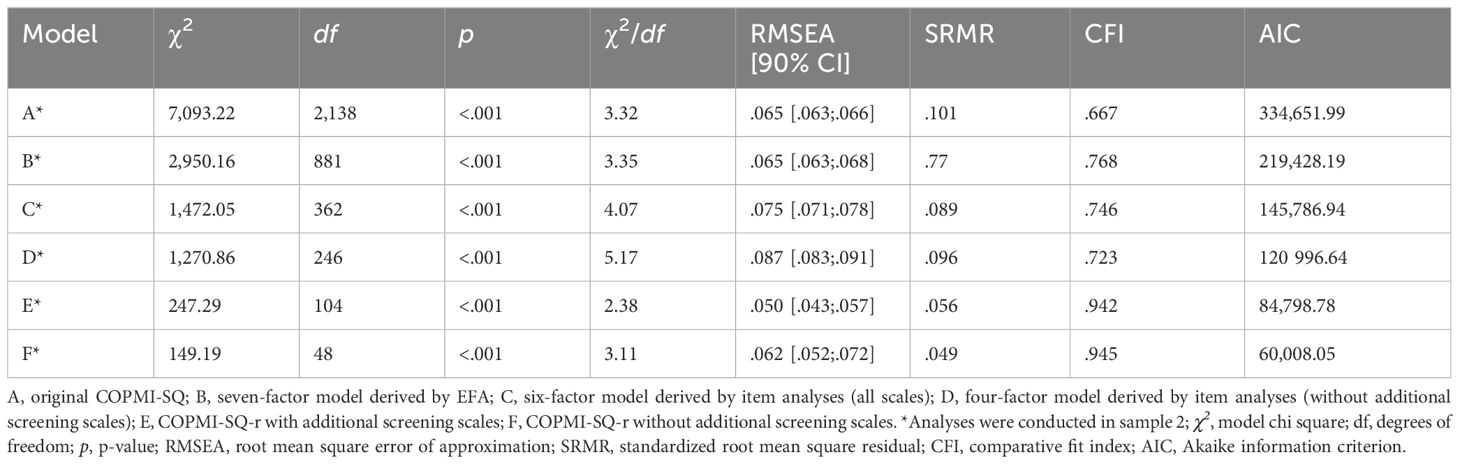
Testing the theoretically derived four-factor structure in sample 1 with a CFA resulted in an inadequate model fit (χ2(2138) = 5495.92, p <.001; RMSEA = .064 (90% CI = .062-.066); SRMR = .092; CFI = .687; AIC = 229 155.63) (see Table 4).
3.4 Exploratory factor analyses (sample 1)
Subsequent exploratory factor analyses were thus conducted in sample 1 to further analyze the factorial structure. According to Bartlett’s test (χ2(2211) = 14,038.49, p <.001) and Kaiser–Meyer–Olkin criterion (KMO = .92), the data were suitable for EFA. MAP test recommended the extraction of nine, parallel analysis the extraction of eight factors. Due to content considerations, eight factors accounting for 41% of the variance were initially extracted. Step by step, all items with factor loadings <.3 and with cross loadings with differences ≤.2 were deleted and EFA repeated five times. At all steps, Bartlett’s test and Kaiser–Meyer–Olkin criterion revealed the data’s suitability for EFA. For factor extraction, we considered the MAP test, parallel analysis, and content at all steps. Finally, EFA resulted in seven factors explaining 49% of the variance.
3.5 Item reduction 1 (sample 1)
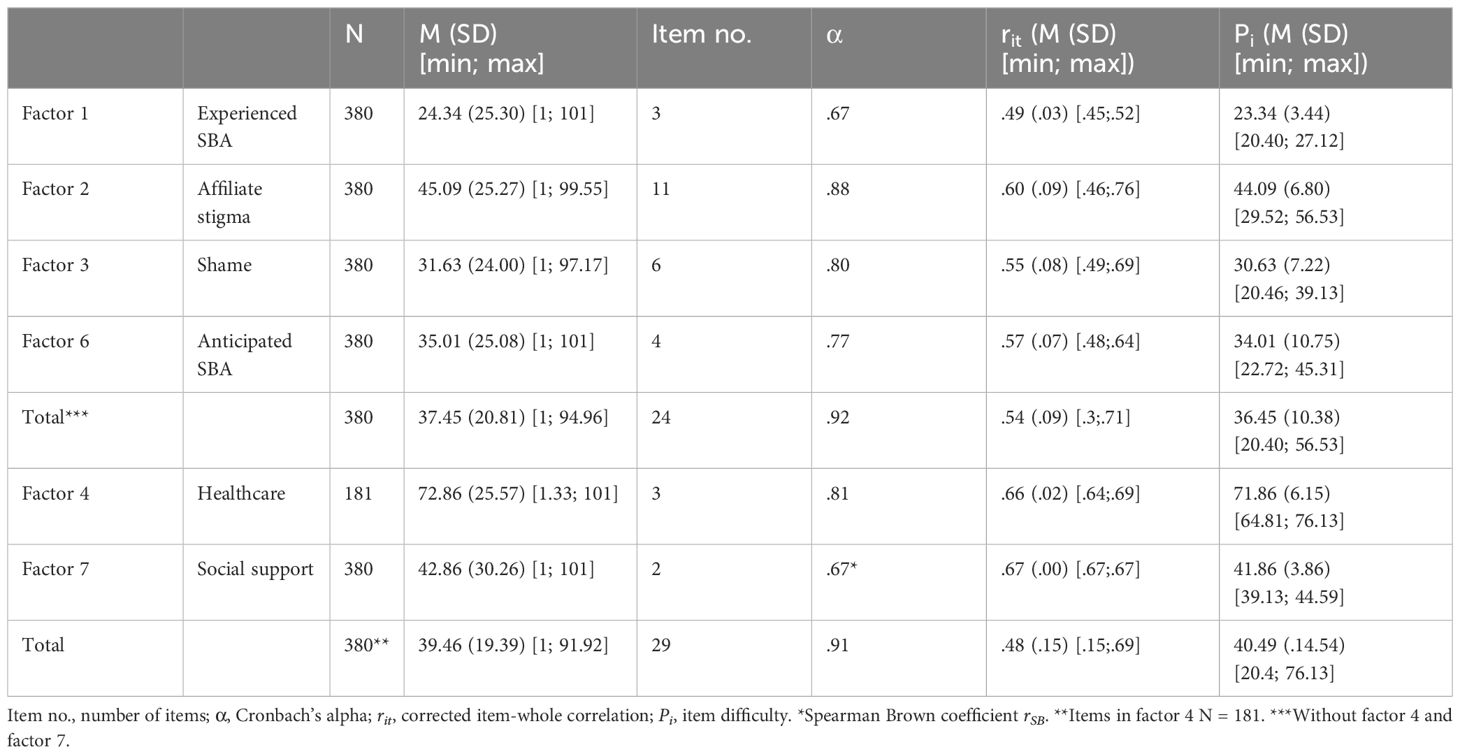
The subscales’ items derived from the EFA and the reduced total scale were named according to their content and then analyzed and revised in sample 1 concerning their difficulty, discriminatory power, and reliability. Detailed characteristics of the reduced scales are found in Table 5.
Factor 1: All but one of the initial items in the first factor were part of the original “Experienced SBA” scale. Thus, factor 1 was named “Experienced SBA”. Initial Cronbach’s alpha was α = .91. Removing any item would not have increased Cronbach’s alpha. All items showed desirable discriminatory power .5 < rit <.7. Nine items showed item difficulties of Pi < 20 and were thus removed. After removal, Cronbach’s alpha was almost acceptable (α = .67) for the remaining three items. The discriminatory power of the remaining three items was acceptable to desirable (.49 ≤ rit ≤.53) and item difficulties ranged from Pi = 20.40 to Pi = 27.12.
Factor 2: All items in the second factor were part of the original “Affiliate stigma” scale. Thus, factor 2 was named “Affiliate stigma”. Initial Cronbach’s alpha was α = .88. Removing any item would not have increased Cronbach’s alpha. All items showed desirable item difficulties 20 ≤ Pi ≤ 80. Two items showed almost desirable discriminatory power .46 ≤ rit ≤.5. All other items showed desirable discriminatory power rit >.50. Thus, no items were removed.
Factor 3: The items in the third factor were originally part of the scales “Anticipated SBA” and “Affiliate stigma”. All items dealt with aspects of keeping the parental mental disorder a secret or being ashamed by the parental mental disorder, thus, factor 3 was named “Shame”. Cronbach’s alpha was α = .80. Removing any item would not have increased Cronbach’s alpha. All items showed desirable item difficulties 20 ≤ Pi ≤ 80. One item showed almost desirable discriminatory power of rit = .49. All other items showed desirable discriminatory power rit >.50. Thus, no items were removed.
Factor 4: All items in the fourth factor were originally part of the healthcare subscale of the “Structural discrimination” scale. Thus, factor 4 was named “Healthcare”. Cronbach’s alpha was α = .74. Removing one item improved Cronbach’s alpha to α = .81. Afterward, all three remaining items showed desirable discriminatory power rit >.5 and desirable item difficulties 20 ≤ Pi ≤ 80. Thus, no further items were removed.
Factor 5: All items in the fifth factor were originally part of the “Anticipated SBA” scale. Thus, factor 5 was named “Anticipated SBA”. Initial Cronbach’s alpha was α = .87. Removing one item would have increased Cronbach’s alpha to α = .88. All items showed desirable discriminatory power rit >.5. Since all items showed inacceptable item difficulty Pi <.2, all items from factor 5 were removed.
Factor 6: All but one of the initial items in the sixth factor were part of the original “Anticipated SBA” scale. Thus, factor 6 was named “Anticipated SBA”. Initial Cronbach’s alpha was α = .71. Removing one item improved Cronbach’s alpha to α = .77. Afterwards, one item showed almost desirable discriminatory power of rit = .48. All other items showed desirable discriminatory power rit >.5. All four remaining items showed desirable item difficulties 20 ≤ Pi ≤ 80. Thus, no further items were removed.
Factor 7: The items in the seventh factor were part of the original “Experienced SBA” scale and dealt with having somebody to talk to in times of need. Thus, factor 7 was named “Social support”. Since factor 7 consists of only two items, Spearman’s brown coefficient (rSB) was calculated as reliability coefficient. Spearman’s brown coefficient was acceptable with rSB = .67. All items showed desirable discriminatory power (rit >.5) and item difficulty (20 ≤ Pi ≤ 80). Thus, no items were removed.
Total scale: Cronbach’s alpha was α = .91 for the total scale. Removing any item would not have improved Cronbach’s alpha. All items showed desirable item difficulties 20 ≤ Pi ≤ 80. Five items showed inacceptable discriminatory power rit <.3. Since all these items loaded on factor 4 (“Healthcare”) as well as factor 7 (“Social support”) those factors were excluded from calculating the total scale. Since stigma experiences in the healthcare system (factor 4) and social support (factor 7) were considered important aspects to assess, the subscales were nevertheless retained as separate screening scales. After excluding factors 4 and 7, Cronbach’s alpha was α = .92. Removing any further item would not have improved Cronbach’s alpha. All remaining items showed desirable item difficulties 20 ≤ Pi ≤ 80 and acceptable to desirable discriminatory power rit >.3.
3.6 Item reduction 2 (sample 1)
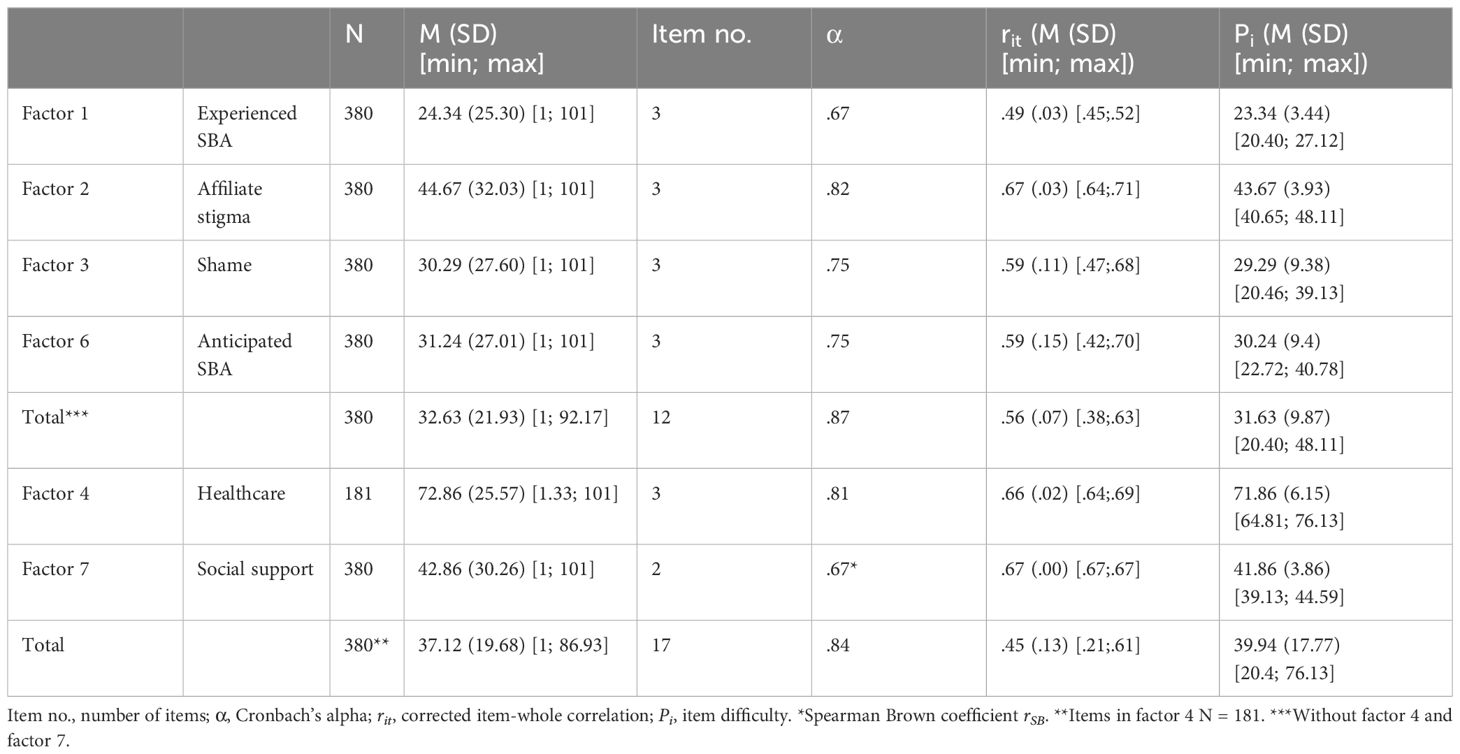
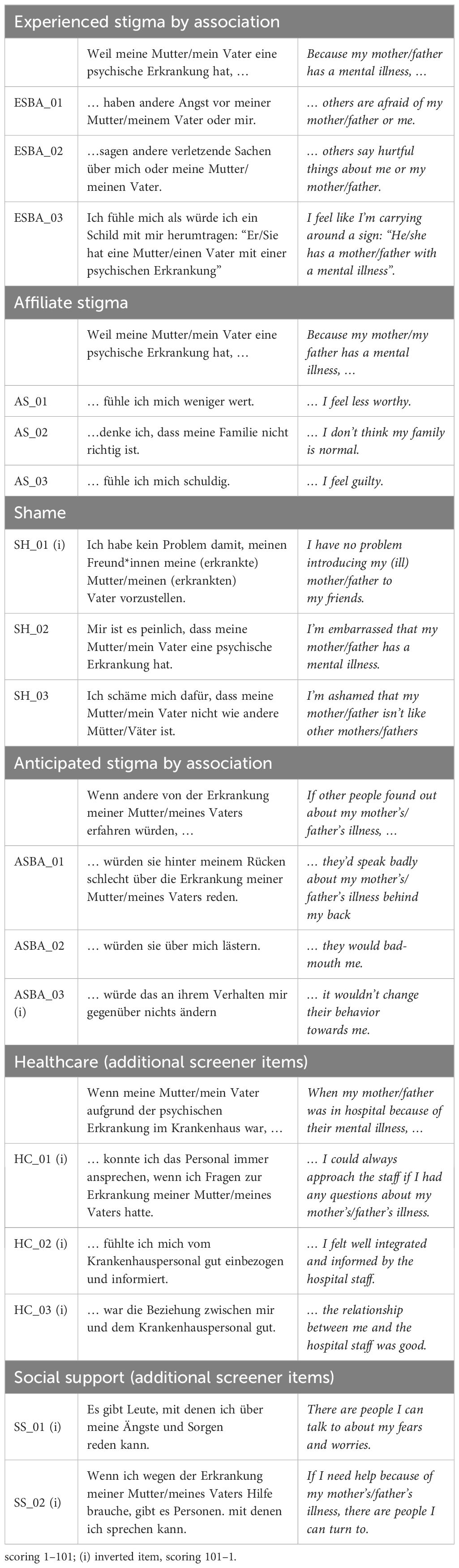
To enhance usability, the scales were further reduced in sample 1 to a maximum of three items per scale. For reduction, discriminatory power, item difficulty, and Cronbach’s alpha were considered and only the best items were retained. Detailed characteristics of the reduced scales are found in Table 6. The final items and scoring instructions of the COPMI-SQ-r are found in Table 7.
Factor 1 (“Experienced SBA”), factor 4 (“Healthcare”), and factor 7 (“Social support”): Since these scales already consisted of only two or three items, no further items were removed.
Factor 2 (“Affiliate stigma”): Step-by-step, eight items were removed. After removal, Cronbach’s alpha was α = .82. Discriminatory power was acceptable to (very) good (.64 ≤ rit ≤.71) and item difficulties ranged from Pi = 40.65 to Pi = 48.11.
Factor 3 (“Shame”): Step-by-step, three items were removed. After removal, Cronbach’s alpha was α = .75. Discriminatory power was (almost) good (.47 ≤ rit ≤.68), and item difficulties range from Pi = 20.46 to Pi = 39.13.
Factor 6 (“Anticipated SBA”): One item was removed. After removal, Cronbach’s alpha was α = .75. Discriminatory power was acceptable to good (.42 ≤ rit ≤.70), and item difficulties range from Pi = 22.72 to Pi = 40.78.
Total scale: Cronbach’s alpha was α = .84 for the total scale. Removing one item from factor 4 would have increased Cronbach’s alpha to α = .85. All items showed desirable item difficulties 20 < Pi < 80. Four items showed inacceptable discriminatory power rit <.3. Since all these items loaded on factor 4 (“Healthcare”) and factor 7 (“Social support”), those factors were excluded when calculating the total scale. Due to content considerations, the subscales were nevertheless retained as separate screening scales. After excluding factors 4 and 7, Cronbach’s alpha was α = .87. Removing any additional item would not have improved Cronbach’s alpha. All remaining items showed desirable item difficulties 20 < Pi < 80 and acceptable to desirable discriminatory power.38 ≤ rit ≤.63. All remaining items and their scale allocation are found in Table 7.
3.7 Results of CFA (sample 2)
Testing the theoretically derived four factor structure (model A*) with a CFA in sample 2 resulted in an inadequate model fit (χ2(2138) = 7,093.22, p <.001; RMSEA = .065 (90% CI = .063–.066); SRMR = .101; CFI = .667; AIC = 334 651.99) (see Table 8, model A*). All calculated models based on EFA and item analyses revealed a better model fit according to AIC than the theoretically derived four factor structure (see Table 8, models A*-F*). According to RMSEA (RMSEA ≤.062), SRMR (SRMR ≤.056), and CFI (CFI ≥.942), the COPMI-SQ-r with and without the additional screening scales showed a good model fit. Regarding AIC, a better model fit was observed for the COPMI-SQ-r without the additional screening scales (AIC = 60 008.05).
3.8 Results of Multiple-Group CFA (sample 1 and sample 2)
In the combined sample of adolescents who reported growing up with and without a parent with a mental illness (sample 1 and sample 2), configural invariance was observed (χ2 (208) = 481.58, p < .001; CFI = .939; RMSEA = .053 (90% CI = .047-.059); SRMR = .056), but metric invariance could not be established (Δχ2 (11) = 35.38; p < .001).
3.9 Item analyses (sample 2)
Item and scale analyses concerning their difficulty, discriminatory power, and reliability were also conducted for the revised instrument in sample 2. Detailed characteristics of the scales are found in Table 9. The final items and scoring instructions of the parallel version of the COPMI-SQ-r are found in Table 10.
Factor 1 (“Experienced SBA”): Cronbach’s alpha was almost acceptable with α = .68. Discriminatory power was acceptable to good (.43 ≤ rit ≤.59), and item difficulties ranged from Pi = 53.62 to Pi = 66.74.
Factor 2 (“Affiliate stigma”): Cronbach’s alpha was acceptable with α = .78. Discriminatory power was good (.57 ≤ rit ≤.67), and item difficulties ranged from Pi = 62.88 to Pi = 64.75.
Factor 3 (“Shame”): Cronbach’s alpha was almost acceptable with α = .69. Discriminatory power was almost acceptable to good (.28 ≤ rit ≤.66) and item difficulties ranged from Pi = 57.78 to Pi = 64.13.
Factor 6 (“Anticipated SBA”): Cronbach’s alpha was almost acceptable with α = .64. Discriminatory power was almost acceptable to good (.25 ≤ rit ≤.59), and item difficulties ranged from Pi = 47.78 to Pi = 60.11.
Factor 4 (“Healthcare”): Cronbach’s alpha was acceptable with α = .75. Discriminatory power was almost good (.58 ≤ rit ≤.59), and item difficulties ranged from Pi = 50.18 to Pi = 60.19.
Factor 7 (“Social support”): Since factor 7 consists of only two items, Spearman’s brown coefficient (rSB) was calculated as reliability coefficient. Spearman’s brown coefficient was acceptable with rSB = .59. The items showed desirable discriminatory power (rit = .61), and item difficulties ranged from Pi = 45.59 to Pi = 47.69.
Total scale: Cronbach’s alpha was α = .81 for the total scale. Item difficulties ranged from Pi = 45.59 to Pi = 66.74. Five items showed inacceptable discriminatory power rit <.3. All these items loaded on factor 4 (“Healthcare”) and factor 7 (“Social support”). After excluding these factors from calculating the total scale, Cronbach’s alpha was α = .84. Item difficulties ranged from Pi = 47.78 to Pi = 66.74. Discriminatory power was acceptable to good (.32 ≤ rit ≤.61) for all but one item (rit = .24).
4 Discussion
Mental disorders are still frequently stigmatized in society, which has negative consequences not only for the people with a mental disorder themselves but also for their family members. This is known as stigma by association (SBA) (9, 13–17). Children of parents with a mental illness carry an increased risk to experience SBA, one of the assumed mechanisms of the transgenerational transmission of mental disorders (25–29). To our knowledge, the COPMI-SQ is the first questionnaire to have been developed assessing such stigma-specific experiences of adolescents who grow up with a parent with a mental illness (30). Promising psychometric properties were reported in an initial small pilot study (30). In the current paper, we investigated the factorial structure and psychometric properties of this instrument in a larger sample and present a shortened and revised version—the COPMI-SQ-r. The structure of the COPMI-SQ-r was identified in a sample of adolescents who reported growing up with a parent with a mental illness (sample 1): Using CFA, the structure was replicated in an independent sample of adolescents who reported not growing up with a parent with a mental illness (sample 2). Furthermore, configural invariance was established in a multiple-group CFA in the combined sample of adolescents who reported growing up with and without a parent with a mental illness (sample 1 and sample 2). In the sample of adolescents who reported growing up with a parent with a mental illness (sample 1), psychometric properties of the COPMI-SQ-r were found to be acceptable to good. In the sample of adolescents who reported not growing up with a parent with a mental illness (sample 2), psychometric properties of the COPMI-SQ-r were found to be almost acceptable to good.
The final version of the COPMI-SQ-r consists of 12 items that load on the four main subscales “Experienced SBA,” “Affiliate stigma,” “Shame,” and “Anticipated SBA” (three items each). Experienced stigma, anticipated stigma, and internalized stigma have been identified as the most relevant mechanisms applying to the primary recipients of stigmatization (5), and it has been argued that SBA involves the same mechanisms (32).
The subscale “Experienced SBA” measures personally experienced stereotypes, prejudices, and discrimination in the past or present. Having unmet emotional needs (e.g., inappropriate language and contents, withdrawal and rejection) and experiencing hostile behaviors of others were identified as important aspects of “Experienced SBA” (32) that are both represented in the Experienced SBA subscale. Furthermore, one item of this subscale relates to the belief of being contaminated, which was originally thought to be part of the “Affiliate stigma” dimension (30). In the literature, children of parents with a mental illness have frequently been described as experiencing “contamination stigma” (20, 22, 32). On the one hand, contamination can refer to a “fear of inheriting their parent’s illness” (55)—an aspect that, due to item reduction, is no longer covered in the COPMI-SQ-r. On the other hand, contamination can also refer to the fear adolescents experience as closely connected to the parent with a mental illness and thus, also be considered to be “crazy” (56). Since the present item (“I feel like I’m carrying around a sign: ‘He/she has a mother/father with a mental illness.’”) refers not to a fear but to actual experiences of adolescents being perceived differently by others because of their parent’s mental illness, it makes sense that this item is incorporated within the subscale “Experienced SBA”.
The subscale “Anticipated SBA” captures the expectation of stigmatization in the future, and fearing hostile behaviors of others, fear of negative attitudes and ascriptions, and fearing others’ lack of understanding and rejections were identified as important aspects of “Anticipated SBA” in adolescents who grow up with a parent with a mental illness (32). Even though the present items were originally devised to specifically assess the aspect of fearing hostile behaviors (30), we find that they adequately capture “Anticipated SBA” in general. Concerning stigmatization, discrimination (e.g., hostile behaviors) is seen as the behavioral reaction to stereotypes and prejudices (5, 6). Attitudes are considered to be an individual’s positive or negative evaluation of a psychological object (57), which largely resembles the definition of prejudices as the approval of an existing stereotype in association with negative emotions (5, 6). The influence of attitudes on behavior has been well established in the theory of planned behavior (58). Therefore, we consider hostile behavior to be both the observable and anticipatable consequence of negative attitudes and of other’s lack of understanding.
“Affiliate stigma” can be understood as the SBA version of internalized stigma (33), and refers to the internalization of stereotypes and prejudices to the self (32). Perceiving themselves as being contaminated and perceiving themselves as being inferior have been identified as important aspects of “Affiliate Stigma” in adolescents who grow up with a parent with a mental illness (32). Stigmatization is understood as a process in which individuals are assigned to a group on the basis of a discrediting characteristic or trait and are subsequently devalued (3, 4). For adolescents who grow up with a parent with a mental illness, this seems to lead to a feeling of being less valuable and abnormal (32), a feeling the present subscale captures.
“Shame” was identified as a separate subscale of the COPMI-SQ-r in this paper. Most of the items in this subscale were originally part of the COPMI-SQ’s “Affiliate stigma” subscale. A recent integrative review identified that stigma experiences of children and adolescents who grow up with a parent with a mental illness often result in feelings of shame and embarrassment, and subsequently the attempt to hide the parental mental illness (21). This implies that “Shame” is more of a consequence of the other stigma dimensions, and therefore, it makes sense to assess it in a separate subscale.
Furthermore, the COPMI-SQ-r includes two additional screening scales: “Healthcare” (three items) and “Social support” (two items). The “Healthcare” subscale consists of the only items retained from the COPMI-SQ’s “Structural discrimination” subscale. Structural discrimination refers to the perpetuation of stigmatization through societal and policy structures (34). The original “Structural discrimination” subscale included a heterogeneous item pool (e.g., concerning media, school, and healthcare) and was not necessarily specific to the stigma experiences of adolescents who grow up with a parent with a mental illness (“Mental illness is portrayed negatively in the media.”). Due to their unspecificity and high heterogeneity, most of the items were already eliminated during the EFAs in sample 1 as they did not load on specific factors. Considering that stigmatization is a major issue in healthcare and has negative effects on treatment seeking and recovery (59), we nevertheless decided to keep these remaining three items as a separate screening scale to assess specific stigmatization experiences of adolescents who grow up with a parent with a mental illness in the healthcare sector. In line with this, two items were found to load on a specific “Social support” factor. Since social support is known to be an important protective factor for mental health (60, 61), we also decided to keep these items as a separate screening scale.
4.1 Limitations
Several limitations need to be considered regarding the present study. Having reduced the COPMI-SQ’s item numbers from initially 109 to now 17 (including the five screener items), some aspects of SBA concerning children and adolescents who grow up with a parent with a mental illness that appeared to be important in the systematic review (32) (e.g., fear of contamination by the parental mental disorder, structural discrimination in school or media) are no longer assessable with the COPMI-SQ-r. Nevertheless, the COPMI-SQ-r still captures the most relevant different aspects of stigma by association as reported in the literature (5, 20, 21, 32). Furthermore, the item reduction enhances its usability for both research and clinical practice. Recruiting adolescents who grow up with a parent with a mental illness into research studies is challenging (35, 36), but by social media advertising, we were able to recruit a large sample of adolescents who reported growing up with at least one parent with a mental illness. While our sample is large, it was not large enough to randomly divide it into two subsample to explore and test the factorial structure. Thus, an independent sample of adolescents who reported not growing up with a parent with a mental illness and who answered a parallel version of the COPMI-SQ that only differed on item stem was used to validate the derived factorial structure. In a multiple-group CFA, configural invariance was observed, but metric invariance could not be established. This implies that even though the factorial structure is the same between the different groups, results from using the COPMI-SQ-r in samples of adolescents who report growing up with and without a parent with a mental illness should not be compared (62, 63). In future studies, the factorial structure of COPMI-SQ-r should also be tested in other independent samples with adolescent who report growing up with a parent with a mental illness. Furthermore, our sample is self-selected and representativeness cannot be assumed (35). Furthermore, all data were collected only through self-report from the participating adolescents. Thus, reported parental symptoms and diagnoses have not been clinically validated. In addition, over 90% of participating adolescents indicated in sample 1 having a mental illness themselves. This number is much higher than reported in other studies (24, 27, 30), but again, one must be bear in mind that those are not clinically validated diagnoses and that the sample might be biased due to the recruitment strategy used (35). On the one hand, this high number of young people already affected emphasizes the need for preventive interventions to break the vicious circle of transgenerational transmission at an early stage (29, 64, 65). On the other hand, this also means that adolescents’ responses may be cofounded by stigma experiences regarding their own mental disorder. Future studies should therefore aim to include more representative samples with clinically validated diagnoses and with young people who do not experience mental health challenges themselves. Nevertheless, the reported rate of adolescents (59.4%), mothers (51.6%), and fathers (30.8%) in sample 1 being treated for their mental disorders indicates that the reported problems and symptoms are for the most part clinically relevant. As the COPMI-SQ-r has been only validated in German so far, its results are not generalizable to other cultures. In future studies, the existing English translation should therefore be used as a starting point to validate the COPMI-SQ-r in other languages and cultures. Most of the COPMI-SQ-r items reveal high item difficulty, meaning that few participants approved very highly of the items. To assess a broader range of stigmatization experiences of adolescents who grow up with a parent with a mental illness, future revisions of the instrument should ideally include items with lower item difficulty. Finally, yet importantly, as research in this field progresses, the COPMI-SQ-r’s concurrent and discriminant validity should be investigated as well as its retest reliability. Only factorial and content validity of the instrument has been ensured so far through the theory-based approach that was complemented by an expert panel during the piloting phase (30).
4.2 Implications
To reduce the stigma of mental illness in general and SBA in children and adolescents affected by a parental mental illness specifically, general anti-stigma campaigns and targeted interventions to reduce SBA in affected children and adolescents are needed (1, 31). One example is the Australian StigmaBeat project (66). In a participatory approach with young people who are affected by parental mental health challenges, films aiming at reducing mental health stigma were developed. The COPMI-SQ-r could be used to help develop, adapt, and evaluate activities such as StigmaBeat.
4.3 Conclusion
We have described here the development and validation of the COPMI-SQ-r transparently and in detail. The COPMI-SQ-r is a theoretically grounded, methodologically sound, reliable, and economic questionnaire to assess SBA in adolescents who grow up with a parent with a mental illness, which can be applied in both research and clinical practice, and it will enable us to better understand the specific stigma experiences of adolescents who grow up with a parent with a mental illness.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Department of Psychology at Philipps University Marburg. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MS: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. L-MD: Conceptualization, Writing – review & editing. HC: Conceptualization, Writing – review & editing, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This paper was written within the COMPARE-family-research project. COMPARE-family is funded by the Federal Ministry of Education and Research (BMBF) (01GL1748B). Open Access funding provided by the Open Acess Publishing Fund of Philipps-Universität Marburg.
Acknowledgments
The authors would like to thank all participating adolescents for their openness, commitment, and support for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1376627/full#supplementary-material
SUPPLEMENTARY TABLE 1 | COPMI-SQ reduction steps.
References
2. Goffmann E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, N.J.: Prentice-Hall (1963).
3. Phelan J, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Soc Sci Med. (2008) 67:358–67. doi: 10.1016/j.socscimed.2008.03.022
4. Hebl MR, Dovidio JF. Promoting the “social” in the examination of social stigmas. Pers Soc Psychol Rev. (2005) 9:156–82. doi: 10.1207/s15327957pspr0902_4
5. Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma: the mental illness stigma framework and critical review of measures. Stigma Health. (2018) 3:348–76. doi: 10.1037/sah0000104
6. Corrigan P, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
7. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. psychol Sci Public Interest. (2014) 15(2):37–70. doi: 10.1177/1529100614531398
8. Mulfinger N, Müller S, Böge I, Sakar V, Corrigan PW, Evans-Lacko S, et al. Honest, Open, Proud for adolescents with mental illness: pilot randomized controlled trial. Child Psychol Psychiatry. (2018) 59:684–91. doi: 10.1111/jcpp.12853
9. Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. (2016) 387:1123–32. doi: 10.1016/S0140-6736(15)00298-6
10. Lannin DG, Vogel DL, Brenner RE, Abraham WT, Heath PJ. Does self-stigma reduce the probability of seeking mental health information? J Couns Psychol. (2016) 63:351–8. doi: 10.1037/cou0000108
11. Farrelly S, Jeffery D, Rüsch N, Williams P, Thornicroft G, Clement S. The link between mental health-related discrimination and suicidality: service user perspectives. Psychol Med. (2015) 45:2013–22. doi: 10.1017/S0033291714003158
12. Corrigan P, Morris S, Larson J, Rafacz J, Wassel A, Michaels P, et al. Self-stigma and coming out about one’s mental illness. J Community Psychol. (2010) 38:259–75. doi: 10.1002/jcop.20363
13. Goldstein SB, Johnson VA. Stigma by association: perceptions of the dating partners of college students with physical disabilities. Basic Appl Soc Psychol. (1997) 19:495–504. doi: 10.1207/15324839751036931
14. Haber DB, Roby JL, High-George LD. Stigma by association: the effects of caring for HIV/AIDS patients in South Africa: Association stigma for HIV/AIDS workers in South Africa. Health Soc Care Community. (2011) 19:541–9. doi: 10.1111/hsc.2011.19.issue-5
15. Östman M, Kjellin L. Stigma by association: Psychological factors in relatives of people with mental illness. Br J Psychiatry. (2002) 181:494–8. doi: 10.1192/bjp.181.6.494
16. van der Sanden RLM, Bos AER, Stutterheim SE, Pryor JB, Kok G. Experiences of stigma by association among family members of people with mental illness. Rehabil Psychol. (2013) 58:73–80. doi: 10.1037/a0031752
17. Pryor JB, Reeder GD, Monroe AE. The infection of bad company: Stigma by association. J Pers Soc Psychol. (2012) 102:224–41. doi: 10.1037/a0026270
18. Campbell DT. Common fate, similarity, and other indices of the status of aggregates of persons as social entities. Syst Res. (1958) 3:14–25. doi: 10.1002/bs.3830030103
19. Park S, Park KS. Family stigma: A concept analysis. Asian Nurs Res. (2014) 8:165–71. doi: 10.1016/j.anr.2014.02.006
20. Corrigan PW, Miller FE. Shame, blame, and contamination: A review of the impact of mental illness stigma on family members. J Ment Health. (2004) 13:537–48. doi: 10.1080/09638230400017004
21. Reupert A, Gladstone B, Helena Hine R, Yates S, McGaw V, Charles G, et al. Stigma in relation to families living with parental mental illness: An integrative review. Int J Ment Health Nurs. (2021) 30:6–26. doi: 10.1111/inm.12820
22. Larson JE, Corrigan P. The stigma of families with mental illness. Acad Psychiatry. (2008) 32:87–91. doi: 10.1176/appi.ap.32.2.87
23. Christiansen H, Reck C, Zietlow AL, Otto K, Steinmayr R, Wirthwein L, et al. Children of mentally III parents at risk evaluation (COMPARE): design and methods of a randomized controlled multicenter study-part I. Front Psychiatry. (2019) 10:128. doi: 10.3389/fpsyt.2019.00128
24. Leijdesdorff S, van Doesum K, Popma A, Klaassen R, van Amelsvoort T. Prevalence of psychopathology in children of parents with mental illness and/or addiction: An up to date narrative review. Curr Opin Psychiatry. (2017) 30:312–7. doi: 10.1097/YCO.0000000000000341
25. Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophr Bull. (2014) 40:28–38. doi: 10.1093/schbul/sbt114
26. Thorup AAE, Laursen TM, Munk-Olsen T, Ranning A, Mortensen PB, Plessen KJ, et al. Incidence of child and adolescent mental disorders in children aged 0–17 with familial high risk for severe mental illness - A Danish register study. Schizophr Res. (2018) 197:298–304. doi: 10.1016/j.schres.2017.11.009
27. Uher R, Pavlova B, Radua J, Provenzani U, Najafi S, Fortea L, et al. Transdiagnostic risk of mental disorders in offspring of affected parents: a meta-analysis of family high-risk and registry studies. World Psychiatry. (2023) 22:433–48. doi: 10.1002/wps.21147
28. van Santvoort F, Hosman CMH, van Doesum KTM, Janssens JMAM. Effectiveness of preventive support groups for children of mentally ill or addicted parents: a randomized controlled trial. Eur Child Adolesc Psychiatry. (2014) 23:473–84. doi: 10.1007/s00787-013-0476-9
29. Hosman CMH, van Doesum KTM, van Santvoort F. Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands: I. The scientific basis to a comprehensive approach. Aust e-Journal Adv Ment Health. (2009) 8:250–63. doi: 10.5172/jamh.8.3.250
30. Dobener LM, Stracke M, Viehl K, Christiansen H. Children of parents with a mental illness—Stigma questionnaire: development and piloting. Front Psychiatry. (2022) 13:800037. doi: 10.3389/fpsyt.2022.800037
31. Peter LJ, Schindler S, Sander C, Schmidt S, Muehlan H, McLaren T, et al. Continuum beliefs and mental illness stigma: a systematic review and meta-analysis of correlation and intervention studies. Psychol Med. (2021) 51:716–26. doi: 10.1017/S0033291721000854
32. Dobener LM, Fahrer J, Purtscheller D, Paul J, Christiansen H. How do children of parents with mental illness experience stigma?: A systematic mixed studies review. Front Psychiatry. (2022) 13:813519. doi: 10.3389/fpsyt.2022.813519
33. Mak WWS, Cheung RYM. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J Appl Res Intellectual Disabilities. (2008) 21:532–45. doi: 10.1111/j.1468-3148.2008.00426.x
34. Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma: advances in theory and research. Basic Appl Soc Psychol. (2013) 35:1–9. doi: 10.1080/01973533.2012.746147
35. Grové C. Using social networking sites in research: an emerging approach to engaging with young people who have a parent with a mental illness and/or substance abuse disorder. Front Psychiatry. (2019) 10:76. doi: 10.3389/fpsyt.2019.00281
36. van Doesum KTM, Riebschleger J, Carroll J, Grové C, Lauritzen C, Mordoch E, et al. Successful recruitment strategies for prevention programs targeting children of parents with mental health challenges: An international study. Child Youth Services. (2016) 37:156–74. doi: 10.1080/0145935X.2016.1104075
37. Stracke M, Gilbert K, Kieser M, Klose C, Krisam J, Ebert DD, et al. COMPARE family (Children of mentally ill parents at risk evaluation): A study protocol for a preventive intervention for children of mentally ill parents (Triple P, evidence-based program that enhances parentings skills, in addition to gold-standard CBT with the mentally ill parent) in a multicenter RCT-part II. Front Psychiatry. (2019) 10:54. doi: 10.3389/fpsyt.2019.00054
38. Leiner DJ. SoSci survey (2019). Available online at: https://www.soscisurvey.de.
39. Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res. (2006) 78:473–87. doi: 10.1007/s11205-005-1607-6
40. R Studio Team. RStudio: Integrated Development for R. Boston, MA: RStudio, PBC (2020). Available at: http://www.rstudio.com/.
41. Revelle W. psych: Procedures for Psychological, Psychometric, and Personality Research. Evanston, Illinois: Northwestern University (2022). Available at: https://CRAN.R-project.org/package=psych.
42. Raiche G, Magis D. nFactors: Parallel Analysis and Other Non Graphical Solutions to the Cattell Scree Test . Available online at: https://CRAN.R-project.org/package=nFactors.
43. Rosseel Y. lavaan: An R package for structural equation modeling. J Stat Soft. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
44. Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology. (2018) 09:2207. doi: 10.4236/psych.2018.98126
45. Coughlan J, Hooper D, Mullen M. Structural Equation Modelling: Guidelines for Determining Model Fit (2008). Available online at: https://arrow.dit.ie/buschmanart/2/.
46. Cavanaugh JE, Neath AA. The Akaike information criterion: Background, derivation, properties, application, interpretation, and refinements. WIREs Comput Stats. (2019) 11:e1460. doi: 10.1002/wics.1460
47. Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res. (2003) 8:23–74. doi: 10.23668/psycharchives.12784
48. Bartlett MS. A note on the multiplying factors for various χ 2 approximations. J R Stat Soc: Ser B (Methodological). (1954) 16:296–8. doi: 10.1111/j.2517-6161.1954.tb00174.x
49. Kaiser HF. A second generation little jiffy. Psychometrika. (1970) 35:401–15. doi: 10.1007/BF02291817
50. Kaiser HF. An index of factorial simplicity. Psychometrika. (1974) 39:31–6. doi: 10.1007/BF02291575
51. O’Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behav Res Methods Instrumentation Comput. (2000) 32:396–402. doi: 10.3758/bf03200807
52. George D, Mallery P. SPSS for Windows step by step: a simple guide and reference, 11.0 update. 4th ed. Boston: Allyn and Bacon (2003).
53. Moosbrugger H, Kelava A. Testtheorie und Fragebogenkonstruktion. Berlin, Heidelberg: Springer Berlin Heidelberg (2020). Available at: https://link.springer.com/10.1007/978–3-662–61532-4.
54. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington, Va (2013). p. 943.
55. Trondsen MV, Tjora A. Communal normalization in an online self-help group for adolescents with a mentally ill parent. Qual Health Res. (2014) 24:1407–17. doi: 10.1177/1049732314547708
56. Carroll L, Tuason M. Perpetually self-reflective. Couns Psychol. (2015) 43:1059–83. doi: 10.1177/0011000015602316
57. Ajzen I, Fishbein M. Attitudes and the attitude-behavior relation: reasoned and automatic processes. Eur Rev Soc Psychol. (2000) 11:1–33. doi: 10.1080/14792779943000116
58. Ajzen I, Fishbein M. The Influence of Attitudes on Behavior. In: The handbook of attitudes. Lawrence Erlbaum Associates Publishers, Mahwah, NJ, US (2005). p. 173–221.
59. Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc Manage Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
60. Werner EE. Resilience in development. Curr Dir Psychol Sci. (1995) 4:81–4. doi: 10.1111/1467-8721.ep10772327
61. Wille N, Bettge S, Ravens-Sieberer U. Risk and protective factors for children’s and adolescents’ mental health: results of the BELLA study. Eur Child Adolesc Psychiatry. (2008) 17:133–47. doi: 10.1007/s00787-008-1015-y
62. van de Schoot R, Lugtig P, Hox J. A checklist for testing measurement invariance. Eur J Dev Psychol. (2012). doi: 10.1080/17405629.2012.686740
63. Svetina D, Rutkowski L, Rutkowski D. Multiple-group invariance with categorical outcomes using updated guidelines: an illustration using Mplus and the lavaan/semTools packages. Structural Equation Modeling: A Multidisciplinary Journal. (2020) 27:111–30. doi: 10.1080/10705511.2019.1602776
64. Siegenthaler E, Munder T, Egger M. Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2012) 51:8–17. doi: 10.1016/j.jaac.2011.10.018
65. Thanhäuser M, Lemmer G, Girolamo G, Christiansen H. Do preventive interventions for children of mentally ill parents work? Results of a systematic review and meta-analysis. Curr Opin Psychiatry. (2017) 30:283–99. doi: 10.1097/YCO.0000000000000342
Keywords: children of parents with a mental illness, stigma, stigma by association, family stigma, questionnaire
Citation: Stracke M, Dobener L-M and Christiansen H (2024) Children of parents with a mental illness – stigma questionnaire: validation and revision. Front. Psychiatry 15:1376627. doi: 10.3389/fpsyt.2024.1376627
Received: 25 January 2024; Accepted: 13 May 2024;
Published: 17 June 2024.
Edited by:
Joanne Nicholson, Brandeis University, United StatesReviewed by:
Holger Muehlan, Health and Medical University Erfurt, GermanyAndrea Reupert, Monash University, Australia
Copyright © 2024 Stracke, Dobener and Christiansen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Markus Stracke, bWFya3VzLnN0cmFja2VAdW5pLW1hcmJ1cmcuZGU=
 Markus Stracke
Markus Stracke Lisa-Marie Dobener
Lisa-Marie Dobener Hanna Christiansen
Hanna Christiansen