
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 28 March 2024
Sec. Computational Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1369720
This article is part of the Research Topic Emotional Impulsivity and Emotion Regulation Deficits as Important Factors in Clinically Challenging Behaviors in Psychiatric Disorders View all 13 articles
A correction has been applied to this article in:
Corrigendum: Emotion dysregulation links pathological eating styles and psychopathological traits in bariatric surgery candidates
 Arianna Belloli1,2†
Arianna Belloli1,2† Luigi F. Saccaro3,4*†
Luigi F. Saccaro3,4*† Paola Landi1
Paola Landi1 Milena Spera1
Milena Spera1 Marco Antonio Zappa5
Marco Antonio Zappa5 Bernardo Dell’Osso1
Bernardo Dell’Osso1 Grazia Rutigliano6
Grazia Rutigliano6Objectives: Approximately one-third of bariatric surgery patients experience weight regain or suboptimal weight loss within five years post-surgery. Pathological eating styles and psychopathological traits (e.g., emotion dysregulation) are recognized as potential hindrances to sustain weight loss efforts and are implicated in obesity development. A comprehensive understanding of these variables and their interplays is still lacking, despite their potential significance in developing more effective clinical interventions for bariatric patients. We investigate the prevalence of and interactions between pathological eating styles and psychopathological traits in this population.
Materials and methods: 110 bariatric surgery candidates were characterized using the Binge Eating Scale (BES), Hamilton Depression/Anxiety Scales (HAM-D/A), Barratt Impulsiveness Scale (BIS-11), Experiences in Close Relationships (ECR), Difficulties in Emotion Regulation Scale (DERS). We analyzed these variables with multiple logistic regression analyses and network analysis.
Results: Patients with pathological eating styles showed more pronounced anxiety/depressive symptoms and emotion dysregulation. Network analysis revealed strong connections between BES and DERS, with DERS also displaying robust connections with HAM-A/D and ECR scales. DERS and attention impulsivity (BIS-11-A) emerged as the strongest nodes in the network.
Discussion: Our findings demonstrate the mediating role of emotion dysregulation between pathological eating styles and psychopathological traits, supporting existing literature on the association between psychopathological traits, insecure attachment styles, and pathological eating behaviors. This research emphasizes the significance of emotion regulation in the complex network of variables contributing to obesity, and its potential impact on bariatric surgery outcomes. Interventions focusing on emotion regulation may thus lead to improved clinical outcomes for bariatric patients.
Obesity is a metabolic and neuroendocrine condition characterized by an excessive accumulation or abnormal distribution of body fat, related to health complications. The etiology of obesity is complex and multifactorial, characterized by the interplay between biological and psychosocial factors (1). Bariatric surgery refers to a variety of inner gastrointestinal surgical techniques that were first intended to help patients who were morbidly obese lose weight. However, the advantages of bariatric surgery go far beyond weight loss and include a significant improvement in type 2 diabetes, hypertension, dyslipidemia, and a decrease in overall mortality. Bariatric surgeries, performed laparoscopically, can be classified into: restrictive (gastric banding and sleeve gastrectomy), malabsorptive (biliopancreatic diversion and mini gastric bypass) and mixed. Restrictive interventions are based on gastric volume reduction, malabsorptive ones are aimed at reducing the size of the stomach by modifying its digestive process, and mixed interventions, such as gastric bypass, reduce the volume of the stomach pouch and the surface area intestinal destined for absorption. Bariatric surgery has significant evidence of efficacy and safety (2) and it currently represents the best intervention for obesity in terms of weight reduction, complication control, and improvement of the quality of life (3).
A thorough psychological assessment, with particular attention to pathological eating styles, can be a useful clinical tool for managing treatment before and after bariatric surgery (4) In the present study, conducted on an Italian sample, we referred to the following taxonomy of eating styles proposed by the Italian Society of Surgery of Obesity and Metabolic Diseases: emotional eating, binge eating, qualitative eating, quantitative eating, gorging, and snacking (3). Details about the main pathological eating styles are provided in the Supplementary Material.
Preoperative psychological assessment is critical for bariatric surgery candidates, because it may help stratify patients based on risk of weight regain after surgery and other post-surgical outcomes (5). For an effective treatment for obesity, it is essential to consider and, ideally to treat, the underlying psychopathology maintaining abnormal eating styles (6). The psychological profile of obese patients is often characterized by anxious and depressive symptoms, impulsivity, insecure and poor attachment quality, low self-esteem, and body dissatisfaction (7). The presence of these psychopathological traits could lead to food consumption as a dysfunctional coping strategy in response to negative emotions, in absence of effective emotion regulation strategies, resulting in development of obesity (8). During the eligibility evaluation for bariatric surgery, emotion regulation and emotion recognition are seldom assessed, although neurobiological processes concerning self-regulation, including control over eating behaviors, are strongly influenced by emotions (9). Emotion regulation can be defined as the “attempt to influence which emotions we have, when we have them, and how these emotions are experienced or expressed” (10). If emotion regulation fails, self-regulation in other areas, like control over eating behaviors, may fail as well (11), hence the importance of emotion dysregulation in pathological eating behaviors, besides in other psychiatric disorders (12). Impulsiveness is also a common trait in patients who present dysregulation in food intake, especially those diagnosed with Binge Eating Disorder, whose psychological profile is characterized by significant impulsivity levels (13). Therefore, the exploration of emotion regulation and impulsivity is crucial in obese patients seeking bariatric surgery (14). Increasing evidence suggests that insecure attachment plays a crucial role in the development of obesity (15). Research indicates that insecure attachment, either anxious and avoidant, is positively associated with emotion dysregulation and can predict disordered eating behaviors, particularly in women (16, 17). In this regard, attachment history could be a key factor to consider in the prevention and treatment of overweight and obesity. Children whose caregiver is unreliable and unresponsive to their needs, may turn to food as a coping mechanism, in absence of alternative functional strategies to manage their emotions. This attitude frequently persists even into adulthood (18). In this regard we hypothesized that the main psychological factors which maintain pathological eating behaviors are emotion dysregulation, impulsivity, and insecure attachment styles.
Nevertheless, it is currently unclear how emotion dysregulation, impulsivity, and insecure attachment styles contribute to the development and maintenance of eating behaviors that can lead to obesity. Understanding these mechanisms is therefore relevant in order to improve bariatric surgery outcomes. To fill this gap, we assessed psychopathological traits and eating behaviors in a sample of bariatric surgery candidates,and applied a network analysis to clarify the interplay between psychopathological traits and eating behaviors. A network statistical approach is essential for investigating the complex interplay between emotion regulation difficulties, pathological eating behaviors, and psychopathological traits in individuals who are candidates for bariatric surgery, as it enables the identification of key nodes within the network that can be targeted for intervention, leading to more effective treatments. A network analysis specifically allows to identify the variables within the psychological profile to be addressed for intervention to prevent weight regain, providing a framework that may help to improve the long-term outcomes of bariatric surgery (19).
110 consecutive subjects (mean age: 45.04 years, standard deviation: 10.44 years, 77% females) were prospectively recruited from the multidisciplinary obesity surgery center of the Fatebenefratelli Sacco Hospital in Milan, between January 2019 and December 2021. Subjects were included if they were scheduled for bariatric surgery, according to SICOb (the Italian Society of Surgery for Obesity and Metabolic Diseases) criteria for bariatric surgery (detailed in the Supplementary Material). They were excluded if they were younger than 18, if they did not speak Italian, or if they did not consent. They underwent a clinical interview to exclude any mental disorders comorbidity, to measure psychopathological traits, and to assess eating behavioral styles. Thus, for instance, patients were included if they presented binge eating style, but not if they presented the full-blown Binge Eating Disorder. Patients signed an informed consent, and their identity was protected. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Fatebenefratelli Sacco Hospital (“psycBAR36”‘, 2020).
During the evaluation of the surgery eligibility, patients were thoroughly monitored through a multi-disciplinary medical consultation (with dietologists, gastroenterologists, psychiatrists, and psychologists). In particular, a psychiatrist (PL) and psychotherapist (MS) clinically assessed and classified the eating behavior styles for each subject, through detailed clinical interviews involving specific questions to assess the presence of the following eating behavioral styles: emotional eating, binge eating, quantitative, qualitative (or external) eating, gorging, and snacking. Details about such clinical interviews are provided in the Supplementary Material. Various psychopathological traits were investigated using specific clinical scores for psychopathological traits. The Difficulties in Emotion Regulation Scale (DERS) was employed to assess emotion regulation difficulties. The Hamilton Depression Scale (HAM-D) and Hamilton Anxiety Scale (HAM-A) were used to measure levels of depression and anxiety, respectively. To evaluate binge eating behaviors, we used the Binge Eating Scale (BES). Impulsivity was assessed using the Barratt Impulsiveness Scale (BIS-11), which was further divided into subscales. The subscales included: Attention (BIS-11, A), Motor impulsivity/impulsiveness (BIS-11, Im), Self-control (BIS-11, Ac), Cognitive complexity (BIS-11, Cc), Perseverance (BIS-11, P), and Cognitive Instability (BIS-11, IC). Attachment styles were evaluated using the Experiences in Close Relationships - Revised (ECR-R) scale, with two subscales of attachment styles for avoidance and anxiety (Av/An).
Details about these clinical scores for psychopathological traits are provided in the Supplementary Material.
The categorical variables were described by absolute and relative frequencies, while the continuous variables by means of median and interquartile range, given their non-Gaussian distribution (evaluated with the D’Agostino and Pearson tests). Differences in the distribution of clinical scale scores between patients with and without the different dysfunctional eating habits were analyzed with independent-samples Mann-Whitney U. After quantifying missing data (Supplementary Table 3), we used the multiple imputation method to generate five complete datasets. Then, six separate multiple logistic regression models (including the original dataset) were run on multiply imputed datasets, with eating behavioral styles (quantity, quality, snack, gorge, binge, emotional eating) as dependent variables and gender and psychopathological traits (DERS, HAM-D/A, BES BIS-11, ECR-R) as independent variables. The results of the six analyses were then combined and we report below the results of the pooled analysis after multiple imputation. Statistical analyses were run in SPSS© version 23. We adjusted the results for multiple comparisons using the Bonferroni correction for multiple comparison. In our case, the adjusted significance threshold is a pcorr value of 0.05/6 = 0.008.
To examine the relationship between eating disorder-specific scales (BES), psychiatric scales (HAM-D and HAM-A), and psychological/personality scales (BIS-11, ECR-R, and DERS), in our sample of candidates to bariatric surgery, we applied network analysis in R (https://www.Rproject.org/, version 3.6.3.), following the methods outlined in the tutorial paper by Epskamp et al. (2017) (20). This method mainly employs the free R packages bootnet and qgraph. In summary, a pairwise Markov random field network model was employed, allowing for the estimation of undirected edges, without implying any causal inference or direction in association, along with their accuracy. Additionally, centrality indices of nodes were estimated to determine their stability among the variables composing the network. The data used in the model were cross-sectional and did not follow a normal distribution. To address this, a “nonparanormal transformation” (20) was applied to convert the data into normally distributed form. In order to retain more robust edges in our sample and ensure interpretability, a “least absolute shrinkage and selection operator” (21) regularization technique was utilized. Furthermore, the Extended Bayesian Information Criterion (22, 23) was set to 0.5.
Lastly, robustness analyses were performed using the R package bootnet to ensure the stability and precision of the results. To evaluate the accuracy of the estimated edges, nonparametric bootstrapping (24) was performed, providing confidence intervals at the 95% level. To assess the role of each variable in the network, we calculated three centrality indexes (node strength, closeness, and betweenness). Node strength is a measure of how strongly a variable (which constitutes a node) is directly connected to other variables in the network (i.e. the total weighted connections that a variable has with other variables in the network) (25). Closeness centrality, i.e. the inverse of the sum of distances between the focal node and all other nodes in the network, measures how quickly information spreads from one variable to others in the network. The higher the closeness centrality value, the more central a variable is within the network, since variables with a high closeness score present the shortest distances to all others (26). Betweenness centrality quantifies the extent to which a variable acts as a bridge or mediator between other variables in the network, by measuring the number of times a node lies on the shortest path between other nodes. A higher betweenness centrality value suggests that the variable plays a crucial role in connecting different parts of the network (25).
Our sample included 85 women and 25 men (total: 110, median age 47 years). The most frequent pathological eating style was the achievement of gratification with large quantity of food (n=78, 70.9%), followed by emotional eating (n=74, 68.5%), achievement of gratification based in food quality (very salty or sweet) (n=66, 60%), snacking (n=59, 53.6%), gorging (n=46, 41.8%), and binge eating (n=18, 16.4%). In 92.7% of cases (n=102) patients presented 2 or more pathological eating behaviors. 31.9% (n=30) of patients showed moderate to severe BES scores (Table 1).
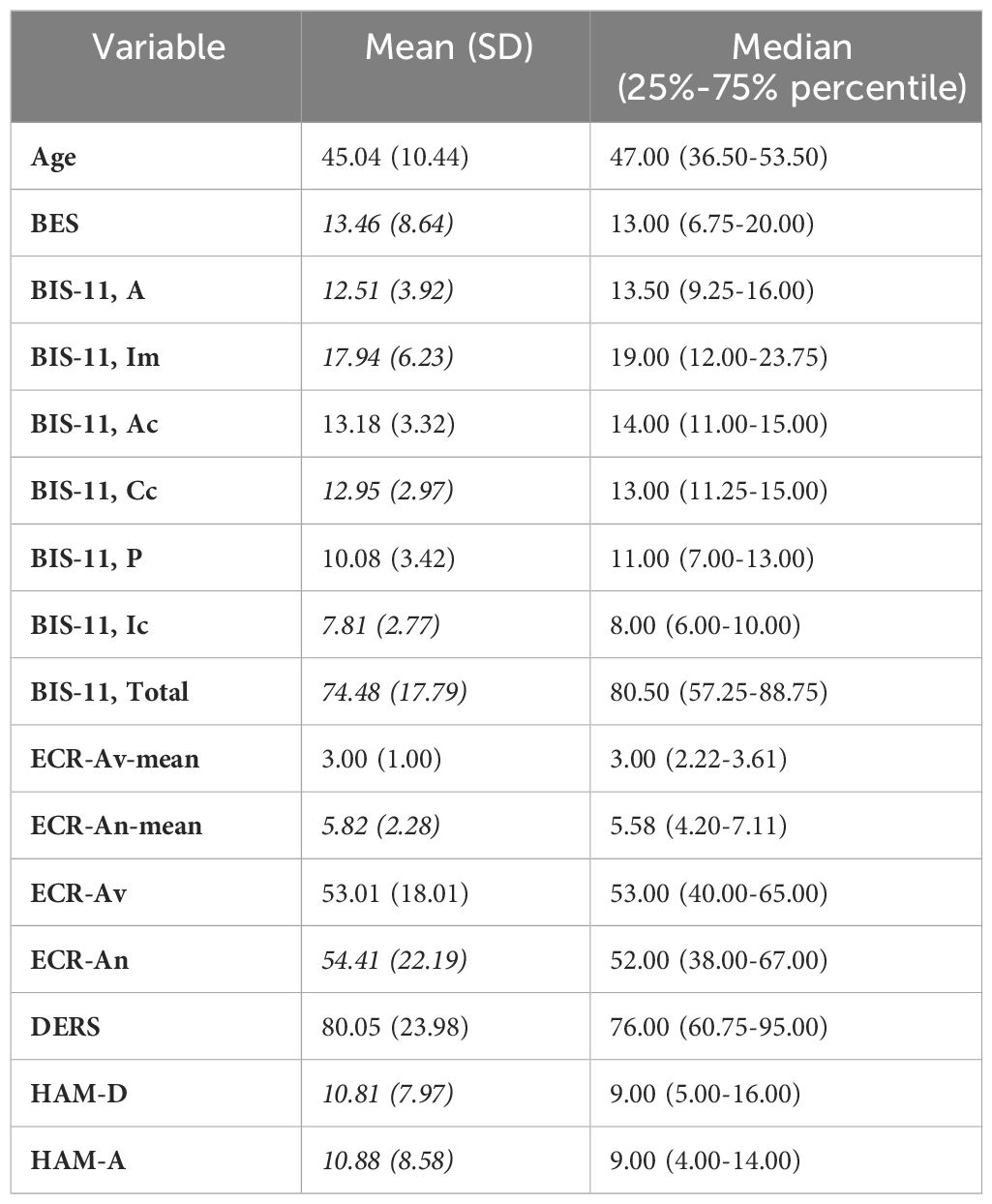
Table 1. Sample characteristics, Continuous variables: Difficulties in Emotion Regulation Scale (DERS), Experiences in Close Relationships Questionnaire - Revised-Avoidance/Anxiety (ECR-Av/An), Hamilton Depression Scale (HAM-D), and Hamilton Anxiety Scale (HAM-A), Binge Eating Scale (BES), Barratt Impulsiveness Scale (BIS-11). BIS-11 is further divided into factors, including Attention (BIS-11, A), Motor impulsiveness (BIS-11, Im), Self-control (BIS-11, Ac), Cognitive complexity (BIS-11, Cc), Perseverance (BIS-11, P) and Cognitive Instability (BIS-11, IC).
As detailed in Supplementary Tables 2A–F, we compared the distribution of psychopathological traits between patients with and without the different dysfunctional eating styles.
Higher scores in different BIS-11 domains were found among patients with gorging than in those without this eating style (BIS-11, A, attention, p=0.012; BIS-11, Im, motor impulsivity, p=0.029; BIS-11, Ac, self-control, p=0.001; BIS-11, P, perseverance, p=0.031).
Patients with binge and emotional eating showed higher scores in: BES (respectively, p<0.001 and p=0.030); ECR-R (avoidant: respectively, p=0.038 and p=0.051; anxious: respectively, p=0.019 and p=0.009); DERS (respectively, p=0.038 and p=0.056); HAM-D (p=0.012 and p=0.001) and HAM-A (p=0.012 and 0.001). Patients seeking quantitative gratification have higher scores in HAM-A (p=0.014).
The following findings survived adjustment for multiple comparisons: higher scores in BIS-11, Ac (self-control) among patients with gorging eating style (U=1220, pcorr<0.008); higher scores in BIS-11, A (attention, U=545, pcorr<0.008) and Im (motor impulsivity, U=518, pcorr<0.008) among patients with qualitative eating style; higher scores in BES among patients with binge eating style (U=918, pcorr<0.001); and higher scores in HAM-D (U=1422, pcorr=0.001) and HAM-A (U=1421, pcorr=0.001) in patients with emotional eating style.
The logistic regression analysis yielded several significant findings before correction for multiple comparisons (Supplementary Table 4). For a one-unit increase in BIS-11-Ac (self-control domain of BIS-11), the odds of gorge eating style increased by 24% (95% CI [1.003, 1.53], p=0.047). For a one-unit increase in BES, the odds of binge eating style increased by 19% (95% CI [1.024, 1.374], p=0.024). Lastly, males were almost 5 times more likely to have a quantitative eating style as compared to females (95% CI [1.053, 22.099]), while their odds of having an emotional eating style were 24% lower (95% CI [0.076, 0.748]). There were no other significant findings.
No result of the logistic regression analysis survived adjustment for multiple comparisons.
The network includes the following psychopathological traits: DERS, HAM-D/A, BES, BIS-11, ECR (Figure 1). The correlation matrix between the variables is shown in Supplementary Figure 1.

Figure 1. Network structure. The variables include eating disorder-specific scales (BES), psychiatric scales (HAM-D and HAM-A) and psychological and personality scales (BIS-11, ECR and DER). Item groups are differentiated by color. Edge colors represent the direction of associations (blue for positive, red for negative), and edge widths indicate the strength of these associations.
Network structure showed that all psychopathological traits were connected, either directly or indirectly, with each other through positive associations. However, psychopathological traits within the same domain were generally connected more strongly than across domains. For instance, impulsiveness scores formed an interconnected cluster that was almost isolated from the rest of the network, apart from a weak connection with BES and DERS. HAM-D and HAM-A were strongly interconnected with each other, as well as ECR-R scores. Regarding connections across domains, BES was most strongly connected with DERS, which was in turn robustly connected with HAM-A/D and ECR-R. This pattern of connectivity was confirmed by the network showing that the shortest path between the BES and HAM-A/D scales was indeed through DERS (Figure 2).

Figure 2. Network showing the shortest path between the BES and Hamilton depression and anxiety scales. The variables include eating disorder-specific scales (BES), psychiatric scales (HAM-D and HAM-A) and psychological and personality scales (BIS-11, ECR and DER). Item groups are differentiated by color. Edge colors represent the direction of associations (blue for positive, red for negative), and edge widths indicate the strength of these associations.
According to the centrality indexes analysis (Figure 3), the strongest nodes in the network were DERS and BIS-11-A (Attention impulsivity). Of note, the high node strength of BIS-11-A seems to be due to the strong connections within the BIS-11 subscores, while DERS strength derives mainly from diverse connections with the remaining variables. BIS-11-C, BIS-11-Ac, and BES had the lowest node strengths.
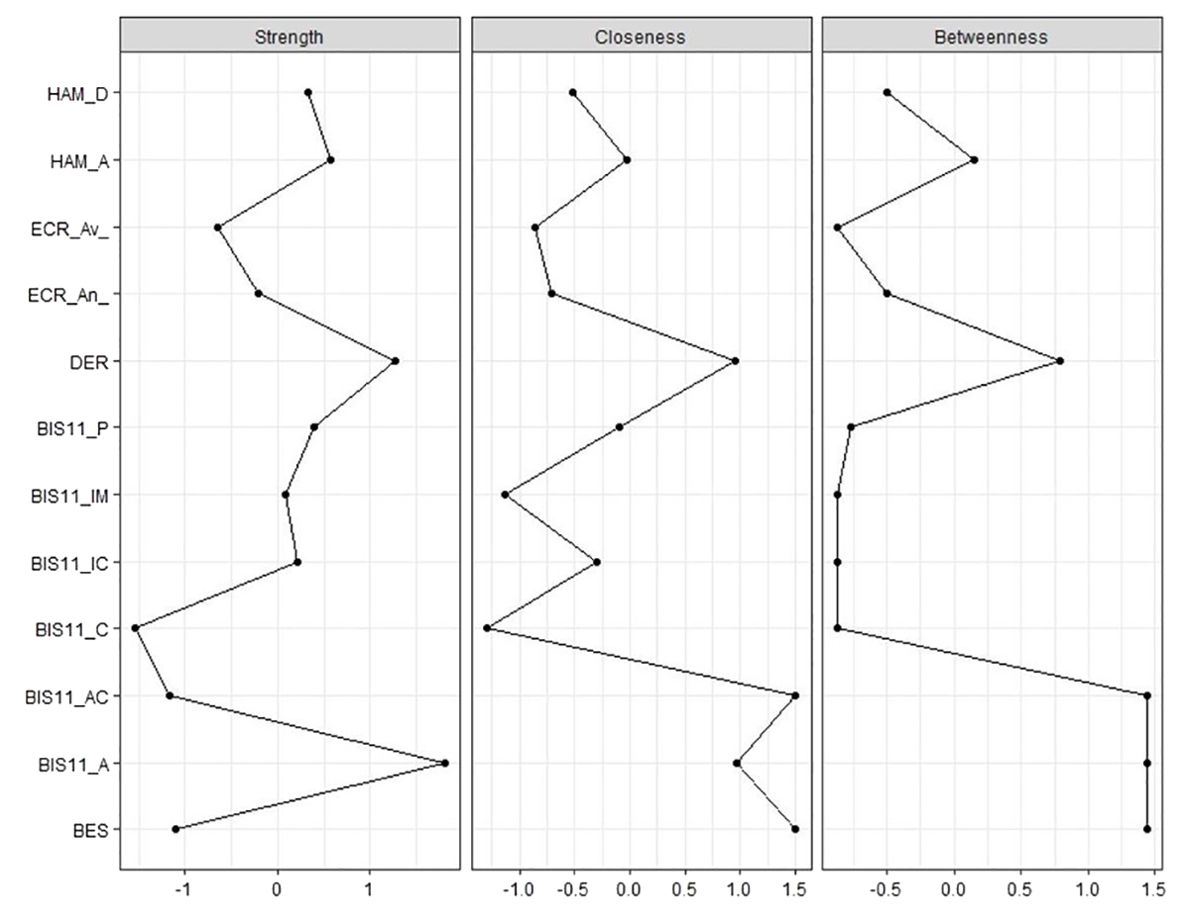
Figure 3. Centrality indexes (node strength, closeness and betweenness) of eating disorder-specific scales (BES), psychiatric scales (HAM-D and HAM-A) and psychological and personality scales (BIS-11, ECR and DERS) in our sample of patients candidate to bariatric surgery. standardized z-scores are shown on x-axis.
Closeness and betweenness were highly correlated in the network. This correlation indicates that the variables that are influential in spreading information quickly throughout the network (high closeness centrality) are also likely to be important in facilitating communication and interactions between different nodes (high betweenness centrality).
The variables with highest closeness and betweenness were DERS, BIS-11-C, BIS-11-Ac, and BES.
These variables act therefore as critical intermediaries, linking different clusters or groups within the network and enabling the flow of information between them.
Further details on stability of centrality indices (Supplementary Figure 3), as well as networks showing the shortest paths between BES and other variables are available in Supplementary Information (Supplementary Figures 4-6).
We assessed the accuracy and stability of edge-weights through robustness analyses (Supplementary Figure 2). These analyses employed bootstrapped confidence intervals for estimated edge-weights within the network encompassing ED-specific scales (BES), psychiatric scales (HAM-D and HAM-A), and psychological and personality scales (BIS-11, ECR, and DERS). These robustness analyses revealed the presence of relatively wide bootstrapped confidence intervals, suggesting a need for caution, especially when interpreting weaker edges. However, it’s noteworthy that the sample values predominantly fall within the bootstrapped confidence intervals, and the bootstrap mean values generally align well with the sample values. These outcomes collectively indicate reasonably accurate estimations and offer results that can be sensibly interpreted.
The average correlations between centrality indices (strength and betweenness) were examined across networks generated by dropping varying proportions of the data through 2500 iterations. The findings indicate that the central stability coefficient, which signifies the maximum drop proportions necessary to maintain a correlation of 0.7 in at least 95% of the sample, was 0.365 for strength and 0 for betweenness (Supplementary Figure 3). It is important to note that networks with dependable centrality should exhibit a stability coefficient equal to or greater than 0.25, ideally surpassing 0.5 for centrality estimates (27). Consequently, particular caution is warranted when interpreting these results and the centrality of betweenness, which may lack stability.
The purpose of the present study is to provide novel evidence on the association between pathological eating styles and psychopathological traits, employing network analysis in a sample of bariatric surgery candidates. The findings of the current study highlight the importance of considering these interconnected factors when assessing and treating individuals with pathological eating behaviors and, specifically, those who are candidates for bariatric surgery.
Finally, we found that subjects with binge eating and emotional eating had a higher psychopathological burden with higher scores on different scales (DERS, HAM-D, HAM-A, BES, and ECR-R). More in detail, our network analysis shows that emotion regulation difficulties have a pivotal role in linking the positive association between anxious attachment style and binge eating, as well as the association between binge eating and symptoms of anxiety and depression. This is in line with existing literature, which shows that emotion dysregulation may be a crucial underlying mechanism linking insecure attachment to emotional eating and other dysfunctional eating styles in bariatric patients (28). In fact, a meta-analytic review (29) highlights how an insecure attachment of the anxious type is significantly associated with dysfunctional eating behaviors such as: binges, bulimic symptoms, consumption of unhealthy food, and emotional eating, as compared to a safe attachment. For these individuals food becomes a self-regulation and self-assurance tool, highlighting the link between emotion regulation and food seeking. These results therefore suggest that psychological interventions aimed at reducing emotion dysregulation may help decrease dysfunctional eating behaviors in bariatric surgery candidates (30). In our study, impulsivity emerged as the other significant factor in the pathophysiology of dysfunctional eating behaviors, specifically gorging. In fact, patients who engaged in gorging had higher scores in the self-control domain of the Impulsiveness Scale. The relationship between impulsivity and pathological eating may be also linked by emotion dysregulation (14).
Our study shows that network analysis represents a promising approach for the exploration of the mechanisms underlying the psychological profile of bariatric surgery candidates. Although little literature (31) is currently available on network analysis applied to bariatric surgery, there is novel evidence on the use of network analysis in the field of eating disorders (EDs) (32–38). Solmi and colleagues applied network analysis to assess ED-specific symptoms, psychiatric symptoms, and general clinical variables on a sample of patients diagnosed with EDs. Their results suggested the central role of drive for thinness, interpersonal functioning, ineffectiveness, interoceptive awareness, and affective symptoms in EDs (39). Although this study does not specifically treat bariatric patients, it stresses like our study how a network approach may highlight a maintaining psychopathologic loop which appears to involve, but transcends, dimensions peculiar to the ED-psychopathology. Similar to our study, these findings’ clinical implications rely on understanding this psychological profile, underlying eating symptoms, in order to prevent relapses.
Monteleone and colleagues applied for the first time a network approach to bariatric surgery candidates to explore the interplay between eating symptoms, personality traits, and anxiety. In line with our findings, their study stressed the importance of incorporating psychological variables into the pre-surgery assessment, as well as considering them as potential targets for psychotherapeutic interventions before and after surgery (31) Instead, differently from our study, their research includes the administration of a specific instrument, the Temperament and Character Inventory-Revised (TCI-R) (40) that comprehensively assesses the patient’s personality profile, allowing a detailed overview of the personological traits of this clinical population. They also combined the network analysis approach with prognostic data. A deeper personological assessment and a longitudinal perspective could therefore be future perspectives for our study. Calugi & Dalle Grave used a network analysis to assess the interplay between psychosocial variables in a large sample of patients with obesity, stressing how this innovative approach allows an in-depth exploration of their complex clinical profile (38). In contrast to our study, their sample does not include bariatric patients and they have only evaluated psychosocial factors associated with obesity, not including personality traits. Their network analysis, however, considered also the internalized weight stigma in patients seeking treatment for obesity, which emerged as one of the most relevant variable in their network, together with interpersonal sensitivity, and shape-weight concern. A growing body of research (32–38) applied network analysis to EDs, even though not specifically on bariatric surgery candidates, their implications are consistent with ours in stressing the interplay between eating behaviors and psychopathological traits and the need to implement a network approach. Our results confirm the need for a multidisciplinary approach to bariatric surgery, implementing psychiatric and psychological interventions in order to discover and treat pathological eating behaviors and psychopathological traits such as emotion dysregulation, impulsivity, anxiety, and depression, that can be either the cause of obesity or of weight-regain (41, 42).
The present network analysis suggests that emotion dysregulation links the relationship between dysfunctional eating patterns and symptoms of anxiety and depression. In conclusion, this study highlights the importance of a comprehensive psychological assessment for patients seeking bariatric surgery as it identifies the presence of multiple pathological eating behaviors and psychopathological traits. In this regard, the present study stresses the utility of a network approach to understand the psychological background of bariatric candidates and develop tailored interventions that address specific nodes in the network, potentially improving the long-term success of bariatric surgery and reducing the risk of relapse into pathological eating behaviors.
Our findings have quickly translatable clinical implications, because interventions on emotion regulation can act as therapeutic targets to break the vicious cycle between dysfunctional eating patterns, emotion dysregulation, and anxious-depressive symptoms in line with previous research (43). This also suggests that interventions that target impulsivity and emotion regulation, such as cognitive-behavioral therapy (44) or mindfulness-based interventions (45), may be beneficial in treating pathological eating behaviors in patients seeking bariatric surgery (e.g., mindfulness for emotional eating) (46).
The cross-sectional design and reliance on self-report questionnaires may represent limitations of the study’s ability to infer causality or temporal dynamics and the monocentric nature of the study may limit its generalizability to other populations. Further research is needed to investigate the associations between eating styles and psychopathological traits, particularly in relation to the risk of excessive weight gain or dysfunctional eating following bariatric surgery and to test the replicability of these findings in other ethnic groups, as well as address potential sources of inequality. It is crucial to assess whether emotion regulation difficulties persist or re-emerge after surgery and their impact on pathological eating styles and weight outcomes in the long term. In particular, longitudinal randomized control trials are needed to evaluate whether treatments targeting emotion regulation difficulties and/or dysfunctional eating styles may improve the outcomes of bariatric surgery, as well as patients’ psychopathological traits.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Fatebenefratelli Sacco Hospital (“psycBAR36”‘, 2020). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
LS: Data curation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. PL: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing. MS: Conceptualization, Investigation, Methodology, Writing – review & editing. MZ: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. BD: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. GR: Data curation, Formal analysis, Software, Supervision, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1369720/full#supplementary-material
1. Bray GA. Evaluation of obesity: Who are the obese? Postgraduate Med. (2003) 114:19–38. doi: 10.3810/pgm.2003.12.1544
2. Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: A review. JAMA. (2020) 324:879. doi: 10.1001/jama.2020.12567
3. Foschi D, De Luca M, Sarro G, Bernante P, Zappa MA, Moroni R, et al. Linee guida di Chirurgia dell’Obesità. (2016).
4. Micanti F, Cerbone MR, Galletta D, Paone E, Sollai C. Suggerimenti per le procedure psicologico-psichiatriche in chirurgia dell’obesità. (2017).
5. Lier HØ, Biringer E, Stubhaug B, Tangen T. Prevalence of psychiatric disorders before and 1 year after bariatric surgery: The role of shame in maintenance of psychiatric disorders in patients undergoing bariatric surgery. Nordic J Psychiatry. (2013) 67:89–96. doi: 10.3109/08039488.2012.684703
6. Zeller MH, Boles RE, Reiter-Purtill J. The additive and interactive effects of parenting style and temperament in obese youth seeking treatment. Int J Obes. (2008) 32:1474–80. doi: 10.1038/ijo.2008.125
7. Robinson E, Roberts C, Vainik U, Jones A. The psychology of obesity: An umbrella review and evidence-based map of the psychological correlates of heavier body weight. Neurosci Biobehav Rev. (2020) 119:468–80. doi: 10.1016/j.neubiorev.2020.10.009
8. Finistrella V, Manco M, Corciulo N, Sances B, Di Pietro M, Di Gregorio R, et al. Eating disorders and psychopathological traits in obese preadolescents and adolescents. J Am Coll Nutr. (2015) 34:142–9. doi: 10.1080/07315724.2014.938182
9. Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends Cogn Sci. (2011) 15:132–9. doi: 10.1016/j.tics.2010.12.005
10. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. (1998) 2:271–99. doi: 10.1037/1089-2680.2.3.271
11. Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity - a systematic review. Neurosci Biobehav Rev. (2015) 49:125–34. doi: 10.1016/j.neubiorev.2014.12.008
12. Petruso F, Giff AE, Milano BA, De Rossi MM, Saccaro LF. Inflammation and emotion regulation: a narrative review of evidence and mechanisms in emotion dysregulation disorders. Neuronal Signaling. (2023) 7:NS20220077. doi: 10.1042/NS20220077
13. Giel K, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder—A systematic update of the evidence. Nutrients. (2017) 9:1170. doi: 10.3390/nu9111170
14. Benzerouk F, Djerada Z, Bertin E, Barrière S, Gierski F, Kaladjian A. Contributions of emotional overload, emotion dysregulation, and impulsivity to eating patterns in obese patients with binge eating disorder and seeking bariatric surgery. Nutrients. (2020) 12:3099. doi: 10.3390/nu12103099
15. Santos AF, Martins MC, Fernandes C, Bost KK, Veríssimo M. Relation between attachment and obesity in preschool years: A systematic review of the literature. Nutrients. (2021) 13:3572. doi: 10.3390/nu13103572
16. Ty M, Francis AJP. Insecure attachment and disordered eating in women: the mediating processes of social comparison and emotion dysregulation. Eating Disord. (2013) 21:154–74. doi: 10.1080/10640266.2013.761089
17. Saccaro LF, Rutigliano G, Landi P, Spera M, Kraslavski A, Zappa MA, et al. Emotional regulation underlies gender differences in pathological eating behavior styles of bariatric surgery candidates. Women. (2023) 3:189–99. doi: 10.3390/women3020015
18. Cooper MJ, Warren L. The relationship between body weight (body mass index) and attachment history in young women. Eating Behav. (2011) 12:94–6. doi: 10.1016/j.eatbeh.2010.11.006
19. Guloksuz S, Pries L-K, van Os J. Application of network methods for understanding mental disorders: pitfalls and promise. Psychol Med. (2017) 47:2743–52. doi: 10.1017/S0033291717001350
20. Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: Be careful what you wish for. PLoS One. (2017) 12:e0179891. doi: 10.1371/journal.pone.0179891
21. Friedman J, Hastie T, Tibshirani R. Glasso: Graphical lasso-estimation of Gaussian graphical models. (2014).
22. Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. (2008) 95:759–71. doi: 10.1093/biomet/asn034
23. Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. (2010). doi: 10.48550/ARXIV.1011.6640
25. Zweig KA. Centrality indices. Network Anal Literacy. (2016), 243–76. doi: 10.1007/978-3-7091-0741-6_9
26. Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med. (2018) 6:301–28. doi: 10.1080/21642850.2018.1521283
27. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
28. Taube-Schiff M, Van Exan J, Tanaka R, Wnuk S, Hawa R, Sockalingam S. Attachment style and emotional eating in bariatric surgery candidates: The mediating role of difficulties in emotion regulation. Eating Behav. (2015) 18:36–40. doi: 10.1016/j.eatbeh.2015.03.011
29. Faber A, Dubé L, Knäuper B. Attachment and eating: A meta-analytic review of the relevance of attachment for unhealthy and healthy eating behaviors in the general population. Appetite. (2018) 123:410–38. doi: 10.1016/j.appet.2017.10.043
30. Shakory S, Van Exan J, Mills JS, Sockalingam S, Keating L, Taube-Schiff M. Binge eating in bariatric surgery candidates: The role of insecure attachment and emotion regulation. Appetite. (2015) 91:69–75. doi: 10.1016/j.appet.2015.03.026
31. Monteleone AM, Cascino G, Solmi M, Pirozzi R, Tolone S, Terracciano G, et al. A network analysis of psychological, personality and eating characteristics of people seeking bariatric surgery: Identification of key variables and their prognostic value. J Psychosomatic Res. (2019) 120:81–9. doi: 10.1016/j.jpsychores.2019.03.010
32. Calugi S, Sartirana M, Misconel A, Boglioli C, Dalle Grave R. Eating disorder psychopathology in adults and adolescents with anorexia nervosa: A network approach. Int J Eat Disord. (2020) 53:690–701. doi: 10.1002/eat.23270
33. Calugi S, Dametti L, Chimini M, Dalle Grave A, Dalle Grave R. Change in eating-disorder psychopathology network structure in patients with anorexia nervosa treated with intensive cognitive behavior therapy. Int J Eat Disord. (2021) 54:1800–9. doi: 10.1002/eat.23590
34. Calugi S, Dametti L, Dalle Grave A, Dalle Grave R. Changes in specific and nonspecific psychopathology network structure after intensive cognitive behavior therapy in patients with anorexia nervosa. Intl J Eating Disord. (2022) 55:1090–9. doi: 10.1002/eat.23755
35. Monteleone AM, Cascino G. A systematic review of network analysis studies in eating disorders: Is time to broaden the core psychopathology to non specific symptoms. Eur Eat Disord Rev. (2021) 29:531–47. doi: 10.1002/erv.2834
36. Calugi S, Dalle Grave R. The network analysis in patients with anorexia nervosa treated with intensive enhanced cognitive behavior therapy: reflections on the research data. IJEDO. (2023) 5:1–3. doi: 10.32044/ijedo.2023.01
37. Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. (2003) 41:509–28. doi: 10.1016/S0005-7967(02)00088-8
38. Calugi S, Dalle Grave R. Psychological features in obesity: A network analysis. Intl J Eating Disord. (2020) 53:248–55. doi: 10.1002/eat.23190
39. Solmi M, Collantoni E, Meneguzzo P, Degortes D, Tenconi E, Favaro A. Network analysis of specific psychopathology and psychiatric symptoms in patients with eating disorders. Intl J Eating Disord. (2018) 51:680–92. doi: 10.1002/eat.22884
40. Fossati A, Cloninger CR, Villa D, Borroni S, Grazioli F, Giarolli L, et al. Reliability and validity of the Italian version of the temperament and character inventory-revised in an outpatient sample. Compr Psychiatry. (2007) 48:380–7. doi: 10.1016/J.COMPPSYCH.2007.02.003
41. Troisi A. Bariatric Psychology and Psychiatry. Cham: Springer International Publishing (2020). doi: 10.1007/978-3-030-44834-9
42. Monteleone AM, Globus I, Cascino G, Klomek AB, Latzer Y. Psychopathology predicts mental but not physical bariatric surgery outcome at 3-year follow-up: a network analysis study. Eat Weight Disord. (2022) 27:3331–40. doi: 10.1007/s40519-022-01463-x
43. Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
44. Boswell RG, Gueorguieva R, Grilo CM. Change in impulsivity is prospectively associated with treatment outcomes for binge-eating disorder. Psychol Med. (2023) 53:2789–97. doi: 10.1017/S003329172100475X
45. Lattimore P. Mindfulness-based emotional eating awareness training: taking the emotional out of eating. Eat Weight Disord. (2020) 25:649–57. doi: 10.1007/s40519-019-00667-y
Keywords: obesity, bariatric surgery, eating style, emotion regulation, network analysis
Citation: Belloli A, Saccaro LF, Landi P, Spera M, Zappa MA, Dell’Osso B and Rutigliano G (2024) Emotion dysregulation links pathological eating styles and psychopathological traits in bariatric surgery candidates. Front. Psychiatry 15:1369720. doi: 10.3389/fpsyt.2024.1369720
Received: 12 January 2024; Accepted: 18 March 2024;
Published: 28 March 2024.
Edited by:
Takashi Nakano, Fujita Health University, JapanReviewed by:
Xinyuan Yan, University of Minnesota Twin Cities, United StatesCopyright © 2024 Belloli, Saccaro, Landi, Spera, Zappa, Dell’Osso and Rutigliano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luigi F. Saccaro, bHVpZ2lmcmFuY2VzY28uc2FjY2Fyb0B1bmlnZS5jaA==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.