- 1Department of Psychiatry, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Department of Medical Nursing School of Nursing, College of Medicine and Health, Science, University of Gondar, Gondar, Ethiopia
Background: Premenstrual dysphoric disorder (PMDD) is the most prevalent but neglected psychiatric disorder, with somatic symptoms that are severe enough to markedly affect usual daily activities and have a negative impact on mental health and quality of life by affecting female patients’ behavior and cognition. Studies regarding premenstrual dysphoric disorder and associated factors among high school students in low- and middle-income countries are limited. Therefore, the aim of this study was to assess the prevalence and associated factors of PMDD among high school students, and this is pivotal in further investigation.
Methods: A school-based cross-sectional study was conducted from March 25 to April 17, 2023 using a simple random-sampling technique to select a sample of 564 participants. Premenstrual dysphoric disorder was assessed using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Self-administered standardized questionnaires were used to collect data.
Result: A total of 548 study participants participated, with a 97.2% response rate. The prevalence of premenstrual dysphoric disorder among high school students was found to be 33.03% (95%CI: 29.20–37.09). In a multivariable analysis, irregular menstruation cycle (AOR = 4.242, 95%CI = 2.182–8.246), depression (AOR = 5.272, 95%CI = 2.779–10.002), having greater than 4 days of menstruation bleeding duration (AOR = 2.138, 95%CI = 1.105–4.138), and high perceived stress (AOR = 3.468, 95%CL = 1.217–9.880) were the factors significantly associated with premenstrual dysphoric disorder.
Conclusion: The overall prevalence of PMDD which was one-third among high school students was high. Moreover, long duration of menstruation bleeding, depressive symptoms, irregular menstruation cycle, and high perceived stress were significant factors in PMDD. Therefore, it needs early screening and intervention in primary healthcare settings, especially for those who have high perceived stress, having depression, having a long duration of menstruation bleeding, and having an irregular menstruation cycle, so as to have good academic achievement and psychological wellbeing.
Introduction
Premenstrual dysphoric disorder (PMDD) is a combination of physical pain and emotional or behavioral abnormalities that start around a week before the start of menstruation (1). Around the world, 3% to 8% of women of reproductive age experience premenstrual dysphoric disorder (PMDD) (2). Prevalence data from around the world reveals that up to 75% of all women of reproductive age may suffer premenstrual syndrome (PMS), with 5% to 20% of women of reproductive age reporting moderate to severe premenstrual complaints. About 94.8% of women of reproductive age had PMS, characterized by one or more physical, emotional, or behavioral symptoms in the days leading up to menstruation (15 to 49 years) (3). In Africa, including Ethiopia, the magnitude of premenstrual dysphoric disorder is between 10.2% and 66.9% (4–7).
Premenstrual dysphoric disorder (PMDD) is a serious condition that seriously impairs a woman’s functionality and quality of life. It affects female behavior, cognitive capacities, mental health status (like being seven times more likely to have suicidal thoughts and nearly four times more likely to attempt suicide), academic performance, interpersonal relationships, daily activities, and work productivity. A woman’s general physical health can all be negatively impacted by PMDD (8–11). Even though the majority of women with PMS can carry out their daily tasks when in its extreme form, this condition has been linked to increased absenteeism from work and school, poor academic performance, high suicide ideation and attempt rates, and significant mental health issues (5, 12).
Students struggle to get out of bed and be at class on time, and unexpected mood changes make it challenging to deal with the fallout. When PMS is not treated and women experience additional personal or environmental stress, the symptoms become more severe, eventually developing into PMDD, a mental disease (13–15).
Different factors affect PMDD, including age, body mass index (BMI <30 kg), monthly pain, amount of menstrual blood loss, history of physical and mental illness, treatment-seeking behavior, history of traumatic events, sleeping hours, physical activity, not using the family planning method, and maternal history of PMS (16–18). Blood loss during periods, the existence of dysmenorrhea, a mother or sister with a positive premenstrual syndrome, and low agreeableness and extroversion as well as high neuroticism were significant risk factors for PMDD in terms of personality traits (10, 19, 20).
A family history of PMS and dysmenorrhea increases the risk. Other menstrual characteristics, such as age at menarche, irregular menstruation, a longer average menstrual cycle, menorrhagia, consuming tea, coffee, sweets or sweetened beverages, and junk food, food intake, and stress were significant predictors of PMDD (4, 10, 21).
While PMDD among high school students has been relatively well researched in developed countries, more premenstrual syndrome studies are available in developing countries, including Ethiopia. Nevertheless, in Africa, including Ethiopia, some premenstrual dysphoric disorder studies are available among university students. According to my research engine, a few studies were conducted among high school students in developing countries. Even though premenstrual disorders (PMDD) have a significant impact on academic performance, yet, in Ethiopia, premenstrual difficulties still receive insufficient attention (19). Those few studies were done without including factors like perceived stress and clinical factors like a history of mental illness (suicide and major depression). Therefore, this study assessed the prevalence of PMDD and various factors that might lead to early interventions for further obstacles among high school students.
Methods and materials
Study area, design, and period
The study was conducted in west Gojjam. Finote Selam town is one of the zones in the Amhara Region of Ethiopia. It is far by 171.2 km from Bahir Dar of Amhara Region town and 246 km from Addis Ababa, the capital city of Ethiopia. Based on the 2007 national census conducted by the Central Statistical Agency of Ethiopia (CSA), this town had a total population of 25,913, of whom 13,035 were men and 12,878 women. Most (97.92%) inhabitants practice Ethiopian Orthodox Christianity, and 2.08% are Muslim. Moreover, 99.45% are members of the Amhara ethnic group. Three governmental high schools currently enroll 4,055 female students, but there are no private schools. There is one primary hospital and two health centers in the district which serve the community. A school-based cross-sectional study design was employed from March 25 to April 17, 2023 in Finote Selam town high school students. The source population was high school students who have been studying in Finote Selam town, and the study population comprised all high school students who were available during the data collection period in 2023.
Inclusion criteria
Students who have attended a class during the data collection time were included.
Exclusion criteria
High school students who were in serious conditions like illness at data collection time were excluded. Students who transferred from other schools to Finote Selam High School in the second semester of 2023 were also excluded.
Sample size determination and sampling techniques
The sample size was determined by assuming a single proportional formula. The prevalence of premenstrual dysphoric disorder was taken from a previously published study in Ethiopia at Ayder High School, Mekelle, and the magnitude of premenstrual dysphoric disorder was at 30.9% (22). The sample size (n) is calculated using a 95% confidence interval (CI) and a margin of error of 4% as follows:
where n = sample
z = critical value, 1.96
p = assumed prevalence of premenstrual dysphoric disorder from the previous study at Mekelle High School, 30.9%
d = precision (marginal error), 0.04
q = 1 - p
So, the minimum sample size was derived as follows:
Including 10% of the non-response rate, the final sample size was 513 + 51 = 564.
Associated factors, including severe menstrual pain, high perceived stress, and severe degree of dysmenorrhea, were highly associated with PMDD from previous studies at the University of Gondar and Wollo University (19, 22, 23). Therefore, using Epinfo version 7 software by double population formula, 95%CI and power 80% can be calculated, and high school students in the area of the study were stratified based on their schools in each grade, which are grade 9, grade 10, grade 11, and grade 12. Data from the Education Office indicated that the total number of high school students during data collection was 4,055 (grade 9 = 1,685, grade 10 = 1,070, grade 11 = 778, and grade 12 = 522). Then, the proportional allocation of study subjects for each school and each grade was calculated. Finally, a computer-generated method was used to select study participants from each stratum.
Data collection tool
Data was gathered using a comprehensive, well-organized questionnaire that was created after evaluating related literature and being adjusted for our situation.
An outcome variable prevalence of premenstrual dysphoric disorder was assessed by using DSM-5. The American Psychiatric Association produced the DSM-5, which is presently used in Ethiopia to diagnose clinical PMDD. Female students were deemed to have PMDD if they reported at least five DSM-5 diagnostic criteria symptoms in most of their menstrual cycles. These symptoms had to be present in the final week before the start of menstruation (1).
The Perceived Stress Scale-10 item (PSS-10), determined to be extremely reliable for assessing the role of stress in the etiology of psychiatric and behavioral illnesses, was used to measure individual stress levels. Scores on the PSS-10 ranging from 0 to 13 indicated low felt stress, scores 14 to 26 indicated moderately perceived stress, and scores 27 to 40 were thought to indicate highly perceived stress. In the evaluation of its dependability, a Cronbach’s alpha of 0.88 was used (24).
Depression in high school was assessed using Patient Health Questioner (PHQ-9). It is a nine-item version, and each item response is rated as “0” (not at all) to “3” (nearly every day); the total score ranges from 0 to 27, with a cutoff ≥5 to indicate having depression symptoms. It has sensitivity of 88% and specificity of 88%. PHQ-9 has been translated and validated in Ethiopia and has been used extensively therein previously to assess depression (25).
The Oslo three-item social support scale, which had a cumulative score range of 3 to 14 and comprised three major categories, was used to evaluate social support. Respondents who scored between 3 and 8, 9 and 12, and 13 and 14 were classified as having weak, moderate, and strong social support, respectively, according to this category. Cronbach’s alpha for the current study was 0.79, indicating acceptable reliability (26).
Structured yes/no questions were used to evaluate clinical factors such as family history of mental illness, history of other mental illnesses, suicidal ideation and attempt, and chronic medical illness.
The World Health Organization’s (WHO) ASSIST (Alcohol, Smoking, and Substance Involvement Screening Test), a highly validated instrument, was utilized in the questionnaire’s behavioral component sections, which include questions about substance use for its evaluation (current use and ever use) (27, 28).
The obstetric and gynecological variables menstrual cycle, menstrual pain, and age of menarche were evaluated using structured questions taken from the literature. The number of pads used per day during the menstrual period was used to calculate the amount of menstruation (22).
Menstrual pain was measured using a three-point verbal rating scale (VRS) with the adjectives mild, moderate, and severe rather than the four-point VRS with a “no pain” category. Only respondents who reported having dysmenorrhea were asked to rate their pain levels (29, 30).
Data collection
Data were collected using self-administered questionnaires. Three BSc nurses collected data using self-administered questionnaires. Two BSc psychiatry profession supervisors and the principal investigator were participating. For those data collectors and the supervisor, one training day was given before the data collection date. During the training, the objectives of the study were discussed. The data collection methods and tools, as well as how to handle ethical issues, were discussed with the data collectors. The structured questionnaire was also discussed in detail by going through each question with clarification for doubt.
Data quality assurance
To control the quality of the data, the questionnaire was translated appropriately into the local
Amharic language. At 1 week before the actual data collection, the questionnaire was pretested. Collection time was on 5% (N = 28) of Jiga High School students’ studies, which was not be included in the primary survey. Therefore, the dependent variable tool assessment (DSM-5) Cronbach alpha was 0.83. The collected data was adequately handled, reviewed, and checked for completeness and consistency by the supervisor and principal investigator each day.
Data processing and analysis
The collected data were coded, cleaned, entered, and checked into the computer using EPI data version 4.6.02 and then imported into STATA version 14 to generate descriptive statistics: means, frequencies, percentages, and standard deviations. Logistic regression was used to determine an association between dependent and independent variables and to adjust odds ratios, and the significance level was determined. Using a confidence interval of 95%, univariable and multivariable logistic regressions were used to identify the independent predictors of premenstrual dysphoric disorder. This was done by entering each independent variable separately into the univariable analysis. The variables with a p-value of less than 0.2 on the univariable analysis were entered into the multivariable analysis. The statistically significant variables are then considered. An association with a p-value less than or equal to 0.05 on logistic regression was considered a predictor of premenstrual dysphoric disorder. Hosmer and Lemeshow test, with a p-value of 0.8026 for premenstrual dysphoric disorder, was applied to test the logistic regression model for the goodness of fit. Multicollinearity was performed for the model, and none of the variables scored above 10 (mean VIF = 1.27). For all statistical tests, a p-value less than 0.05 was considered significant.
Results
Sociodemographic characteristics of the respondents
Data were obtained from 548 female high school students with a response rate of 97.2%. The mean age of the participants was 17.312 ± 1.631, ranging from 15 to 22 years old, and 415 (75.73%) were between 15 to 18 years old. Almost three-fourths, 409 (74.64%), of students were originally from urban areas. The majority of students were single, 469 (85.58%), and more than half of the students lived with their two parents, 316 (57.66%) (Table 1).
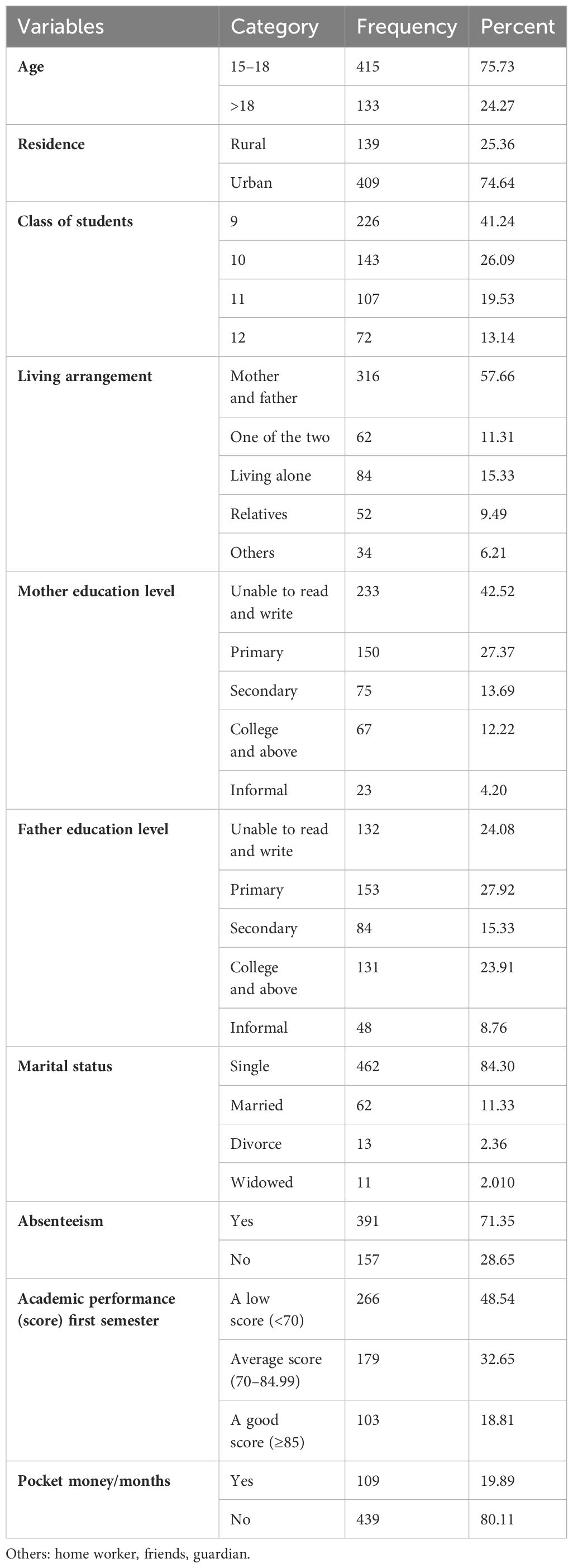
Table 1 Sociodemographic characteristics of the participants among high school students in Finote Selam town (n = 548), 2023.
Clinical characteristics of the respondents
Out of the total participants,12 (2.19%) students had a known chronic medical illness, 19 (3.47%) had a history of mental illness, 47 (8.58%) had a family history of mental illness, 31 (5.66%) had lifetime suicide ideation, and 13 (2.32%) students had suicidal ideation within the last 12 months—from those students, seven (1.28%) had a suicide attempt within the last 3 months—and 209 (38.14%) students had depression symptoms (Table 2).
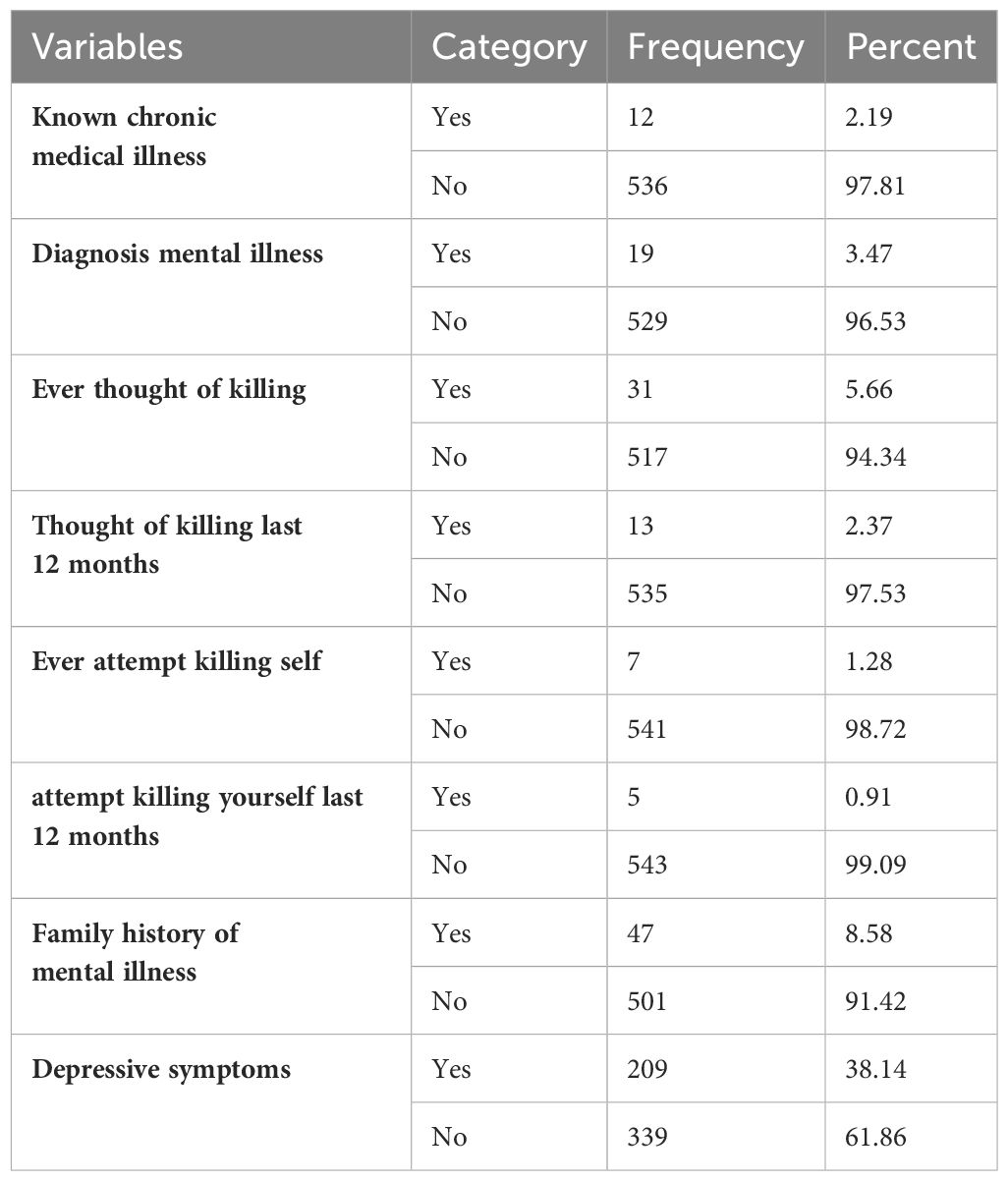
Table 2 Clinical characteristics of the participants among high school students at Finote Selam town (n = 548), 2023.
Substance-related factors of the respondents
Regarding substance use, out of out of 548 students, 86 (89.58%) had drunk alcohol at least once in their lifetime, whereas khat and cigarette lifetime users were seven (7.29%) and three (3.13%), respectively. Within the last 3 months, the total number of respondents who used alcohol was 26 (100%) (Table 3).
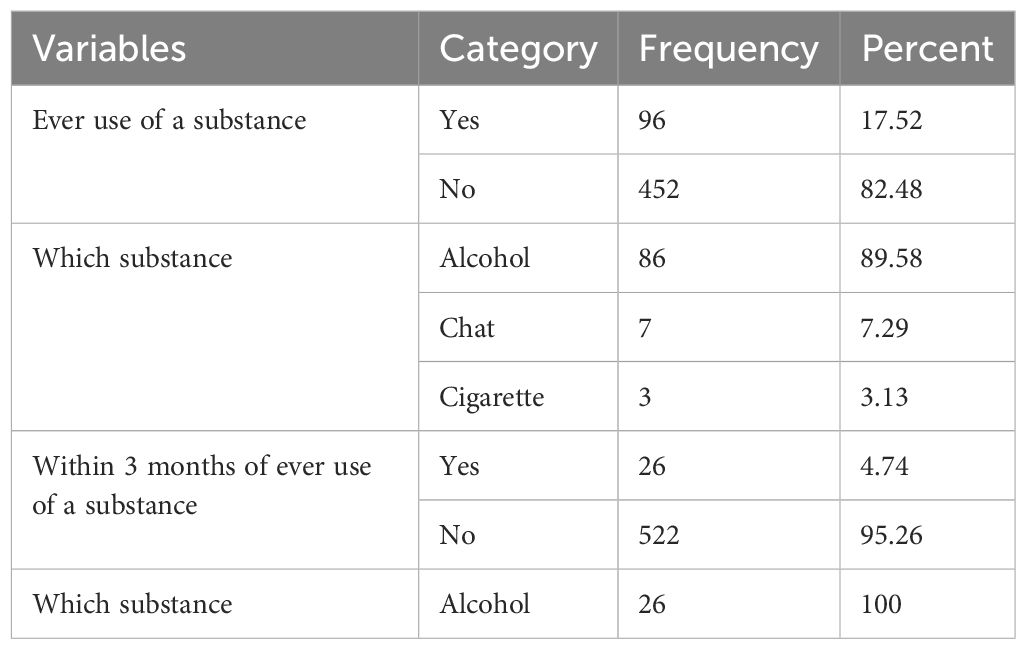
Table 3 Substance-related description of the participants among high school students in Finote Selam town (n = 548), 2023.
Psychosocial-related factors of the respondents
Regarding social support factors, among the total participants, 165 (30.11%) had poor social support, 308 (56.20%) had moderate social support, and 75 (13.69%) had strong social support (Figure 1).
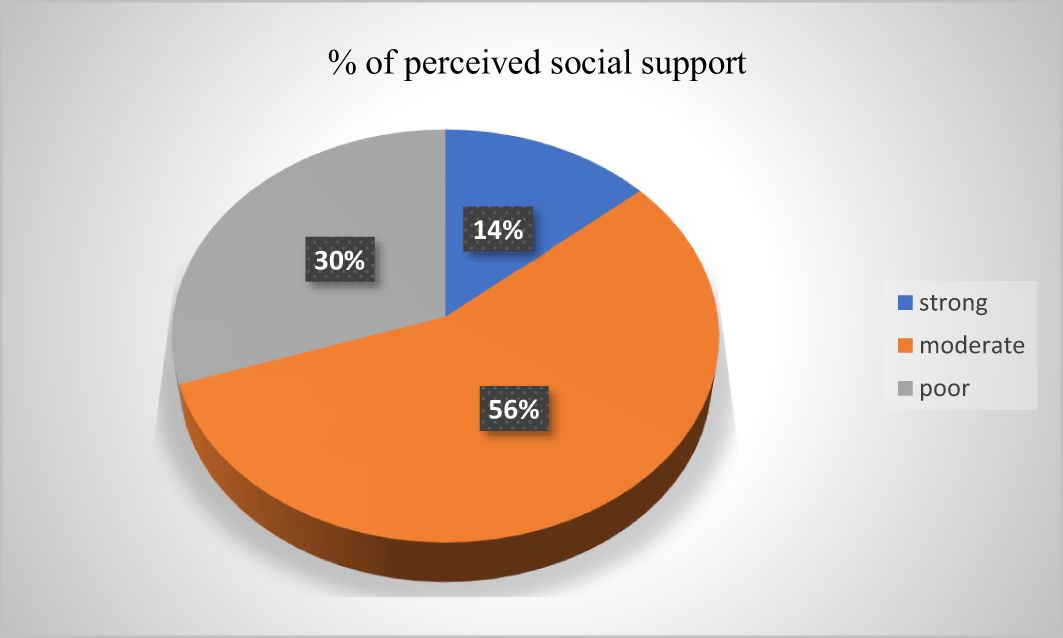
Figure 1 Psycho-social characteristics of participants among high school students in Finote Selam town (n = 548), 2023.
Regarding perceived stress factors, from the total participants, 324 (59.12%) had low stress,176 (32.12%) had moderate stress, and 48 (8.7%) had high stress (Figure 2).
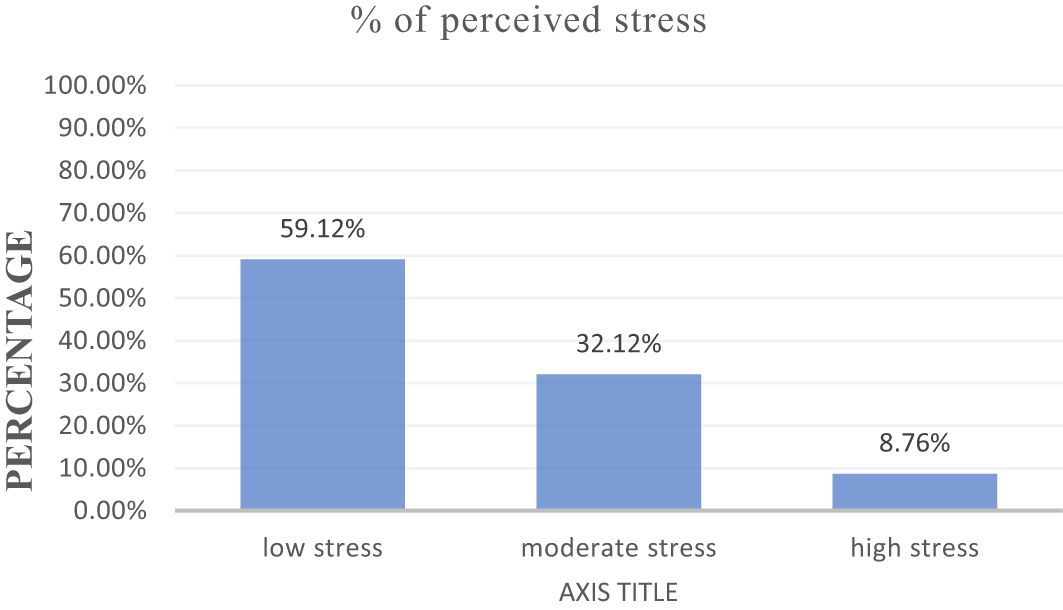
Figure 2 Perceived stress characteristics of low “felt” stress (0 to 13), moderate “felt” stress (14 to 26), and high “felt” stress (27 to 40) among high school in Finote Selam town (n = 548), 2023.
Gynecological and obstetric characteristics of the respondents
Of the total participants, 386 (67.15%) had menses that started at the age of 13 to 16 years, and more than half of the respondents, 304 (55.47%), had irregular menstruation periodicity. There were 447 (81.57%) students who reported to have menstrual pain from those, 172 (31.39%) had a long duration of menstruation bleeding, 158 (28.83%) had severe menstrual pain, 214 (39.05%) perceived that the menstrual pain had an impact on their academic performance, and 356 (64.96%) missed their class at least once in their school. A total of 115 (20.99%) respondents had a family history of menstrual-related problems. Of the total respondents, 217 (39.60) used greater than four pads during the menstrual period; those were high amounts of menstrual bleeding. Students who had menstrual pain used different pain management techniques: non-prescribed pain killer for 122 (22.26%), hot drinks for 362 (66.06%), massage for nine (1.64%), and consultation for 55 (10.04%) (Table 4).
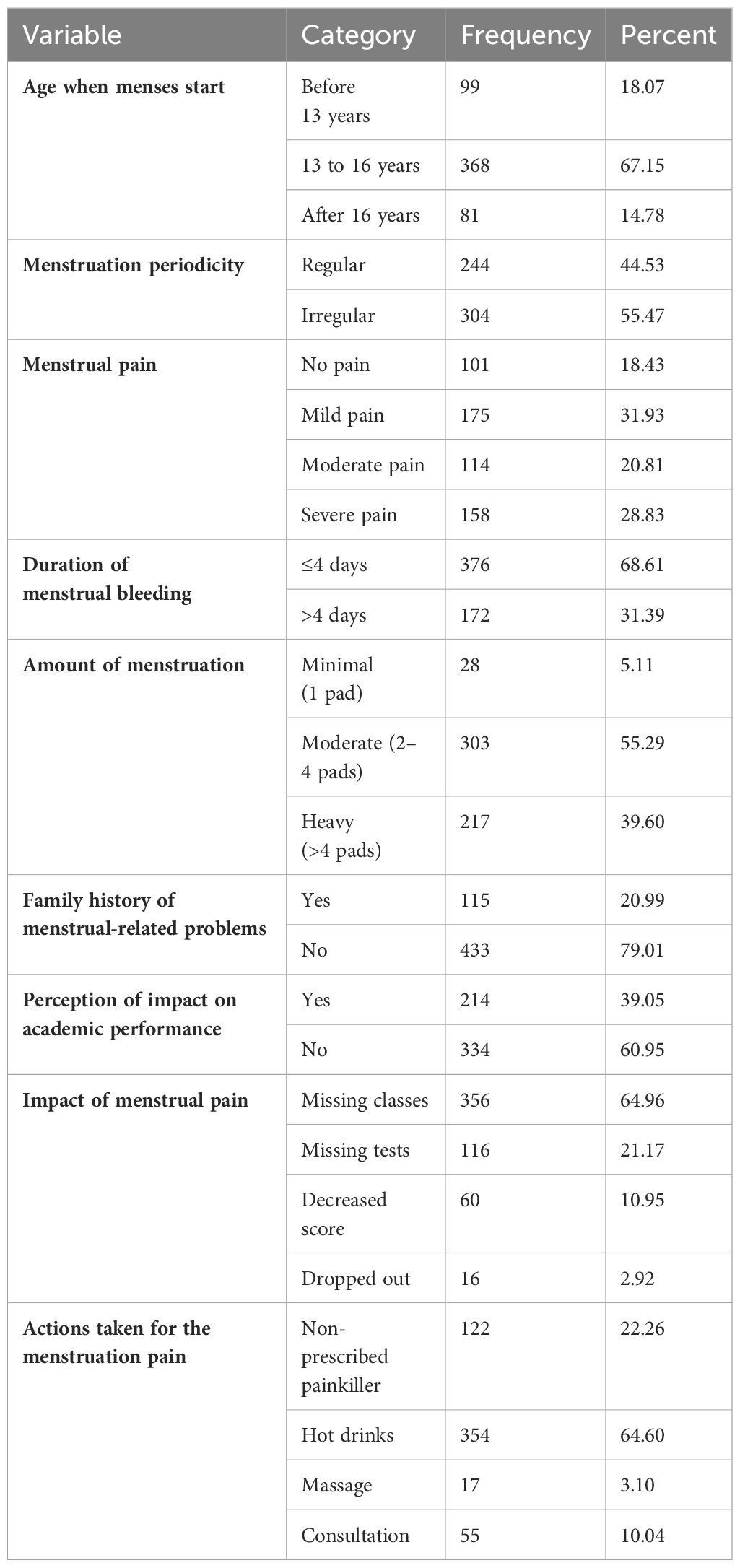
Table 4 Description of the gynecological and obstetric factors of the participants among high school students in Finote Selam town (n = 548), 2023.
Prevalence of premenstrual dysphoric disorder
In this study, the overall prevalence of premenstrual dysphoric disorder among high school students was 33.03% (181) (95%CI: 29.20–37.09). The most commonly reported symptom was physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “‘bloating,” and weight gain (55.39%), followed by being easily fatigued or a marked lack of energy (48.36%) (Table 5).

Table 5 Frequency distribution of DSM-5 criteria to assess premenstrual dysphoric symptoms among high school students in Finote Selam town (n = 548), 2023.
Factors associated with premenstrual dysphoric disorder
In a univariable logistic regression analysis, the factors that fulfilled a p-value less than 0.2 were starting age of menses at 13 to 16 years old, menstrual pain, amount of menstruation bleeding, duration of menstruation bleeding days, menstruation periodicity, family history menstruation related problem, perception impact of menstruation pain, perceived stress, having depression symptoms, and treatment seeking behavior. Finally, a multivariable analysis revealed that irregular menstrual cycle, having depressive symptoms, high perceived stress, and duration of menstruation bleeding greater than 4 days were found to be significantly associated with PMDD with 95%CI and at a p-value less than or equal to 0.05.
Those who had an irregular menstruation cycle were about (AOR = 4.242, 95%CI = 2.182–8.246) four times more likely to develop PMDD compared with those who had a regular menstruation cycle, and students who had depressive symptoms were about (AOR = 5.272, 95%CI = 2.779–10.002) five times to develop PMDD when compared to students who had no depression. Another associated factor with PMDD was having greater than 4 days of menstruation duration, which is (AOR = 2.138, 95%CI = 1.105, 4.138) two times more odds of having PMDD than those who had less than 4 days of menstruation duration. Students who had high perceived stress were about (AOR = 3.468, 95%CI = 1.217–9.880) 3.5 times to develop PMDD compared to those with low perceived stress (Table 6).
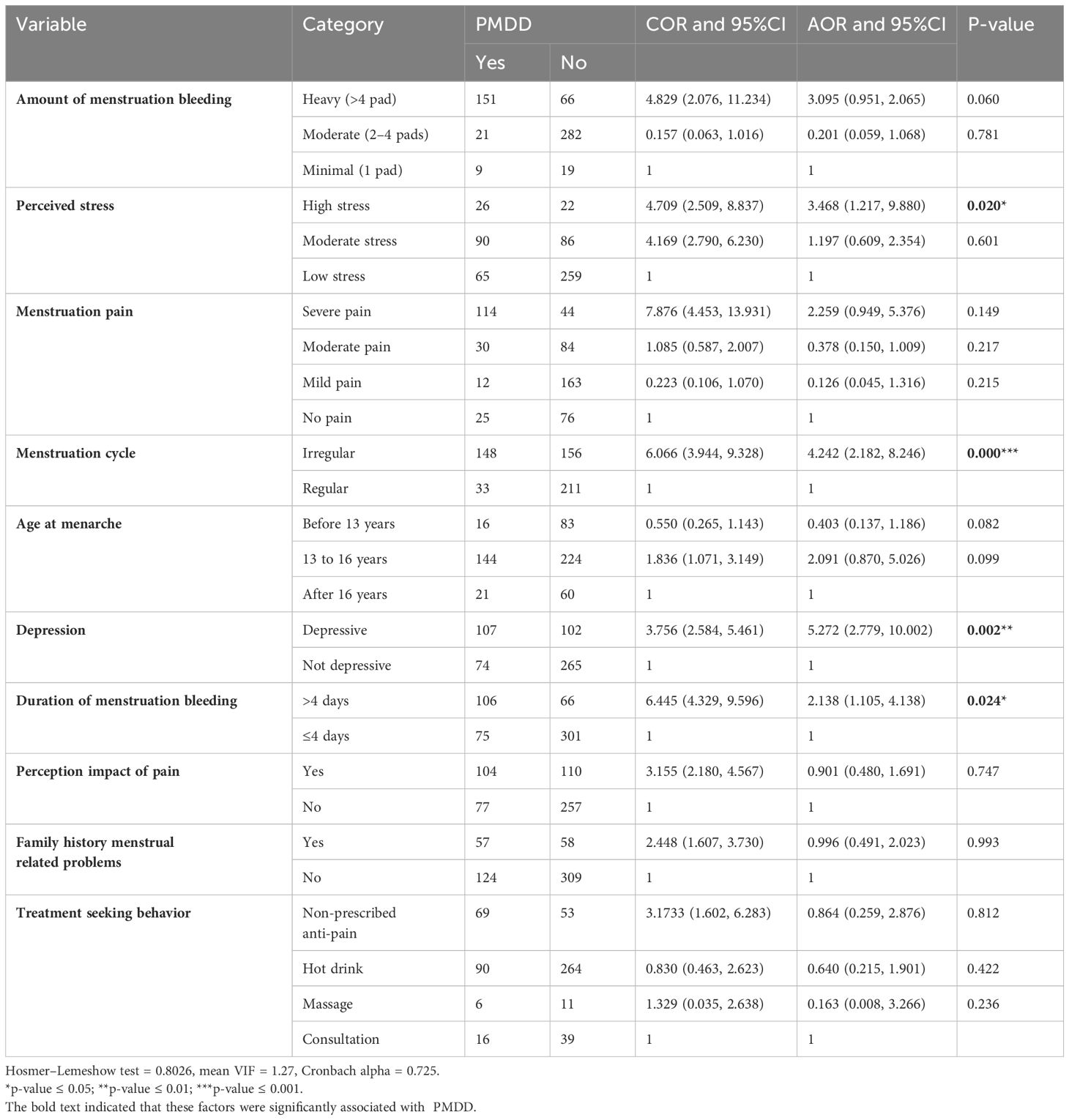
Table 6 Overall bivariable and multivariable logistic regression analysis of factors associated with premenstrual dysphoric disorder among high school students in Finote Selam town (n = 548), 2023.
Discussion
Premenstrual dysphoric disorder has a negative impact on social interaction and educational achievement by increasing school absenteeism. Because of premenstrual symptoms, students prevent the participants from going to school due to their ignorance of menstruation, and women experience a range of feelings during menarche, including fear, embarrassment, and guilt (31). Those symptoms persist for days to a week: breast tenderness or swelling, joint or muscle pain, a sensation of “bloating,” weight gain, easily fatigued or a marked lack of energy, and difficulty in concentrating. As a result, it is important to ascertain the prevalence of PMDD and identify the risk factors for it. Additionally, this would aid in problem prevention and the development of treatment plans that support female high school students’ academic success.
This study found that the prevalence of PMDD among female high school students was 33.03% (95%CI: 29.20—37.09). This is consistent with other studies done in Ethiopia reported to be 30.9% in Mekelle High School (6) and 34.7% in the University of Gondar (19). Another study in Africa was consistent with this study at Nigeria University (36.1%) (5).
However, the prevalence of premenstrual dysphoric disorder in this study was higher than the previous research findings in Ethiopian students whose prevalence at Debr Berhan University was 13.8% (30) and at Assosa Technical Training College was 26.8% (32). The study’s variation may be due to differences in the study population, with younger individuals more likely to experience premenstrual dysphoric disorder, while older students are less susceptible (33).
The current premenstrual dysphoric disorder prevalence was also higher in studies done in Egypt University (21.1%) (10) and South Africa University (10.2%) (34). The discrepancy might be the difference in the study population as well as sociocultural and socioeconomic characteristics. In Ethiopia, high school students reach puberty and start menstruating often without adequate information and have no psychological readiness to manage it, causing the onset of menstruation (menarche) to be shocking for girls. In high school, the lack of information is accompanied by a lack of access to appropriate sanitary wear and proper facilities for managing menstruation (35).
The finding of the current study was also higher in studies conducted at Kuwait University (5.6%) (36), at Jordan University (7.7%) (37), in Vietnam high schools (1.0%) (38), in Korea (2.4%) (39), in India high schools (4.89%) (40), in Japan high schools (3.1%) (41), among Iran high school students (12.22%) (42), and in Germany (5.8%) (43) as well as with American rates of 6% and 4.7% PMDD, respectively (44, 45). The possible reason for the variation may be differences in socioeconomic determinants. This means that, in developed countries, there are good sanitary products, adequate water supply, and privacy for changing sanitary pads, which continue to leave high school students unlimited options for safe and sufficient menstrual hygiene in high-income settings. Because of this reason, female students in menstruation will feel less shame, self-isolation, irritability, emotional liability, headaches, anxiety, depression, and traumatic experiences (46). Furthermore, the availability of health facilities between those countries and Ethiopia could be poor due to poor healthcare infrastructure and a shortage of trained health staff, which would lead to the delivery of inadequate healthcare services. In turn, premenstrual dysphoric disorder might not be identified and treated early.
In terms of sociocultural aspects, in Ethiopia, there is also a common belief (more commonly held by men) that menstruation does not start until a girl has a sexual intercourse for the first time (31). The existence of this false belief presents a potential hazard for girls approaching menarche if they live in families where this belief is held. The beginning of menses in girls is manifested when irritability, emotional liability, headaches, anxiety, depression, and traumatic experiences appear.
The other reason is that menstrual hygiene management is influenced by a variety of factors, including knowledge of reproductive biology, background beliefs about menstruation that are prevalent in societies, and the limitations that these beliefs place on female-related activities. Due to their confusion, embarrassment, and lack of preparation for the abrupt and unexpected onset of menstruation, adolescent girls may find it difficult to grow academically and socially due to menstrual hygiene management issues (47, 48). In terms of the type of study populations, between high school and university students, the latter have increased their knowledge about menstruation and experience of menses and thus have decreased behavioral changes due to menstruation.
On the other hand, the current study’s finding is lower than the previous study done at Ethiopian Wollo University (66.9%) (21). The discrepancy may be the fact that the study at Wolo University surveyed first year to fourth year students, primarily first year students. As students transition into higher education, they face challenges like integrating into university culture, socioeconomic issues, interpersonal problems, demanding course loads, and insufficient institutional support, making them vulnerable to stress and depression (49), which might increase the prevalence of PMDD.
The current study’s finding was also lower in studies conducted at Morocco University (55%) (50). The discrepancy might be due to the tools of assessment used in Morocco. The Moroccan high school students used the Daily Record of Severity of Problems (DRSP), but DRSP is a screening tool and not a diagnostic tool, and this might overestimate the prevalence of premenstrual dysphoric disorder among students (51). Moreover, the other discrepancy might be the sociocultural aspect since students in Ethiopia do not express their actual feelings related to premenstrual symptoms such as depressed mood, irritability, emotional, and somatic symptoms because of the culture of silence and associated stigma around menstruation; thus, this topic is not openly discussed at the family level. The abovementioned reason might be the reason for the lower prevalence of PMDD in this study (33).
Regarding factors affecting premenstrual dysphoric disorder, the duration of menstruation bleeding was significantly associated with a higher rate of premenstrual dysphoric disorder. The odds of premenstrual dysphoric disorder were two times among those students having longer durations of menstruation bleeding than students with shorter durations (<4 days). These findings were supported by other studies done among Mekelle high school students, Ethiopia (6), and among university students from Egypt (10) and Nigeria (5). The possible reason might be that having a long duration of menstruation bleeding days could cause fluctuations ranging from hormone-related issues like estrogen and progesterone that can increase the vulnerability to premenstrual dysphoric disorder because a drop in estrogen and progesterone may lead to a reduced level of serotonin, which can result in increased levels of sadness, anxiety, and irritability when women are on menses. Other reasons might be that, with a long duration of menstruation bleeding, students become absent from school and have decreased social interaction, which can increase the academic burden on students and which, in turn, can lead them to have low self-confidence and poor academic performance (31, 35, 52).
The present study also showed that premenstrual dysphoric disorder is significantly associated with high perceived stress among high school students. The odds of premenstrual dysphoric disorder were more than three times higher among students with high perceived stress than those without such stress. Similar findings were reported in the University of Gondar, Ethiopia, and Jordan (19, 53). The possible reason might be the development of anxiety and depressive symptoms like tension, a sense of difficulty in controlling one’s self, a depressed mood, and irritability resulting from people becoming more stressed, thus impairing their ability to concentrate in school.
The aggravation of cardinal mood symptoms may be caused by premenstrual symptoms like anger and irritability which are linked to stress-related premenstrual severity. Others claim that students with low-income levels had a higher perceived stress, which can indirectly affect the prevalence of PMDD compared to those with higher incomes. Furthermore, this may be due to believing that having a low income is a very stressful situation in life, making premenstrual symptoms more severe and prevalent (54, 55).
Students with irregular menstrual cycles had about four times higher odds of premenstrual dysphoric disorder than students with regular menstrual cycles. This finding is consistent with other findings at Assosa Technical Training College, Ethiopia (32). Students who experience irregular menstrual cycles may develop a premenstrual dysphoric disorder for various reasons, i.e., students may experience high rates of absenteeism from class due to irregularities of menstruation each month, premenstrual symptoms, a lack of attention to their problems, and a lack of confidence during bleeding, all impacting their capacity to learn (56).
Students with depressive symptoms had about five times higher odds of premenstrual dysphoric disorder as compared with those who had no depressive symptoms. This finding is consistent with findings from Nigeria University (5) and among Korean women (57). The possible reason could be that women have more depressive symptoms, such as different somatic and affective symptoms that interrupt their function, which can aggravate those somatic and affective symptoms like joint pain, irritability, lack of energy, depressed mood, and difficulty in concentrating during menstruation (58).
Strength and limitation of the study
We used an adequate sample for the study using an appropriate probability sampling technique and data collection procedure. However, there is recall bias—for example, age when menses started—, and the cross sectional study design by itself cannot assess the cause and effect relationship.
Conclusion
In this study, the magnitude of premenstrual dysphoric disorder was one-third among high school students, and it was higher compared to other studies. Long-duration menstruation periods, irregular menstruation cycles, high perceived stress, and depressive symptoms were factors significantly associated with PMDD among students. Therefore, it needs early screening and intervention in primary healthcare settings, especially for those who have high perceived stress, depressive symptoms, a long duration of menstruation bleeding, and an irregular menstruation cycle, so as for them to have good academic achievement and psychological wellbeing. Before menstrual symptoms can have an impact on students’ academic performance, early diagnosis and intervention are required. Stress reduction programs could be a useful non-pharmaceutical treatment for relieving psychological and physical symptoms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical review committee of the University of Gondar. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
GK: Writing – review & editing, Writing – original draft, Visualization, Supervision, Project administration, Methodology, Formal analysis, Conceptualization. DD: Software, Supervision, Writing – review & editing. SK: Writing – review & editing, Supervision, Software. SY: Writing – review & editing, Visualization, Supervision, Software. MK: Writing – review & editing, Visualization, Supervision, Investigation, Formal analysis. MM: Writing – review & editing, Methodology. GT: Writing – review & editing, Visualization, Supervision, Formal analysis. SF: Writing – review & editing, Visualization, Supervision, Software, Formal analysis. GN: Writing – review & editing, Visualization, Supervision, Software, Formal analysis. YW: Writing – review & editing, Methodology, Supervision, Visualization. TA: Writing – review & editing, Visualization, Methodology, Investigation, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the University of Gondar for giving ethical clearance. We would like to acknowledge the Education Bureau employees and the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PMDD, premenstrual dysphoric disorder; PMS, premenstrual syndrome; PSS-10, Perceived Stress Scale—10 items; AOR, adjusted odds ratio; ASSIST, Alcohol, Smoking, and Substance Involvement Screening Test; CI, confidence interval; COD, crude odd ratio; DSM, Diagnostic and Statistical Manual of Mental Disorders; WHO, World Health Organization.
References
1. Association AP. Diagnostic and statistical manual of mental disorders. Arlington: American Psychiatric Publishing (2013).
2. Dennerstein L, Lehert P, Heinemann K. Epidemiology of premenstrual symptoms and disorders. Menopause Int. (2012) 18:48–51. doi: 10.1258/mi.2012.012013
3. Ehalaiye B, Eigbefoh J, Eifediyi RA, Omorogbe F, Isabu PA, Ugiagbe OA, et al. Premenstrual syndrome: prevalence, pattern and severity among female university students in Ekpoma, Nigeria. Trop J Obstetrics Gynaecology. (2009) 26:142–50.
4. Adewuya A, Loto O, Adewumi T. Premenstrual dysphoric disorder amongst Nigerian university students: prevalence, comorbid conditions, and correlates. Arch Womens Ment Health. (2008) 11:13–8. doi: 10.1007/s00737-008-0213-4
5. Issa BA, Yussuf AD, Olatinwo AWO, Ighodalo M. Premenstrual dysphoric disorder among medical students of a Nigerian university. Ann Afr Med. (2010) 9. doi: 10.4103/1596-3519.68354
6. Mossie TB, Tesfaye YB, Metekiya WM, Tegegne MT. Magnitude of premenstrual dysphoric disorder and associated factors among high school girls, Mekelle, North Ethiopia. Ethiopian Journal of Health Development (2015) 29(3):170-5.
7. Tadesse MG, Dire DD, Abraham YY. Prevalence of premenstrial disphoric disorder associated factors among students of tabor secondary and preparatory school in Hawassa City, Ethiopia cross sectional. (2020). doi: 10.21203/rs.3.rs-35797/v1
8. Branecka-Woźniak D, Cymbaluk-Płoska A, Kurzawa R. The impact of premenstrual syndrome on women’s quality of life–a myth or a fact? Eur Rev Med Pharmacol Sci. (2022) 26:598–609.
9. Petersen N, London ED, Liang L, Ghahremani DG, Gerards R, Goldman L, et al. Emotion regulation in women with premenstrual dysphoric disorder. Arch Women's Ment Health. (2016) 19:891–8. doi: 10.1007/s00737-016-0634-4
10. Eldeeb SM, Eladl AM, Elshabrawy A, Youssef AM, Ibrahim MH. Prevalence, phenomenology and personality characteristics of premenstrual dysphoric disorder among female students at Zagazig University, Egypt. Afr J Primary Health Care Family Med. (2021) 13:2924. doi: 10.4102/phcfm.v13i1.2924
11. Prasad D, Wollenhaupt-Aguiar B, Kidd KN, de Azevedo Cardoso T, Frey BN. Suicidal risk in women with premenstrual syndrome and premenstrual dysphoric disorder: a systematic review and meta-analysis. J Women's Health. (2021) 30:1693–707. doi: 10.1089/jwh.2021.0185
12. Baca-García E, González AS, Diaz-Corralero PG, García IG, De Leon J. Menstrual cycle and profiles of suicidal behaviour. Acta Psychiatrica Scandinavica. (1998) 97:32–5. doi: 10.1111/j.1600-0447.1998.tb09959.x
13. Takeda T, Tasaka K, Sakata M, Murata Y. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in Japanese women. Arch Women's Ment Health. (2006) 9:209–12. doi: 10.1007/s00737-006-0137-9
14. Harrison WM, Endicott J, Nee J, Glick H, Rabkin JG. Characteristics of women seeking treatment for premenstrual syndrome. Psychosomatics. (1989) 30:405–11. doi: 10.1016/S0033-3182(89)72246-5
15. Wang M, Seippel L, Purdy RH, Bãckström T. Relationship between symptom severity and steroid variation in women with premenstrual syndrome: study on serum pregnenolone, pregnenolone sulfate, 5 alpha-pregnane-3, 20-dione and 3 alpha-hydroxy-5 alpha-pregnan-20-one. J Clin Endocrinol Metab. (1996) 81:1076–82. doi: 10.1210/jcem.81.3.8772579
16. Dutta A, Sharma A. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in India: A systematic review and meta-analysis. Health promotion perspectives. (2021) 11:161. doi: 10.34172/hpp.2021.20
17. Duko B, Mekuriaw B, Molla A, Ayano G. The prevalence of premenstrual dysphoric disorder among adolescents in Ethiopia: a systematic review and meta-analysis. Irish J Med Sci (1971-). (2021) 190:419–27. doi: 10.1007/s11845-020-02275-7
18. Jember D, Duko B, Mihretie G. Premenstrual dysphoric disorder among assosa techinical premenstrual & Vocational education school students, assosa, Ethiopia. J Psychiatry. (2017) 20:2.
19. Minichil W, Eskindir E, Demilew D, Mirkena Y. Magnitude of premenstrual dysphoric disorder and its correlation with academic performance among female medical and health science students at University of Gondar, Ethiopia, 2019: a cross-sectional study. BMJ Open. (2020) 10:e034166. doi: 10.1136/bmjopen-2019-034166
20. Patil R, Patil T, Chaudhary A, Maldhure S, Gulhane R. Premenstrual dysphoric disorder-its prevalence and associated factors in nursing staff of medical college of central India. NVEO-NATURAL VOLATILES ESSENTIAL OILS Journal| NVEO. (2021) 24: 1359–64.
21. Tsegaye D, Getachew Y. Premenstrual dysphoric disorder and associated factors among female health science students in Wollo University, Ethiopia, 2017/18. Maternal Health Neonatology Perinatology. (2019) 5:1–8. doi: 10.1186/s40748-019-0102-z
22. Mossie TB, Tesfye YB, Metekiya WM, Tegegne MT. Magnitude of premenstrual dysphoric disorder and associated factors among high school girls, Mekelle, North Ethiopia. Ethiopian J Health Dev. (2009) 23.
23. Tsegaye D, Getachew Y. Premenstrual dysphoric disorder and associated factors among female health science students in Wollo University, Ethiopia, 2017/18. Maternal Health, Neonatology and Perinatol. (2019) 5(1):1–8. doi: 10.1186/s40748-019-0102-z
24. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
25. Padhy SK, Sarkar S, Beherre PB, Rathi R, Panigrahi M, Patil PS. Relationship of premenstrual syndrome and premenstrual dysphoric disorder with major depression: relevance to clinical practice. Indian J psychol Med. (2015) 37:159–64. doi: 10.4103/0253-7176.155614
26. Dowrick C, Shiels C, Page H, Ayuso-Mateos J, Casey P, Dalgard O, et al. Predicting long-term recovery from depression in community settings in Western Europe: evidence from ODIN. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:119–26. doi: 10.1007/s00127-009-0179-1
27. Newcombe D, Tanielu-Stowers H, McDermott R, Stephen J, Nosa V. The validation of the alcohol, smoking and substance involvement screening test (ASSIST) amongst Pacific people in New Zealand. NZJ Psychol. (2016) 45. doi: 10.1037/t57104-000
28. Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. (2008) 103:1039–47. doi: 10.1111/j.1360-0443.2007.02114.x
29. Ameade EK, Mohammed BS. Menstrual pain assessment: comparing verbal rating scale (VRS) with numerical rating scales (NRS) as pain measurement tools. (2016). doi: 10.23937/2474-1353
30. Alemu SM, Habtewold TD, Haile YG. Mental and reproductive health correlates of academic performance among Debre Berhan university female students, Ethiopia: the case of premenstrual dysphoric disorder. BioMed Res Int. (2017) 2017. doi: 10.1155/2017/9348159
31. Tegegne TK, Sisay MM. Menstrual hygiene management and school absenteeism among female adolescent students in Northeast Ethiopia. BMC Public Health. (2014) 14(1):1–14. doi: 10.1186/1471-2458-14-1118
32. Jember D, Duko B, Mihretie G. Premenstrual dysphoric disorder among female students at assosa techinical & Vocational education training school, assosa, Ethiopia. Prevalence. (2017) 16:17.
34. Roomaney R, Lourens A. Correlates of premenstrual dysphoric disorder among female university students. Cogent Psychol. (2020) 7:1823608. doi: 10.1080/23311908.2020.1823608
35. Bulto GA. Knowledge on menstruation and practice of menstrual hygiene management among school adolescent girls in Central Ethiopia: a cross-sectional study. Risk Manag Healthc Policy. (2021) 14:911–23. doi: 10.2147/RMHP.S296670
36. Omu FE, Al-Marzouk R, Delles H, Oranye NO, Omu AE. Premenstrual dysphoric disorder: prevalence and effects on nursing students’ academic performance and clinical training in Kuwait. J Clin Nurs. (2011) 20:2915–23. doi: 10.1111/j.1365-2702.2011.03708.x
37. Shehadeh JH, Hamdan-Mansour AM. Prevalence and association of premenstrual syndrome and premenstrual dysphoric disorder with academic performance among female university students. Perspect Psychiatr Care. (2018) 54:176–84. doi: 10.1111/ppc.2018.54.issue-2
38. Dinh Trieu Ngo V, Bui LP, Hoang LB, Tran MTT, Nguyen HVQ, Tran LM, et al. Associated factors with Premenstrual syndrome and Premenstrual dysphoric disorder among female medical students: A cross-sectional study. PloS One. (2023) 18:e0278702. doi: 10.1371/journal.pone.0278702
39. Rapkin AJ, Korotkaya Y, Taylor KC. Contraception counseling for women with premenstrual dysphoric disorder (PMDD): current perspectives. Open Access J Contraception. (2019) 10:27–39. doi: 10.2147/OAJC
40. Pattanashetty NO, Mugali J, Niharika H. Prevalence of premenstrual dysphoric disorder among high school girls of Gadag district, Karnataka, India-a school-based cross-sectional study. Kerala J Psychiatry. (2021) 34:90–5. doi: 10.30834/KJP.34.2.2021.273
41. Tadakawa M, Takeda T, Monma Y, Koga S, Yaegashi N. The prevalence and risk factors of school absenteeism due to premenstrual disorders in Japanese high school students—a school-based cross-sectional study. BioPsychoSocial Med. (2016) 10:1–7. doi: 10.1186/s13030-016-0067-3
42. Boustani F, Ziagham S, Jahangirimehr A, Honarmandpour A. Prevalence of premenstrual syndrome, premenstrual dysphoric disorder and associated factors among female high school students. J Inflammatory Diseases. (2019) 23:332–41. doi: 10.32598/JQUMS
43. Wittchen H-U, Becker E, Lieb R, Krause P. Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. psychol Med. (2002) 32:119–32. doi: 10.1017/S0033291701004925
44. Sveindóttir H, Bäckström T. Prevalence of menstrual cycle symptom cyclicity and premenstrual dysphoric disorder in a random sample of women using and not using oral contraceptives. Acta obstetricia gynecologica Scandinavica. (2000) 79:405–13. doi: 10.1080/j.1600-0412.2000.079005405.x
45. Chawla A, Swindle R, Long S, Kennedy S, Sternfeld B. Premenstrual dysphoric disorder: is there an economic burden of illness? Med Care. (2002) 40:1101–12. doi: 10.1097/00005650-200211000-00011
46. Bajracharya S, Baniya A. Awareness of menstrual hygiene among adolescent girls at a government school, Chitwan, Nepal. J Chitwan Medical College. (2022) 12(2):14–8. doi: 10.54530/jcmc.652
47. Alam M-U, Luby SP, Halder AK, Islam K, Opel A, Shoab AK, et al. Menstrual hygiene management among Bangladeshi adolescent schoolgirls and risk factors affecting school absence: results from a cross-sectional survey. BMJ Open. (2017) 7(7):. doi: 10.1136/bmjopen-2016-015508
48. Biruk E, Tefera W, Tadesse N, Sisay AJB. Assessment of menstrual hygiene management and its determinants among adolescent girls: A cross-sectional study in school adolescent girls in Addis Ababa, Ethiopia. bioRxiv. (2018) 450007. doi: 10.1101/450007
49. Henok Shiferaw N, Anand S, Gugsa Nemera N. Stress and coping strategies among generic B. Sc. nursing students of Jimma University, South West Ethiopia. Int J Recent Adv Multidiscip Res. (2015) 2(7):511–7.
50. Belakbir O, Rhaouti A, Belbachir S, Ouanass A. Characteristics of premenstrual dysphoric disorder in moroccan women: A cross-sectional study. Sch J Med Case Rep. (2022) 11:1108–14. doi: 10.36347/sjmcr.2022.v10i11.011
51. Endicott J, Nee J, Harrison W. Daily Record of Severity of Problems (DRSP): reliability and validity. Arch Womens Ment Health. (2006) 9:41–9. doi: 10.1007/s00737-005-0103-y
52. Belayneh Z, Mekuriaw B. Knowledge and menstrual hygiene practice among adolescent school girls in southern Ethiopia: a cross-sectional study. BMC Public Health. (2019) 19:1–8. doi: 10.1186/s12889-019-7973-9
53. Hamaideh S, Al-Ashram S, Al-Modallal H. Premenstrual syndrome and premenstrual dysphoric disorder among J ordanian women. J Psychiatr Ment Health nursing. (2014) 21:60–8. doi: 10.1111/jpm.12047
54. Gupta M, Dua D, Kaur H, Grover S. Prevalence of premenstrual dysphoric disorder among school-going adolescent girls. Ind Psychiatry J. (2019) 28(2):198. doi: 10.4103/ipj.ipj_79_19
56. West S, Lashen H, Bloigu A, Franks S, Puukka K, Ruokonen A, et al. Irregular menstruation and hyperandrogenaemia in adolescence are associated with polycystic ovary syndrome and infertility in later life: Northern Finland Birth Cohort 1986 study. Hum. Reprod (2014) 29(10):2339–51. doi: 10.1093/humrep/deu200
57. Hong JP, Park S, Wang H-R, Chang SM, Sohn JH, Jeon HJ, et al. Prevalence, correlates, comorbidities, and suicidal tendencies of premenstrual dysphoric disorder in a nationwide sample of Korean women. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1937–45. doi: 10.1007/s00127-012-0509-6
Keywords: premenstrual dysphoric disorder, high school students, prevalence, associated factors, Ethiopia
Citation: Kibralew G, Demilew D, Koye S, Yitayih S, Kelebie M, Melkam M, Tadesse G, Fentahun S, Nakie G, Wassie YA and Amare T (2024) Prevalence and associated factors of premenstrual dysphoric disorder among high school students in Finote Selam town, northwest Ethiopia. Front. Psychiatry 15:1362118. doi: 10.3389/fpsyt.2024.1362118
Received: 27 December 2023; Accepted: 22 May 2024;
Published: 21 June 2024.
Edited by:
Karen Tabb, University of Illinois at Urbana-Champaign, United StatesReviewed by:
Samaneh Torkian, Iran University of Medical Sciences, IranJohn M. Davis, University of Illinois Chicago, United States
Copyright © 2024 Kibralew, Demilew, Koye, Yitayih, Kelebie, Melkam, Tadesse, Fentahun, Nakie, Wassie and Amare. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getasew Kibralew, d2FsZWxpZ25lZ2V0YXNld0BnbWFpbC5jb20=; R2V0YXNldy5LaWJyYWxld0B1b2cuZWR1LmV0
 Getasew Kibralew
Getasew Kibralew Demeke Demilew1
Demeke Demilew1 Mulualem Kelebie
Mulualem Kelebie Gebresilassie Tadesse
Gebresilassie Tadesse Setegn Fentahun
Setegn Fentahun Girum Nakie
Girum Nakie Yilkal Abebaw Wassie
Yilkal Abebaw Wassie