- 1Department of Human Physiology, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Department of Human Physiology, College of Medicine and Health Sciences, Ambo University, Ambo, Oromia Region, Ethiopia
Background: The conflict between the Ethiopian government and the Tigray People’s Liberation Front (TPLF) in the Dabat district of Ethiopia has led to significant civilian casualties, instances of rape, sexual abuse, and property theft. These traumatic events contribute to the development of post-traumatic stress disorder (PTSD) among local residents. However, there is currently no available data on the prevalence of PTSD and its associated factors in this region. This study seeks to fill this gap by assessing PTSD prevalence and identifying related factors among residents of the war-affected Dabat district in northwest Ethiopia.
Method: A community-based correctional study was conducted in the Woken and China kebeles of Dabat district, northwest Ethiopia, spanning from July 13 to September 19, 2023. A total of 410 participants were selected using systematic random sampling, making a 100% response rate. The study utilized an interviewer-administered questionnaire, which included the Post-Traumatic Stress Disorder Checklist (PCL-5) to assess PTSD. The research investigated the association between PTSD and various demographic and psychosocial characteristics using both bivariate and multivariable binary logistic regression analyses. Statistical significance was set at a P-value of 0.05.
Results: The majority of participants in the study were male (62%) with a mean age of 33 ( ± 1.67) years. The overall prevalence of PTSD was 30.7% (95% CI: 26.6–35.10). Multivariable logistic regression analysis identified several factors significantly associated with PTSD: symptoms of depression (AOR=3.5; 95% CI: 1.13-6.89), age between 45 and 67 years (AOR=1.68; 95% CI: 1.04-5.78), experiencing stressful life events (AOR=1.63; 95% CI: 1.05-7.86), experiencing sexual abuse or rape (AOR=1.53; 95% CI: 1.07-6.75), chewing khat (AOR=1.48; 95% CI: 1.08-4.56), being female (AOR=1.43; 95% CI: 1.13-3.67), and having an income of 34.6 USD (AOR=1.28; 95% CI: 1.07-4.67).
Conclusion and recommendation: This study reported that the prevalence of PTSD was high. As a result, the study suggested that governments and other stakeholders should be involved in implementing efficient interventions and quick measures to mitigate the effects of war on mental health following the conflict. The government and nongovernmental organizations were also advised by these studies to continue providing humanitarian assistance, which should include access to food, clean water, clothing, shelter, and education. This study also suggested that people living in conflict zones should be legally protected from rape, sexual abuse, arson, detention without cause, and kidnapping.
Introduction
The Tigray conflict in Ethiopia lasted from November 2020 to November 2022 and was mainly concentrated in the Tigray region (1). It involved the Ethiopian federal government and the Tigray People Liberation Front. The Ethiopian government declared war following accusations of Tigray forces attacking its northern command base (2). The conflict, which initially started in Tigray, later extended to neighbouring regions like Afar and Amhara, impacting over 20 million people, predominantly women and children. Approximately 5.5 million individuals were displaced, fleeing to other parts of Ethiopia (3). The situation, particularly in Dabat District in northwest Ethiopia, worsened displacement, exposing many to homelessness and various criminal acts, including murder, sexual abuse, rape, and abduction. This significantly increased the risk of posttraumatic stress disorder among those affected.
Posttraumatic stress disorder is a highly prevalent mental disorder in war-affected areas or natural disasters (4–6). Posttraumatic stress disorder can result from experiencing or witnessing distressing events such as murder, threats, kidnapping, loss of loved ones, displacement from one’s home, and deprivation of basic needs such as food (7). It manifests symptoms such as nightmares and flashbacks, avoiding triggers connected to trauma, elevated alertness, and detrimental cognitive alterations (8). Post-war settings are frequently characterized by instability, peril, and a scarcity of humanitarian aid, factors that may contribute to the onset of posttraumatic symptoms (9, 10). In the absence of effective management, Posttraumatic stress disorder can lead to a deterioration in quality of life, disruptions in daily functioning, and, in severe cases, even mortality (11).
Posttraumatic stress disorder is more prevalent in low- and middle-income countries where mental health services are often less accessible (12). Worldwide, the documented prevalence of Posttraumatic stress disorder among global populations affected by war is 12.9% (13). There is significant regional variation in Posttraumatic stress disorder prevalence, ranging from 0.3% to 8.7% (14, 15). A systematic review across 40 nations found that 30.6% of internally displaced individuals affected by war experienced Posttraumatic stress disorder (16). War-affected regions of sub-Saharan Africa also show high rates, with reported prevalence reaching up to 30% (17). In Uganda, Posttraumatic stress disorder prevalence is identified at 11.8% In Uganda (18), whereas in Kenya, it notably rises to 62.1% (18), South Sudan has reported a prevalence of 28% (19). Within Ethiopia, there is significant variation in Posttraumatic stress disorder rates: Addis Ababa reports a lower rate of 3.7% (20), while Dessie reports a higher prevalence of 34.5% (5).
Several factors contribute to the development of posttraumatic stress disorder following exposure to wartime trauma. These factors include age, gender, experiences of potentially traumatic events during and after the war, unemployment, lower educational levels, and the presence of chronic diseases (19, 21–23).
Limited information exists regarding the prevalence of mental disorders, particularly posttraumatic stress disorder, among individuals directly involved in armed conflicts in low- and middle-income countries such as Ethiopia. However, a substantial number of individuals in such contexts are vulnerable to various mental health challenges due to their exposure to conflict-related trauma (24, 25). In the Dabat district of Ethiopia, a substantial conflict involving the Ethiopian government and the TPLF erupted, leading to numerous civilian casualties, incidents of rape and sexual abuse, cessation of hostilities, and property theft. These traumatic events may have contributed to the development of posttraumatic stress disorder among the affected population. However, available data on the prevalence of posttraumatic stress disorder and its associated risk factors among individuals residing in conflict-affected areas post-war are lacking. Therefore, this study aimed to investigate the extent of posttraumatic stress disorder and identify factors associated with it. The findings from this research have the potential to inform the government and other stakeholders, guiding them in implementing interventions and appropriate actions to address the lingering issues following the war.
Methods
Study area and period
This study was conducted in Woken and China Kebeles, which are located in the Dabat district of the Amhara regional state in Northwest Ethiopia, spanning from July 13 to September 19, 2023. The Dabat district is located approximately 775 kilometres away from Addis Ababa. These two kebeles comprise 2000 households with a total population of 8,000. Unfortunately, during the study period, China and Woken Kebeles became battlegrounds between the Tigray People’s Liberation Front and Ethiopian government forces. The Amhara Media Corporation documented that China and Woken Kebeles witnessed the tragic loss of hundreds of civilians, either through massacres or shelling. Furthermore, many residents endured severe hardships, including instances of sexual abuse and rape.
Study design and population
A community-based cross-sectional study was carried out within war-affected regions of the Dabat district, specifically in China and Woken Kebeles. The source population consisted of adult residents aged 18 and above living in China and Woken Kebeles, who had been residing in the two kebeles for at least six months. However, the target population or study population included all adult individuals aged 18 years and above who presented themselves during the data collection period.
Sample size calculation
By applying a single proportion population formula, the sample size was determined using the estimated prevalence rate of PTSD, which was 58.4%, as identified in a study conducted in southern Ethiopia (26).
With the 10% nonresponse rate added, the total sample size was 412 with a 5% margin of error, a 95% confidence level, and a 10% nonresponse rate.
Sampling technique and procedure
Participants for the study in both China and Woken Kebeles were recruited using a systematic random sampling technique. Initially, the number of households and the total population were determined for both kebeles. Then, 30% of households were selected from each kebele. Proportional allocation was applied to the selected households. Finally, the sampled population was chosen through a systematic random sampling technique after proportional allocation (refer to Figure 1).
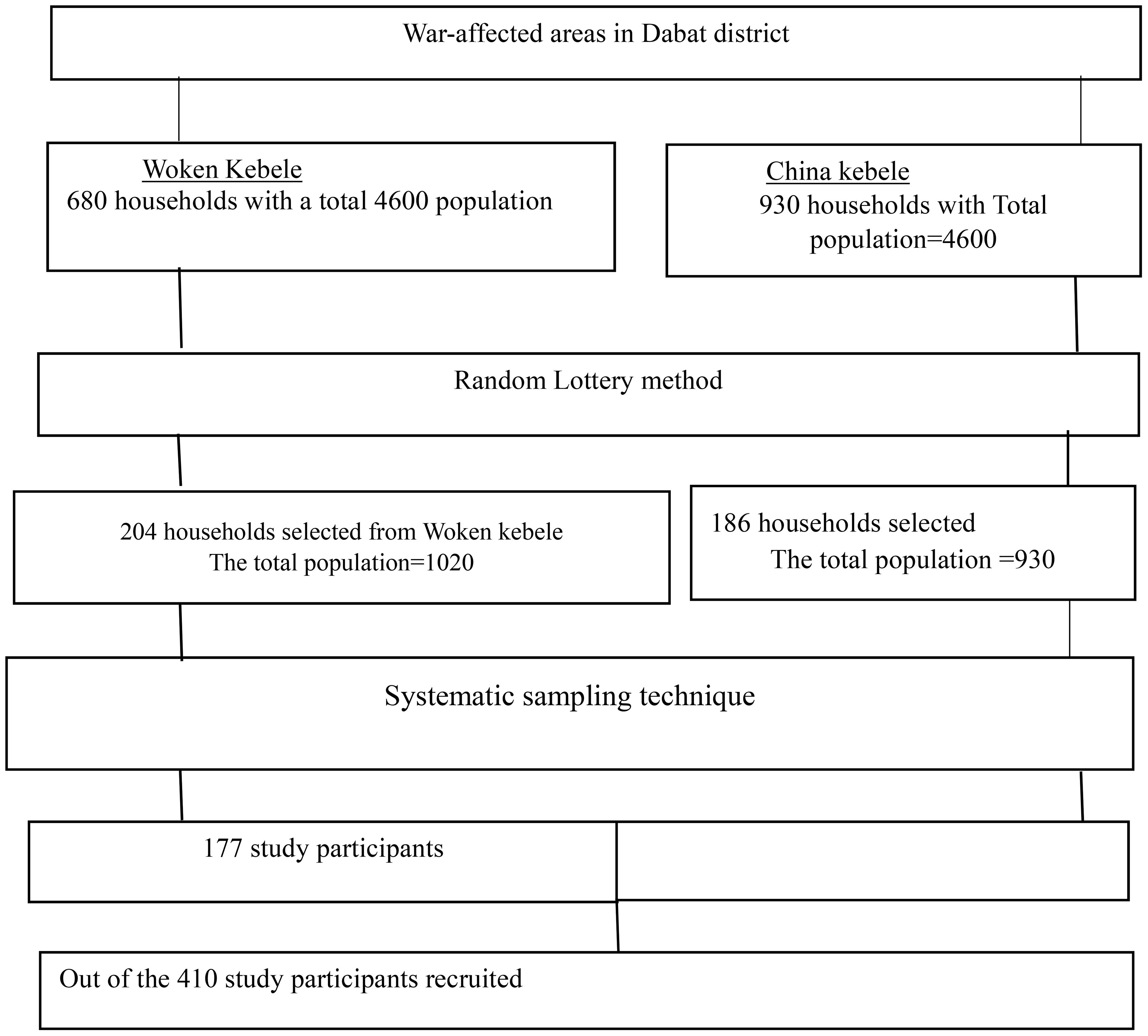
Figure 1 sampling procedure for the war-affected area in the Dabat district, northwest Ethiopia, 2023.
Eligibility criteria and study variables
The inclusion criteria for this study included all adult individuals aged 18 years or older, residing in China and Woken Kebele for a minimum duration of 6 months.
Individuals who reported being severely ill and unable to participate in interviews for data collectors, those who provided a medical certificate or related document indicating their current illness, and those with observable verbal communication problems were excluded from the study.
Posttraumatic stress disorder: A 20- item post-traumatic checklist (PCL-5) was used to assess PTSD). A cumulative score was derived by summing the 20 items, with scores ranging from 0 to 80 on a five-point Likert scale (0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit, and 4 = extremely), Which means adults who score< 50 have no PTSD and ≥ 50 have PTSD (27).
Depression
Participants exhibiting depression were identified through their scores on the Patient Health Questionnaire (PHQ), specifically those individuals who scored 10 or more on the nine items (28).
Stressful life event. It was determined by the presence of one or more life-threatening events within the last six months, as indicated by the relevant questions (29).
Social support
Social support was assessed using the Social Support Scale (OSS-3), which consists of three items with scores ranging from 3 to 14. A score within the range of 3–8 indicates poor social support, while a score between 9–11 suggests intermediate social support. A score of 12–14 on the OSS-3 reflects strong social support (30).
Substance abuse was defined as the consumption of cigarettes, alcohol, or khat by individuals who met the criteria of (31, 32).
Data collection tools
Data collection was conducted by psychiatric professionals with Bachelor of Science (BSc) degrees, trained in data collection techniques and ethical principles. The questionnaire was initially developed in English and translated into Amharic, with a back-translation into English to ensure accuracy. Training was provided to study participants about the study’s objectives, handling ambiguous questions, and adhering to ethical standards, including informed consent, confidentiality, anonymity, and data management. PTSD was assessed using the 20-item self-report Post-Traumatic Stress Disorder Checklist (PCL-5), which measures the 20 DSM-5 PTSD symptoms. We validated this assessment tool internally, achieving a Cronbach’s alpha reliability coefficient of 0.78. It has been previously utilized in Ethiopia (5, 20). The Validity and reliability of the PCL-5 had been tested and proven in a different country, for example, Zimbabwe (Cronbach’s alpha = 0.92) with sensitivity and specificity of 74.5% and 70.6% respectively (33), (5). We validated this assessment tool, achieving a Cronbach’s alpha reliability coefficient of 0.78. Depression was measured using the Patient Health Questionnaire-9 (PHQ-9), where a person is considered depressed if their score is 10 or higher on the nine items. The PHQ-9 has 4 items with corresponding scores: not at all (0), several days (34), more than half a day (15), nearly every day (35), and over the last week (28).
Data processing and statistical analysis
The collected data was coded and entered into Epi-Data version 4.6, followed by analysis using IBM SPSS Statistics version 25.0 software. Summary statistics, including proportions and frequencies, were utilized to summarize the results in tables. Bivariable and multivariable logistic regression models was fitted to identify factors associated with the outcome variable. In the bivariable logistic regression, variables with a p value ≤ 0.2 were considered candidates for inclusion in the multivariable logistic regression. Binary logistic regression was employed. Adjusted odds ratios (ORs) was used to determine the relationships between PTSD and associated variables at a significance level of p ≤ 0.05. The normality of continuous data was assessed using the Shapiro−Wilk test, and the model’s fitness was checked using the Hosmer–Lemshow goodness-of-fit test.
Ethics approval and consent to participate
We obtained ethical approval from the Institutional Review Board of the University of Gondar, School of Medicine, College of Medicine, and Health Sciences Ethical Review Committee, with reference number IRB/373/2023, subsequent to the review of our research proposal. After adequately briefing the educated study participants about the study, written informed consent was obtained from each individual. Conversely, during data collection from illiterate study participants, the data collectors began by reading aloud the consent form, providing a thorough explanation of the study’s objectives and procedures. Upon participants’ voluntary agreement to participate, the data collectors marked “Yes” on the consent form. Subsequently, participants confirmed their consent by providing their signature using a “thumbprint” as acknowledgment. This approach was approved by the Institutional Review Board (IRB) of the University of Gondar. To uphold confidentiality and privacy, participants’ names and other personal identifiers were excluded from the documentation. To maintain confidentiality, potential identifiers were omitted from the questionnaire, and all collected data were securely stored. Our procedures adhered to the relevant rules and guidelines outlined in the Helsinki Declaration (36).
Results
Background characteristics of the study participants
In this study, a total of 410 study participants were included, making 100% response rate. The majority of participants were male (62%). The mean age of the study participants was 33 years ( ± 1.67). Approximately 45% of the participants were married, and 43% had completed elementary school. Nearly 63% of participants resided in rural areas, and approximately 45% were employed as farmers. Majority the participants reported a monthly income ranging from 34.6 USD (see Table 1).
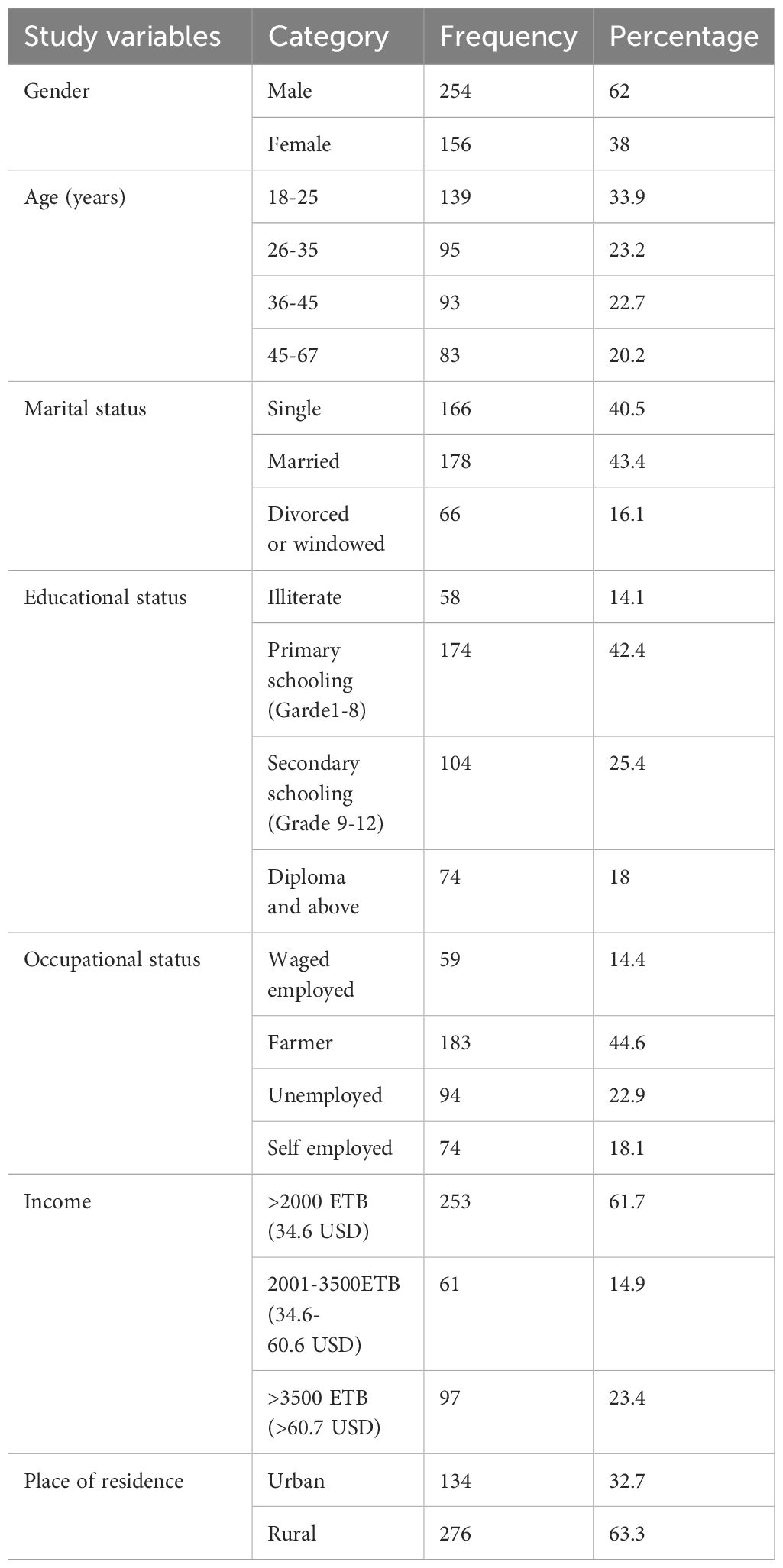
Table 1 background characteristics of study participants who reside in the ware affected area in the Dabat district, northwest Ethiopia, 2023.
Clinical and behavioural characteristics of the study participants
In the present study, 17% of all participants reported a family history of mental illness. Approximately one-third of the participants (32%) had a known diagnosis of a chronic medical condition, 43% of whom were specifically diagnosed with diabetes. Symptoms of depression and morbidity were exhibited by approximately thirty percent of the research participants. More than thirty percent of the participants had engaged in khat chewing at some point in their lifetime. Additionally, one-third of the study participants reported experiencing sexual abuse or rape during the war (refer to Table 2).
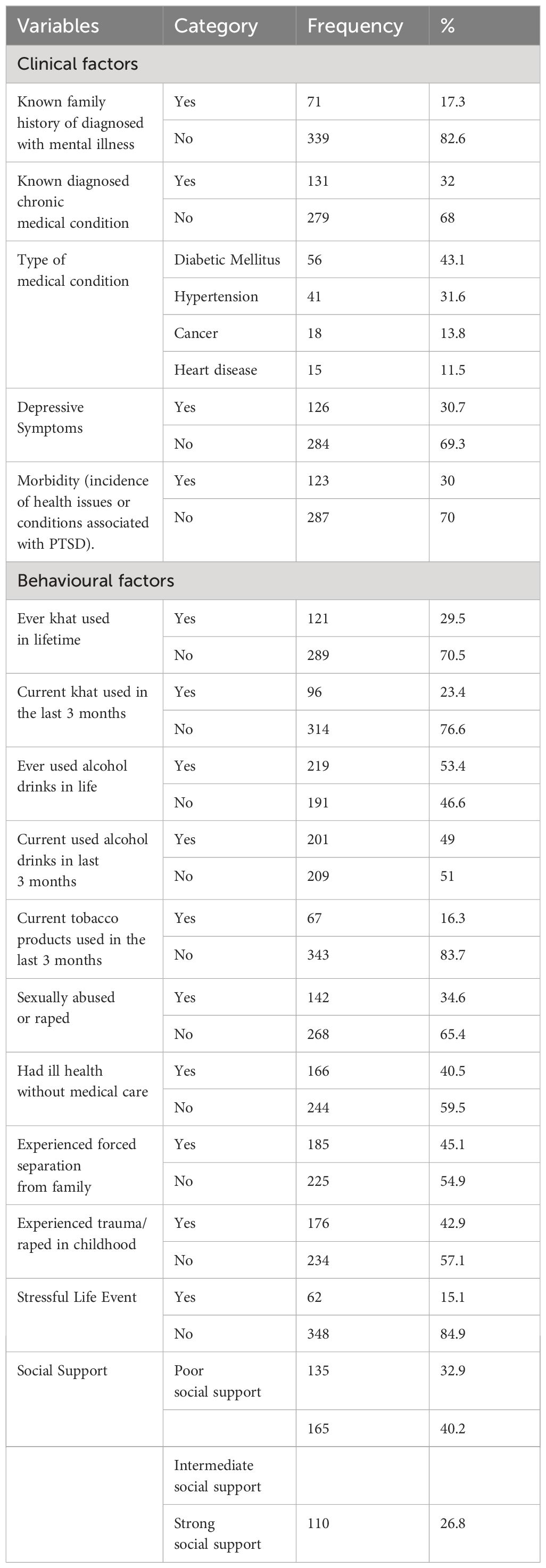
Table 2 Clinical and behavioural factors among study participants who reside in the ware-affected area in the Dabat district, northwest Ethiopia, in 2023.
Prevalence of posttraumatic stress disorder
In this study, 30.7% of the participants (126 out of 410) had posttraumatic stress disorder (95% CI 26.6–35.1).
Factors associated with posttraumatic stress disorder
Bivariable and multivariable logistic regression analyses of PTSD were conducted, as detailed in Table 3. In the bivariable analysis, sex, age, marital status, monthly income, educational status, khat chewing status, alcohol consumption status, family history of mental illness, depression symptoms, sexual abuse or rape status, and stressful life events were considered candidate variables for the multivariable analysis (p ≤ 0.2). Multivariable logistic regression analysis revealed several statistically significant factors associated with PTSD: having symptoms of depression (AOR=3.5; 95% CI: 1.13-6.89), age 45-67 years (AOR=1.68; 95% CI: 1.04-5.78), experiencing stressful life events (AOR=1.63; 95% CI: 1.05-7.86), experiencing sexual abuse or rape (AOR=1.53; 95% CI: 1.07-6.75), chewing khat (AOR=1.48; 95% CI: 1.08-4.56), being female (AOR=1.43; 95% CI: 1.13-3.67),an d having an income 34.6 USD (AOR=1.28; 95% C: (1.07-4.67). Symptoms of depression were the strongest predictor (AOR=3.5; 95% CI: 1.13-6.89), indicating that individuals with depression symptoms were 3.5 times more likely to develop PTSD compared to those without. Age 45-67 years (AOR=1.68; 95% CI: 1.04-5.78), showing that participants in this age group were 1.68 times more likely to develop PTSD compared to those aged 18 to 25 years. Stressful life events (AOR=1.63; 95% CI: 1.05-7.86), indicating a 1.63 times higher likelihood of PTSD among those who experienced such events. Sexual abuse or rape (AOR=1.56; 95% CI: 1.07-6.75), showing a 1.56 times greater odds of PTSD among individuals who experienced these incidents. Khat chewing (AOR=1.47; 95% CI: 1.08-4.56), indicating a 1.47 times higher likelihood of PTSD among khat chewers compared to non-chewers. Female gender (AOR=1.43; 95% CI: 1.13-3.67), with females having a 1.43 times greater likelihood of PTSD compared to males. Compared to study participants with incomes with of >60.7 USD, those with less than 34.6 USD had a higher likelihood of developing PTSD (AOR=1.28; 95% CI: 1.07-4.67).
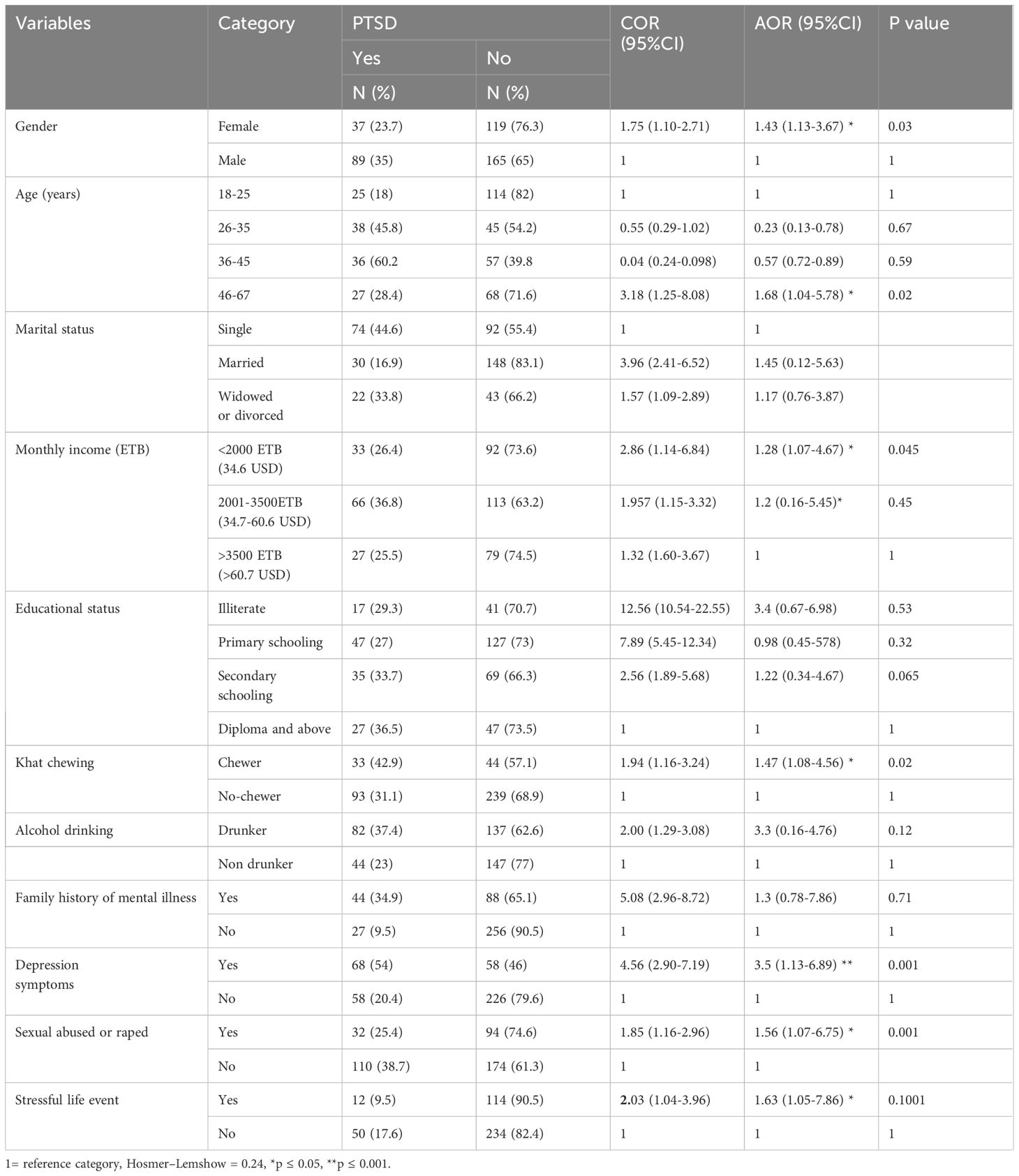
Table 3 factors associated with PTSD among study participants who reside in the ware-affected area in the Dabat district, northwest Ethiopia, 2023.
Discussion
The observed prevalence of PTSD among people living in war-affected areas in Dabat district, was determined to be 30.7% (95% CI 26.6–35.1). These finding suggest a higher prevalence of PTSD among residents of war-affected regions in the study settings, this result is similar to findings from studies conducted in Dessie, Ethiopia (34.5%) (5), Israel (27%) (37), Servia (32.3%) (38) and South Sudan (28%) (19). However, this result is lower than those of studies conducted in Kenya, which reported a prevalence of 62.1% (39); in South Sudan Juba, which reported a prevalence of 37.6% (40); and in Croatia, which reported a prevalence of 56.7% (41). On the other hand, this prevalence is higher than that reported in studies conducted in Uganda, 18% (21), and in Libya 25.23% (42). In the Dabat district of Ethiopia, cultural beliefs profoundly influence responses to war-related atrocities such as rape, torture, murder, and abduction. Stigma often prevents victims from seeking justice or support services due to fears of social ostracization and reputation damage, potentially exacerbating PTSD development. Societal pressures and familial honor heavily influence whether victims disclose their experiences and the type of community support they receive. Additionally, religious and spiritual beliefs shape interpretations of trauma, affecting coping mechanisms and attitudes toward seeking professional help versus traditional healing practices (26, 43–45).
This study revealed that PTSD was positively associated with having symptoms of depression, ages 45-67, experiencing stressful life events, enduring sexual abuse or rape, chewing khat, being female, and having an income of less than 34.60 USD.
Symptoms of depression were the strongest predictor, showing that individuals with depression symptoms were more likely to develop PTSD compared to those without. This study is supported by a study performed in Nigeria (46), northeaster Ethiopia (5), the Maikadra massacre in Ethiopia (47),. This is because people with depression may have heightened sensitivity to stress and trauma, impaired coping mechanisms, and neurobiological changes that increase their vulnerability to developing PTSD (48). Elderly study participants were more prone to developing PTSD than their male counterparts were. This result is in line with research conducted in Netherland (49). This could be attributed to the greater prevalence of chronic health conditions such as heart disease, hypertension, and diabetes among elderly people, coupled with challenges such as sleep disturbances, insomnia, physical and mental fatigue, changes in appetite, muscle tension, pain, chest discomfort, an upset stomach, and other issues more commonly experienced in the elderly population. All these factors may contribute to the development of posttraumatic stress disorder (50, 51).
According to the results of this study, women were more likely to develop PTSD than men were. These findings align with research conducted in northeast Ethiopia (5) and Uganda (52).This could be attributed to the greater vulnerability of females to sexual abuse or rape during times of war, making them more susceptible to developing PTSD than men are (53).
A potential explanation could be the influence of sex hormones and neuro-steroids on emotional learning and memory formation, coupled with disparities in brain anatomy and activation in response to traumatic stress (54). Contrary to current findings, research conducted in the US found no significant difference in PTSD rates between men and women, even after adjusting for demographic factors and lifetime trauma exposure (55). Hence, it is reasonable to deduce that when males and females experience similar types and levels of traumatic stressors, disparities in PTSD rates between the genders may not be as pronounced (53). Individuals with lower incomes were more likely to develop PTSD than their higher-income counterparts were. This study aligns with the study conducted in low-income countries (56). This can be attributed to the vulnerability of individuals with low incomes, who are more prone to experiencing depression, anxiety, and increased levels of the hormone cortisol. These factors collectively contribute to heightened stress levels (57). Compared with no chewers, study participants who chewed khat had greater odds of developing PTSD. This study is supported by a study performed in Somali (58). A possible explanation is that chewing khat can result in side effects such as headaches, vertigo, decreased cognitive function, fine tremors, sleeplessness, heightened alertness, dependence, tolerance, and anxiety. All these effects could contribute to the development of posttraumatic stress disorder (59).
Compared to study participants who were not sexually abused or raped, those who suffered these events had a greater chance of developing PTSD. This study is in line with previous findings in the Balkans (4). This correlation may be attributed to the impact of depression, which influences susceptibility to trauma and contributes to the development of posttraumatic stress disorder by elevating steroid hormones such as cortisol (60). Finally, participants who experienced stressful life events exhibited a greater likelihood of developing posttraumatic stress disorder (PTSD) than did those who had not experienced such events. This study consistent with findings from a prior investigation conducted in southern Sudan (40) and northeast Ethiopia (5). This can be explained by the fact that stressful life events, such as problems with work, relationships, or finances, can exacerbate PTSD (61).
Strengths and limitations of the study
The strength of this study was its use of primary or original data, which increased its relevance. This study and this study had certain limitations, including social desirability bias, as participants might be hesitant to provide socially acceptable responses to sensitive questions concerning sexual abuse and substance use. Additionally, there was a recall bias due to the limitations of the study design.
Conclusion and recommendation
The results of this study showed that a significant proportion of people living in war-affected areas had PTSD. As a result, the study suggested that governments and other stakeholders should be involved in implementing efficient interventions and quick measures to mitigate the effects of war on mental health following the conflict. The government and nongovernmental organizations were also advised by these studies to continue providing humanitarian assistance, which should include access to food, clean water, clothing, shelter, and education. This study also suggested that people living in conflict zones should be legally protected from rape, sexual abuse, arson, detention without cause, and kidnapping. This study recommends that scholars employ a combination of qualitative and quantitative approaches to gain a comprehensive understanding of PTSD in war-affected areas. Furthermore, it highlights the critical role of cohort studies in establishing causal relationships between exposure to war and the development of PTSD.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by the institutional review board of the University of Gondar’s School of Medicine, College of Medicine, and Health Sciences ethical review committee, with the reference number (IRB/373/2023). Upon explaining the study’s significance to participants, both verbal and written informed consent were obtained. To maintain confidentiality, potential identifiers were omitted in the questionnaire, and the collected data was securely stored. All procedures adhered to the relevant rules and guidelines of the Helsinki Declaration. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MM: Writing – original draft, Writing – review & editing. LM: Data curation, Conceptualization, Writing – original draft, Writing – review & editing. DE: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank all study participants and data collectors for their contributions to the success of this study. The authors also thank the University of Gondar for providing ethical clearance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence interval; COR, Crude odds ratio; HTQ, Harvard Trauma Questionnaire; OSSS, Oslo Social Support Scale; PCL-C, posttraumatic stress disorder civilian version; PHQ-9, Patient Health Questionnaire; PTSD, posttraumatic stress disorder; SD, standard deviation.
References
2. Mifetu FA. Sexual Violence in Armed Conflicts: The Case of Tigray, Ethiopia (2020-2022). Norwegian University of Life Sciences (2023).
3. Abbink J. The politics of conflict in Northern Ethiopia, 2020–2021: a study of war-making, media bias and policy struggle Vol. 152. African Studies Centre Leiden the Netherlands, ASCL (2021). p. 2021. Working Paper.
4. Priebe S, Bogic M, Ashcroft R, Franciskovic T, Galeazzi GM, Kucukalic A, et al. Experience of human rights violations and subsequent mental disorders–A study following the war in the Balkans. Soc Sci Med. (2010) 71:2170–7. doi: 10.1016/j.socscimed.2010.09.029
5. Birhan Z, Deressa Y, Shegaw M, Asnakew S, Mekonen T. Posttraumatic stress disorder in a war-affected area of Northeast Ethiopia: a cross-sectional study. BMC Psychiatry. (2023) 23:627. doi: 10.1186/s12888-023-05116-w
6. Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. (2004) 161:3–31.
7. Holmes JS, De Piñeres SAG. Conflict-induced displacement and violence in Colombia. Stud Conflict Terrorism. (2011) 34:572–86. doi: 10.1080/1057610X.2011.578552
8. Flory JD, Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin Neurosci. (2015) 17:141–50. doi: 10.31887/DCNS.2015.17.2/jflory
9. West S. War against kids” in southern Africa. Black Scholar. (1987) 18:26–33. doi: 10.1080/00064246.1987.1
10. Kibel S, Bass D, Cywes S. Five years’ experience of injured children. South Afr Med J. (1990) 78:387–91.
11. Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry. (2015) 28:307. doi: 10.1097/YCO.0000000000000167
12. Kalia M. Assessing the economic impact of stress [mdash] The modern day hidden epidemic. Metabolism-Clinical Experimental. (2002) 51:49–53. doi: 10.1053/meta.2002.33193
14. Bezabh YH, Abebe SM, Fanta T, Tadese A, Tulu M. Prevalence and associated factors of post-traumatic stress disorder among emergency responders of Addis Ababa Fire and Emergency Control and Prevention Service Authority, Ethiopia: institution-based, cross-sectional study. BMJ Open. (2018) 8:e020705. doi: 10.1136/bmjopen-2017-020705
15. Koenen K, Ratanatharathorn A, Ng L, McLaughlin K, Bromet E, Stein D, et al. Posttraumatic stress disorder in the world mental health surveys. psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708
16. Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. (2019) 394:240–8. doi: 10.1016/S0140-6736(19)30934-1
17. Ng LC, Stevenson A, Kalapurakkel SS, Hanlon C, Seedat S, Harerimana B, et al. National and regional prevalence of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. PloS Med. (2020) 17:e1003090. doi: 10.1371/journal.pmed.1003090
18. Mugisha J, Muyinda H, Wandiembe P, Kinyanda E. Prevalence and factors associated with posttraumatic stress disorder seven years after the conflict in three districts in northern Uganda (The Wayo-Nero Study). BMC Psychiatry. (2015) 15:1–12. doi: 10.1186/s12888-015-0551-5
19. Ayazi T, Lien L, Eide AH, Ruom MM, Hauff E. What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BMC Psychiatry. (2012) 12:1–12. doi: 10.1186/1471-244X-12-175
20. Asnakew S, Shumet S, Ginbare W, Legas G, Haile K. Prevalence of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ Open. (2019) 9:e028550. doi: 10.1136/bmjopen-2018-028550
21. Karunakara UK, Neuner F, Schauer M, Singh K, Hill K, Elbert T, et al. Traumatic events and symptoms of post-traumatic stress disorder amongst Sudanese nationals, refugees and Ugandans in the West Nile. Afr Health Sci. (2004) 4:83–93.
22. Hauff E, Vaglum P. Organised violence and the stress of exile: Predictors of mental health in a community cohort of Vietnamese refugees three years after resettlement. Br J Psychiatry. (1995) 166:360–7. doi: 10.1192/bjp.166.3.360
23. Hauff E, Vaglum P. Organised violence and the stress of exile. Predictors Ment. (1995) 360–7. doi: 10.1192/bjp.166.3.360
24. Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. New Engl J Med. (2013) 368:2182–91. doi: 10.1056/NEJMoa1211853
25. Williams CL, Berry JW. Primary prevention of acculturative stress among refugees: application of psychological theory and practice. Am Psychol. (1991) 46:632. doi: 10.1037/0003-066X.46.6.632
26. Madoro D, Kerebih H, Habtamu Y, G/tsadik M, Mokona H, Molla A, et al. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. (2020)18:2317–26. doi: 10.2147/NDT.S267307
27. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The ptsd checklist for dsm-5 (pcl-5). American psychological association. (2013).
28. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210:653–61. doi: 10.1016/j.psychres.2013.07.015
29. Motrico E, Moreno-Küstner B, de Dios Luna J, Torres-González F, King M, Nazareth I, et al. Psychometric properties of the List of Threatening Experiences—LTE and its association with psychosocial factors and mental disorders according to different scoring methods. J Affect Disord. (2013) 150:931–40. doi: 10.1016/j.jad.2013.05.017
30. Kocalevent R-D, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. (2018) 6:1–8. doi: 10.1186/s40359-018-0249-9
31. Aklog T, Tiruneh G, Tsegay G. Assessment of substance abuse and associated factors among students of debre markos poly technique college in debre markos town, East Gojjam Zone, Amhara Regional State, Ethiopia, 2013. Global J Med Res. (2013) 13:1. doi: 10.4236/ojepi.2014.44026
32. Teferi KA. Psychoactive substance abuse and intention to stop among students of Mekelle University. Ethiopia: Mekele University (2011). MPH thesis.
33. Verhey R, Chibanda D, Gibson L, Brakarsh J, Seedat S. Validation of the posttraumatic stress disorder checklist–5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry. (2018) 18:1–8. doi: 10.1186/s12888-018-1688-9
34. Ruggiero KJ, Ben KD, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist—Civilian version. J traumatic stress. (2003) 16:495–502. doi: 10.1023/A:1025714729117
35. Priebe S, Bogic M, Ajdukovic D, Franciskovic T, Galeazzi GM, Kucukalic A, et al. Mental disorders following war in the Balkans: a study in 5 countries. Arch Gen Psychiatry. (2010) 67:518–28. doi: 10.1001/archgenpsychiatry.2010.37
36. Goodyear MD, Krleza-Jeric K, Lemmens T. The declaration of helsinki. Br Med J Publishing Group;. (2007) p:624–5. doi: 10.1136/bmj.39339.610000.BE
37. Besser A, Neria Y. PTSD symptoms, satisfaction with life, and prejudicial attitudes toward the adversary among Israeli civilians exposed to ongoing missile attacks. J Traumatic Stress: Off Publ Int Soc Traumatic Stress Stud. (2009) 22:268–75. doi: 10.1002/jts.20420
38. Lecic-Tosevski D, Pejuskovic B, Miladinovic T, Toskovic O, Priebe S. Posttraumatic stress disorder in a Serbian community: seven years after trauma exposure. J nervous Ment disease. (2013) 201:1040–4. doi: 10.1097/NMD.0000000000000051
39. Musau JN, Omondi M, Khasakhala L. The prevalence of post-traumatic stress disorder (PTSD) among internally displaced persons (IDPs) in Maai Mahiu Camp in Nakuru County, Kenya. J Internal Displacement. (2018) 8:20–33.
40. Roberts B, Damundu EY, Lomoro O, Sondorp E. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC Psychiatry. (2009) 9:1–10. doi: 10.1186/1471-244X-9-7
41. Arbanas G. Patients with combat-related and war-related posttraumatic stress disorder 10 years after diagnosis. Croatian Med J. (2010) 51:209–14. doi: 10.3325/cmj.2010.51.209
42. Abuhadra BD, Doi S, Fujiwara T. The prevalence of post-traumatic stress disorder, depression, and anxiety in Libya: a systematic review. Middle East Curr Psychiatry. (2023) 30:49. doi: 10.1186/s43045-023-00322-4
43. Zarowsky C. Trauma stories: Violence, emotion and politics in Somali Ethiopia. Transcultural Psychiatry. (2000) 37:383–402. doi: 10.1177/136346150003700306
44. Nordanger DØ. Beyond PTSD: socio-economic bereavement in Tigray, Ethiopia. Anthropology Med. (2007) 14:69–82. doi: 10.1080/13648470601106426
45. Shannon PJ, Wieling E, McCleary JS, Becher E. Exploring the mental health effects of political trauma with newly arrived refugees. Qual Health Res. (2015) 25:443–57. doi: 10.1177/1049732314549475
46. Aluh DO, Okoro RN, Zimboh A. The prevalence of depression and post-traumatic stress disorder among internally displaced persons in Maiduguri, Nigeria. J Public Ment Health. (2020) 19:159–68. doi: 10.1108/JPMH-07-2019-0071
47. Ali D, Azale T, Wondie M, Tadesse J. About six in ten survivors of the november 2020 Maikadra massacre suffer from posttraumatic stress disorder, northwest Ethiopia. Psychol Res Behav Manage. (2022) 14:251–60. doi: 10.2147/PRBM.S338823
48. Tafet GE, Nemeroff CB. The links between stress and depression: psychoneuroendocrinological, genetic, and environmental interactions. J neuropsychiatry Clin neurosciences. (2016) 28:77–88. doi: 10.1176/appi.neuropsych.15030053
49. de Vries GJ, Olff M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. J Traumatic Stress: Off Publ Int Soc Traumatic Stress Stud. (2009) 22:259–67. doi: 10.1002/jts.20429
50. McCutcheon VV, Sartor CE, Pommer NE, Bucholz KK, Nelson EC, Madden PA, et al. Age at trauma exposure and PTSD risk in young adult women. J traumatic stress. (2010) 23:811–4. doi: 10.1002/jts.20577
51. Norris FH, Kaniasty K, Conrad ML, Inman GL, Murphy AD. Placing age differences in cultural context: A comparison of the effects of age on PTSD after disasters in the United States, Mexico, and Poland. J Clin Geropsychology. (2002) 8:153–73. doi: 10.1023/A:1015940126474
52. Ainamani HE, Elbert T, Olema DK, Hecker T. Gender differences in response to war-related trauma and posttraumatic stress disorder–A study among the Congolese refugees in Uganda. BMC Psychiatry. (2020) 20:1–9. doi: 10.1186/s12888-019-2420-0
53. Wilker S, Kolassa S, Ibrahim H, Rajan V, Pfeiffer A, Catani C, et al. Sex differences in PTSD risk: evidence from post-conflict populations challenges the general assumption of increased vulnerability in females. Eur J psychotraumatology. (2021) 12:1930702. doi: 10.1080/20008198.2021.1930702
54. Kornfield SL, Hantsoo L, Epperson CN. What does sex have to do with it? The role of sex as a biological variable in the development of posttraumatic stress disorder. Curr Psychiatry Rep. (2018) 20:1–8. doi: 10.1007/s11920-018-0907-x
55. Hourani L, Williams J, Bray RM, Wilk JE, Hoge CW. Gender differences in posttraumatic stress disorder and help seeking in the US Army. J women’s Health. (2016) 25:22–31. doi: 10.1089/jwh.2014.5078
56. Santiago CD, Wadsworth ME, Stump J. Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. J Economic Psychol. (2011) 32:218–30. doi: 10.1016/j.joep.2009.10.008
57. Holmes SC, Callinan L, Facemire VC, Williams MT, Ciarleglio MM, Smith MV. Material hardship is associated with posttraumatic stress disorder symptoms among low-income black women. J Traumatic Stress. (2021) 34:905–16. doi: 10.1002/jts.22741
58. Odenwald M, Hinkel H, Schauer E, Schauer M, Elbert T, Neuner F, et al. Use of khat and posttraumatic stress disorder as risk factors for psychotic symptoms: a study of Somali combatants. Soc Sci Med. (2009) 69:1040–8. doi: 10.1016/j.socscimed.2009.07.020
59. Wondemagegn AT, Cheme MC, Kibret KT. Perceived psychological, economic, and social impact of khat chewing among adolescents and adults in Nekemte Town, East Welega Zone, West Ethiopia. BioMed Res Int. (2017) 2017:1–9. doi: 10.1155/2017/7427892
60. Aluh DO, Okoro RN, Zimboh A. The prevalence of depression and post-traumatic stress disorder among internally displaced persons in Maiduguri, Nigeria. J Public Ment Health. (2019) 19:159–68. doi: 10.1108/JPMH-07-2019-0071
Keywords: stress related disorders, trauma, war, Ethiopia, prevalence
Citation: Melese M, Maru L and Esubalew D (2024) Posttraumatic stress disorder and its associated factors among people living in Dabat district, northwest Ethiopia. Front. Psychiatry 15:1359382. doi: 10.3389/fpsyt.2024.1359382
Received: 16 January 2024; Accepted: 10 July 2024;
Published: 30 July 2024.
Edited by:
Gülseren Keskin, Ege University, TürkiyeReviewed by:
S. M. Yasir Arafat, Biomedical Research Foundation, BangladeshMohammadreza Shalbafan, Iran University of Medical Sciences, Iran
Atefeh Zandifar, Alborz University of Medical Sciences, Iran
Copyright © 2024 Melese, Maru and Esubalew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mihret Melese, bWloaHJldDg2QGdtYWlsLmNvbQ==
 Mihret Melese
Mihret Melese Lemlemu Maru1
Lemlemu Maru1 Dereje Esubalew
Dereje Esubalew