- 1Centre referent de rehabilitation psychosociale, GCSMS REHACOOR 42, Saint-Étienne, France
- 2University Claude Bernard Lyon1, Research on Healthcare Performance (RESHAPE) INSERM U1290, Lyon, France
- 3AURORE Perinatal Network, Hospices civiles de Lyon, Croix Rousse Hospital, Lyon, France
- 4Departments of Psychiatry and Child & Adolescent Psychiatry, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
- 5Medical Library, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
- 6University Hospital of Saint-Étienne & EA 7423 (Troubles du Comportement Alimentaire, Addictions et Poids Extrêmes (TAPE), Université Jean Monnet - Saint-Etienne), Saint-Etienne, France
- 7University Hospital of Saint-Étienne, Department of Child and Adolescent Psychiatry, France & Marc Jeannerod Institute of Cognitive Sciences UMR 5229, CNRS & Claude Bernard University, Lyon, France
Background: Midwives may be key stakeholders to improve perinatal mental healthcare (PMHC). Three systematic reviews considered midwives’ educational needs in perinatal mental health (PMH) or related interventions with a focus on depression or anxiety. This systematic review aims to review: 1) midwives’ educational/training needs in PMH; 2) the training programs in PMH and their effectiveness in improving PMHC.
Methods: We searched six electronic databases using a search strategy designed by a biomedical information specialist. Inclusion criteria were: (1) focus on midwives; (2) reporting on training needs in PMH, perinatal mental health problems or related conditions or training programs; (3) using quantitative, qualitative or mixed-methods design. We used the Mixed Methods Appraisal Tool for study quality.
Results: Of 4969 articles screened, 66 papers met eligibility criteria (47 on knowledge, skills or attitudes and 19 on training programs). Study quality was low to moderate in most studies. We found that midwives’ understanding of their role in PMHC (e.g. finding meaning in opening discussions about PMH; perception that screening, referral and support is part of their routine clinical duties) is determinant. Training programs had positive effects on proximal outcomes (e.g. knowledge) and contrasted effects on distal outcomes (e.g. number of referrals).
Conclusions: This review generated novel insights to inform initial and continuous education curriculums on PMH (e.g. focus on midwives’ understanding on their role in PMHC or content on person-centered care).
Registration details: The protocol is registered on PROSPERO (CRD42021285926)
1 Introduction
Perinatal Mental Health Problems (PMHPs) affect parents during pregnancy and the first year after childbirth and commonly consist of anxiety, non-psychotic depressive episode, psychotic episodes, post-traumatic stress disorder and adjustment disorder. Despite being often associated with poor parental and child outcomes (1), PMHPs remain predominantly unrecognized, undiagnosed and untreated (2).
Given their role in perinatal care providing multiple occasions to discuss perinatal mental health (3) - midwives may be key stakeholders to improve the detection, referral and management of PMHPs. Parents usually welcome midwives’ interest in their mental health and report to prefer discussing mental health issues with obstetric providers than with mental health providers (4, 5). Assessing perinatal mental health (PMH) and detecting symptoms of postpartum depression, anxiety and psychosis are part of the essential competencies for midwifery practice according to the International Confederation of Midwives (2019) (6). However, and despite being in general interested in assessing perinatal mental health (PMH) and wellbeing (7), midwives report feeling less comfortable with putting competencies related to PMH into practice compared to those related physical health (8, 9).
To our knowledge, three literature reviews have been conducted on midwives’ educational needs in perinatal mental health (7, 10, 11). These reviews reported a lack of knowledge, skills and confidence influential at different levels of the care pathway, e.g. detection, decision-making about referral and support. However, there remain some limitations to the current body of evidence. First, all reviews found low-to-moderate quality studies coming predominantly from high-income countries. Second, two out of three reviews (10, 11) - conducted in 2017 (n=17 articles) and 2022 (43 articles) - focused on perinatal depression or perinatal anxiety and did not cover the full range of PMHPs as well as related conditions (e.g. substance use disorder, serious mental illness (SMI)) or autism). The third review (7) conducted in 2017 (n=22 articles) covered a wider range of PMHPs using an integrative review design, the other two (10, 11) being systematic reviews. Third, previous reviews (7, 10, 11) focused on midwives’ knowledge, skills and attitudes and context-related factors. However, it remains unclear whether improvements in these areas translate into in routine clinical practice (e.g. improved detection of PMHPs or facilitated decision-making about referral to mental health providers). Fourth, case identification - using formal or informal screening methods - have contrasted effects on referral rates (7) and patient outcomes [e.g. limited effects of screening on depressive symptoms (12, 13)]. Fifth, two systematic reviews reported on training programs in perinatal depression [n=7 studies (10), n=12 studies (14)]. However, these reviews included mixed samples [e.g. 37% midwives in Wang et al., 2022 (14) and 54% midwives in Legere et al., 2017 (10)] and did not target the same set of skills [e.g. improving knowledge and detection (10); providing evidence-based interventions (14)]. Reviews either investigated midwives’ training needs (7, 11) or training interventions (10, 14). The literature on training programs in PMH for student midwives and midwives remains scarce [n=4 studies (10)]. A synthesis of evidence before this study is presented on Table 1.
The present review primarily aims to identify and review: 1) midwives’ educational/training needs in PMH (i.e. beyond perinatal depression or anxiety to include PMHPs, SMI, substance use disorder, and autism); 2) the existing interventions and their effectiveness in improving detection and management of PMHPs.
2 Methods
2.1 Search strategy
The protocol for this systematic review was reported according to PRISMA guidelines (15). The search strategy was designed by a biomedical information specialist (WMB) from the Medical Library of Erasmus MC, University Medical Center Rotterdam (16). We searched Embase, MEDLINE, Web of Science, Cochrane Central Register of Controlled Trials, CINAHL and, PsycINFO for published, peer reviewed original articles. The search combined terms for (1) perinatal mental health problems, serious mental illness (i.e. schizophrenia, mood disorders, personality disorders, anxiety), eating disorders, substance use disorders or autism, and (2) midwives’ knowledge, attitudes, skills or training needs, as well as existing training programs for midwives on PMH. We included only published articles in English or French. No time restriction was set. The search was updated prior to publication on 21 June 2023. We hand-searched the reference list of three systematic literature reviews (7, 10, 11) for additional relevant articles. The full search strategy, search terms and syntax are presented in online Supplementary Table 1.
2.2 Inclusion/exclusion criteria
To be included, articles had to meet all the following criteria: 1) focus on midwives (included midwives, nurse-midwives, registered midwives, registered midwives tutors, registered midwives prescribers and registered advanced midwives practitioners - referred as “midwives” in this review); 2) reporting on midwives’ training needs in PMH, PMHPs or related conditions or existing training programs that focus on the use of screening tools to detect PMHPs, on PMH in general or specific aspects of PMH; 3) using quantitative, qualitative or mixed-methods design. For training programs, we included uncontrolled and controlled studies (placebo, TAU or active comparators).
Our exclusion criteria were: 1) no full text available or studies published in languages other than English or French; 2) grey literature because the aim of this systematic review was to guide the development of future interventions; 3) training programs on psychological interventions (e.g. cognitive behavior therapy) because this review focused on interventions aiming at improving midwives’ training on essential competencies related to PMH (e.g. PMH assessment, detection, referral and support of parents with PMHPs).
2.3 Selection and coding
The screening process was conducted in two separate stages: 1) Two authors (M.D. and J.D) independently screened the title and abstracts of all non-duplicated papers excluding those not relevant. Potential discrepancies were resolved by consensus; 2) Two authors (M.D. and J.D) independently applied eligibility criteria and screened the full-text papers to select the included studies. Disputed items were solved discussing together and reading further the paper to reach a final decision. Supplementary Tables 2, 3 present the list of included/excluded studies. Inter-rater reliability was calculated (kappa=0.90).
2.4 Data extraction
Two authors (MD and JD) performed independently the data extraction. For each study, we extracted the following information: general information (author, year of publication, country, design, type of study, population considered, period), assessment tools or methods, cultural aspects, the main findings and variables relating to quality assessment. For studies reporting on training programs, we also extracted information about the intervention (nature, type, length, targeted skills or outcomes, format), outcome measures and effectiveness on midwives’ knowledge, attitude, skills or routine use of screening tools to detect PMHPs or parents’ outcomes (e.g. depressive symptoms). Tables 2–6 present the factors associated with knowledge, skills, confidence and decisions about screening, referral or support. Supplementary Tables 4, 5 present the detailed characteristics of the included studies.
2.5 Quality assessment
Quality assessment was realized using the Mixed Methods Appraisal Tool (MMAT) (61). MMAT is a validated instrument to assess the methodological quality of qualitative, randomized controlled trials, non-randomized trials, descriptive studies, and mixed methods studies. It is comprised of five 5-item subscales assessing different aspects of quality (e.g. appropriateness of the selected design/methods/measurements, integration of quantitative and qualitative parts for mixed-methods studies). Two researchers (MD and JD) independently assessed methodological quality using the MMAT and extracted MMAT scores for each article. Discrepancies were resolved through consensus. The MMAT overall quality score and detailed scores are provided in Supplementary Tables 4, 5. The study protocol was registered on PROSPERO on November 1, 2021 (CRD42021285926).
3 Results
Of the 9650 articles found during searches from inception to June 26th 2023, 4969 references remained after removing all duplicates. Based on titles and abstracts, 4772 papers were excluded for lack of relevance. Our search strategy yielded 197 full-text articles. After conducting a full-text analysis of all these papers, we ended up with 66 relevant papers (47 on knowledge, skills or attitudes and 19 on training programs; PRISMA diagram on Figure 1).
3.1 Study characteristics
The characteristics of the 66 included studies are presented on Tables 7, 8. Most studies were conducted in high-income countries (89.4%) and published after 2015 (50%). Study designs were quantitative (n=33; 50%), qualitative (n=22; 33.3%) or mixed-methods (n=11; 16.7%). Samples included qualified midwives (n=37; 56.0%), qualified midwives and other perinatal health providers (n=17; 25.8%) and student midwives (n=11; 16.7%). Qualified midwives had a variable level of training in PMH ranging from none to 90% (specified in 24 studies; most covered topics: general information about PMH and PMHPs; least covered topics: interviewing/counseling skills, psychopharmacology and suicide risk assessment). Eight studies (12.1%) reported on midwives’ mental health nursing experience (ranging from 0.8% to 30%) or placement experience in a mental health setting or a mother-baby unit during their studies (ranging to 9% to 23.2%). Four studies (6%) mentioned family or personal experience of mental health problems ranging from 25% to 66.3%. Most studies covered the entire perinatal period (n=44; 66.7%) and reported on PMHPs (n=32; 48.5%). The definition of PMHPs was highly variable across the studies (e.g. inclusion of conditions usually not considered as PMHPs, such as schizophrenia, bipolar disorder, personality disorders, self-harm, suicide eating disorders or SUD in 16 studies; definition restricted to anxiety, depression, postpartum psychosis and/or posttraumatic stress disorder in 9 studies; unspecified in 7 studies). One third of the included studies used validated instruments to assess outcomes (n=16; 36.4%). Five studies (7.6%) investigated the influence of cultural aspects on the detection and management of PMHPs.
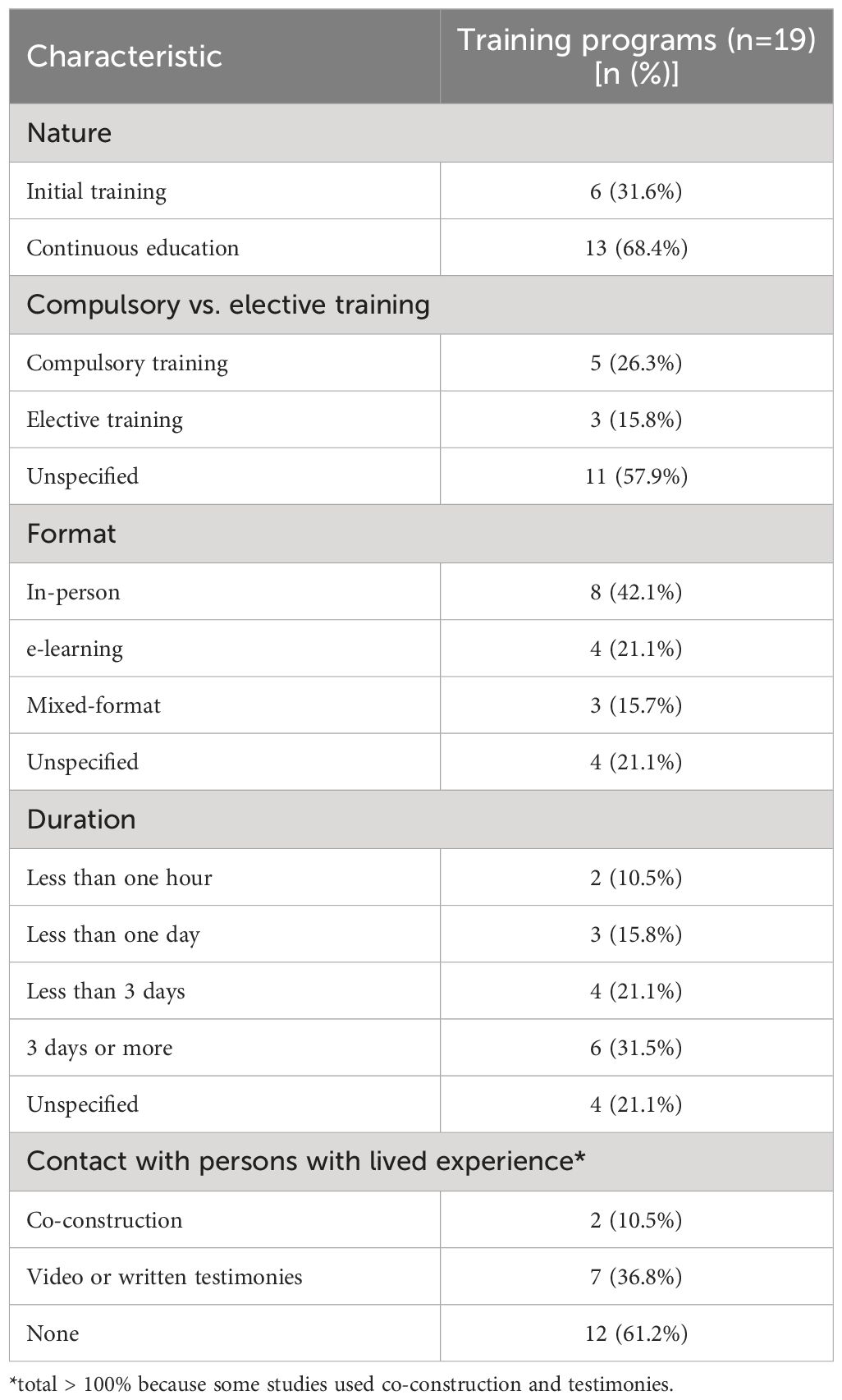
Of 15 studies reporting on a training program using a quantitative or a mixed-methods design, three used a waiting-list control group (20%; one randomized controlled trial (RCT)) and 13 (86.7%) were uncontrolled. Sample size was small in most studies (< 50 participants; n=9 studies). Nine studies (47.3%) reported contact with persons with lived experience when designing their training program. The training programs were heterogeneous in nature (initial training, n=6, 31.6%; continuous education, n=13, 68.4%), type, format and duration (ranging from 2 minutes to a fifteen-week module). All studies assessed training outcomes either immediately after (n=15; 79%) or up to 3 months after the intervention is delivered (n=4; 21%).
3.2 Quality assessment
The overall assessment score ranged from low (n=30, 45.4%; n=13, 68.4% for training programs) to high (n=11, 16.7%; n=2, 10.5%). For quantitative or mixed-methods studies, the reasons were convenience sampling (n=61 studies, 92.4%), sample size, low response rate (n=18 studies > 60%), limited use of validated outcome measures (36.4%), use of self-reported measures, absence or short duration of the follow-up period, limited integration of the results in mixed-methods studies and lack of controlled/RCT studies to evaluate the effectiveness of training programs. For qualitative studies, the reasons were interpretation bias (e.g. no investigator triangulation, the data being analyzed by only one researcher), absence of data saturation and lack of reflexivity.
3.3 Narrative review
Many studies found that midwives felt ill equipped to care for parents with PMHPs [e.g. ranging from 69.2% of 815 midwives in Jones et al., 2011 (17) to 82.2% of 157 midwives in Noonan et al., 2018 (28)]. The reasons included insufficient initial training/continuous education on PMH (n=2 studies), perception that PMH assessment is not part of their role (n=2 studies), lack of knowledge about the detection, referral and management of PMHPs (n=12 studies). Compared with other perinatal health providers (GPs, health visitors, maternal child health nurses; n=11 studies), midwives had lower knowledge on PMH (n=2), felt less confident in the detection, referral or management of PMHPs (n=3) and had more negative attitudes toward their role in perinatal mental healthcare (PMHC) (57) or suicide prevention (40). Self-reported barriers to discuss PMH issues or self-reported interviewing skills did not differ between nurses and midwives (25). Student midwives’ knowledge, skills and attitudes in PMH did not clearly differ from those of qualified midwives (n=5 studies). On the job experience, learning from peers and attending to workshops/conferences were midwives’ main sources of knowledge (n=3 studies).
The factors positively associated with knowledge about PMHPs included the perception to be well equipped to provide PMHC (66.7% significance), previous training in PMH (50% significance), younger age (17), shorter work experience in general and as a midwife (20% significance), frequent contact with parents with PMHPs (50% significance) and type of practice (33.3% significance). Mental health nursing experience was positively associated with the perception to be well equipped to provide PMHC, but not with higher knowledge about PMH (8). No significant association was found between confidence in providing PMHC and other factors [e.g. age, personal experience of mental health problems, frequent contact with parents with PMHPs (29)], except for PMH education and case identification (8). Compared with suicide risk assessment and other conditions (e.g. postpartum psychosis, SMI, eating disorders or posttraumatic stress disorder; n=4 studies), midwives reported higher knowledge, better skills and more confidence in detecting and managing perinatal depression and anxiety. Midwives felt in general ill equipped to care for postpartum psychosis, eating disorders, posttraumatic stress and SMI (n=10 studies) and reported ambivalent or negative attitudes toward parents with these conditions (n=7 studies). Knowledge about PMHPs varied according to the assessment method [i.e. higher self-report knowledge than researcher-rated knowledge (19, 43)] and the timing of perinatal period (i.e. higher in the postpartum than during pregnancy, n=5 studies).
3.3.1 Detection/screening
The practices and policies around screening for PMHPs varied across studies. There was a considerable overlap between the factors influencing the decision to screen, refer and support parents with PMHPs. Midwives’ attitudes toward their role in PMHC (e.g. personal interest in PMHPs and perception that it is part of their role) played a central role in decision-making about opening discussions about PMH (n=12 studies), referral (42, 57) and support parents with PMHPs (n=6). Cultural aspects and stigma toward parents with ethnic minority background (e.g. underestimation of depression and suicide risks) impacted midwives’ ability to detect and manage PMHPs and parents’ maternity care experiences (n=4 studies). Other common factors included lack of knowledge about PMHPs (n=20 studies), referral pathways (n=8) and treatment options (n=10), lack of time/clear referral pathways (n=22) and stigma related to preexisting mental health problems/SMI (n=8).
Midwives considered routine universal screening as useful in two studies (5, 56). Facilitators included self-efficacy in screening (n=10 studies), person-centered care (n=3), the presence of a specialist team (n=2 studies) and mandatory routine screening (n=2). Barriers to screening included longer work experience (42), lack of knowledge about screening tools (n=11 studies), local/national guidelines on screening (ranging from 12.8% to 53%, n=4 studies), and negative attitudes toward the use of formal screening tools (n=12 studies). The relationship between personal/family experience of PMHPs was either positive [e.g. reduces stigma and allows to relate with parents (29)] or negative (45). For student midwives, the presence of specialist midwives was both a facilitator [e.g. provides referral options and placement opportunities (50)] and a barrier to screening [e.g. perception that it is not part of their role (43)]. Of note, specialist midwives reported to lack confidence in opening discussions about PMH and to lack knowledge about SMI (21).
The reasons underlying negative attitudes toward the use of formal screening tools included perceiving the questions as intrusive (n=3 studies), not clearly understanding the purpose of doing so (n=3 studies), inexperience in conducting assessment and feeling compelled to undertake it as a standardized survey (23), the fear of “not doing it right” (n=2) and discomfort when disclosure occurs (n=7 studies). Some studies reported a flexible use of screening tools (e.g. modified wording or timing of the questions; n=4 studies) and one study outlined the importance of person-centered care in conducting assessment (23). Conversely, midwives who lacked clarity about their role in PMHC reported feelings of inadequacy resulting in a non-flexible use of screening tools and a distant and superficial manner of asking questions (23). Midwives reported to feel more comfortable in opening discussions about PMH during follow-up visits compared with the booking appointment (n=5 studies). Alternatives to formal screening included assessing previous psychiatric history/current symptoms (28), using general open-ended questions (n=5 studies), behavioral observation (n=4 studies) and labor debriefing (46). Training needs covered knowledge about PMHPs (n=9 studies), screening tools (n=4 studies) and cultural issues and interviewing/distress management skills (n=10 studies).
3.3.2 Referral/support
Midwives reported to feel confident in their ability to refer parents with PMHPs to other health providers including specialist mental health services (n=7 studies). The opposite was found for parents with postpartum psychosis, eating disorders or SMI. High self-reported confidence in referring parents to other providers did not in practice lead to a higher number of referrals (37). The proportion of midwives indicating to feel confident in supporting parents with PMHPs in self-report questionnaires ranged from 34% to 53% (n=5 studies). Accurate case identification (9), an established diagnosis of PMHP (53) and parents’ preferences (53) influenced decision-making about referral. Other factors included the intention to collaborate with other providers (n=2) or conversely a lack of trust/a reluctance to disclose sensitive information to other providers (n=3 studies).
3.3.3 Training outcomes
All training programs reported improved self-rated knowledge, skills, attitudes and confidence in screening, referring and supporting parents with PMHPs (n=19). Few significant positive training effects were reported due to small-sized samples and lack of controlled/RCT studies. Results included positive effects on empathic communication skills (62, 63), case identification (64, 65) and the detection of PMHPs in maternity wards (66–68). Contrasted results were found on the number of referrals [n=2 studies; 50% significance; positive effect on self-reported referrals in Pearson et al. (2019) (69) and no significant effect in Wickberg et al. (2005, 70)]. No significant effects were found on depressive symptoms (70) and attitudes toward providing psychological support to parents with PMHPs (63). Participants’ satisfaction rates were high, the insight provided by parents with lived experience of PMHP being determinant for student midwives (n=4 studies). Barriers included an excessive workload (71) and for student midwives, elective participation and late delivery within midwifery studies (72). No difference related to the format of the intervention was reported.
4 Discussion
To our knowledge, this systematic review of 66 studies is one of the first exploring both the training needs in PMH identified by student midwives and midwives and the training programs designed for this population. Overall, a main finding of this systematic review is that although detection, referral and support of parents with PMHPs are part of the essential competencies for midwifery practice according to the ICM (2019) (6), their effective translation into routine clinical practice may depend on midwives’ understanding of their role in PMHC, i.e. finding meaning in opening discussions about PMH with all parents and the perception that this is part of their routine clinical duties. This suggests that this factor should be targeted by raining interventions aiming at improving detection and management of PMHPs, above and beyond knowledge, confidence, and skills.
Extending the findings of previous reviews (7, 10, 11), we found that although most midwives consider they have a role in PMHC (this aligning with ICM essential competencies for midwifery practice; 2019 (6)), their understanding of that role remains often unclear. Several potential explaining factors have been identified. First, while this topic may be central for a meaningful engagement into providing PMHC, only a few training programs explored the role of midwives in PMHC (71, 73). Second, there is a view - in particular in student midwives - that addressing PMH needs is less a priority than addressing physical health needs and that other providers should assume this responsibility (31, 35, 39, 43, 50, 52). The interaction between this view, mental illness stigma and racism toward parents with ethnic minority background contributed to poorer maternity experiences and under-detection of PMHPs (19, 35, 73).
Third, some midwives consider their role as limited to assessing PMH and wellbeing and as appropriate, referring to other health providers (9, 18, 55, 57, 58), whereas others have a broad perception of their role that include providing support, psychoeducation and with adequate training counseling interventions (21, 24, 25, 42). Recent meta-analyses showed positive effects of midwife-led counseling on anxiety and depressive symptoms after at least 3 days of training (14, 74). This concurs with recent calls for a better integration of mental health and perinatal health care and an extension of the scope of midwifery practice to include strengths-based case management and psychological interventions for parents with PMHPs (50, 75–77). Given there is some degree of difference between midwives’ perception of their role in PMHC and what is required as essential competencies for midwifery practice (ICM, 2019) (6), an explicit focus on midwives’ role in PMHC should be made in initial and continuous midwifery education (72, 73, 76, 78). Fourth, most student midwives, midwives and specialist midwives reported negative attitudes toward parents with suicide ideations, postpartum psychosis and SMI (21, 35, 40, 43, 57, 79). Aligning with this, Hawthorne et al. (2020) (79) found that student midwives had more negative attitudes toward persons with mental illness compared with mental health nursing students. However, other studies reported that midwives consider caring for parents with these conditions as part of their role but felt ill equipped to do so and expressed the need for additional training (8, 28, 29, 34, 39, 49).
4.1 Implications for training interventions
While the need to improve midwives’ initial and continuous education in PMH is now well established (7, 10), student midwives, midwives and even specialist midwives continue reporting to feel ill prepared to care for parents with PMHP in particular in case of co-occurring SMI (9, 21, 24, 33, 34, 36). Moreover, the proportion of midwives who received education in PMH - in particular in topics such as mental health/suicide risk assessment - remains consistently low. Given suicide is the leading cause of maternal mortality in the 1st year postpartum in high-income countries, this is concerning (1, 80).
Aligning with previous research (7, 10, 11), this systematic review found that education/training programs had positive effects on proximal outcomes (e.g. midwives’ knowledge, skills, attitudes and confidence in providing PMHC) and contrasted effects on distal outcomes (e.g. screening in maternity wards, the number of referrals or depressive symptoms). This could be related to methodological bias (e.g. lack of RCT or quasi-experimental studies). There is a need for high-quality studies on interventions designed following the Medical Research Council framework for complex interventions (81), which proposes among other core elements to: 1) take into account the context of delivery; 2) use a clear theoretical basis (e.g. how the intervention is expected to produce positive effects and under which conditions) and; 3) promote a meaningful engagement of persons with lived experience among other relevant stakeholders.
According to Wadephul et al. (2018) (82) framework for assessing midwifery practice in PMH, knowledge, confidence, attitudes and organizational factors influence midwives’ ability to detect and manage PMHPs. However, higher knowledge about PMH does not necessarily translate into higher confidence in providing PMHC and the opposite (8). As reported in one of the articles included in this review (42) and aligning with the theory of planned behavior (82), additional factors such as individual values, e.g. personal interest in PMH, and behavioral intent (e.g. the intention to open discussions about PMH) could influence detection and decision-making about referral and support in PMHPs and thus be relevant for midwifery education.
To improve midwives’ engagement into PMHC, training programs should put PMH in context (e.g. the positive outcomes that could be achieved with appropriate support) before covering topics related to specific knowledge or skills (5, 38, 49, 50, 53, 54). Instead of focusing only on biomedical aspects (e.g. the signs, risk factors, consequences and treatments of PMHPs), programs should propose a continuum approach of PMH that covers the positive aspects of the person’s life including wellbeing and personal recovery (83–86).
Extending the findings of previous reviews (7, 10, 11), training programs should target student midwives, midwives and specialist midwives and cover interviewing and distress management skills with a focus on specific aspects (e.g. opening discussions without feeling intrusive, using flexibly screening tools and reacting in case of a positive answer) (5, 21, 38, 45, 49, 50, 53, 54). In addition, training programs should include clinical supervision by mental health providers during and after intervention delivery (14). Future studies should include a longer follow-up period, as the embedding of practice change requires a minimum of nine months after the intervention is delivered (87).
Finally, while contact with persons with lived experience is one of the most effective strategies to reduce mental illness stigma in the general public and in frontline health providers (88, 89), this review found a very low proportion of training programs that engaged persons with lived experience in the conception and delivery of the intervention. Initial and continuous midwifery education curriculums on PMH should involve persons with lived experience - co-design and co-intervention - and include content about personal recovery/person-centered care (72, 73, 81, 84, 90–92).
4.2 Limitations
There are limitations. First, despite a growing number of published studies on midwives’ training needs in PMH and training interventions designed for this population (n=66 studies in this review vs. n=22 (7); n=17 (10); n=43 (11);), the quality of the included studies remains low to moderate, a concerning finding given the clinical relevance of this topic that is also a considerable limitation. Among other methodological bias, the absence of a clear theoretical basis for designing interventions (81), the small or unjustified sample sizes, the lack of RCT/quasi-experimental studies, the absence of control groups (or active comparators in controlled studies) and the absence or short duration of follow-up makes unclear whether interventions have positive effects on proximal or distal outcomes. Future high-quality studies on this topic are therefore needed. Despite these limitations, the inclusion of quantitative, qualitative and mixed-methods studies provided a complete synthesis of the available evidence and consistent messages emerged across studies. Second, relevant studies may have been missed since we excluded studies published in other languages than English or French and did not include the grey literature in our searches.
5 Conclusion
This review generated novel insights to inform initial and continuous midwifery education curriculums on PMH (e.g. co-design with persons with lived experience, focus on midwives’ understanding on their role in PMHC or inclusion on content on person-centered care).
Author contributions
MD: Conceptualization, Formal analysis, Writing – original draft. CD: Writing – review & editing. ML: Conceptualization, Writing – review & editing. WB: Conceptualization, Data curation, Methodology, Writing – review & editing. CM: Writing – review & editing. JD: Conceptualization, Formal analysis, Project administration, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to thank Dr. M.F.M. Engel and Mrs. C.D. Niehot medical information specialist from the Erasmus MC Medical Library for updating the search strategies. The authors are grateful to the reviewers of a previous version of the manuscript for their helpful comments.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1345738/full#supplementary-material
Supplementary Table 1 | Search strategy, search terms and syntax.
Supplementary Table 2 | List of excluded studies.
Supplementary Table 3 | List of included studies.
Supplementary Table 4 | Characteristics of included studies about midwives' knowledge, skills and attitude.
Supplementary Table 5 | Characteristics of included studies about midwives' needs for peripartum mental health training program.
Supplementary Table 6 | List of abbreviations.
References
1. Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. (2020) 19:313–27. doi: 10.1002/wps.20769
2. Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade: baby steps toward improving outcomes. J Clin Psychiatry. (2016) 77:1189–200. doi: 10.4088/JCP.15r10174
3. Moss KM, Reilly N, Dobson AJ, Loxton D, Tooth L, Mishra GD. How rates of perinatal mental health screening in Australia have changed over time and which women are missing out. Aust N Z J Public Health. (2020) 44:301–6. doi: 10.1111/1753-6405.12999
4. Kingston D, McDonald S, Tough S, Austin MP, Hegadoren K, Lasiuk G. Public views of acceptability of perinatal mental health screening and treatment preference: a population based survey. BMC Preg. Childbirth. (2014) 14:67. doi: 10.1186/1471-2393-14-67
5. Williams CJ, Turner KM, Burns A, Evans J, Bennert K. Midwives and women’s views on using UK recommended depression case finding questions in antenatal care. Midwifery. (2016) 35:39–46. doi: 10.1016/j.midw.2016.01.015
6. International Confederation of Midwives (ICM). Essential competences for midwifery practice (2019). Available online at: file:///C:/Users/marin/Downloads/icm-competencies-en-print-october-2019_final_18-oct-5db05248843e8.pdf.
7. Noonan M, Doody O, Jomeen J, Galvin R. Midwives’ perceptions and experiences of caring for women who experience perinatal mental health problems: An integrative review. Midwifery. (2017) 45:56–71. doi: 10.1016/j.midw.2016.12.010
8. Hauck YL, Kelly G, Dragovic M, Butt J, Whittaker P, Badcock JC. Australian midwives knowledge, attitude and perceived learning needs around perinatal mental health. Midwifery. (2015) 31:247–55. doi: 10.1016/j.midw.2014.09.002
9. Magdalena CD, Tamara WK. Antenatal and postnatal depression - Are Polish midwives really ready for them? Midwifery. (2020) 83:102646. doi: 10.1016/j.midw.2020.102646
10. Legere LE, Wallace K, Bowen A, McQueen K, Montgomery P, Evans M. Approaches to health-care provider education and professional development in perinatal depression: a systematic review. BMC Preg. Childbirth. (2017) 17:239. doi: 10.1186/s12884-017-1431-4
11. Branquinho M, Shakeel N, Horsch A, Fonseca A. Frontline health professionals’ perinatal depression literacy: A systematic review. Midwifery. (2022) 111:103365. doi: 10.1016/j.midw.2022.103365
12. Waqas A, Koukab A, Meraj H, Dua T, Chowdhary N, Fatima B, et al. Screening programs for common maternal mental health disorders among perinatal women: report of the systematic review of evidence. BMC Psychiatry. (2022) 22:54. doi: 10.1186/s12888-022-03694-9
13. Beck A, Hamel C, Thuku M, Esmaeilisaraji L, Bennett A, Shaver N, et al. Screening for depression among the general adult population and in women during pregnancy or the first-year postpartum: two systematic reviews to inform a guideline of the Canadian Task Force on Preventive Health Care. Syst Rev. (2022) 11:176. doi: 10.1186/s13643-022-02022-2
14. Wang TH, Tzeng YL, Teng YK, Pai LW, Yeh TP. Evaluation of psychological training for nurses and midwives to optimise care for women with perinatal depression: a systematic review and meta-analysis. Midwifery. (2022) 104:103160. doi: 10.1016/j.midw.2021.103160
15. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
16. Bramer WM, Milic J, Mast F. Reviewing retrieved references for inclusion in systematic reviews using EndNote. J Med Libr Assoc. (2017) 105:84–7. doi: 10.5195/jmla.2017.111
17. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ knowledge of antenatal and postpartum depression: a national survey. J Midwifery Womens Health. (2011) 56:353–61. doi: 10.1111/j.1542-2011.2011.00039.x
18. Buist A, Bilszta J, Milgrom J, Barnett B, Hayes B, Austin MP. Health professional’s knowledge and awareness of perinatal depression: results of a national survey. Women Birth. (2006) 19:11–6. doi: 10.1016/j.wombi.2005.12.001
19. Işık SN, Bilgili N. Postnatal depression: Midwives’ and nurses’ knowledge and practices. Erciyes Med J. (2010) 32:265–74.
20. Salomonsson B, Alehagen S, Wijma K. Swedish midwives’ views on severe fear of childbirth. Sex Reprod Healthc. (2011) 2:153–9. doi: 10.1016/j.srhc.2011.07.002
21. Savory NA, Sanders J, Hannigan B. Midwives’ experiences of supporting women’s mental health: A mixed-method study. Midwifery. (2022) 111:103368. doi: 10.1016/j.midw.2022.103368
22. de Vries NE, Stramrood CAI, Sligter LM, Sluijs AM, van Pampus MG. Midwives’ practices and knowledge about fear of childbirth and postpartum posttraumatic stress disorder. Women Birth. (2020) 33:e95–e104. doi: 10.1016/j.wombi.2018.11.014
23. Andersen CG, Thomsen LLH, Gram P, Overgaard C. ‘It’s about developing a trustful relationship’: A Realist Evaluation of midwives’ relational competencies and confidence in a Danish antenatal psychosocial assessment programme. Midwifery. (2023) 122:103675. doi: 10.1016/j.midw.2023.103675
24. Carroll M, Downes C, Gill A, Monahan M, Nagle U, Madden D, et al. Knowledge, confidence, skills and practices among midwives in the republic of Ireland in relation to perinatal mental health care: The mind mothers study. Midwifery. (2018) 64:29–37. doi: 10.1016/j.midw.2018.05.006
25. Higgins A, Downes C, Carroll M, Gill A, Monahan M. There is more to perinatal mental health care than depression: Public health nurses reported engagement and competence in perinatal mental health care. J Clin Nurs. (2017) 27:e476–87. doi: 10.1111/jocn.13986
26. Higgins A, Downes C, Monahan M, Gill A, Lamb SA, Carroll M. Barriers to midwives and nurses addressing mental health issues with women during the perinatal period: The Mind Mothers study. J Clin Nurs. (2018) 27:872–1883. doi: 10.1111/jocn.14252
27. Keng SL. Malaysian midwives’ views on postnatal depression. Br J Midwifery. (2005) 13:78–86. doi: 10.12968/bjom.2005.13.2.17465
28. Noonan M, Jomeen J, Galvin R, Doody O. Survey of midwives’ perinatal mental health knowledge, confidence, attitudes and learning needs. Women Birth. (2018) 31:e358–66. doi: 10.1016/j.wombi.2018.02.002
29. Noonan M, Galvin R, Jomeen J, Doody O. Public health nurses’ perinatal mental health training needs: A cross sectional survey. J Adv Nurs. (2019) 75:2535–47. doi: 10.1111/jan.14013
30. Stewart C, Henshaw C. Midwives and perinatal mental health. Br J Midwifery. (2002) 10:117–21. doi: 10.12968/bjom.2002.10.2.10186
31. Edge D. Falling through the net - black and minority ethnic women and perinatal mental healthcare: health professionals’ views. Gen Hosp Psychiatry. (2010) 32:17–25. doi: 10.1016/j.genhosppsych.2009.07.007
32. Whitehead R, O’Callaghan F, Gamble J, Reid N. Contextual influences experienced by Queensland midwives: a qualitative study focusing on alcohol and other substance use during pregnancy. Int J Childbirth. (2019) 9:80–91. doi: 10.1891/2156-5287.9.2.80
33. Cunningham C, Galloway S. Let’s end the postcode lottery. Community Practitioner. (2019) 92:26–9.
34. Dubreucq M, Jourdan S, Poizat A, Dubreucq J. Ressenti des sages-femmes dans la prise en charge en suites de couche des patientes avec troubles psychiques sévères: une analyse qualitative (Midwives’ feelings about the post-partum care of women with severe mental illness: A qualitative analysis). Encephale. (2020) 46:226–30. doi: 10.1016/j.encep.2019.07.009
35. Phillips L. Assessing the knowledge of perinatal mental illness among student midwives. Nurse Educ Pract. (2015) 15:463–9. doi: 10.1016/j.nepr.2014.09.003
36. Bye A, Shawe J, Bick D, Easter A, Kash-Macdonald M, Micali N. Barriers to identifying eating disorders in pregnancy and in the postnatal period: a qualitative approach. BMC Preg. Childbirth. (2018) 18:114. doi: 10.1186/s12884-018-1745-x
37. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ awareness and management of antenatal and postpartum depression. Women Birth. (2012) 25:23–8. doi: 10.1016/j.wombi.2011.03.001
38. Oni HT, Buultjens M, Blandthorn J, Davis D, Abdel-Latif M, Islam MM. Barriers and facilitators in antenatal settings to screening and referral of pregnant women who use alcohol or other drugs: A qualitative study of midwives’ experience. Midwifery. (2020) 81:102595. doi: 10.1016/j.midw.2019.102595
39. McCauley K, Elsom S, Muir-Cochrane E, Lyneham J. Midwives and assessment of perinatal mental health. J Psychiatr Ment Health Nurs. (2011) 18:786–95. doi: 10.1111/jpm.2011.18.issue-9
40. Lau R, McCauley K, Barnfield J, Moss C, Cross W. Attitudes of midwives and maternal child health nurses towards suicide: A cross-sectional study. Int J Ment Health Nurs. (2015) 24:561–8. doi: 10.1111/inm.12162
41. Sanders LB. Attitudes, perceived ability, and knowledge about depression screening: a survey of certified nurse-midwives/certified midwives. J Midwifery Womens Health. (2006) 51:340–6. doi: 10.1016/j.jmwh.2006.02.011
42. Fontein-Kuipers YJ, Budé L, Ausems M, de Vries R, Nieuwenhuijze MJ. Dutch midwives’ behavioural intentions of antenatal management of maternal distress and factors influencing these intentions: an exploratory survey. Midwifery. (2014) 30:234–41. doi: 10.1016/j.midw.2013.06.010
43. Jarrett P. Student midwives’ knowledge of perinatal mental health. Br J Midwifery. (2015) 23:32–9. doi: 10.12968/bjom.2015.23.1.32
44. Shahid Ali S, Letourneau N, Rajan A, Jaffer S, Adnan F, Asif N, et al. Midwives’ perspectives on perinatal mental health: A qualitative exploratory study in a maternity setting in Karachi, Pakistan. Asian J Psychiatr. (2023) 80:103356. doi: 10.1016/j.ajp.2022.103356
45. Fletcher A, Murphy M, Leahy-Warren P. Midwives’ experiences of caring for women’s emotional and mental well-being during pregnancy. J Clin Nurs. (2021) 30:1403–16. doi: 10.1111/jocn.15690
46. Gibb S, Hundley V. What psychosocial well-being in the postnatal period means to midwives. Midwifery. (2007) 23:413–24. doi: 10.1016/j.midw.2006.07.005
47. Asare SF, Rodriguez-Muñoz MF. Understanding healthcare professionals’ Knowledge on perinatal depression among women in a tertiary hospital in Ghana: A qualitative study. Int J Environ Res Public Health. (2022) 19:15960. doi: 10.3390/ijerph192315960
48. Jomeen J, Glover LF, Davies SA. Midwives’ illness perceptions of antenatal depression. Br J Midwifery. (2009) 17:296–303. doi: 10.12968/bjom.2009.17.5.42221
49. McGlone C, Hollins Martin CJ, Furber C. Midwives’ experiences of asking the Whooley questions to assess current mental health: a qualitative interpretive study. J Reprod infant Psychol. (2016) 34:383–93. doi: 10.1080/02646838.2016.1188278
50. McGookin A, Furber C, Smith DM. Student midwives’ awareness, knowledge, and experiences of antenatal anxiety within clinical practice. J Reprod Infant Psychol. (2017) 35:380–93. doi: 10.1080/02646838.2017.1337270
51. Ross-Davie M, Elliott S, Sarkar A, Green L. A public health role in perinatal mental health: are midwives ready? Br J Midwifery. (2006) 14:330–4. doi: 10.12968/bjom.2006.14.6.21181
52. Schouten BC, Westerneng M, Smit AM. Midwives’ perceived barriers in communicating about depression with ethnic minority clients. Patient Educ Couns. (2021) 104:2393–9. doi: 10.1016/j.pec.2021.07.032
53. Madden D, Sliney A, O’Friel A, McMackin B, O’Callaghan B, Casey K, et al. Using action research to develop midwives’ skills to support women with perinatal mental health needs. J Clin Nurs. (2018) 27:561–71. doi: 10.1111/jocn.13908
54. Jarrett P. Attitudes of student midwives caring for women with perinatal mental health problems. Br J Midwifery. (2014) 22:718–24. doi: 10.12968/bjom.2014.22.10.718
55. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ attitudes towards care for women with emotional distress. Midwifery. (2012) 28:216–21. doi: 10.1016/j.midw.2010.12.008
56. Willey SM, Gibson-Helm ME, Finch TL, East CE, Khan NN, Boyd LM, et al. Implementing innovative evidence-based perinatal mental health screening for women of refugee background. Women Birth. (2020) 33:e245–55. doi: 10.1016/j.wombi.2019.05.007
57. Rothera I, Oates M. Managing perinatal mental health: A survey of practitioners’ views. Br J Midwifery. (2011) 19:04–313. doi: 10.12968/bjom.2011.19.5.304
58. McCann TV, Clark E. Australian Bachelor of Midwifery students’ mental health literacy: an exploratory study. Nurs Health Sci. (2010) 12:14–20. doi: 10.1111/j.1442-2018.2009.00477.x
59. Salomonsson B, Wijma K, Alehagen S. Swedish midwives’ perceptions of fear of childbirth. Midwifery. (2010) 26:327–37. doi: 10.1016/j.midw.2008.07.003
60. Nyberg K, Lindberg I, Öhrling K. Midwives’ experience of encountering women with posttraumatic stress symptoms after childbirth. Sex Reprod Healthc. (2010) 1:55–60. doi: 10.1016/j.srhc.2010.01.003
61. Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright (#1148552). (2018) Canadian Intellectual Property Office, Industry Canada.
62. Fox D, Solanki K, Brown G, Catling C, Scarf V, Sheehy A, et al. Perinatal mental healthcare: Developing skills in midwifery students. Women Birth. (2023) 36:167–70. doi: 10.1016/j.wombi.2022.11.005
63. Shinohara E, Ohashi Y, Hada A, Usui Y. Effects of 1-day e-learning education on perinatal psychological support skills among midwives and perinatal healthcare workers in Japan: a randomised controlled study. BMC Psychol. (2022) 10:133. doi: 10.1186/s40359-022-00832-6
64. Badiya PK, Siddabattuni S, Dey D, Hiremath AC, Nalam RL, Srinivasan V, et al. Task-sharing to screen perinatal depression in resource limited setting in India: Comparison of outcomes based on screening by non-expert and expert rater. Asian J Psychiatr. (2021) 62:102738. doi: 10.1016/j.ajp.2021.102738
65. Yamashita H, Ariyoshi A, Uchida H, Tanishima H, Kitamura T, Nakano H. Japanese midwives as psychiatric diagnosticians: application of criteria of DSM-IV mood and anxiety disorders to case vignettes. Psychiatry Clin Neurosci. (2007) 61:226–33. doi: 10.1111/j.1440-1819.2007.01659.x
66. Elliott S, Ross-Davie M, Sarkar A, Green L. Detection and initial assessment of mental disorder: the midwife’s role. Br J Midwifery. (2007) 15:759–64. doi: 10.12968/bjom.2007.15.12.27791
67. Jardri R, Maron M, Pelta J, Thomas P, Codaccioni X, Goudemand M, et al. Impact of midwives’ training on postnatal depression screening in the first week post delivery: a quality improvement report. Midwifery. (2010) 26:622–9. doi: 10.1016/j.midw.2008.12.006
68. Toler S, Stapleton S, Kertsburg K, Callahan TJ, Hastings-Tolsma M. Screening for postpartum anxiety: A quality improvement project to promote the screening of women suffering in silence. Midwifery. (2018) 62:161–70. doi: 10.1016/j.midw.2018.03.016
69. Pearson P, Klima C, Snyder M. Reducing barriers that hinder obstetric providers from addressing perinatal depression: A provider education module. J Dr Nurs Pract. (2019) 12:212–24. doi: 10.1891/2380-9418.12.2.212
70. Wickberg B, Tjus T, Hwang P. Using the EPDS in routine antenatal care in Sweden: a naturalistic study. J Reprod infant Psychol. (2005) 23:33–41. doi: 10.1080/02646830512331330956
71. Forrest E, Poat A. Perinatal mental health education for midwives in Scotland. Br J Midwifery. (2010) 18:280–4. doi: 10.12968/bjom.2010.18.5.47853
72. Higgins A, Carroll M, Sharek D. It opened my mind: student midwives’ views of a motherhood and mental health module. MIDIRS Midwifery Digest. (2012) 22:287–92.
73. Larkin V, Flaherty A, Keys C, Yaseen J. Exploring maternal perinatal mental health using a blended learning package. Br J Midwifery. (2014) 22:210–7. doi: 10.12968/bjom.2014.22.3.210
74. Wang TH, Pai LW, Tzeng YL, Yeh TP, Teng YK. Effectiveness of nurses and midwives-led psychological interventions on reducing depression symptoms in the perinatal period: A systematic review and meta-analysis. Nurs Open. (2021) 8:2117–30. doi: 10.1002/nop2.764
75. Laios L, Rio I, Judd F. Improving maternal perinatal mental health: integrated care for all women versus screening for depression. Australas Psychiatry. (2013) 21:171–5. doi: 10.1177/1039856212466432
76. Coates D, Foureur M. The role and competence of midwives in supporting women with mental health concerns during the perinatal period: A scoping review. Health Soc Care Community. (2019) 27:e389–405. doi: 10.1111/hsc.12740
77. WHO. Guide for integration of perinatal mental health in maternal and child health services. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO (2022).
78. Higgins A, Carroll M, Sharek D. Impact of perinatal mental health education on student midwives’ knowledge, skills and attitudes: A pre/post evaluation of a module of study. Nurse Educ Today. (2016) 36:364–9. doi: 10.1016/j.nedt.2015.09.007
79. Hawthorne A, Fagan R, Leaver E, Baxter J, Logan P, Snowden A. Undergraduate nursing and midwifery student’s attitudes to mental illness. Nurs Open. (2020) 7:1118–28. doi: 10.1002/nop2.494
80. ENCMM 6e rapport de l’Enquête Nationale Confidentielle sur les Morts Maternelles, 2013-2015. In: Les morts maternelles en France: mieux comprendre pour mieux prévenir. Santé publique France, Saint-Maurice. Available at: www.santepubliqueFrance.fr. 237 p.
81. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. (2021) 374:n2061. doi: 10.1136/bmj.n2061
82. Wadephul F, Jarrett PM, Jomeen J, Martin CR. A mixed methods review to develop and confirm a framework for assessing midwifery practice in perinatal mental health. J Adv Nurs. (2018) 74:2258–72. doi: 10.1111/jan.13786
83. Williams P. Mothers’ descriptions of recovery from postpartum depression. MCN Am J Matern Child Nurs. (2013) 38:276–81. doi: 10.1097/NMC.0b013e3182993fbf
84. Slade M, Bird V, Clarke E, Le Boutillier C, McCrone P, Macpherson R, et al. Supporting recovery in patients with psychosis through care by community-based adult mental health teams (REFOCUS): a multisite, cluster, randomised, controlled trial. Lancet Psychiatry. (2015) 2:503–14. doi: 10.1016/S2215-0366(15)00086-3
85. Law S, Ormel I, Babinski S, Plett D, Dionne E, Schwartz H, et al. Dread and solace: Talking about perinatal mental health. Int J Ment Health Nurs. (2021) 30 Suppl 1:1376–85. doi: 10.1111/inm.12884
86. Powell C, Bedi S, Nath S, Potts L, Trevillion K, Howard L. Mothers’ experiences of acute perinatal mental health services in England and Wales: a qualitative analysis. J Reprod Infant Psychol. (2022) 40:155–67. doi: 10.1080/02646838.2020.1814225
87. Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs: the four levels. 3rd ed. San Francisco, CA: Berrett-Koehler Publishers, Inc (2006).
88. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
89. Kohrt BA, Jordans MJD, Turner EL, Rai S, Gurung D, Dhakal M, et al. Collaboration with people with lived experience of mental illness to reduce stigma and improve primary care services: A pilot cluster randomized clinical trial. JAMA Netw Open. (2021) 4:e2131475. doi: 10.1001/jamanetworkopen.2021.31475
90. Davies L, Page N, Glover H, Sudbury H. Developing a perinatal mental health module: An integrated care approach. Br J Midwifery. (2016) 24:118–21. doi: 10.12968/bjom.2016.24.2.118
91. Verbiest S, Tully K, Simpson M, Stuebe A. Elevating mothers’ voices: recommendations for improved patient-centered postpartum. J Behav Med. (2018) 41:577–90. doi: 10.1007/s10865-018-9961-4
Keywords: midwifery, perinatal care, mental health services, education, attitude of health personnel, literature review
Citation: Dubreucq M, Dupont C, Lambregtse-Van den Berg MP, Bramer WM, Massoubre C and Dubreucq J (2024) A systematic review of midwives’ training needs in perinatal mental health and related interventions. Front. Psychiatry 15:1345738. doi: 10.3389/fpsyt.2024.1345738
Received: 28 November 2023; Accepted: 02 April 2024;
Published: 22 April 2024.
Edited by:
Maria Muzik, University of Michigan, United StatesReviewed by:
Lisa Kane Low, University of Michigan, United StatesJoanne Bailey, University of Michigan, United States
Copyright © 2024 Dubreucq, Dupont, Lambregtse-Van den Berg, Bramer, Massoubre and Dubreucq. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marine Dubreucq, bWFyaW5lLmJlbmVAaG90bWFpbC5mcg==
 Marine Dubreucq
Marine Dubreucq Corinne Dupont2,3
Corinne Dupont2,3 Mijke P. Lambregtse-Van den Berg
Mijke P. Lambregtse-Van den Berg Wichor M. Bramer
Wichor M. Bramer Catherine Massoubre
Catherine Massoubre