
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 20 March 2024
Sec. Adolescent and Young Adult Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1343792
 Junxiang Cheng1,2
Junxiang Cheng1,2 Juan Zhao1
Juan Zhao1 Baoli Song1
Baoli Song1 Hong Han3
Hong Han3 Na Liu4
Na Liu4 Yangjie Chen1
Yangjie Chen1 Xiaomei Liu1
Xiaomei Liu1 Yue Dong5
Yue Dong5 Weina Bian6
Weina Bian6 Zhifen Liu1*
Zhifen Liu1* Shifan Han1,2*
Shifan Han1,2*Background: Nonsuicidal self-injury (NSSI) among adolescents is a growing global concern. However, effective interventions for treating NSSI are limited.
Method: A 36-week quasi-experimental study design of parent–child group resilience training (intervention group) for adolescents aged 12–17 years was used and compared with treatment-as-usual (control group). The primary endpoint was the frequency of NSSI assessed with the Ottawa Self-Injury Inventory (OSI), and the secondary endpoints were the levels of depression, hope, resilience, and family adaptability and cohesion as assessed by the 24-item Hamilton depression rating scale (HAMD-24), Herth Hope Scale (HHS), Connor-Davidson Resilience Scale (CD-RISC), and Family Adaptability and Cohesion Evaluation Scale, second edition (FACES-II-CV), respectively.
Result: A total of 118 participants completed the trial. Both groups showed a significant reduction in NSSI frequency after 12, 24, and 36 weeks of intervention (p< 0.05), although the intervention group did not differ significantly from the control group. After 12, 24, and 36 weeks of intervention, the CD-RISC, HHS, HAMD-24, and FACES-II-CV scores in the intervention and control groups improved over baseline (p< 0.05). Furthermore, the intervention group had higher scores on the CD-RISC, HHS, and FACES-II-CV and lower scores on the HAMD-24 than the control group after 12, 24, and 36 weeks of intervention (p < 0.05).
Conclusion: Parent–child group emotional regulation and resilience training showed promise as treatment options for NSSI among adolescents, leading to increased hope, resilience, and improved family dynamics among NSSI teens. Moreover, NSSI frequency significantly decreased in the intervention group compared to baseline.
Nonsuicidal Self-injury (NSSI) refers to the act of intentionally injuring one’s own body through scratching, cutting, biting, or scalding without suicidal intention (1). A study conducted by the Centers for Disease Control (CDC) in the USA revealed that the prevalence of NSSI typically peaks during adolescence, around the ages of 15–16, with a rate of 15.3% (2). Zhang et al. reported that at least one instance of NSSI occurred in 21.7% of individuals and that its onset occurred earlier in females compared to in males (3). Although NSSI and suicidal behavior are different diagnoses in the Diagnostic and Statistical Manual of Mental Disorders Fifth edition (DSM-V), studies have found that non-suicidal self-injury is often a precursor to suicide and is considered a significant risk factor for suicide (4–6). The high prevalence of NSSI and its association with attempted and completed suicides impose a substantial financial burden on families and societies, making it a pressing public health concern (7).
The onset of NSSI in adolescents is a complex phenomenon influenced by multiple factors, including psychological factors, problematic parental relationships, adverse childhood experiences, rumination, and sleep disorders (8–11). Parent–child relationships play a crucial role in children’s development at all stages. The biosocial model posits that early vulnerability and family environment risk factors may contribute to more severe emotional and behavioral dysregulation, such as NSSI (12, 13). A longitudinal cohort study showed that poor-quality attachment to parents could predict the frequency of NSSI (14). Findings from China also demonstrated that poor parent–child relationships are a high-risk factor for adolescent NSSI (11, 15). NSSI not only affects adolescents themselves, but it also has a substantial impact on the entire family. Parents constantly navigate a delicate balance and are unaware of words or events that might trigger their children’s self-harming behavior. This constant state of tension can lead to “empathetic burnout,” where parents struggle to respond with compassion. Moreover, the negative emotions experienced by adolescents in response to their parents’ reactions can further exacerbate their self-injurious behavior (16). The human birth theory suggests that defects in the mother-newborn relationship from birth to one year of age may be associated with the development of mental illness later in adolescence. If the needs of the newborn’s development and the relationship with caregivers are not met, this hidden deficiency may lead to mental disordor in the child during the puberty (17). Therefore, improving the quality of parent–child relationships is an essential factor in preventing self-injurious behavior in adolescents.
A study found a negative association between adolescent resilience and NSSI (18). Resilience is a multidimensional and dynamic process that encompasses the development of a sense of purpose or meaning in life, positive emotions, self-esteem, positive coping strategies, optimism, social support, and cognitive flexibility (19, 20). It is a positive personality trait that enables individuals to effectively deal with adverse and stressful situations and can be enhanced through training (21). A high level of resilience indicates strong coping abilities and adaptability, enabling individuals to maintain a positive perspective and effectively navigate future adversities (11, 18). Therefore, resilience training is a viable and potentially valuable intervention for promoting patient well-being.
Stress management and resilience training (SMART) was set up by health managers Werneburg et al. at the Mayo Clinic in Rochester, USA (22). Previous studies have shown that SMART training improves resilience among medical practitioners, breast cancer patients after surgery, and patients with major depressive disorder, reducing their anxiety, depression, and stress levels (22–24). However, to the best of our knowledge, no study has reported the effects of SMART on NSSI in adolescents. Herein, we hypothesized that parent–child emotional regulation and resilience group training conducted by professional psychotherapists based on SMART might reduce the frequency of adolescent NSSI behavior by improving the parent–child relationship and resilience.
Adolescent inpatients were recruited from the Mental Health Department of the First Hospital of Shanxi Medical University between April 2020 and September 2021. The inclusion criteria were as follows: (1) engaging in NSSI for at least five days during the previous six months and at least once during the past month, and (2) aged 12–17 years old. The exclusion criteria were as follows: (1) acute psychotic symptoms, acute intent to self-harm, or suicidal thoughts or behaviors; (2) inability of parents or patients to cooperate with 12 weeks of training therapy; (3) diagnosis of other somatic or psychotic diseases; (4) receiving non-convulsive electroconvulsive therapy (MECT) within the past two months; and (5) parents with a previous or present diagnosis of mental illness. The recommended patients and their families were informed about the treatment and signed informed consent forms if they agreed to participate. Both patients and their parents signed informed consent forms, and the study was reviewed and approved by the Ethics Committee of the First Hospital of Shanxi Medical University (ethics number: k-k159). A total of 132 adolescents were admitted and assigned numbers at the time of recruitment, with odd numbers assigned to the intervention group and even numbers assigned to the control group, maintaining a 1:1 allocation ratio. Two experienced clinical psychologists, who were blinded to the participant’s group allocation, conducted assessments and the Kappa value for the consistency test of scale assessment was 0.82 (p > 0.05).
The present study utilized a quasi-experimental design to compare the effects of parent–child group emotional regulation and resilience training with treatment as usual (TAU) on adolescent NSSI.
Participants were recruited based on recommendations from psychiatrists, residents, and nurses in the psychiatric ward (Figure 1). The investigators conducted baseline surveys and evaluations, and both groups completed a second assessment 12 weeks after enrollment; a third assessment was performed at 24 weeks, and a fourth assessment at 36 weeks. Psychotherapy was used in both groups of participants.
Brent and Kolko defined “psychotherapy as a modality of treatment in which the therapist and patient(s) work together to ameliorate psychopathologic conditions and functional impairment through focus on the therapeutic relationship; the patient’s attitudes, thoughts, affect, and behavior; and social context and development” (25). Although there are various clinical psychotherapy techniques, they are generally divided into individual therapy, group therapy, and family therapy according to the population. Polese et al. found that group therapy was effective in interventions for psychiatric disorders even in young patients suffering from psychosis who were resistant to pharmacotherapy (26).
Patients in the intervention group received parent–child group emotional regulation and resilience training conducted by the same psychotherapist and assistant in each session. The therapists in the intervention group were qualified psychotherapists with 10 years of experience, and the assistant was a graduate student in psychology. The intervention group was carried out in a group form and was divided into 11 closed groups, with each group consisting of 12 people, including six patients and their mothers or fathers. The training consisted of 12 weekly sessions, each lasting 80 minutes. The training schedule was agreed upon by the patients and their parents, and the training time per week was fixed for each group. The entire treatment, including the post-discharge phase, required discussions with parents and children to ensure adherence to the training schedule. Considering adolescents’ psychological characteristics, the training content integrated emotional regulation strategies and resilience training and focused on four areas: awareness of the propensity for nervous system stress, attention training, learning the five core principles of increased emotional resilience (gratitude, compassion, acceptance, meaning, and forgiveness), and relaxation training (Table 1).
During the sessions, participants were asked to practice in life scenarios and record the difficulties in daily practice for discussion. Each session included daily practice feedback on the previous and current training assignments. The day before each treatment, the assistant called the patients and parents to remind them of the upcoming training session to ensure their adherence.
The control group received routine treatment according to the psychiatrists’ treatment regimens, which commonly included weekly individual or group psychotherapy. To minimize the intervention bias in both groups, the control group required a minimum of 12 treatments. The psychotherapy content in the control group was not restricted and determined by the therapists. Psychotherapists in both groups received regular supervision. To minimize information bias among family members of patients in both groups, parents in both groups were required to attend the first session on “understanding NSSI.”
Patients’ demographic data were gathered through a semi-structured interview developed for this study. Sociodemographic data included gender, age, educational level, and family structure. Clinically relevant variables included the Ottawa Self-Injury Inventory (OSI), 24-item Hamilton Depression Rating Scale (HAMD-24), Herth Hope Scale (HHS), Connor-Davidson Resilience Scale (CD-RISC), and Family Adaptability and Cohesion Evaluation Scale, second edition (FACES-II-CV).
The Ottawa Self-Injury Inventory (OSI) is a self-report questionnaire used to assess NSSI across multiple dimensions, including self-harm frequency in the past 1, 6, and 12 months, as well as its functions, alternative coping strategies, and potential addictive features. In this study, the item “How often in the past month have you injured yourself without the intention to kill yourself?” was used to investigate the frequency of self-injury. The Cronbach’s α coefficient of the Chinese version of this questionnaire was 0.952 (3).
The HAMD-24 (27) Chinese version is a commonly used clinical depression assessment scale that assesses the severity of depression. The Cronbach’s α coefficient of the HAMD-24 in the present study was > 0.8, while test-retest reliability was > 0.7, indicating good internal consistency and stability across different studies.
The Herth Hope Scale (HHS) is a tool for evaluating patients’ hope and consists of 12 questions scored on a 4-point Likert scale. The total score ranged from 12 to 48 points (28), with a higher score indicating a higher level of hope, which may predict better outcomes for patients with psychological health issues (29).
The Connor-Davidson Resilience Scale (CD-RISC) is a concise self-assessment tool with 25 questions; a higher score indicates a higher level of resilience. The Cronbach’s α coefficient for the Chinese version was 0.97 (30). The reliability and validity of this scale have been demonstrated in community samples, primary care outpatients, and psychiatric outpatients (31).
The Chinese version of the Family Adaptability and Cohesion Evaluation Scale, second edition (FACES-II-CV) was used to assess family function, and it has shown good validity and reliability in different studies (32, 33). Adaptability refers to a family’s ability to adjust to problems that arise at different stages of development, whereas cohesion refers to the emotional connection between family members; the higher the score, the better the family’s adaptability and cohesion.
SPSS 26.0 was used for data analysis. All analyses were full analysis sets (FAS). Based on Cohen’s guidelines, with an expected medium effect in the intervention group (f = 0.25), power (1-β) set at 0.8, and α = 0.05, a minimum of 64 participants were needed in each group. Quantitative data following a normal distribution were expressed as mean ± SD, and intergroup comparisons were conducted using t-tests. Quantitative data that did not conform to a normal distribution were expressed as median (P25, P75), and intergroup comparisons were conducted using the Mann-Whitney U test. Numerical data were expressed as rates, and the chi-square test or Fisher’s exact test was used for intergroup comparisons. Repeated measures analysis of variance (ANOVA) was used to test the effects of group (intervention vs. control) and time (baseline, 12 weeks, 24 weeks, and 36 weeks) on the CD-RISC, HHS, HADM-24, and FACES-II-CV scores. The main effects of group and time, as well as their interaction effect, were examined.
To account for the potential correlation among the self-injury outcomes from repeated measures at baseline and post-test, data were analyzed using generalized estimating equations. Generalized estimating equations (GEE) also estimated the working correlation parameters for the total sample and detected differences between the intervention and control groups. The GEE models incorporated baseline data and changes in outcomes over time across different groups. The significance level was set at p< 0.05.
A total of 132 eligible participants were enrolled in the study and randomly allocated to the intervention (n = 66) or control (n = 66) group. The reasons for dropping out included being unable to contact (n = 9), not wanting to continue believing they were cured (n = 2), experiencing suicidal behavior and dropping out of the study (n = 1), and stopping intervention (n = 2). A total of 61 participants remained in the intervention group and 57 in the control group at the 36-week follow-up, with a follow-up completion rate of 89.4% (Figure 1).
Table 2 presents the patients’ demographic and clinical characteristics. The mean age of the subjects was 15.00 ± 1.00 years. The intervention group included 21 men and 40 women, and the control group comprised 25 men and 32 women. No significant differences were found in terms of gender, age, education level, or family structure between the intervention and control groups at baseline (p > 0.05).
No significant difference was observed in each score between the two groups at baseline (p > 0.05). After 12, 24, and 36 weeks of intervention, the CD-RISC, HHS, HAMD-24, and FACES-II-CV scores in the intervention and control groups improved over baseline. As shown in Figure 2, at 12 weeks of intervention, the CD-RISC and HHS scores of the intervention group reached their highest values, the HADM scores decreased with the increase in training time, and the FACES-II-CV scores improved with increasing training time. At the end of the intervention, the experimental group showed significant improvement compared to the control group, which suggests that the effects of the intervention were sustained during subsequent follow-up visits. The scores of the control group improved to some extent over time. Furthermore, the total CD-RISC, HHS, and FACES-II-CV scores were higher in the intervention group than in the control group after 12, 24, and 36 weeks of intervention (p < 0 .05 for all categories). Similarly, the HAMD-24 scores in the intervention group were lower than those in the control group after 12, 24, and 36 weeks of intervention (p< 0.05, Table 3). Moreover, the main effect of group (intervention vs. control) on the CD-RISC, HHS, HADM-24, and FACES-II-CV scores was significant, as was the effect of time (baseline, 12, 24, and 36 weeks). The interaction effect of group and time was also significant, which suggests that the intervention had different effects on the outcomes over time (Table 3).
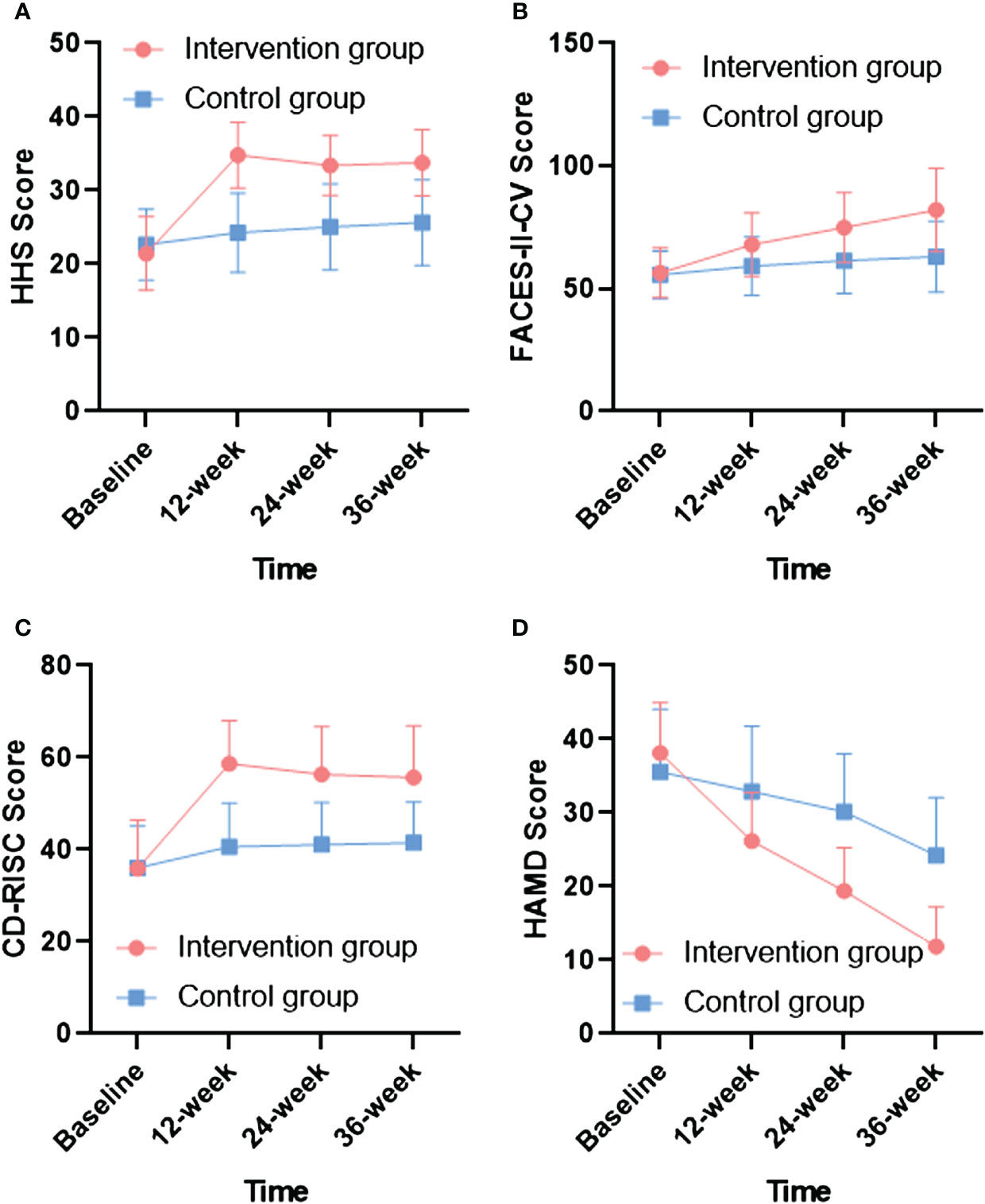
Figure 2 Comparison of HHS, FACES-II-CV, CD-RISC and HAMD-24 scores for intervention and control groups during different intervention times. (A) The changes of HHS scores in different intervention times; (B) The changes of FACES-II-CV scores in different intervention times; (C) The changes of CD-RISC scores in different intervention times; (D) The changes of HAMD-24 scores in different intervention times.
The GEE test showed that the frequency of NSSI in the control group was not significantly different from that in the intervention group (Wald = 0.55, p = 0.46 > 0.05, Table 4). In addition, the results of the repeated-measures time comparison showed that the frequency of self-injury improved in both groups after 12, 24, and 36 weeks of intervention compared to baseline (p< 0.05, Table 4).
SMART is widely used in various contexts; thus far, however, it has not been used in parent–child groups for adolescents with NSSI. The training content is based on conscious, short daily practice and is applicable to daily life scenarios, emphasizing attention training and developing a core mindset to reinterpret life events and consciously reconstruct them; helping participants learn novel cognitive, emotional, and behavioral strategies; and enhancing their sense of control (24). In the current study, we compared the effect of parent–child group emotion regulation and resilience training with usual treatment in adolescents with NSSI. The results showed that CD-RISC, HHS, HAMD-24, and FACES-II-CV scores improved in the intervention group compared to the control group; this suggests that parent–child group emotional regulation and resilience training can improve depression, hope, resilience, and adaptive and cohesive family functioning in adolescents with NSSI. However, no significant difference was observed in the frequency of self-injury between the two groups. The results indicated that adherence to individual or group therapy had comparable effects to that of the intervention group on self-injurious behaviour in adolescents with NSSI.
Parent–child group interventions may be more cost-effective than family therapy and provide ample opportunities for parents and adolescents to discuss NSSI and its implications for them. Furthermore, teens and parents can benefit from the support of other teens and parents. Parents who participate tend to gain a sense of belonging to the group, which also benefits their psychological well-being. For parents who lack knowledge about NSSI, the parent–child therapy model serves as a classroom where they can gain disease-related knowledge and conflict resolution skills, which allows them to actively participate in their children’s recovery process (34). Mutual encouragement and support from parents in the group may also contribute to maintaining the intervention’s effectiveness. Furthermore, an environment with adult participation provides opportunities for social connection, socialization, and behavioral activation, which may be lacking in adolescent group therapy (35).
The psychological problem of adolescence may stem from the difficulty of the parent-child relationship or lack of security (etc.) during infancy or growth (17) so providing an environment for adolescents and parents to work together may also promote the repair of the parent-child relationship. The “gratitude and acceptance” training increases family intimacy and enables parents and children to express their love for each other, thus enhancing mutual understanding and creating a safe environment where parents and children can accept their imperfections. After excessive or unrealistic expectations are reduced, the parent–child relationship can be improved, eventually influencing NSSI behavior. This finding is consistent with a cohort study of 2,127 adolescents that explored the relationship between parent–child dynamics and NSSI, demonstrating that positive parental behaviors can reduce the incidence of NSSI (14). In addition, a harmonious family atmosphere fosters children’s resilience.
Resilience refers to an undisturbed mental health trajectory during periods of adversity or stress or successful recovery from temporary dysfunction (36). Resilience is the outcome of dynamic interactions between an individual and the environment, which can be modulated by both personal (e.g., optimism) and environmental factors (e.g., social support) and can be increased through intervention (37, 38). Although there was no statistical difference between the two groups in self-injury behavior, the reduction in HAMD score among adolescents in the intervention group may be attributed to the improvement in resilience, consistent with the findings of Seshadri et al. (37, 38). The practice of mindfulness meditation in the intervention group instructed patients and their parents to focus on the “present moment” without engaging in judgmental thinking. The cultivation of nonjudgmental thinking, focusing on the present moment and mental phenomena (e.g., physical sensations, thoughts, and emotions), along with attention training, enables patients to accept what is and helps them adapt to stress more calmly. By focusing on the present moment, one may become more aware of the positive aspects of life; therefore, mindfulness-based resilience interventions may enhance participants’ optimism or frequency of positive emotions. Conversely, learning to accept negative emotions and situations may improve participants’ cognitive flexibility (39, 40). Psychopathological theory suggests that emotional regulation dysfunction is primarily caused by mental inflexibility (41). Therefore, resilience interventions in intervention groups that adopt relaxation techniques, mindfulness concepts, and skills can improve the resilience of both adolescents and their parents, enhancing their ability to adapt to stress and fostering hope in life (42).
O’Doherty suggests that stimulating inner hope is a way to promote recovery in individuals experiencing psychological distress (43). Parent–child group therapy provides a continuous supportive environment for family members. Stressor analysis can help patients and parents become aware of the difficulties that adolescents face during this stage of life, and the parent–child interaction mode increases parents’ understanding of their children and improves their understanding of key psychosocial resources, such as inherent strengths and abilities. Alternatively, meditation also helps increase the participants’ hope levels. An intervention study with Indian college students found that meditation intervention improved students’ resilience and hope levels, and the two were positively correlated and mutually reinforcing; this is beneficial for buffering anxiety and depression and promoting positive mental health outcomes (44).
Nevertheless, no significant difference in NSSI frequency was observed between the intervention and control groups, which implies that the intervention program in this study was not more effective than the control program in reducing the occurrence of NSSI. This might be related to factors such as an insufficient sample size, short intervention duration, and lack of specificity in the intervention content of this study. However, both groups showed improved NSSI frequency after 12, 24, and 36 weeks of intervention compared to baseline. This may indicate that both regular psychological counseling and parent–child group emotion regulation and resilience training could alleviate adolescent self-injury behavior to some extent. Long-term interventions are needed to explore the long-term effects of parent–child group emotional regulation and resilience training on adolescent NSSI behavior.
Effect in intervention group persisted over time at follow-up may be due to the simultaneous involvement of parents and children, so that the family atmosphere does not change immediately with the end of treatment, as evidenced by the continuous decline in depression scores and the increase in family cohesion and hope levels. Future studies should extend follow-up to observe the long-term development and growth of adolescents and family under this intervention and supporting further clinical practice of non-pharmacological treatments for depression and NSSI in adolescents.
This study had some limitations. First, we only collected data from patients and did not evaluate the parents. Future studies should analyze parental contributions to the outcomes. Second, parents who were willing to spend time with their children to complete the entire study may have been strongly motivated to find an appropriate solution, which may have caused some sample bias.
Parent–child group emotional regulation and resilience training is a comprehensive training model that integrates cognitive training, positive thinking, relaxation, and other psychotherapeutic techniques to reduce NSSI behaviors in adolescents by enhancing parent–child relationships and fostering resilience in both parents and children. This study applied this method to adolescents with NSSI, increasing their hope and resilience levels and improving family harmony and resilience. Although the intervention group did not differ significantly from the control group in terms of reduced NSSI frequency, both groups exhibited a significant decrease in NSSI frequency compared to baseline.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by First hospital of Shanxi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
JC: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. JZ: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. BS: Conceptualization, Data curation, Resources, Writing – original draft, Writing – review & editing. HH: Data curation, Visualization, Writing – original draft, Writing – review & editing. NL: Data curation, Writing – original draft, Writing – review & editing. YC: Project administration, Visualization, Writing – original draft, Writing – review & editing. XL: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. YD: Data curation, Writing – original draft, Writing – review & editing. WB: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. ZL: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. SH: Data curation, Formal Analysis, Investigation, Project administration, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank participating families and the mental health staff in the first hospital of Shanxi medical university for their support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rodriguez-Blanco L, Carballo-Belloso JJ, de Leon S, Baca-Garcia E. A longitudinal study of adolescents engaged in Non-Suicidal Self Injury (NSSI): clinical follow-up from adolescence to young adulthood. Psychiatry Res. (2021) 297:113711. doi: 10.1016/j.psychres.2021.113711
2. Swannell SV, Martin GE, Page A, Hasking P, St JN. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. (2014) 44:273–303. doi: 10.1111/sltb.12070
3. Zhang F, Cloutier PF, Yang H, Liu W, Cheng W, Xiao Z. Non-suicidal self-injury in Shanghai inner bound middle school students. Gen Psychiatr. (2019) 32:e100083. doi: 10.1136/gpsych-2019-100083
4. Halicka J, Kiejna A. Non-suicidal self-injury (NSSI) and suicidal: Criteria differentiation. Adv Clin Exp Med. (2018) 27:257–61. doi: 10.17219/acem/66353
5. Groschwitz RC, Kaess M, Fischer G, Ameis N, Schulze UM, Brunner R, et al. The association of non-suicidal self-injury and suicidal behavior according to DSM-5 in adolescent psychiatric inpatients. Psychiatry Res. (2015) 228:454–61. doi: 10.1016/j.psychres.2015.06.019
6. Son Y, Kim S, Lee JS. Self-injurious behavior in community youth. Int J Environ Res Public Health. (2021) 18:1955. doi: 10.3390/ijerph18041955
7. Hauber K, Boon A, Vermeiren R. Non-suicidal self-injury in clinical practice. Front Psychol. (2019) 10:502. doi: 10.3389/fpsyg.2019.00502
8. Coleman SE, Dunlop BJ, Hartley S, Taylor PJ. The relationship between rumination and NSSI: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:405–43. doi: 10.1111/bjc.12350
9. Singhal N, Bhola P, Reddi V, Bhaskarapillai B, Joseph S. Non-suicidal self-injury (NSSI) among emerging adults: Sub-group profiles and their clinical relevance. Psychiatry Res. (2021) 300:113877. doi: 10.1016/j.psychres.2021.113877
10. Rahman F, Webb RT, Wittkowski A. Risk factors for self-harm repetition in adolescents: A systematic review. Clin Psychol Rev. (2021) 88:102048. doi: 10.1016/j.cpr.2021.102048
11. Fan YY, Liu J, Zeng YY, Conrad R, Tang YL. Factors associated with non-suicidal self-injury in chinese adolescents: A meta-analysis. Front Psychiatry. (2021) 12:747031. doi: 10.3389/fpsyt.2021.747031
12. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. Psychol Bull. (2009) 135:495–510. doi: 10.1037/a0015616
13. Thomassin K, Shaffer A, Madden A, Londino DL. Specificity of childhood maltreatment and emotion deficit in nonsuicidal self-injury in an inpatient sample of youth. Psychiatry Res. (2016) 244:103–8. doi: 10.1016/j.psychres.2016.07.050
14. Victor SE, Hipwell AE, Stepp SD, Scott LN. Parent and peer relationships as longitudinal predictors of adolescent non-suicidal self-injury onset. Child Adolesc Psychiatry Ment Health. (2019) 13:1. doi: 10.1186/s13034-018-0261-0
15. Shao C, Wang X, Ma Q, Zhao Y, Yun X. Analysis of risk factors of non-suicidal self-harm behavior in adolescents with depression. Ann Palliat Med. (2021) 10:9607–13. doi: 10.21037/apm-21-1951
16. Whitlock J, Lloyd-Richardson E, Fisseha F, Bates T. Parental secondary stress: the often hidden consequences of nonsuicidal self-injury in youth. J Clin Psychol. (2018) 74:178–96. doi: 10.1002/jclp.22488
17. Maccari S, Polese D, Reynaert ML, Amici T, Morley-Fletcher S, Fagioli F. Early-life experiences and the development of adult diseases with a focus on mental illness: The Human Birth Theory. NEUROSCIENCE. (2017) 342:232–51. doi: 10.1016/j.neuroscience.2016.05.042
18. Turner BJ, Chapman AL, Gratz KL. Why stop self-injuring? Development of the reasons to stop self-injury questionnaire. Behav MODIF. (2014) 38:69–106. doi: 10.1177/0145445513508977
19. Johnston MC, Porteous T, Crilly MA, Burton CD, Elliott A, Iversen L, et al. Physical disease and resilient outcomes: a systematic review of resilience definitions and study methods. PSYCHOSOMATICS. (2015) 56:168–80. doi: 10.1016/j.psym.2014.10.005
20. Kunzler AM, Helmreich I, Chmitorz A, Konig J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev. (2020) 7:CD012527. doi: 10.1002/14651858.CD012527.pub2
21. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8:e017858. doi: 10.1136/bmjopen-2017-017858
22. Sood A, Sharma V, Schroeder DR, Gorman B. Stress Management and Resiliency Training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore (NY). (2014) 10:358–63. doi: 10.1016/j.explore.2014.08.002
23. Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clin Breast CANCER. (2011) 11:364–8. doi: 10.1016/j.clbc.2011.06.008
24. Seshadri A, Clark MM, Kung S, Fuller-Tyszkiewicz M, Sood A, Dammen KC, et al. Feasibility study of stress management and resiliency training (SMART) in patients with major depressive disorder. Prim Care Companion CNS Disord. (2020) 22:364–8. doi: 10.4088/PCC.19m02556
25. Brent DA, Kolko DJ. Psychotherapy: definitions, mechanisms of action, and relationship to etiological models. J Abnorm Child Psychol. (1998) 26:17–25. doi: 10.1023/a:1022678622119
26. Polese D, Fornaro M, Palermo M, De Luca V, de Bartolomeis A. Treatment-resistant to antipsychotics: A resistance to everything? Psychotherapy in treatment-resistant schizophrenia and nonaffective psychosis: A 25-year systematic review and exploratory meta-analysis. Front Psychiatry. (2019) 10:210. doi: 10.3389/fpsyt.2019.00210
27. Sun XY, Li YX, Yu CQ, Li LM. [Reliability and validity of depression scales of Chinese version: a systematic review]. Zhonghua Liu Xing Bing Xue Za Zhi. (2017) 38:110–6. doi: 10.3760/cma.j.issn.0254-6450.2017.01.021
28. Chan KS, Li HC, Chan SW, Lopez V. Herth hope index: psychometric testing of the Chinese version. J Adv NURS. (2012) 68:2079–85. doi: 10.1111/j.1365-2648.2011.05887.x
29. Morote R, Hjemdal O, Krysinska K, Martinez UP, Corveleyn J. Resilience or hope? Incremental and convergent validity of the resilience scale for adults (RSA) and the Herth hope scale (HHS) in the prediction of anxiety and depression. BMC Psychol. (2017) 5:36. doi: 10.1186/s40359-017-0205-0
30. Kuiper H, van Leeuwen C, Stolwijk-Swuste JM, Post M. Measuring resilience with the Connor-Davidson Resilience Scale (CD-RISC): which version to choose? SPINAL CORD. (2019) 57:360–6. doi: 10.1038/s41393-019-0240-1
31. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). DEPRESS ANXIETY. (2003) 18:76–82. doi: 10.1002/da.10113
32. He XY, Hou CL, Huang ZH, Huang YH, Zhang JJ, Wang ZL, et al. Individuals at ultra-high risk of psychosis and first-degree relatives of patients with schizophreniaexperience impaired family functionality and social support deficit in comparison to healthy controls. Compr Psychiatry. (2021) 109:152263. doi: 10.1016/j.comppsych.2021.152263
33. Du N, Ran MS, Liang SG, SiTu MJ, Huang Y, Mansfield AK, et al. Comparison of family functioning in families of depressed patients and nonclinical control families in China using the Family Assessment Device and the Family Adaptability and Cohesion Evaluation Scales II. Ann Clin Psychiatry. (2014) 26:47–56.
34. Kelada L, Whitlock J, Hasking P, Melvin G. Parents’ Experiences of nonsuicidal self-injury among adolescents and young adults. J Child Family Stud. (2016) 25:3403–16.
35. Waals L, Baetens I, Rober P, Lewis S, Van Parys H, Goethals ER, et al. The NSSI family distress cascade theory. Child Adolesc Psychiatry Ment Health. (2018) 12:52. doi: 10.1186/s13034-018-0259-7
36. Kalisch R, Baker DG, Basten U, Boks MP, Bonanno GA, Brummelman E, et al. The resilience framework as a strategy to combat stress-related disorders. Nat Hum Behav. (2017) 1:784–90. doi: 10.1038/s41562-017-0200-8
37. Rutten BP, Hammels C, Geschwind N, Menne-Lothmann C, Pishva E, Schruers K, et al. Resilience in mental health: linking psychological and neurobiological perspectives. Acta Psychiatr Scand. (2013) 128:3–20. doi: 10.1111/acps.12095
38. Connor KM, Zhang W. Recent advances in the understanding and treatment of anxiety disorders. Resilience: determinants, measurement, and treatment responsiveness. CNS Spectr. (2006) 11:5–12. doi: 10.1017/s1092852900025797
39. Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J PSYCHOSOM Res. (2004) 57:35–43. doi: 10.1016/S0022-3999(03)00573-7
40. Dykens EM, Fisher MH, Taylor JL, Lambert W, Miodrag N. Reducing distress in mothers of children with autism and other disabilities: a randomized trial. PEDIATRICS. (2014) 134:e454–63. doi: 10.1542/peds.2013-3164
41. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. (2006) 44:1–25. doi: 10.1016/j.brat.2005.06.006
42. Senger AR. Hope's relationship with resilience and mental health during the COVID-19 pandemic. Curr Opin Psychol. (2023) 50:101559. doi: 10.1016/j.copsyc.2023.101559
43. Kartalova-O'Doherty Y, Tedstone DD. Recovering from recurrent mental health problems: giving up and fighting to get better. Int J Ment Health Nurs. (2010) 19:3–15. doi: 10.1111/j.1447-0349.2009.00636.x
Keywords: adolescent, emotional regulation, nonsuicidal self-injury, parent-child relation, resilience
Citation: Cheng J, Zhao J, Song B, Han H, Liu N, Chen Y, Liu X, Dong Y, Bian W, Liu Z and Han S (2024) Positive effects of parent–child group emotional regulation and resilience training on nonsuicidal self-injury behavior in adolescents: a quasi-experimental study. Front. Psychiatry 15:1343792. doi: 10.3389/fpsyt.2024.1343792
Received: 24 November 2023; Accepted: 06 March 2024;
Published: 20 March 2024.
Edited by:
Hanliang Fu, Xi’an University of Architecture and Technology, ChinaReviewed by:
Daniela Polese, Sant’Andrea University Hospital, ItalyCopyright © 2024 Cheng, Zhao, Song, Han, Liu, Chen, Liu, Dong, Bian, Liu and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhifen Liu, bGl1emhpZmVuNTUxOEAxNjMuY29t; Shifan Han, c2hpZmFuLmhhbkBzeG11LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.