- 1School of Public Health, North China University of Science and Technology, Tangshan, China
- 2Beijing Key Laboratory of Mental Disorders, National Clinical Research Center for Mental Disorders & National Center for Mental Disorders, Beijing Anding Hospital, Capital Medical University, Beijing, China
- 3Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
- 4Department of Psychiatry, Fengtai Mental Health Center, Beijing, China
- 5Independent Researcher, Beijing, China
Objective: The aim of this study was to investigate the impact of early life adversity on cognitive function in patients with schizophrenia, with a focus on social cognition (SC).
Methods: Two groups of patients with schizophrenia were recruited and matched on sociodemographic and clinical characteristics. One group consisted of 32 patients with a history of childhood trauma (SCZ-ct), and the other group consisted of 30 patients without a history of childhood trauma (SCZ-nct). In addition, 39 healthy controls without a history of childhood trauma (HC-nct) were also recruited. The intelligence of the three groups was assessed using the Wechsler Abbreviated Scale of Intelligence (WAIS—RC) short version. The cognitive function evaluation was conducted using the MATRICS Consensus Cognitive Battery (MCCB), and early life adversity was measured using the Childhood Trauma Questionnaire-Short Form (CTQ) and Bullying Scale for Adults (BSA).
Results: Patients with schizophrenia endosed significantly higher scores on the CTQ (F=67.61, p<0.001) and BSA (F=9.84, p<0.001) compared to the HC-nct. Analysis of covariance (ANCOVA) and post-hoc analyses revealed that SCZ-ct (F=11.20, p<0.001) exhibited the most pronounced cognitive impairment among the three groups, as indicated in MCCB total scores and in the domain score of SC. CTQ exhibited a negative correlation with MCCB (r=-0.405, p< 0.001); SC was negatively correlated with physical abuse (PA) of CTQ (r=-0.271, p=0.030) and emotional abuse (EA) of BSA (r=-0.265, p=0.034) in the whole patient sample. Higher SC performance was significantly predicted by CT_total (Beta =-0.582, p<0.001, 95% CI -0.96-0.46), and years of education (Beta=0.260, p =0.014, 95% CI 0.20-1.75) in schizophrenia.
Conclusions: Besides familial trauma, schizophrenia patients appear to have a higher likelihood of experiencing bullying in their early life. These experiences seem to contribute significantly to their severe impairments in SC.
1 Introduction
Schizophrenia is recognized as a severe and complex mental disorder (1, 2) that is often associated with impairments in social cognitive (SC) function (3–5). Patients with schizophrenia may experience difficulties in accurately understanding the emotions, intentions, and social norms of others (6, 7). These issues frequently lead to conflicts and instances of aggressive behavior between patients with schizophrenia and their close caregivers, resulting in strained interpersonal relationships (8, 9). Consequently, these factors disrupt normal social interactions and significantly impact the individual’s quality of life and career development (10, 11).
The pathogenic mechanisms underlying schizophrenia are not yet fully elucidated. Besides genetic dispositions, previous research has focused on sociopsychological factors (5, 12). Among these factors, childhood trauma (CT) has been proposed as a potential risk factor for schizophrenia onset (13–15). This includes experiences such as physical abuse, emotional abuse, sexual abuse, physical neglect, and emotional neglect (14, 16, 17). These traumatic experiences may not only potentially heighten the risk of adolescents exhibiting psychotic symptoms (17–19) but also increase their vulnerability to the development of schizophrenia (20).
Furthermore, experiences of bullying during adolescence may serve as another potential factor in the onset of schizophrenia (12, 21). A study found that boys who frequently engage in bullying behaviors, or those who frequently find themselves the victims of such behaviors, are more susceptible to developing schizophrenia in early adulthood (22). This finding is further substantiated by a longitudinal investigation involving 4,720 participants, which concluded that regardless of whether one is a perpetrator or victim of bullying, experiencing bullying during adolescence increases the risk of developing mental disorders (23). This body of evidence points toward a discernable connection between bullying and mental illness, specifically schizophrenia.
The cognitive function of patients with schizophrenia is impaired, as established by previous research (3, 4, 24, 25). However, limited studies have implemented the threshold value of the Childhood Trauma Questionnaire-Short Form (CTQ) to differentiate patients with schizophrenia who have experienced childhood trauma from those who have not and to investigate potential differences in cognitive functioning between these two groups. This is particularly significant in the context of their social cognition function, which significantly impacts their quality of life and successful reintegration into society. Existing literature suggests that exposure to social adversity during childhood may contribute to the formation of negative internal working models, selective attention toward emotional stimuli and greater difficulties with emotional self-regulation (26). Moreover, studies have revealed that CT can affect an individual’s social cognitive functioning, particularly in terms of their intimate relationship with their mother (5). The presence of physical neglect significantly influences the intimacy between patients with schizophrenia and their parents, standing as the most potent predictor for their challenges in emotional recognition (5).
The purpose of the present study was to explore the effects of self-reported CT and bullying on the cognitive function of schizophrenia patients, with a focus on social cognition. The hypotheses formulated for this study were as follows (1): Patients with schizophrenia are likely to have endured more adversities during their early life - as quantified by the CTQ and the Bullying Scale for Adults (BSA) - in comparison to those without any such diagnosis (2); Experiencing adversities during early life could potentially impair cognitive function, with a particular impact on SC.
2 Methods
2.1 Participant enrollment
A total of 32 schizophrenia patients with a history of childhood trauma (SCZ-ct), 30 schizophrenia patients without a history of childhood trauma (SCZ-nct), and 39 healthy controls (HC-nct) without childhood trauma or any form of mental illness were recruited for this study (see Table 1). Eligible patients were referred to the study from both inpatient and outpatient departments at Beijing Anding Hospital, Capital Medical University. The inclusion criteria for the study were as follows (1): a diagnosis of schizophrenia according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (2); a minimum of 9 years of education (3), an IQ of at least 80 (4), native Chinese speakers, and (5) aged between 18 and 60. Patients were excluded from the study if they had a history of substance abuse or had undergone any form of brain stimulation therapies within the 3 months prior to the study. The HCs were recruited from nearby communities. Prior to their participation, informed consent was obtained from all participants. The study protocol was approved by the Ethics Committee of Beijing Anding Hospital, Capital Medical University, and North China University of Science and Technology.
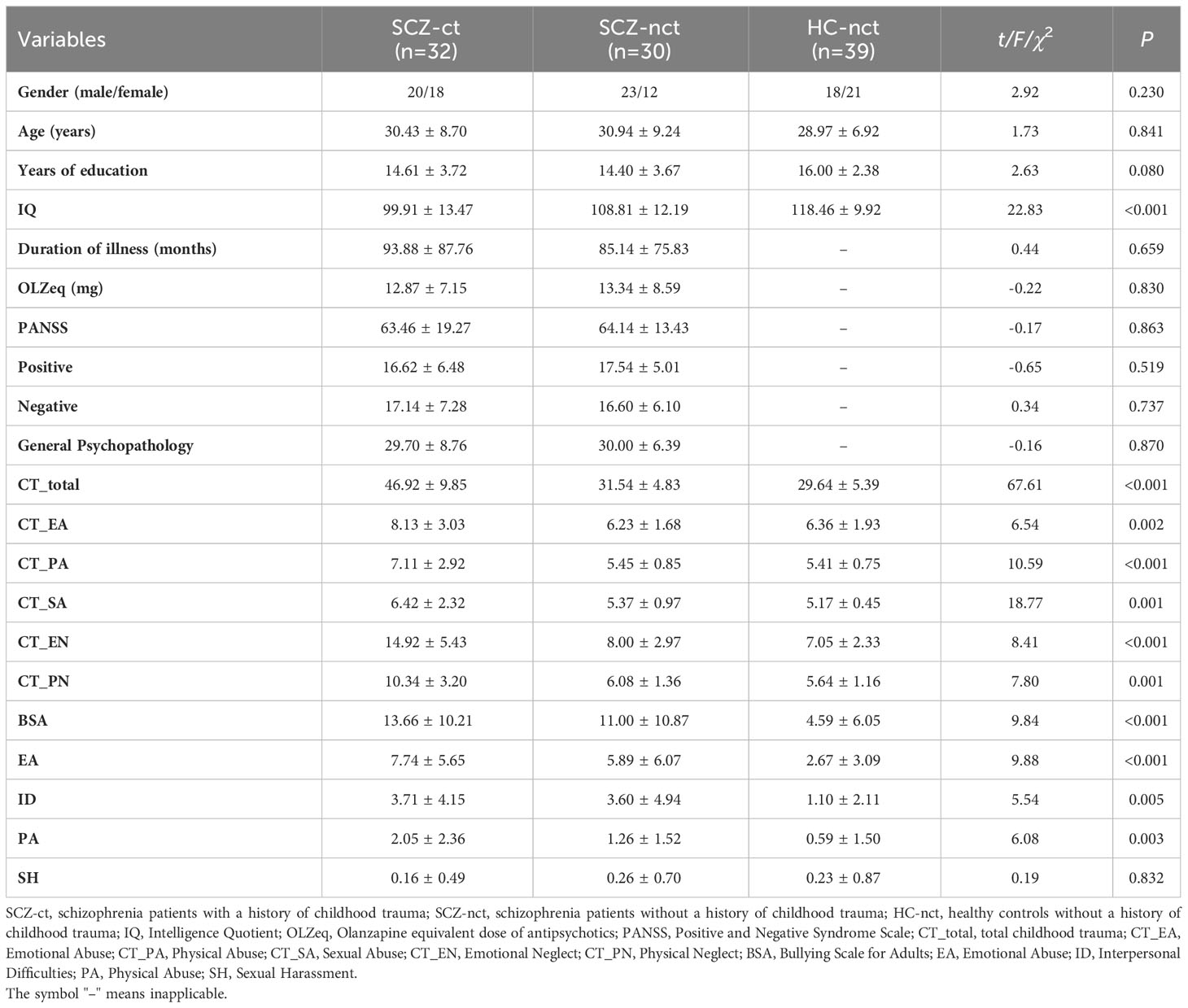
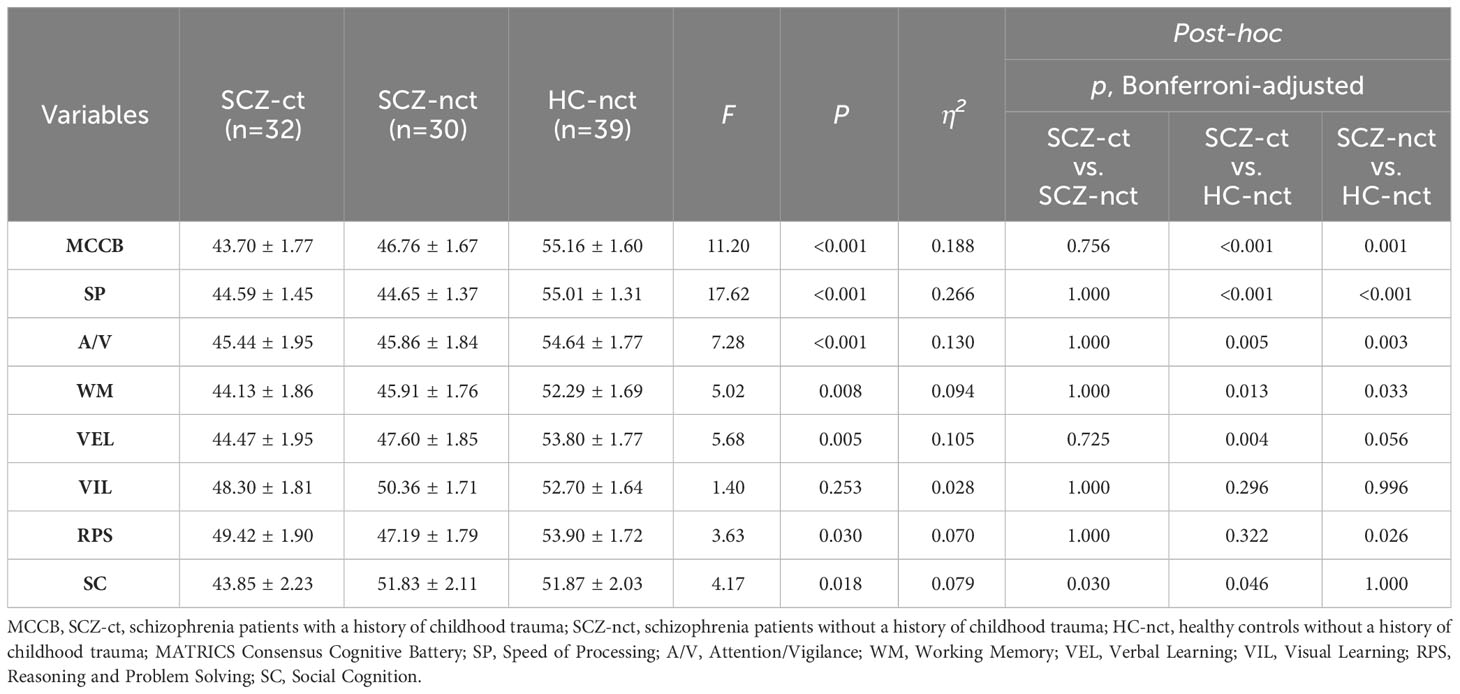
Table 1 Sociodemographic characteristics and early life adversities among the three groups of participants ().
2.2 Assessment
2.2.1 Clinical Assessments
The diagnosis of schizophrenia in patients was conducted using the Chinese version of the MINI International Neuropsychiatric Interview (MINI) (7.0.2) (27–29). The Chinese version of the Positive and Negative Syndrome Scale (PANSS) (30, 31) was administered to assess the clinical symptoms of patients with schizophrenia.
2.2.2 Cognitive Assessments
The Wechsler Abbreviated Scale of Intelligence (WAIS—RC) short version (32, 33) was utilized to evaluate the intelligence of the three groups.
The MATRICS Consensus Cognitive Battery (MCCB) (34–37) was administered to measure cognitive function across the three groups. The MCCB has been developed for assessing the cognitive functions of schizophrenia and related disorders and has exhibited good reliability and small practice effects in a wide range of clinical studies in individuals with psychosis. There are 10 subtests in the Chinese version of MCCB (35) which are organized into the following 7 domains: 1. Speed of Processing (SP): Trail Making Test: Part A (TMT), Brief Assessment of Cognition in Schizophrenia (BACS): Symbol Coding, and Category Fluency Test: Animal naming (Fluency); 2. Attention/Vigilance (A/V): Continuous Performance Test-Identical Pairs (CPT-IP); 3. Working Memory (WM): Wechsler Memory Scale—Third Edition (WMS-III): Spatial Span; 4. Verbal Learning (VEL): Hopkins Verbal Learning Test—Revised (HVLT-R); 5. Visual Learning (VIL): Brief Visuospatial Memory Test-Revised (BVMT-R); 6. Reasoning and Problem Solving (RPS): Neuropsychological Assessment Battery (NAB): Mazes; 7. Social Cognition (SC): Mayer–Salovey–Caruso Emotional Intelligence Test (MSCEIT): Managing Emotions.
In particular, the Mayer–Salovey–Caruso Emotional Intelligence Test (MSCEIT) serves as a social cognitive measurement that evaluates the participant’s capacity to perceive, use, understand, and regulate emotions through a series of questions. The MSCEIT applies questions based on everyday situations to gauge the ability with which individuals navigate social tasks, interpret facial expressions, and address emotionally-charged problems (38, 39).
2.3 The childhood trauma questionnaire-short form
The CTQ developed by Bernstein and Fink (40, 41) was utilized in our study. The CTQ is a widely recognized self-assessment tool specifically designed to retrospectively evaluate experiences of maltreatment and neglect during childhood. This tool is composed of 28 items, each rated on a five-point Likert scale, with response options extending from “0” (indicating ‘never’) to “4” (indicating ‘very often’).
The CTQ assigns different threshold scores for each of its subscales: emotional abuse (EA) has a threshold of 13, physical abuse (PA) is set at 10, sexual abuse (SA) requires a minimum of 8, emotional neglect (EN) is set at 15, and physical neglect (PN) has a threshold of 10 (42). Patients with scores meeting or exceeding the designated threshold on any dimension are classified as SCZ-ct (42).
2.4 The Bullying Scale for Adults
The BSA, derived from the Bully Survey (43), was developed as a modified version to assess adults’ past experiences of bullying (44). The BSA comprises three distinct parts. Part A concentrates on personal experiences related to bullying. It includes 13 items representing four types of bullying behavior, namely Emotional Abuse (EA), Interpersonal Difficulties (ID), Physical Abuse (PA), and Sexual Harassment (SH). Participants rate each item using a five-point Likert scale, ranging from “0” (never) to “4” (always), with an additional option of “don’t know”. If a score other than “0” is selected, respondents are required to provide more detailed information regarding the perpetrator, time, and duration of the incidents. Part B examines the personal consequences of bullying, encompassing six items measured on a five-point Likert scale (“0-Never a problem” to “4-Always a problem”). Last, Part C includes two items that inquire about the experience of acting as a bullying perpetrator. Our previous study yielded favorable outcomes in terms of reliability and validity in the Chinese version of the BSA (45).
2.5 Statistical analysis
Statistical analysis was performed using SPSS 22.0 software. Categorical data were analyzed by the chi-square test. Analysis of covariance (ANCOVA) was employed to compare the differences in cognitive function among the groups, with IQ as a covariate. To understand the relationships between the variables, the Pearson correlation was applied. To investigate the influencing factors of SC, relevant sociodemographic and clinical variables were entered as independent variables in a stepwise multiple linear regression analysis. Numerical data are expressed as the mean ± standard deviation d. Multiple comparisons were adjusted using the Bonferroni correction, P<0.05 means the difference is statistically significant, and a two-tailed test is adopted.
3 Results
3.1 Sociodemographic characteristics and early life adversities
Six patients were excluded from the SCZ-ct group and 5 patients were excluded from the SCZ-nct group due to low IQ scores (IQ<80). Consequently, 32 SCZ-ct patients, 30 SCZ-nct patients and 39 heathy controls were included in the analyses. There was a significant difference in the scores of IQ among the three groups (Table 1). Post-hoc analyses revealed that individuals in SCZ-ct group had the lowest IQ scores (Supplementary Table 1). Apart from IQ, no statistically significant differences were observed in sociodemographic among the three groups or in the clinical features between the two groups of patients.
The BSA total score and dimensional scores were compared between SCZ-ct, SCZ-nct, and HC. One-way ANOVA and post hoc analyses showed that SCZ-ct had significantly higher scores in BSA (F=9.84, p<0.001), EA (F=9.88, p<0.001), ID (F=5.54, p =0.005), and PA (F=6.08, p =0.003) than HC-nct. SCZ-ct and SCZ-nct had comparable scores in BSA and all dimensional scores.
In the whole patient sample, the mean scores of BSA (F=9.84, p< 0.001) and ID (F=5.54, p=0.005) were significantly higher than that of HC-nct (Table 1; Supplementary Figure 1).
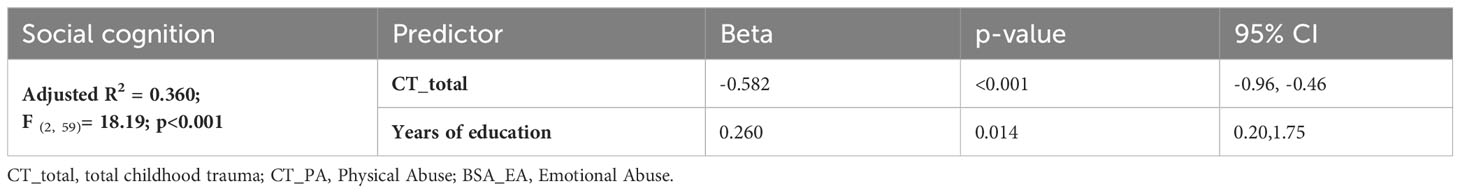
3.2 Cognitive result
Analysis of Covariance (ANCOVA) was conducted with IQ as a covariate, revealing significant differences in MCCB total score among the three groups (F=11.20, p<0.001). Post-hoc analyses indicated that SCZ-ct exhibited the most severe cognitive impairment with the lowest scores. Similar results were observed in several domain scores, including SP (F=17.62, p<0.001), A/V (F=7.28, p<0.001), WM (F=5.02, p=0.008), VEL (F=5.68, p=0.005), RPS (F=3.63, p=0.030), and SC (F=4.17, p=0.018). In terms of SC, the score of SCZ-nct was not significantly different from that of HC-nct (p=1.000) but was significantly higher than that of SCZ-ct (p=0.030) (Table 2; Figure 1).
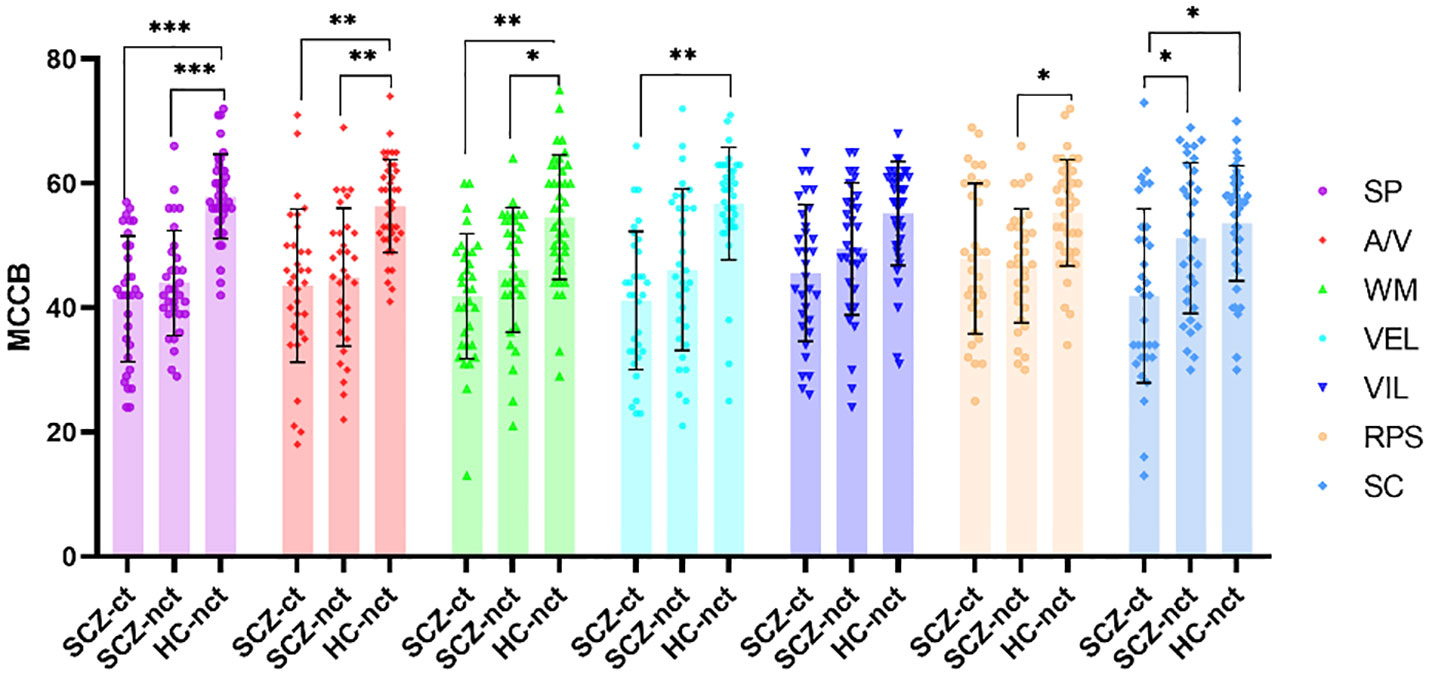
Figure 1 Comparisons of MCCB among three groups of participants. SCZ-ct, schizophrenia patients with a history of childhood trauma; SCZ-nct, schizophrenia patients without a history of childhood trauma; HC-nct, healthy controls without a history of childhood trauma; MCCB, MATRICS Consensus Cognitive Battery; SP, Speed of Processing; A/V, Attention/Vigilance; WM: Working Memory; VEL, Verbal Learning; VIL, Visual Learning; RPS, Reasoning and Problem Solving; SC, Social Cognition. *p<0.05; **p<0.01; ***p<0.001.
3.3 Correlation between CT, BSA and MCCB results
In the whole sample of schizophrenia patients, CTQ showed a significant negative correlation with MCCB (r = -0.405, p< 0.001), and CTQ_PA exhibited a negative association with the SC scores (r = -0.271, p = 0.030) on the MCCB. Furthermore, the BSA_EA exhibited a negative correlation with the SC scores (r = -0.265, p = 0.034) on the MCCB (Supplementary Table 2).
3.4 Exploring factors that predict SC function
In the stepwise linear regression analyses, SC was entered as the dependent variable, and the scores of CTQ, CTQ_PA, BSA_EA, and education were entered as independent variables. The results suggested that higher SC score was significantly predicted by CTQ (Beta =-0.582, p<0.001, 95% CI -0.96-0.46) and education (Beta = 0.260, p =0.014, 95% CI 0.20-1.75) in schizophrenia patients (Table 3).
4 Discussion
To the best of our knowledge, this is the first study in which the CTQ, BSA, and MCCB have been employed to examine the impact of early life adversity on cognitive functioning, particularly in the domain of SC, in patients with schizophrenia. The findings of the study have confirmed our hypothesis that, compared to healthy controls, patients with schizophrenia experience more early life adversity, including bullying. These early life adversities are associated with poorer cognitive functioning, especially SC, which has been considered to be closely related to quality of life and occupational development of the patients.
As hypothesized, patients with schizophrenia had significantly higher scores on the CTQ and BSA than healthy controls, which means that patients with schizophrenia experience more early life adversities. The study findings are in line with previous research studies. A meta-analysis of 36 studies (46) revealed that, compared to healthy controls, the odds ratio (OR) for CT in patients with schizophrenia was 2.78 (95% CI: 2.34-3.31). Specific forms of trauma showed an OR of 2.90 (95% CI: 1.71-4.92) for neglect, 3.40 (95% CI: 2.06-5.62) for emotional abuse, 2.95 (95% CI: 2.25-3.88) for physical abuse, and 2.38 (95% CI: 1.98-2.87) for sexual abuse. Another study (47) indicated that patients with schizophrenia had higher scores on measures of sexual abuse than healthy controls. According to a prospective cohort study (23) of 4720 children aged 8 to 11 years, children who reported bullying had a higher likelihood of developing a mental illness by age 18 than children who did not (OR=2.4, 95% CI: 1.6-3.4). A case‒control study (12) also found that schizophrenia patients were bullied twice as much as healthy controls. According to revictimization theory (48–50), individuals who experience childhood trauma may be more likely to become targets of bullying and attacks and are more likely to experience further trauma. A longitudinal study (51) validated this theory, as 213 (11.1%) out of 1915 young adults who experienced sexual abuse before adulthood reported experiencing sexual abuse again in adulthood.
SCZ-ct group was observed to have the lowest IQ scores among the three groups in the current study. This finding aligns with a 6-year follow-up study involving 1,119 patients with schizophrenia spectrum disorders. The study revealed that patients with schizophrenia spectrum disorders who had a history of childhood trauma exhibited the least progress in intellectual abilities, suggesting the lowest learning effect (52). Similar results were found in a study examining the impact of childhood trauma on intellectual functioning in patients with bipolar disorder, indicating that the presence of childhood trauma further impairs their intellectual abilities (53). This may be attributed to the negative effect of trauma on neural development, leading to alterations in brain structure and function (7, 54, 55).
In terms of SC, patients with schizophrenia have difficulty accurately understanding others’ emotions, intentions, and social signals when communicating with caregivers (5) or during social interactions. They may misunderstand others’ facial expressions, language, and nonverbal cues (6, 56), leading to poor communication and interpersonal tension. The results confirm our hypothesis that SC was significantly associated with childhood trauma, as indicated in the stepwise linear regression analyses. We found that the factors of “physical abuse” in CTQ and “emotional abuse” in BSA (bullying scales for adult) were significantly anti-correlated with social cognitive function (r = -0.271 and -0.265, respectively). In the multivariate regression, no specific type of trauma or bullying experience were identified to be independent predictors for social cognition, and the only contributor was the total score of CTQ (Beta=-0.582). This suggests that the social cognition impairments would better be explained by a cumulative effects of various kinds of childhood adversities.
Previous studies have shown that cognitive function is impaired in patients with schizophrenia (3, 4, 24, 25), with CT playing an important role in SC impairment in schizophrenia (5, 7, 26, 56–58). One study showed that schizophrenia patients had significantly lower scores in parental relationships and SC than healthy controls, with physical neglect being the strongest predictor of emotional recognition impairment. Good parental relationships were found to alleviate this emotional problem (5). Another survey involving 204 children aged 8-11 found that victims of bullying had difficulty in some moral judgment tasks (59), indicating that bullying has a negative impact on individuals’ SC. Furthermore, CT was found not only to affect the SC of schizophrenia patients but also to contribute to the cognitive impairment of bipolar disorder patients, specifically in working memory and executive function (60). A comprehensive review of 1,723 mood disorders and 797 healthy controls also confirmed that CT has a certain impact on the cognitive and executive functions of mood disorders (61).
Schizophrenia is a complex and severe mental disorder that involves various biological, psychological, social, and environmental factors (1, 2, 62–65), and CT increases the risk of developing this illness. Long-term and repeated exposure to negative environments, such as trauma and bullying, disrupts the balance of neurohormones (particularly glucocorticoids) (66), which can affect neuronal development and connectivity while altering epigenetic modifications (67). This process also impacts synaptic pruning during critical periods of early brain development (68, 69), as early life is a crucial period for individual brain development (53, 70, 71). Therefore, early-life adversities, including childhood trauma, disturb the balance of neurohormone secretion and lead to structural changes in the brain. These structural alterations can affect the cognitive functioning of patients with schizophrenia.
Notably, we found that the SC scores of SCZ-ct were significantly lower than those of SCZ-nct, while there was no significant difference in neural cognition dimensions (58, 72). It appears that CT independently contributes to the shaping of SC. Childhood is considered an important stage for both individual neural development and SC development (53, 70, 71, 73). During this period, the social environment in which children exist has a profound impact on their SC and behavioral patterns (74). According to Bowlby’s attachment theory (75), developing a secure attachment with a caregiver, especially one related to the mother, during childhood enables individuals to form a positive and secure “internal working model” in their interactions with others. This secure attachment relationship is an important prerequisite for successful social interactions. In contrast, experiencing adverse traumatic events during childhood, such as low levels of care and neglect, hinder the development of a secure attachment relationship, leading to difficulties in trusting others, exhibiting poor adaptability to the environment in adulthood (76), and even manifesting psychotic symptoms. Bowlby’s attachment theory (75) provides a cognitive-developmental framework for understanding the potential mechanisms by which early-life adversity may impact SC abilities later in life.
4.1 Limitations
There are some limitations to this study that need to be mentioned. First, the sample size employed was relatively small, thereby resulting in a decrease in statistical power. For example, no effort was made to match the intelligence levels among the three groups, although a covariance analysis was undertaken to mitigate the effects of intellectual impairment on the differences in cognitive function. Second, the study’s reliance on the self-assessment retrospective nature of the childhood trauma questionnaire introduces the possibility of potential recall biases in the patients’ reported experiences of childhood trauma. Furthermore, SC is a complex set of mental abilities that involve many aspects. A limitation of the MCCB is that there is only one test in the domain of SC. Future studies should consider the utilization of an integrated social cognition battery to assess various aspects of this cognitive function. Last but not least, additional variables such as genetic factors and psychiatric comorbidities could potentially confound the result but were not collected in the present study. These factors should be taken into consideration for a more comprehensive interpretation of the results in the future.
5 Conclusion
In addition to familial trauma, patients with schizophrenia are more susceptible to experiencing bullying during their early life. Both factors contribute significantly to the exacerbation of their social cognitive impairments. Our research enhances the understanding of the impact of early life adversity on cognitive functioning, specifically social cognitive function, in individuals with schizophrenia.
Moreover, the findings of this study offer valuable insights for the development of innovative psychological interventions. These interventions aim at alleviating the long-term repercussions of early life adversity for individuals with schizophrenia. This underscores not only the importance of childhood trauma experiences, which are currently considered during clinical assessments and treatment plans but also elevates the significance of bullying experiences in individuals with schizophrenia.
Therefore, to prevent and mitigate the lasting effects of childhood trauma and bullying on individual development and potential psychiatric disorders in individuals with schizophrenia, the development of new social-psychological intervention strategies is essential. These would facilitate their recovery and social reintegration.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of North China University of Science and Technology and the Ethics Committee of Beijing Anding Hospital, Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. W-PH: Writing – review & editing, Writing – original draft. Y-SD: Writing – review & editing, Writing – original draft. QW: Writing – review & editing, Data curation. FL: Writing – review & editing, Funding acquisition. SS: Writing – review & editing. C-CY: Writing – review & editing. X-JZ: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. F-CZ: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. C-YW: Conceptualization, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was sponsored by National Natural Science Foundation of China (Grant No. 82171501), Early Psychosis Cohort Program of Beijing Anding Hospital (Grant No. ADDL-03), Beijing Hospitals Authority Youth Program (Grant No. QML20231907) and STI2030-Major Projects (Grant No. 2021ZD0200701).
Acknowledgments
The authors would like to thank all the participants in this study. They are also very grateful to the referring physicians for their assistance with the project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1343188/full#supplementary-material
References
1. Jauhar S, Johnstone M, McKenna PJ. Schizophrenia. Lancet. (2022) 399:473–86. doi: 10.1016/S0140-6736(21)01730-X
2. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. (2010) 468:203–12. doi: 10.1038/nature09563
3. Mihaljević-Peleš A, Bajs JM, Šagud M, Živković M, Janović Š, Jevtović S. Cognitive deficit in schizophrenia: an overview. Psychiatr Danub. (2019) 31:139–42.
4. Gebreegziabhere Y, Habatmu K, Mihretu A, Cella M, Alem A. Cognitive impairment in people with schizophrenia: an umbrella review. Eur Arch Psychiatry Clin Neurosci. (2022) 272:1139–55. doi: 10.1007/s00406-022-01416-6
5. Rokita KI, Dauvermann MR, Mothersill D, Holleran L, Holland J, Costello L, et al. Childhood trauma, parental bonding, and social cognition in patients with schizophrenia and healthy adults. J Clin Psychol. (2021) 77:241–53. doi: 10.1002/jclp.23023
6. Thibaudeau É, Achim AM, Parent C, Turcotte M, Cellard C. A meta-analysis of the associations between theory of mind and neurocognition in schizophrenia. Schizophr Res. (2020) 216:118–28. doi: 10.1016/j.schres.2019.12.017
7. Quidé Y, Ong XH, Mohnke S, Schnell K, Walter H, Carr VJ, et al. Childhood trauma-related alterations in brain function during a Theory-of-Mind task in schizophrenia. Schizophr Res. (2017) 189:162–68. doi: 10.1016/j.schres.2017.02.012
8. Pawełczyk A, Łojek E, Radek M, Pawełczyk T. Prosodic deficits and interpersonal difficulties in patients with schizophrenia. Psychiatry Res. (2021) 306:114244. doi: 10.1016/j.psychres.2021.114244
9. Ford TC, Hugrass LE, Jack BN. The relationship between affective visual mismatch negativity and interpersonal difficulties across autism and schizotypal traits. Front Hum Neurosci. (2022) 16:846961. doi: 10.3389/fnhum.2022.846961
10. Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. (2015) 16:620–31. doi: 10.1038/nrn4005
11. Koelkebeck K, Kuegler L, Kohl W, Engell A, Lencer R. Social cognition in schizophrenia: The role of mentalizing in moral dilemma decision-making. Compr Psychiatry. (2018) 87:171–78. doi: 10.1016/j.comppsych.2018.10.013
12. Trotta A, Di Forti M, Mondelli V, Dazzan P, Pariante C, David A, et al. Prevalence of bullying victimisation amongst first-episode psychosis patients and unaffected controls. Schizophr Res. (2013) 150:169–75. doi: 10.1016/j.schres.2013.07.001
13. Ruby E, Rothman K, Corcoran C, Goetz RR, Malaspina D. Influence of early trauma on features of schizophrenia. Early Interv Psychiatry. (2017) 11:322–33. doi: 10.1111/eip.12239
14. Kaufman J, Torbey S. Child maltreatment and psychosis. Neurobiol Dis. (2019) 131:104378. doi: 10.1016/j.nbd.2019.01.015
15. Asmal L, Kilian S, du Plessis S, Scheffler F, Chiliza B, Fouche JP, et al. Childhood trauma associated white matter abnormalities in first-episode schizophrenia. Schizophr Bull. (2019) 45:369–76. doi: 10.1093/schbul/sby062
16. Adverse childhood experiences international questionnaire (ACE-IQ) . Available online at: https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) (Accessed 2023-7-18).
17. Bhavsar V, Boydell J, McGuire P, Harris V, Hotopf M, Hatch SL, et al. Childhood abuse and psychotic experiences – evidence for mediation by adulthood adverse life events. Epidemiol Psychiatr Sci. (2019) 28:300–09. doi: 10.1017/S2045796017000518
18. Bücker J, Kapczinski F, Post R, Ceresér KM, Szobot C, Yatham LN, et al. Cognitive impairment in school-aged children with early trauma. Compr Psychiatry. (2012) 53:758–64. doi: 10.1016/j.comppsych.2011.12.006
19. Dominguez MD, Wichers M, Lieb R, Wittchen HU, van Os J. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr Bull. (2011) 37:84–93. doi: 10.1093/schbul/sbp022
20. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: A systematic review and meta-analysis. Schizophr Bull. (2018) 44:1111–22. doi: 10.1093/schbul/sbx161
21. Pergola G, Papalino M, Gelao B, Sportelli L, Vollerbergh W, Grattagliano I, et al. Evocative gene-environment correlation between genetic risk for schizophrenia and bullying victimization. World Psychiatry. (2019) 18:366–67. doi: 10.1002/wps.20685
22. Sourander A, Jensen P, Rönning JA, Niemelä S, Helenius H, Sillanmäki L, et al. What is the early adulthood outcome of boys who bully or are bullied in childhood? The Finnish “From a Boy to a Man” study. Pediatrics. (2007) 120:397–404. doi: 10.1542/peds.2006-2704
23. Wolke D, Lereya ST, Fisher HL, Lewis G, Zammit S. Bullying in elementary school and psychotic experiences at 18 years: a longitudinal, population-based cohort study. Psychol Med. (2014) 44:2199–211. doi: 10.1017/S0033291713002912
24. Cao Y, Han C, Peng X, Su Z, Liu G, Xie Y, et al. Correlation between resting theta power and cognitive performance in patients with schizophrenia. Front Hum Neurosci. (2022) 16:853994. doi: 10.3389/fnhum.2022.853994
25. Javitt DC. Cognitive impairment associated with schizophrenia: from pathophysiology to treatment. Annu Rev Pharmacol Toxicol. (2023) 63:119–41. doi: 10.1146/annurev-pharmtox-051921-093250
26. Rokita KI, Dauvermann MR, Donohoe G. Early life experiences and social cognition in major psychiatric disorders: A systematic review. Eur Psychiatry. (2018) 53:123–33. doi: 10.1016/j.eurpsy.2018.06.006
27. Nejatisafa AA, Sharafi E, Motamed M, Mohammadjafari A, Etesam F, Shahmansouri N, et al. Persian translation and cultural adaptation of mini international neuropsychiatric interview and its psychometric properties. Arch Iran Med. (2022) 25:294–99. doi: 10.34172/aim.2022.48
28. Pettersson A, Modin S, Wahlström R, Af WHS, Krakau I. The Mini-International Neuropsychiatric Interview is useful and well accepted as part of the clinical assessment for depression and anxiety in primary care: a mixed-methods study. BMC Fam Pract. (2018) 19:19. doi: 10.1186/s12875-017-0674-5
29. Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. (1997) 12:232–41. doi: 10.1016/S0924-9338(97)83297-X
30. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
31. Wu BJ, Lan TH, Hu TM, Lee SM, Liou JY. Validation of a five-factor model of a Chinese Mandarin version of the Positive and Negative Syndrome Scale (CMV-PANSS) in a sample of 813 schizophrenia patients. Schizophr Res. (2015) 169:489–90. doi: 10.1016/j.schres.2015.09.011
32. Gong YX. Revision of wechsler’s adult intelligence scale in China. Acta Psychol Sin. (1983) 15:362–70.
33. Dai XY, Gong YX. A comparative study of factor analysis: Original vs revised version of Chinese Version Wechsler adult intelligence scale (WAIS to WAIS-R). Acta Psychol Sin. (1987) 19:70–8.
34. August SM, Kiwanuka JN, McMahon RP, Gold JM. The MATRICS Consensus Cognitive Battery (MCCB): clinical and cognitive correlates. Schizophr Res. (2012) 134:76–82. doi: 10.1016/j.schres.2011.10.015
35. Shi C, Kang L, Yao S, Ma Y, Li T, Liang Y, et al. The MATRICS consensus cognitive battery (MCCB): co-norming and standardization in China. Schizophr Res. (2015) 169:109–15. doi: 10.1016/j.schres.2015.09.003
36. Green MF, Nuechterlein KH. The MATRICS initiative: developing a consensus cognitive battery for clinical trials. Schizophr Res. (2004) 72:1–03. doi: 10.1016/j.schres.2004.09.006
37. Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. (2008) 165:203–13. doi: 10.1176/appi.ajp.2007.07010042
38. Mayer JD, Roberts RD, Barsade SG. Human abilities: emotional intelligence. Annu Rev Psychol. (2008) 59:507–36. doi: 10.1146/annurev.psych.59.103006.093646
39. Brackett MA, Salovey P. Measuring emotional intelligence with the Mayer-Salovery-Caruso Emotional Intelligence Test (MSCEIT). Psicothema. (2006) 18 Suppl:34–41.
40. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
41. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. (1997) 36:340–48. doi: 10.1097/00004583-199703000-00012
42. Shannon C, Douse K, McCusker C, Feeney L, Barrett S, Mulholland C. The association between childhood trauma and memory functioning in schizophrenia. Schizophr Bull. (2011) 37:531–37. doi: 10.1093/schbul/sbp096
43. Swearer SM, Cary PT. Perceptions and attitudes toward bullying in middle school youth. J Appl Sch Psychol. (2003) 19:63–79. doi: 10.1300/J008v19n02_05
44. Haidl TK, Schneider N, Dickmann K, Ruhrmann S, Kaiser N, Rosen M, et al. Validation of the bullying scale for adults - results of the PRONIA-study. J Psychiatr Res. (2020) 129:88–97. doi: 10.1016/j.jpsychires.2020.04.004
45. Zhao J, Lu XH, Liu Y, Wang N, Chen DY, Lin IA, et al. The unique contribution of past bullying experiences to the presence of psychosis-like experiences in university students. Front Psychiatry. (2022) 13:839630. doi: 10.3389/fpsyt.2022.839630
46. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. (2012) 38:661–71. doi: 10.1093/schbul/sbs050
47. Li X, Bo Q, Tian Q, Yang N, Mao Z, Zheng W, et al. Impact of childhood trauma on sensory gating in patients with first-episode schizophrenia. BMC Psychiatry. (2018) 18:258. doi: 10.1186/s12888-018-1807-7
48. Culatta E, Clay-Warner J, Boyle KM, Oshri A. Sexual revictimization: A routine activity theory explanation. J Interpers Violence. (2020) 35:2800–24. doi: 10.1177/0886260517704962
49. Wöller W. [Trauma repetition and revictimization following physical and sexual abuse]. Fortschr Neurol Psychiatr. (2005) 73:83–90. doi: 10.1055/s-2004-830055
50. Walker HE, Wamser-Nanney R. Revictimization risk factors following childhood maltreatment: A literature review. Trauma Violence Abuse. (2023) 24:2319–32. doi: 10.1177/15248380221093692
51. Pittenger SL, Pogue JK, Hansen DJ. Predicting sexual revictimization in childhood and adolescence: A longitudinal examination using ecological systems theory. Child Maltreat. (2018) 23:137–46. doi: 10.1177/1077559517733813
52. van Os J, Marsman A, van Dam D, Simons CJ. Evidence that the impact of childhood trauma on IQ is substantial in controls, moderate in siblings, and absent in patients with psychotic disorder. Schizophr Bull. (2017) 43:316–24. doi: 10.1093/schbul/sbw177
53. Martins DS, Hasse-Sousa M, Petry-Perin C, Arrial-Cordeiro RT, Rabelo-da-Ponte FD, Lima FM, et al. Perceived childhood adversities: Impact of childhood trauma to estimated intellectual functioning of individuals with bipolar disorder. Psychiatry Res. (2019) 274:345–51. doi: 10.1016/j.psychres.2019.02.046
54. Arnsten AF. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. (2009) 10:410–22. doi: 10.1038/nrn2648
55. Rokita KI, Holleran L, Dauvermann MR, Mothersill D, Holland J, Costello L, et al. Childhood trauma, brain structure and emotion recognition in patients with schizophrenia and healthy participants. Soc Cognit Affect Neurosci. (2020) 15:1336–50. doi: 10.1093/scan/nsaa160
56. Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. (2009) 109:1–09. doi: 10.1016/j.schres.2008.12.020
57. Quidé Y, Cohen-Woods S, O’Reilly N, Carr VJ, Elzinga BM, Green MJ. Schizotypal personality traits and social cognition are associated with childhood trauma exposure. Br J Clin Psychol. (2018) 57:397–419. doi: 10.1111/bjc.12187
58. Rodriguez V, Aas M, Vorontsova N, Trotta G, Gadelrab R, Rooprai NK, et al. Exploring the interplay between adversity, neurocognition, social cognition, and functional outcome in people with psychosis: A narrative review. Front Psychiatry. (2021) 12:596949. doi: 10.3389/fpsyt.2021.596949
59. Gini G. Social cognition and moral cognition in bullying: What’s wrong? Aggressive Behavior: Off J Int Soc Res Aggression. (2006) 32:528–39. doi: 10.1002/ab.20153.
60. Aas M, Steen NE, Agartz I, Aminoff SR, Lorentzen S, Sundet K, et al. Is cognitive impairment following early life stress in severe mental disorders based on specific or general cognitive functioning? Psychiatry Res. (2012) 198:495–500. doi: 10.1016/j.psychres.2011.12.045
61. Barczyk ZA, Foulds JA, Porter RJ, Douglas KM. Childhood trauma and cognitive functioning in mood disorders: a systematic review. Bipolar Disord. (2023) 25:263–77. doi: 10.1111/bdi.13321
62. Adell A. Brain NMDA receptors in schizophrenia and depression. Biomolecules. (2020) 10:947. doi: 10.3390/biom10060947
63. Stilo SA, Murray RM. Non-genetic factors in schizophrenia. Curr Psychiatry Rep. (2019) 21:100. doi: 10.1007/s11920-019-1091-3
64. Zwicker A, Denovan-Wright EM, Uher R. Gene-environment interplay in the etiology of psychosis. Psychol Med. (2018) 48:1925–36. doi: 10.1017/S003329171700383X
65. Wahbeh MH, Avramopoulos D. Gene-environment interactions in schizophrenia: a literature review. Genes (Basel). (2021) 12:1850. doi: 10.3390/genes12121850
66. Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. (2006) 58:145–73. doi: 10.1146/annurev.psych.58.110405.085605
67. Stramecki F, Frydecka D, Misiak B. The role of the interaction between the FKBP5 gene and stressful life events in the pathophysiology of schizophrenia: A narrative review. Arch Psychiatr Psychother. (2020) 22:7–16. doi: 10.12740/APP/124985
68. Schmitt A, Falkai P, Papiol S. Neurodevelopmental disturbances in schizophrenia: evidence from genetic and environmental factors. J Neural Transm (Vienna). (2023) 130:195–205. doi: 10.1007/s00702-022-02567-5
69. Tyborowska A, Volman I, Niermann H, Pouwels JL, Smeekens S, Cillessen A, et al. Early-life and pubertal stress differentially modulate grey matter development in human adolescents. Sci Rep. (2018) 8:9201. doi: 10.1038/s41598-018-27439-5
70. Gentner MB, Leppert M. Environmental influences on health and development: nutrition, substance exposure, and adverse childhood experiences. Dev Med Child Neurol. (2019) 61:1008–14. doi: 10.1111/dmcn.14149
71. Miguel PM, Pereira LO, Silveira PP, Meaney MJ. Early environmental influences on the development of children’s brain structure and function. Dev Med Child Neurol. (2019) 61:1127–33. doi: 10.1111/dmcn.14182
72. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. (2019) 18:146–61. doi: 10.1002/wps.20624
73. Guinosso SA, Johnson SB, Riley AW. Multiple adverse experiences and child cognitive development. Pediatr Res. (2016) 79:220–26. doi: 10.1038/pr.2015.195
74. Wachs TD, Gruen GE. The relationship between social and cognitive development. In: Wachs TD, Gruen GE, editors. Early experience and human development. Springer US, Boston, MA (1982). p. 167–83. doi: 10.1007/978-1-4615-9215-0.
75. Altschul S. Attachment and loss, vol. 3. Loss, sadness and depression. By john bowlby. J Am Psychoanal Assoc. (1984) 32:216–18. doi: 10.1177/000306518403200125
Keywords: early life adversity, childhood trauma, bullying, schizophrenia, social cognition
Citation: Peng X, Hou W-P, Ding Y-S, Wang Q, Li F, Sha S, Yu C-C, Zhang X-J, Zhou F-C and Wang C-Y (2024) Independent effects of early life adversity on social cognitive function in patients with schizophrenia. Front. Psychiatry 15:1343188. doi: 10.3389/fpsyt.2024.1343188
Received: 23 November 2023; Accepted: 01 February 2024;
Published: 05 March 2024.
Edited by:
Luca De Peri, Cantonal Sociopsychiatric Organization, SwitzerlandReviewed by:
Karina S. MacDowell, Complutense University of Madrid, SpainStefano Barlati, University of Brescia, Italy
Copyright © 2024 Peng, Hou, Ding, Wang, Li, Sha, Yu, Zhang, Zhou and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fu-Chun Zhou, ZnJhbmtjaG93QGNjbXUuZWR1LmNu; Xiu-Jun Zhang, emh4akBuY3N0LmVkdS5jbg==
 Xing Peng
Xing Peng Wen-Peng Hou2,3
Wen-Peng Hou2,3 Yu-Shen Ding
Yu-Shen Ding Feng Li
Feng Li Sha Sha
Sha Sha Xiu-Jun Zhang
Xiu-Jun Zhang Fu-Chun Zhou
Fu-Chun Zhou Chuan-Yue Wang
Chuan-Yue Wang