
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 14 February 2024
Sec. Autism
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1342504
This article is part of the Research Topic COVID and Autism 2023: Lessons Learnt and Future Directions for Research View all 10 articles
 Olivia M. Pokoski1,2
Olivia M. Pokoski1,2 Hayley Crain2,3
Hayley Crain2,3 Carolyn DiGuiseppi4
Carolyn DiGuiseppi4 Sarah M. Furnier1,2
Sarah M. Furnier1,2 Eric J. Moody5
Eric J. Moody5 Cy Nadler6
Cy Nadler6 Karen Pazol7
Karen Pazol7 Jessica Sanders8
Jessica Sanders8 Lisa D. Wiggins7
Lisa D. Wiggins7 Maureen S. Durkin1,2,3*
Maureen S. Durkin1,2,3*Background: To control the spread of the coronavirus disease (COVID-19), many jurisdictions throughout the world enacted public health measures that had vast socio-economic implications. In emergency situations, families of children with developmental disabilities (DDs), including autism, may experience increased difficulty accessing therapies, economic hardship, and caregiver stress, with the potential to exacerbate autism symptoms. Yet, limited research exists on the economic impacts of the COVID-19 pandemic on families of children with autism or another DD compared to families of children from the general population.
Objectives: To assess impact of the COVID-19 pandemic related to parental employment and economic difficulties in families of children with autism, another DD, and in the general population, considering potential modification by socioeconomic disadvantage before the pandemic and levels of child behavioral and emotional problems.
Methods: The Study to Explore Early Development (SEED) is a multi-site, multi-phase, case-control study of young children with autism or another DD as compared to a population comparison group (POP). During January-July 2021, a COVID-19 Impact Assessment Questionnaire was sent to eligible participants (n=1,789) who had enrolled in SEED Phase 3 from September 2017-March 2020. Parents completed a questionnaire on impacts of the pandemic in 2020 and completed the Child Behavior Checklist (CBCL) to measure behavioral and emotional health of their child during this time. Multiple logistic regression models were built for employment reduction, increased remote work, difficulty paying bills, or fear of losing their home. Covariates include group status (autism, DD, POP), household income at enrollment, child’s race and ethnicity, and binary CBCL Total Problems T-score (<60 vs. ≥60). Unadjusted and adjusted odds ratios (aOR) and 95% confidence intervals (CI) were calculated.
Results: The study included 274 children with autism, 368 children with another DD, and 385 POP children. The mean age of 6.1 years (standard deviation, 0.8) at the COVID-19 Impact Assessment did not differ between study groups. Parents of children with autism were less likely to transition to remote work (aOR [95% CI] = 0.6 [0.4, 1.0]) and more likely to report difficulty paying bills during the pandemic (1.8 [1.2, 2.9]) relative to parents of POP children. Lower income was associated with greater employment reduction, difficulty paying bills, and fear of losing their home, but inversely associated with transitioning to remote work. Parents of non-Hispanic (NH) Black children experienced greater employment reduction compared to parents of NH White children (1.9 [1.1, 3.0]). Parents from racial and ethnic minority groups were more likely to experience difficulty paying bills and fear losing their home, relative to NH White parents. Caregivers of children with CBCL scores in the clinical range were more likely to fear losing their home (2.1 [1.3, 3.4]).
Conclusion: These findings suggest that families of children with autism, families of lower socio-economic status, and families of racial and ethnic minority groups experienced fewer work flexibilities and greater financial distress during the pandemic. Future research can be used to assess if these impacts are sustained over time.
In March of 2020, a nationwide emergency was declared in the United States in an effort to control the spread of the coronavirus disease (COVID-19) (1). Many jurisdictions enacted stay-at-home orders, recommended quarantine protocols for healthy contacts of infected individuals, restricted personal travel, and temporarily closed non-essential businesses (2). These measures had vast socio-economic implications. Notably, the national unemployment rate increased to 13% from 3.8% at the beginning of the pandemic, with women losing employment at a significantly higher rate than men (3). The pandemic was also associated with increases in reported anxiety and depression and decreases in social participation and financial well-being (4).
Families of young children with autism and other developmental disabilities (DD) may have been more negatively affected by the pandemic restrictions than those of typically developing children. Autism is a neurodevelopmental disorder that is characterized by difficulties with social communication and social interaction as well as restricted and repetitive patterns in behaviors, interests, and activities (5). Children with autism may have a broad range of difficulties, including a strong preference for sameness, behavioral problems, and a need for assistance with activities of daily living. These difficulties may contribute to the higher levels of stress (6), depression and anxiety (7), and employment or financial insecurity (8, 9) reported by parents of children with autism. To mitigate these difficulties, many children with autism and other DDs see allied health professionals to help with addressing their various needs (10). Public health measures put in place to control the spread of COVID-19 disrupted the ability of some families to attend these appointments (11–13). Thus, the COVID-19 pandemic had the potential to exacerbate the potential stressors surrounding families of children with autism and other DDs.
Due to the recency of the COVID-19 pandemic, literature on its impact on families of children with autism or another DD is limited (14, 15). Some studies have documented intensified psychological and behavioral symptoms in children with autism (16–19), which could potentially be associated with increased parental stress or depression (17, 18, 20, 21). Several studies have found the COVID-19 pandemic to be associated with decreased quality of life or well-being for autistic individuals and their families (16, 22) and increased financial burden (21, 23), particularly in Black families (24). Other studies had conflicting results, with some families reporting perceived benefits of remote work or experiencing the pandemic as a welcome break, and others reporting that adjusting to the new normal with an autistic child exacerbated pre-existing challenges (25, 26). To facilitate effective planning for future public health emergencies, further research can help in understanding how families of children with autism as well as other DDs fared during the COVID-19 pandemic.
This study aimed to fill the aforementioned gaps in knowledge by surveying three groups of families of young children: those with a child with autism, those with a child with another DD, and those with a child sampled from the general population (POP). Our primary objectives were to identify differential impacts of the COVID-19 pandemic related to childcare, parental employment, and household financial security by group. We hypothesized that: (1) the impacts would be greater for families of children with autism or another DD than for POP children; (2) lower levels of socioeconomic status before the pandemic would exacerbate the adverse effects of the pandemic on families of children with disabilities; and (3) higher levels of child behavioral and emotional problems reported by parents would be associated with greater adverse impacts of the pandemic on families.
Participants in this study originally completed the Study to Explore Early Development, Phase 3 (SEED3), a case-control study of young children funded by the Centers for Disease Control and Prevention (CDC) and implemented during 2017-2020 in six communities across the United States (Colorado, Georgia, Maryland, Missouri, North Carolina, and Wisconsin). SEED3 aimed to increase the understanding of autism and other DDs through the study of risk factors, co-occurring conditions, and behavioral phenotypes. Children were eligible for SEED3 if they were 2-5 years old, born and resided in the geographic study catchment area, and consistently lived with their biological mother from 6 months of age (or younger); additionally, the mother had to be able to communicate in English (or Spanish in the Colorado site). The mother participated in an extensive interview about sociodemographic characteristics, parental and child medical history, and services or treatments received. Additionally, several standardized assessments were performed by clinicians or completed by the mother.
Three groups of children were included: 1) children with autism; 2) children with another DD; and 3) POP children, as identified during their original participation in SEED3. Children were ascertained for potential inclusion in the autism or DD groups through sources serving or evaluating children with developmental difficulties, including but not limited to early intervention, special education, hospitals, and clinics. Participants who had previously received either an autism diagnosis from a clinical provider, or services for autism through early intervention or special education, or who scored ≥11 on the Social Communication Questionnaire (27) at enrollment, received a comprehensive developmental evaluation. A final autism classification was based on results from the Autism Diagnostic Observation Schedule (ADOS) (28, 29) and the Autism Diagnostic Interview-Revised (ADIR) (30, 31), administered in-person by research reliable clinicians. POP group children were identified through random sampling of birth records in the pre-specified birthdate geographic range at delivery. Prior publications document detailed descriptions of SEED eligibility criteria, enrollment methods, study group classification, and data collection (32–34).
The COVID-19 Impact Assessment was developed in 2020 to evaluate how changes related to the COVID-19 pandemic impacted children in SEED3 and their families. The 110-item questionnaire assessed changes in services and treatments, impacts on child development, changes in household routines, and impacts on household finances or parental employment during the pandemic in 2020. Families who completed SEED3 prior to March 31, 2020 were invited to participate in the COVID-19 Impact Assessment. Eligible families received the COVID-19 Impact survey along with a parent-report version of the Child Behavior Checklist (CBCL) (35) via mail and completed the items between January and June 2021. Parents who did not initially return the survey were contacted and provided with the option to complete the survey over the phone. The COVID-19 Impact Assessment was completed by the biological mother or father or another knowledgeable caregiver (hereinafter “parent” as 97.4% were completed by the mother or father).
The SEED3 protocol was approved by the CDC Institutional Review Board (IRB) and IRBs at each study site. In December 2020, the COVID-19 Impact Assessment was approved as an amendment to the SEED3 protocol. Reporting for this study was based on the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (36).
All measures come from caregiver responses to the COVID-19 Impact Assessment. This assessment is published online (https://omb.report/icr/202102-0920-008/doc/108634700.pdf).
Parents who reported having any type of childcare during January or February of 2020 were asked if changes related to COVID affected their regular childcare during 2020. This was a dichotomous variable in which respondents could report yes or no. Due to the skip pattern, those who did not have childcare pre-COVID did not answer this question and were not included in this outcome measure.
Parents who responded that they had a paying job in January or February of 2020 were asked if they lost their job permanently, temporarily, or had their work hours reduced due to changes related to COVID in 2020. If the respondent had a spouse or partner with a paying job during January or February of 2020, they were similarly asked if their spouse or partner lost their job permanently, temporarily, or had their work hours reduced due to changes related to COVID in 2020. Each question was reported as a dichotomous (yes or no) answer. Provided that either the respondent or their spouse or partner had a paying job in January or February of 2020, a ‘yes’ response to any of the questions above was coded as having employment reduced. If the parent responded ‘no’ to all the questions, they were coded as not having their employment reduced due to changes related to COVID. Parents who did not have a paying job in January or February 2020 and did not have a partner or did not have a partner who had a paying job in January or February 2020 were not included in this outcome measure.
Respondents with paying jobs in January or February 2020 were also asked if they either transitioned to remote work or increased hours worked remotely or from home due to COVID-related changes in 2020. Again, if the respondent had a spouse or partner with a paying job during January or February of 2020, they were asked the same questions. These four questions were consolidated into one variable, with a ‘yes’ response indicating that either the respondent or their partner either began working from home or increased hours worked from home. If all questions elicited ‘no’ responses, the respondent was coded as not working from home due to changes related to COVID. Respondents who did not have a paying job in January or February 2020 and did not have a partner or they had a partner who also did not have a paying job in January or February 2020 were not included in this outcome measure.
Parents were asked how often they had difficulty paying their bills for each season of 2020 (i.e., pre-COVID: January-February; Spring: March-May; Summer: June-August; Fall: September-December). Response options were never, rarely, sometimes, very often, or extremely often. Never and rarely responses were combined, as were sometimes to extremely often due to small sample sizes. The seasons after the onset of the COVID-19 pandemic (Spring, Summer, and Fall) were also collapsed to gain an overall understanding of impacts during the pandemic. The response indicating the highest recorded difficulty throughout the seasons of the pandemic was used when consolidating variables.
Parents were asked how often in each season of 2020 they feared they might lose their home due to a lack of money. Response options fell on a 5-point Likert scale ranging from never to extremely often. Binary coding for analytic purposes combined never with rarely responses versus sometimes to extremely often responses. Questions inquiring about fear during the Spring, Summer, and Fall were combined to form a variable indicating fear throughout the pandemic, with the response option indicating the highest frequency being reported for the variable.
The CBCL was completed by parents who received the invitation to participate in the COVID-19 Impact Assessment to determine the presence or absence of behavioral and emotional problems during the pandemic (35). Respondents were asked to characterize a list of child behaviors as “not true,” “somewhat or sometimes true,” or “very true or often true” for children ages 1.5-5. Parents completing the CBCL version for children 6-8 years characterized a list of child behaviors as “below average,” “average,” or “above average” compared to other children of the same age. Responses formed two broad scales: internalizing behavior problems and externalizing behavior problems, which made up an overall total problems scale. For this analysis, T-scores for total behavior problems (mean = 50, SD = 10) were converted to a binary variable. Scores of ≥60 indicate borderline to clinically significant behavior problems and scores <60 indicate no behavior problems compared to other children the same age.
Study sample characteristics were reported as numbers of observations (percentages) for categorical variables and means (standard deviations) for continuous variables. To assess differences between the autism, DD, and POP groups, likelihood ratio chi-square tests were performed for nominal descriptive variables, Mantel-Haenszel chi-square tests for ordinal variables, and one-way ANOVAs for continuous variables. Multivariable logistic regression was performed to assess associations between group status and impacts of the pandemic on parental employment (employment reduction and increased remote work) and household income related variables (difficulty paying bills and fear of losing home). Covariates for adjustment included group status (autism, DD, POP), family income at SEED3 relative to the federal poverty level (FPL) as a four-level categorical variable, child’s race and ethnicity, and binary CBCL Total Problems t-score. To evaluate potential effect modification by household income and behavioral problems, we performed logistic regression analyses stratified by the respective potential modifiers. We tested for an interaction between group status and household income relative to the FPL at SEED3 as well as between group status and binary CBCL Total Problems t-score. Bayesian information criteria (37) indicated that the models without interaction terms better fit the data and likelihood ratio tests were insignificant for most interaction terms (data not shown). Adjusted analyses were conducted using complete case analysis, removing 28 individuals (2.7%) with incomplete covariates.
Statistical analyses were performed using SAS software, Version 9.4 (38). All tests of statistical significance were two-tailed and a p-value of less than 0.05 was considered statistically significant.
Of the 1,789 families from SEED3 invited to participate in the COVID-19 Impact assessment, 1,027 parents completed the survey (57.4%). Distribution of some key demographic characteristics stratified by study group are outlined in Table 1. At SEED3, children from the autism, DD, and POP groups significantly differed by demographic characteristics including, sex (p<0.0001), race and ethnicity (p=0.0018), and age (p<0.0001). Additionally, groups at SEED3 significantly differed by maternal education (p<0.0001), household income relative to the FPL (p<0.0001), health insurance status (p<0.0001) and study site (p=0.0082). There was not a statistically significant difference in the change in health insurance coverage between groups at the COVID-19 Impact Assessment (p=0.2955).
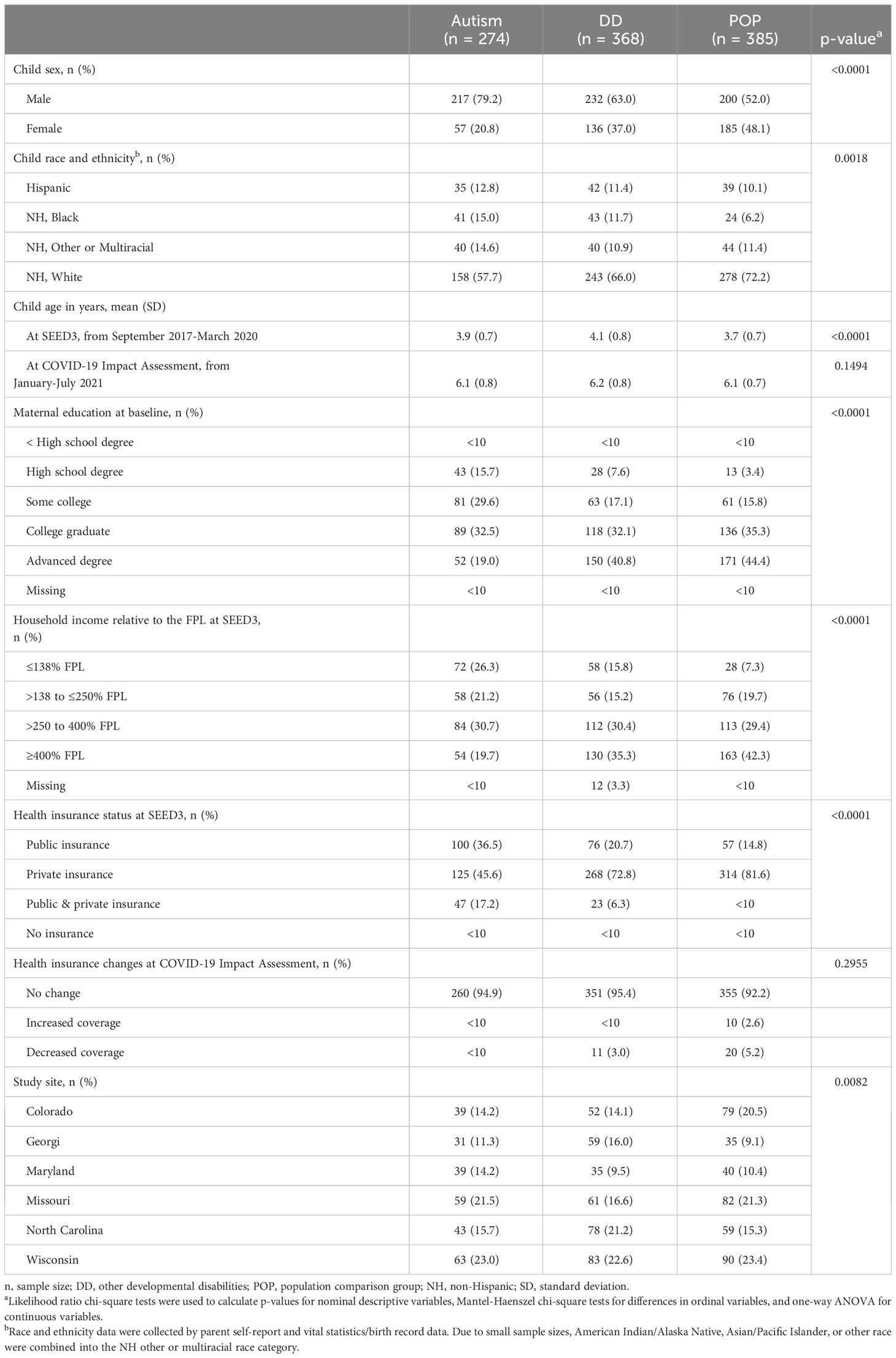
Table 1 Key characteristics of the Study to Explore Early Development COVID-19 Impact Assessment analytical sample.
In January and February of 2020, 89.4% (autism group) to 92.9% (DD group) of the children in the study population attended a school or preschool outside of the home (Table 2). This percentage was not statistically different by group status (p=0.2903). However, not including preschool or school, only 28.2% of families of a child with autism reported having childcare in January or February 2020 before the onset of the COVID-19 pandemic, which was lower than families of children in the DD (42.7%) or POP (44.2%) groups. Despite a smaller percentage of families of children with autism reporting having childcare pre-COVID, a high percentage of participants in all groups responded that changes related to COVID affected their regular childcare (88.3%-91.8%; p=0.5395). Due to a small number of families with childcare pre-pandemic responding that their childcare was not affected by COVID, investigations by socioeconomic status or emotional and behavioral problems could not be made.
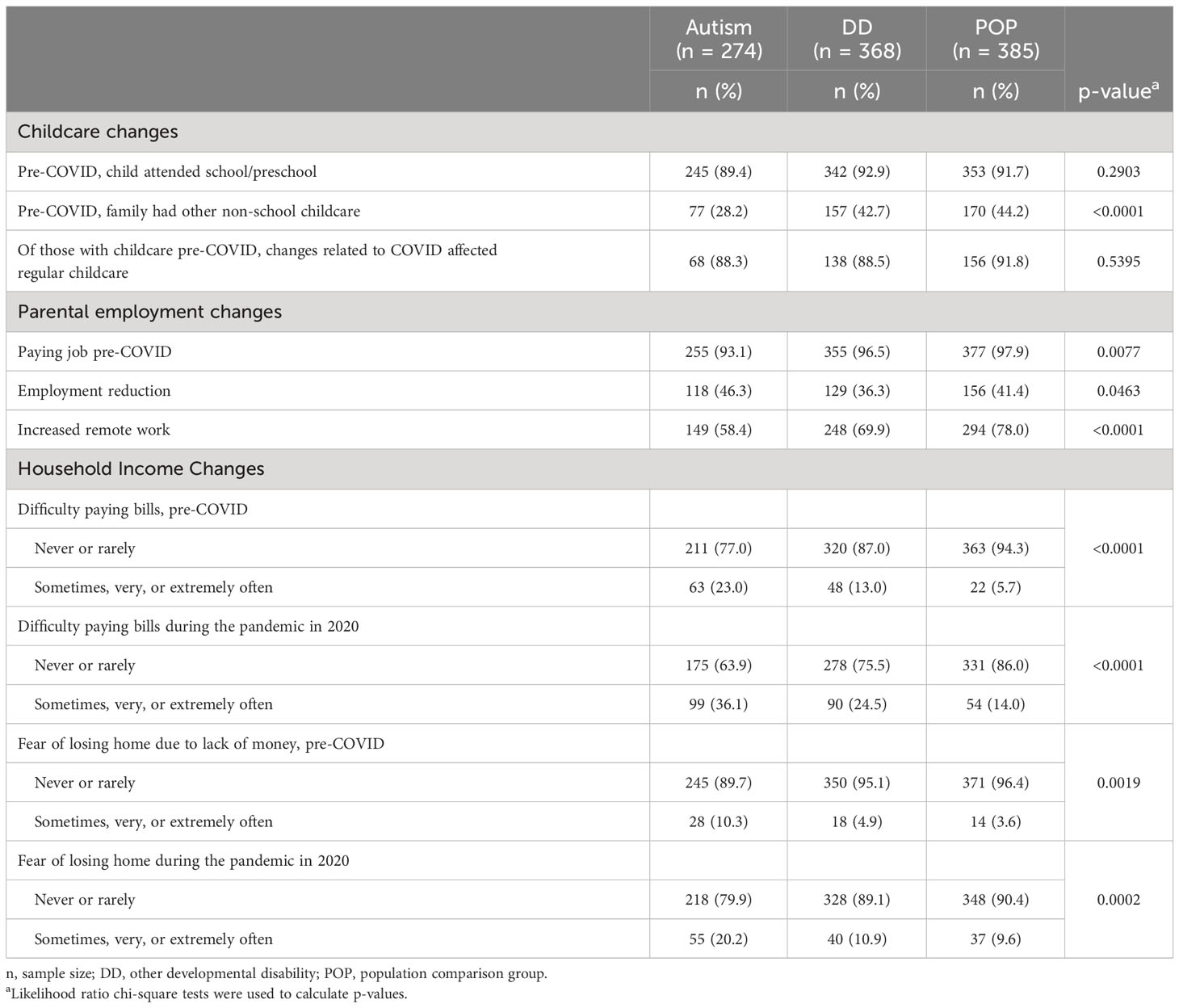
Table 2 Childcare, parental employment, and household income: Pre-COVID-19 and changes during the pandemic, Study to Explore Early Development COVID-19 Impact Assessment.
In the study sample, only 40 respondents reported neither they nor their partner had a paying job in January or February of 2020; 30 of these individuals reported not having a partner. There was a significant difference in the distribution of parents having a paying job by study group (Table 2, p=0.0077); families of children with autism had the lowest percentage, though for all three groups over 90% of respondents had a paying job pre-COVID. Nonetheless, participants in the autism group reported the greatest percentage of reduced work hours, permanently losing their job, or temporarily losing their job, due to changes related to COVID-19 in 2020 (46.3%). Parents also reported working remotely or from home at different percentages by group (p<0.0001), with parents of children with autism reporting the lowest percentage (58.4%), followed by parents of children with other DDs (69.9%), then parents of children in the POP group (78.0%).
However, in adjusted models, individuals in the DD group had significantly lower odds of reduced employment compared to the POP group (Table 3, aOR [95% CI] = 0.7 [0.5, 0.9]), but there was no significant difference in employment reduction between the autism and POP groups (0.8 [0.6, 1.2]). Families with lower household income experienced a significantly higher odds of having reduced employment due to the pandemic with decreasing household income categories, relative to those with a household income ≥400% of the FPL (Table 3). By race-ethnicity, parents of NH Black children had 90% higher odds of having reduced employment due to the pandemic, compared to NH White parents (1.9 [1.1, 3.0]). After adjustment for covariates, no difference was observed in employment reduction among families with children with and without behavioral problems as measured by the CBCL (1.2 [0.9, 1.7]).
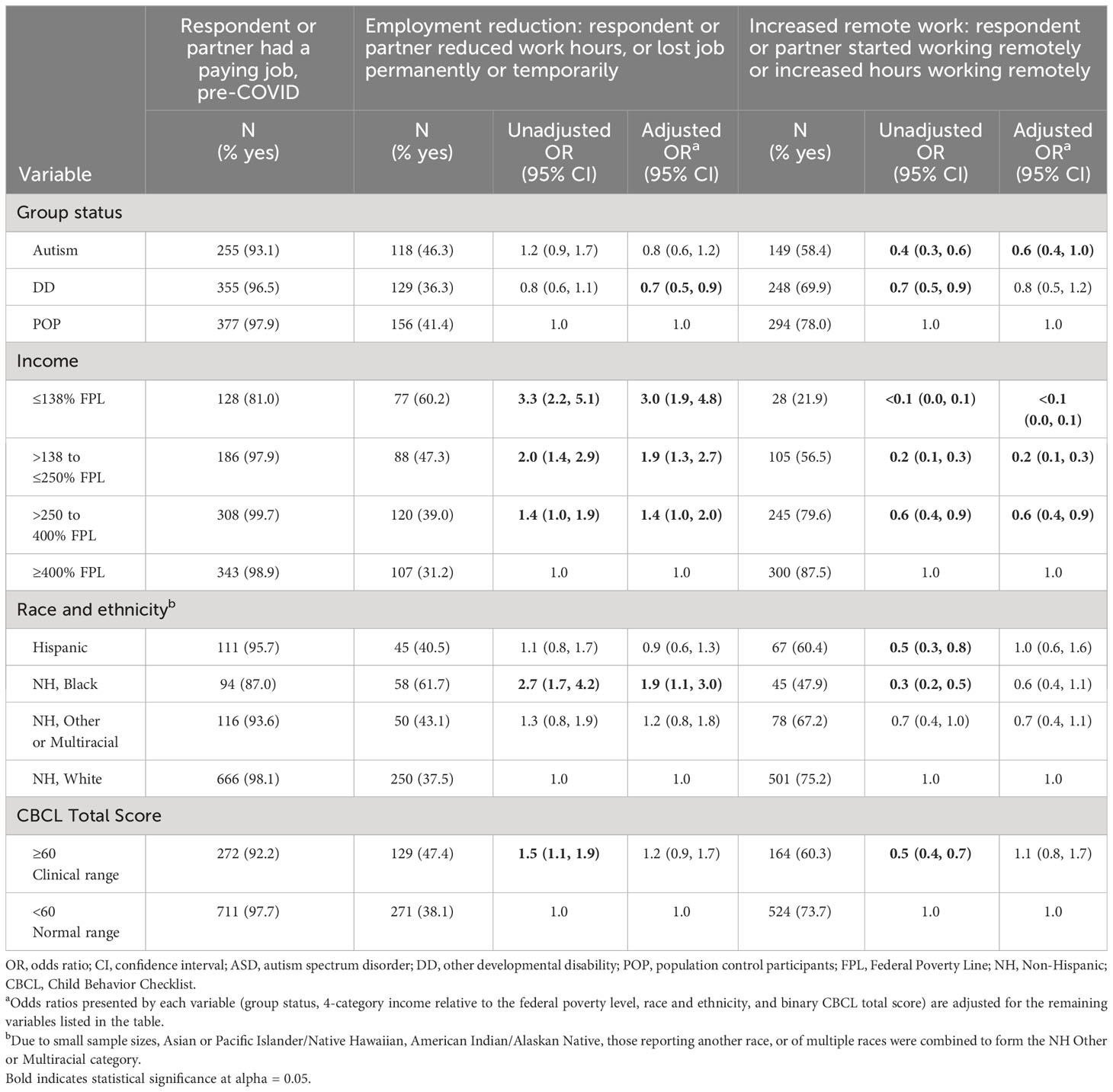
Table 3 Odds ratios for parental employment changes during 2020 of the COVID-19 pandemic, Study to Explore Early Development COVID-19 Impact Assessment.
Respondents in the autism and DD groups who reported having a paying job or a partner with a paying job in January or February of 2020, had lower odds of beginning to work remotely or from home or increasing hours worked remotely or from home (autism group: 0.4 [0.3, 0.6], DD group: 0.7 [0.5, 0.9]) relative to the POP group. These results were attenuated after adjusting for covariates (0.6 [0.4, 1.0] for the autism group and 0.8 [0.5, 1.2] for the DD group). Each income category below 400% of the FPL had significantly lower odds of increasing remote work hours with the COVID-19 pandemic (Table 3). After adjusting for covariates, no differences were observed between increased remote work in minority families relative to NH White families, or between families of children with or without clinically significant CBCL scores.
Pre-COVID and during the COVID-19 pandemic, higher percentages of respondents with a child in the autism and DD groups reported having difficulty paying bills sometimes, very, or extremely often compared to the POP group (Table 2). Table 4 depicts the unadjusted and covariate-adjusted results from the multivariable logistic regression models for difficulty paying bills during the COVID-19 pandemic in 2020. After adjusting for covariates, families of children in the autism group had 80% higher odds (1.8 [1.2, 2.9]) of reporting difficulty paying bills during the pandemic compared to the POP group. Similarly, families of children with other DDs had 60% higher odds of reporting difficulty paying bills during the pandemic compared to the POP group after adjustment (1.6 [1.0, 2.5]). By income, those with the lowest income relative to the FPL at SEED3 had the highest odds of difficulty paying bills (12.6 [7.3, 22.0]). Furthermore, each household income category relative to the FPL had significantly higher odds of difficulty paying bills during the pandemic compared to those with income ≥400% FPL, with decreasing magnitude as income increased (Table 4). Parents from racial and ethnic minority groups were more likely to experience difficulty paying bills during the pandemic, with parents of NH Black children experiencing the most difficulty compared to NH White children (3.6 [2.2, 6.0]). After adjustment for covariates, difficulty paying bills during the pandemic did not differ between families of a child with a clinically significant CBCL score relative to those with a child with a CBCL score <60 (1.3 [0.9, 1.9]).
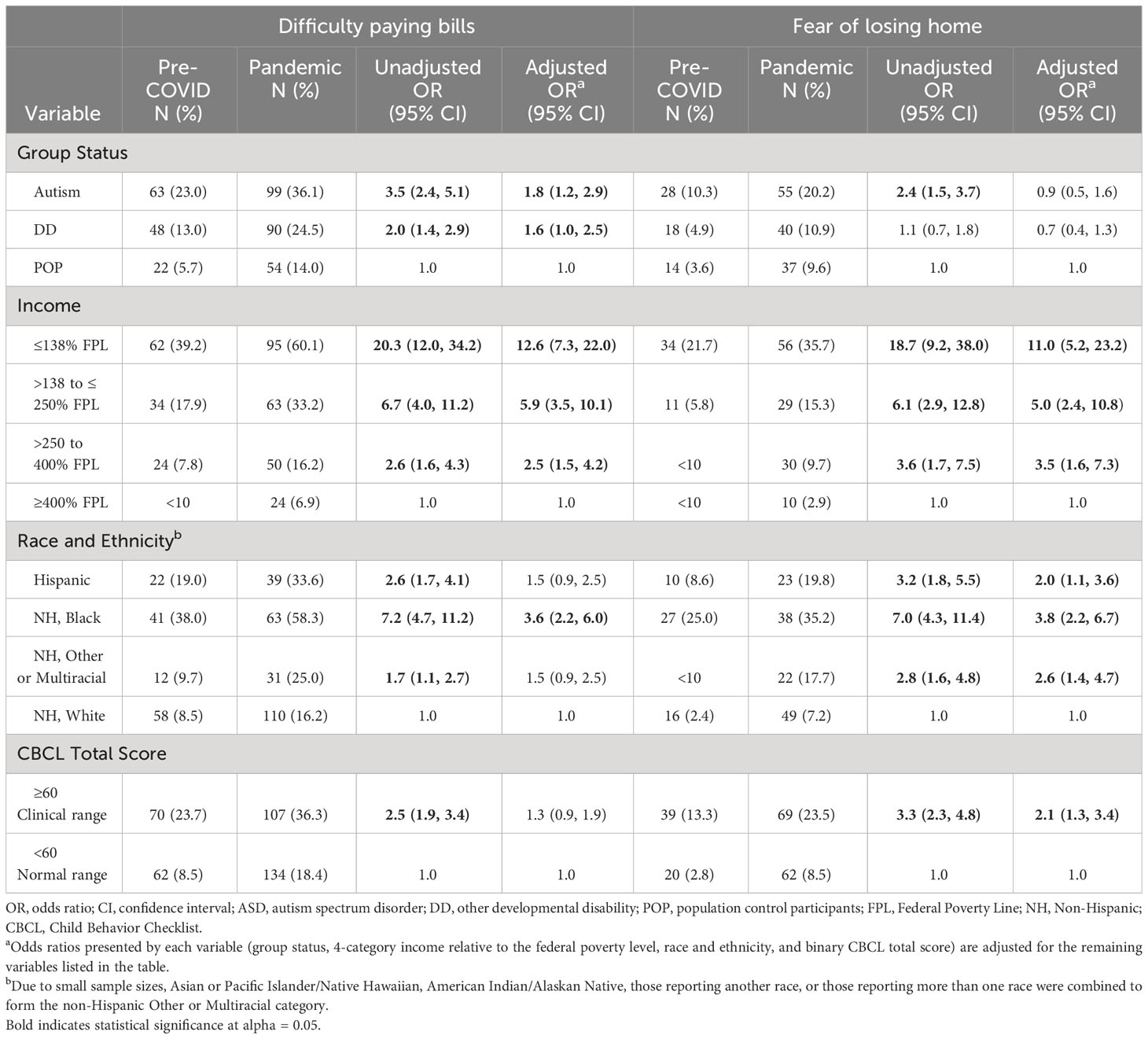
Table 4 Odds ratios for household income changes during 2020 of the COVID-19 pandemic, Study to Explore Early Development COVID-19 Impact Assessment.
The percentages of respondents who reported that they feared losing their home sometimes, very, or extremely often during the COVID-19 pandemic differed across groups, with the highest percentage in the autism group (20.2%) and the lowest percentage in the POP group (9.6%, Table 2). After adjusting for covariates, there was no significant difference in fear of losing one’s home during the COVID-19 pandemic between the autism (0.9 [0.5, 1.6]) or DD (0.7 [0.4, 1.3]) groups relative to the POP group. Relative to families with a household income ≥400% of the FPL, families of lower income had higher odds of being fearful of losing their home during the pandemic, with increasing magnitude as household income decreased (Table 4). Families from racial and ethnic minority groups were more fearful of losing their homes during the pandemic compared to families of NH White children, after adjusting for covariates (Table 4). Caregivers of children who have clinically significant behavioral and emotional health problems had 2.1 times higher odds (95% CI: 1.3, 3.4) of being fearful of losing their home during the pandemic compared to those with children with CBCL score <60.
The odds ratios indicating impacts of the pandemic on families of children with autism relative to families in the POP group were similar for lower income (≤200% FPL) and higher income (>200% FPL) families (Table 5). In contrast, the odds ratios comparing the DD group to the POP group differed somewhat by income level. In families of higher income, the DD group was less likely to experience employment reduction compared to the POP group (0.6 [0.4, 0.9]), whereas in lower income families, parents of children with other DDs had similar employment reduction compared to the POP group (1.1 [0.5, 2.3]). Additionally, in lower income families, those in the DD group had an increased odds of difficulty paying bills (2.2 [1.1, 4.4]) compared to families of children in the POP group, whereas, among higher income families, the odds of having difficulty paying bills was similar in the DD and POP groups (1.3 [0.8, 2.2]). The likelihood ratio test for the group status by household income interaction was only statistically significant for the logistic regression model examining parents who increased remote work during the pandemic (p=0.0422). However, model coefficients and resulting odds ratios were similar with or without the inclusion of this interaction term (data not shown).
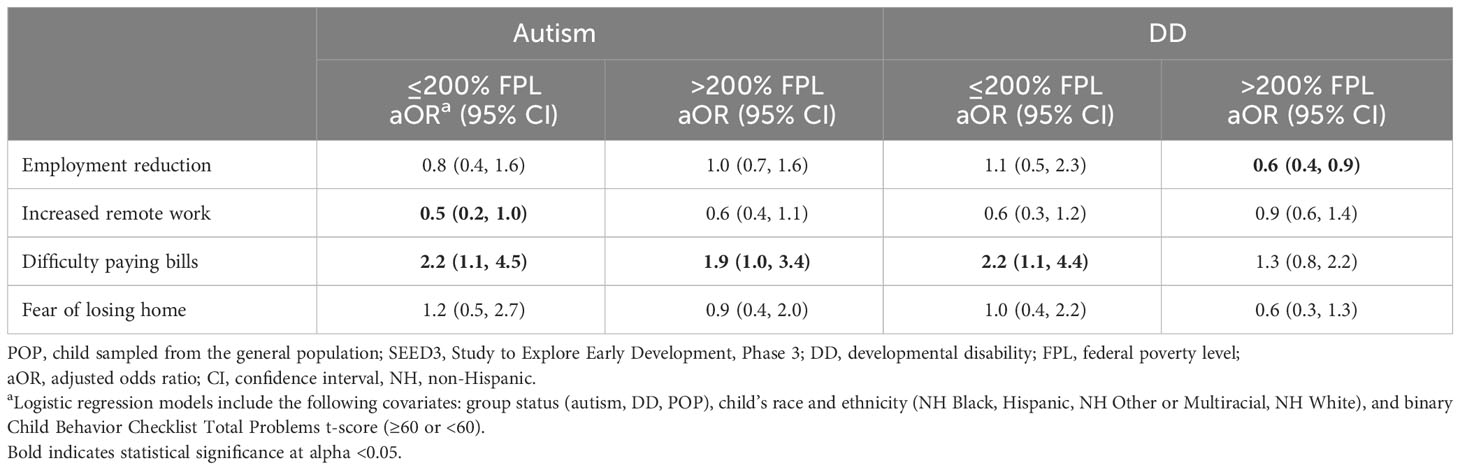
Table 5 Odds ratios relative to the POP group for parental employment changes and household income changes during 2020 of the COVID-19 pandemic stratified by binary household income at SEED3, Study to Explore Early Development COVID-19 Impact Assessment .
We found no evidence of effect modification in analyses stratified by CBCL Total Problems t-score categories (Table 6). In families of children with autism and families of children with other DDs compared to the POP group, the odds ratios were largely similar for families of children with typical CBCL scores (<60) and those scoring in the borderline to clinically significant range (≥60). For each outcome, likelihood ratio tests for the interaction between binary CBCL Total Problems t-score and group status were not statistically significant (data not shown).
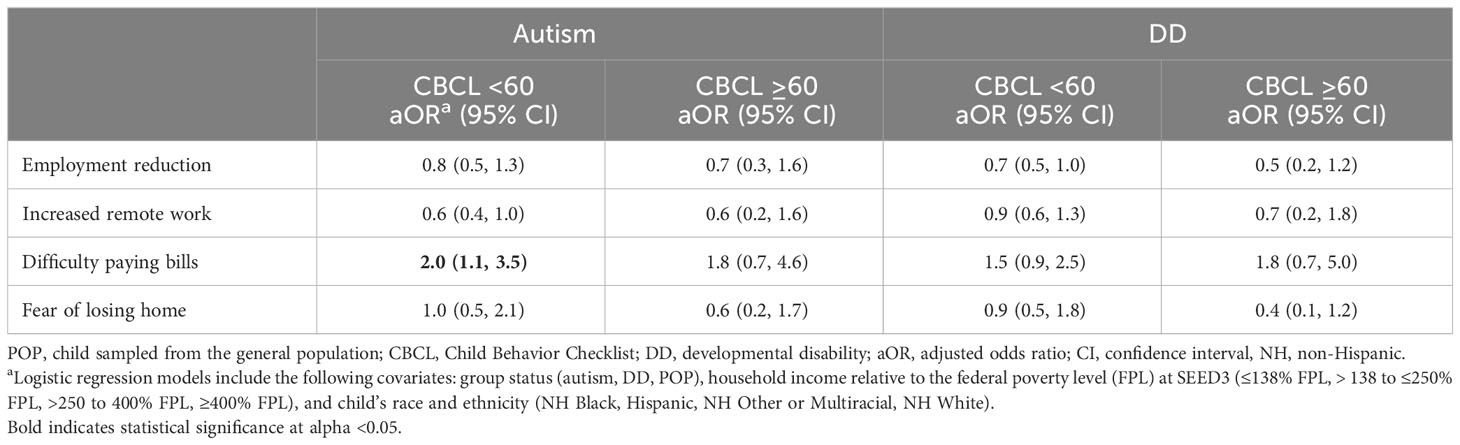
Table 6 Odds ratios relative to the POP group for parental employment changes and household income changes during 2020 of the COVID-19 pandemic stratified by CBCL Total Problems binary score, Study to Explore Early Development COVID-19 Impact Assessment.
Our study examined impacts of the COVID-19 pandemic on measures of childcare, parental employment, and household income on a sample of families of three groups of children: those with autism, those with another DD, and a population comparison group. Even after adjusting for household income, race and ethnicity, and the behavioral and emotional problems of the child, families of children with autism reported increased odds of difficulty paying bills and decreased odds of working remotely or from home compared to families of POP children. Targeted support systems may need to be established in anticipation of future emergency situations to assist vulnerable populations, including families of children with disabilities.
We found parents of children in the autism group were less likely to have a paying job and had greater difficulty paying bills prior to the onset of the pandemic, when compared to parents of children in the POP group. This finding is consistent with previous studies documenting the economic impacts of autism, including decreased parental employment and productivity due to therapy schedules and caregiving needs as well as the high out-of-pocket costs of autism services and the excess healthcare expenditures in general for children with autism relative to children without disabilities (39–45). However, our overall sample had a high frequency of parents with a paying job pre-COVID, as 93% of parents of children with autism reported having a paying job. Still, we attempted to mitigate potential confounding by adjusting for household income at SEED3. While some previous studies reported that parents of children with either autism or another DD had financial concerns due to the pandemic, these studies lacked a comparison group, making it difficult to determine if financial concerns were universal or associated with having a child with a DD (21, 23). Simply examining frequencies, each group had an elevated difficulty paying bills during the pandemic, which aligns with the findings of these studies.
We found that families of children with autism had 40% lower odds of working remotely or from home during the COVID-19 pandemic after adjusting for race and ethnicity, income, and behavioral and emotional problems, compared to families of POP children. Previous literature cites remote work and parenting a child with autism as increasing parental stress due to the difficulty of balancing work obligations and facilitating the child’s therapies and schoolwork (23, 25), and parents who switched to working from home felt that the pandemic increased their responsibilities (46). This perceived increase in stress and responsibility may help explain why parents of children with autism were less likely to work from home during the pandemic in this study, though the data do not allow us to determine the reason for being less likely to work remotely. The increased demands on working parents with the COVID-19 pandemic were not specific to parents of children with autism, as research indicates that many parents of children without disabilities also experienced difficulties balancing remote work and caregiving (47, 48). In developing preparations for future public health emergencies, it may be important to recognize that parents of children with autism may face additional challenges in working from home.
An abundance of research has documented how the pandemic disproportionately impacted lower income families (49–52). After adjusting for group status, race and ethnicity, and behavioral and emotional problems, families with a lower household income prior to the pandemic had significantly greater odds of employment reduction, difficulty paying bills, and fear of losing their home during the pandemic relative to families in the highest income category. There are likely additional factors that contributed to the disproportionate disadvantages faced by families with lower income that we could not measure. Individuals with a lower household income pre-pandemic also had lower odds of working remotely or from home than those with a higher household income. While it is possible that individuals of lower income were working jobs that could not be performed remotely, a lack of resources such as a computer or internet accessibility might have also served as a barrier.
We hypothesized lower levels of socioeconomic status before the pandemic would exacerbate the adverse effects of the pandemic on families of children with disabilities. However, we found little evidence that the impact of having a child with autism or other disabilities on COVID-related measures of parental employment and household income changes was greater for low income than high income families.
Several studies have highlighted the impacts of the pandemic on behavioral problems in children with autism (16–18, 53, 54). In light of this, we hypothesized that higher levels of child behavioral and emotional problems would be associated with greater adverse economic and employment impacts on their families during the pandemic. We found that families of children with behavioral problems in the clinical range were more than twice as likely to report fear of losing their home compared to families of children without behavioral problems. Prior to the pandemic, in non-emergency settings, research indicated that parental stress is a consequence and antecedent of child behavior problems, while simultaneously, child behavior problems are both an antecedent and consequence of parental stress (55). Evidence supporting this idea during the COVID-19 pandemic has been documented as the “spillover hypothesis” that suggests that high levels of stress or anxiety in parents can “spill over” to their children and lead to an increase in child behavior problems (56–58). It is possible that the increased economic stressors of the pandemic may have exacerbated the emotional and behavioral problems in children. It is also possible that parents who reported being fearful of losing their home had increased stress relative to those who were not fearful of losing their home. However, we did not find evidence that the economic impact of having a child with autism or other DD differed by the presence or absence of behavior problems in the child.
We found that families of racial and ethnic minority groups experienced greater adverse economic impacts than other families. These findings align with previous research suggesting that Black and Hispanic individuals had more frequent job or wage loss and more trouble paying bills compared to White individuals during the pandemic (59–61). The disproportionate socioeconomic impact of the COVID-19 pandemic on racial and ethnic minority groups may have only worsened the disparities that are already present (62). Initiatives to assist communities that may experience disproportionate impacts may help mitigate the heightened negative impacts in future public health emergencies.
At SEED3, the groups were not balanced on key variables of interest, with families of children in the autism and DD groups being of a lower socioeconomic status than families of POP children. We attempted to eliminate the potential confounding by socioeconomic status by adjusting the models for household income at SEED3, but residual confounding is possible. Additionally, by conducting a complete case analysis, individuals who had missing data in any of the outcomes or covariates were excluded from the analysis. However, only 2.5% of the sample had a missing variable so it is likely that the results would remain unchanged if these individuals were to be included. Finally, our analyses relied on self-reported measures of employment and income changes during 2020 from the COVID-19 Impact Assessment which was completed between January and June of 2021, which may have introduced measurement bias in the form of social desirability, recall bias, or errors in reporting.
Families of children with autism and other DDs may be especially vulnerable in public health emergencies. Using data from the COVID-19 Impact Assessment, we found that families of children with autism more often reported difficulty paying bills and lower odds of transitioning to remote work during 2020 of the pandemic compared to families of children sampled from the general population. We also found that families of lower socio-economic status as well as families of racial and ethnic minority groups experienced fewer work flexibilities and greater financial distress during the pandemic. Future research can help us better understand if these impacts are sustained over time and how best to support families who might lie at the intersection of these disadvantages during future emergency situations.
The original data presented in this paper are protected to ensure participant confidentiality. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by The SEED3 protocol, CDC Institutional Review Board (IRB) and IRBs at each study site. In December 2020, the SEED3 COVID-19 Impact Assessment was approved as an amendment to the SEED3 protocol. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
OP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. HC: Methodology, Supervision, Writing – review & editing. CD: Funding acquisition, Investigation, Supervision, Writing – review & editing. SF: Data curation, Investigation, Methodology, Validation, Writing – review & editing. EM: Writing – review & editing. CN: Investigation, Supervision, Writing – review & editing. KP: Funding acquisition, Investigation, Supervision, Writing – review & editing. JS: Writing – review & editing. LW: Investigation, Methodology, Supervision, Writing – review & editing. MD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Implementation of SEED was supported by five cooperative agreements from the Centers for Disease Control and Prevention: Cooperative Agreement Number U01DD001210, The Regents of the University of Colorado; Cooperative Agreement Number U01DD001214 and 1U01DD001209, Johns Hopkins University; Cooperative Agreement Number U01DD001205, University of North Carolina at Chapel Hill; Cooperative Agreement Number U01DD001216, Washington University; and Cooperative Agreement Number U01DD001215, University of Wisconsin System. CDC collaborated in the conduct of the research and collection of data, and in the preparation of the article, including interpretation of data, writing of the report, and in the decision to submit the article for publication. This study was supported in part by a core grant to the Waisman Center from the National Institute of Child Health and Human Development (P50HD105353).
The authors would like to thank SEED study staff and children and families who completed SEED3 and the COVID-19 Impact Assessment.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. The findings and conclusions in this report are those of the authors and do not necessarily represent the view of the Centers for Disease Control and Prevention.
1. Executive Office of the President. Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. Washington, DC, USA: Office of the Federal Register, National Archives and Records Administration. (2020) 85(53):15337–8. Available at: https://www.federalregister.gov/documents/2020/03/18/2020-05794/declaring-a-national-emergency-concerning-the-novel-coronavirus-disease-covid-19-outbreak.
2. Jacobsen GD, Jacobsen KH. Statewide COVID-19 stay-at-home orders and population mobility in the United States. World Med Health Policy (2020) 12(4):347–56. doi: 10.1002/wmh3.350
3. Smith SM, Edwards R, Duong HC. Unemployment rises in 2020, as the country battles the COVID-19 pandemic. Washington, DC, USA: Monthly Labor Review. (2021). doi: 10.21916/mlr.2021.12
4. Beach SR, Schulz R, Donovan H, Rosland AM. Family caregiving during the COVID-19 pandemic. Gerontologist (2021) 61(5):650–60. doi: 10.1093/geront/gnab049
5. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5-tr). 5th rev ed. Washington, DC, USA: American Psychiatric Publishing (2023).
6. Hayes SA, Watson SL. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord (2013) 43(3):629–42. doi: 10.1007/s10803-012-1604-y
7. Scherer N, Verhey I, Kuper H. Depression and anxiety in parents of children with intellectual and developmental disabilities: A systematic review and meta-analysis. PloS One (2019) 14(7):e0219888. doi: 10.1371/journal.pone.0219888
8. Ou J-J, Shi L-J, Xun G-L, Chen C, Wu R-R, Luo X-R, et al. Employment and financial burden of families with preschool children diagnosed with autism spectrum disorders in urban China: results from a descriptive study. BMC Psychiatry (2015) 15(1):3. doi: 10.1186/s12888-015-0382-4
9. Saunders BS, Tilford JM, Fussell JJ, Schulz EG, Casey PH, Kuo DZ. Financial and employment impact of intellectual disability on families of children with autism. Families Syst (2015) 33(1):36–45. doi: 10.1037/fsh0000102
10. Cogswell ME, Coil E, Tian LH, Tinker SC, Ryerson AB, Maenner MJ, et al. Health needs and use of services among children with developmental disabilities — United states, 2014–2018. MMWR Morb Mortal Wkly Rep (2022) 71(12):453–8. doi: 10.15585/mmwr.mm7112a3
11. Allison KM, Levac DE. Impact of the COVID-19 pandemic on therapy service delivery and functioning for school-aged children with disabilities in the United States. Disability Health J (2022) 15(2):101266. doi: 10.1016/j.dhjo.2021.101266
12. Neece C, McIntyre LL, Fenning R. Examining the impact of COVID-19 in ethnically diverse families with young children with intellectual and developmental disabilities. J Intellect Disabil Res (2020) 64(10):739–49. doi: 10.1111/jir.12769
13. Zhang S, Hao Y, Feng Y, Lee NY. COVID-19 pandemic impacts on children with developmental disabilities: service disruption, transition to telehealth, and child wellbeing. Int J Environ Res Public Health (2022) 19(6):3259. doi: 10.3390/ijerph19063259
14. World Health Organization. Director-General's opening remarks at the media briefing - 5 May 2023. (2023). Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing---5-may-2023.
15. Silk BJ, Scobie HM, Duck WM, Palmer T, Ahmad FB, Binder AM, et al. COVID-19 Surveillance After Expiration of the Public Health Emergency Declaration — United States, May 11, 2023. MMWR Morb Mortal Wkly Rep (2023) 72(19):523–8. doi: 10.15585/mmwr.mm7219e1
16. Teixeira OFB, Xavier SPL, Felix NDC, Silva JWMD, Abreu RMSX, Miranda KCL. Repercussions of the COVID-19 pandemic for people with autism and their family members: A scoping review. Rev Lat Am Enfermagem (2022) 30:e3729. doi: 10.1590/1518-8345.5965.3729
17. Lee V, Albaum C, Tablon Modica P, Ahmad F, Gorter JW, Khanlou N, et al. The impact of COVID-19 on the mental health and wellbeing of caregivers of autistic children and youth: A scoping review. Autism Res (2021) 14(12):2477–94. doi: 10.1002/aur.2616
18. Guller B, Yaylaci F, Eyuboglu D. Those in the shadow of the pandemic: impacts of the COVID-19 outbreak on the mental health of children with neurodevelopmental disorders and their parents. Int J Dev Disabil (2022) 68(6):943–55. doi: 10.1080/20473869.2021.1930827
19. Vibert B, Segura P, Gallagher L, Georgiades S, Pervanidou P, Thurm A, et al. CRISIS AFAR: an international collaborative study of the impact of the COVID-19 pandemic on mental health and service access in youth with autism and neurodevelopmental conditions. Mol Autism (2023) 14(1):7. doi: 10.1186/s13229-022-00536-z
20. Northrup RA, Jones E, Singh V, Holingue C, Meck M, Gurnett CA, et al. Caregiver perspectives on the continued impact of the COVID-19 pandemic on children with intellectual/developmental disabilities. Front Pediatr (2023) 11:1196275. doi: 10.3389/fped.2023.1196275
21. Tarzi G, Mendoza O, Lunsky Y, St John L. The experiences and attitudes of family caregivers of adults with intellectual and developmental disabilities at different timepoints in the COVID-19 pandemic. Disability Health J (2023) 16(3):101472. doi: 10.1016/j.dhjo.2023.101472
22. Sanders JS, Pillai RLI, Sturley R, Sillau S, Asato MR, Aravamuthan BR, et al. Impact of the COVID-19 pandemic on the behavioral health of people with intellectual and developmental disabilities. Psychiatr Services (2022) 73(12):1389–92. doi: 10.1176/appi.ps.202100524
23. Manning J, Billian J, Matson J, Allen C, Soares N. Perceptions of families of individuals with autism spectrum disorder during the COVID-19 crisis. J Autism Dev Disord (2021) 51(8):2920–8. doi: 10.1007/s10803-020-04760-5
24. Koffer Miller KH, Cooper DS, Ventimiglia JC, Shea LL. Feeling intimidated and uncomfortable: Established and exacerbated educational inequities experienced by black parents of autistic children. Autism Res (2023) 16(5):1040–51. doi: 10.1002/aur.2919
25. Stadheim J, Johns A, Mitchell M, Smith CJ, Braden BB, Matthews NL. A qualitative examination of the impact of the COVID-19 pandemic on children and adolescents with autism and their parents. Res Dev Disabil (2022) 125:104232. doi: 10.1016/j.ridd.2022.104232
26. Davy G, Unwin KL, Barbaro J, Dissanayake C. Leisure, employment, community participation and quality of life in caregivers of autistic children: A scoping review. Autism (2022) 26(8):1916–30. doi: 10.1177/13623613221105836
27. Rutter M, Bailey A, Lord C. The Social Communication Questionnaire. Los Angeles, CA: Western Psychological Services (2003).
28. Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. 2nd ed. Los Angeles, CA: Western Psychological Services (2012).
29. Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles, CA: Western Psychological Services (1999).
30. Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord (1994) 24(5):659–85. doi: 10.1007/BF02172145
31. Rutter M, Le Couteur A, Lord C. ADI-R: The Autism Diagnostic Interview-Revised. Los Angeles, CA: Western Psychological Services (2003).
32. Schendel DE, Diguiseppi C, Croen LA, Fallin MD, Reed PL, Schieve LA, et al. The Study to Explore Early Development (SEED): a multisite epidemiologic study of autism by the Centers for Autism and Developmental Disabilities Research and Epidemiology (CADDRE) network. J Autism Dev Disord (2012) 42(10):2121–40. doi: 10.1007/s10803-012-1461-8
33. Wiggins LD, Reynolds A, Rice CE, Moody EJ, Bernal P, Blaskey L, et al. Using standardized diagnostic instruments to classify children with autism in the study to explore early development. J Autism Dev Disord (2015) 45(5):1271–80. doi: 10.1007/s10803-014-2287-3
34. Wiggins LD, Overwyk K, Daniels J, Barger B, Crain H, Grzadzinski R, et al. Risk factors and clinical correlates of sensory dysfunction in preschool children with and without autism spectrum disorder. Autism Res (2024) 17(1):162–72. doi: 10.1002/aur.3074
35. Achenbach TM. Child Behavior Checklist. Burlington, VT: Achenbach System of Empirically Based Assessment (1992).
36. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (2007) 370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X
37. Neath AA, Cavanaugh JE. The Bayesian information criterion: background, derivation, and applications.. WIRES Comp Stat (2012) 4(2):199–203. doi: 10.1002/wics.199
39. Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics (2012) 129(4):617–23. doi: 10.1542/peds.2011-2700
40. Liao X, Li Y. Economic burdens on parents of children with autism: a literature review. CNS spectrums (2020) 25(4):468–74. doi: 10.1017/S1092852919001512
41. McCall BP, Starr EM. Effects of autism spectrum disorder on parental employment in the United States: evidence from the National Health Interview Survey. Community Work Family (2018) 21(4):367–92. doi: 10.1080/13668803.2016.1241217
42. Callander EJ, Lindsay DB. The impact of childhood autism spectrum disorder on parent's labour force participation: Can parents be expected to be able to re-join the labour force? Autism (2018) 22(5):542–8. doi: 10.1177/1362361316688331
43. Lynch FL, Bulkley JE, Varga A, Crawford P, Croen LA, Daida YG, et al. The impact of autism spectrum disorder on parent employment: Results from the r-Kids study. Autism Res (2023) 16(3):642–52. doi: 10.1002/aur.2882
44. Zuvekas SH, Grosse SD, Lavelle TA, Maenner MJ, Dietz P, Ji X. Healthcare costs of pediatric autism spectrum disorder in the United States, 2003–2015. J Autism Dev Disord (2021) 51(8):2950–8. doi: 10.1007/s10803-020-04704-z
45. Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics (2006) 118(4):e1203–11. doi: 10.1542/peds.2006-0127
46. Bozkus-Genc G, Sani-Bozkurt S. How parents of children with autism spectrum disorder experience the COVID-19 pandemic: Perspectives and insights on the new normal. Res Dev Disabil (2022) 124:104200. doi: 10.1016/j.ridd.2022.104200
47. Dunatchik A, Gerson K, Glass J, Jacobs JA, Stritzel H. Gender, parenting, and the rise of remote work during the pandemic: implications for domestic inequality in the United States. Gender Society (2021) 35(2):194–205. doi: 10.1177/08912432211001301
48. Manzo LKC, Minello A. Mothers, childcare duties, and remote working under COVID-19 lockdown in Italy: Cultivating communities of care. Dialogues Hum Geography (2020) 10(2):120–3. doi: 10.1177/2043820620934268
49. Andrade C, Gillen M, Molina JA, Wilmarth MJ. The Social and Economic Impact of Covid-19 on Family Functioning and Well-Being: Where do we go from here? J Family Economic Issues (2022) 43(2):205–12. doi: 10.1007/s10834-022-09848-x
50. Chen CY-C, Byrne E, Vélez T. Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: roles of income level and race. J Family Issues (2022) 43(3):719–40. doi: 10.1177/0192513X21994153
51. Kochhar R, Sechopoulos S. COVID-19 pandemic pinches finances of America's lower- and middle-income families. pewresearch.org. (2022). Available at: https://www.pewresearch.org/social-trends/2022/04/20/covid-19-pandemic-pinches-finances-of-americas-lower-and-middle-income-families/ (Accessed November 20, 2023).
52. Qian Y, Fan W. Who loses income during the COVID-19 outbreak? Evidence from China. Res Soc Stratification Mobility (2020) 68:100522. doi: 10.1016/j.rssm.2020.100522
53. Termine C, Galli V, Dui LG, Berlusconi V, Lipari R, Lunardini F, et al. Autism in preschool-aged children: the effects of COVID-19 lockdown. J Autism Dev Disord (2023). doi: 10.1007/s10803-023-06078-4
54. Shorey S, Lau LST, Tan JX, Ng ED, Aishworiya R. Families with children with neurodevelopmental disorders during COVID-19: A scoping review. J Pediatr Psychol (2021) 46(5):514–25. doi: 10.1093/jpepsy/jsab029
55. Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil (2012) 117(1):48–66. doi: 1944-7558-117.1.48/1944-7558-117.1.48
56. Eshraghi AA, Cavalcante L, Furar E, Alessandri M, Eshraghi RS, Armstrong FD, et al. Implications of parental stress on worsening of behavioral problems in children with autism during COVID-19 pandemic: “the spillover hypothesis”. Mol Psychiatry (2022) 27(4):1869–70. doi: 10.1038/s41380-021-01433-2
57. Spinelli M, Lionetti F, Pastore M, Fasolo M. Parents' Stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Front Psychol (2020) 11:1713. doi: 10.3389/fpsyg.2020.01713
58. Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum Dev (2020) 51(5):671–82. doi: 10.1007/s10578-020-01037-x
59. Lopez MH, Rainie L, Budiman A. Financial and Health Impacts of Covid-19 Vary Widely By Race and Ethnicity Pew Research Center (2020). Available at: https://www.pewresearch.org/short-reads/2020/05/05/financial-and-health-impacts-of-covid-19-vary-widely-by-race-and-ethnicity/.
60. Moore SE, Jones-Eversley SD, Tolliver WF, Wilson BL, Jones CA. Six feet apart or six feet under: The impact of COVID-19 on the Black community. Death Stud (2022) 46(4):891–901. doi: 10.1080/07481187.2020.1785053
61. Artiga S, Garfield R, Orgera K. Communities of Color at Higher Risk for Health and Economic Challenges Due to Covid-19. San Francisco, CA, USA: Kaiser Family Foundation (2020). Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/.
Keywords: COVID-19, autism spectrum disorder, neurodevelopmental disorder, COVID-19 pandemic impacts, family impacts
Citation: Pokoski OM, Crain H, DiGuiseppi C, Furnier SM, Moody EJ, Nadler C, Pazol K, Sanders J, Wiggins LD and Durkin MS (2024) Economic impacts of the COVID-19 pandemic on families of children with autism and other developmental disabilities. Front. Psychiatry 15:1342504. doi: 10.3389/fpsyt.2024.1342504
Received: 21 November 2023; Accepted: 26 January 2024;
Published: 14 February 2024.
Edited by:
Michaela DuBay, University of Virginia, United StatesReviewed by:
Cecilia Montiel Nava, The University of Texas, United StatesCopyright © 2024 Pokoski, Crain, DiGuiseppi, Furnier, Moody, Nadler, Pazol, Sanders, Wiggins and Durkin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maureen S. Durkin, bWF1cmVlbi5kdXJraW5Ad2lzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.