- 1Institute of Clinical Psychiatry, V.M.Bekhterev National Medical Research Centre for Psychiatry and Neurology, Saint Petersburg, Russia
- 2Psychiatry Department, Kirov Military Medical Academy, Saint Petersburg, Russia
- 3Department of Neurology and Manual Medicine of the Faculty of Postgraduate Education, Pavlov First Saint Petersburg State Medical University, Saint–Petersburg, Russia
- 4Neurology Department, Kirov Military Medical Academy, Saint Petersburg, Russia
- 5Department of Computer Science and Engineering, Saint-Petersburg Electrotechnical University “LETI”, Saint–Petersburg, Russia
- 6Department of Old Age Psychiatry, Institute of Psychiatry, Psychology and Neuroscience (IoPPN), King’s College London, London, United Kingdom
- 7Radio Engineering Systems Department, Saint-Petersburg Electrotechnical University “LETI”, Saint–Petersburg, Russia
- 8Research Centre “Saint Petersburg Institute of Bioregulation and Gerontology”, Saint Petersburg, Russia
- 9Institute of Postgraduate Education, V.M.Bekhterev National Medical Research Centre for Psychiatry and Neurology, Saint Petersburg, Russia
Introduction: Factors such as coronavirus neurotropism, which is associated with a massive increase in pro-inflammatory molecules and neuroglial reactivity, along with experiences of intensive therapy wards, fears of pandemic, and social restrictions, are pointed out to contribute to the occurrence of neuropsychiatric conditions.
Aim: The aim of this study is to evaluate the role of COVID-19 inflammation-related indices as potential markers predicting psychiatric complications in COVID-19.
Methods: A total of 177 individuals were examined, with 117 patients from a temporary infectious disease ward hospitalized due to COVID-19 forming the experimental group and 60 patients from the outpatient department showing signs of acute respiratory viral infection comprising the validation group. The PLR index (platelet-to-lymphocyte ratio) and the CALC index (comorbidity + age + lymphocyte + C-reactive protein) were calculated. Present State Examination 10, Hospital Anxiety and Depression Scale, and Montreal Cognitive Assessment were used to assess psychopathology in the sample. Regression and Receiver operating characteristic (ROC) analysis, establishment of cutoff values for the COVID-19 prognosis indices, contingency tables, and comparison of means were used.
Results: The presence of multiple concurrent groups of psychopathological symptoms in the experimental group was associated (R² = 0.28, F = 5.63, p < 0.001) with a decrease in the PLR index and a simultaneous increase in CALC. The Area Under Curve (AUC) for the cutoff value of PLR was 0.384 (unsatisfactory). For CALC, the cutoff value associated with an increased risk of more psychopathological domains was seven points (sensitivity = 79.0%, specificity = 69.4%, AUC = 0.719). Those with CALC > 7 were more likely to have disturbances in orientation (χ² = 13.6; p < 0.001), thinking (χ² = 7.07; p = 0.008), planning ability (χ² = 3.91; p = 0.048). In the validation group, an association (R²McF = 0.0775; p = 0.041) between CALC values exceeding seven points and the concurrent presence of pronounced anxiety, depression, and cognitive impairments was demonstrated (OR = 1.52; p = 0.038; AUC = 0.66).
Discussion: In patients with COVID-19, the CALC index may be used for the risk assessment of primary developed mental disturbances in the context of the underlying disease with a diagnostic threshold of seven points.
Introduction
The end of the coronavirus pandemic in May 2023 left many issues that could improve the health system as a whole and prepare it to face possible global challenges in the future. One such organizational issue was the provision of specialized care for patients with COVID-19 in the presence or development of comorbid pathology, particularly psychiatric (1). The conditions of the pandemic, which required the conversion of psychiatric wards into infectious disease hospitals and the reduction of face-to-face consultations, provoking a shortage of specialists in specific medical profiles, made it difficult to maintain the mental health of the population (2). Conversely, due to the difficulty of assessing mental pathology in patients with an actual infectious disease by general practitioners or infectious disease specialists, care for this population group in temporary infectious disease hospitals and outpatient services was not always provided promptly (3). At the same time, the imposition of anti-epidemic restrictions in society, fear of the pandemic, and fear of being in intensive care wards were available actual factors that contributed to the development of symptoms of mental disorders: anxiety, depression, and dyssomnia (4).
On the other hand, the role of inflammation in the development and course of mental disorders has been considered quite extensively before (5, 6). For example, in a large study conducted since 2003, it was shown that the elevated levels of C-reactive protein are associated with an increased risk of psychological distress and depression in the general population (7, 8), as well as more, specifically, the role of C-reactive protein levels has recently been discussed in the development of psychiatric complications in COVID-19 (9, 10). However, the detected neurotropism of SARS-COV-2 has raised the question of whether there is a direct link between the severity of the course of the infectious process and mental state, as well as their various bidirectional associations (4, 11, 12). A retrospective analysis of data from 62,000 cases of novel coronavirus infection revealed an increased risk of developing symptoms of psychiatric disorders, primarily anxiety, sleep disturbances, and cognitive decline in patients with advanced novel coronavirus infection, and that having a history of psychiatric diagnosis may be an independent risk factor for COVID-19 (13). In a study evaluating the association of pre-pandemic CRP levels with the likelihood of developing depressive symptoms during a pandemic, it was found that respondents with higher baseline CRP concentrations were 40% more likely to develop depressive symptoms during the pandemic (14).
However, isolated inflammatory markers cannot always predict the presence of comorbid psychiatric symptomatology (15). The use of inflammatory indices in clinical practice is effective in assessing the severity of a patient’s current condition and is predictive of possible deterioration in patients with COVID-19 (16–18). Their significant advantage, in particular, is the composition of the monitored parameters, which are not always as informative as in combination. Moreover, most of the available inflammation indices are calculated on the basis of routine laboratory and instrumental diagnostic methods, which allows them to be used almost universally (19).
Objective
The aim of this study is to evaluate the role of COVID-19 inflammation-related indices as potential markers predicting psychiatric complications in COVID-19.
Method
Materials
A total of 177 individuals were examined: 89 men (50.3%) and 88 women (49.7%). Mean age 50.9 (18.3) years [M (SD)]. One hundred seventeen inpatients from a temporary infectious disease ward for COVID-19 were included in the experimental group (66.1%) after signing their informed consent. For most of them, the main reason for hospitalization was the unfavorable course of COVID-19. Most of them also did not have any previous mental disorders (92.7% of the experimental group).
The inclusion criteria for the experimental group were as follows: 1) ability to read and understand and readiness to sign a voluntary informed consent to take part in the study; 2) a hospitalization due to COVID-19 diagnosis in a temporary infectious disease ward; and 3) ability to fulfill the study procedures (diagnostic interview). The non-inclusion criteria were as follows: 1) extremely high severity of the current condition with insufficient respiratory function and 2) age less than 18 years. The exclusion criteria were as follows: 1) absence of sufficient for the current study clinical data in medical documentation (somatic comorbidity, lymphocyte count, C-reactive protein, etc.) and 2) refusal to comply with the study procedures at any stage of the study. In this portion of the sample, the utilization of systemic indices of inflammation was tested. We evaluated the non-specific platelet-to-lymphocyte ratio (PLR) as a possible predictive index for the risk assessment of psychiatric complications development along the course of COVID-19. The rationale for its use was based on previously obtained data on the role of platelet count in the formation of various psychopathological conditions in patients with COVID-19 (20). In addition, a specific SARS-CoV-2 CALL index was evaluated in slightly modified version to settle its prognostic potential as a tool for risk assessment of psychiatric complications during COVID-19. In contrast with originally developed CALL index (19), we used comorbidity of neurological, endocrinological, or cardiovascular disorders, the age of patients, lymphocyte count, and C-reactive protein instead of lactate dehydrogenase level. Thus, the second inflammation associated index was CALC (comorbidity, age, lymphocyte, and C-reactive protein).
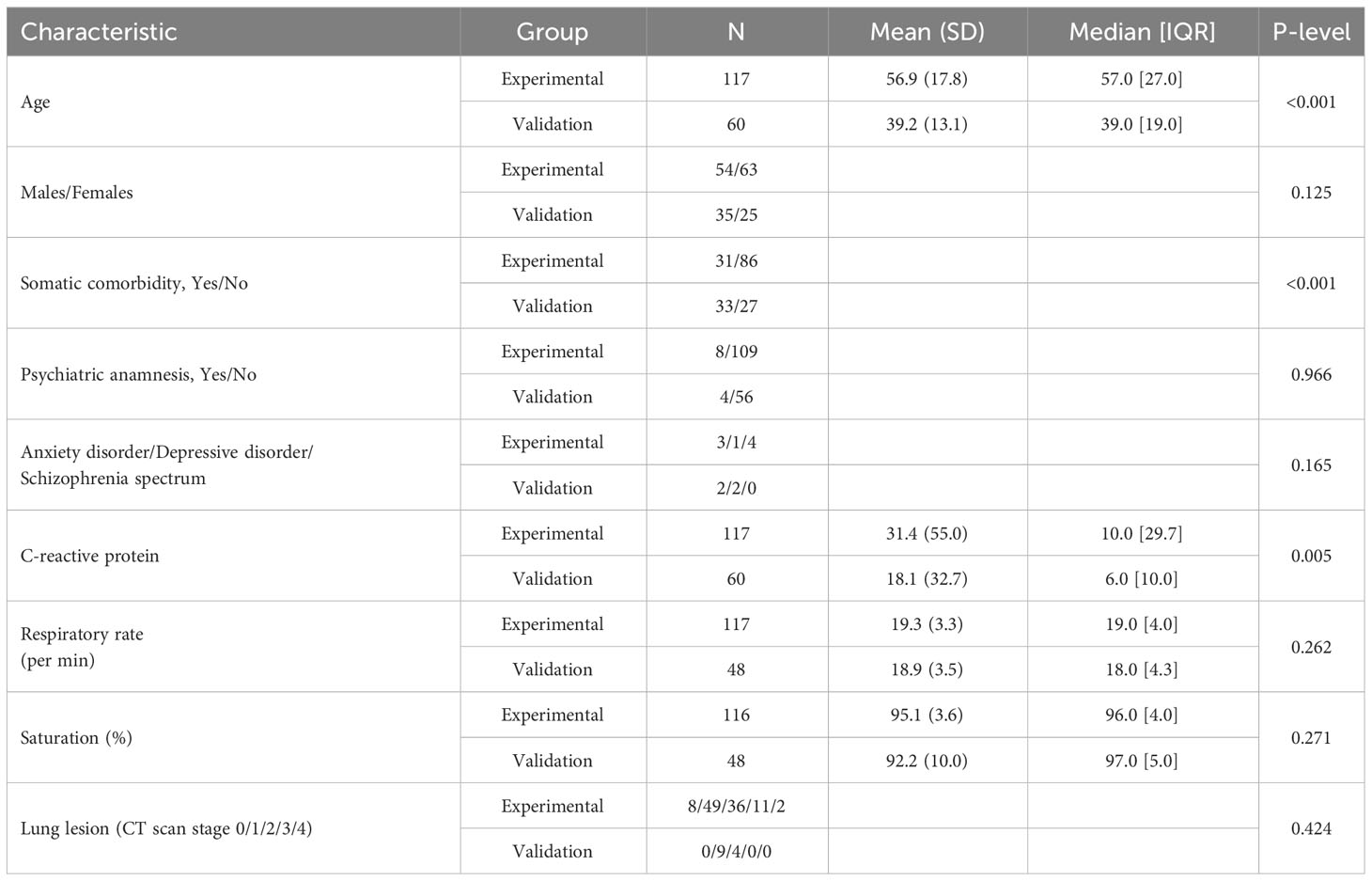
Sixty patients from the outpatient departments with signs of acute respiratory viral infection comprised the validation group (33.9%). Most of them were randomly invited to participate in the current study during an appointment with a general practitioner for outpatient treatment of an acute respiratory viral infection. Most of them also did not have any previous mental disorders (92.9% of the validation group). The inclusion, non-inclusion, and exclusion criteria for validation group were the same as that for the experimental group except the inclusion criteria # 2: outpatients of the North-West region of Russia with the presence of an acute respiratory viral infection. Forty patients in the validation group had PCR-smear or X-ray (CT-based) confirmed diagnosis of COVID-19 (66.7% of the validation group). Clinical and demographic characteristics of the experimental group and the validation group are presented in Table 1. It describes the more complicated state of inpatients in terms of demographic risk-factors (age) and general health (somatic comorbidity and C-reactive protein).
Assessments
In the experimental group, the inpatients mental state was assessed by 14 resident psychiatrists, neurologists, and psychotherapists using a semi-standardized diagnostic questionnaire, based on “Present State Examination 10” (PSE-10) with binary response options (“yes” or “no”) for specific psychopathological domains. The choice of the clinical semi-standardized interview as a psychopathological assessment tool rather than a psychometric assessment using questionnaires in experimental group was based on the high expected levels of insight decline and formal cognitive impairment in patients with COVID-19 (20, 21). PSE-10 implies that the decision about the presence or absence of a symptom is made by the physician, not the patient. This instrument assumes descriptive psychopathology as a core skill of a specialist in clinical psychiatry also (22). Inpatients in the experimental group were considered to have significant mental disorders if they exhibited disturbances in three or more psychopathological domains.
In the validation group, the prevalence and severity of anxiety and depressive symptoms were assessed using the validated version of Hospital Anxiety and Depression Scale (HADS) (23), and cognitive impairments were assessed using the Montreal Cognitive Assessment (MoCA). Outpatients in the validation group were considered to have significant mental disturbances if they scored seven or more points on the depression and anxiety sub-scales of HADS and less than 25 points on MoCA. For the uniformity of discrete psychopathological characteristics in the experimental and the validation groups, PSE-10 items 2, 3a, and 3b were taken into account to register the presence of anxiety; PSE-10 item 5 to register depressive symptoms; and PSE-10 items 6, 10a, and 13 to register cognitive disturbances in experimental group. For both groups, we calculated the patients’ PLR and the CALC index (comorbidity + age + lymphocyte + C-reactive protein). The latter one was developed on the basis of the criteria of the previously invented CALL index (19) with the lactate dehydrogenase level replaced by the C-reactive protein level.
Statistical analysis
Statistical software packages (jamovi) were used for linear regression analysis to test the overall predictive potential of PLR and CALC indices in risk assessment of psychiatric complications in COVID-19. ROC analysis in jamovi and an additional package (ppda) was employed to establish cutoff values for the COVID-19 prognosis indices. Contingency table construction and comparison of mean trends were performed to confirm the clinical significance of the established cutoffs. Finally, binomial logistic regression was used to confirm predictive power of inflammation indices with cutoffs in the independent (validation) group of patients.
The study design was controlled by an Independent Ethics Committee, and compliance with the Helsinki Declaration was confirmed in two ethical opinions: in 2020 (EK-I-132-20) and revised in 2023 (EK-I-44/23).
Results
In the experimental group, 39 patients (33.3% of the group) had three or more domains of psychopathological symptoms in their current mental state. The median number of psychopathological domains (Me [IQR]) was 1[2]. The presence of multiple concurrent groups of psychopathological symptoms in the current mental state of patients in the experimental group, based on linear regression analysis (R² = 0.28, F = 5.63, p < 0.001), was associated with a decrease in the PLR index (OR = −0.004; 95% CI, −0.007 to −0.001; p = 0.004) and a simultaneous increase in CALC (OR = 0.21; 95% CI, 0.08–0.34; p = 0.002). Lung tissue involvement, as indicated by X-ray (CT) scans, also showed associations with more groups of psychopathological symptoms: CT second stage of lung tissue involvement (OR = 1.99; 95% CI, 0.60–3.37; p = 0.005) and CT fourth stage of lung tissue involvement (OR = 2.27; 95% CI, 0.59–5.95; p = 0.017).
An increased risk of a greater number of psychopathological domains was associated with the cutoff value of 70 points for PLR. According to ROC analysis, an AUC for this model was 0.384, which is considered unsatisfactory. For CALC, the cutoff value associated with an increased risk of more psychopathological domains in current mental state was seven points, and a good AUC = 0.719 was revealed. Table 2 provides evidence supporting the choice of cutoff scores to simultaneously maximize values of sensitivity and specificity as well as the Youden’s index. Cases with PLR indices above 70 points (according to the identified cutoff) were not matched with cases with CALC indices above seven points [χ² = 0.84, d(f) = 1, p = 0.77]. Thus, both of the indices characterized clinically different cases with the more preferable predictive power of CALC (based on AUC calculation). The latter was further assessed more comprehensively.
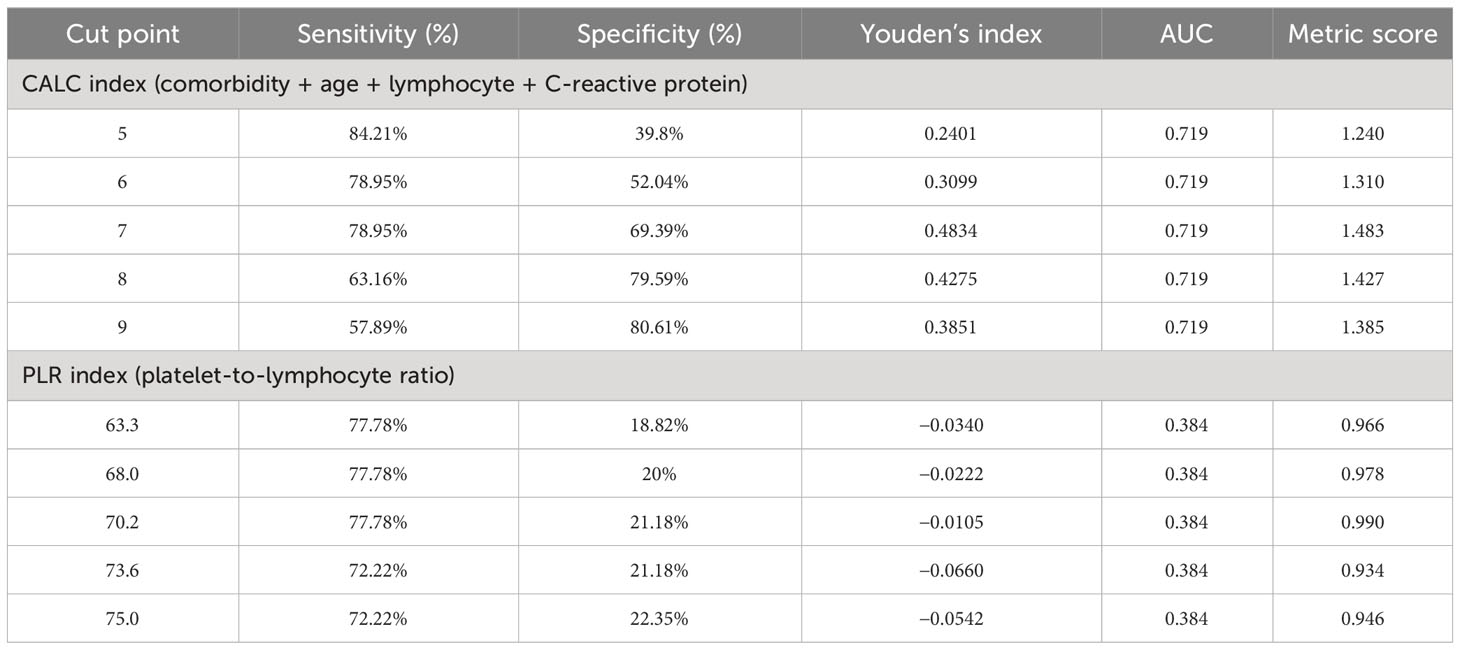
Table 2 Cutoff scores for inflammation-related measures at risk of presenting symptoms in three or more domains of psychopathology.
Inpatients with CALC values exceeding seven points were older (rrb = 0.675, p < 0.001) and then those with CALC < 7 had higher CT stage of lung lesion (rrb = 0.193, p = 0.026), higher level of C-reactive protein (rrb = 0.585, p < 0.001), and higher respiratory rate (rrb = 0.397, p < 0.001). According to the PSE-10, they had the more simultaneously presented domains of psychopathology in the current mental state (rrb = 0.204, p = 0.008) and were more likely to have disturbances in orientation [χ² = 13.6; d(f) = 1, p < 0.001], thinking [χ² = 7.07; d(f) = 1, p = 0.008], and constructive future planning ability [χ² = 3.91; d(f) = 1, p = 0.048]. It is important to note that patients with a CALC index greater than seven points were no more likely to have previously been diagnosed with mental disorders than those with a CALC < 7 [χ² = 6.07; d(f) = 3, p = 0.108]. In this sense, CALC was more related to current psychopathological symptoms than to previously presented mental illnesses.
The predictive value of the established cutoff score for CALC was independently tested in the validation group and compared with the implementation of the total CALC score. Here, 26 patients (43.3% of the validation group) had three or more domains of psychopathological symptoms according to the thresholds presented in the literature for HADS and MoCA scales. Binomial logistic regression model with total CALC score as a predictor of the presence of significant mental disturbances was insignificant (R2McF= 0.0697; p = 0.052). At the same time the other binomial logistic regression model with the dichotomous CALC value less or exceeding seven points demonstrated an association (R²McF = 0.0775; p = 0.041) between CALC values exceeding seven points (OR = 1.52; p = 0.038) and the concurrent presence of simultaneous and pronounced anxiety, depression, and cognitive disturbances. The value of AUC = 0.66 was also satisfactory for the model with dichotomous CALC (Figure 1).
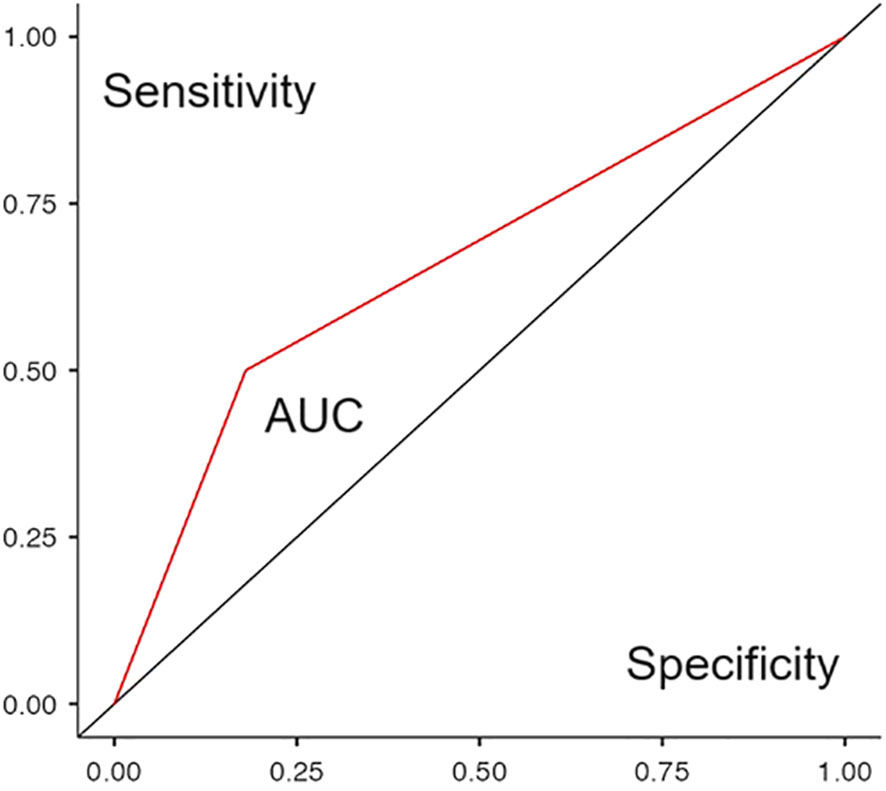
Figure 1 ROC curve of a binomial logistic regression model predicting the presence of significant mental disorders in patients of the validation group based on a dichotomous CALC value of less than or more than seven points.
Discussion
The present study demonstrated an association between serum/plasma inflammatory markers and the manifestation of psychopathological symptoms in patients undergoing acute viral infection, specifically COVID-19. The newly developed CALC index, an adaptation of the CALL index (19), exhibited good accuracy in discriminating between patients with and without psychopathological disturbances. However, the discriminative ability of another common inflammation-related index, PLR, did not prove satisfactory.
The divergence in these findings could be attributed to the more complex nature of the population’s psychopathological responses to the COVID-19 pandemic. It has been established that pre-existing psychosocial stress correlates with adverse outcomes in COVID-19 cases (24). Consequently, an index that more accurately represents the patient’s proinflammatory status, one that incorporates general health and age factors like the CALC index, is likely to demonstrate greater accuracy. In the present study, this was evidenced in both the experimental and validation cohorts.
The impact of patient demographics and historical health data on the emergence of psychopathology may be examined through the lens of a network approach to understanding psychopathology (25). This perspective posits that the phenomenological evaluation of mental disorders might rest on the systematic interplay among cognition, emotional states, and behaviors (26, 27). Previous research has also suggested the role of affective state in the presence of mild cognitive impairment in patients with COVID-19 (21). Consequently, individuals perceiving themselves as susceptible to SARS-CoV-2 infection—a notion amplified by media particularly concerning the elderly and those with pre-existing health issues—may have encountered the meditative role of psychosocial stress (28), which, along with the development of coronavirus-related inflammation, may have contributed to the higher incidence of psychopathology in the temporary infection ward.
The recent decade has witnessed a surge in studies of inflammatory biomarkers associated with psychiatric disorders. This growing body of evidence has undeniably enhanced our understanding of the mechanisms underlying mental disorders: inflammation is now known to be intertwined with glucocorticoid neurotoxicity, microglia activation, and neurogenesis (29, 30; https://www.biologicalpsychiatryjournal.com/article/S0006-3223(22)01715-2/fulltext#:~:text=Indeed%2C%20biomarkers%20of%20inflammation%20such,responses%20and%20poor%20clinical%20outcomes); however, the clinical utility of inflammatory markers is yet to be established.
This study represents an example of integrating our basic knowledge (e.g., from multiple studies of CRP associations with psychiatric conditions) with clinical data to develop a prognostic index. The CALC index has shown good discriminative properties in cross-sectional data; future studies should aim to employ longitudinal designs to ascertain the ability of inflammatory markers and indices, specifically CALC, to identify individuals at risk of psychiatric complications. The study’s main strength lies in its naturalistic, non-interventional nature and two-stage design, where the experimental group’s results were confirmed in an independent sample of patients with a similar condition. Another benefit was the ability to set a threshold for the newly developed CALC index to assess better the risk of developing psychiatric complications in patients with COVID-19.
The main limitation of the study was the incomplete number of pathophysiological and psychosocial factors assessed in the sample as possible predictors of psychopathological reactions during SARS-CoV-2 infection. This weakness, in turn, was because the sample size of inpatients who may undergo psychopathological examination in a life-threatening condition was provisionally considered to be limited. Another weakness is the assumption of a causal relationship between neuroinflammation and mental function in patients, which empirically is not always confirmed (10).
Conclusion
In patients with COVID-19, the prognosis index for the course of the infectious process, CALC (comorbidity + age + lymphocyte + C-reactive protein), may represent a valuable marker for the risk assessment of primary development of mental disorders in the context of the underlying disease. The diagnostic threshold is set at seven points for the prediction of psychiatric complications in inpatients with COVID-19.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Independent Ethics Committee of V.M.Bekhterev National Medical Research Centre for Psychiatry and Neurology. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MS: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. KM: Conceptualization, Investigation, Project administration, Writing – original draft. AT: Conceptualization, Resources, Writing – review & editing. MB: Formal Analysis, Investigation, Methodology, Writing – review & editing. DT: Resources, Writing – review & editing. AK: Formal Analysis, Resources, Writing – original draft. YS: Formal Analysis, Resources, Writing – review & editing. DM: Resources, Writing – review & editing. EZ: Conceptualization, Methodology, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Ministry of Science and Higher Education of the Russian Federation by the Agreement № 075-15-2022-291 dated 15.04.2022 on the provision of a grant in the form of subsidies from the federal budget for the implementation of state support for the establishment and development of the world-class scientific center (Pavlov center Integrative physiology for medicine, high-tech healthcare, and stress-resilience technologies).
Acknowledgments
The authors wish to thank Vladislav Rymar, Andrey Kibitov and the Young Scientists Council of the V.M. Bekhterev National Medical Research Center for Psychiatry and Neurology: Buzmakova M.V., Gorbunova O.V., Yusupov S.A., Abolmasov V.O., Repkina V.V., Gerasimchuk E.S.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Duden GS, Gersdorf S, Stengler K. Global impact of the COVID-19 pandemic on mental health services: A systematic review. J Psychiatr Res. (2022) 154:354–77. doi: 10.1016/j.jpsychires.2022.08.013
2. Radfar A, Ferreira MM, Sosa JP, Filip I. Emergent crisis of COVID-19 pandemic: mental health challenges and opportunities. Front Psychiatry. (2021) 12:631008. doi: 10.3389/fpsyt.2021.631008
3. Salukhov W, Tarumov DA, Asyamov KV, Surzhikov PV, Markin KV, et al. Experience in organizing medical care for patients with a new coronavirus infection and concomitant mental pathology in a temporary hospital. Military medical journal. (2023) 2:26–34. (In Russ.) doi: 10.52424/00269050_2023_344_2_26
4. Steardo L, Steardo L, Verkhratsky A. Psychiatric face of COVID-19. Transl Psychiatry. (2020) 10:1–12. doi: 10.1038/s41398-020-00949-5
5. Yuan N, Chen Y, Xia Y, Dai J, Liu C. Inflammation-related biomarkers in major psychiatric disorders: a cross-disorder assessment of reproducibility and specificity in 43 meta-analyses. Transl Psychiatry. (2019) 9:1–13. doi: 10.1038/s41398-019-0570-y
6. Carvalho AF, Solmi M, Sanches M, MaChado MO, Stubbs B, Ajnakina O, et al. Evidence-based umbrella review of 162 peripheral biomarkers for major mental disorders. Transl Psychiatry. (2020) 10:1–13. doi: 10.1038/s41398-020-0835-5
7. Wium-Andersen MK, Ørsted DD, Nielsen SF, Nordestgaard BG. Elevated C-reactive protein levels, psychological distress, and depression in 73, 131 individuals. JAMA Psychiatry. (2013) 70:176–84. doi: 10.1001/2013.jamapsychiatry.102
8. Pitharouli MC, Hagenaars SP, Glanville KP, Coleman JR, Hotopf M, Lewis CM, et al. Elevated C-reactive protein in patients with depression, independent of genetic, health, and psychosocial factors: results from the UK Biobank. Am J Psychiatry. (2021) 178:522–9. doi: 10.1176/appi.ajp.2020.20060947
9. Effendy E, Mardhiyah SA. Covid-19 survivors: The link between C-reactive protein and psychopathologies. IJID Regions. (2023) 8:S27–S30. doi: 10.1016/j.ijregi.2023.04.010
10. Sorokin M, Markin K, Kibitov A, Palchikova E, Zubova E. The mind-body problem in the context of neuropsychiatric symptoms in patients with coronavirus disease 2019. Alpha Psychiatry. (2023) 24:257–60. doi: 10.5152/alphapsychiatry.2023.231178
11. Raony Í, de Figueiredo CS, Pandolfo P, Giestal-de-Araujo E, Oliveira-Silva Bomfim P, Savino W. Psycho-neuroendocrine-immune interactions in COVID-19: potential impacts on mental health. Front Immunol. (2020) 11:1170. doi: 10.3389/fimmu.2020.01170
12. Bauer L, Laksono BM, Vrij FMS, Kushner SA, Harschnitz O, van Riel D. The neuroinvasiveness, neurotropism, and neurovirulence of SARS-CoV-2. Trends Neurosci. (2022) 45:358–68. doi: 10.1016/j.tins.2022.02.006
13. Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. (2021) 8:130–40. doi: 10.1016/S2215-0366(20)30462-4
14. Hamilton OS, Cadar D, Steptoe A. Systemic inflammation and emotional responses during the COVID-19 pandemic. Transl Psychiatry. (2021) 11:1–7. doi: 10.1038/s41398-021-01753-5
15. Tuna Ö, Ermis C, Enez Darcin A, Dagistan E, Salman S. Comparison of inflammation markers and severity of illness among patients with COVID-19, acute psychiatric disorders and comorbidity. Eur J Psychiatry. (2023) 37:125–32. doi: 10.1016/j.ejpsy.2022.01.008
16. Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R, et al. The systemic inflammation index on admission predicts in-hospital mortality in COVID-19 patients. Molecules. (2020) 25:5725. doi: 10.3390/molecules25235725
17. Eissa M, Shaarawy S, Abdellateif MS. The role of different inflammatory indices in the diagnosis of COVID-19. Int J Gen Med. (2021) 14:7843–53. doi: 10.2147/IJGM.S337488
18. Mangoni AA, Zinellu A. Systemic inflammation index, disease severity, and mortality in patients with COVID-19: a systematic review and meta-analysis. Front Immunol. (2023) 14:1212998. doi: 10.3389/fimmu.2023.1212998
19. Ji D, Zhang D, Xu J, Chen Z, Yang T, Zhao P, et al. Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score. Clin Infect Dis. (2020) 71:1393–9. doi: 10.1093/cid/ciaa414
20. Sorokin MY, Palchikova EI, Kibitov AA, Kasyanov ED, Khobeysh MA, Zubova EY. Mental state of inpatients with COVID-19: A computational psychiatry approach. Front Psychiatry. (2022) 13:801135. doi: 10.3389/fpsyt.2022.801135
21. Gomzyakova NA, Palchikova EI, Tumova MA, Kasyanov ED, Sorokin MY. Association of anxiety and depression with objective and subjective cognitive decline in outpatient healthcare consumers with COVID-19: А Cross-Sectional study. Consortium Psychiatricum. (2022) 3:46–57. doi: 10.17816/CP189
22. Chakraborty N. The importance of embedding psychopathology and phenomenology in clinical practice and training in psychiatry. BJPsych Adv. (2020) 26:287–95. doi: 10.1192/bja.2020.6
23. Morozova MA, Potanin SS, Beniashvili AG, Burminsky DS, Lepilkina TA, Rupchev GE, et al. Validation of the Hospital Anxiety and Depression Scale Russian-language version in the general population. Profilakticheskaya Meditsina. (2023) 2(4):7–14. (In Russ.) doi: 10.17116/profmed2023260417
24. Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, Koenen KC, et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post–COVID-19 conditions. JAMA Psychiatry. (2022) 79:1081–91. doi: 10.1001/jamapsychiatry.2022.2640
25. Bower M, Smout S, Donohoe-Bales A, O’Dean S, Teesson L, Boyle J, et al. A hidden pandemic? An umbrella review of global evidence on mental health in the time of COVID-19. Front Psychiatry. (2023) 14:1107560. doi: 10.3389/fpsyt.2023.1107560
26. Kalis A, Borsboom D. Folk psychology as a causal language. Theory Psychol. (2020) 30:723–8. doi: 10.1177/0959354320933940
27. Bringmann LF, Albers C, Bockting C, Borsboom D, Ceulemans E, Cramer A, et al. Psychopathological networks: Theory, methods and practice. Behav Res Ther. (2022) 149:104011. doi: 10.1016/j.brat.2021.104011
28. He S, Chen S, Kong L, Liu W. Analysis of risk perceptions and related factors concerning COVID-19 epidemic in Chongqing, China. J Community Health. (2020) 46:278–85. doi: 10.1007/s10900-020-00870-4
29. Bassil K, Krontira AC, Leroy T, Escoto AIH, Snijders C, Pernia CD, et al. In vitro modeling of the neurobiological effects of glucocorticoids: A review. Neurobiol Stress. (2023) 23:100530. doi: 10.1016/j.ynstr.2023.100530
Keywords: inflammation, biomarkers COVID-19, SARS-CoV-2, psychopathology, ROC curve
Citation: Sorokin M, Markin K, Trufanov A, Bocharova M, Tarumov D, Krasichkov A, Shichkina Y, Medvedev D and Zubova E (2024) Risk assessment of psychiatric complications in infectious diseases: CALCulation of prognostic indices on example of COVID-19. Front. Psychiatry 15:1341666. doi: 10.3389/fpsyt.2024.1341666
Received: 20 November 2023; Accepted: 25 January 2024;
Published: 15 February 2024.
Edited by:
Gonzalo Haro, Universidad CEU Cardenal Herrera, SpainReviewed by:
Anett Hudák, Pharmacoidea Ltd., HungaryArif Nur Muhammad Ansori, Airlangga University, Indonesia
Copyright © 2024 Sorokin, Markin, Trufanov, Bocharova, Tarumov, Krasichkov, Shichkina, Medvedev and Zubova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mikhail Sorokin, bS5zb3Jva2luQGxpc3QucnU=
 Mikhail Sorokin
Mikhail Sorokin Kirill Markin
Kirill Markin Artem Trufanov
Artem Trufanov Mariia Bocharova
Mariia Bocharova Dmitriy Tarumov
Dmitriy Tarumov Alexander Krasichkov
Alexander Krasichkov Yulia Shichkina5
Yulia Shichkina5 Dmitriy Medvedev
Dmitriy Medvedev Elena Zubova
Elena Zubova